Abstract
This study integrates previously isolated findings of nursing outcomes research into an explanatory framework in which care left undone and nurse education levels are of key importance. A moderated mediation analysis of survey data from 11,549 patients and 10,733 nurses in 217 hospitals in eight European countries shows that patient care experience is better in hospitals with better nurse staffing and a more favorable work environment in which less clinical care is left undone. Clinical care left undone is a mediator in this relationship. Clinical care is left undone less frequently in hospitals with better nurse staffing and more favorable nurse work environments, and in which nurses work less overtime and are more experienced. Higher proportions of nurses with a bachelor’s degree reduce the effect of worse nurse staffing on more clinical care left undone.
Keywords: baccalaureate nursing education, work schedule tolerance, patient satisfaction, nursing administration research, personnel staffing and scheduling
Introduction
Although the patient safety movement has emphasized systems for avoiding errors of commission in the delivery of health care (e.g., marking the wrong eye for surgery), low-quality nursing care also inheres in the omission of beneficial care (Kalisch, Landstrom, & Hinshaw, 2009). Studies in England (Ball, Murrells, Rafferty, Morrow, & Griffiths, 2014) and the United States (Sochalski, 2004) have shown that units evaluated by nurses as having lower quality of care are often those in which required patient care tasks are being missed or omitted.
Kalisch (2006) has delineated nine specific aspects of regularly missed nursing care—ambulation, turning, delayed or missed feedings, patient teaching, discharge planning, emotional support, hygiene, intake and output documentation, and surveillance—and observes that nursing staff typically attribute their omission to factors that are indicative of organizational deficiencies, including too few staff, poor use of existing staff resources, delays in nursing intervention, poor teamwork, and ineffective delegation, habit and denial (Kalisch, Doumit, Lee, & Zein, 2013; Kalisch, Tschannen, & Lee, 2011).
In this article, we elaborate the role of the provision of nursing care—specifically, the amplitude of nursing care tasks that are left undone—on the relationship between the organization of hospital nursing and care as experienced by patients. The conceptual framework underlying this study builds on the missed nursing care model by Kalisch et al. (2009) and Schubert et al.’s (2008) framework of “implicit rationing of nursing care,” which are conceptually similar extensions of Donabedian’s (1988) theory of Quality Health Care. Donabedian advanced the idea that the quality of care can be assessed by examining health care structures, processes, and outcomes. Organizational structures (hospitals, nursing units) with better work environments and better labor or capital (i.e., nurse staffing and education) achieve better patient outcomes. Work environments supportive of professional nursing practice, that is, those in which well-trained nurses have the autonomy and time to exercise maximally their professional competences in service to patient care, are critically important in providing safe, high quality patient care (Aiken et al., 2011; Aiken et al., 2012; McHugh et al., 2013). High-quality labor, indicated by better nurse staffing (or lower patient-to-nurse ratios) and higher proportions of bachelor prepared nurses, has been shown to produce better outcomes than low-quality labor (Blegen, Goode, Spetz, Vaughn, & Park, 2011). It is theorized that organizations with more favorable work environments, adequate nurse staffing levels, and a higher educated nurse workforce increase productivity, in the sense of allocating tasks more efficiently across the available labor supply, resulting in less care left undone, which in turn results in better patient outcomes. This model is tested empirically in two steps.
First, we measure the extent to which nursing care that is left undone mediates the relationship between the organization of hospital nursing and patient experiences with hospital care. The direct association between patient experiences and two key elements of the organization of hospital nursing, patient-to-nurse ratios and the character of the nurse work environment, is well-attested (Aiken et al., 2012; Kutney-Lee et al., 2009; Vahey, Aiken, Sloane, Clarke, & Vargas, 2004; You et al., 2013). In addition, the recent Registered Nurse Forecasting (RN4CAST) study (Sermeus et al., 2011), conducted in 12 European countries, demonstrates that although necessary care activities are frequently omitted in the nursing care process, this happens less often in hospitals with more favorable work environments, lower patient-to-nurse ratios, lower proportions of nurses performing nonnursing tasks, more experienced nurses, greater use of full-time nurses (Ausserhofer et al., 2014), and lower proportions of nurses working overtime (Griffiths et al., 2014). The study by Griffiths et al. also shows that overtime is associated with nurses’ reports of poor or failing patient safety and poor or fair quality of care. Researchers in the United States have found that working overtime is associated with an increased likelihood of making errors, an effect that is stronger with longer shifts (Rogers, Hwang, Scott, Aiken, & Dinges, 2004). Patient experiences with care are lower with extended shifts, and nurses are also at a higher risk of burnout (Stimpfel, Sloane, & Aiken, 2012). Patients recognize when needed care is omitted (Kalisch, McLaughlin, & Dabney, 2012), and patients’ reports of missed care correlate with adverse events and converge with nurses’ reports of missed care (Kalisch, Xie, & Dabney, 2013).
We show that relationships similar to those observed in the United States—from nursing organization and the extent of care left undone to patient care experiences—obtain in the European data as well. We then decompose the association between nursing organization and patient care experiences into the direct relationship and the portion that is mediated by the provision of nursing care. In particular, we establish the dimensions of nursing care left undone that figure most prominently in the path to lower patient care experiences.
Second, we specify and measure how the importance of care left undone, as an intervening variable, is moderated by the effects of the educational level of hospital staff nurses. Previous analyses of RN4CAST study data have shown a significant association between better educated nurses and lower patient mortality (Aiken et al., 2014), a result also found in comparable data for the United States (Aiken et al., 2011). However, these data did not show a direct effect of education on patient experiences with care (Aiken et al., 2012). Nevertheless, hospitals with a better educated nurse workforce may increase productivity, in the sense of allocating tasks more efficiently across the available labor supply. We know that similar interactions have been observed elsewhere—for example, that increases in staffing are less productive in deleterious nursing work environments than in good work environments (Aiken et al., 2011).
Our analytic model thus emphasizes the synergy between nursing education and nurse staffing. Nurses educated to at least a bachelor’s degree may be better able to mitigate the negative impacts of constraints posed on nurse staffing within a hospital (Griffiths, Maben, & Murrells, 2011). Nurse staffing levels will interact with nurse education in their effect on care left undone. It is in this sense that nursing education is a moderating factor (Baron & Kenny, 1986; James & Brett, 1984).
New Contribution
Process variables explaining why the organization of nursing care impacts care outcomes have long been theorized, but their effects have not been empirically tested through the application of appropriate statistical techniques. Advances in multilevel mediation and moderation analysis allow us to better represent statistically the evolving theory. Using quality measures that are the basis for public reporting of patients’ hospital experiences and for hospital value-based purchasing in the United States, we now provide evidence on the interrelationship between the structure, the process, and patient outcomes of nursing care. We also provide decision makers with evidence of the joint effect of nurse workload and education levels on the completion of necessary nursing care.
Method
Study Design
We analyze the cross-sectional RN4CAST study data from eight countries in which surveys of both nurses and patients on general surgical and internal medicine units were collected in 2009–2010. Patients provided information on their experiences with hospital care. Nurses provided information on nursing care in their hospital, their well-being, their last shift, and staff characteristics. For both the nurse and patient surveys, a rigorous translation procedure and cultural adaptation of items was undertaken (Squires et al., 2012; Squires et al., 2013). The full data collection protocol is described by Sermeus et al. (2011).
Measures
Patient Experiences With Hospital Care (Outcome Variables)
Patients’ overall ratings of the hospital and their willingness to recommend the hospital to friends and family, two global items derived from the U.S. Hospital Consumer Assessment of Healthcare Providers and Systems survey (Darby, Hays, & Kletke, 2005), are used as measures of patient experiences with care. Both measures are rescaled to reflect the empirical densities of responses and the modal response categories used by patients. Ratings of the hospital from 0 (worst) to 10 (best) were dichotomized to contrast ratings of 0 to 8 versus 9 to 10. For recommending the hospital to family and friends, we contrasted respondents who would definitely recommend the hospital with respondents who had reservations about doing so (probably yes, probably no, definitely no; Aiken et al., 2012; Jha, Orav, Zheng, & Epstein, 2008).
Organization of Nursing Care (Main Explanatory Variables)
Nurse staffing is calculated as the mean number of patients assigned to nurses on their last shift. The nurse work environment is defined by organizational characteristics that facilitate or constrain professional nursing practice, using the 32-item Practice Environment Scale of the Nursing Work Index (PES-NWI). This measure consists of five subscales of items rated on a 4-point scale, with responses ranging from strongly disagree to strongly agree (Lake, 2002). The mean of four subscales is used to calculate a composite nursing work environment score (Aiken et al., 2012). The four subscales reflect “collegial nurse-physician relations,” “nurse participation in hospital affairs,” “nursing foundations for quality of care,” and “nurse manager ability, leadership, and support of nurses.” A fifth subscale, which measures “staffing and resource adequacy,” was not included as it overlaps empirically with the direct measure of nurse staffing we employ in our models. The concept of nonnursing tasks performed is measured from nurses’ responses about the extent (never, sometimes, or often) to which they had performed nonnursing tasks during their last shift. Responses are categorized as often versus never or sometimes. Overtime was measured from nurses’ answers to whether or not they had worked beyond their contracted hours on the last shift they worked. We also employ measures of nurses’ type of employment (full-time, part-time) and years of experience as a nurse.
Nursing Care Left Undone (Mediating Variables)
Our construct of nursing care left undone is based on nurses’ reports of tasks that were left undone on their last shift because of lack of time, from a list of 13 nursing activities. Exploratory factor analysis was used to examine the dimensions of care left undone. Two dimensions emerged (comparative fit index = .98; Tucker–Lewis index = .95; root mean square error of approximation = .050; standardized root mean square residual = .035). The first factor contains seven items (adequate patient surveillance, skin care, oral hygiene, pain management, treatments and procedures, administering medication on time, frequently changing the patient’s position) that reflect clinical nursing care activities left undone. The second factor consists of five items that reflect planning and communication activities left undone (comfort/talk with patients, educating patients and family, preparing patients and families for discharge, developing or updating nursing care plans/ care pathways, planning care). The item “adequately documenting patient care” did not have a significant loading on any of these factors and was therefore excluded. We evaluated measurement invariance of this factor solution across the eight countries, applying progressively more stringent constraints in multiple group confirmatory factor analysis (Chen, 2007; Meredith, 1993). We found evidence of configural (invariant factor loading pattern), metric (invariant factor loadings), and scalar invariance (invariant factor intercepts) of the factor solution (Horn & McArdle, 1992). This implies that scores can be compared across countries.
Nurse Education Levels (Moderating Variable)
Nurse education was measured by the percentage of nurses in the hospital that had obtained at least a bachelor’s degree. This information was available from the nurse survey.
Hospital Structural Characteristics (Confounding Variables)
Data on hospital characteristics were provided by the hospital management using their own institutional record systems. We distinguished hospitals with respect to size (number of beds), teaching status (teaching hospital or nonteaching hospital), and technology level (with open heart surgery, organ transplantation, or both defining high-technology hospitals).
Statistical Analysis
Nurse and patient survey data and administrative data on hospital structural characteristics are linked through common identifiers at the country and hospital levels. For patients, the original data structure with patients nested within hospitals within countries is preserved, and outcomes are observable at the individual level. These are linked with aggregated (hospital-level) measures of the main explanatory, mediating, moderating, and confounding variables derived from the nurse survey and the administrative data. For the outcome measures of patients ratings of their hospital and willingness to recommend it, percentages of missing values were low, respectively, 4.3% (n = 498) and 4.5% (n = 555). The rates of missing data values from the patient survey are similar to rates in the nurse survey data. Since missing values were evenly distributed across hospitals and since these data were aggregated to the hospital level, this was not of concern in the statistical analyses.
To frame the mediation analysis we estimate the associations between (a) the main explanatory variables and the outcomes, (b) the main explanatory variables and the hypothesized mediating variables, and (c) the hypothesized mediating variables and the outcomes while also including the main explanatory variables (Baron & Kenny, 1986; MacKinnon, Fairchild, & Fritz, 2007). Statistical techniques and practical examples of (multilevel) mediation and moderated mediation models have recently been extensively discussed in organizational sciences. This study uses the framework proposed by Preacher, Rucker, and Hayes (2007). To account for the clustering of patients within hospitals within countries, our computational model includes three levels. We apply a multilevel (random intercepts) mediation model to analyze whether the two dimensions of care left undone mediate the relationship between hospital-level patient-to-nurse ratios and nursing work environments and patient experiences with care. We then specify a multilevel moderated mediation model to evaluate whether the indirect effect of patient-to-nurse ratios on patient experiences with care through the amount of care left undone remains similar across hospitals with different nurse education levels. The direct effect of care left undone on patient outcomes remains constant. The variables involved in the interaction analysis are group-mean centered, meaning that they deviate around the country mean (Enders & Tofighi, 2007). In all models, we control for hospital size, teaching status, and technology level.
Mplus Version 7.2 was used for this study (Muthén & Muthén, 2012). The three-level models were estimated using Bayesian methods, which are imposed by the statistical software for estimating this type of model. This is the first report using multilevel moderated mediation models to estimate the relationship between nursing organization of care and patient outcomes. This technique, including model fit evaluation, is discussed in more detail in the appendix. Our method of model fit evaluation was used previously in the context of Bayesian analysis in nursing outcomes research (Bruyneel et al., 2014).
Results
Descriptive Findings
Table 1 provides an overview of nurse and patient surveys that were collected in the eight European countries. We obtained data for 11,549 patients and 10,733 nurses in 217 hospitals in eight countries (Belgium, Finland, Germany, Greece, Ireland, Poland, Spain, and Switzerland).
Table 1.
Hospitals, Patients, and Nurses Sampled in Eight European Countries.
| Country | Number of hospitals | Number of nurses | Number of patients |
|---|---|---|---|
| Belgium | 60 | 2,866 | 2,623 |
| Finland | 32 | 1,131 | 1,947 |
| Germany | 12 | 504 | 244 |
| Greece | 24 | 367 | 847 |
| Ireland | 10 | 486 | 285 |
| Poland | 30 | 2,605 | 4,136 |
| Spain | 15 | 1,181 | 470 |
| Switzerland | 34 | 1,593 | 997 |
| Total | 217 | 10,733 | 11,549 |
Table 2 displays descriptive statistics for the main explanatory variables, hypothesized mediators, and patient experiences with care. The means and ranges are estimated from hospital-level data and show, for example, that nurses in the 60 hospitals in Belgium reported an average of 1.79 clinical care activities left undone and that the average ranges from 0.66 to 3.32 across the 60 hospitals. Most of these descriptive findings have been extensively discussed in previous work (Aiken et al., 2012; Aiken et al., 2014; Aiken, Sloane, Bruyneel, Van den Heede, & Sermeus, 2013; Ausserhofer et al., 2014; Griffiths et al., 2014), but the variation in nurse-reported care left undone requires additional comment. In all countries but Greece, the average number of planning and communication activities left undone is higher than the average number of clinical care activities left undone, despite being measured by two fewer items. On average, Greek nurses’ reports on clinical care left undone by far exceed those of other countries, while German nurses report the highest average number of planning and communication activities left undone. Relative to the other countries in this study, Switzerland and Finland are on average rather low on both dimensions of care left undone. Like the other explanatory variables and outcomes included in this analysis, both dimensions of care left undone vary substantially across countries and across hospitals in each country.
Table 2.
Measures Derived From the Nurse and Patient Surveys, by Country (Estimated Using Hospital-Level Data).
| Country | Nurse survey
|
Patient survey
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Patient-to-nurse ratio | Mean nurse work environment score | % Nurses with bachelor’s degree | % Nurses often performing tasks below skill level | % Nurses working beyond contracted hours | Mean number of clinical care activities left undone | Mean number of planning/communication activities left undone | % Patients rating the hospital 9 or 10 | % Patients definitely recommending the hospital | |
| Belgium | 10.88 (6.17–16.24) | 2.58 (2.30–3.11) | 53 (26–86) | 60.71 (35.90–84.09) | 37.70 (0–80.56) | 1.79 (.66–3.32) | 1.99 (.36–2.94) | 46.50 (24.56–82.76) | 58.31 (19.23–80.77) |
| Finland | 8.33 (5.26–15.64) | 2.66 (2.43–3.05) | 53 (29–77) | 21.43 (6.82–45.45) | 17.89 (3.03–37.50) | 1.31 (.15–2.92) | 1.43 (.60–2.73) | 58.70 (25.81–77.23) | 65.22 (35.71–8.00) |
| Germany | 12.95 (7.46–16.26) | 2.67 (2.45–2.91) | 0 | 60.47 (40.00–75.00) | 34.35 (25.00–51.72) | 1.76 (0.83–2.38) | 2.55 (1.83–3.48) | 47.42 (23.53–71.43) | 65.23 (17.65–85.71) |
| Greece | 10.13 (6.27–15.84) | 2.35 (1.87–2.74) | 26 (0–100) | 27.39 (0–55.56) | 30.52 (0–72.73) | 3.20 (1.27–4.29) | 2.20 (0.75–3.10) | 41.96 (15.00–76.47) | 56.64 (20.97–84.62) |
| Ireland | 6.41 (5.35–7.34) | 2.66 (2.28–3.14) | 70 (46–85) | 51.08 (41.86–68.18) | 47.06 (28.07–57.89) | 1.42 (1.00–2.15) | 2.27 (1.50–3.13) | 60.18 (36.00–80.00) | 74.10 (60.00–96.67) |
| Poland | 10.50 (7.16–14.89) | 2.44 (2.13–2.83) | 22 (5–45) | 43.86 (21.50–65.06) | 11.78 (2.35–23.68) | 1.29 (0.62–1.95) | 2.09 (1.22–2.93) | 54.17 (33.57–76.32) | 56.61 (34.43–69.75) |
| Spain | 12.60 (9.50–15.51) | 2.40 (2.06–2.67) | 100 | 16.89 (4.76–28.76) | 18.21 (4.92–42.86) | 1.39 (0.83–1.92) | 2.08 (1.51–2.73) | 34.87 (0–68.18) | 54.11 (18.52–83.33) |
| Switzerland | 7.85 (4.64–12.63) | 2.93 (2.41–3.34) | 11 (0–40) | 54.05 (32.61–94.12) | 40.78 (17.86–72.73) | 1.02 (0.45–1.88) | 1.58 (0.67–2.35) | 61.20 (36.11–100) | 76.94 (40.00–100) |
Note. The numbers in parentheses indicate the range in the means and percentages across the hospitals in each country.
Effects of Organization of Nursing Care to Patient Experiences With Care and Clinical Care Left Undone
Table 3 displays the findings from the regression analysis preceding the mediation analysis. Step 1 shows that patients report better experiences with care in hospitals with more favorable nursing work environments and lower patient-to-nurse ratios. Performing nonnursing tasks, years of experience, type of employment, and performing overtime did not relate to patient experiences with care. Step 2 shows that more favorable work environments, lower patient-to-nurse ratios, and performing less overtime significantly relate to fewer clinical nursing care tasks left undone and fewer planning and communication activities left undone. Fewer clinical care tasks left undone is also associated with more years of experience, while fewer planning and communication activities left undone related to nurses performing fewer nonnursing tasks. There was no interaction between any of these variables that explained missed nursing care. Step 3 shows that clinical care left undone is associated with patient experiences of their hospitals and their willingness to recommend them, while planning and communication activities left undone is not. Only significant effects will be included in the mediation analysis. Thus, while clinical care activities left undone will be hypothesized to mediate the effect of more favorable work environments and lower patient-to-nurse ratios on better patient experiences with care, type of employment will not be included in the model since it does not relate to patient experiences with care or to the hypothesized mediators of care left undone.
Table 3.
Coefficients From the Regression Analyses Preceding the Mediation Analysis.
| Step 1: Association between the main explanatory variables and the two outcomes
|
Step 2: Association between the main explanatory variables and the hypothesized mediating variables
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Patients recommending the hospital (patient-level outcome)
|
Patients rating the hospital (patient-level outcome)
|
Clinical care left undone (hypothesized hospital-level mediator)
|
Planning/communication left undone (hypothesized hospital-level mediator)
|
|||||
| Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | |
| Organization of nursing care (hospital-level main covariates) | ||||||||
| Nursing work environment | 0.324* | [0.081, 0.508] | 0.261* | [0.032, 0.482] | −1.636* | [−2.044, −1.248] | −0.904* | [−1.164, −0.636] |
| Patient-to-nurse ratio | −0.040* | [−0.062, −0.015] | −0.042* | [−0.064, −0.020] | 0.039* | [0.002, 0.072] | 0.051* | [0.027, 0.077] |
| Nonnursing tasks | −0.149 | [−0.540, 0.249] | −0.164 | [−0.588, 0.239] | 0.084 | [−0.410, 0.564] | 0.647* | [0.239, 1.024] |
| Years of experience | −0.004 | [−0.021, 0.014] | 0.000 | [−0.015, 0.015] | −0.030* | [−0.058, −.003] | −0.011 | [−0.031, 0.008] |
| Type of employment | −0.333 | [−0.724, 0.105] | −0.166 | [−0.595, 0.231] | 0.294 | [−0.273, 0.889] | 0.263 | [−0.160, 0.584] |
| Overtime | 0.005 | [−0.378, 0.386] | 0.168 | [−0.197, 0.527] | 1.332* | [0.578, 1.984] | 0.582* | [0.010, 1.075] |
|
| ||||||||
| Step 3: Associations between the two hypothesized mediating variables and the two outcomes, from models including the main explanatory variables | ||||||||
|
| ||||||||
| Est. | 95% CI | Est. | 95% CI | |||||
|
| ||||||||
| Clinical care left undone | −0.194* | [−0.309, −.075] | −0.144* | [−0.255, −0.050] | ||||
| Planning/communication left undone | −0.013 | [−0.148, 0.113] | −0.038 | [−0.161, 0.080] | ||||
Note. Est. = estimate; CI = credibility interval;
indicates statistical significance.
Mediation Effects
Table 4 shows the regression coefficients estimated in the mediation analyses. The amount of clinical care left undone partially mediates the effects of patient-to-nurse ratios and work environment on patients recommending the hospital. It also partially mediates the effect of patient-to-nurse ratios on patient ratings of their hospitals, and fully mediates the effect of work environments on patient ratings of their hospitals. This can be seen from the non-significant association between work environment and patient ratings of their hospitals.
Table 4.
Findings for the Eight-Country Mediation Analyses Estimating the Indirect Effect of Nursing Work Environments and Patient-to-Nurse Ratios on Patient Experiences With Care Through Clinical Care Left Undone.
| Patients recommending the hospital (patient-level outcome)
|
Patients rating the hospital (patient-level outcome)
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical care left undone (hospital-level mediator) |
Planning/communication left undone (hospital-level outcome) |
Patient experience (patient-level outcome) |
Clinical care left undone (hospital-level mediator) |
Planning/communication left undone (hospital-level outcome) |
Patient experience (patient-level outcome) |
|||||||
| Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | |
| Organization of nursing care (hospital-level main covariates) | ||||||||||||
| Nursing work environment | −1.740* | [−2.127, −1.369] | −0.904* | [−1.164, −0.667] | 0.246* | [0.152, 0.341] | −1.736* | [−2.109, −1.389] | −0.890* | [−1.142, −0.636] | 0.151 | [−0.126, 0.318] |
| Patient-to-nurse ratio | 0.037* | [0.006, 0.073] | 0.051* | [0.030, 0.075] | −0.027* | [−0.055, −0.002] | 0.037* | [0.003, 0.071] | 0.051* | [0.027, 0.076] | −0.033* | [−0.055, −0.010] |
| Nonnursing tasks | — | — | 0.402* | [0.002, 0.734] | — | — | — | — | 0.387* | [0.042, 0.725] | — | — |
| Years of experience | −0.031* | [−0.057, −0.008] | — | — | — | — | −0.031* | [−0.057, −0.006] | — | — | — | — |
| Overtime | 1.165* | [0.613, 1.694] | 0.579* | [0.175, 0.948] | — | — | 1.169* | [0.614, 1.687] | 0.561* | [0.166, 0.953] | — | — |
| Care left undone (hospital-level mediator) | ||||||||||||
| Clinical care left undone | −0.163* | [−0.269, −0.070] | −0.168* | [−0.257, −0.088] | ||||||||
| Indirect effects | ||||||||||||
| Work environment on patient experience, through clinical care left undone | 0.280* | [0.112, 0.509] | 0.289* | [0.147, 0.470] | ||||||||
| Staffing on patient experience, through clinical care left undone | −0.006* | [−0.014, −0.001] | −0.006* | [−0.014, 0.000] | ||||||||
Note. Est. = estimate; CI = credibility interval;
indicates statistical significance.
Moderated Mediation Effects
Table 5 provides the estimated regression coefficients from the moderated mediation models for the two patient outcomes, which extends the mediation analyses by introducing nurse education level as a moderating variable. Clinical care left undone mediates the effect of nurse staffing levels on both patient outcomes differently depending on the proportion of nurses trained to a bachelor’s degree. The significant interaction effect in the upper part of Table 5 indicates that the effect of having higher hospital patient-to-nurse ratios on clinical care left undone is smaller in hospitals with higher proportions of nurses with at least a bachelor’s degree. These findings of moderated mediation are illustrated in the path diagram in Figure 1. This graphical representation follows Donabedian’s (1988) triad depiction of structure, process, and outcome and Edwards and Lambert’s (2007) display of first stage moderated mediation. The lower part of Table 5 shows that the extent to which clinical care left undone mediates the effect of nurse staffing is conditional on nurse education levels. The conditional indirect effect is statistically significant only for hospitals with lower than average nurse education levels. The mediation effect with regard to nursing work environment found previously was included in the moderated mediation analysis and remained stable. As described in the appendix, model fit was acceptable.
Table 5.
Findings for the Eight-Country Moderated Mediation Analyses Estimating the Effect of Nurse Education on the Relationship Between Patient-to-Nurse Ratios on Patient Experiences With Care Through Clinical Care Left Undone.
| Patients recommending the hospital (patient-level outcome)
|
Patients rating the hospital (patient-level outcome)
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical care left undone (hospital-level mediator) |
Planning/communication left undone (hospital-level outcome) |
Patient experience (patient-level outcome) |
Clinical care left undone (hospital-level mediator) |
Planning/communication left undone (hospital-level outcome) |
Patient experience (patient-level outcome) |
|||||||
| Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | |
| Organization of nursing care (hospital-level main covariates) | ||||||||||||
| Nursing work environment | −1.658* | [−2.024, −1.309] | −0.893* | [−1.154, −0.621] | 0.087* | [−0.096, 0.329] | −1.661* | [−2.026, −1.285] | −0.893* | [−1.142, −0.639] | 0.205* | [0.029, 0.358] |
| P/N | 0.042* | [0.007, 0.076] | 0.051* | [0.027, 0.075] | −0.029* | [−0.053, −0.005] | 0.042* | [0.007, 0.075] | 0.051* | [0.028, 0.075] | −0.033* | [−0.055, −0.011] |
| NE | 0.142 | [–0.501, 0.767] | — | — | 0.067 | [−0.301, 0.424] | .130 | [-.510, 0.761] | — | — | −0.056 | [−0.387, 0.284] |
| P/N * NE interaction | −0.416* | [−0.669, −0.160] | — | — | −0.081 | [−0.240, 0.083] | −0.418* | [−0.687, −0.161] | — | — | 0.034 | [−0.113, 0.179] |
| Nonnursing tasks | — | — | 0.390* | [0.050, 0.733] | — | — | — | — | 0.386* | [0.049, 0.733] | — | — |
| Years of experience | −0.034* | [−0.060, −0.008] | — | — | — | — | −0.034* | [−0.060, −0.009] | — | — | — | — |
| Overtime | 1.110* | [0.555, 0.1669] | 0.566* | [0.192, 0.951] | — | — | 1.102* | [0.584, 1.630] | 0.567* | [0.173, 0.963] | — | — |
| Care left undone (hospital-level mediator) | ||||||||||||
| Clinical care left undone | −0.205* | [−0.308, −0.103] | −0.154* | [−0.242, −0.069] | ||||||||
| Indirect effects | ||||||||||||
| Work environment on patient experience through clinical care left undone | 0.337* | [0.166, 0.536] | 0.253* | [0.113, 0.417] | ||||||||
| Conditional indirect effects at range of minimum to maximum deviation around group mean | ||||||||||||
| Effect of education on the indirect effect of staffing on patient experience through clinical care left undone | ||||||||||||
| −0.30 | −0.032* | [−0.062, −0.012] | −0.025* | [−0.049, −0.009] | ||||||||
| −0.20 | −0.024* | [−0.046, −0.010] | −0.019* | [−0.036, −0.007] | ||||||||
| −0.10 | −0.016* | [−0.031, −0.006] | −0.012* | [−0.024, −0.004] | ||||||||
| 0.0 | −0.008* | [−0.018, −0.001] | −0.006* | [−0.014, −0.001] | ||||||||
| 0.10 | 0.000 | [−0.009, 0.009] | 0.000 | [−0.007, 0.007] | ||||||||
| 0.20 | 0.008 | [−0.004, 0.023] | 0.006 | [−0.003, 0.018] | ||||||||
| 0.30 | 0.016 | [0.000, 0.039] | 0.012 | [0.000, 0.025] | ||||||||
Note. Est. = estimate; CI = credibility interval; P/N = patient-to-nurse ratio; NE = nurse education;
indicates statistical significance.
Figure 1.
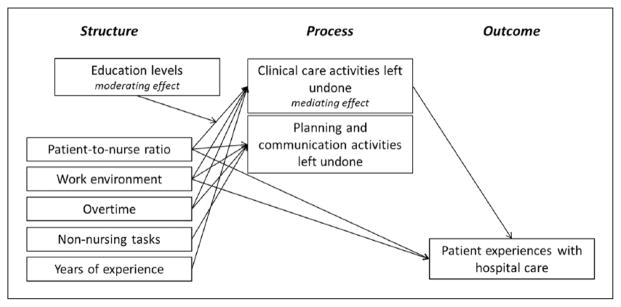
Path diagram illustrating (a) the relationship between work environments and patient experiences with care through clinical care left undone (mediator) and (b) the effect of nurse education (moderator) on the relationship between patient-to-nurse ratios and patient experiences with care through clinical care left undone (mediator).
Sensitivity Analysis
Several sensitivity analyses were performed to evaluate these findings. First, we tested for configural similarity of our construct relations across levels (Chen & Bliese, 2005). We aggregated the main covariates, mediators, and moderator to the nursing unit level (n = 887), rather than the hospital level, and again linked them to patient experience data using common unit identifiers. Significance tests and the direction of effects were consistent with the hospital-level analysis. This suggests that our theory and findings are homologous across levels. Second, results were also consistent when we used the original values for staffing and education in the moderated mediation analyses instead of group-mean centered values. Third, all analyses that included nurse education levels were repeated omitting the two countries with no variation in nurse education across hospitals (Germany and Spain). Omitting the two countries did not alter our findings.
Discussion
Nursing- and patient-oriented health services researchers should align the theoretical basis for their research with appropriate statistical techniques (Griffiths, 2009; Levy, Landerman, & Davis, 2011; Mark, 2006; Mark, Hughes, & Jones, 2004). This article responds to those calls by empirically testing a more comprehensive conceptualization of the mechanisms underlying the association between patient experiences with care and the organizational context of nursing care. Our findings showed that higher patient-to-nurse ratios, worse work environments, and higher proportions of nurses working overtime lead to more clinical care activities left undone as well as more planning and communication activities left undone. Previous reports using the RN4CAST study data have shown that nurses all over Europe report having performed nonnurs-ing care and tasks below their skill level during their last shift (Bruyneel et al., 2013). Our findings suggest that, partly as a consequence of this, planning and communication activities are being omitted rather than clinical care activities. Our findings also showed that the omission of planning and communication activities, while decidedly more common than the omission of clinical care, did not affect patient experiences. Work by Kalisch et al. (2012) has shown that patients are able to partially or fully report on missed nursing care activities that are comparable to the items included in our dimension of planning and communication activities. “Preparing patients and families for discharge” was included in their study as “Discharge planning” (fully reportable) and “Educating patients and family” as “Patient education” (partially reportable). It could be argued that for some items included in the planning and communication dimension, it is unclear whether patients recognize them, particularly “developing or updating nursing care plans/care pathways” and “planning care.” On the other hand, omitting these tasks might lead to disorganized patient care, which patients would be able to recognize. Thus, our findings might suggest that patient recognition of omitted planning and communication activities and their consequences does not necessarily result in lower ratings or recommendations of the hospital, whereas this is the case with respect to clinical nursing care left undone. Future studies of the expectations of patients regarding professional hospital care would help confirm this.
Findings on the moderating effect of nurse education suggest that in hospitals with relatively low proportions of nurses with at least a bachelor’s degree, the positive effect of better staffing on patient experiences with hospital care, which occurs partly through reduced clinical care left undone, may be undermined. Bachelor prepared nurses have a wider range of skills and competencies and might especially increase the productivity of the nursing labor through better planning of nursing care and priority setting, which in turn results in lower nursing care activities undone. Important to note is that nurse education seems not equivalent across individual and organizational levels. A multicountry analysis of RN4CAST study data at the individual nurse level showed that nurses with a bachelor’s degree had higher reports of missed nursing care (Ausserhofer et al., 2014). A U.S. study did not find such association (Kalisch, Tschannen, Lee, & Friese, 2011). Repeating the 12-country RN4CAST analysis, we also did not find such effects for the organizational construct of nurse education, neither when we linked in to an organizational-level construct (hospital or nursing unit) of care left undone nor when we related it to care left undone at the individual nurse level. Moreover, our findings on the interaction between nurse staffing and education also support our belief that evaluating such interaction effects leads to more tangible conclusions than studying the effect of the proportion of bachelor educated nurses on outcomes in multiple regressions also including nurse staffing, but without an interaction effect.
Our findings suggest that patient experiences are an indicator of quality deficiencies in structures and processes of nursing care. A reasonable evolution of our findings would be to systematically register care activities left undone, to complement the already widely implemented reports on nursing care performed. This would provide a more complete understanding of care intensity and productivity, and illuminate actionable interventions to improve nurse work environments. Second, quality improvement strategies to efficiently allocating nurses’ time and resources should be more widely implemented. The Productive Ward—Releasing Time to Care Programme, which is based on lean methodology, is one strategy that is drawing increased attention in this regard. This program aims to provide staff with more time to provide direct patient care and offers 15 modules to optimize the organization of patient care (Wilson, 2009). Another critically acclaimed frontline project is Transforming Care at the Bedside, which also aims to increase time spent in direct patient care. Transforming Care at the Bedside is designed for medical and surgical nursing units in hospitals where it aims to empower nurses in redesigning work processes (The Robert Wood Johnson Foundation, & The Institute for Healthcare Improvement, 2007).
Last, this study provides additional support for national and European policy makers to fund international research agendas that focus on the quality of human capital in health care. Appropriate steps need to be taken to increase the proportion of hospital nurses with a bachelor’s degree, in line with propositions made in the United States (Institute of Medicine Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing at the Institute of Medicine, 2011).
Limitations
Our findings and policy implications assume that the associations we have uncovered are causal, though firm evidence of this is lacking since the data employed are cross-sectional. Omitted variable bias may have occurred by not including elements of nurse wellbeing, which has also been shown to link with the main explanatory variables used in this study and with patient experiences with care. We also did not study whether the same effects persist across morning, day and night shifts, or across shifts with different lengths. While random effects were included for the hospital and country level, we cannot conclude that all findings could exactly be replicated in each country individually.
Conclusions
This is the first study to explicate within an integrative theoretical and statistical framework that patient experiences with care comprise a critical overview of both the structure and process of nursing care. It is shown that less clinical care activities left undone and higher proportions of bachelor-prepared nurses exert important effects in patients denoting nursing excellence. These findings reinforce the need for nursing management to implement process improvement strategies that aim for nurses spending more time on direct patient care. Hospital hiring policies should reflect the growing body of research associating bachelor-educated nurses with safe, high quality patient care.
Acknowledgments
RN4CAST Consortium: Walter Sermeus (Director), Koen Van den Heede, Luk Bruyneel, Emmanuel Lesaffre, Luwis Diya (Belgium, Katholieke Universiteit Leuven); Linda Aiken (Codirector), Herbert Smith, Douglas Sloane (U.S.A., University of Pennsylvania); Anne Marie Rafferty, Jane Ball, Simon Jones (U.K., King’s College London); Peter Griffiths (U.K., University of Southampton); Juha Kinnunen, Anneli Ensio, Virpi Jylhä (Finland, University of Eastern Finland); Reinhard Busse, Britta Zander, Miriam Blümel (Germany, Berlin University of Technology); John Mantas, Dimitrios Zikos, Marianna Diomidous (Greece, University of Athens); Anne Scott, Anne Matthews, Anthony Staines (Ireland, Dublin City University); Ingeborg Strømseng Sjetne (Norway, Norwegian Knowledge Centre for the Health Services); Inger Margrethe Holter (Norway, Norwegian Nurses Organization); Tomasz Brzostek, Maria Kózka, Piotr Brzyski (Poland, Jagiellonian University Collegium Medicum); Teresa Moreno-Casbas, Carmen Fuentelsaz-Gallego, Esther Gonzalez-María, Teresa Gomez-Garcia (Spain, Institute of Health Carlos III); Carol Tishelman, Rikard Lindqvist, Lisa Smeds (Sweden, Karolinska Institute); Dietmar Ausserhofer, Sabina De Geest, Maria Schubert, René Schwendimann (Switzerland, Basel University); Maud Heinen, Lisette Schoonhoven, Theo van Achterberg (Netherlands, Radboud University Nijmegen Medical Centre).
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research received funding from the European Union’s Seventh Framework Programme (FP7/2007-2013, Grant Agreement No. 223468, Walter Sermeus, PI) and the National Institute of Nursing Research, National Institutes of Health (R01NR004513, Linda H. Aiken, PI).
Appendix
Three-Level Mediation Model
The equation for the three-level mediation model equals
where yijk represents the binary score measured on patient i from hospital j in country k. The link function is probit, which corresponds to the inverse of the cumulative distribution function of the standard normal distribution. xjk is the nurse staffing variable at the hospital level with coefficient βx. zjk is the measure of nursing work environment at the hospital level with coefficient βz. mjk represents the two potential hospital-level missed nursing care mediators with coefficient vector βm. cjk represents the vector of all other hospital-level covariates included with βc the coefficient vector. ujk and uk represent the random effects at the hospital level and country level, respectively. In the models of the mediators, xjk and zjk are included with the coefficients γx and γz, respectively.
Replacing m1jk and m2jk, we get
βx is the direct effect of x and β1γ1x and β2γ2x are its indirect effects via the hospital-level mediators m1 and m2, respectively. Similarly, βz is the direct effect of z and β1γ1z and β2γ2z are its indirect effects via m1 and m2, respectively.
Three-level moderated mediation model
The equation for the three-level moderated mediation analysis equals
where yijk represents the binary score measured on patient i from hospital j in country k. xjk is the nurse staffing variable at the hospital level with coefficient βx. mjk represents the two potential hospital-level missed nursing care mediators with coefficient βm. wjk is the hospital-level moderator with the coefficient βm. βxw is the interaction effect of xjk and wjk . cjk represents the vector of all other hospital-level covariates included with βc the coefficient vector. ujk and uk represent the random effects at the hospital level and country level, respectively. In the model of the mediator mjk, covariates xjk, wjk, and their interaction are included with the respective coefficients γx, γw, and γxw.
Replacing mjk, we get
βx + βxwwjk is the direct effect of x with βxwwjk the moderator effect, while βmγx + βmγxwwjk is its indirect effect with βmγxwwjk the moderator effect in the first path.
Model Fit Evaluation
The default noninformative priors in Mplus were used, that is, a normal prior of mean zero and variance 5 for all β parameters (β0, , βx, βz, , βw, βxw), a normal prior of mean zero and variance 1010 for all γ parameters (γ0, γx, γz, γw, γxw), and an improper inverse gamma prior which corresponds to a uniform distribution of (0, +∞) for all variance parameters ( ). Given the large sample size, the priors are not very crucial in our case. The convergence of all parameters is assessed by the potential scale reduction factor (PSRF; Gelman & Rubin, 1992), which should be smaller than 0.01 for all parameters in the model. Model fit was evaluated by using the mixed posterior predictive check (PPC) suggested by Marshall and Spiegelhalter (2003). The mixed PPC first generates the predictive values for the random effects. The final PPC (uses mean as discrepancy function) is subsequently based on the posterior estimates of the fixed effects and the predictive values of the random effects. This is said to be able to overcome the overoptimistic problem of the classic PPC that is based on the posterior estimates of all effects for hierarchical models. We obtain posterior predictive p-values (PPp) for each of the 32 PES-NWI items within each nursing unit. From this, we generate quantile-quantile (QQ) plots of the PPps for each item across all nursing units against the uniform distribution of (0,1). A uniform distribution suggests an acceptable model fit. As displayed in the Appendix Figure, the QQ plots did not violate the uniform distribution.

Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Aiken LH, Cimiotti JP, Sloane DM, Smith HL, Flynn L, Neff DF. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Medical Care. 2011;49:1047–1053. doi: 10.1097/MLR.0b013e3182330b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, Kutney-Lee A. Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. British Medical Journal. 2012;344:e1717. doi: 10.1136/bmj.e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, Sermeus W. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet. 2014;383:1824–1830. doi: 10.1016/S0140-6736(13)62631-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Sermeus W. Nurses’ reports of working conditions and hospital quality of care in 12 countries in Europe. International Journal of Nursing Studies. 2013;50:143–153. doi: 10.1016/j.ijnurstu.2012.11.009. [DOI] [PubMed] [Google Scholar]
- Ausserhofer D, Zander B, Busse R, Schubert M, De Geest S, Rafferty AM, Schwendimann R. Prevalence, patterns and predictors of nursing care left undone in European hospitals: Results from the multicountry cross-sectional RN4CAST study. BMJ Quality & Safety. 2013;23:126–135. doi: 10.1136/bmjqs-2013-002318. [DOI] [PubMed] [Google Scholar]
- Ball J, Murrells T, Rafferty AM, Morrow E, Griffiths P. “Care left undone” during nursing shifts: Associations with workload and perceived quality of care. BMJ Quality & Safety. 2014;23:116–125. doi: 10.1136/bmjqs-2012-001767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Blegen MA, Goode CJ, Spetz J, Vaughn T, Park SH. Nurse staffing effects on patient outcomes: Safety-net and non-safety-net hospitals. Medical Care. 2011;49:406–414. doi: 10.1097/MLR.0b013e318202e129. [DOI] [PubMed] [Google Scholar]
- Bruyneel L, Li B, Aiken LH, Lesaffre E, Van den Heede K, Sermeus W. A multi-country perspective on nurses’ tasks below their skill level: Reports from domestically trained nurses and foreign trained nurses from developing countries. International Journal of Nursing Studies. 2013;50:202–209. doi: 10.1016/j.ijnurstu.2012.06.013. [DOI] [PubMed] [Google Scholar]
- Bruyneel L, Li B, Squires A, Spotbeen S, Meuleman B, Lesaffre E, Sermeus W. Bayesian multilevel MIMIC modeling for studying measurement invariance in cross-group comparisons. Medical Care. 2014 doi: 10.1097/MLR.0000000000000164. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling. 2007;14:464–504. [Google Scholar]
- Chen G, Bliese PD. Conceptual framework and statistical procedures for delineating and testing multilevel theories of homology. Academy of Management Annual Meeting Proceedings. 2005;8:A1–A6. [Google Scholar]
- Darby C, Hays RD, Kletke P. Development and evaluation of the CAHPS hospital survey. Health Services Research. 2005;40:1973–1976. doi: 10.1111/j.1475-6773.2005.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donabedian A. The quality of care. How can it be assessed? Journal of the American Medical Association. 1988;260:1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- Edwards JR, Lambert LS. Methods for integrating moderation and mediation: A general analytical framework using moderated path analysis. Psychological Methods. 2007;12(1):1–22. doi: 10.1037/1082-989X.12.1.1. [DOI] [PubMed] [Google Scholar]
- Enders CK, Tofighi D. Centering predictor variables in cross-sectional multilevel models: A new look at an old issue. Psychological Methods. 2007;12:121–138. doi: 10.1037/1082-989X.12.2.121. [DOI] [PubMed] [Google Scholar]
- Gelman A, Rubin DB. Inference from iterative simulation using multiple sequences. Statistial Science. 1992;7:457–472. [Google Scholar]
- Griffiths P. RN + RN = better care? What do we know about the association between the number of nurses and patient outcomes? International Journal of Nursing Studies. 2009;46:1289–1290. doi: 10.1016/j.ijnurstu.2009.07.007. [DOI] [PubMed] [Google Scholar]
- Griffiths P, Dall’Ora C, Simon M, Ball J, Lindqvist R, Rafferty AM, Aiken LH. Nurses’ shift length and overtime working in 12 European countries: The association with perceived quality of care and patient safety. Medical Care. 2014;52:975–981. doi: 10.1097/MLR.0000000000000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths P, Maben J, Murrells T. Organisational quality, nurse staffing and the quality of chronic disease management in primary care: Observational study using routinely collected data. International Journal of Nursing Studies. 2011;48:1199–1210. doi: 10.1016/j.ijnurstu.2011.03.011. [DOI] [PubMed] [Google Scholar]
- Horn JL, McArdle JJ. A practical and theoretical guide to measurement invariance in aging research. Experimental Aging Research. 1992;18:117–144. doi: 10.1080/03610739208253916. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing at the Institute of Medicine. The future of nursing: Leading change, advancing health. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- James LR, Brett JM. Mediators, moderators, and tests for mediation. Journal of Applied Psychology. 1984;69:307–321. [Google Scholar]
- Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. New England Journal of Medicine. 2008;359:1921–1931. doi: 10.1056/NEJMsa0804116. [DOI] [PubMed] [Google Scholar]
- Kalisch BJ. Missed nursing care: A qualitative study. Journal of Nursing Care Quality. 2006;21:306–313. doi: 10.1097/00001786-200610000-00006. [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Doumit M, Lee KH, Zein JE. Missed nursing care, level of staffing, and job satisfaction: Lebanon versus the United States. Journal of Nursing Administration. 2013;43:274–279. doi: 10.1097/NNA.0b013e31828eebaa. [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Landstrom GL, Hinshaw AS. Missed nursing care: A concept analysis. Journal of Advanced Nursing. 2009;65:1509–1517. doi: 10.1111/j.1365-2648.2009.05027.x. [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, McLaughlin M, Dabney BW. Patient perceptions of missed nursing care. Joint Commission Journal on Quality and Patient Safety. 2012;38:161–167. doi: 10.1016/s1553-7250(12)38021-5. [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Tschannen D, Lee KH. Do staffing levels predict missed nursing care? International Journal for Quality in Health Care. 2011;23:302–308. doi: 10.1093/intqhc/mzr009. [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Tschannen D, Lee KH, Friese CR. Hospital variation in missed nursing care. American Journal of Medical Quality. 2011;26:291–299. doi: 10.1177/1062860610395929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalisch BJ, Xie B, Dabney BW. Patient-reported missed nursing care correlated with adverse events. American Journal of Medical Quality. 2013;29:415–422. doi: 10.1177/1062860613501715. [DOI] [PubMed] [Google Scholar]
- Kutney-Lee A, McHugh MD, Sloane DM, Cimiotti JP, Flynn L, Neff DF, Aiken LH. Nursing: A key to patient satisfaction. Health Affairs. 2009;28:w669–w677. doi: 10.1377/hlthaff.28.4.w669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET. Development of the practice environment scale of the Nursing Work Index. Research in Nursing & Health. 2002;25:176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- Levy JA, Landerman LR, Davis LL. Advances in mediation analysis can facilitate nursing research. Nursing Research. 2011;60:333–339. doi: 10.1097/NNR.0b013e318227efca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark BA. Methodological issues in nurse staffing research. Western Journal of Nursing Research. 2006;28:694–709. doi: 10.1177/0193945905277354. [DOI] [PubMed] [Google Scholar]
- Mark BA, Hughes LC, Jones CB. The role of theory in improving patient safety and quality health care. Nursing Outlook. 2004;52(1):11–16. doi: 10.1016/j.outlook.2003.10.010. [DOI] [PubMed] [Google Scholar]
- Marshall EC, Spiegelhalter DJ. Approximate cross-validatory predictive checks in disease mapping models. Statistics in Medicine. 2003;22:1649–1660. doi: 10.1002/sim.1403. [DOI] [PubMed] [Google Scholar]
- McHugh MD, Kelly LA, Smith HL, Wu ES, Vanak JM, Aiken LH. Lower mortality in magnet hospitals. Medical Care. 2013;51:382–388. doi: 10.1097/MLR.0b013e3182726cc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith W. Measurement invariance, factor analysis and factorial invariance. Psychometrika. 1993;58:525–543. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 7. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- The Robert Wood Johnson Foundation, & The Institute for Healthcare Improvement. A new era in nursing: Transforming care at the bedside. 2007 Retrieved from http://www.rwjf.org/content/dam/files/legacy-files/article-files/2/TCABBrochure041007.pdf.
- Rogers AE, Hwang WT, Scott LD, Aiken LH, Dinges DF. The working hours of hospital staff nurses and patient safety. Health Affairs. 2004;23:202–212. doi: 10.1377/hlthaff.23.4.202. [DOI] [PubMed] [Google Scholar]
- Schubert M, Glass TR, Clarke SP, Aiken LH, Schaffert-Witvliet B, Sloane DM, De Geest S. Rationing of nursing care and its relationship to patient outcomes: The Swiss extension of the International Hospital Outcomes Study. International Journal for Quality in Health Care. 2008;20:227–237. doi: 10.1093/intqhc/mzn017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sermeus W, Aiken LH, Van den Heede K, Rafferty AM, Griffiths P, Moreno-Casbas MT, Zikos D. Nurse forecasting in Europe (RN4CAST): Rationale, design and methodology. BMC Nursing. 2011;10:6. doi: 10.1186/1472-6955-10-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sochalski J. Is more better? The relationship between nurse staffing and the quality of nursing care in hospitals. Medical Care. 2004;42(2 Suppl):II67–II73. doi: 10.1097/01.mlr.0000109127.76128.aa. [DOI] [PubMed] [Google Scholar]
- Squires A, Aiken LH, van den Heede K, Sermeus W, Bruyneel L, Lindqvist R, Matthews A. A systematic survey instrument translation process for multi-country, comparative health workforce studies. International Journal of Nursing Studies. 2013;50:264–273. doi: 10.1016/j.ijnurstu.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squires A, Bruyneel L, Aiken LH, Van den Heede K, Brzostek T, Busse R, Sermeus W. Cross-cultural evaluation of the relevance of the HCAHPS survey in five European countries. International Journal for Quality in Health Care. 2012;24:470–475. doi: 10.1093/intqhc/mzs040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stimpfel AW, Sloane DM, Aiken LH. The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Affairs. 2012;31:2501–2509. doi: 10.1377/hlthaff.2011.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse burnout and patient satisfaction. Medical Care. 2004;42(2 Suppl):II57–II66. doi: 10.1097/01.mlr.0000109126.50398.5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson G. Implementation of releasing time to care: The productive ward. Journal of Nursing Management. 2009;17:647–654. doi: 10.1111/j.1365-2834.2009.01026.x. [DOI] [PubMed] [Google Scholar]
- You L, Aiken LH, Sloane DM, Liu K, He G, Hu Y, Sermeus W. Hospital nursing, care quality, and patient satisfaction: Cross-sectional surveys of nurses and patients in hospitals in China and Europe. International Journal of Nursing Studies. 2013;50:154–161. doi: 10.1016/j.ijnurstu.2012.05.003. [DOI] [PubMed] [Google Scholar]


