Abstract
Background
Gender differences in the prevalence of alcohol use disorder (AUD) have motivated the separate study of its risk factors and consequences in men and women. However, leveraging gender as a third variable to help account for the association between risk factors and consequences for AUD could elucidate etiological mechanisms and clinical outcomes.
Method
Using data from a large, community sample followed longitudinally from ages 17 to 29, we tested for gender differences in psychosocial risk factors and consequences in adolescence and adulthood after controlling for gender differences in the base rates of AUD and the psychosocial factor. Psychosocial factors included alcohol use, other drug use, externalizing and internalizing symptoms, deviant peer affiliation, family adversity, academic problems, attitudes and use of substances by a romantic partner, and adult socio-economic status.
Results
At both ages 17 and 29, mean-levels of psychosocial risks and consequences were higher in men and those with AUD. However, the amount of risk exposure in adolescence was more predictive of AUD in women than men. By adulthood, AUD consequences were larger in women than men and internalizing risk had a stronger relationship with AUD in women at both ages.
Conclusion
Despite higher mean-levels of risk exposure in men overall, AUD appears to be a more severe disorder in women characterized by higher levels of adolescent risk factors and a greater magnitude of the AUD consequences among women than men. Furthermore, internalizing symptoms appear to be a gender specific risk factor for AUD in women.
Relative to women, men consume alcohol more frequently and in greater quantities, and so have higher rates of alcohol use disorder (AUD) (DSM-IV abuse, 24.6%; dependence, 17.4%) than women (abuse, 11.5%; dependence, 8.0%) (Keyes et al., 2008). These differences have encouraged the separate study of risk exposure and outcomes in men and women; however, leveraging gender as a third variable to help account for the association between psychosocial factors and AUD may advance understanding of etiological mechanisms and clinical outcomes (Rutter et al., 2003).
Two types of gender effects—mean-level and structural—help to organize our understanding of the links among gender, AUD, and important psychosocial variables. Mean-level gender effects (i.e., the main effect of gender) refer to the absolute amount or severity of risk exposure experienced by men and women with AUD (e.g., a risk factor may occur at a higher rate in men than women). Another important source of gender differences are structural effects or the strength of the association between a risk factor and AUD within each gender. In particular, gender differences in both AUD and a psychosocial variable can obscure gender's moderating effects (i.e., interaction effects). For instance, a psychosocial variable could have a stronger association with AUD in one gender than the other, irrespective of mean-level gender differences for that variable. Risk factors with strong structural effects on AUD may be more potent in one gender and, consequently, require a lower mean-level of exposure to produce AUD. By controlling for the mean-level effect of gender, the strength of the association between AUD and each psychosocial variable (i.e., interaction effects) can be estimated directly.
Delineating the mean-level and structural effects of gender for multiple psychosocial variables can increase insight regarding the accumulation of impairment across different domains that may comprise gender-specific pathways for AUD. Further, evaluating mean-level and structural effects at key developmental periods for AUD will help identify patterns of psychosocial impairment that contribute to the onset and persistence of AUD. Specifically, late adolescence (when early onset AUD cases emerge) and young adulthood (when drinking reduces and serious consequences accumulate if AUD persists) are particularly informative periods to examine how gender differences in early risk factors and consequences of AUD underlie gender difference in its prevalence.
Common Risk Factors and Outcomes for AUD
AUD represents the end point in a long history of biological, psychosocial, and environmental risk factors interacting and accumulating over the course of development (Blazei et al., 2006; Zucker, 2006; Caspi et al., 1995, 1996; Masse & Tremblay 1997; Wong et al., 2006). Importantly, these variables may exhibit gender differences in their mean-level and structural associations with AUD. For example, behavioral disinhibition—a heritable cluster of disinhibited personality traits and externalizing disorders (Moffitt et al., 2001; Rutledge & Sher, 2001; Krueger et al., 2002; Slutske et al., 2002, Kendler et al., 2003)—increases the odds of early onset AUD and other problem behaviors (e.g., drug use, delinquency, precocious sexual behavior; Iacono et al., 2008; Hawkins et al., 1992; Iacono et al., 2008). A cycle of coercive parent-child interactions, conflict with socializing agents (e.g., teachers and prosocial peers) and affiliation with deviant peers (Dishion et al., 1991; Tangney et al., 1996; Patterson & Yoerger, 1997, 1999; Granic & Patterson, 2006) also contributes to AUD and related adult impairment (e.g., unemployment, romantic partnership problems, and life satisfaction; Cranford et al., 2011). Other non-specific risk factors for AUD include internalizing disorders and exposure to traumatic life events like physical and sexual abuse and assault (Cutler & Nolen-Hoeksema, 1991; Widom et al., 1995; Wilsnack et al., 1997; Kilpatrick et al., 2000; Nolen-Hoeksema & Hilt, 2006). While these patterns of risk and consequences are generally associated with AUD, there may be gender differences in their mean-level and the strength of their association with AUD (i.e., structural effects). Examining the nature of gender differences in risk factors and consequences can help explain the prevalence, etiological course, and relative severity of AUD.
Gender Differences in Mean-levels of Risk Factors for AUD
The greater prevalence of AUD in men suggests that men experience higher mean-levels of risk exposure than women (i.e., between-gender differences in those with AUD). To express AUD, then, a woman must be more deviant relative to the norm for her gender (i.e., within-gender mean-level effects) than a man. Therefore, elucidating gender differences in the risks and consequences for AUD requires comparing men and women with alcohol use problems to those of the same gender that do not (e.g., AUD women vs non-AUD women). However, risk factors are often studied individually using between-gender comparisons of mean-level effects, making it difficult to discern their relative contributions to the development of AUD in men and women (Labouvie & McGee, 1986; Waldeck & Miller, 1997; Moffitt et al., 2001; Petry et al., 2002). For example, though mean-levels of behavioral disinhibition and sexual trauma vary significantly by gender, both are equally predictive of AUD in boys and girls (Moffit et al., 2001; Iacono et al., 2008; Stein et al., 1988; Cutler & Nolen-Hoeksema, 1991). Studies conducting between-gender comparisons of a single factor are not well-equipped to test the etiological importance of these factors as gender-specific pathways to AUD. Within-gender comparisons of mean-levels of risk between those with and without AUD estimates the importance of a risk factor on AUD separately for men and women. These comparisons are vital for identifying which risk factors are more predictive of AUD in men relative to women.
Gender Differences in Structural Associations between AUD Risk Factors and Consequences
An additional cause of gender differences in AUD is that psychosocial factors may have different structural associations with AUD in men and women. Notably, the association (e.g., correlation) between AUD and several psychosocial factors differs across gender. For example, alcohol's rewarding effects have been linked with AUD in men (Schuckit, 1994; Wilhelmsen et al., 2003) while, the lower threshold for alcohol-related impairment and toxicity in women has been conceptualized as a deterrent of heavy drinking (Klassen & Wilsnack, 1986; Niaura et al., 1987; Nixon, 1994; Blume & Russell, 2001). Also, internalizing disorders may play a more prominent role in the development of AUD among women (Nolen-Hoeksema, 2004). For example, even after controlling for higher rates of depression in women relative to men, depressive symptoms have been prospectively associated with AUD in women (Kendler et al., 1997; Brady & Randall, 1999; Sannibale & Hall, 2001). Finally, even among those who desist by young adulthood, a greater proportion of women than men exhibit enduring consequences of AUD, including prolonged polysubstance abuse, psychiatric problems, and poor psychosocial adjustment (Hicks et al., 2010; Foster et al., 2014). As such, AUD may be less prevalent in women because it is a more extreme form of psychopathology, requiring a greater loading of risk before the disorder is expressed. These findings suggest then that gender-specific associations between AUD and its risk factors may contribute to gender differences in the prevalence of AUD.
Leveraging Gender Differences to Study the Etiology of AUD
Research on AUD has often been constrained within gender under the assumption that the link between AUD and its risks and consequences differs by gender. Consequently, few studies have compared the relative effects of multiple risk factors and outcomes for AUD in men and women in the same study. Without such tests, it is unclear if psychosocial risks and outcomes are simply more prevalent in one gender, or if gender-specific influences increase their association with AUD in one gender more than the other. To examine the potential moderating role of gender, we directly compared the effects of several well-replicated risk factors for and outcomes of AUD in a large, community sample of men and women at ages 17 and 29. Specifically, separately for men and women, we first estimated the odds of developing AUD by age 29 given the mean level of risk evident for each age-17 risk factor after controlling for gender differences in the average amount of exposure to the risk factor within each gender. We then estimated the association between AUD and several psychosocial outcomes at age 29, after adjusting for gender differences in the base rates of AUD and the psychosocial outcome. We hypothesized that mean-level but not structural gender effects would be present across risk factors. One exception, however, was internalizing disorders for which we predicted a stronger association with AUD in women relative to men.
Method
Sample
Participants were male (n=578) and female (n=674) twins of the Minnesota Twin and Family Study (MTFS), a prospective, community-based study designed to investigate the etiology of substance use disorders (for extensive details on study design see Iacono et al., 1999). Twin pairs born between the years of 1972 and 1979 were recruited from Minnesota public birth records at age 17. Of the 90% of families located, 83% completed the in-person laboratory assessment at the University of Minnesota. Nearly all participants were of European American ancestry (96%) and were similar to non-participating families in parental occupation, education, and history of mental health treatment.
Assessment
At the age 17 assessment, multiple informants (twins, parents, and teachers) provided information on alcohol and other substance use along with psychiatric, psychosocial, and environmental functioning. Follow-up assessments occurred every 3–5 years at the target ages of 20 (n = 1110, 89% retention rate, 83% of men and 93% of women), 24 (n = 1159, 92% retention rate, 94% of men and 91% of women) and 29 years old (n =1164, 93% retention rate, 91% of men and 94% of women). The current report focused on risk factors and domains of psychosocial functioning at ages 17 and 29 (Hicks et al., 2009, 2010) to assess both risk and outcomes for lifetime AUD by age 29. More comprehensive descriptions of the measures are provided elsewhere (Hicks et al., 2009, 2010).
AUD Diagnosis
Trained staff administered the Substance Abuse Module (SAM; Robins et al., 1987) of the Composite International Diagnostic Interview (Robins et al., 1988) to determine lifetime AUD status at age 17. Subsequent evaluations assessed AUD symptoms since the last assessment. Consistent with DSM-5, AUD was defined as 2 or more symptoms of alcohol abuse or dependence for at least one assessment by age 29 (men, n=316; women, n=155). Multiple studies using the MTFS sample have demonstrated the validity of this approach (Elkins et al., 2004; McGue & Iacono, 2005; Elkins et al., 2006; Elkins et al. 2007). For each gender, an AUD group was compared with a non-AUD group (i.e., no more than one AUD symptom at any assessment; men, n=226; women, n=449) on the risk factors and outcomes.
Measures of Risk and Impairment
Prior studies using the MTFS sample have linked several measures of risk and consequences with AUD in both genders (Hicks et al., 2010; Foster et al., 2014). Using principal components analysis and theoretical considerations, we combined variables into composites (i.e., mean z-score across constituent variables) to assess critical domains of AUD risk exposure and impairment at age 17 and age 29. Whenever possible, the same measures were used to assess each factor at ages 17 and 29. However, certain domains were age-specific including family adversity and academic problems in adolescence (age 17 only) and romantic partner relationships and socio-economic status in adulthood (age 29 only).
Alcohol, nicotine and illicit substance use
Alcohol use was assessed using past year average quantity and the maximum number of drinks consumed in 24 hours. Nicotine and illicit drug use were estimated using DSM-IV symptoms of nicotine dependence and abuse/dependence for illicit drugs, along with quantity and frequency of use and the number of drug classes tried. Substances assessed included nicotine, amphetamine, cannabis, cocaine, hallucinogen, inhalant, opioid, PCP, and sedatives. The illicit drug class with the greatest number of reported symptoms was used for each participant's drug abuse/dependence variable.
Externalizing symptoms
At age 17, symptoms of adult antisocial behavior were assessed using a structured interview similar to the SCID-II module for antisocial personality disorder. Personality traits of disinhibition were assessed using the behavioral constraint (i.e., inclination toward planning, traditional social values, and caution) factor of the Multidimensional Personality Questionnaire (MPQ; Tellegen & Waller, 2008). At age 29, symptoms of adult antisocial behavior over the past 6-years were assessed in conjunction with behavioral constraint.
Internalizing distress
Internalizing distress was assessed using lifetime symptoms of major depressive disorder, negative emotionality, and significant mental health problems (i.e., prior suicide attempts, mental health treatment, or psychiatric hospitalization). Symptoms of major depression were assessed using the Structured Clinical Interview for DSM-III-R. Trait negative emotionality (i.e., propensity toward breakdown under stress and a suspicious, aggressive interpersonal style) was assessed using the MPQ. Mental health problems were assessed using the Lifetime Events Interview (Bemmels et al., 2008). At age 29, the same variables were used to estimate internalizing distress (i.e., major depression symptoms, mental health problems over the past 6 years, and negative emotionality scores).
Deviant peer group affiliation
Adolescent peer groups were assessed for antisocial (α = 0.82; e.g., my friends enjoy getting drunk, get into fights, can't seem to hold a job) and prosocial behaviors (α = 0.60; e.g., my friends work hard, do volunteer work, have a regular job) using a teacher rating form (5-items each; Walden et al., 2004). At age 29, participants reported antisocial (coded positive) and prosocial (coded negative) qualities of their own peer group (27-item questionnaire).
Family adversity
At age 17, family adversity was indexed by socioeconomic status for the family of origin, quality of the parent-child relationship, and parental externalizing disorder symptoms. Socio-economic status was defined as the mean z-score for each parent's years of education, occupational status (Hollingshead Index) and annual income. The Parent Environment Questionnaire (PEQ; Elkins et al., 1997) measured quality of the parent-child relationship from each parent and adolescent (mean z-score of the three informant ratings for the first principle component of the PEQ scales; Hicks et al., 2009). Parental externalizing disorders were indexed using the symptoms of antisocial personality disorder and alcohol, nicotine, and drug abuse/dependence.
Academic problems
At age 17, difficulties in school were assessed using the Academic History Questionnaire (Johnson et al., 2006) that queried mother and child for cumulative grade point average and positive engagement with academics (7-items; α = 0.83).
Adult romantic partner drug use
Participants in a current romantic relationship (i.e., married, cohabiting, or consistently dating the same person for 3 months or more) at age 29 reported their partner's past year drinking patterns including the frequency, quantity and proportion of intoxicating drinking episodes and attitudes toward substance use (e.g., “my spouse/partner would be upset if he knew I was smoking”; “my spouse/partner would purchase alcohol if I asked him to”; “my spouse's/partner's friends use marijuana”) using an 11-item scale (α = 0.84).
Adult socio-economic status
Measures of educational attainment, a Hollingshead rating of current occupational status, and annual income all reported in the Life Events Interview and the Social Adjustment Inventory were used to create a composite for socio-economic status.
Statistical Analysis
A series of hierarchical linear models were fit to estimate the associations between AUD, Gender and the risk factors assessed at age 17. Generalized estimating equations were used to model the associations between adolescent risk exposure and the odds of developing AUD by age 29 in men and women using the following model:
Data for this model were mean-centered within each gender to facilitate interpretation as follows. The main effect of gender (γ10) was the increase in the odds of AUD by age 29 given gender status and an average level of risk exposure for that gender (e.g., increase in odds for men compared to women, given average levels of risk within men and women). The main effect for the risk factor (γ20) was estimated as the increase in the odds of AUD by age 29 given a 1 SD increase in risk exposure. The Gender x Risk interaction term (γ30) tested whether the association between AUD and the risk factor was moderated by gender. Models were fit using the Bernoulli option in HLM 7.0 specifically designed to predict binary outcomes (i.e., AUD or non-AUD by age 29 in this case). Data were nested within families (γ00) to adjust for the non-independence of the twin data and any non-normal distributions for the risk factor variables. A residual term was also included (μ0j) to account for variation in the outcome not accounted for by the predictor variables.
At age 29, we estimated the associations between lifetime AUD, gender, and several psychosocial consequences using the following model:
This model included the main effects of gender (γ10) and AUD status (γ20) and the Gender x AUD interaction (γ30) in the prediction of each psychosocial outcome at age 29. Parameters were adjusted for other variables in the model so that the effect of gender on the outcome was adjusted for AUD vs. non-AUD group differences in outcome, while the effect of AUD was adjusted for gender differences on the outcome. The Gender x AUD interaction term tested whether gender moderated the association between AUD and the adult outcome. Models for age 29 outcome variables were fit using the cluster option and the MLR estimator in Mplus 5.0 that is appropriate for continuous outcomes (i.e., degree of the risk outcome). All standard errors and p-values were adjusted for the non-independence of the family-level data (i.e., nested by γ00) and any non-normal distributions for risk factor variables. A residual term was also included (μ0j) to account for variance in the outcome independent of gender, AUD, and their interaction.
Results
Over a third of the sample (n=471, 37.6%) reported 2 or more symptoms of AUD at one or more assessments by age 29. In our sample, lifetime AUD was more prevalent among men than women (Odds Ratio [OR]: 2.37, 95% Confidence Interval [CI]: 1.90–2.90).
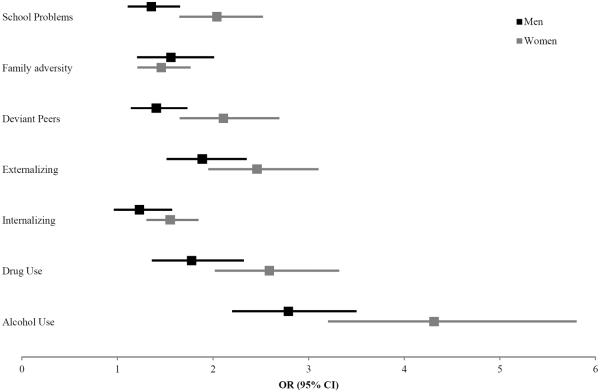
Risk Exposure at Age 17 and Lifetime AUD Outcomes by Gender
Results for the main effects of Gender, Risk factor, and the Gender x Risk factor interaction terms at age 17 are reported in Table 1. The average level of risk exposure common to boys at age 17 significantly increased odds of developing AUD relative to the average level of risk exposure common to girls at 17. The significant main effects of risk exposure at age 17 indicated that higher levels of risk increased the odds of developing AUD by age 29. Within both men and women, a 1 SD increase in alcohol use, other drug use, externalizing problems, deviant peers, family adversity and academic problems increased the odds of AUD. Internalizing distress at age 17 was associated with increased odds of AUD in women (OR: 1.55, 95% CI: 1.30–1.85, p < 0.001) but not men (OR: 1.23, 95% CI: 0.96–1.57, p = 0.098), suggesting a gender-specific risk factor for AUD. Finally, the association between each risk exposure and AUD was stronger for women except for family adversity, suggesting that similar increases in risk for both genders are linked with more severe consequences in women compared to men (see Figure 1). For instance, a 1 SD increase in drug use was associated with a greater increase in the odds of AUD in women (OR: 2.59, 95% CI: 2.02–3.32) compared to men (OR: 1.78, 95% CI: 1.36–2.32). Consequently, we detected Gender x Risk factor interactions for alcohol use, other substance use, deviant peers, and academic problems, such that greater risk exposure on these variables had a significantly stronger association with AUD in women relative to men.
Table 1.
T-score means, standard deviations, Cohen's d, and results for the generalized estimating equation using risk factors at age 17 and gender to predict the odds of developing AUD by age 29.
| Gender Difference | AUD Status by Age 29 | Risk Effect at age 17 | Gender Effect (men vs. women) | Risk x Gender | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Predictors at 17 | Overall | da | Control | AUD | db | β (SE) | OR | 95% CI | β (SE) | p-value |
| Alcohol Use | ||||||||||
| Total | 50.0 (10.0) | 46.4 (6.2) | 56.1 (12.0) | 1.02 | ||||||
| Women | 48.6 (7.9) | 46.4 (5.6) | 55.1 (9.9) | 1.09 | 1.46 (0.15) | 4.31** | 3.20–5.80 | |||
| Men | 52.3 (12.0) | 0.36 | 46.3 (7.2) | 56.5 (12.9) | 0.98 | 1.02 (0.12) | 2 79** | 2.19–3.54 | 1.78 (0.16)** | 0.025† |
| Other Drug Use | ||||||||||
| Total | 50.0 (10.0) | 47.6 (6.3) | 53.5 (13.0) | 0.58 | ||||||
| Women | 50.1 (9.8) | 47.7 (5.7) | 56.9 (14.9) | 0.82 | 0.95 (0.12) | 2.59** | 2.02–3.32 | |||
| Men | 50.0 (10.3) | −0.01 | 47.4 (7.3) | 51.9 (11.6) | 0.46 | 0.57 (0.13) | 1.78** | 1.36–2.32 | 1.51 (0.15)** | 0.043† |
| Externalizing | ||||||||||
| Total | 50.0 (10.0) | 47.2 (7.3) | 54.7 (11.7) | 0.77 | ||||||
| Women | 48.0 (9.1) | 46.1 (7.0) | 53.5 (12.0) | 0.76 | 0.90 (0.12) | 2.46** | 1.95–3.10 | |||
| Men | 52.8 (10.5) | 0.49** | 49.3 (7.6) | 55.2 (11.6) | 0.61 | 0.63 (0.11) | 1.89** | 1.51–2.35 | 1.56 (0.15)** | 0.112 |
| Internalizing | ||||||||||
| Total | 50.0 (10.0) | 48.8 (9.3) | 51.5 (10.2) | 0.28 | ||||||
| Women | 50.0 (11.1) | 48.9 (10.0) | 54.7 (13.1) | 0.51 | 0.43 (0.08) | 1.55** | 1.30–1.85 | |||
| Men | 49.5 (8.0) | 0.09 | 48.7 (7.7) | 50.0 (8.1) | 0.16 | 0.20 (0.12) | 1.23 | 0.96–1.57 | 1.45 (0.15)** | 0.129 |
| Deviant Peers | ||||||||||
| Total | 50.0 (10.0) | 48.1 (8.5) | 52.5 (11.0) | 0.45 | ||||||
| Women | 49.8 (9.3) | 48.2 (8.4) | 54.8 (10.2) | 0.71 | 0.74 (0.12) | 2.11** | 1.65–2.69 | |||
| Men | 50.0 (10.4) | 0.02 | 48.0 (8.7) | 51.5 (11.2) | 0.35 | 0.34 (0.10) | 1.41* | 1.14–1.73 | 1.55 (0.16)** | 0.014† |
| Family Adversity | ||||||||||
| Total | 50.0 (10.0) | 48.6 (9.6) | 51.6 (9.9) | 0.32 | ||||||
| Women | 50.0 (11.0) | 48.8 (10.6) | 53.3 (11.6) | 0.40 | 0.37 (0.09) | 1.46** | 1.21–1.76 | |||
| Men | 49.7 (8.4) | −0.02 | 48.1 (7.4) | 50.9 (8.9) | 0.35 | 0.44 (0.12) | 1.56* | 1.21–2.01 | 1.45 (0.15)** | 0.687 |
| Academic Problems | ||||||||||
| Total | 50.0 (10.0) | 47.8 (9.0) | 52.9 (10.5) | 0.53 | ||||||
| Women | 48.6 (9.7) | 46.8 (8.9) | 53.6 (10.1) | 0.71 | 0.71 (0.10) | 2.03** | 1.65–2.52 | |||
| Men | 51.4 (10.0) | 0.28 | 49.6 (8.8) | 52.6 (10.7) | 0.30 | 0.30 (0.10) | 1.35* | 1.11–1.65 | 1.47 (0.15)** | 0.006* |
p < 0.001,
p < 0.01,
p < 0.05,
T-score means arranged by gender and AUD status (Women: n=155 AUD, 449 control; Men: n=316 AUD, 226 non-AUD) reflect mean-level of risk exposure for each group at age 17. Cohen's d effect sizes estimate the magnitude of the difference in the average level of risk between males and females overall (i.e., all Men vs. all Women; da). and the change in risk exposure coinciding with AUD in each gender (e.g., Control Women vs. AUD Women; db). The Risk Effect for each gender estimates the increased odds of developing AUD by age 29 as a result of a 1 SD increase in risk exposure for a person of that gender (i.e., potency of the risk). The Gender Effect estimates the increase in odds of developing AUD by age 29 in men compared to women given an average level of risk exposure within each gender. Positive β-value denotes higher odds in men compared to women. The Risk x Gender interaction effect tested if gender moderated the relationship between the risk factor and the AUD outcome.
Figure 1.
Odds of developing AUD by age 29 for each one SD increase from average level of risk exposure for a person of that gender at age 17.
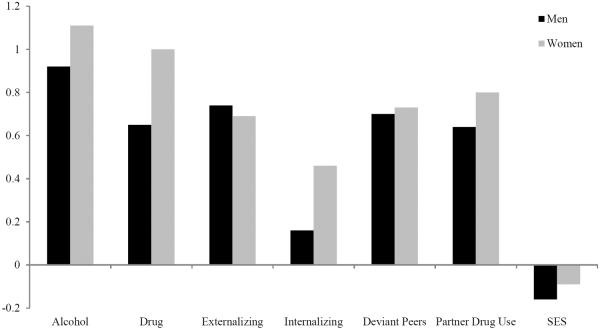
Consequences of AUD at Age 29
Results for the main effects for Gender, AUD, and the Gender x AUD interactions for the age 29 outcomes are reported in Table 2. Lifetime AUD predicted greater alcohol consumption, nicotine and illicit drug use, internalizing distress, externalizing problems, deviant peer affiliation and substance use by a romantic partner at age 29. Men exhibited significantly greater alcohol use, other substance use, externalizing symptoms, deviant peer affiliation, and socioeconomic status. Women reported greater partner substance use. Although mean-level comparisons at age 29 suggest men with AUD were more impaired than women with AUD, the difference in psychosocial outcome between non-AUD and AUD groups was larger among women than men for alcohol use, drug use, internalizing, deviant peers, and romantic partner drug use. That is, AUD coincided with greater overall decrements in functioning among women than men compared to those of the same gender without the disorder (see Figure 2). For example, the effect size of AUD on other drug use was larger in women (d = 1.00) relative to men (d = 0.65). We also detected a Gender x AUD interaction for internalizing distress, such that the differences between AUD and non-AUD groups was greater among women than men.
Table 2.
T-Score means, standard deviations, Cohen's d, and β-value using AUD status and gender to predict psychosocial functioning at age 29.
| AUD Status by age 29 | AUD Effect | Gender Effect | AUD x Gender | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Criterion at age 29 | Overall | Control | AUD | da | β-value | db | β-value | β-value |
| Alcohol Use | ||||||||
| Total | 50.0 (10.0) | 46.0 (6.9) | 56.5 (10.7) | 1.17** | 0.43** | 0.84** | 0.24** | 0.01 |
| Women | 46.6 (7.7) | 44.4 (5.4) | 53.2 (9.7) | 1.11** | ||||
| Men | 54.5 (10.8) | 49.2 (8.5) | 58.1 (10.8) | 0.92** | ||||
| Other Drug Use | ||||||||
| Total | 50.0 (10.0) | 46.9 (6.8) | 54.7 (12.0) | 0.82** | 0.40** | 0.37† | 0.08† | −0.05 |
| Women | 48.5 (8.0) | 46.4 (5.8) | 54.8 (10.0) | 1.00** | ||||
| Men | 51.7 (11.6) | 47.8 (8.9) | 54.7 (12.8) | 0.65** | ||||
| Externalizing | ||||||||
| Total | 50.0 (10.0) | 46.8 (8.1) | 55.0 (10.6) | 0.87** | 0.29** | 0.75** | 0.22** | 0.06 |
| Women | 46.7 (8.4) | 45.3 (7.4) | 51.1 (9.5) | 0.69** | ||||
| Men | 53.8 (10.3) | 49.7 (8.6) | 56.9 (10.5) | 0.74** | ||||
| Internalizing | ||||||||
| Total | 50.0 (10.0) | 48.9 (8.9) | 51.4 (11.0) | 0.26** | 0.27** | −0.08 | −0.02 | −0.18* |
| Women | 50.3 (10.6) | 49.0 (9.3) | 54.3 (13.3) | 0.46** | ||||
| Men | 49.5 (8.9) | 48.7 (8.2) | 50.1 (9.3) | 0.16 | ||||
| Deviant Peers | ||||||||
| Total | 50.0 (10.0) | 47.0 (8.8) | 54.8 (9.7) | 0.84** | 0.32** | 0.60** | 0.17** | 0.01 |
| Women | 47.5 (9.1) | 45.9 (8.4) | 52.4 (9.4) | 0.73** | ||||
| Men | 53.2 (10.1) | 49.3 (9.3) | 56.0 (9.7) | 0.70** | ||||
| Romantic Partner Drug Use | ||||||||
| Total | 50.0 (10.0) | 48.2 (9.4) | 52.9 (10.1) | 0.48** | 0.38** | −0.36** | −0.25** | −0.09 |
| Women | 51.5 (10.1) | 49.3 (9.5) | 57.5 (10.0) | 0.80** | ||||
| Men | 48.1 (9.3) | 44.8 (8.5) | 50.5 (9.2) | 0.64** | ||||
| Socio-economic Status | ||||||||
| Total | 50.0 (10.0) | 50.2 (10.3) | 49.7 (9.3) | −0.05 | −0.05 | 0.20* | 0.14* | −0.03 |
| Women | 49.1 (10.1) | 49.3 (10.2) | 48.4 (9.8) | −0.09 | ||||
| Men | 51.0 (9.6) | 52.0 (10.3) | 50.3 (8.9) | −0.16† | ||||
p < 0.001,
p < 0.01,
p < 0.05,
T-score means arranged by gender and AUD status (Women: n=155 AUD, 449 control; Men: n=316 AUD, 226 non-AUD) reflect mean-level of consequences for each group at age 29. Cohen's d effect sizes estimate the magnitude of the change in consequence factor coinciding with AUD in each gender (i.e., Control Women vs. AUD women) and the difference in each mean-level consequence between men and women at age 29 (i.e., all Men vs. all Women; db). The AUD Effect estimates the level of consequences at age 29 associated with lifetime AUD status compared to control status. The Gender effect estimates the difference in consequences at age 29 for men compared to women. The AUD x Gender interaction effect tests if gender moderates the relationship between AUD and consequences at age 29.
Figure 2.
Cohen's d effect sizes for the main effect of AUD within each gender at age 29.
Discussion
The higher prevalence of AUD in men relative to women suggests that mean-levels of risk exposure for AUD are either greater in men or that certain risk factors have differential effects across gender. To test the moderating role of gender, we estimated the strength of the association between AUD and several established risk factors and negative outcomes after adjusting for gender differences in their prevalence. Our results confirmed the hypothesis that women with AUD have a greater loading of risk at age 17 and that AUD increases mean-levels of psychosocial impairment in young adulthood for both men and women, but that internalizing distress has a stronger structural relationship with AUD for women than men.
Greater exposure to each risk factor was associated with increased the odds of AUD by age 29. Further, men tended to have higher mean-levels of risk exposure that contributed to a higher prevalence of AUD in men relative to women. Despite the higher level of absolute risk in men, AUD in women was associated with an especially high level of risk exposure during adolescence relative to their gender norm, and a higher level of risk exposure was necessary for women to exhibit AUD relative to men. Gender variation in the psychosocial consequences of AUD during young adulthood followed a similar pattern. That is, the magnitude of the difference between AUD and non-AUD impairment levels at age 29 (i.e., effect size) was larger in women than men for most variables. Compared to their gender norm, women with AUD tended to experience both higher risk exposure in adolescence and more negative outcomes in young adulthood relative to men with AUD. Consequently, AUD appears to be a more severe form of psychopathology in women, with a risk structure that is present early in development (i.e., at least by adolescence).
We detected several interactions between gender and adolescent risk factors, such that increases in alcohol use, other substance use, deviant peer relationships and academic problems increased odds of developing AUD more dramatically in women compared to men. Notably, these risks are not necessarily associated with concurrent AUD, as our AUD groups were derived using lifetime diagnoses by age 29. That is, the risk structure for AUD appears to emerge by adolescence, irrespective of the onset and chronicity of alcohol problems. The higher levels of adolescent risk exposure and young adult consequences associated with AUD in women provides further evidence that it is a more severe and debilitating disorder in women than men. While psychosocial problems in young adulthood may be consequences of AUD they may, alternatively, also reflect the persistence of the high loading of risk present in adolescence for women with AUD. Studies aiming to understand the etiology of AUD in women would benefit from examining risk structure at even earlier ages to track how risk exposure relates to the onset and persistence of AUD and psychosocial problems.
Consistent with previous reports (Nolen-Hoeksema, 2004; Foster et al., 2014), internalizing distress exhibited a unique structural relationship with AUD in women compared to men, suggesting it may be a gender-specific risk factor for AUD. In women, increases in internalizing distress significantly increased the odds of AUD during adolescence and also had a significant relationship with AUD in young adulthood. In contrast, AUD had a near zero association with internalizing distress in men at both ages, suggesting it is neither a risk for or a consequence of AUD in men. While previous literature has documented that women develop internalizing symptoms at a higher rate than men, our results suggest that, even after controlling for gender differences in their prevalence, internalizing symptoms likely play a role in the development of AUD in women but not men. The early emergence of internalizing symptoms in girls may potentiate alcohol use problems later in life through a developmental cascade. For example, symptoms of depression and anxiety that are more common in girls than boys during adolescence may be commonly associated with difficulties in school, work, and peer relationships during puberty and catalyze alcohol use problems as a method of coping with negative emotions. As a result, alcohol use may exacerbate internalizing distress indirectly through its negative influence on psychosocial development.
The temporal relationship between internalizing distress and alcohol problems, however, remains unclear. Another possibility is that girls may engage in early and heavy use of alcohol independent of internalizing distress. Heavy alcohol use by adolescent girls has been shown to impair neurocognitive functioning (Squeglia et al., 2010, 2011) and may increase isolation, disrupt social relationships, and hinder academic engagement. A lack of stability in social support and academic success may substantially diminish girls' self-esteem and efficacy for coping with negative emotions in adaptive and prosocial ways (Lopez & DuBois, 2005). Subsequently, internalizing symptoms may emerge during young adulthood. Directly testing the temporal relationship between internalizing distress and alcohol problems using longitudinal methods will be vital for explicating this aspect of women's vulnerability to AUDs.
Overall, we provided evidence that AUD is a more severe disorder in women and that internalizing distress may play a gender-specific role in AUD symptoms among women. As only a few studies of gender differences have directly compared men and women in the association between multiple risk variables and the development of AUD at multiple time points, this research represents an important advancement of current research. However, these findings are limited in a number of ways. First, the same associations between each risk factor and AUD may not apply to more diverse samples of men and women. Replication among a more racially and ethnically diverse sample are needed to determine the generalizability of our findings. Second, the associations between risk factors and AUD may be better explained by a third variable that also varies by gender. Third, the use of multiple comparisons is not ideal but allowed for the comparison of the relative contributions of a number of risks to identify candidates for causal pathways that should be validated through future replication of this work and other investigations of individual risk factors. Finally, our analyses do not address the co-development between each risk exposure and AUD. Future work in these areas will be important for determining the etiological role of these for AUD and its clinical features (i.e., onset and course).
Acknowledgements
This research was supported by National Institute on Drug Abuse Awards R37 DA005147 and R01 DA034606 and National Institute on Alcohol Abuse and Alcoholism Award R01AA 009367. Katherine T. Foster was supported by National Institute on Alcohol Abuse and Alcoholism F31 AA 023121. Brian M. Hicks was supported by National Institute on Drug Abuse K01 DA 025868. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors have no financial involvement or affiliation with any organizations whose financial interests may be affected by material in this work, or that might potentially bias it.
References
- Bemmels HR, Burt SA, Legrand LN, Iacono WG, McGue M. The heritability of life events: An adolescent twin and adoption study. Twin Research and Human Genetics. 2008;11:257–265. doi: 10.1375/twin.11.3.257. [DOI] [PubMed] [Google Scholar]
- Blazei RW, Iacono WG, Krueger RF. Intergenerational transmission of antisocial behavior: How do kids become antisocial adults? Applied & Preventive Psychology. 2006;11:230–253. [Google Scholar]
- Blume SB, Russell M. Alcohol and substance abuse in obstetrics and gynecology practice. In: Stotland NL, editor. Psychological aspects of women's health care: The interface between psychiatry and obstetrics and gynecology. 2nd ed American Psychiatric Press; Washington, DC: 2001. [Google Scholar]
- Brady KT, Randall CL. Gender differences in substance use disorders. Psychiatric Clinics of North America. 1999;22:241. doi: 10.1016/s0193-953x(05)70074-5. [DOI] [PubMed] [Google Scholar]
- Caspi A, Henry B, McGee R, Moffitt T, Silva P. Temperamental origins of child and adolescent behavior problems from age 3 to age 15. Child Development. 1995;66:55–68. doi: 10.1111/j.1467-8624.1995.tb00855.x. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders: Longitudinal evidence from a birth cohort. Archives of General Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- Cranford JA, Floyd FJ, Schulenberg JE, Zucker RA. Husbands' and wives' alcohol use disorders and marital interactions as longitudinal predictors of marital adjustment. Journal of Abnormal Psychology. 2011;120:210–222. doi: 10.1037/a0021349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler SE, Nolen-Hoeksema S. Accounting for sex differences in depression through female victimization: Childhood sexual abuse. Sex Roles. 1991;24:425–438. [Google Scholar]
- Dishion TJ, Patterson GR, Stoolmiller M, Skinner ML. Family, school, and behavioral antecedents to early adolescent involvement with antisocial peers. Developmental Psychology. 1991;27:172–180. [Google Scholar]
- Elkins I, King S, McGue M, Iacono W. Personality traits and the development of nicotine, alcohol, and illicit drug disorders: Prospective links from adolescence to young adulthood. Journal of Abnormal Psychology. 2006;115:26–39. doi: 10.1037/0021-843X.115.1.26. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Archives of General Psychiatry. 2007;64:1145–1152. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, McGue M, Iacono WG, Tellegen A. Genetic and environmental influence on parent-son relationships: Evidence for increasing genetic influence during adolescence. Developmental Psychology. 1997;33:351–363. doi: 10.1037//0012-1649.33.2.351. [DOI] [PubMed] [Google Scholar]
- Elkins I, McGue M, Malone S, Iacono W. The effect of parental alcohol and drug disorders on adolescent personality. American Journal of Psychiatry. 2004;161:670–676. doi: 10.1176/appi.ajp.161.4.670. [DOI] [PubMed] [Google Scholar]
- Foster KT, Hicks BM, Iacono WG, McGue M. Alcohol use disorder in women: Risks and consequences of an adolescent onset and persistent course. Psychology of Addictive Behaviors. 2014;28:322–335. doi: 10.1037/a0035488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granic I, Patterson GR. Toward a comprehensive model of antisocial development: a dynamic systems approach. Psychological Review. 2006;113:101–131. doi: 10.1037/0033-295X.113.1.101. [DOI] [PubMed] [Google Scholar]
- Hawkins JJD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Durbin CE, Blonigen DM, Iacono WG, McGue M, Zucker R. Alcohol dependence and personality change in young adulthood: Effects of an adolescent onset, persistence, and desistence. Alcoholism-Clinical and Experimental Research. 2010;34:242A–242A. [Google Scholar]
- Hicks BM, DiRago AC, Iacono WG, McGue M. Gene-environment interplay in internalizing disorders: consistent findings across six environmental risk factors. Journal of Child Psychology and Psychiatry. 2009;50:1309–1317. doi: 10.1111/j.1469-7610.2009.02100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks BM, Iacono WG, McGue M. Consequences of an adolescent onset and persistent course of alcohol dependence in men: Adolescent risk factors and adult outcomes. Alcoholism-Clinical and Experimental Research. 2010;34:819–833. doi: 10.1111/j.1530-0277.2010.01154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-case disorders: Findings from the Minnesota Twin Family Study. Development and Psychopathology. 1999;11:869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Malone SM, McGue M. Behavioral disinhibition and the development of early-onset addiction: Common and specific influences. Annual Review of Clinical Psychology. 2008;4:12.1–12.24. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- Johnson W, McGue M, Iacono WG. Genetic and environmental influences on academic achievement trajectories during adolescence. Developmental Psychology. 2006;42:514–532. doi: 10.1037/0012-1649.42.3.514. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott C, Myers J, Neale M. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Walters EE, Kessler RC. The prediction of length of major depression episodes: Results from an epidemiological sample of female twins. Psychological Medicine. 1997;27:107–117. doi: 10.1017/s0033291796003893. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Grant BF, Hasin DS. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug and Alcohol Dependence. 2008;93:21–29. doi: 10.1016/j.drugalcdep.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick D, Acierno R, Saunders B, Resnick H, Best C, Schnurr P. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68:19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- Klassen A, Wilsnack S. Sexual experience and drinking among women in a United-States national survey. Archives of Sexual Behavior. 1986;15:363–392. doi: 10.1007/BF01543109. [DOI] [PubMed] [Google Scholar]
- Krueger R, Hicks B, Patrick C, Carlson S, Iacono W, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Labouvie E, McGee C. Relation of personality to alcohol and drug-use in adolescence. Journal of Consulting and Clinical Psychology. 1986;54:289–293. doi: 10.1037//0022-006x.54.3.289. [DOI] [PubMed] [Google Scholar]
- Lopez C, DuBois D. Peer victimization and rejection: Investigation of an integrative model of effects on emotional, behavioral, and academic adjustment in early adolescence. Journal of Clinical Child and Adolescent Psychology. 2005;34:25–36. doi: 10.1207/s15374424jccp3401_3. [DOI] [PubMed] [Google Scholar]
- Masse L, Tremblay R. Behavior of boys in kindergarten and the onset of substance use during adolescence. Archives of General Psychiatry. 1997;54:62–68. doi: 10.1001/archpsyc.1997.01830130068014. [DOI] [PubMed] [Google Scholar]
- McGue M, Iacono W. The association of early adolescent problem behavior with adult psychopathology. American Journal of Psychiatry. 2005;162:1118–1124. doi: 10.1176/appi.ajp.162.6.1118. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Rutter M, Silva PA. Sex differences in antisocial behaviour: Conduct disorder, delinquency, and violence in the Dunedin Longitudinal Study. Cambridge Cambridge University Press; 2001. [Google Scholar]
- Niaura R, Nathan P, Frankenstein W, Shapiro A, Brick J. Gender differences in acute psychomotor, cognitive, and pharmacokinetic response to alcohol. Addictive Behaviors. 1987;12:345–356. doi: 10.1016/0306-4603(87)90048-7. [DOI] [PubMed] [Google Scholar]
- Nixon S. Cognitive deficits in alcoholic women. Alcohol Health & Research World. 1994;18:228–232. [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clinical psychology review. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Hilt L. Possible contributors to the gender differences in alcohol use and problems. Journal of General Psychology. 2006;133:357–374. doi: 10.3200/GENP.133.4.357-374. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Yoerger K. Intraindividual growth in covert antisocial behaviour: A necessary precursor to chronic juvenile and adult arrests? Criminal Behaviour and Mental Health. 1999;9:24–38. [Google Scholar]
- Patterson GR, Yoerger K. A developmental model for late-onset delinquency. In: Osgood DW, editor. Motivation and delinquency. University of Nebraska Press; Lincoln, NE: 1997. pp. 119–177. [PubMed] [Google Scholar]
- Petry N, Kirby K, Kranzler H. Effects of gender and family history of alcohol dependence on a behavioral task of impulsivity in healthy subjects. Journal of Studies on Alcohol. 2002;63:83–90. [PubMed] [Google Scholar]
- Robins LM, Baber T, Cottler LB. Composite international diagnostic interview: Expanded substance abuse module. Author; St. Louis, MO: 1987. [Google Scholar]
- Robins LM, Wing J, Wittchen H, Weler J, Babor T, Burke J, Farmer A, Jablenski A, Pickens R, Regier D, Sartorius N, Towle L. The composite international diagnostic interview: An epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry. 1988;45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- Rutledge P, Sher K. Heavy drinking from the freshman year into early young adulthood: The roles of stress, tension-reduction drinking motives, gender and personality. Journal of Studies on Alcohol. 2001;62:457–466. doi: 10.15288/jsa.2001.62.457. [DOI] [PubMed] [Google Scholar]
- Rutter M, Caspi A, Moffitt T. Using sex differences in psychopathology to study causal mechanisms: unifying issues and research strategies. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2003;44:1092–1115. doi: 10.1111/1469-7610.00194. [DOI] [PubMed] [Google Scholar]
- Sannibale C, Hall W. Gender-related symptoms and correlates of alcohol dependence among men and women with a lifetime diagnosis of alcohol use disorders. Drug and Alcohol Review. 2001;20:369–383. [Google Scholar]
- Schuckit MA. Low-level of response to alcohol as a predictor of future alcoholism. American Journal of Psychiatry. 1994;151:184–189. doi: 10.1176/ajp.151.2.184. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Heath AC, Madden PA, Bucholz KK, Statham DJ, Martin NG. Personality and the genetic risk for alcohol dependence. Journal of Abnormal Psychology. 2002;111:124–133. [PubMed] [Google Scholar]
- Squeglia LM, Schweinsburg AD, Pulido C, Tapert SF. Adolescent binge drinking linked to abnormal spatial working memory brain activation: Differential gender effects. Alcoholism-Clinical and Experimental Research. 2011;35:1831–1841. doi: 10.1111/j.1530-0277.2011.01527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, Spadoni AD, Infante MA, Myers MG, Tapert SF. Initiating moderate to heavy alcohol use predicts changes in neuropsychological functioning for adolescent girls and boys. Psychology of Addictive Behaviors. 2010;23:715–722. doi: 10.1037/a0016516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JA, Golding JM, Siegel JM, Burnam MA, Sorenson SB. Long-term psychological sequelae of child sexual abuse: The Los Angeles Epidemiologic Catchment Area study. In: Wyatt GE, Powell GJ, editors. Lasting effects of child sexual abuse. Sage; Thousand Oaks, CA: 1988. pp. 135–154. [Google Scholar]
- Tangney JP, Miller RS, Flicker L, Barlow DH. Are shame, guilt, and embarrassment distinct emotions? Journal of Personality and Social Psychology. 1996;70:1256–1269. doi: 10.1037//0022-3514.70.6.1256. [DOI] [PubMed] [Google Scholar]
- Tellegen A, Waller NG. Exploring personality through test construction: Development of the Multidimensional Personality Questionnaire. In: Boyle GJ, Matthews B, Saklofske DH, editors. Handbook of personality theory and testing: Vol. II. Personality measurement and assessment. Sage; Thousand Oaks, CA: 2008. pp. 261–292. [Google Scholar]
- Waldeck T, Miller L. Gender and impulsivity differences in licit substance use. Journal of Substance Abuse. 1997;9:269–275. doi: 10.1016/s0899-3289(97)90021-3. [DOI] [PubMed] [Google Scholar]
- Walden B, McGue M, Iacono WG, Burt SA, Elkins I. Identifying shared environmental contributions to early substance use: The respective roles of peers and parents. Journal of Abnormal Psychology. 2004;113:440–450. doi: 10.1037/0021-843X.113.3.440. [DOI] [PubMed] [Google Scholar]
- Widom C, Ireland T, Glynn P. Alcohol-abuse in abused and neglected children followed-up: Are they at increased risk. Journal of Studies on Alcohol. 1995;56:207–217. doi: 10.15288/jsa.1995.56.207. [DOI] [PubMed] [Google Scholar]
- Wilhelmsen K, Schuckit M, Smith T, Lee J, Segall S, Feiler H, Kalmijn J. The search for genes related to a low-level response to alcohol determined by alcohol challenges. Alcoholism-Clinical and Experimental Research. 2003;27:1041–1047. doi: 10.1097/01.ALC.0000075551.02714.63. [DOI] [PubMed] [Google Scholar]
- Wilsnack S, Vogeltanz N, Klassen A, Harris T. Childhood sexual abuse and women's substance abuse: National survey findings. Journal of Studies on Alcohol. 1997;58:264–271. doi: 10.15288/jsa.1997.58.264. [DOI] [PubMed] [Google Scholar]
- Wong MM, Nigg JT, Zucker RA, Puttler LI, Fitzgerald HE, Jester JM, Glass JM, Adams K. Behavioral control and resiliency in the onset of alcohol and illicit drug use: A prospective study from preschool to adolescence. Child Development. 2006;77:1016–1033. doi: 10.1111/j.1467-8624.2006.00916.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA. Alcohol use and the alcohol use disorders: A developmental-biopsychosocial systems formulation covering the life course. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 3. Risk, disorder and adaptation. 2nd ed. Wiley; New York: 2006. pp. 620–656. pp.620–656. [Google Scholar]