Abstract
Objectives
This observational study aimed to determine the relationship between time of birth and maternal morbidity during childbirth hospitalization.
Study Design
Composite maternal morbidities were determined using ICD9-CM and vital records codes, using linked hospital discharge and vital records data for 1,475,593 singleton births in California from 2005-2007. Time of birth, day of week, sociodemographic, obstetric, and hospital volume risk factors were estimated using mixed effects logistic regression models.
Results
The odds for pelvic morbidity were lowest between 11PM and 7AM compared to other time periods and the reference value of 7AM-11 AM. The odds for pelvic morbidity peaked between 11AM and 7PM [Adjusted Odds Ratio (AOR) 1101-1500=1.07 (1.06, 1.09); 1501-1900=1.08 (1.06, 1.10)]. Odds for severe morbidity were higher between 11PM and 7AM [AOR 2301-0300=1.31 (1.21, 1.41); 0300-0700=1.30 (1.20-1.41)] compared to other time periods. The adjusted odds were not statistically significant for weekend birth on pelvic morbidity [AOR Saturday=1.00 (0.98, 1.02); Sunday=1.01 (0.99, 1.03)] or severe morbidity [AOR Saturday=1.09 (1.00, 1.18); Sunday=1.03 (0.94, 1.13)]. Cesarean birth, hypertensive disorders, birthweight, and sociodemographic factors that include age, race, ethnicity, and insurance status, were also significantly associated with severe morbidity.
Conclusions
Even after controlling for sociodemographic factors and known risks such as cesarean birth and pregnancy complications like hypertensive disorders, birth between 11PM and 7AM is a significant independent risk factor for severe maternal morbidity.
Keywords: Childbirth hospitalization, maternal morbidity, time of birth
Introduction
Admission for childbirth is the most common reason for hospitalization in the United States (US), yet the nation continues to rank poorly in maternal and neonatal outcomes relative to other developed countries.1-3 The US maternal mortality ratio has increased steadily from 7.2 per 100,000 live births in 1987 to 17.8 per 100,000 live births in 2011.4 Moreover, approximately 25% of women suffer some type of childbirth-related morbidity,5, 6 and severe maternal morbidity (e.g. blood transfusion, disseminated intravascular coagulation, hysterectomy, organ system failure) has increased significantly over the past 15 years.6, 7 Racial and ethnic disparities in maternal morbidity and mortality are well documented,5, 7, 8 and provider factors such as incomplete or inappropriate treatment have been associated with preventable progression of maternal morbidity to severe morbidity or death.9
Work hours, shift length, and off-hours shifts have long been implicated as contributors to medical errors and poor outcomes,10-17 suggesting that interventions addressing circadian physiology and fatigue in health care workers may improve clinical outcomes. Several European and Canadian studies report associations between time of birth and maternity complications,18-25 but US studies on how time of day and weekend births influence maternal and neonatal outcomes are limited and present mixed results.26-31 Furthermore, US studies on the relationship between time of birth and maternal outcomes were focused primarily on unscheduled cesarean and excluded vaginal birth from the analysis.27, 29 While change in cesarean birth rates may largely explain changing morbidity parameters,32 vaginal births still account for 70% of all births, and their exclusion from evaluation of morbidity and mortality in studies of the effect of time of birth is problematic. The relationship between time of day and maternity outcomes is a potentially important patient safety issue that remains poorly understood. This observational study aimed to determine the relationship between time or day of birth and maternal morbidity during childbirth hospitalizations in California. We hypothesized that there would be a relationship between night-time birth and/or day of week and maternal morbidity.
Materials and Methods
We identified two composite forms of maternal morbidity on opposite ends of the spectrum of morbidity that can occur during childbirth hospitalization, using methods previously described.5 The two composite morbidities, pelvic and severe, were identified using International Classification of Diseases, 9th Revision (ICD9-CM) diagnosis and procedure codes, supplemented with birth certificate data. Pelvic morbidity comprised episiotomy, 3rd or 4th degree laceration, and vulvar or perineal hematoma or other trauma; severe morbidity comprised hysterectomy, unplanned return to operating room, transfer to intensive care unit, maternal death, or length of stay ≥90th percentile for mode of birth with a diagnosis of severe postpartum hemorrhage, maternal sepsis, deep vein thrombosis, pulmonary embolism, uterine rupture, respiratory failure, heart failure, puerperal CVA, severe anesthetic complication, maternal shock, disseminated intravascular coagulation, or renal failure. A complete list of the ICD-9-CM and Vital Statistics codes used to determine these composite morbidities is available elsewhere.5
The dataset linked California Vital Statistics Records with state-wide hospital discharge data for 2005, 2006, and 2007 from the Office of Statewide Planning and Development using a probabilistic matching algorithm33 that produced valid linkage for >96% of records.5 These were the most recently available linked data at the time of the data request. This linked dataset allows for evaluation of demographic characteristics such as race and ethnicity that are not available in hospital discharge data. Births that occurred in military hospitals, birth centers, or at home were excluded because they do not report hospital discharge data. Because multiple births and vaginal births after cesarean represent a small number of births with very different morbidity profiles, we limited our analysis to singleton births and excluded cases of trial of labor after cesarean (TOLAC). TOLAC (resulting in either vaginal or cesarean birth) accounted for <1% of births and is not offered in all facilities in California.34 The California Perinatal Quality Care Collaborative developed and executed the linkage strategy under a grant from the March of Dimes. Stanford University and University of California San Francisco Institutional Review Boards approved the study.
We conducted unadjusted and adjusted analyses to evaluate the relationship between time of day and day of the week that birth occurred, maternal demographic and obstetric characteristics, hospital volume, and maternal morbidity during childbirth hospitalization. Maternal age, race, ethnicity, level of education, insurance status, and adequacy of prenatal care were determined from birth certificate data. Adequacy of prenatal care was calculated using the Kotelchuck Index.35 Maternal co-morbidities such as preeclampsia and chronic hypertension could be classified as either risk factors or morbidities. We chose to evaluate preeclampsia and chronic hypertension as risk factors for morbidity as in our previous work.5 We did not evaluate diabetes as a risk factor in this study because it had minimal effect in our previous morbidity study findings.5
Time of birth was identified from the birth certificate. We analyzed time of birth in one-hour and four-hour blocks. Four-hour blocks were defined as 0701-1100, 1101-1500, 1501-1900, 1901-2300, 2301-0300, and 0301-0700 to allow analysis of ‘early’ and ‘late’ day and night shift 26, as well as accommodate interpretation of 8- and 12-hour nursing shifts. We used 0701-1100 as the reference value for these analyses. Similarly, day of the week was adjusted to a 24-hour day from 2300 to 2259 to be inclusive of 8-hour night shift (11PM-7AM). We accounted for clustering at the hospital level for all analyses. For unadjusted analyses we used bivariate logistic regression with robust variance estimation. Adjusted analyses were done with mixed effects logistic regression, where individual hospital was a random effect and predictor variables were fixed effects. Adjusted odds ratios with 95% confidence intervals (CI) were estimated using xtmelogit in STATA SE 13. For our two key outcomes and extremely large sample size, no adjustments were made for multiple comparisons.36
Results
The demographic characteristics of the 1,475,593 women in the final cohort are presented in Table 1.
Table 1. Maternal Demographic and Morbidity Characteristics (N=1,475,593).
| % | Total | |
|---|---|---|
| Maternal age | ||
| <18 | 3.3 | 48,487 |
| 18-25 | 34.6 | 511,239 |
| 26-35 | 49.1 | 724,614 |
| >35 | 13.0 | 191,253 |
| Race | ||
| White | 79.1 | 1,168,008 |
| Black | 5.3 | 78,142 |
| American Indian/Alaskan Native | 0.5 | 7,040 |
| Asian | 11.8 | 174,242 |
| Hawaiian/Pacific Islander | 0.5 | 6,802 |
| Other/Multi-race | 2.8 | 41,359 |
| Ethnicity | ||
| Non-Hispanic | 46.5 | 685,953 |
| Hispanic | 53.5 | 789,640 |
| Education | ||
| Less than High School | 31.5 | 465,191 |
| High School | 24.5 | 361,891 |
| Some college | 35.2 | 518,712 |
| Some post-graduate | 8.8 | 129,799 |
| Payor | ||
| None/self | 2.6 | 38,532 |
| Medi-cal/government | 50.1 | 738,998 |
| Private | 47.3 | 698,063 |
| Parity – Mode of Birth | ||
| Primiparous Vaginal | 28.0 | 412,976 |
| Multiparous Vaginal | 42.0 | 619,611 |
| Primiparous Primary Cesarean | 11.7 | 173,410 |
| Multiparous Primary Cesarean | 5.0 | 73,110 |
| Repeat Cesarean | 13.3 | 196,486 |
| Prenatal carea | ||
| Inadequate | 19.8 | 291,808 |
| Adequate | 80.2 | 1,183,785 |
| Co-Morbidities | ||
| Preeclampsia | ||
| No | 94.1 | 1,387,921 |
| Yes | 5.9 | 87,672 |
| Chronic Hypertension | ||
| No | 99.0 | 1,461,553 |
| Yes | 1.0 | 14,040 |
| Infant Birthwight | ||
| <2500 g | 5.1 | 74,836 |
| 2500 – 3999 g | 86.1 | 1,270,643 |
| ≥4000 g | 8.8 | 130,114 |
| Hour of Birth | ||
| 0701-1100 | 20.0 | 295,775 |
| 1101-1500 | 21.2 | 312,299 |
| 1501-1900 | 18.8 | 277,594 |
| 1901-2300 | 15.8 | 233,777 |
| 2301-0300 | 12.4 | 182,300 |
| 0301-0700 | 11.8 | 173,845 |
| Day of birthb | ||
| Monday | 14.1 | 208,926 |
| Tuesday | 15.9 | 234,099 |
| Wednesday | 15.9 | 234,148 |
| Thursday | 15.9 | 235,267 |
| Friday | 15.7 | 231,204 |
| Saturday | 12.1 | 178,051 |
| Sunday | 10.4 | 153,898 |
| Composite Morbidities | ||
| Pelvic floor morbidityc | 15.6 | 230,041 |
| Severe morbidityd | 0.6 | 8,398 |
Kotelchuck Adequacy of Prenatal Care Utilization Index35
Day of Week adjusted to a 24-hour day from 2300 to 2259 to be inclusive of 8-hour night shift from 11PM-7AM.
Pelvic floor morbidity includes episiotomy, 3-4th degree laceration, and vulvar or perineal hematoma or other trauma to vulva or perineum.
Severe morbidity = ICD9-CM or birth certificate codes present for hysterectomy, ventilation, unplanned return to operating room, transfer to intensive care, or maternal death, OR an ICD9-CM or birth certificate code for severe postpartum hemorrhage, maternal sepsis, deep vein thrombosis, pulmonary embolism, uterine rupture, respiratory failure, heart failure, hysterectomy, puerperal CVA, severe anesthetic complication, maternal shock, DIC, or renal failure and length of stay ≥90th percentile for mode of birth.
Pelvic Floor Morbidity
In unadjusted analyses, the risk for pelvic morbidity by hour was lowest at 8-9AM, rising in the early afternoon to a relative plateau of 40-57% increased risk from 2PM to 6AM (Figure 1). The time interval 2301-0300 had the highest odds of pelvic morbidity [OR=1.53 (1.50, 1.56)] (Table 2) despite fewer births during this time period (Figure 1). Weekend birth, young maternal age, higher education, Asian race, lack of insurance, and birth in hospitals with <3600 annual births were also associated with increased odds of pelvic floor morbidity. Non-white, non-Asian race, Hispanic ethnicity, multiparity, cesarean birth, hypertensive disorders, and low birthweight were associated with decreased odds of observed pelvic morbidity (Table 2).
Figure 1.
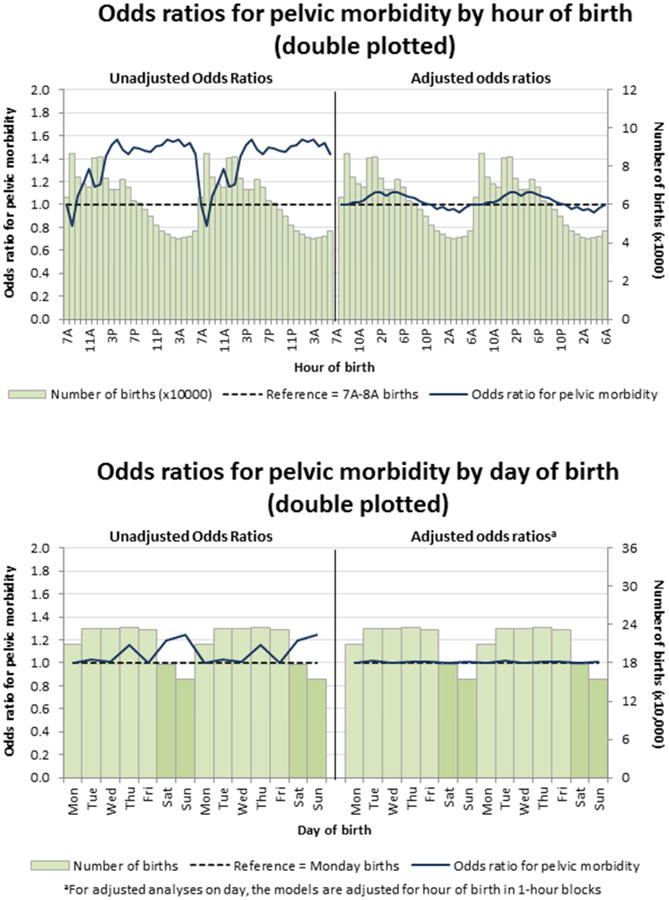
Table 2. Pelvic Morbidity, by Risk Factors (1,475,593).
| Predictor Variable | Unadjusted Odds Ratioa (95% Confidence Interval) | Adjusted Odds Ratiob (95% Confidence Interval) | |
|---|---|---|---|
| Maternal Age | |||
| <18 | 1.85 (1.81, 1.90) | 1.12 (1.09, 1.15) | |
| 18-25 | 1 | 1 | |
| 26-35 | 0.70 (0.69, 0.70) | 1.05 (1.03, 1.06) | |
| >35 | 0.52 (0.51, 0.52) | 1.17 (1.14, 1.19) | |
| Race | |||
| White | 1 | 1 | |
| Black | 0.66 (0.64, 0.67) | 0.61 (0.59, 0.63) | |
| American Indian/Alaskan Native | 0.79 (0.73, 0.85) | 0.76 (0.69, 0.83) | |
| Asian | 1.76 (1.74, 1.79) | 1.68 (1.65, 1.71) | |
| Hawaiian/ Pacific Islander | 0.81 (0.75, 0.87) | 0.80 (0.74, 0.88) | |
| Other / Multi-race | 0.93 (0.90, 0.96) | 0.83 (0.80, 0.86) | |
| Ethnicity | |||
| Hispanic | 0.73 (0.72, 0.74) | 0.83 (0.82, 0.85) | |
| Non-Hispanic | 1 | 1 | |
| Education | |||
| Less than High School | 1 | 1 | |
| High School | 1.09 (1.08, 1.11) | 1.03 (1.01, 1.04) | |
| Some college | 1.29 (1.28, 1.31) | 1.12 (1.10, 1.14) | |
| Some post-graduate | 1.58 (1.55, 1.61) | 1.26 (1.23, 1.29) | |
| Payor | |||
| None/self | 1.13 (1.10, 1.16) | 1.08 (1.05, 1.12) | |
| Medi-cal/government | 0.89 (0.88, 0.90) | 0.98 (0.97, 1.00) | |
| Private | 1 | 1 | |
| Parity – Mode of Birth | |||
| Primiparous Vaginal | 1 | 1 | |
| Multiparous Vaginal | 0.21 (0.21, 0.21) | 0.202 (0.200, 0.204) | |
| Primiparous Primary Cesarean | 0.003 (0.003, 0.003) | 0.003 (0.003, 0.003) | |
| Multiparous Primary Cesarean | 0.002 (0.002, 0.003) | 0.002 (0.002, 0.002) | |
| Repeat Cesarean | 0.001 (0.001, 0.001) | 0.001 (0.001, 0.001) | |
| Prenatal carec | |||
| Inadequate | 0.94 (0.93, 0.95) | 0.98 (0.97, 1.00) | |
| Adequate | 1 | 1 | |
| Co-Morbidities | |||
| Preeclampsia | |||
| Yes | 0.75 (0.73, 0.76) | 0.97 (0.95, 1.00) | |
| No | 1 | 1 | |
| Chronic Hypertension | |||
| Yes | 0.41 (0.38, 0.44) | 0.80 (0.74, 0.86) | |
| No | 1 | 1 | |
| Infant Birthweight | |||
| <2500 g | 0.54 (0.53, 0.55) | 0.55 (0.53, 0.56) | |
| 2500-3999 g | 1 | 1 | |
| ≥4000 g | 0.93 (0.92, 0.95) | 1.61 (1.58, 1.64) | |
| Hour of birth | |||
| 0701-1100 | 1 | 1 | |
| 1101-1500 | 1.25 (1.23, 1.27) | 1.07 (1.06, 1.09) | |
| 1501-1900 | 1.50 (1.48, 1.52) | 1.08 (1.06, 1.10) | |
| 1901-2300 | 1.47 (1.45, 1.50) | 1.03 (1.01, 1.05) | |
| 2301-0300 | 1.53 (1.50, 1.56) | 0.97 (0.95, 0.98) | |
| 0301-0700 | 1.50 (1.48, 1.53) | 0.95 (0.94, 0.97) | |
| Day of birthd | |||
| Monday | 1 | 1 | |
| Tuesday | 1.03 (1.01, 1.04) | 1.02 (1.00, 1.04) | |
| Wednesday | 1.01 (0.99, 1.03) | 1.00 (0.98, 1.02) | |
| Thursday | 1.02 (1.00, 1.03) | 1.01 (0.99, 1.02) | |
| Friday | 1.00 (0.98, 1.02) | 1.01 (0.99, 1.03) | |
| Saturday | 1.20 (1.18, 1.22) | 1.00 (0.98, 1.02) | |
| Sunday | 1.25 (1.23, 1.27) | 1.01 (0.99, 1.03) | |
| Hospital volume (births per year) | |||
| <1200 | 1.11 (1.03, 1.19) | 1.17 (1.07, 1.27) | |
| 1200-2399 | 1.18 (1.13, 1.23) | 1.23 (1.17, 1.29) | |
| 2400-3599 | 1.13 (1.10, 1.16) | 1.15 (1.11, 1.19) | |
| 3600+ | 1 | 1 | |
Bivariate logistic regression with robust variance estimation, clustered by hospital.
Mixed effects logistic regression model with individual hospital as random effect and predictor variables as fixed effects.
Kotelchuck Adequacy of Prenatal Care Utilization Index35
Day of Week adjusted to a 24-hour day from 2300 to 2259 to be inclusive of 8-hour night shift from 11PM-7AM.
In the adjusted analysis, the effect of time of birth was substantially reduced by controlling for other variables and more closely followed the pattern of births per hour (Figure 1). The risk of pelvic morbidity was increased 3-8% from 1101 to 2300, while time of birth between 2301 and 0700 was associated with a 3-5% decreased risk of pelvic floor morbidity. Weekday was not significant in the adjusted model. Maternal age under 18 and over 35, higher education, Asian race, lack of insurance, birthweight over 4000g, and birth at lower-volume hospitals were associated with increased odds of pelvic morbidity. The strongest independent risk factor was Asian race [AOR=1.68, (1.65, 1.71)].
Severe morbidity
In unadjusted analyses, there were fluctuations in risk for severe morbidity of +/- approximately 10% throughout the hours of 7AM to 7PM (Figure 2). These fluctuations were not statistically significant. Unadjusted risk for severe morbidity spiked at about 12AM and remained elevated by approximately 20% until about 4 AM when the risk began to decline toward baseline (Figure 2). Overall, the odds for severe morbidity were elevated for births between 2301 and 0700 [AOR 2301-0300=1.2 (1.12, 1.30); 0301-0700=1.15 (1.06, 1.24)] (Table 3). Friday or Saturday birth was also associated with severe morbidity, as was maternal age (under 18 and over 35), and Black and American Indian/Alaskan Native race (Table 3). Birthweight, cesarean birth, hypertensive disorders, and lack of private insurance also conferred increased odds of severe morbidity. Hospital volume, Hispanic ethnicity, education level, and adequacy of prenatal care were not associated with severe morbidity.
Figure 2.
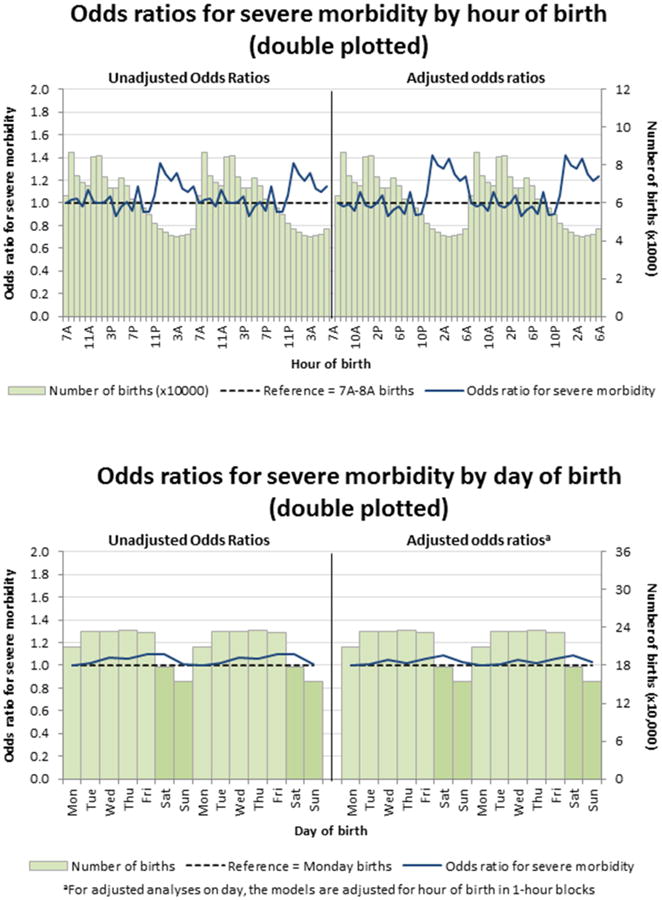
Table 3. Severe Morbidity, by Risk Factors (n=1,475,593).
| Predictor Variable | Unadjusted Odds Ratioa (95% Confidence Interval) | Adjusted Odds Ratiob (95% Confidence Interval) |
|---|---|---|
| Maternal Age | ||
| <18 | 1.45 (1.29, 1.62) | 1.15 (1.02, 1.29) |
| 18-25 | 1 | 1 |
| 26-35 | 1.06 (1.01, 1.12) | 1.22 (1.15, 1.29) |
| >35 | 1.76 (1.65, 1.87) | 1.88 (1.76, 2.02) |
| Race | ||
| White | 1 | 1 |
| Black | 1.53 (1.41, 1.66) | 1.39 (1.27, 1.53) |
| American Indian/Alaskan Native | 1.34 (1.02, 1.76) | 1.32 (1.00, 1.74) |
| Asian | 1.08 (1.00, 1.16) | 1.13 (1.04, 1.22) |
| Hawaiian/Pacific Islander | 1.22 (0.92, 1.62) | 1.22 (0.91, 1.62) |
| Other/Multi-race | 1.07 (0.94, 1.22) | 1.05 (0.92, 1.20) |
| Ethnicity | ||
| Hispanic | 0.97 (0.92, 1.02) | 1.10 (1.03, 1.17) |
| Non-Hispanic | 1 | 1 |
| Education | ||
| Less than High School | 1 | 1 |
| High School | 0.94 (0.89, 1.00) | 0.93 (0.87, 0.99) |
| Some college | 0.94 (0.89, 1.00) | 0.90 (0.84, 0.96) |
| Some post-graduate | 0.84 (0.77, 0.92) | 0.80 (0.72, 0.88) |
| Payor | ||
| None/Self | 1.19 (1.04, 1.38) | 1.14 (0.99, 1.32) |
| Medi-Cal/Govt/Other | 1.16 (1.10, 1.23) | 1.20 (1.11, 1.28) |
| Private | 1 | 1 |
| Parity – Mode of Birth | ||
| Primiparous Vaginal | 1 | 1 |
| Multiparous Vaginal | 0.56 (0.53, 0.59) | 0.53 (0.50, 0.56) |
| Primiparous Primary Cesarean | 1.46 (1.36, 1.55) | 1.16 (1.09, 1.24) |
| Multiparous Primary Cesarean | 1.73 (1.59, 1.88) | 1.20 (1.10, 1.31) |
| Repeat Cesarean | 1.35 (1.26, 1.44) | 1.18 (1.10, 1.27) |
| Prenatal carec | ||
| Inadequate | 1.00 (0.95, 1.06) | 1.08 (1.02, 1.14) |
| Adequate | 1 | 1 |
| Co-Morbidities | ||
| Preeclampsia | ||
| Yes | 3.71 (3.52, 3.92) | 2.55 (2.41, 2.71) |
| No | 1 | 1 |
| Chronic Hypertension | ||
| Yes | 3.50 (3.12, 3.93) | 1.33 (1.18, 1.50) |
| No | 1 | 1 |
| Infant Birthweight | ||
| <2500 g | 4.15 (3.92, 4.39) | 2.91 (2.75, 3.09) |
| 2500-3999 g | 1 | 1 |
| ≥4000 g | 1.24 (1.15, 1.33) | 1.21 (1.12, 1.31) |
| Hour of birth | ||
| 0701-1100 | 1 | 1 |
| 1101-1500 | 1.02 (0.95, 1.09) | 1.03 (0.97, 1.11) |
| 1501-1900 | 0.97 (0.90, 1.04) | 0.99 (0.92, 1.06) |
| 1901-2300 | 0.97 (0.90, 1.05) | 0.98 (0.91, 1.06) |
| 2301-0300 | 1.20 (1.12, 1.30) | 1.31 (1.21, 1.41) |
| 0301-0700 | 1.15 (1.06, 1.24) | 1.30 (1.20, 1.41) |
| Day of birthd | ||
| Monday | 1 | 1 |
| Tuesday | 1.03 (0.95, 1.11) | 1.01 (0.93, 1.09) |
| Wednesday | 1.08 (0.99, 1.17) | 1.04 (0.96, 1.13) |
| Thursday | 1.05 (0.97, 1.13) | 1.02 (0.94, 1.10) |
| Friday | 1.09 (1.01, 1.18) | 1.06 (0.98, 1.15) |
| Saturday | 1.10 (1.01, 1.20) | 1.09 (1.00, 1.18) |
| Sunday | 1.01 (0.92, 1.11) | 1.03 (0.94, 1.13) |
| Hospital volume (births per year) | ||
| <1200 | 1.05 (0.86, 1.29) | 1.12 (0.92, 1.37) |
| 1200-2399 | 1.08 (0.90, 1.28) | 1.10 (0.93, 1.30) |
| 2400-3599 | 1.01 (0.87, 1.17) | 1.02 (0.88, 1.18) |
| 3600+ | 1 | 1 |
Bivariate logistic regression with robust variance estimation, clustered by hospital.
Mixed effects logistic regression model with individual hospital as random effect and predictor variables as fixed effects.
Kotelchuck Adequacy of Prenatal Care Utilization Index35
Day of Week adjusted to a 24-hour day from 2300 to 2259 to be inclusive of 8-hour night shift from 11PM-7AM.
In the multivariable analysis, the temporal pattern of fluctuation in risk for severe morbidity was very similar to the unadjusted pattern, but slightly more pronounced (Figure 2). Odds for severe morbidity were higher between 2301 and 0700 compared to all other time periods [AOR 2301-0300=1.31 (1.21, 1.41); 0300-0700=1.30 (1.20-1.41)] (Table 3). The point estimate of the odds ratio was also higher on Saturday compared to other days of the week, but this did not reach statistical significance. Cesarean birth was significantly associated with severe morbidity. The highest odds for severe morbidity occurred in women with preeclampsia or maternal age over 35 years. Chronic hypertension was also associated with severe morbidity. Lack of insurance or government insurance, Hispanic ethnicity, and non-White race were associated with severe morbidity; Black women had 39% greater odds and American Indian/Alaskan Native had 34% greater odds of severe morbidity compared to White women.
To further evaluate the relationship between time of birth and severe maternal morbidity we tested the individual diagnoses that contribute to the composite severe morbidity indicator on time of birth in 4-hour blocks. This analysis showed that severe postpartum hemorrhage, maternal sepsis, heart failure, and hysterectomy varied significantly by time of birth, while the other contributing morbidities did not. Severe morbidity from hysterectomy was associated with time of birth between 0701 and 1500 (χ2=76.67, p<0.001). On the other hand, severe morbidity from heart failure and severe postpartum hemorrhage were each associated with time of birth between 2301 and 0700 (χ2=121.56, p<0.001 and χ2=52.58, p<0.001, respectively). Severe morbidity from maternal sepsis was associated with 1901-0700 time of birth (χ2=15.03, p=0.01).
Comment
Time of birth was a significant independent risk factor for maternal morbidity during childbirth hospitalization in our study, which is the first to our knowledge to evaluate time of birth on maternal morbidity for both vaginal and cesarean births in a population-based cohort in the US. Disparities in maternal outcomes according to age and race were observed. Patterns varied for type of maternal morbidity in relation to time of birth, even after controlling for maternal sociodemographic, obstetric, and facility risk factors. During night-time hours (2301-0700), adjusted odds for severe morbidity were elevated 30-31%. However, there was no significant effect for odds of morbidity with weekend birth.
For severe morbidity, we found that severe postpartum hemorrhage, maternal sepsis, heart failure, and hysterectomy varied significantly by time of birth, while other morbidities that qualified for severe morbidity (such as respiratory failure and anesthetic complications) were not associated with time of birth. An association is expected between hysterectomy and daytime birth (0700-1500), due to the likelihood of scheduling planned cesarean, planned hysterectomy, and cases at high risk for hysterectomy during these hours. In a study of 115,502 births in the Maternal-Fetal Medicine Units Network, placenta accreta had the strongest association with severe morbidity.37 This is also a likely explanation for the association between daytime birth and hysterectomy.
Other published studies of maternal outcomes in night-time birth have mixed results. The Maternal-Fetal Medicine Units Network (MFMU) found no difference in maternal or neonatal complications for night-time births in a cohort of 18,939 unplanned cesarean births in 13 academic medical centers between 1999-2000,27 whereas a study of 9,944 unscheduled cesarean births at a single tertiary center in Israel found increased risk for urgent unscheduled cases, increased use of general anesthesia, increased operating time, and increased complications in night-time unscheduled cesarean births.38 Further analysis of the MFMU cohort for differences in complications at times spanning planned handoffs (scheduled nursing and physician shift changes) found increases in neonatal facial nerve palsy and maternal hysterectomy associated with nursing shift changes but not physician shift changes.29 A key difference between our investigation and these prior studies is their exclusion of vaginal births. In addition, the MFMU hospitals are premiere regional referral centers that are likely to be well resourced, even at night. Our study examined risks in a population-based cohort across a wider variety of hospital settings.
Reasons for the observed association between night-time birth, heart failure, postpartum hemorrhage, and maternal sepsis are not clear. There may be an as-yet-unknown physiologic difference between women who give birth at night compared to women who give birth during day-time hours; it is also conceivable that a systematic difference in risk factors exists among women who present for birth at different times in the 24-hour cycle. However, the nature of such risk factors is difficult to envision considering that we adjusted for known medical and social risk factors in the final models. These adjusted models also markedly attenuated the odds for pelvic morbidity but not the odds for severe morbidity.
It is possible that early opportunities for recognition and mitigation of complications may be missed in women who give birth at night, resulting in progression of less serious morbidity to potentially preventable severe morbidity. Fatigue and sleep deprivation can impair cognitive performance. Cognitive impairment, reduced staffing, and fewer nighttime resources may limit the clinical team's capacity to respond to changes in clinical status. Rotating shifts typically result in shift lag disruption of circadian rhythms and acute sleep deprivation.16, 39 While permanent night work allows for some degree of adaptation to altered day-night circadian time cues, it is common for night shift workers to have some degree of chronic sleep deprivation due to competing daytime demands that can make it difficult to achieve adequate sleep. Fatigue prevalence in nurses working in acute care settings was reported to be 71-92% in one study, compared with 38% in the general population,16 and extended shifts and night work are common among both nurses and physicians.15-17 Both acute and chronic sleep deprivation degrade cognitive performance, resulting in impaired ability to integrate information, perform activities accurately, maintain vigilance and concentration, and communicate effectively.17, 39 These deficits also occur in the context of the sleep-deprived person's inability to perceive the degradation in their own performance. Furthermore, the night shift is where many new nurses start and are employed in their beginning professional experience, and their ability to recognize worsening conditions may be limited due to inexperience. In other words, fatigued, sleep-deprived, and inexperienced clinicians all face significant challenges to maintaining the situation awareness and effective teamwork that are necessary to effectively mitigate the progression of complications when they arise, and they are likely to face these challenges in the context of reduced staffing and limited clinical resources. This may contribute to failure to rescue or the progression from mild or moderate to severe morbidity.
Limitations of our study include the potential for over- and under-reporting of morbidities in administrative data, the inclusion of data from only one large state in the US, and the lack of evaluation of behavioral risk factors or specific care processes. Studies of coding accuracy for the types of outcomes reported here suggest that any systematic bias present would be toward under-reporting, rather than over-reporting, of morbidity.40-42 While there are limitations to restricting our analysis to one state and limitations to what variables can be analyzed using administrative data, California has robust data for childbirth cohorts and accounts for over 12% of US births.43 The size of the annual birth cohort allows for analysis of rare outcomes over a relatively short period of time. Future studies using California vital records data will allow for inclusion of body mass index and smoking status for records reported beginning in 2007. Future studies could also consider hours of labor, length of second stage, cesarean after labor and other processes of care that occur during labor and birth. While some algorithms have been developed to enhance the ability to extract information about processes of care, not all of these issues can be addressed at the population level with available data systems.
In summary, we find that night-time birth is a risk factor for maternal morbidity independent of other known obstetric and sociodemographic risk factors such as cesarean birth, hypertensive disorders, and maternal race, ethnicity, education, and insurance status. The 30% increased risk of severe morbidity when birth occurred between 11PM and 7AM in our cohort is concerning and additional research is needed to understand this phenomenon. While our study design cannot assess causality, a large body of literature suggests that clinician fatigue, fewer staff, inexperience, and sleep deprivation may be contributing factors to night-time morbidity in health care environments. In addition to compliance with work-hour regulations, the Joint Commission has outlined a series of steps that all inpatient facilities should take to address the risks posed by extended work hours, fatigue, and sleep deprivation that are common features of 24-hour health care operations. These steps include assessing scheduling and staffing policies, ensuring effective handoff practices, involving staff in designing schedules that reduce fatigue, and implementing fatigue management plans, and ensuring that staff are knowledgeable about sleep hygiene.14 Similarly, the American Nurses Association has called upon both nurses and employers to take steps to mitigate the effects of sleep deprivation and fatigue.44 Literature from sleep medicine, occupational safety, and health care domains supports the use of rest breaks and strategic scheduling of a nap during the night shift before the circadian nadir that occurs at about 4AM.16, 39, 45 A full understanding of the reasons for the observed association between severe morbidity and night-time birth will require additional research. However, based on the available evidence, comprehensive strategies to improve the safety and quality of maternity care should include attention to the nocturnal conditions in hospital environments and evidence-based strategies for mitigating degradation of performance from fatigue and sleep deprivation.
Acknowledgments
We thank Ms. Chengshi Jin and Dr. Lance Pollack, at University of California San Francisco for programming support funded by NIH/NCRR/OD UCSF-CTSI Grant number KL2 RR024130.
Funding: This study was supported by NIH/NCRR/OD UCSF-CTSI Grant number KL2 RR024130. Its contents are the sole responsibility of the authors and do not necessarily represent the official views of the NIH. The linkage of OSHPD and California Vital Statistics Data was made possible by a grant from the March of Dimes. Sponsor role: none.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to report
Condensation: Night time birth is a significant independent risk factor for severe maternal morbidity during childbirth hospitalization.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pfuntner A, Wier LM, Stocks C. Most Frequent Conditions in U S Hospitals, 2011. Rockville, MD: Agency for Healthcare Research and Quality; 2013. vol HCUP Statistical Brief #162. [PubMed] [Google Scholar]
- 2.World Health Organization. Trends in maternal mortality: 1990 to 2010. 2012 http://whqlibdoc.who.int/publications/2012/9789241503631_eng.pdf.
- 3.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol. 2015;125:5–12. doi: 10.1097/AOG.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Pregnancy Mortality Surveillance System. 2014 www.cdc.gov/reproductivehealth/MaternalInfantHealth/PMSS.html.
- 5.Lyndon A, Lee HC, Gilbert WM, Gould JB, Lee KA. Maternal morbidity during childbirth hospitalization in California. J Matern Fetal Neonatal Med. 2012;25:2529–35. doi: 10.3109/14767058.2012.710280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120:1029–36. doi: 10.1097/aog.0b013e31826d60c5. [DOI] [PubMed] [Google Scholar]
- 7.Creanga AA, Berg CJ, Ko JY, et al. Maternal mortality and morbidity in the United States: where are we now? J women's health (2002) 2014;23:3–9. doi: 10.1089/jwh.2013.4617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Creanga AA, Bateman BT, Kuklina EV, Callaghan WM. Racial and ethnic disparities in severe maternal morbidity: a multistate analysis, 2008-2010. Am J Obstet Gynecol. 2013 doi: 10.1016/j.ajog.2013.11.039. [DOI] [PubMed] [Google Scholar]
- 9.Geller SE, Rosenberg D, Cox SM, et al. The continuum of maternal morbidity and mortality: factors associated with severity. Am J Obstet Gynecol. 2004;191:939–44. doi: 10.1016/j.ajog.2004.05.099. [DOI] [PubMed] [Google Scholar]
- 10.Jha AK, Duncan BW, Bates DW. Fatigue, sleepiness, and medical errors. In: Shojania KG, Duncan BW, McDonald KM, Wachter RM, editors. Making health care safer: A critical analysis of patient safety practices. Rockville: Agency for Healthcare Research and Quality, United States Department of Health and Human Services; 2001. Publication 01-E058. [PMC free article] [PubMed] [Google Scholar]
- 11.Rogers AE. The Effects of Fatigue and Sleepiness on Nurse Performance and Patient Safety. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Vol. 2009. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- 12.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing intern's work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 13.Barger LK, Ayas NT, Cade BE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006;3:e487. doi: 10.1371/journal.pmed.0030487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Joint Commission. Sentinel Event Alerts. Vol. 48. The Joint Commission; 2011. Sentinel Event Alert: Health care worker fatigue and patient safety. [PubMed] [Google Scholar]
- 15.Mccormick F, Kadzielski J, Landrigan CP, Evans B, Herndon JH, Rubash HE. Surgeon fatigue: a prospective analysis of the incidence, risk, and intervals of predicted fatigue-related impairment in residents. Arch Surg. 2012;147:430–5. doi: 10.1001/archsurg.2012.84. [DOI] [PubMed] [Google Scholar]
- 16.Smith-Miller CA, Shaw-Kokot J, Curro B, Jones CB. An integrative review: fatigue among nurses in acute care settings. J Nurs Adm. 2014;44:487–94. doi: 10.1097/NNA.0000000000000104. [DOI] [PubMed] [Google Scholar]
- 17.Mansukhani MP, Kolla BP, Surani S, Varon J, Ramar K. Sleep deprivation in resident physicians, work hour limitations, and related outcomes: a systematic review of the literature. Postgrad Med. 2012;124:241–9. doi: 10.3810/pgm.2012.07.2583. [DOI] [PubMed] [Google Scholar]
- 18.Luo ZC, Karlberg J. Timing of birth and infant and early neonatal mortality in Sweden 1973-95: longitudinal birth register study. BMJ. 2001;323:1327. doi: 10.1136/bmj.323.7325.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olof S, Dickman PW, Johansson ALV, Kieler H, Cnattingius S. Time of Birth and Risk of Intrapartum and Early Neonatal Death. Epidemiology. 2003;14:218. doi: 10.1097/01.EDE.0000037975.55478.C7. [DOI] [PubMed] [Google Scholar]
- 20.Stewart JH, Andrews J, Cartlidge PHT. Numbers of deaths related to intrapartum asphyxia and timing of birth in all Wales perinatal survey, 1993-5. BMJ. 1998;316:657–60. doi: 10.1136/bmj.316.7132.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stewart JH, Andrews J, Cartlidge PH. Numbers of deaths related to intrapartum asphyxia and timing of birth in all Wales perinatal survey, 1993-5. BMJ. 1998;316:657–60. doi: 10.1136/bmj.316.7132.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee SK, Lee DS, Andrews WL, Baboolal R, Pendray M, Stewart S. Higher mortality rates among inborn infants admitted to neonatal intensive care units at night. J Pediatr. 2003;143:592–7. doi: 10.1067/s0022-3476(03)00367-6. [DOI] [PubMed] [Google Scholar]
- 23.Luo ZC, Liu S, Wilkins R, Kramer MS. Risks of stillbirth and early neonatal death by day of week. CMAJ. 2004;170:337–41. [PMC free article] [PubMed] [Google Scholar]
- 24.De Graaf JP, Ravelli AC, Visser GH, et al. Increased adverse perinatal outcome of hospital delivery at night. BJOG. 2010;117:1098–107. doi: 10.1111/j.1471-0528.2010.02611.x. [DOI] [PubMed] [Google Scholar]
- 25.Gijsen R, Hukkelhoven CW, Schipper CM, Ogbu UC, De Bruin-Kooistra M, Westert GP. Effects of hospital delivery during off-hours on perinatal outcome in several subgroups: a retrospective cohort study. BMC Pregnancy Childbirth. 2012;12:92. doi: 10.1186/1471-2393-12-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gould JB, Qin C, Chavez G. Time of birth and the risk of neonatal death. Obstet Gynecol. 2005;106:352–8. doi: 10.1097/01.AOG.0000168627.33566.3c. [DOI] [PubMed] [Google Scholar]
- 27.Bailit JL, Landon MB, Thom E, et al. The MFMU Cesarean Registry: Impact of time of day on cesarean complications. Am J Obstet Gynecol. 2006;195:1132. doi: 10.1016/j.ajog.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 28.Caughey AB, Urato AC, Lee KA, Thiet MP, Washington AE, Laros RK., Jr Time of delivery and neonatal morbidity and mortality. Am J Obstet Gynecol. 2008;199:496.e1. doi: 10.1016/j.ajog.2008.03.046. [DOI] [PubMed] [Google Scholar]
- 29.Bailit JL, Landon MB, Lai Y, et al. Maternal-Fetal Medicine Units Network Cesarean Registry: impact of shift change on cesarean complications. Am J Obstet Gynecol. 2008;198:173.e1. doi: 10.1016/j.ajog.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 30.Gould JB, Qin C, Marks AR, Chavez G. Neonatal mortality in weekend vs weekday births. JAMA. 2003;289:2958–62. doi: 10.1001/jama.289.22.2958. [DOI] [PubMed] [Google Scholar]
- 31.Hamilton P, Restrepo E. Weekend birth and higher neonatal mortality: a problem of patient acuity or quality of care? J Obstet Gynecol Neonatal Nurs. 2003;32:724–33. doi: 10.1177/0884217503258306. [DOI] [PubMed] [Google Scholar]
- 32.Kuklina EV, Meikle SF, Jamieson DJ, et al. Severe obstetric morbidity in the United States: 1998-2005. Obstet Gynecol. 2009;113:293–9. doi: 10.1097/AOG.0b013e3181954e5b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jaro MA. Probabilistic linkage of large public health data files. Stat Med. 1995;14:491–8. doi: 10.1002/sim.4780140510. [DOI] [PubMed] [Google Scholar]
- 34.Barger MK, Dunn JT, Bearman S, Delain M, Gates E. A survey of access to trial of labor in California hospitals in 2012. BMC Pregnancy Childbirth. 2013;13:83. doi: 10.1186/1471-2393-13-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health. 1994;84:1414–20. doi: 10.2105/ajph.84.9.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1:43–6. [PubMed] [Google Scholar]
- 37.Grobman WA, Bailit JL, Rice MM, et al. Frequency of and factors associated with severe maternal morbidity. Obstet Gynecol. 2014;123:804–10. doi: 10.1097/AOG.0000000000000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peled Y, Melamed N, Chen R, Pardo J, Ben-Shitrit G, Yogev Y. The effect of time of day on outcome of unscheduled cesarean deliveries. J Matern Fetal Neonatal Med. 2011;24:1051–4. doi: 10.3109/14767058.2010.545913. [DOI] [PubMed] [Google Scholar]
- 39.Caldwell JA, Caldwell JL, Schmidt RM. Alertness management strategies for operational contexts. Sleep Med Rev. 2008;12:257–73. doi: 10.1016/j.smrv.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 40.Lydon-Rochelle MT, Holt VL, Nelson JC, et al. Accuracy of reporting maternal in-hospital diagnoses and intrapartum procedures in Washington State linked birth records. Paediatr Perinat Epidemiol. 2005;19:460–71. doi: 10.1111/j.1365-3016.2005.00682.x. [DOI] [PubMed] [Google Scholar]
- 41.Yasmeen S, Romano PS, Schembri ME, Keyzer JM, Gilbert WM. Accuracy of obstetric diagnoses and procedures in hospital discharge data. Am J Obstet Gynecol. 2006;194:992–1001. doi: 10.1016/j.ajog.2005.08.058. [DOI] [PubMed] [Google Scholar]
- 42.Cheesman K, Brady JE, Flood P, Li G. Epidemiology of anesthesia-related complications in labor and delivery, New York State, 2002-2005. Anesth Analg. 2009;109:1174–81. doi: 10.1213/ane.0b013e3181b2ef75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. Natl Vital Stat Rep. Vol. 62. Hyattsville: National Center for Health Statistics; 2013. Births: Final data for 2012. [PubMed] [Google Scholar]
- 44.American Nurses Association. Addressing nurse fatigue to promote safety and health: Joint responsiblities of registered nurses and employers to reduce risks. Silver Spring, MD: Author; 2014. http://www.nursingworld.org/Addressing-Nurse-Fatigue-ANA-Position-Statement.pdf. [Google Scholar]
- 45.Ruggiero JS, Redeker NS. Effects of napping on sleepiness and sleep-related performance deficits in night-shift workers: a systematic review. Biol Res Nurs. 2014;16:134–42. doi: 10.1177/1099800413476571. [DOI] [PMC free article] [PubMed] [Google Scholar]


