Abstract
Sleep represents a set of biological functions necessary for the maintenance of life. Performing these functions, though, requires that an individual engage in behaviors, which are affected by social and environmental factors. Race/ethnicity and socioeconomic position represent categories of factors that likely play a role in the experience of sleep in the community. Previous studies have suggested that racial/ethnic minorities and the socioeconomically disadvantaged may be more likely to experience sleep patterns that are associated with adverse health outcomes. It is possible that disparities in sleep represent a pathway by which larger disparities in health emerge. This review (1) contextualizes the concept of race/ethnicity in biomedical research, (2) summarizes previous studies that describe patterns of sleep attainment across race/ethnicity groups, (3) discusses several pathways by which race/ethnicity may be associated with sleep, (4) introduces the potential role of socioeconomic position in the patterning of sleep, and (5) proposes future research directions to address this issue.
Keywords: Sleep, Health disparities, Race/ethnicity, Socioeconomic status, Epidemiology, Sleep duration
1. Introduction
Despite remarkable improvements in health and health care over the last century, striking and well-documented racial, ethnic, and socioeconomic health disparities persist in inequitably determining the welfare of social groups in the United States [1–3]. Both non-white and other socioeconomically disadvantaged populations have worse outcomes across a range of health conditions. Cardiovascular disease, diabetes, asthma, HIV/AIDS, and tuberculosis are all significantly more common among Blacks/African Americans and Hispanics than among non-Hispanic Whites [1,3,4]. Racial and ethnic disparities persist even after stratification by education or household income [1,3]. Such pervasive health disparities at the individual and societal level are likely mediated by a combination of structural, physiological, psychological, and behavioral differences across populations [2,3,5–7]. In addition, neighborhood factors play a significant role in perpetuating health disparities. Neighborhoods affect health through differential exposures to social (eg, cultural norms about health behaviors), psychological (eg, neighborhood safety and experience of discrimination), and physical (eg, exposure to toxins, air or noise pollution, access to healthy food) factors [8,9]. All of these differential neighborhood experiences are shaped by structural/ institutional forces that determine both vulnerability to harmful exposures and access to helpful resources. Understanding and reducing health disparities is an important public health goal.
Understanding the population burden of insufficient sleep and poor sleep quality is also an important public health goal. A recent report from the Institute of Medicine identified “sleep deprivation and sleep disorders” as a major unmet public health problem [10]. Another recent Institute of Medicine report, which discussed medical resident duty hours, also identified inadequate sleep as a major risk factor for iatrogenic problems [11]. Adequate sleep has been highlighted as a public health priority by Healthy People 2020, the document that guides federal health-related funding across the US Department of Health and Human Services [12]. In a statement of a joint task force of the American Academy of Sleep Medicine and the Sleep Research Society that identifies the most pressing goals of the sleep research field, the first noted goal was to gain better understanding of the public health implications of insufficient sleep and circadian disruption [13].
Insufficient sleep, operationalized as habitual short sleep duration in epidemiologic studies or enforced sleep restriction in laboratory studies, has been associated with weight gain and obesity [14], hypertension [15–17], hyperlipidemia [15,16], inflammation [18], diabetes [15,19–21], stroke [16,22], heart attack [16,23], and mortality [24–28]. In addition, relationships with neurocognitive impairment [29–31] and other systems have been explored [32–34]. A number of studies have also documented adverse health outcomes associated with poor sleep quality [35]. Sleep is an important domain of health and functioning, and it is possible that sleep represents not only a modifiable risk factor for cardiometabolic disease in general, but also an important moderator in the relationship among minority status, socioeconomic disadvantage, and health.
2. The problematic definition of “race” in biomedical research
Race has been used as a research variable in the social and biological sciences for centuries [36,37]. Despite the acceptance of “race” in scientific research, there is no clear, agreed-upon definition of what “race” is [38]. Some researchers define race as a biological category [36,37]. For example, some definitions of race rely on modern concepts of population genomics to describe groups of humans with shared genetic features. This definition assumes that since race groups are defined by shared genetic characteristics, genetic characteristics should be able to define who is and is not a member of a race. But there are no known combinations of genetic markers that reliably distinguish members of large population group from one another in order for them to qualify as biological races. There is more variability within groups identified as races than between them [39]. Despite the circular nature of this biological definition of race and the inconsistency with which it is applied, it remains the most common way to appropriate race in biomedical research. In reality, however, researchers typically apply socially constructed concepts of race, such as the “one-drop” rule, whereby a single ancestor of a particular race rather than an individual’s complete ancestry confers group membership. (For example, a person with a single Black grandparent and three White grandparents is commonly considered “Black” by this social definition.) Thus, researchers often confuse the prevailing social conceptualizations of race with biological definitions.
If race cannot be reliably defined biologically, is it a relevant variable for use in biomedical research [40]? Understanding the causes of and solutions to stark racial inequities in health – how racism affects the body – requires using racial categories in research. Researchers disagree, however, about the function race can serve in identifying the reasons for these gaps – as a social grouping, as a proxy for other correlated genetic or nongenetic variables, or as a biologically distinctive category. Race is relevant if treated as a social category that may capture variance in outcomes of interest. If race is a social and not a biological category, though, what does it represent? It could represent a proxy for other social, environmental, and cultural factors that may tend to aggregate in social groups but do not define those groups. As an important example, race may serve as a proxy for exposure to (and/or perception of) racial discrimination, especially when studies are restricted to socio-geographic strata for which discrimination across group lines is more homogeneous [41]. Race is an important category to documents and record health disparities, and to study the impact of racism on health. Therefore, race represents a relevant variable if whatever race is standing in for reliably determines outcomes. It is then incumbent on researchers, though, to “unpack” the significance of race to the research question and to determine which factors actually play a causal role.
Ethnicity is sometimes used as an alternative to race. Ethnicity refers to a group that shares history, culture, and (usually) geographic ancestry. Many people who share an ethnicity may also identify as the same race, but this concept more fully recognizes the fluidity of characteristics within and between groups and the role of social factors in defining group membership. Although “race” is usually restricted to a few categories, “ethnicity” can be much more varied.
If the definitions of race and ethnicity vary and overlap, how can researchers use these categories? Certainly, any operationalization comes with limitations [42]. The concept of race/ethnicity has emerged as a research variable and research subjects are typically grouped by self-identification, avoiding thorny definitional issues. The acceptance of self-identification essentially recognizes that “race/ ethnicity” is a social category, based on whatever factors research subjects consider appropriate.
Because health disparities among racial/ethnic groups exist, there is good reason for biomedical researchers and practitioners to try to define and use these groupings. However, as discussed here, these groups are socially determined, heterogeneous, dynamic, and socioculturally complex. If we are to truly understand these health disparities, we must more carefully consider how to appropriately use race/ethnicity in biomedical, epidemiological, and public health research in order to understand the development, persistence, and elimination of health disparities.
3. Studies of sleep by race/ethnicity
Traditionally, sleep research did not consider race, ethnicity, or other such social stratifications. Most laboratory-based studies did not report race/ethnicity. In more recent years, laboratory studies still infrequently report the race/ethnicity of subjects. However, many studies, especially those that attempt to generalize to the general population, now attempt to measure race/ethnicity to some degree. There has been a growing recognition that race/ethnicity represents a factor (or set of factors) that are relevant to the study of sleep.
3.1. Studies measuring sleep across race/ethnicity groups
Several studies have attempted to understand whether habitual sleep patterns differ according to race/ethnicity group. Studies of polysomnographic (PSG) sleep have the benefit of using an objective, gold-standard measure of sleep. However, PSG sleep does not accurately reflect habitual sleep, as it is in an artificial situation. There is a well-documented literature casting doubt on the generalizability of one night of PSG [43,44]. PSG is the only way to assess sleep architecture; however, despite the Hawthorne effect, PSG will continue to be used. As such, several studies have explored group differences using PSG [45–48], and these studies were summarized in a meta-analysis by Ruiter and colleagues [49]. Of the eight studies found, the meta-analysis found that Blacks/ African Americans obtained approximately 28 min less PSG sleep than Whites. This translated to an effect size of approximately 0.48 standard deviations (p < 0.05). There were also significant differences in stage 2 and slow-wave sleep (stages 3 and 4), such that Blacks/African Americans obtained less slow-wave sleep, which seems to be made up for by an increased stage 2 sleep. These findings are consistent with those of other studies, who found that Blacks/African Americans obtained less slow-wave sleep [50–54] and had a poorer sleep efficiency [52,54] than non-Hispanic Whites. This suggests that, on average, for Blacks/African Americans, sleep is less deep and restful.
Similarly, this meta-analysis evaluated six studies of subjective sleep duration [49]. This included two studies that used sleep diaries, as well as four studies that used a (non-validated) retrospective sleep questionnaire. When combined, a similar effect was found, with Blacks/African Americans reporting less sleep on average than Whites (15.1 min less, p < 0.05) [49].
Another objective estimate of sleep duration and quality is wrist actigraphy, and a few studies compared sleep among racial/ethnic groups using this methodology. A study in San Diego reported significantly shorter mean sleep duration (5.9 vs. 6.3 h) and lower sleep efficiency (79% vs. 83%) for minorities compared to whites [55]. A study in adults aged 35–50 years found that sleep duration and quality was significantly lower in African Americans, particularly men, compared to white women, even after adjustment for numerous sociodemographic and behavioral factors [56]. Finally, a study in Massachusetts compared the sleep of non-Hispanic African/ Caribbean immigrant and non-Hispanic white employees in long-term health care, and it found that the African/Caribbean immigrants slept an hour less on average [57]. Once socioeconomic and occupational characteristics were adjusted for, the difference was reduced to approximately 40 min, suggesting that socioeconomic position (SEP) and work factors partially account for the difference.
Another approach that has been taken is to evaluate whether people of various groups are more or less likely to report sleep duration by category (usually short or long, relative to normative (7–8 h)). This is because much of the evidence on the relationship of habitual sleep duration and health suggests that the pattern of results fits best with categorical definitions of sleep duration, rather than continuous definitions [32]. Hale and Do evaluated data from the 1990 National Health Interview Survey [58]. They found that, relative to non-Hispanic White Americans, Blacks/African Americans were 41% more likely to be short sleepers (6 or fewer hours); similarly, non-Mexican Hispanic adults were 26% more likely to be short sleepers, and those in the “other” category were 35% more likely to be short sleepers. Regarding long sleep duration, the only group that was more likely than non-Hispanic Whites to be long sleepers (9 or more hours) were Blacks/African Americans, who were 62% more likely. Similarly, Nunes and colleagues found that among respondents to the National Health Interview Survey, Blacks/African Americans were less likely to report sleep of 7–8 h, versus non-Hispanic Whites, with increased likelihood of both short and long sleep [59].
Stamatakis and colleagues evaluated the likelihood of short sleep duration (6 h or less on average) from the Alameda County Health and Ways of Living Study [60]. Compared to self-identified Whites, those who self-identified as African American were about twice as likely to be short sleepers, and those in the “other” category were approximately 50% more likely. Those who were Hispanic/Latino were not more or less likely to be short sleepers. These relationships were adjusted for age, living conditions, current health, health behaviors, body mass index, depression, and likely insomnia.
In a more recent study, Whinnery and colleagues examined nationally representative data from the 2007–2008 National Health and Nutrition Examination Survey (NHANES) [61]. The sleep duration categories examined were very short sleep (<5 h), short sleep (5–6 h), and long sleep (9 or more hours), compared to normal sleep (7–8 h). These categories were chosen because the majority of short sleepers are in the 5–6-h group, but the greatest cardiometabolic risks may be found in the extremes of sleep duration. For this reason, it may be useful to separate the short sleepers (5–6 h, more populous but with somewhat decreased risk) and the very short sleepers (<5 h, representing fewer people but at an increased risk). In this study, Whinnery and colleagues compared those who self-identified as non-Hispanic Whites to those who self-identified as Black/ African American, Mexican American, non-Mexican Hispanic/ Latino, and Asian/other. Those who identified as Black/African American were approximately three and a half times as likely to be a very short sleeper; similarly, non-Mexican Hispanics/Latinos were approximately 3.5 times as likely and Asians/others were approximately five times as likely to be a very short sleeper. Regarding short sleep, those who identified as Black/African American were about twice as likely to be short sleepers, and those who identified as Asian/ other were approximately two and a half times as likely. Mexican Americans were 60% less likely to be long sleepers.
This study also examined the degree to which these relationships are attenuated by other factors, including age, sex, relationship status, primary language spoken at home, immigration status, education, income, access to health insurance, home ownership, and food security. Self-identified Blacks/African Americans were approximately 2.5 times as likely to be very short sleepers and approximately twice as likely to be short sleepers. Mexican Americans were approximately 60% less likely to be long sleepers. Non-Mexican Hispanics/Latinos were approximately 2.7 times as likely to be very short sleepers and Asians/others were approximately four times as likely to be very short sleepers and twice as likely to be short sleepers [61].
3.2. Studies assessing sleep–race interactions in health outcomes
It is possible that sleep plays an important role in health disparities. Sleep may represent a modifiable risk factor for poor health, or it may simply be a marker of some other risk factor [62]. Although several longitudinal studies suggest a causal role of sleep in a number of cardiometabolic conditions [33,63–65], this role has not been well studied. However, several reports have begun to examine this issue. For example, Knutson and colleagues [66] found that racial differences in a 5-year change in blood pressure were explained by differences in sleep duration. Relative to non-Hispanic White Women, Black/African-American men demonstrated a 4.4-mm Hg change in systolic blood pressure and a 2.7-mm Hg change in diastolic blood pressure over five years, and Black/African-American women demonstrated a 3.48-mm Hg increase in diastolic blood pressure. These effects were completely mediated by sleep duration.
In another study, Grandner and colleagues [67] found that the relationship between sleep duration and C-reactive protein (a cardiovascular risk marker) differed by race, with a U-shaped relationship in non-Hispanic Whites, no relationship in Hispanic/ Latinos, a pseudo-positive linear relationship in Asians/others (with the lowest levels in the short sleepers, mid-range levels in 7–8 h sleepers, and highest values in long sleepers), and increased levels associated with short sleep in Blacks/African Americans.
Grandner and colleagues also examined whether the relationship between sleep duration and cardiometabolic disease risk factors depended on self-identified race/ethnicity [15]. When a nationally representative sample of the US population was examined, familiar patterns were found: very short sleep duration (<5 h) was associated with self-reported and objectively assessed hypertension, hyperlipidemia, diabetes, and obesity, relative to normal (7–8 h) sleep. Short sleep duration (5–6 h, also relative to 7–8 h) was associated with self-reported and objectively determined hypertension and obesity. Long sleep duration (9 h or more) was associated with objectively determined diabetes. However, for all eight outcomes (self-reported and objectively determined hypertension, hyperlipidemia, diabetes, and obesity), race/ethnicity by sleep duration interactions was significant (all p < 0.0001). When the sample was stratified by self-identified race/ethnicity, different patterns emerged.
For example, when the sample was restricted to non-Hispanic Whites, very short sleep was associated with an increased risk of self-reported hypertension, self-reported and objective hyperlipidemia, and self-reported diabetes; long sleep was associated with objectively determined hyperlipidemia. When the sample was restricted to only self-identified Blacks/African Americans, very short sleep was associated with self-reported hypertension and both self-reported and objectively determined obesity. Among Mexican Americans, short sleep was associated with self-reported hypertension only. Among self-identified non-Mexican Hispanics/ Latinos, very short sleep was associated with self-reported and objective hypertension, and short sleep was associated with a lower risk of objectively determined diabetes. Finally, among self-identified Asians/others, very short sleep was associated with self-reported and objectively determined hyperlipidemia. It is unclear why these patterns differ so much among groups. These results highlight the importance of understanding differential pathways linking sleep and cardiovascular risk across racial/ethnic groups and, in particular, what cultural or behavioral factors may exacerbate or protect against the potential effects of inadequate sleep.
3.3. Studies assessing risk of sleep disorders
A second meta-analysis by Ruiter and colleagues also examined differences in sleep disorders by race/ethnicity [68]. A total of five studies were identified that examined the prevalence of sleep disordered breathing. Taken together, a small effect was found (effect size = 0.13), with African Americans being more likely to have sleep disordered breathing than Whites. Consistent with this, a total of eight studies were identified that examined differences in sleep disordered breathing severity. Taken together, a modest effect was again found (effect size = 0.10), such that the severity of sleep disordered breathing was greater among African Americans versus Whites. Regarding insomnia, nine studies were identified that examined sleep complaints consistent with insomnia across groups. When these were taken together, consistent differences were not found, though African Americans were slightly less likely to report sleep complaints (effect size = −0.23, p < 0.05). Later studies of larger, population-level samples helped to clarify some of these findings.
There are a limited number of studies that have examined whether sleep symptoms are disproportionately reported among race/ ethnicity groups in the general population. In one study, > 150,000 respondents from the 2006 Behavioral Risk Factor Surveillance System reported the frequency of experiencing difficulty “falling asleep, staying asleep or sleeping too much,” and responses were dichotomized at three days per week [69]. In evaluating the proportion of the population reporting these difficulties at least three nights per week on an average, men and women were evaluated separately. Among men, no significant differences were seen between non-Hispanic Whites and Blacks/African Americans, Hispanics/Latinos, or those reporting more than one race/ethnicity. A significant difference was seen, though, between non-Hispanic Whites and Asians/ others, who were less likely to report general sleep disturbance than the non-Hispanic Whites. Among women, relative to non-Hispanic Whites, Blacks/African Americans, Hispanics/Latinas, and Asians/ others reported significantly lower rates of general sleep disturbance. Furthermore, among women, those reporting more than one race/ ethnicity were more likely to report general sleep disturbance at least three nights per week. Despite an increased likelihood of short sleep duration and associated outcomes (described above), racial/ ethnic minorities tended to report fewer sleep disturbances.
Regarding more specific sleep symptoms, data from the 2007–2008 NHANES examined race/ethnicity differences in self-reported sleep symptoms, including sleep latency >30 min, difficulty falling asleep, difficulty maintaining sleep, early morning awakenings, nonrestorative sleep, daytime sleepiness, snoring, and choking/ gasping during sleep [70]. In models that included age, sex, race/ ethnicity, marital status, immigrant status, income, education, access to health insurance, and household food security, the following results were found: Blacks/African Americans were more likely to report sleep latency >30 min, compared to non-Hispanic Whites. Contrastingly, self-reported difficulty falling asleep was reported less frequently among Blacks/African Americans, Mexican Americans, and other Hispanics/Latinos. Difficulty maintaining sleep, early morning awakenings, non-restorative sleep, and daytime sleepiness were all reported less frequently among Blacks/African Americans and Mexican Americans, and both non-restorative and daytime sleepiness were also reported less frequently among other Hispanics/Latinos. Non-Mexican Hispanics/Latinos were more likely to report choking/gasping during sleep and snoring.
Further, several studies have found relationships with adherence to continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea. The importance of these findings is underscored by the high prevalence and public health significance of sleep apnea as a health risk factor, as well as the fact that CPAP is a safe and effective therapy but requires individuals to engage in the health-promoting behavior of wearing a potentially uncomfortable mask to sleep every night. Wallace and Wohlgemuth found that, compared to Whites and Hispanics/Latinos (combined), Blacks/ African Americans used their CPAP for fewer days overall, with fewer individuals using their device daily [71]. Further, increased CPAP use was correlated with an increased functioning and quality of life in this group, suggesting that this lack of use was associated with detrimental effects. This supported the previous work by Billings and colleagues, who showed that Blacks/African Americans (compared to non-Hispanic Whites) used CPAP more infrequently and for less time at night [72]. Similarly, Means and colleagues found that African Americans with mental health diagnoses were least likely among groups studied to adhere to CPAP treatment recommendations [73]. Interestingly, Shaw and colleagues found that beliefs and attitudes about sleep apnea among Blacks in the New York metropolitan area may be partially to blame [74]. For example, many individuals felt that sleep apnea was a type of insomnia, that it was a natural part of aging, and/or that it was caused by bedtime activities such as diet. These beliefs would presumably be barriers to adherence to CPAP, which treats sleep apnea as a disorder separate from insomnia, a disorder that is not a natural part of aging, and something that cannot simply be addressed through dietary interventions. Another potential mediating factor is the role of short sleep duration. Billings and colleagues found that the overlapping phenomena of short sleep duration and the lack of CPAP adherence among Blacks/African Americans may be somewhat related [75]. In this study, short sleep duration (which presumably affords less opportunity for CPAP use) and long sleep latency (which may lead to increased discomfort with the mask) were important partial mediators of race/ethnicity differences in CPAP adherence.
Some studies have examined CPAP adherence in other groups as well. Among Hispanic/Latino veterans in southern Florida, Wallace and colleagues found that insomnia in this group was a potential predictor of CPAP non-adherence [76]. In a study from New Zealand, Bakker and colleagues found that when Maori and non-Maori adults with sleep apnea were evaluated, it was socioeconomic factors, rather than ethnicity, that predicted CPAP adherence [77].
Other studies have found inconsistent relationships between race/ethnicity and sleep symptoms. Some studies have found that general sleep quality is worse among racial/ethnic minorities [78–81], whereas others have failed to find this association [69,82,83]. There are several potential explanations for the inconsistency in the literature. First, it is possible that some of this inconsistency is due to measurement error that may be different across studies and populations. Cross-cultural validity of sleep assessments has rarely been assessed, and some instruments may demonstrate variable psychometric properties. Second, some of the inconsistency may be accounted for by differences among cohorts. For example, a national sample assessed over the phone may be different from a local sample assessed in clinic. Third, the effects of geographical location and other environmental variables may moderate these relationships [84]. Fourth, there may be differences in the levels of bias in reporting. For example, questions asked in a non-judgmental way (eg, sleep duration, sleep latency) may lead to different reporting patterns than questions asked in a way that asks for an explicit complaint (eg, difficulty initiating or maintaining sleep). This may explain why “difficulty falling asleep” was reported less among minorities, but >30 min sleep duration was reported more often.
Another potential explanation is the variable, interactive roles of race/ethnicity, and socioeconomic factors. These will be addressed in further detail below.
4. Unpacking race/ethnicity findings
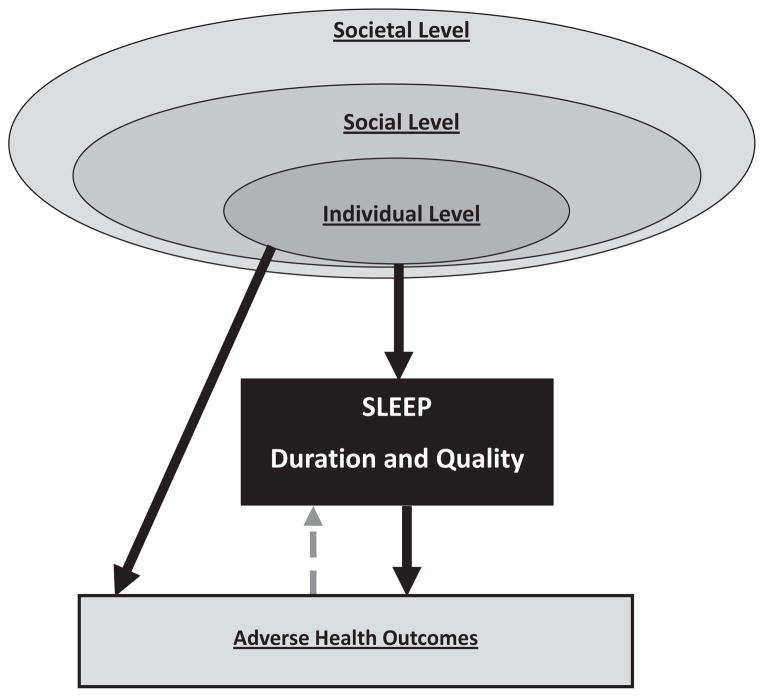
Why do race/ethnicity differences exist regarding sleep? Differing social and environmental factors may play a role in different beliefs and attitudes about sleep, or different ways of approaching sleep assessments. Further, these mechanisms may simply be working through (at least partially) other factors that are separate from race/ethnicity as a unique construct but, in our society, they are inexorably linked with race for social reasons. These may include socioeconomic variables, aspects of the physical environment, etc. The social–ecological model of sleep and health (first presented by Grandner and colleagues [28]) describes how sleep, which plays a role in a number of health outcomes, is determined by individual-level factors, which are embedded within social level factors, which themselves are embedded within societal level factors. For example, individual-level beliefs, behaviors, and biology are embedded within the aspects of the social environment, such as culture, neighborhood, and socioeconomics, and these are themselves embedded in societal issues such as 24/7 society, public policy and technology (Fig. 1).
Fig. 1.
Social–ecological model of sleep and health. Adapted from Grandner, Hale, Moore, and Patel [28].
4.1. Sleep as a sociocultural phenomenon
In addition to being a physiological phenomenon, sleep is a social and cultural phenomenon [85,86]. Simon Williams observes, “When we sleep, where we sleep, and with whom we sleep are all important markers or indicators of social status, privilege, and prevailing power relations” [85]. Also, “[Sleep] displays a high degree of socio-cultural plasticity … through the interplay of biological and psychological processes, environmental and structural circumstances, and socio-cultural forms of elaboration, conceived in temporally, spatially, and contextually bounded and embodied terms” [85].
Cultures vary widely regarding sleep practices and beliefs. For example, the practice of bed-sharing with infants, children, and adult family members occurs to varying degrees across cultures [87–92]. Sleeping surfaces also vary widely across cultures [86]; these range from mats on the ground, to firm, unadorned beds, to the plush style of beds that predominate in the Western world. Beliefs and attitudes about sleep also vary widely across cultures. For example, the cultural significance and impact of dreaming varies widely across traditional Chinese, Indian, Native, Mediterranean, and modern Western societies [93]. In addition, as influences of globalization, technology, and industrialization encroach into an area, the sleep-related beliefs and practices change dramatically, with the institutionalization of long working hours [94–101] and shiftwork [102–105], and banning of culturally appropriate naps [106–108].
4.2. Beliefs and attitudes about sleep
Few studies have systematically examined beliefs and attitudes about sleep that may differ across race/ethnicity groups. Two studies have specifically looked at beliefs and attitudes in self-identified Blacks/African Americans. Pandey and colleagues found, in a sample from Brooklyn, NY, USA, that Blacks/African Americans who were at high risk of obstructive sleep apnea had higher scores on the dysfunctional beliefs and attitudes about sleep scale, compared to those who were not at high risk [109]. This scale specifically measures commonly held unhealthy or unhelpful beliefs about sleep, which are thought to be related to increased worry about sleep and, consequently, worse sleep quality [110].
In a study in the Philadelphia area, Grandner and colleagues examined quantitative data obtained from a sample of 41 Black and 32 White older women (mean age 72 and 64 years in the Black and White groups, respectively), with no difference in household income level [111]. All participants were administered a questionnaire to evaluate sleep-related beliefs and practices. On most questions, there were no statistically significant differences. Some questions did show differences, though. For example, Black women were more likely to indicate that they “agree” or “strongly agree” to the incorrect statements that, “Boredom makes you sleep even if you slept enough the night before,” and “Lying in bed with your eyes shut is as good as sleeping.” White women were more likely to indicate that they “agree” or “strongly agree” to, “My sleep is important to my health,” and “Getting enough sleep is important for me to be able to enjoy the daytime.” They were also more likely to more strongly endorse the statement that “Dozing while driving a vehicle is serious.” But White women were also more likely to endorse the incorrect beliefs that “Turning up the volume of the radio or music is a good way to wake me up if I am drowsy while driving,” and “Opening the car window is a good way to wake me up if I am drowsy while driving.” Nonsignificant trends were seen for several items, with the Black women more likely to endorse the statement that, “People who fall asleep at work or at school are lazy or have bad habits,” and White women more likely to endorse statements including, “Poor sleep affects the quality of my life,” and “Not enough sleep can lead to serious consequences.” Beliefs about specific practices were also examined. When asked what respondents would do if they had difficulties with insomnia, the Black group was more likely to endorse the potentially unhealthy practices of “Drink alcohol,” and “Do something in bed (like read or watch TV),” as well as the potentially healthy practice of “Get up and start the day.” Although there was no difference in the degree to which Black and White groups endorsed an item indicating that they use the bed “for sleep and sex only,” when specific activities were queried, the Black group was more likely to “Read or watch TV,” “Eat or drink,” “Worry or spend time thinking,” and “Argue or be angry,” and a trend was seen for “Do work.” This is important as excess activity in bed is a risk factor for developing insomnia.
Less work has been done in Hispanic/Latino groups. Sell and colleagues examined sleep knowledge among Mexican Americans in San Diego [112]. Similar rates of knowledge were seen for insomnia. Regarding sleep apnea, non-Hispanic Whites were more likely than Mexican Americans to know what sleep apnea was by name, but when describing the symptoms, both groups had similar knowledge that such a problem exists. Regarding restless legs syndrome though, non-Hispanic Whites were more likely to have heard of the disorder, and when the symptoms were described, they were also more likely to have known that such a disorder exists. When the sample of Mexican Americans was dichotomized as either being more acculturated (to American culture) or less acculturated, those who were more acculturated responded in general like the non-Hispanic Whites, with similar rates of knowledge about insomnia, but much more knowledge about sleep apnea and restless legs syndrome.
4.3. Demand characteristics and measurement issues
Even the definition of “what is a sleep problem” likely varies across cultures. In a study of child sleep problems reported by parents, Sadeh and colleagues evaluated survey responses indicating whether parents believed that their children had a sleep problem across several countries [113]. These countries were classified as “primarily Caucasian” (United States, United Kingdom, New Zealand, Canada, and Australia) or “primarily Asian” (Vietnam, Thailand, Taiwan, Singapore, Philippines, Malaysia, Korea, Japan, India, Indonesia, Hong Kong, and China). Of all these, the greatest prevalence of self-reported “severe sleep problem” was found in China, Taiwan, and Hong Kong. The investigators found, though, that the correlates of a self-reported sleep problem varied according to the type of country. For example, in “primarily Caucasian” countries, the presence of a sleep problem was more strongly related to the child’s sleep characteristics, including longest sleep episode, nocturnal wakefulness, number of night wakings, and total sleep time. On the other hand, sleep problems in “primarily Asian” countries were more likely to reflect the child’s age, parental education level, and parent’s age.
The authors suggest that this finding supports the hypothesis that the definition of what a problem is can be culturally bound [113]. Although this is a possibility, there is another possible interpretation: that simply asking a question about sleep problems carries sociocultural implications that interfere with valid assessment. Stated another way, it is possible that although some self-reported sleep assessment measures may demonstrate an apparent face validity to Western/White respondents, this changes when brought to other groups. In this way, the question does not simply ask what it appears to ask. This is consistent with the findings by Grandner and colleagues [111] in the study of older women in Philadelphia, where simply asking about activities in bed did not elicit any differences, but asking about specific activities did. Although the question “I use my bed for sleep and sex only” may be straightforward, in that this should not be meant to include activities such as reading or watching TV, this may not be apparent in some respondents. Furthermore, this hypothesis is consistent with the finding by Grandner and colleagues using nationally representative data, which found that even though Blacks/African Americans were less likely to endorse a “problem falling asleep” they were more likely to report a sleep latency over 30 min, which is frequently seen as the clinical cutoff for a “problem” but may not be considered a “problem” to the respondent. Thus, how the question is asked and interpreted may play a role in what responses are elicited. This makes cross-cultural sleep research very difficult. The next sections address other factors that may be playing a role.
A number of factors may underlie cultural differences in sleep-related knowledge and attitudes. These may include socioeconomics, work/home environment, neighborhood, health literacy, acculturation, bed-sharing, access to health information, trust in Western medicine, trust in traditional medicine, other factors determined by religion and/or culture, and perhaps some differences in sleep as a priority. In individuals concerned about meeting the basic needs in the face of high amounts of social and physiological stress, healthy sleep may seem like more of a luxury than of a goal. Making sleep more of a priority may be a challenge, though. The traditional approach capitalizes on the literature that demonstrates the relationship of sleep to heart disease, blood pressure, cholesterol, cancer, longevity, energy level, and psychiatric outcomes; in short, the argument for better sleep is that “You will be healthier.” It may be useful to capitalize on other findings, though, which suggest relationships to weight gain, family relationships, work performance, sick leave, accidents, sex drive, and income – arguing that “You will be more productive.” This may better address the sorts of issues that are relevant to people who may not value sleep as an important part of their life.
Another way that beliefs and attitudes may impact sleep is that those with poor sleep quality tend to think about sleep more – they attend more readily to sleep-related stimuli, and they are more likely to perceive neutral stimuli as being related to sleep [114–117]. In other words, they experience their sleeplessness as pervasive. They are also more sensitive to sleep priming. For example, one study by Ellis and colleagues replicated the finding that people with insomnia did reliably interpret neutral stimuli as sleep-related, but they also found that this effect can be amplified if the participants are asked to report their sleep problems immediately before taking the test [118].
4.4. Perceived racial discrimination and racism
There have been very few studies to examine the impact of racism or racial discrimination on sleep. The only population-level study was undertaken by Grandner and colleagues, and they examined the independent association of perceived racial discrimination in health care settings on self-reported sleep disturbance (“difficulty falling asleep, staying asleep, or sleeping too much” at least three nights per week) and self-reported daytime tiredness/fatigue (also at least three days per week) [119]. Data from the Michigan and Wisconsin cohorts of the 2006 Behavioral Risk Factor Surveillance System were used, as they were the only states to ask both sleep and racism questions. As expected, self-identified non-Hispanic Whites reported much less racial discrimination (3.25%), compared to Blacks/ African Americans (20.67%). In models that accounted for race, gender, age, education, income, employment, marital status, and state, those who reported racial discrimination in health care settings were approximately twice as likely to report sleep disturbance and 60% more likely to report daytime tiredness/fatigue. As racism is associated with depression, which is also causally related to both sleep disturbance and fatigue, the question remained as to whether the increased risk was simply attributable to depression associated with racism. This was the case for daytime fatigue/tiredness, for which the effect was completely mediated by depression. However, in the case of sleep disturbance, the effect was still statistically significant, with those reporting racism in health care settings being 60% more likely to experience sleep disturbance, even after accounting for all covariates. This finding was expanded upon by Slopen and Williams, who showed that major experiences of discrimination were associated with shorter sleep duration and more sleep difficulties [120].
A few studies have evaluated aspects of this relationship. One previous study examined PSG sleep characteristics that differentiated White and Black/African-American adults, in the context of racial discrimination [121]. The White group demonstrated more slow-wave sleep (stage 3 and 4 sleep) and decreased daytime fatigue, which has important health implications. Interestingly, Thomas and colleagues found that this relationship was completely mediated by perceived racism [121]. In a follow-up study from the same group, the finding that differences in slow-wave sleep were mediated by discrimination was replicated [122]. Another study found that increased sleep disturbances among Hispanics/Latinos completely mediated the relationship between perceived racism and depressed mood [123]. A study from the Pittsburgh SleepSCORE project found that among middle-aged adults, perceived discrimination was associated with worse subjective and objective sleep [124], and that this was partially mediated by nightly worry. Taken together, perceived racism likely leads to sleep disturbance, independent of depression. Further, this sleep disturbance associated with racism not only explains part of the relationship between racism and depression but may also account for racial differences in sleep architecture.
4.5. The role of the physical environment
One set of factors that may be associated with race/ethnicity is represented by the physical and social environment. This can be reflected on many levels: the bedroom, the home, the neighborhood, the county, the state, and beyond.
In the bedroom, co-sleeping likely impacts sleep quality in a negative way [89,92,125,126], which is reflected by the finding that an increased household size is negatively associated with sleep sufficiency [127]. In addition, several studies have shown that noise in the sleep environment can cause reliable and profound changes to sleep, even if it does not cause frank awakenings [128–131]. For example, loud noise outside the bedroom may result in stage transitions, electroencephalographic arousals, and other changes in sleep architecture that reduce the restful quality of sleep. Excess light in the bedroom may also inhibit melatonin production at night [132–134], which may also interfere with sleep continuity and architecture. Interestingly, there are almost no data on mattresses. In general “comfortable” mattresses produce better sleep than “uncomfortable” mattresses, though these definitions seem to be completely subjective [135]. The bedroom may also serve to be a unique emotional stressor. One study found that exposure to intimate partner violence at any point across a lifetime accounted for a one- to twofold increased likelihood of current sleep disturbance; this was increased to a three- to sevenfold increase if the violence occurred in the past year [136].
In the home, several factors play a role in sleep. As mentioned above, more crowded households tend to be associated with more insufficient sleep [127]. Further, relationship quality and the presence of family members in the home as a support system may have profound implications for sleep [137]. However, being in a home with an infant or a child that is having sleep difficulty may interfere with sleep [138–141], as is being a caregiver [142], growing up with a depressed family member [143], and living in a home with someone who works long hours [144,145].
Several studies have explored the relationship between aspects of neighborhoods and sleep, and the potential role in health. In a study that examined neighborhoods in Texas, Hill and colleagues examined the role of perceived neighborhood disorder and psychological distress [146]. They found that neighborhood disorder, defined as the degree to which neighborhoods are perceived by residents to be socially disorganized, hazardous, crime-ridden, dirty, noisy, and in disrepair, was associated with general psychological distress and sleep disturbance in particular. Further, the association between neighborhood disorder and psychological distress was partially mediated by sleep disturbance. In a follow-up study in the same cohort, Hale and colleagues [147] also found that sleep disturbance partially mediated the relationship of neighborhood disorder to poor physical health, even after accounting for other unhealthy behaviors (irregular exercise, poor diet, smoking, binge alcohol drinking, obesity, and other factors). These findings were replicated in an analysis of the Study of the Health Of Wisconsin study, which found that poor neighborhood quality was associated with poor sleep quality, and that this relationship partially mediated the relationship between neighborhood and both physical and mental health [148].
At the regional level, recent studies have shown that geography explains sleep disturbance [84] and insufficient sleep [149] in the United States. Specifically, a state-by-state analysis by Grandner and colleagues [84] examined 36 US states to show that those in southern states were more likely to report difficulty sleeping over the past two weeks. The states with the highest rates of sleep disturbance included West Virginia, Oklahoma, Missouri, Arkansas, Mississippi and Alabama, but notably data on some nearby states (eg, Kentucky or Ohio) were unavailable, making it difficult to observe clustering of insufficient sleep across states. Explanations for geographic variation in sleep disturbance revealed that a whole host of factors may be relevant to these geographical differences, including differences in racial makeup of the population, temperature and weather patterns, regional health issues, regional health care access, and others [84]. This was followed up by an analysis from the 2009 Behavioral Risk Factor Surveillance System, which examined perceived insufficient sleep, which was measured at the county level [149]. Geospatial regression analyses tested for the presence of geographic hot and cold spots, which contain statistically unlikely high or low prevalence of insufficient sleep. There were several notable hot spots, particularly one very large concentration in the Central Appalachia region that connects Tennessee, Virginia, West Virginia, Kentucky, and Ohio. Other hot spots were identified, particularly in the southeast and Midwest of the US. A number of cold spots were also identified, primarily in the Midwest, Texas, and northern Virginia.
5. The role of socioeconomics
When attempting to model SEP, researchers frequently investigate individual socioeconomic factors. These typically include education level, household income, and occupational status. Previous studies that have examined associations between sleep quality and socioeconomic factors have tended to report that lower SEP is associated with higher rates of sleep disturbance (represented as either general overall sleep disturbance or specific symptoms such as difficulty falling asleep, staying asleep, or waking too early) [54,69,83,150–154]. In addition, several studies have shown that those of lower SEP are more likely to report less sleep [60,155]. Krueger and Friedman found that the mean family income was highest among 7-h sleepers and lowest among the shortest and longest sleepers [156]. Similarly, Stamatakis and colleagues found that a short sleep duration was most commonly reported among the lowest quintile of income [60]. Although few studies have measured this relationship using sleep assessed with PSG, these have also generally found that a lower SEP is associated with poorer sleep quality [52,54,153,157].
In the aforementioned study of general sleep disturbance measured using the BRFSS 2006 [69], an increased sleep disturbance was more frequently reported among those who did not graduate from college, received lower income (especially <$25,000 among men), and were unemployed. In the study by Whinnery and colleagues [155], in fully adjusted models, very short sleep (<5 h) was more likely to be reported among those earning <$20,000, as well as $65,000–75,000 (relative to >$75,000). It was also more frequently reported among those who did not complete college, those with public health insurance only (relative to no health insurance at all), and those with a marginal or very low food security. Short sleep (5–6 h) was also more likely to be reported among those who attended high school but did not graduate from college, and those with very low food security. Long sleep was more frequently reported among those earning $20,000–$25,000 per year and those with public insurance only. In a complementary study by Grandner and colleagues [70], habitual sleep latency of >30 min was associated with less than a college education, lack of access to private health insurance, and marginal, low, and/or very low food security. Insomnia symptoms (including difficulty falling asleep, difficulty maintaining sleep, and early morning awakenings) were associated with food security as well. Non-restorative sleep, daytime sleepiness, and sleep apnea symptoms including snorting/gasping and snoring were associated with lower education levels and food insecurity. Gellis and colleagues found that insomnia was negatively associated with educational attainment [83]. Lallukka and colleagues found that among men, childhood economic difficulties predicted adult insomnia symptoms, and among women both childhood and current economic difficulties predicted adult insomnia symptoms [158]. These findings echo those of Tomfohr and colleagues, who found that a lower childhood SEP (operationalized as highest educational attainment by either parent) was associated with decreased slow-wave sleep and increased stage 2 sleep [157].
One aspect of socioeconomics in relation to race that is often neglected is the impact of shift work and multiple jobs. Racial/ ethnic minorities are more likely to work later shifts, multiple jobs, and long work hours, which can have profound implications for sleep opportunity and timing, which are important for both sleep duration and sleep quality [159,160]. Although these factors are often characterized as occupational, they may be better characterized as socioeconomic. This is because it is only rare that an individual would choose such a work schedule; rather, this schedule is usually a result of a lack of more preferred options. This may be less the case for military, doctors, nurses, and other jobs with round-the-clock operations, but these usually come with better access to health care and better pay. It should also be noted that racial/ethnic minorities are more likely to engage in jobs that are more physically demanding. Barilla and colleagues recently reported that individuals with manual labor jobs were more likely to also report short sleep duration [161].
Relationships between sleep and some socioeconomic factors may depend on sex, and this may further depend on race/ethnicity. For example, Kim and Ruger [162] found that among Korean men, insufficient sleep increased along with education level even though the opposite relationship was seen for women (with lower insufficient sleep among those with a higher educational attainment). This echoes the previous work which shows that among women, elevated sleep disturbances associated with lower educational levels are more pronounced among Asian-American women [69]. It should be noted, though, that this study also found that Latina women with a lower educational attainment did not show elevated sleep disturbance.
Several studies have explored socioeconomic factors associated with adherence to therapy for obstructive sleep apnea. For example, Platt and colleagues found that treatment adherence was negatively associated with neighborhood socioeconomic indicators, assessed at the census block level. Further, Simon-Tuval and colleagues found that low-income adults were more likely to decline treatment for obstructive sleep apnea, and of those who declined, 29% indicated that this was due to costs [163]. Socioeconomic factors may also dictate who is referred for sleep apnea. For example, Brouillette and colleagues found that children of a lower socioeconomic status were less likely to be referred for sleep apnea treatment [164].
Further comment on the interactive role of race/ethnicity and socioeconomics is needed, with a caveat regarding interpretation of data. The relationship between race/ethnicity and socioeconomic status is complex. For example, at least in the US, some racial/ ethnic groups are much more likely to also be socioeconomically disadvantaged than others. Further, some degree of disparity seen among groups is likely a by-product either of the socioeconomic disadvantage or of a parallel process, such as racism, issues regarding acculturation, and the ability to “pass” as white. Further research is needed to disentangle the role of race/ethnicity from that of socioeconomic status in the risk of disadvantageous sleep. There is some evidence that minority groups that generally experience less socioeconomic disadvantage than non-Hispanic Whites (eg, Asians) may be at less risk than other groups, and they may even present with lower risks than non-Hispanic Whites in the US [165].
6. Other contextual factors
In addition to race/ethnicity, racism, socioeconomics, knowledge, beliefs and attitudes, the home environment, family factors, occupational factors, neighborhood, and geographic region, other factors have been examined as well. For example, sleep has been described as a component of healthy behavior. Other healthy behaviors have been examined relative to sleep. Those with the healthiest dietary habits also tend to report the best quality sleep [166,167]. Also, those who are sedentary report the highest rates of sleep disturbance and daytime fatigue [168]. Smokers are more likely to report insomnia [169–172] and insufficient sleep [127]. Short sleepers tend to consume more alcohol [173], and high-risk alcohol consumption is associated with insomnia symptoms [169] and adverse sleep architecture changes [174].
The increasing role of technology in the bedroom is likely interfering with sleep. This is relevant because mobile technology is becoming rapidly adopted among minority groups, with steep increases seen among Blacks/African Americans [175] and Hispanics/ Latinos [176]. Further, as mobile technology (eg, smartphones) becomes readily available to those of a lower socioeconomic status, most individuals use these devices on a regular basis [177], and those already at risk of poor sleep outcomes may experience an additional detrimental effect of technology use that interferes with sleep. In a recent study by Gradisar and colleagues [178], a national survey from the National Sleep Foundation found that approximately 90% of Americans report some technology use in the hour before bed. Of the types of technology used, TV was the most popular, though young adults were most likely to use cell phones. The authors found that the more types of devices used, the more sleep problems were also reported. This supports previous studies that have found adverse relationships between technology use at night and sleep. Brunborg and colleagues [179] found that young adults who used a computer in the bedroom often also reported that they got out of bed later on both weekdays and weekends, turned off the lights to go to sleep later on weekends, slept more hours on weekends, and had a greater discrepancy between time turning off the lights to go to sleep on weekdays versus weekends. A study by Munezawa and colleagues [180] found that mobile phone use after lights out was associated with shorter sleep duration and poorer sleep quality. It did not matter if the use was calling or texting.
Many questions still remain. Underlying these questions is the recognition that no matter how race/ethnicity is operationalized, how socioeconomic factors are measured, and how many potentially intervening contextual factors are captured, these are heterogeneous and complex issues. Perhaps, a more thorough measurement, a more comprehensive assessment, and more nuanced statistics will be useful. However, there will likely still be inconsistencies when trying to discern relatively straightforward interpretations of findings describing associations that seem to be anything but straightforward. For example, if environmental and contextual factors are such a powerful explanatory factor in differences in sleep, it should be the case that laboratory studies (where most or all of these adverse contextual factors are not present) should not reveal differences. It is possible that effects of some factors (such as racism) will linger or produce systemic physiological changes over time. Although these changes should be susceptible to modeling, no consistent set of paths has yet emerged. This highlights an important agenda for future research. It will be important not only to investigate which contextual factors generally play a role, but also the conditions that modify the effects of these factors. Additionally, whether (and how) some of these contextual factors produce short-lived or even long-term physiological changes that could affect sleep (and other aspects of health) will be important for discerning which associations are circumstantial and which are the result of systemic effects. Further, it is clear that effects are not uniformly experienced among individuals of any group; therefore, it is imperative to understand what modifies these effects at the individual level, be they genetic, psychological, environmental, or other protective factors.
7. Moving forward
Taken together, there is a relatively small but growing body of literature that casts sleep in a social–environmental context, where factors such as race/ethnicity, as well as socioeconomics, home and family, school and work, neighborhood, culture, and other factors play a role. As sleep is so important to health and functioning, understanding the role of these contextual factors is critically important to improving health. Further, because of the well-documented existence of health disparities, understanding the relationship between the role of sleep in population health and contextual factors is essential to developing successful interventions for improving sleep and reducing health inequalities.
7.1. Clinical implications of existing evidence
The research we discussed suggests that many people, especially racial/ethnic minorities and the socioeconomically disadvantaged, have difficulty achieving healthy sleep. Clinicians should be aware of the importance of sleep, and they should include sleep assessments as part of any lifestyle or preventive care assessment. Clinicians should develop practices which recognize that racial/ ethnic minorities are more likely to present with high-risk sleep characteristics (including short sleep duration and sleep disorders), even if they do not specifically endorse complaints, without making biological assumptions about patients based on their race. Clinicians should counsel all their patients regarding healthy sleep. They need to take the patients’ structural, social, and environmental context into consideration, as occupational and/or home demands, environmental disturbances, and other social factors may all present challenges to achieving healthy sleep. As more information regarding the pathways linking contextual factors and sleep is learned, clinicians should include these in their evaluations. For example, future assessments of sleep may include questions about racism, neighborhood, occupational stress, and other factors.
7.2. Research agenda
There is much need for future research examining the role of race, racism, and socioeconomic disadvantage in sleep and the role of sleep in health disparities. Several important questions need to be addressed in order to develop a research agenda for examining these issues.
What are the reasons for the differences in sleep studies have identified according to self-identified race/ethnicity? Researchers need to better unpack the concept of race/ethnicity as it relates to sleep. Some research findings remain consistent and some become very inconsistent upon attempted replication. This may be because the role of self-identified race/ethnicity may change, depending on other social–environmental factors in which this construct is embedded. For example, to what degree do the relationships between race/ethnicity and sleep identified by researchers generalize across neighborhoods, across regions, and across nations? And if they do generalize, what are the mechanisms that create differences according to race/ethnicity?
How can sleep assessments maintain validity across different groups? As mentioned above, simply asking about sleep may not be sufficient to obtain reliable and valid estimates of sleep. This seems to be especially the case for the assessment of sleep difficulties. Future research is needed to identify ways of measuring sleep that can be applied to more people, so that findings can be generalizable across groups.
What are the relevant social and environmental factors that present the most important barriers to healthy sleep? It is highly unlikely that observed racial and socioeconomic differences in sleep are caused by genetic differences. More likely, social and environmental factors represent the relevant forces determining group differences in sleep behaviors. Identifying which of these are most significant will help researchers, clinicians, and policy-makers develop successful interventions to close the gaps in health sleep.
What is the role of sleep as a modifiable risk factor in health disparities? Health disparities remain an important injustice, and initiatives are needed to reduce these inequities. Although sleep disparities stem from structural, social, and environmental factors that are challenging to change, sleep represents, to some extent, a modifiable risk factor. Research is needed to see whether sleep-related interventions can serve to prevent other adverse health outcomes. At the same time, research and policy must address the contextual forces that lead to the inequitable experience of sleep.
Conclusions
Sleep is an essential pillar of health. Because of the critical significance of sleep, understanding the relationship of race/ethnicity, racism, and socioeconomic disadvantage to sleep is an important part of understanding and eliminating health inequities. This task requires conceptualizing sleep in a social–environmental framework that recognizes that the quantity and quality of sleep, like diet, depend on a set of behaviors that are influenced by the structural, social, and environmental context. A number of studies have discovered that self-identified race/ethnicity and socioeconomic factors are associated with differing sleep patterns, with racial/ethnic minorities and the socioeconomically disadvantaged tending to get less sleep and experiencing a higher risk of sleep problems. Because race is a social category rather than an innate genetic trait, researchers must more carefully unpack the function race can serve in identifying the reasons for these sleep disparities. We recommend a research agenda that examines the role of race, racism, and socioeconomic disadvantage in sleep and the role of sleep in health disparities, and we suggest several important questions that need to be addressed.
Acknowledgments
Dr. Grandner is supported by the National Heart, Lung, and Blood Institute (K23HL110216) and the National Institute of Environmental Health Science (R21ES022931). He is also supported by the University of Pennsylvania Clinical and Translational Research Center (UL1RR024134). Dr. Knutson is supported by the National Institute for Diabetes and Digestive and Kidney Diseases (R01DK095207). Dr. Jean-Louis and Dr. Williams are supported by the National Heart, Lung, and Blood Institute (R01HL095799) and the National Institute of Minority Health and Health Disparities (R01MD004113).
Footnotes
Conflict of interest
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: http://dx.doi.org/10.1016/j.sleep.2015.01.020.
References
- 1.Centers for Disease Control and Prevention. CDC health disparities and inequalities report – United States. Atlanta, GA: CDC; 2011. p. 2011. [Google Scholar]
- 2.Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–52. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 3.Smedley BD, Stith AY, Nelson AR Institute of Medicine (U.S.) Unequal treatment: confronting racial and ethnic disparities in health care. Washington, D.C: National Academy Press; 2003. Committee on understanding and eliminating racial and ethnic disparities in health care. [PubMed] [Google Scholar]
- 4.Ong KL, Cheung BM, Wong LY, Wat NM, Tan KC, Lam KS. Prevalence, treatment, and control of diagnosed diabetes in the U.S. National Health and Nutrition Examination Survey 1999–2004. Ann Epidemiol. 2008;18:222–9. doi: 10.1016/j.annepidem.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 6.Jackson JS, Hudson D, Kershaw K, Mezuk B, Rafferty J, Tuttle KK. Discrimination, chronic stress, and mortality among black Americans: A life course framework. In: Rogers RG, Crimmins EM, editors. International handbook of adult mortality. NY: Springer; 2011. pp. 311–28. [Google Scholar]
- 7.Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100:933–9. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finch BK, Phuong Do D, Heron M, Bird C, Seeman T, Lurie N. Neighborhood effects on health: concentrated advantage and disadvantage. Health Place. 2010;16:1058–60. doi: 10.1016/j.healthplace.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123(Suppl 3):S174–84. doi: 10.1542/peds.2008-2233H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Colten HR, Altevogt BM. Sleep disorders and sleep deprivation: an unmet public health problem. Washington, DC: Institute of Medicine: National Academies Press; 2006. Institute of medicine committee on sleep medicine and research. [PubMed] [Google Scholar]
- 11.Ulmer C, Wolman DM, Johns MME. Resident duty hours: enhancing sleep, supervision, and safety. Washington, D.C: National Academies Press; 2009. Institute of medicine committee on optimizing graduate medical trainee (resident) hours and work schedules to improve patient safety. [PubMed] [Google Scholar]
- 12.Office of Disease Prevention and Health Promotion. Healthy people 2020 objective topic areas. Washington, DC: US Department of Health and Human Services; 2011. [Google Scholar]
- 13.Zee PC, Badr MS, Kushida C, et al. Strategic opportunities in sleep and circadian research: report of the joint task force of the sleep research society and American academy of sleep medicine. Sleep. 2014;37:219–27. doi: 10.5665/sleep.3384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel SR. Reduced sleep as an obesity risk factor. Obes Rev. 2009;10(Suppl 2):61–8. doi: 10.1111/j.1467-789X.2009.00664.x. [DOI] [PubMed] [Google Scholar]
- 15.Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014;15:42–50. doi: 10.1016/j.sleep.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Altman NG, Izci-Balserak B, Schopfer E, et al. Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes. Sleep Med. 2012;13:1261–70. doi: 10.1016/j.sleep.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meng L, Zheng Y, Hui R. The relationship of sleep duration and insomnia to risk of hypertension incidence: a meta-analysis of prospective cohort studies. Hypertens Res. 2013;36:985–95. doi: 10.1038/hr.2013.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grandner MA, Sands-Lincoln MR, Pak VM, Garland SN. Sleep duration, cardiovascular disease, and proinflammatory biomarkers. Nat Sci Sleep. 2013;5:93–107. doi: 10.2147/NSS.S31063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morselli LL, Guyon A, Spiegel K. Sleep and metabolic function. Pflugers Arch. 2012;463:139–60. doi: 10.1007/s00424-011-1053-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zizi F, Pandey A, Murrray-Bachmann R, et al. Race/ethnicity, sleep duration, and diabetes mellitus: analysis of the National Health Interview Survey. Am J Med. 2012;125:162–7. doi: 10.1016/j.amjmed.2011.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71:1027–36. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 22.Hamazaki Y, Morikawa Y, Nakamura K, et al. The effects of sleep duration on the incidence of cardiovascular events among middle-aged male workers in Japan. Scand J Work Environ Health. 2011;37:411–17. doi: 10.5271/sjweh.3168. [DOI] [PubMed] [Google Scholar]
- 23.Meisinger C, Heier M, Lowel H, Schneider A, Doring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population: the MONICA/KORA Augsburg cohort study. Sleep. 2007;30:1121–7. doi: 10.1093/sleep/30.9.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 25.Grandner MA, Patel NP. From sleep duration to mortality: implications of meta-analysis and future directions. J Sleep Res. 2009;18:145–7. doi: 10.1111/j.1365-2869.2009.00753.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cappuccio FP, Miller MA. Sleep and mortality: cause, consequence, or symptom? Sleep Med. 2013;14:587–8. doi: 10.1016/j.sleep.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 27.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grandner MA, Patel NP, Hale L, Moore M. Mortality associated with sleep duration: the evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010;14:191–203. doi: 10.1016/j.smrv.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maia Q, Lam B, Grandner MA, Findley J, Gurubhagavatula I. Short sleep duration associated with drowsy driving and the role of perceived sleep insufficiency. Sleep. 2013;36:A328. doi: 10.1016/j.aap.2013.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Banks S, Van Dongen HP, Maislin G, Dinges DF. Neurobehavioral dynamics following chronic sleep restriction: dose-response effects of one night for recovery. Sleep. 2010;33:1013–26. doi: 10.1093/sleep/33.8.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–28. [PMC free article] [PubMed] [Google Scholar]
- 32.Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI. Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. Sleep Med Rev. 2010;14:239–47. doi: 10.1016/j.smrv.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Knutson KL. Does inadequate sleep play a role in vulnerability to obesity? Am J Hum Biol. 2012;24:361–71. doi: 10.1002/ajhb.22219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab. 2010;24:731–43. doi: 10.1016/j.beem.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grandner MA. Addressing sleep disturbances: an opportunity to prevent cardiometabolic disease? Int Rev Psychiatry. 2014;26:155–76. doi: 10.3109/09540261.2014.911148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roberts DE. Fatal invention: how science, politics, and big business re-create race in the twenty-first century. New York: New Press; 2011. [Google Scholar]
- 37.Zuberi T. Thicker than blood: how racial statistics lie. Minneapolis: University of Minnesota Press; 2001. [Google Scholar]
- 38.Kaplan JB. The quality of data on “race” and “ethnicity”: Implications for health researchers, policy makers, and practitioners. Race Soc Probl. 2014;6:214–36. [Google Scholar]
- 39.Barbujani G, Magagni A, Minch E, Cavalli-Sforza LL. An apportionment of human DNA diversity. Proc Natl Acad Sci U S A. 1997;94:4516–19. doi: 10.1073/pnas.94.9.4516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fullilove MT. Comment: abandoning “race” as a variable in public health research–an idea whose time has come. Am J Public Health. 1998;88:1297–8. doi: 10.2105/ajph.88.9.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Romero AJ, Roberts RE. Perception of discrimination and ethnocultural variables in a diverse group of adolescents. J Adolesc. 1998;21:641–56. doi: 10.1006/jado.1998.0185. [DOI] [PubMed] [Google Scholar]
- 42.Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: toward antiracism praxis. Am J Public Health. 2010;100(Suppl 1):S30–5. doi: 10.2105/AJPH.2009.171058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Agnew HW, Jr, Webb WB, Williams RL. The first night effect: an EEG study of sleep. Psychophysiology. 1966;2:263–6. doi: 10.1111/j.1469-8986.1966.tb02650.x. [DOI] [PubMed] [Google Scholar]
- 44.Hauri PJ, Olmstead EM. Reverse first night effect in insomnia. Sleep. 1989;12:97–105. doi: 10.1093/sleep/12.2.97. [DOI] [PubMed] [Google Scholar]
- 45.Irwin M, Miller C, Gillin JC, Demodena A, Ehlers CL. Polysomnographic and spectral sleep EEG in primary alcoholics: an interaction between alcohol dependence and African-American ethnicity. Alcohol Clin Exp Res. 2000;24:1376–84. [PubMed] [Google Scholar]
- 46.Profant J, Ancoli-Israel S, Dimsdale JE. Are there ethnic differences in sleep architecture? Am J Hum Biol. 2002;14:321–6. doi: 10.1002/ajhb.10032. [DOI] [PubMed] [Google Scholar]
- 47.Stepnowsky CJ, Jr, Moore PJ, Dimsdale JE. Effect of ethnicity on sleep: complexities for epidemiologic research. Sleep. 2003;26:329–32. doi: 10.1093/sleep/26.3.329. [DOI] [PubMed] [Google Scholar]
- 48.Rao U, Poland RE, Lutchmansingh P, Ott GE, McCracken JT, Lin KM. Relationship between ethnicity and sleep patterns in normal controls: implications for psychopathology and treatment. J Psychiatr Res. 1999;33:419–26. doi: 10.1016/s0022-3956(99)00019-9. [DOI] [PubMed] [Google Scholar]
- 49.Ruiter ME, Decoster J, Jacobs L, Lichstein KL. Normal sleep in African-Americans and Caucasian-Americans: a meta-analysis. Sleep Med. 2011;12:209–14. doi: 10.1016/j.sleep.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 50.Hong S, Mills PJ, Loredo JS, Adler KA, Dimsdale JE. The association between interleukin-6, sleep, and demographic characteristics. Brain Behav Immun. 2005;19:165–72. doi: 10.1016/j.bbi.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 51.Mokhlesi B, Pannain S, Ghods F, Knutson KL. Predictors of slow-wave sleep in a clinic-based sample. J Sleep Res. 2012;21:170–5. doi: 10.1111/j.1365-2869.2011.00959.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mezick EJ, Matthews KA, Hall M, et al. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosom Med. 2008;70:410–16. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch Intern Med. 2004;164:406–18. doi: 10.1001/archinte.164.4.406. [DOI] [PubMed] [Google Scholar]
- 54.Hall MH, Matthews KA, Kravitz HM, et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32:73–82. [PMC free article] [PubMed] [Google Scholar]
- 55.Jean-Louis G, Kripke DF, Ancoli-Israel S, Klauber MR, Sepulveda RS. Sleep duration, illumination, and activity patterns in a population sample: effects of gender and ethnicity. Biol Psychiatry. 2000;47:921–7. doi: 10.1016/s0006-3223(99)00169-9. [DOI] [PubMed] [Google Scholar]
- 56.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 57.Ertel KA, Berkman LF, Buxton OM. Socioeconomic status, occupational characteristics, and sleep duration in African/Caribbean immigrants and US White health care workers. Sleep. 2011;34:509–18. doi: 10.1093/sleep/34.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nunes J, Jean-Louis G, Zizi F, et al. Sleep duration among black and white Americans: results of the National Health Interview Survey. J Natl Med Assoc. 2008;100:317–22. doi: 10.1016/s0027-9684(15)31244-x. [DOI] [PubMed] [Google Scholar]
- 60.Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17:948–55. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37:601–11. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stamatakis KA, Punjabi NM. Long sleep duration: a risk to health or a marker of risk? Sleep Med Rev. 2007;11:337–9. doi: 10.1016/j.smrv.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jaussent I, Empana JP, Ancelin ML, et al. Insomnia, daytime sleepiness and cardio-cerebrovascular diseases in the elderly: a 6-year prospective study. PLoS ONE. 2013;8:e56048. doi: 10.1371/journal.pone.0056048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kita T, Yoshioka E, Satoh H, et al. Short sleep duration and poor sleep quality increase the risk of diabetes in Japanese workers with no family history of diabetes. Diabetes Care. 2012;35:313–18. doi: 10.2337/dc11-1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Watanabe M, Kikuchi H, Tanaka K, Takahashi M. Association of short sleep duration with weight gain and obesity at 1-year follow-up: A large-scale prospective study. Sleep. 2010;33:161–7. doi: 10.1093/sleep/33.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Knutson KL, Van Cauter E, Rathouz PJ, et al. Association between sleep and blood pressure in midlife: the CARDIA sleep study. Arch Intern Med. 2009;169:1055–61. doi: 10.1001/archinternmed.2009.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grandner MA, Buxton OM, Jackson N, Sands-Lincoln M, Pandey A, Jean-Louis G. Extreme sleep durations and increased C-reactive protein: effects of sex and ethnoracial group. Sleep. 2013;36:769–79. doi: 10.5665/sleep.2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Sleep disorders in African Americans and Caucasian Americans: a meta-analysis. Behav Sleep Med. 2010;8:246–59. doi: 10.1080/15402002.2010.509251. [DOI] [PubMed] [Google Scholar]
- 69.Grandner MA, Patel NP, Gehrman PR, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep disturbance. Sleep Med. 2010;11:470–9. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Grandner MA, Petrov ME, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9:897–905. A–D. doi: 10.5664/jcsm.2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wallace DM, Wohlgemuth WK. Does race-ethnicity moderate the relationship between CPAP adherence and functional outcomes of sleep in US veterans with obstructive sleep apnea syndrome? J Clin Sleep Med. 2014;10:1083–91. doi: 10.5664/jcsm.4106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Billings ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34:1653–8. doi: 10.5665/sleep.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Means MK, Ulmer CS, Edinger JD. Ethnic differences in continuous positive airway pressure (CPAP) adherence in veterans with and without psychiatric disorders. Behav Sleep Med. 2010;8:260–73. doi: 10.1080/15402002.2010.509255. [DOI] [PubMed] [Google Scholar]
- 74.Shaw R, McKenzie S, Taylor T, et al. Beliefs and attitudes toward obstructive sleep apnea evaluation and treatment among blacks. J Natl Med Assoc. 2012;104:510–19. doi: 10.1016/s0027-9684(15)30217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Billings ME, Rosen CL, Wang R, et al. Is the relationship between race and continuous positive airway pressure adherence mediated by sleep duration? Sleep. 2013;36:221–7. doi: 10.5665/sleep.2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wallace DM, Vargas SS, Schwartz SJ, Aloia MS, Shafazand S. Determinants of continuous positive airway pressure adherence in a sleep clinic cohort of South Florida Hispanic veterans. Sleep Breath. 2013;17:351–63. doi: 10.1007/s11325-012-0702-6. [DOI] [PubMed] [Google Scholar]
- 77.Bakker JP, O’Keeffe KM, Neill AM, Campbell AJ. Ethnic disparities in CPAP adherence in New Zealand: effects of socioeconomic status, health literacy and self-efficacy. Sleep. 2011;34:1595–603. doi: 10.5665/sleep.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kripke DF, Jean-Louis G, Elliott JA, et al. Ethnicity, sleep, mood, and illumination in postmenopausal women. BMC Psychiatry. 2004;4:8. doi: 10.1186/1471-244X-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Boss EF, Smith DF, Ishman SL. Racial/ethnic and socioeconomic disparities in the diagnosis and treatment of sleep-disordered breathing in children. Int J Pediatr Otorhinolaryngol. 2011;75:299–307. doi: 10.1016/j.ijporl.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 80.Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010;10:475. doi: 10.1186/1471-2458-10-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C, Redline S. Correlates of adolescent sleep time and variability in sleep time: The role of individual and health related characteristics. Sleep Med. 2011;12:239–45. doi: 10.1016/j.sleep.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hale L, Rivero-Fuentes E. Negative acculturation in sleep duration among Mexican immigrants and Mexican Americans. J Immigr Minor Health. 2011;13:402–7. doi: 10.1007/s10903-009-9284-1. [DOI] [PubMed] [Google Scholar]
- 83.Gellis LA, Lichstein KL, Scarinci IC, et al. Socioeconomic status and insomnia. J Abnorm Psychol. 2005;114:111–18. doi: 10.1037/0021-843X.114.1.111. [DOI] [PubMed] [Google Scholar]
- 84.Grandner MA, Jackson NJ, Pigeon WR, Gooneratne NS, Patel NP. State and regional prevalence of sleep disturbance and daytime fatigue. J Clin Sleep Med. 2012;8:77–86. doi: 10.5664/jcsm.1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Williams S. Sleep and society: sociological ventures into the (Un)known. London: Taylor & Francis; 2005. [Google Scholar]
- 86.Brunt L, Steger B. Worlds of sleep. Berlin: Frank & Timme; 2008. [Google Scholar]
- 87.Hooker E, Ball HL, Kelly PJ. Sleeping like a baby: attitudes and experiences of bedsharing in northeast England. Med Anthropol. 2001;19:203–22. doi: 10.1080/01459740.2001.9966176. [DOI] [PubMed] [Google Scholar]
- 88.Thoman EB. Co-sleeping, an ancient practice: issues of the past and present, and possibilities for the future. Sleep Med Rev. 2006;10:407–17. doi: 10.1016/j.smrv.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 89.Mindell JA, Sadeh A, Wiegand B, How TH, Goh DY. Cross-cultural differences in infant and toddler sleep. Sleep Med. 2010;11:274–80. doi: 10.1016/j.sleep.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 90.Norton PJ, Grellner KW. A retrospective study on infant bed-sharing in a clinical practice population. Matern Child Health J. 2011;15:507–13. doi: 10.1007/s10995-010-0600-0. [DOI] [PubMed] [Google Scholar]
- 91.Gettler LT, McKenna JJ. Evolutionary perspectives on mother-infant sleep proximity and breastfeeding in a laboratory setting. Am J Phys Anthropol. 2011;144:454–62. doi: 10.1002/ajpa.21426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jain S, Romack R, Jain R. Bed sharing in school-age children–clinical and social implications. J Child Adolesc Psychiatr Nurs. 2011;24:185–9. doi: 10.1111/j.1744-6171.2011.00293.x. [DOI] [PubMed] [Google Scholar]
- 93.Shulman D, Strousma GG. Dream cultures: explorations in the comparative history of dreaming. New York: Oxford University Press; 1999. [Google Scholar]
- 94.Spurgeon A, Harrington JM, Cooper CL. Health and safety problems associated with long working hours: a review of the current position. Occup Environ Med. 1997;54:367–75. doi: 10.1136/oem.54.6.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Goto A, Yasumura S, Nishise Y, Sakihara S. Association of health behavior and social role with total mortality among Japanese elders in Okinawa, Japan. Aging Clin Exp Res. 2003;15:443–50. doi: 10.1007/BF03327366. [DOI] [PubMed] [Google Scholar]
- 96.Lockley SW, Landrigan CP, Barger LK, Czeisler CA. When policy meets physiology: the challenge of reducing resident work hours. Clin Orthop Relat Res. 2006;449:116–27. doi: 10.1097/01.blo.0000224057.32367.84. [DOI] [PubMed] [Google Scholar]
- 97.Ko GT, Chan JC, Chan AW, et al. Association between sleeping hours, working hours and obesity in Hong Kong Chinese: the ‘better health for better Hong Kong’ health promotion campaign. Int J Obes (Lond) 2007;31:254–60. doi: 10.1038/sj.ijo.0803389. [DOI] [PubMed] [Google Scholar]
- 98.Basner M, Dinges DF. Dubious bargain: trading sleep for Leno and Letterman. Sleep. 2009;32:747–52. doi: 10.1093/sleep/32.6.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gangwisch JE. All work and no play makes Jack lose sleep. Sleep. 2009;32:717–18. doi: 10.1093/sleep/32.6.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Virtanen M, Ferrie JE, Gimeno D, et al. Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep. 2009;32:737–45. doi: 10.1093/sleep/32.6.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nakata A. Effects of long work hours and poor sleep characteristics on workplace injury among full-time male employees of small- and medium-scale businesses. J Sleep Res. 2011;20:576–84. doi: 10.1111/j.1365-2869.2011.00910.x. [DOI] [PubMed] [Google Scholar]
- 102.Mahan RP, Carvalhais AB, Queen SE. Sleep reduction in night-shift workers: is it sleep deprivation or a sleep disturbance disorder? Percept Mot Skills. 1990;70:723–30. doi: 10.2466/pms.1990.70.3.723. [DOI] [PubMed] [Google Scholar]
- 103.Rajaratnam SM, Arendt J. Health in a 24-h society. Lancet. 2001;358:999–1005. doi: 10.1016/S0140-6736(01)06108-6. [DOI] [PubMed] [Google Scholar]
- 104.Nag PK, Nag A. Shiftwork in the hot environment. J Hum Ergol (Tokyo) 2001;30:161–6. [PubMed] [Google Scholar]
- 105.Costa G. Shift work and health: current problems and preventive actions. Saf Health Work. 2010;1:112–23. doi: 10.5491/SHAW.2010.1.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Owens J. Sleep in children: cross-cultural perspectives. Sleep Biol Rhythm. 2004;2:165–73. [Google Scholar]
- 107.Milner CE, Cote KA. Benefits of napping in healthy adults: impact of nap length, time of day, age, and experience with napping. J Sleep Res. 2009;18:272–81. doi: 10.1111/j.1365-2869.2008.00718.x. [DOI] [PubMed] [Google Scholar]
- 108.Worthman CM, Brown RA. Sleep budgets in a globalizing world: biocultural interactions influence sleep sufficiency among Egyptian families. Soc Sci Med. 2013;79:31–9. doi: 10.1016/j.socscimed.2012.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Pandey A, Gekhman D, Gousse Y, et al. Short sleep and dysfunctional beliefs and attitudes toward sleep among Black men. Sleep. 2011;34:261–2. [Google Scholar]
- 110.Morin CM, Vallieres A, Ivers H. Dysfunctional beliefs and attitudes about sleep (DBAS): validation of a brief version (DBAS-16) Sleep. 2007;30:1547–54. doi: 10.1093/sleep/30.11.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Grandner MA, Patel NP, Jean-Louis G, et al. Sleep-related behaviors and beliefs associated with race/ethnicity in women. J Natl Med Assoc. 2013;105:4–15. doi: 10.1016/s0027-9684(15)30080-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sell RE, Bardwell W, Palinkas L, Ancoli-Israel S, Dimsdale J, Loredo JS. Ethnic differences in sleep-health knowledge. Sleep. 2009;32:A392. [Google Scholar]
- 113.Sadeh A, Mindell J, Rivera L. “My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep Med. 2011;12:478–82. doi: 10.1016/j.sleep.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 114.Espie CA. Understanding insomnia through cognitive modelling. Sleep Med. 2007;8(Suppl 4):S3–8. doi: 10.1016/S1389-9457(08)70002-9. [DOI] [PubMed] [Google Scholar]
- 115.Harvey AG, Tang NK. (Mis)perception of sleep in insomnia: a puzzle and a resolution. Psychol Bull. 2012;138:77–101. doi: 10.1037/a0025730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Marchetti LM, Biello SM, Broomfield NM, Macmahon KM, Espie CA. Who is pre-occupied with sleep? A comparison of attention bias in people with psychophysiological insomnia, delayed sleep phase syndrome and good sleepers using the induced change blindness paradigm. J Sleep Res. 2006;15:212–21. doi: 10.1111/j.1365-2869.2006.00510.x. [DOI] [PubMed] [Google Scholar]
- 117.Woods H, Marchetti LM, Biello SM, Espie CA. The clock as a focus of selective attention in those with primary insomnia: an experimental study using a modified Posner paradigm. Behav Res Ther. 2009;47:231–6. doi: 10.1016/j.brat.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 118.Ellis J, Gardani M, Hogh H. Priming affects poor sleepers but not normal sleepers on an insomnia ambiguity task. J Sleep Res. 2010;19:27–30. doi: 10.1111/j.1365-2869.2009.00792.x. [DOI] [PubMed] [Google Scholar]
- 119.Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behav Sleep Med. 2012;10:235–49. doi: 10.1080/15402002.2012.654548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Slopen N, Williams DR. Discrimination, other psychosocial stressors, and self-reported sleep duration and difficulties. Sleep. 2014;37:147–56. doi: 10.5665/sleep.3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Thomas KS, Bardwell WA, Ancoli-Israel S, Dimsdale JE. The toll of ethnic discrimination on sleep architecture and fatigue. Health Psychol. 2006;25:635–42. doi: 10.1037/0278-6133.25.5.635. [DOI] [PubMed] [Google Scholar]
- 122.Tomfohr L, Pung MA, Edwards KM, Dimsdale JE. Racial differences in sleep architecture: the role of ethnic discrimination. Biol Psychol. 2012;89:34–8. doi: 10.1016/j.biopsycho.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Steffen PR, Bowden M. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethn Dis. 2006;16:16–21. [PubMed] [Google Scholar]
- 124.Beatty DL, Hall MH, Kamarck TA, et al. Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychol. 2011;30:351–9. doi: 10.1037/a0022976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kelmanson IA. Sleep disturbances in two-month-old infants sharing the bed with parent(s) Minerva Pediatr. 2010;62:161–9. [PubMed] [Google Scholar]
- 126.Mindell JA, Sadeh A, Kohyama J, How TH. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep Med. 2010;11:393–9. doi: 10.1016/j.sleep.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 127.Grandner MA, Lang RA, Jackson NJ, Patel NP, Murray-Bachmann R, Jean-Louis G. Biopsychosocial predictors of insufficient rest or sleep in the American population. Sleep. 2011;34:A260. [Google Scholar]
- 128.Yoder JC, Staisiunas PG, Meltzer DO, Knutson KL, Arora VM. Noise and sleep among adult medical inpatients: far from a quiet night. Arch Intern Med. 2012;172:68–70. doi: 10.1001/archinternmed.2011.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157:170–9. doi: 10.7326/0003-4819-157-3-201208070-00472. [DOI] [PubMed] [Google Scholar]
- 130.Elmenhorst EM, Pennig S, Rolny V, et al. Examining nocturnal railway noise and aircraft noise in the field: Sleep, psychomotor performance, and annoyance. Sci Total Environ. 2012;424:48–56. doi: 10.1016/j.scitotenv.2012.02.024. [DOI] [PubMed] [Google Scholar]
- 131.Basner M, Glatz C, Griefahn B, Penzel T, Samel A. Aircraft noise: effects on macro- and microstructure of sleep. Sleep Med. 2008;9:382–7. doi: 10.1016/j.sleep.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 132.Burgess HJ. Evening ambient light exposure can reduce circadian phase advances to morning light independent of sleep deprivation. J Sleep Res. 2013;22:83–8. doi: 10.1111/j.1365-2869.2012.01042.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Chang AM, Santhi N, St Hilaire M, et al. Human responses to bright light of different durations. J Physiol. 2012;590:3103–12. doi: 10.1113/jphysiol.2011.226555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Evans JA, Elliott JA, Gorman MR. Circadian effects of light no brighter than moonlight. J Biol Rhythms. 2007;22:356–67. doi: 10.1177/0748730407301988. [DOI] [PubMed] [Google Scholar]
- 135.Pigeon WR, Grandner MA. Creating an optimal sleep environment. In: Kushida CA, editor. Encyclopedia of sleep. Oxford: Elsevier; 2013. pp. 72–6. [Google Scholar]
- 136.Oliver L, Segal AG, Grandner MA, Perlis M. Sleep disturbance partially mediates the relationship between intimate partner violence and physical/mental health. Sleep. 2013;36:A308. doi: 10.1177/0886260515592651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Troxel WM. It’s more than sex: exploring the dyadic nature of sleep and implications for health. Psychosom Med. 2010;72:578–86. doi: 10.1097/PSY.0b013e3181de7ff8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Insana SP, Montgomery-Downs HE. Sleep and sleepiness among first-time postpartum parents: a field- and laboratory-based multimethod assessment. Dev Psychobiol. 2013;55:361–72. doi: 10.1002/dev.21040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Okun ML, Luther J, Prather AA, Perel JM, Wisniewski S, Wisner KL. Changes in sleep quality, but not hormones predict time to postpartum depression recurrence. J Affect Disord. 2011;130:378–84. doi: 10.1016/j.jad.2010.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Insana SP, Stacom EE, Montgomery-Downs HE. Actual and perceived sleep: associations with daytime functioning among postpartum women. Physiol Behav. 2011;102:234–8. doi: 10.1016/j.physbeh.2010.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Sloan EP. Sleep deprivation and postpartum mental health: case report. Arch Womens Ment Health. 2011;14:509–11. doi: 10.1007/s00737-011-0247-x. [DOI] [PubMed] [Google Scholar]
- 142.von Kaanel R, Mausbach BT, Ancoli-Israel S, et al. Sleep in spousal Alzheimer caregivers: a longitudinal study with a focus on the effects of major patient transitions on sleep. Sleep. 2012;35:247–55. doi: 10.5665/sleep.1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Siu HYK, Chakravorty S, Perlis M, Grandner MA. Growing up with a depressed family member is associated with insufficient sleep and moderates the relationship between insufficient sleep and mental health. Sleep. 2013;36:A299. [Google Scholar]
- 144.Gu JK, Charles LE, Burchfiel CM, et al. Long work hours and adiposity among police officers in a US northeast city. J Occup Environ Med. 2012;54:1374–81. doi: 10.1097/JOM.0b013e31825f2bea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sekine M, Chandola T, Martikainen P, Marmot M, Kagamimori S. Work and family characteristics as determinants of socioeconomic and sex inequalities in sleep: the Japanese Civil Servants Study. Sleep. 2006;29:206–16. doi: 10.1093/sleep/29.2.206. [DOI] [PubMed] [Google Scholar]
- 146.Hill TD, Burdette AM, Hale L. Neighborhood disorder, sleep quality, and psychological distress: testing a model of structural amplification. Health Place. 2009;15:1006–13. doi: 10.1016/j.healthplace.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 147.Hale L, Hill TD, Burdette AM. Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Prev Med. 2010;51:275–8. doi: 10.1016/j.ypmed.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 148.Hale L, Hill TD, Friedman E, et al. Perceived neighborhood quality, sleep quality, and health status: evidence from the Survey of the Health of Wisconsin. Soc Sci Med. 2013;79:16–22. doi: 10.1016/j.socscimed.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Grandner MA, Smith T, Jackson NJ, Jackson T, Burgard S, Branas C. Geographic distribution of insufficient sleep across the USA: a county-level hotspot analysis. Sleep. 2013;36:A335–6. doi: 10.1016/j.sleh.2015.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Nomura K, Yamaoka K, Nakao M, Yano E. Social determinants of self-reported sleep problems in South Korea and Taiwan. J Psychosom Res. 2010;69:435–40. doi: 10.1016/j.jpsychores.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 151.Geroldi C, Frisoni GB, Rozzini R, De Leo D, Trabucchi M. Principal lifetime occupation and sleep quality in the elderly. Gerontology. 1996;42:163–9. doi: 10.1159/000213788. [DOI] [PubMed] [Google Scholar]
- 152.Patel NP, Grandner MA, Gehrman P, et al. Effects of sociodemographic and socioeconomic factors on sleep complaints depend on an individual’s race/ ethnicity. Sleep. 2010;33:A307. [Google Scholar]
- 153.Friedman EM, Hayney MS, Love GD, et al. Social relationships, sleep quality, and interleukin-6 in aging women. Proc Natl Acad Sci U S A. 2005;102:18757–62. doi: 10.1073/pnas.0509281102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Grandner MA, Petrov MER, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9:897–905. doi: 10.5664/jcsm.2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Sleep symptoms, race/ethnicity, and socioeconomic position. Sleep. 2014;37:601–11. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;169:1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Tomfohr LM, Ancoli-Israel S, Dimsdale JE. Childhood socioeconomic status and race are associated with adult sleep. Behav Sleep Med. 2010;8:219–30. doi: 10.1080/15402002.2010.509236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Lallukka T, Arber S, Rahkonen O, Lahelma E. Complaints of insomnia among midlife employed people: the contribution of childhood and present socioeconomic circumstances. Sleep Med. 2010;11:828–36. doi: 10.1016/j.sleep.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 159.Cheng Y, Du CL, Hwang JJ, Chen IS, Chen MF, Su TC. Working hours, sleep duration and the risk of acute coronary heart disease: a case-control study of middle-aged men in Taiwan. Int J Cardiol. 2014;171:419–22. doi: 10.1016/j.ijcard.2013.12.035. [DOI] [PubMed] [Google Scholar]
- 160.Bannai A, Tamakoshi A. The association between long working hours and health: a systematic review of epidemiological evidence. Scand J Work Environ Health. 2014;40:5–18. doi: 10.5271/sjweh.3388. [DOI] [PubMed] [Google Scholar]
- 161.Barilla HE, Corbitt C, Chakravorty S, Perlis M, Grandner MA. Are those with more physically demanding jobs more likely to exhibit short/long sleep duration? Sleep. 2013;36:A325–6. [Google Scholar]
- 162.Kim HJ, Ruger JP. Socioeconomic disparities in behavioral risk factors and health outcomes by gender in the Republic of Korea. BMC Public Health. 2010;10:195. doi: 10.1186/1471-2458-10-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Simon-Tuval T, Reuveni H, Greenberg-Dotan S, Oksenberg A, Tal A, Tarasiuk A. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009;32:545–52. doi: 10.1093/sleep/32.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Brouillette RT, Horwood L, Constantin E, Brown K, Ross NA. Childhood sleep apnea and neighborhood disadvantage. J Pediatr. 2011;158:789–95. e1. doi: 10.1016/j.jpeds.2010.10.036. [DOI] [PubMed] [Google Scholar]
- 165.Whinnery J, Schopfer E, Jackson NJ, Perlis M, Grandner MA. Short and long sleep duration in the US: associations with race/ethnicity, country of origin, socioeconomic position, and acculturation. Sleep. 2013;36:A336–7. [Google Scholar]
- 166.Grandner MA, Jackson N, Gerstner JR, Knutson KL. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite. 2013;64:71–80. doi: 10.1016/j.appet.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Grandner MA, Jackson N, Gerstner JR, Knutson KL. Sleep symptoms associated with intake of specific dietary nutrients. J Sleep Res. 2014;23:22–34. doi: 10.1111/jsr.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Grandner MA, Patel NP, Perlis ML, et al. Obesity, diabetes, and exercise associated with sleep-related complaints in the American population. J Public Health. 2011;19:463–74. doi: 10.1007/s10389-011-0398-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Chakravorty S, Grandner MA, Kranzler HR, et al. Insomnia in alcohol dependence: predictors of symptoms in a sample of veterans referred from primary care. Am J Addict. 2013;22:266–70. doi: 10.1111/j.1521-0391.2012.12009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Jaehne A, Unbehaun T, Feige B, Lutz UC, Batra A, Riemann D. How smoking affects sleep: a polysomnographical analysis. Sleep Med. 2012;13:1286–92. doi: 10.1016/j.sleep.2012.06.026. [DOI] [PubMed] [Google Scholar]
- 171.Stipelman BA, Augustson E, McNeel T. The relationship among smoking, sleep, and chronic rheumatic conditions commonly associated with pain in the national health interview survey. J Behav Med. 2013;36:539–48. doi: 10.1007/s10865-012-9447-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Okun ML, Levine MD, Houck P, Perkins KA, Marcus MD. Subjective sleep disturbance during a smoking cessation program: associations with relapse. Addict Behav. 2011;36:861–4. doi: 10.1016/j.addbeh.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Chaput JP, McNeil J, Despres JP, Bouchard C, Tremblay A. Short sleep duration is associated with greater alcohol consumption in adults. Appetite. 2012;59:650–5. doi: 10.1016/j.appet.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 174.Colrain IM, Turlington S, Baker FC. Impact of alcoholism on sleep architecture and EEG power spectra in men and women. Sleep. 2009;32:1341–52. doi: 10.1093/sleep/32.10.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Smith A. African americans and technology use: a demographic portrait. Washington, DC: Pew Research Center; 2014. [Google Scholar]
- 176.Lopez MH, Gonzalez-Barrera A, Patten E. Closing the digital divide: latinos and technology adoption. Washington, DC: Pew Hispanic Center; 2013. [Google Scholar]
- 177.Zickuhr K, Smith A. Digital differences: while increased internet adoption and the rise of mobile connectivity have reduced many gaps in technology access over the past decade, for some groups digital disparities still remain. Washington, DC: Pew Research Center; 2012. [Google Scholar]
- 178.Gradisar M, Wolfson AR, Harvey AG, Hale L, Rosenberg R, Czeisler CA. The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 Sleep in America poll. J Clin Sleep Med. 2013;9:1291–9. doi: 10.5664/jcsm.3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Brunborg GS, Mentzoni RA, Molde H, et al. The relationship between media use in the bedroom, sleep habits and symptoms of insomnia. J Sleep Res. 2011;20:569–75. doi: 10.1111/j.1365-2869.2011.00913.x. [DOI] [PubMed] [Google Scholar]
- 180.Munezawa T, Kaneita Y, Osaki Y, et al. The association between use of mobile phones after lights out and sleep disturbances among Japanese adolescents: a nationwide cross-sectional survey. Sleep. 2011;34:1013–20. doi: 10.5665/SLEEP.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]