Abstract
Although recent diagnostic and therapeutic advances have substantially improved the survival of patients with gastric cancer (GC), the overall prognosis is still poor. Surgery is the only curative treatment and should be performed in experienced centers. Due to high relapse following surgery, complementary and systemic treatment aimed at eradicating micrometastasis should be performed in most cases. Cytotoxic treatments are effective in downstaging locally advanced cancer, but different sensitivities and toxicities probably exist in different GC subtypes. Current treatment protocols are based primarily on clinical data and histological features, but molecular biomarkers that would allow for the prediction of treatment responses are urgently needed. Understanding how host factors are responsible for inter-individual variability of drug response or toxicity will also contribute to the development of more effective and less toxic treatments.
Keywords: Gastric cancer, Multidisciplinary treatment, Therapeutic strategies, Curative surgery
Core tip: There has been much progress in the past decades regarding the identification of risk factors for gastric cancer and understanding its pathogenesis. Diagnostic and therapeutic management of this disease has also improved significantly in the past few years. Despite these advances, prognosis remains dismal, and new therapeutic options are urgently needed. Hopefully, in the years to come, treatments will be tailored for a given patient based on tumor characteristics and host factors, with the aim of increasing therapeutic efficacy and decreasing toxicity. Faraway, so close!
INTRODUCTION
Gastric cancer (GC) is a major public health issue, and it is the fourth most common cancer and the second leading cause of cancer-related death[1]. It is usually diagnosed at an advanced stage, and, consequently, the prognosis is dismal. Although surgery is the definitive therapy, rates of recurrence are high, creating the need for neoadjuvant or adjuvant therapy. These therapies have improved significantly the 5 year survival of these patients but not all patients benefit equally from these treatment options. The ability to predict patient response to specific therapies would be particularly valuable and would allow for the stratification of patients for personalized treatment strategies, likely with less toxicity. Recent advances have improved our understanding of gastric carcinogenesis with an unprecedented opportunity of developing novel therapeutic strategies. Exploring and validating tissue-based biomarkers are ongoing processes, which will certainly open new avenues for treating and improving the prognosis of patients with GC.
RISK FACTORS FOR GC
Like other human cancers, GC is the end result of the interplay of environmental and susceptibility factors. The striking geographic variation in GC incidence reflects early role of environmental exposure rather than genetics, as migration studies have confirmed a decline in incidence in subsequent generations. The only environmental factor that is considered to be a type I carcinogen by the World Health Organization is Helicobacter pylori (H. pylori)[2]. This bacterium can have a lifelong uneventful relation with its host but, in a minority of cases, causes peptic ulcer, both intestinal and diffuse type gastric adenocarcinoma and gastric mucosa associated lymphoid tissue (MALT) lymphoma. About 50% of the world’s population is infected with H. pylori, but less than 0.5% of infected individuals will develop GC. This disparity reflects the variation in the pathogenicity of bacterial strains as well as host inflammatory genetic susceptibility factors such as interleukin (IL)-1B, IL-8, IL-10, interferon (IFN)-gamma, and tumor necrosis factor beta (TNF-β) polymorphisms[2]. H. pylori infection causes chronic inflammation, accumulation of reactive oxygen species (ROS), and oxidative damage in the gastric mucosa, thereby promoting the sequential progression of normal gastric epithelium through atrophic gastritis, intestinal metaplasia, and dysplasia to carcinoma. Advanced atrophic corpus-predominant gastritis and subsequent development of intestinal metaplasia provide the histological base for GC genesis[3]. This model of precancerous lesions is currently accepted, and surveillance recommendations apply to patients at increased risk[3]. The intestinal-type GCs are more related to atrophic gastritis, intestinal metaplasia, and dysplasia, but H. pylori infection is also associated with an increased risk of diffuse-type GC.
In addition to H. pylori, dietary and lifestyle factors may also modify the risk of developing GC. Low socioeconomic status and associated conditions have been linked with a two-fold increase in GC risk[4]. Subjects belonging to a low socioeconomic status have a higher prevalence of H. pylori infection, more frequent smoking habit, and less vegetables and fruit intake than the general population[5]. In an analysis of the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST), there was a 45% higher risk of GC associated with ever smoking compared to never smoking[6]. In a meta-analysis with 42 articles, Ladeiras-Lopes et al[7] concluded that smoking is the most important behavioral risk factor for GC. Heavy alcohol intake has been linked to some increased GC risk, mainly in men[8]. Nonetheless, as heavy drinkers usually smoke and have a poor diet, there may be some confounding factors in these conclusions[4]. Among dietary factors, N-nitroso compounds (including nitrosamine) are proven animal carcinogens. Potential sources of N-nitroso compounds are beer, processed (smoked, cured, salted, and pre- served) meats, red meat, and tobacco smoke[8]. In the EPIC cohort, the authors found no association between nitrites and nitrosodimethylamine intake and GC risk, but endogenous production of N-nitroso compounds was significantly associated with non-cardia cancer risk[9].
A meta-analysis in 2012, including 2076498 patients, showed a significant positive association between high salt intake and GC[10]. High salt intake damaged gastric mucosa and increased the susceptibility to carcinogenesis in studies with rodents.
In respect to protective factors, intake of non-starchy vegetables and fruits has been associated with a moderately decreased risk of GC in many cohort-, population- and hospital-based case-control studies[4,5]. In a reanalysis of the EPIC cohort, a negative and significant association was observed between total vegetable, fruit, and flavonoid intake and dietary total antioxidant capacity and risk of GC[11-13]. This protection afforded by vegetables and fruits may derive from their content in antioxidants (such as vitamin C), which may reduce the formation of N-nitroso compounds in the stomach[5].
A recent large European prospective cohort study investigated the combined impact of the above-cited behaviors on GC risk using a healthy lifestyle index[14]. The authors concluded that adopting a combination of lifestyle behaviors, including not smoking, limiting alcohol consumption, following a healthy dietary pattern (represented by the Mediterranean diet), and having a normal body mass index can dramatically decrease the burden of GC. In 2003, in a meta-analysis by Wang et al[15] including 2831 GC patients, regular NSAIDs users had a reduced risk of GC (OR = 0.78, 95%CI: 0.69-0.87). These results have recently been confirmed in a wide systematic review[16]. The pro-apoptotic and anti-angiogenesis effects of NSAIDs are known to inhibit carcinogenesis in patients with colonic polyps, and NSAIDs may act in a similar way in gastric mucosa[4]. To date, no randomized controlled studies exist on the long-term effect of NSAIDs alone on the development of GC, and the alleged protective effect could simply reflect the “protective user effect”, as most individuals eligible for sustained NSAID chemoprophylaxis do not usually suffer from gastric disease.
The decrease of distal GC prevalence that has been consistently described in a number of studies[17] could very well be the result of life style changes associated with improvement of economic status, better hygiene, and consequent decrease of H. pylori infection[4,5].
PATHOGENETIC MECHANISMS OF GASTRIC CARCINOGENESIS
About 95% of gastric tumors are adenocarcinomas, which can be classified into well differentiated (intestinal), undifferentiated (diffuse), and mixed types. Further knowledge about GC heterogeneity has been provided by The Cancer Genome Atlas Research Network. Through the molecular characterization of 295 gastric adenocarcinomas, four GC subtypes have been proposed: microsatellite unstable tumors; genomically stable tumors; tumors displaying chromosomal instability; and Epstein-Barr positive tumors[18]. Hopefully, this subtype analysis will aid in the development of tailored therapeutic strategies for selected patients.
Like other cancers, GC is a complex, multistep, and molecularly heterogeneous disease, involving deregulation of canonical oncogenic pathways, such as p53, Wnt/β-catenin, and nuclear factor (NF)-κB, among others. While most intestinal-type of GCs progress through the multistep cellular dedifferentiation described by Correa[19], most diffuse-type cancers involve the sporadic or syndromic loss of expression of adhesion protein E-cadherin (CDH1). This is a calcium dependent cell-to-cell adhesion glycoprotein that plays a critical role in maintaining the normal epithelium architecture. The cytoplasmic domain of this molecule interacts with β-catenin, forming strong cohesive nets between the actin cytoskeleton, essential for processes of cell-cell adhesion. Inactivation of CDH1 by mutation, deletion, or aberrant methylation leads to enhanced cellular motility resulting in tumor dedifferentiation and invasiveness[20]. Inactivation of CDH1 has been described in over 50% of diffuse GC but also in a small proportion of intestinal-type tumors[20].
Stem cell hypothesis
Most of the molecular events described above have been extensively characterized. Irrespective of the type or order in which these events to promote gastric carcinogenesis, the stem cell hypothesis states that tumors are heterogeneous, and there is a subset of cells capable of self-renewal, asymmetrical division, and differentiation with the ability of generating a new tumor. Takaishi et al[21] identified CD44 as a gastric stem cell marker. The origin of cancer stem cells (CSCs) could be differentiation of epithelial stem cells (epithelial-mesenchymal transition (EMT)) or recruitment of bone marrow derived stem cells (BMDSCs). Houghton et al[22] published a breakthrough paper in Science in 2004, claiming that GC could originate in the bone marrow. Using a model of Helicobacter infected mice, the authors demonstrated that BMDSCs repopulated the gastric epithelium and progressed from metaplasia to dysplasia and later to intra-epithelial cancer. The authors proposed that chronic inflammation induced by H. pylori promoted cytokine release and mesenchymal stem cell recruitment from the bone marrow. These bone marrow stem cells are capable of homing to the stomach epithelium and differentiating into gastric cells through fusion[23].
One of the most important steps in carcinogenesis is the moment when cancer becomes a systemic disease. The EMT is the developmental process whereby epithelial cells acquire the migratory capacities of mesenchymal cells. These mechanisms involve replacement of E-cadherin by N-cadherin, metalloproteinase increase, and transcription of Snail and ZEB[24]. Very recently, Choi et al[25] showed that H. pylori induced EMT by comparing the expression of TGF-B1 and EMT markers (Twist, Snail, Slug, vimentin, and E-cadherin) in controls and patients with gastric dysplasia and early GC (EGC) before and after H. pylori eradication with a follow up of 46 mo. TGF-B1, Twist, Snail, Slug, vimentin, and CD44 were upregulated in patients with dysplasia and EGC while E-cadherin was decreased. After H. pylori eradication, E-cadherin expression was enhanced while the other markers were reduced. These authors proposed that H. pylori triggers both the EMT pathway and the emergence of gastric stem cells.
As appealing and out of the box as the stem cell hypothesis may be, it has not yet produced specific therapeutic targets, and its mechanisms seem too ubiquitous to be targeted.
Although much has been made in the past decades regarding the understanding and identification of genetic and epigenetic events that can drive normal gastric mucosa to cancer, we now need to use proteomic and metabolic approaches to design targeted and effective therapies in patients with GC. Given the role of these molecular events in directing the pathogenesis of GC, studying their signatures and developing them as biomarkers for targeted therapies is likely to impact significantly the outcome of these patients
THERAPEUTIC STRATEGIES IN GC
Perioperative therapies - chemo and chemoradiotherapy
Currently, surgical resection is the only curative therapy for non-metastatic gastric adenocarcinoma. However, since GC may be a systemic disease from the beginning, it follows that patients submitted to surgery alone were prone to locoregional or distant recurrences of their disease.
Due to large scale randomized trials demonstrating that preoperative and perioperative chemotherapy (CT) improves the clinical outcome for patients with GC[26-28], a standard medical treatment of GC has been defined[29]. Patients with potentially resectable tumors are treated with surgery and perioperative CT or postoperative chemoradiotherapy (CRT)[30,31]. In most European countries, combined preoperative and postoperative administration of CT, as in the multinational MAGIC trial[27], is the preferred treatment strategy. In North America, most centers perform postoperative CRT according to the large American Intergroup trial (INT0116). The latter is criticized by some, as inadequate surgical lymphadenectomy may have led to overestimation of the benefit[31]. This is supported by retrospective data from the Dutch D1D2 trial, which demonstrated that CRT reduced local recurrence rates following D1 resection but provided no benefit in patients who have undergone D2 resection[32].
Cytotoxic therapy provides positive response rates ranging from 20%-60%[33], which is a major breakthrough if we remember that two decades ago CT was used solely in the palliative setting because the chemosensitivity of GC was considered very mild.
Although there are a few studies evaluating clinical and pathological predictors of response and prognostic factors in the neoadjuvant setting, none of the potential markers have been validated in prospective studies[34-36].
Neoadjuvant/ perioperative chemotherapy
Neoadjuvant CT is administered as a means of “downstaging” a locally advanced tumor prior to an attempt at curative resection. This approach has been applied to patients thought to have resectable disease as well as those with apparently unresectable but nonmetastatic disease. One proposed advantage is better compliance to CT, usually, in the neoadjuvant setting. Another benefit of neoadjuvant CT is in patients who are at high risk of developing distant metastases (e.g., those with bulky T3/T4 tumors, visible perigastric nodes) who may be spared the morbidity of unnecessary gastrectomy if evidence of distant metastases emerges after CT.
Three large, adequately powered trials have directly compared surgery with or without neoadjuvant or perioperative CT, two of which demonstrated a survival benefit for this approach[26-28]. A meta-analysis of these three trials plus two other trials, which compared preoperative oral fluoropyrimidine vs surgery alone[37,38], and seven other smaller trials, which compared a variety of preoperative CT regimens vs surgery alone, concluded that neoadjuvant CT was associated with a statistically significant benefit in terms of both overall survival (OR = 1.32, 95%CI: 1.07-1.64) and progression free survival (PFS) (OR = 1.85, 95%CI: 1.39-2.46)[30]. Furthermore, neoadjuvant CT was associated with a significantly higher complete (R0) tumor resection rate (OR = 1.38, 95%CI: 1.08-1.78) and did not significantly worsen rates of operative complications, perioperative mortality, or grade 3 or 4 adverse effects (Table 1).
Table 1.
Randomized trials of surgery with and without neoadjuvant or perioperative chemotherapy in resected gastric cancer
| Ref. | n | Chemotherapy | Hazard ratio for survival (95%CI) |
| Cunningham et al[27], 2006 | 503 | ECF | 0.75 (0.60-0.93) |
| Ychou et al[49], 2011 | 224 | PF | 0.69 (0.50-0.95) |
| Schuhmacher et al[28], 2010 | 144 | PF | No significant survival difference |
ECF: Epirubicin/cisplatin/5-fluorouracil; PF: Cisplatin/5-fluorouracil.
In terms of patient selection for this approach, it is reasonable to utilize the eligibility criteria for the MAGIC trial: patients of any age with a performance status of 0 or 1, with a histologically proven adenocarcinoma of the stomach that was considered to invade the muscular propria (T2) and/or with positive lymph nodes N+, and with no evidence of distant metastases or locally advanced inoperable disease, as evaluated by computed tomography, ultrasonography, and laparoscopy[27].
Neoadjuvant chemotherapy vs neoadjuvant chemoradiotherapy
Preoperative combined CRT and radiation therapy (RT) is more commonly used for esophageal, esophagogastric junction (EGJ), and gastric cardia cancers than for potentially resectable non-cardia gastric adenocarcinomas. Neoadjuvant CRT was compared with induction CT alone in the multicenter German POET[39]. Although there were potentially clinically meaningful survival differences that favored CRT, they were not statistically significant. Furthermore, whether the results can be extrapolated to patients with true non-cardia GC is uncertain. The ongoing TOPGEAR trial addresses the question whether neoadjuvant CRT is superior to CT in a phase II/III setting[40].
Adjuvant chemoradiotherapy vs adjuvant chemotherapy
Adjuvant CT has been directly compared with adjuvant CRT in several trials[41-46], only one of which has shown a significant overall survival benefit for the addition of RT to CT[41]. The largest trial, the ARTIST trial, compared CT alone with the addition of RT to cisplatin plus capecitabine (XP). CRT did not significantly reduce recurrence rates, although in a post-hoc subgroup analysis, patients with nodal metastases had superior disease-free survival with combined therapy compared with CT alone[41]. In the latest update, at a median follow-up of 84 mo, 3 year disease-free survival (the primary endpoint) was not significantly better in patients who received combined modality therapy[42]. The hypothesis that adjuvant CRT may represent a better approach than adjuvant CT for patients with node-positive disease will be tested in a successor trial, the ARTIST-II trial.
The only trial to show a significant survival benefit for the addition of RT, randomly assigned 68 patients undergoing complete resection with a D1 or D2 lymph node dissection. The 3 year disease-free survival rate was significantly higher in the CT group (56% vs 29%), as was overall survival (68% vs 44%)[45].
Although studies are still ongoing, the available data does favor the addition of adjuvant radiotherapy in the treatment of GC (Table 2).
Table 2.
Randomized trials of adjuvant chemo or chemoradiotherapy in resected gastric cancer
| Ref. | n | Regimen | 3 yr Disease free survival rate (%; P value) |
| Lee et al[41], 2012 | 458 | XP vs XP/XRT/XP | No significant Disease free survival difference |
| Yu et al[45], 2012 | 68 | 5FU/LV vs 5FU /LV/RT | 44.1 vs 67.7 (P < 0.05) |
| Kim et al[44], 2012 | 90 | 5FU/LV vs 5FU/LV/RT | No significant Disease free survival difference |
| Kwon et al[46], 2010 | 61 | 5FU/LV vs 5FU/LV/RT | No significant Disease free survival difference |
| Bamias et al[43], 2010 | 147 | DP vs DP/RT | No significant Disease free survival difference |
X: Capecitabine; 5-FU: 5-fluorouracil; LV: Leucovorin; P: Cisplatin; D: docetaxel; RT: Radiotherapy (45 Gy).
When adjuvant therapy is used, the optimal regimen has not been established. Acceptable alternatives include epirubicin, cisplatin, and infusional 5-fluorouracil (ECF), as was used in the perioperative MAGIC trial[27]. Results with adjuvant capecitabine plus oxaliplatin (CAPOX, XELOX), as was used in the CLASSIC trial[47]; or XP, as was used in the ARTIST trial[41], are not as advanced as those of perioperative ECF (as was used in the MAGIC trial) or S-1[48].
The optimal time between surgery and postoperative treatment varies widely. In the MAGIC trial[27], it was initiated 6 to 12 wk after surgery, in the Intergroup trial (INT0116)[31], it was between 4 to 7 wk, and in ACTS-GC[48] patients, it started within 6 wk after surgery.
Regarding compliance to treatment, MAGIC[27] and FCCNLC[49] trials reported that postoperative treatment was concluded in only 42% to 50% of the patients, demonstrating the importance of preoperative CT and questioning the use of postoperative treatment in the perioperative setting.
In conclusion, the optimal way to integrate combined modality therapy has not been definitively established. Decisions are often made based on institutional and/or patient preference. As science moves increasingly toward molecular targeted therapy, biologic agents hold great promise in the treatment of this disease as well.
CURATIVE SURGERY IN GC
Optimal type of gastrectomy and the length of proximal resection margin
It is of paramount importance to discuss surgical treatment of GC, given its central role in the overall management of the disease.
Total gastrectomy (TG) is the recommended therapy for more proximal tumors in order to guarantee an appropriate proximal resection margin (PRM). For distally located tumors, subtotal gastrectomy (SG) was recommended with a PRM of more than 2-3 cm for early GC and 5-6 cm for advanced GC. In patients with poorly differentiated diffuse cancer, infiltration of the proximal resection margin by microscopic tumor deposits was a major concern, and TG was classically recommended. However, a randomized controlled trial (RCT)[50,51] assessed the incidence of microscopic resection margin involvement in patients with diffuse type GC and found no statistically significant difference between total and SG and no effect on survival. Furthermore, the authors claim that SG is associated with better nutritional status and quality of life as compared to TG. There is no total agreement regarding what should be considered an appropriate PRM in SG. As shown on Table 3, distances recommended by the German Society differ from those proposed by the Japanese Gastric Cancer Association (JGCA).
Table 3.
Criteria for adequate surgical margins
| German S3 | JGCA | |
| Resection margins | Oral, aboral circumferential | Proximal |
| Proximal resection margins | 5 cm (intestinal type) | -cT1: 2 cm |
| 8 cm (difuse type) | -cT2-T4: | |
| 3 cm (expansive) | ||
| 5 cm (infiltrative) |
Nonetheless, if one considers SG in patients with distally located diffuse-type GC, a wider excision with intraoperative frozen section (IFS) of the resection margin is recommended[52] because they are more likely to have a positive margin. On multivariate analysis, higher T stage, higher N stage, larger tumor size, and diffuse histologic type were significant independent predictive factors for a positive margin[52-54]. Studies have shown that if PRM is confirmed to be negative for malignancy but shorter than the recommended length, further resection for a larger PRM is unnecessary, since the length of PRM has no prognostic impact as long as resection margin is free of tumor[55].
When PRM is positive, the benefits of reoperation always have to be balanced against the risks of this technically demanding procedure. Redo surgery appears to have the most obvious survival advantage in early stage patients, especially when few nodes are involved (N0 or N1)[56,57]. In contrast, advanced N stage patients with positive margins may not benefit from an extended re-excision. Multidisciplinary options, including CT and radiotherapy, are probably more appropriate treatments for positive-margin patients, especially in patients with bulky node disease[56,58]. This is further supported by a retrospective comparison of the Dutch D1D2 trial, where the authors observed significant improvement in survival and local recurrence rates with the use of CRT after a microscopically incomplete R1 resection[56,58].
Lymphadenectomy in resectable GC
The extent of lymphadenectomy in the treatment of GC has been debated for more than two decades. The majority of Japanese and Korean (i.e., Eastern) surgeons would agree that an extended lymphadenectomy (D2) leads to improved outcomes and survival. Several large retrospective studies from those groups have illustrated an impressive overall survival that was unfortunately not reproduced in most Western series.
Early published studies in the West did not show any advantage in long-term survival of D2 lymphadenectomy as compared to D1 dissection, mainly due to an elevated morbidity and mortality associated with D2 procedure[59-62].
As shown in Table 4, only a Taiwanese study[63,64] found a significant survival advantage of D2 with respect to D1, while the British[60,65], Dutch[59,66] and Italian[67,68] trials did not find a significant difference in long-term survival comparing the two procedures. The Japanese trial[69] did not find any survival advantage of prophylactic para-aortic nodal dissection (PAND).
Table 4.
Selected randomized controlled trials studying the extent of the lymph node dissection for patients with gastric cancer
| Ref. | Year published | Region | Extent of Lymph node dissection | Patients (n) | Morbidity | Mortality | 5 yr overall survival (%) |
| Dent et al[62] | 1988 | South Africa | D1 | 22 | 22% | 0% | N/A |
| D2 | 21 | 43% | 0% | N/A | |||
| BonenKamp et al[59,66] | 1995 | The Netherlands | D1 | 380 | 25% | 4% | 45 |
| D2 | 331 | 43% | 10% | 47 | |||
| Cuschieri et al[60,65] | 1996 | Europe | D1 | 200 | 28% | 6.5% | 35 |
| D2 | 200 | 46% | 13% | 33 | |||
| Wu et al[63,64] | 2004 | Taiwan | D1 | 110 | 7.3% | 0% | 53.6 |
| D3 | 111 | 17.1% | 0% | 59.5 | |||
| Sasako et al[69] | 2008 | Japan | D2 | 263 | 20.9% | 0.8% | 69.2 |
| D2 + PAND | 260 | 28.1% | 0.8% | 70.3 | |||
| Degiuli et al[67,68] | 2010 | Italy | D1 | 133 | 12% | 3% | 66.5 |
| D2 | 134 | 17.9% | 2.2% | 64.2 |
PAND: Para-aortic node dissection.
In contrast Roviello et al[70] showed that D2 dissection was performed with acceptable mortality and morbidity (2% and 17%, respectively) and Siewert et al[71] found improved survival for stage II patients that underwent D2 lymphadenectomy with no increased morbidity.
More recently, the Dutch GC Group Trial[32] showed that, compared with D1, D2 lymphadenectomy was associated with lower local recurrence and lower cancer-related death rates, despite a significantly higher postoperative mortality, morbidity, and reoperation rates. The Italian GC Study Group[67] randomized 267 patients and compared the short-term results of D1 and D2 lymphadenectomy for curable GC. Pancreaticosplenectomy was not considered as a routine part of the D2 gastrectomy. This study did not show significant differences in operative mortality, morbidity, and duration of postoperative hospital stay. The authors concluded that modified D2 lymphadenectomy, a spleen-preserving D2 resection technique currently available in high-volume centers, is a safe option to treat GC of Western patients.
In order to achieve better surgical outcomes, Northern European countries carried out a centralization and standardization of surgical procedures in GC. In Denmark, this process improved short term results, where 30 d hospital mortality decreased from 8.2% to 2.4%, and the proportion of patients with at least 15 lymph nodes removed was increased from 19% to 76%[72]. Centralization of GC surgery and/or audits for GC are currently implemented in the United Kingdom, Sweden, Finland, and the Netherlands[73,74].
In conclusion, the current consensus is that for medically fit patients D2 lymphadenectomy should be the standard procedure. It should be carried out in specialized, high-volume centers with appropriate surgical expertise and postoperative care[75,76]. The German, British, and ESMO-ESSO-ESTRO guidelines adopted this as the standard of care for surgical treatment with curative intent[77].
Is there a place for laparoscopic gastrectomy?
Laparoscopic gastrectomy in GC is gaining popularity worldwide as a minimally invasive alternative treatment to traditional open surgery.
Laparoscopic surgery has the potential benefits of a decreased operative morbidity and reduced recovery times but with longer operative time.
Most meta-analyses support these benefits in distal gastrectomy, however, the oncological and long-term outcomes still need to be validated[75,76]. Postoperative morbidity is greater, particularly in total gastrectomy. According to the JGCA guidelines, D2 dissection of stations 12a or 10 can be technically demanding due to the risks of organ injury, bleeding, and/or bile and pancreatic leakage. There is also no consensus on the technique of anastomosis following a laparoscopic total gastrectomy. The introduction of a circular stapler with transorally inserted anvil has enabled esophago-jejunostomy anastomosis. This procedure resembles the conventional approach by laparotomy[78].
The most common technique is laparoscopic assisted distal gastrectomy (LADG) without hand assistance, which is also the most frequently reported procedure in the current literature[79-81]. Trials are currently ongoing in Japan (JCOG-0912), South Korea (KLASS and KLASS-02), and China to compare open and laparoscopic surgery in EGC[81,82]. These should provide further insight into the role of laparoscopic approach before moving to the laparoscopic treatment of locally advanced GC, especially when a TG with D2 lymphadenectomy is recommended. As such, and at the time of writing this paper, one cannot advise laparoscopic gastrectomy for treating GC, outside a clinical trial.
TREATING GC IN THE 21st CENTURY: ARE WE READY FOR PERSONALIZED THERAPY?
This is certainly an active topic of clinical and basic research not only because GC is a highly prevalent disease, but also because the treatments used may be effective but sometimes very toxic[83]. Although the prognosis and 5 year survival is still poor for patients with locally advanced GC, considerable progress has been achieved in the past two decades[84]. Besides staging procedures, which allow for a more accurate staging of the disease and enable a more appropriate selection of patients for pre-operative cytoreductive CT, both surgical and medical therapies have evolved substantially. From a surgical point of view, a modified D2 lymphadenectomy is now the standard procedure for medically fit patients with locally advanced GC in most European Centers. Short and long term results improved substantially in Western studies, as long as surgery was carried out in specialized, high-volume centers with appropriate surgical expertise and postoperative care. This was certainly a major step towards curative therapy in GC patients in the Western world.
Peri-operative CT using ECF, as in the MAGIC trial, is now the standard of care for stages II and III disease as recommended by ESMO-ESSO-ESTRO clinical practice guidelines[77]. This was also a major breakthrough, as up to one decade ago, CT was not systematically considered part of the curative treatment of GC.
Host factors responsible for heterogeneity of response
Although, peri-operative CT followed by radical surgery is now the standard of care for most patients with stage II-III non-metastatic GC, less than 50% of patients complete the full protocol due to its toxicity[27]. In this respect, there has been recent interest in exploring the relationship between body composition, especially proportions of lean and fat tissues, with treatment toxicities. The most recent definition of cancer cachexia specifically involves depletion of muscle mass, which sometimes may not impact body weight. As shown in Figure 1, patients may become sarcopenic despite a normal or even high body mass index. Muscle depletion is characterized both by a reduction in muscle size and increased proportion of inter- and intramuscular fat. Fat infiltration given by muscle attenuation (MA) is a further manifestation of the wasting process (Figure 1).
Figure 1.
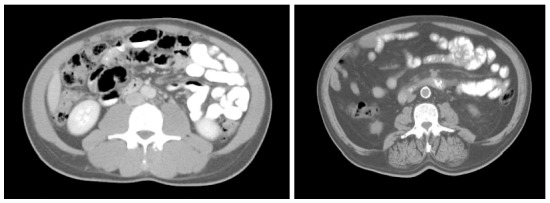
Axial computed tomography images of the third lumbar vertebra region from two patients with similar body mass index but different muscle and fat tissue cross sectional areas. Paraspinal muscles are clearly different between the two subjects as is mesenteric fat and fat infiltrating muscle - muscle radiation attenuation. Low relative muscularity and expanded visceral fat are associated with increased toxicity and decreased survival.
Prado et al[85] observed in metastatic breast cancer patients receiving capecitabine treatment that sarcopenia was a significant predictor of toxicity and time to tumor progression. The authors reported a 28-fold increase in the relative risk of grade 3 and 4 neutropenia if a patient’s lean body mass (LBM) was < 89% of age and sex-adjusted norms. They hypothesized that this relationship was primarily due to a pharmacokinetic effect, as fat-free mass (LBM plus bone tissue) and total body water were better predictors of 5-FU pharmacokinetics (clearance and volume of distribution) than body surface or body weight. This has also been reproduced in patients with metastatic lung and pancreatic cancer[86]. Sarcopenia has also been associated with unfavorable clinical outcomes, such as increased length of hospital stay, increased incidence of infections for hospitalized patients, and mortality in surgical patients[87]. Lieffers et al[87] observed in patients aged more than 65 years operated for colorectal cancer, sarcopenia was an independent predictor of both infection and rehabilitation care and, consequently, a longer length of hospital stay. Finally, it is important to stress that imaging of sarcopenia can be done using the CT scan performed at the time of routine imaging studies for tumor evaluation and/or restaging[88], as long as the appropriate software is available, as shown in Figure 2.
Figure 2.
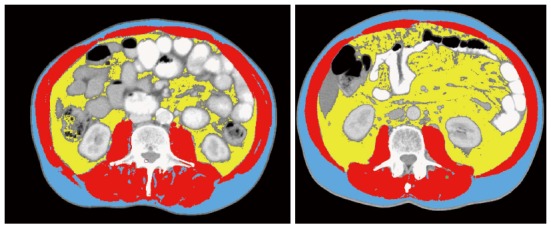
Lumbar computed tomography was analyzed for muscle and fat tissue cross sectional areas using an appropriate software developed by Martin et al[88]. Muscle mass is shown in red and were quantified within a Hounsfield unit (HU) range of -29-150, visceral fat shown in yellow, range from -150 to -50, and subcutaneous fat shown in blue, range from -190 to 30. Muscle radiation attenuation was calculated for muscle area. Although these two images might refer to two individuals with the same body mass index (23 kg/m2) and age (73 yr), the amount of muscle mass and visceral fat, which amplifies inflammatory response, are very distinct.
It would then be interesting to test whether these observations of body composition, muscle mass measurement, and CT toxicity also hold true in respect to patients with advanced GC selected to perioperative CT followed by radical surgery. This could shed some light on the issue why patients do not benefit equally from these treatment options.
Analysis of tumor factors that might allow for more personalized therapy
Inter-individual variability of drug response or resistance may also be related to tumor heterogeneity. The identification of predictive tumor markers at the time of diagnosis would allow for stratifying patients to more effective treatments, as current therapeutic strategies do not uniformly benefit all patients. Although very toxic in some patients, one cannot forget that complete pathologic responses are being reported with increasing frequency[89], thus making the identification of these predictive factors mandatory.
In a recent study, the authors found that pathologic complete response was observed in 20% (10/50) of patients and a further 20% (10/50) achieved near complete histological remission (< 10% residual tumor). Among these very good responders, 85% (17/20) had intestinal type tumors, 10% (2/20) had diffuse tumors, and 5% (1/20) had mixed type tumors[89].
In regard to molecular markers, and similarly to what occurs in colorectal cancer[90], MSI status seems to affect both the prognosis and the response to 5-FU based chemotherapies. One study found 5-FU based adjuvant CT prolonged disease-free survival in patients with GC stage II and III disease only in patients with tumors MSS or MSI-low, in contrast with the MSI-high group who did not seem to benefit from this type of therapy[91]. However, these are conflicting data, as another study did not find that MSI status significantly affected response to 5-FU CT[92].
Current research is thus focusing on identifying cancer biomarkers, which will elucidate treatment response and drug resistance mechanisms[93]. Real progress will only be achieved through the development of new treatment options that have reduced cell toxicity compared with that of standard therapeutic regimens. Currently, except for the status of human epidermal growth factor-2, which is used to guide trastuzumab therapy, no other biomarkers are used in clinical practice.
CONCLUSION
Considering the amount of effort that has been put in clarifying the pathogenesis of GC, we are now hoping that these new discoveries will lead to the translation of these insights into the clinical arena. New proteomic technologies that promote large-scale sample screening will hopefully open new avenues for targeted and personalized therapies in patients with GC[94]. As much as unraveling gastric carcinogenesis seems closer and closer, concepts such as the migrating cancer stem cell remind us that this enigma is still faraway from being solved. Faraway, so close!
Footnotes
Conflict-of-interest statement: No conflict of interest to declare.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: June 3, 2015
First decision: June 23, 2015
Article in press: September 15, 2015
P- Reviewer: Paydas S, Verlato G S- Editor: Ma YJ L- Editor: Filipodia E- Editor: Wang CH
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.González CA, Sala N, Rokkas T. Gastric cancer: epidemiologic aspects. Helicobacter. 2013;18 Suppl 1:34–38. doi: 10.1111/hel.12082. [DOI] [PubMed] [Google Scholar]
- 3.Dinis-Ribeiro M, Areia M, de Vries AC, Marcos-Pinto R, Monteiro-Soares M, O’Connor A, Pereira C, Pimentel-Nunes P, Correia R, Ensari A, et al. Management of precancerous conditions and lesions in the stomach (MAPS): guideline from the European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter Study Group (EHSG), European Society of Pathology (ESP), and the Sociedade Portuguesa de Endoscopia Digestiva (SPED) Endoscopy. 2012;44:74–94. doi: 10.1055/s-0031-1291491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Massarrat S, Stolte M. Development of gastric cancer and its prevention. Arch Iran Med. 2014;17:514–520. [PubMed] [Google Scholar]
- 5.Denova-Gutiérrez E, Hernández-Ramírez RU, López-Carrillo L. Dietary patterns and gastric cancer risk in Mexico. Nutr Cancer. 2014;66:369–376. doi: 10.1080/01635581.2014.884237. [DOI] [PubMed] [Google Scholar]
- 6.González CA, Pera G, Agudo A, Palli D, Krogh V, Vineis P, Tumino R, Panico S, Berglund G, Simán H, et al. Smoking and the risk of gastric cancer in the European Prospective Investigation Into Cancer and Nutrition (EPIC) Int J Cancer. 2003;107:629–634. doi: 10.1002/ijc.11426. [DOI] [PubMed] [Google Scholar]
- 7.Ladeiras-Lopes R, Pereira AK, Nogueira A, Pinheiro-Torres T, Pinto I, Santos-Pereira R, Lunet N. Smoking and gastric cancer: systematic review and meta-analysis of cohort studies. Cancer Causes Control. 2008;19:689–701. doi: 10.1007/s10552-008-9132-y. [DOI] [PubMed] [Google Scholar]
- 8.Duell EJ, Travier N, Lujan-Barroso L, Clavel-Chapelon F, Boutron-Ruault MC, Morois S, Palli D, Krogh V, Panico S, Tumino R, et al. Alcohol consumption and gastric cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Am J Clin Nutr. 2011;94:1266–1275. doi: 10.3945/ajcn.111.012351. [DOI] [PubMed] [Google Scholar]
- 9.Jakszyn P, Bingham S, Pera G, Agudo A, Luben R, Welch A, Boeing H, Del Giudice G, Palli D, Saieva C, et al. Endogenous versus exogenous exposure to N-nitroso compounds and gastric cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST) study. Carcinogenesis. 2006;27:1497–1501. doi: 10.1093/carcin/bgl019. [DOI] [PubMed] [Google Scholar]
- 10.Ge S, Feng X, Shen L, Wei Z, Zhu Q, Sun J. Association between Habitual Dietary Salt Intake and Risk of Gastric Cancer: A Systematic Review of Observational Studies. Gastroenterol Res Pract. 2012;2012:808120. doi: 10.1155/2012/808120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zamora-Ros R, Agudo A, Luján-Barroso L, Romieu I, Ferrari P, Knaze V, Bueno-de-Mesquita HB, Leenders M, Travis RC, Navarro C, et al. Dietary flavonoid and lignan intake and gastric adenocarcinoma risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Am J Clin Nutr. 2012;96:1398–1408. doi: 10.3945/ajcn.112.037358. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez CA, Lujan-Barroso L, Bueno-de-Mesquita HB, Jenab M, Duell EJ, Agudo A, Tjønneland A, Boutron-Ruault MC, Clavel-Chapelon F, Touillaud M, et al. Fruit and vegetable intake and the risk of gastric adenocarcinoma: a reanalysis of the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST) study after a longer follow-up. Int J Cancer. 2012;131:2910–2919. doi: 10.1002/ijc.27565. [DOI] [PubMed] [Google Scholar]
- 13.Serafini M, Jakszyn P, Luján-Barroso L, Agudo A, Bas Bueno-de-Mesquita H, van Duijnhoven FJ, Jenab M, Navarro C, Palli D, Boeing H, et al. Dietary total antioxidant capacity and gastric cancer risk in the European prospective investigation into cancer and nutrition study. Int J Cancer. 2012;131:E544–E554. doi: 10.1002/ijc.27347. [DOI] [PubMed] [Google Scholar]
- 14.Buckland G, Travier N, Huerta JM, Bueno-de-Mesquita HB, Siersema PD, Skeie G, Weiderpass E, Engeset D, Ericson U, Ohlsson B, et al. Healthy lifestyle index and risk of gastric adenocarcinoma in the EPIC cohort study. Int J Cancer. 2015;137:598–606. doi: 10.1002/ijc.29411. [DOI] [PubMed] [Google Scholar]
- 15.Wang WH, Huang JQ, Zheng GF, Lam SK, Karlberg J, Wong BC. Non-steroidal anti-inflammatory drug use and the risk of gastric cancer: a systematic review and meta-analysis. J Natl Cancer Inst. 2003;95:1784–1791. doi: 10.1093/jnci/djg106. [DOI] [PubMed] [Google Scholar]
- 16.Algra AM, Rothwell PM. Effects of regular aspirin on long-term cancer incidence and metastasis: a systematic comparison of evidence from observational studies versus randomised trials. Lancet Oncol. 2012;13:518–527. doi: 10.1016/S1470-2045(12)70112-2. [DOI] [PubMed] [Google Scholar]
- 17.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 18.Cancer Genome Atlas Research N. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Correa P. A human model of gastric carcinogenesis. Cancer Res. 1988;48:3554–3560. [PubMed] [Google Scholar]
- 20.Graziano F, Humar B, Guilford P. The role of the E-cadherin gene (CDH1) in diffuse gastric cancer susceptibility: from the laboratory to clinical practice. Ann Oncol. 2003;14:1705–1713. doi: 10.1093/annonc/mdg486. [DOI] [PubMed] [Google Scholar]
- 21.Takaishi S, Okumura T, Tu S, Wang SS, Shibata W, Vigneshwaran R, Gordon SA, Shimada Y, Wang TC. Identification of gastric cancer stem cells using the cell surface marker CD44. Stem Cells. 2009;27:1006–1020. doi: 10.1002/stem.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Houghton J, Stoicov C, Nomura S, Rogers AB, Carlson J, Li H, Cai X, Fox JG, Goldenring JR, Wang TC. Gastric cancer originating from bone marrow-derived cells. Science. 2004;306:1568–1571. doi: 10.1126/science.1099513. [DOI] [PubMed] [Google Scholar]
- 23.Ferrand J, Noël D, Lehours P, Prochazkova-Carlotti M, Chambonnier L, Ménard A, Mégraud F, Varon C. Human bone marrow-derived stem cells acquire epithelial characteristics through fusion with gastrointestinal epithelial cells. PLoS One. 2011;6:e19569. doi: 10.1371/journal.pone.0019569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;119:1420–1428. doi: 10.1172/JCI39104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choi YJ, Kim N, Chang H, Lee HS, Park SM, Park JH, Shin CM, Kim JM, Kim JS, Lee DH, et al. Helicobacter pylori-induced epithelial-mesenchymal transition, a potential role of gastric cancer initiation and an emergence of stem cells. Carcinogenesis. 2015;36:553–563. doi: 10.1093/carcin/bgv022. [DOI] [PubMed] [Google Scholar]
- 26.Boige V PJ, Saint-Aubert B, Lasser P, Conroy T, Bouché O, Segol P, Bedenne L, Rougier P, Ychouet M. Final results of a randomized trial comparing preoperative 5-fluorouracil (F)/cisplatin (P) to surgery alone in adenocarcinoma of stomach and lower esophagus (ASLE): FNLCC ACCORD07-FFCD 9703 trial (abstract) J Clin Oncol. 2007;25:4510. [Google Scholar]
- 27.Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, Scarffe JH, Lofts FJ, Falk SJ, Iveson TJ, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20. doi: 10.1056/NEJMoa055531. [DOI] [PubMed] [Google Scholar]
- 28.Schuhmacher C, Gretschel S, Lordick F, Reichardt P, Hohenberger W, Eisenberger CF, Haag C, Mauer ME, Hasan B, Welch J, et al. Neoadjuvant chemotherapy compared with surgery alone for locally advanced cancer of the stomach and cardia: European Organisation for Research and Treatment of Cancer randomized trial 40954. J Clin Oncol. 2010;28:5210–5218. doi: 10.1200/JCO.2009.26.6114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lordick F, Lorenzen S, Yamada Y, Ilson D. Optimal chemotherapy for advanced gastric cancer: is there a global consensus? Gastric Cancer. 2014;17:213–225. doi: 10.1007/s10120-013-0297-z. [DOI] [PubMed] [Google Scholar]
- 30.Xiong BH, Cheng Y, Ma L, Zhang CQ. An updated meta-analysis of randomized controlled trial assessing the effect of neoadjuvant chemotherapy in advanced gastric cancer. Cancer Invest. 2014;32:272–284. doi: 10.3109/07357907.2014.911877. [DOI] [PubMed] [Google Scholar]
- 31.Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC, Stemmermann GN, Haller DG, Ajani JA, Gunderson LL, Jessup JM, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345:725–730. doi: 10.1056/NEJMoa010187. [DOI] [PubMed] [Google Scholar]
- 32.Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ. Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol. 2010;11:439–449. doi: 10.1016/S1470-2045(10)70070-X. [DOI] [PubMed] [Google Scholar]
- 33.Jiang Y, Ajani JA. Multidisciplinary management of gastric cancer. Curr Opin Gastroenterol. 2010;26:640–646. doi: 10.1097/MOG.0b013e32833efd9b. [DOI] [PubMed] [Google Scholar]
- 34.Persiani R, D’Ugo D, Rausei S, Sermoneta D, Barone C, Pozzo C, Ricci R, La Torre G, Picciocchi A. Prognostic indicators in locally advanced gastric cancer (LAGC) treated with preoperative chemotherapy and D2-gastrectomy. J Surg Oncol. 2005;89:227–36; discussion 237-8. doi: 10.1002/jso.20207. [DOI] [PubMed] [Google Scholar]
- 35.Rohatgi PR, Mansfield PF, Crane CH, Wu TT, Sunder PK, Ross WA, Morris JS, Pisters PW, Feig BW, Gunderson LL, et al. Surgical pathology stage by American Joint Commission on Cancer criteria predicts patient survival after preoperative chemoradiation for localized gastric carcinoma. Cancer. 2006;107:1475–1482. doi: 10.1002/cncr.22180. [DOI] [PubMed] [Google Scholar]
- 36.Nagashima F, Boku N, Ohtsu A, Yoshida S, Hasebe T, Ochiai A, Sakata Y, Saito H, Miyata Y, Hyodo I, et al. Biological markers as a predictor for response and prognosis of unresectable gastric cancer patients treated with irinotecan and cisplatin. Jpn J Clin Oncol. 2005;35:714–719. doi: 10.1093/jjco/hyi194. [DOI] [PubMed] [Google Scholar]
- 37.Kobayashi T, Kimura T. [Long-term outcome of preoperative chemotherapy with 5’-deoxy-5-fluorouridine (5’-DFUR) for gastric cancer] Gan To Kagaku Ryoho. 2000;27:1521–1526. [PubMed] [Google Scholar]
- 38.Nio Y, Koike M, Omori H, Hashimoto K, Itakura M, Yano S, Higami T, Maruyama R. A randomized consent design trial of neoadjuvant chemotherapy with tegafur plus uracil (UFT) for gastric cancer--a single institute study. Anticancer Res. 2004;24:1879–1887. [PubMed] [Google Scholar]
- 39.Stahl M, Walz MK, Stuschke M, Lehmann N, Meyer HJ, Riera-Knorrenschild J, Langer P, Engenhart-Cabillic R, Bitzer M, Königsrainer A, et al. Phase III comparison of preoperative chemotherapy compared with chemoradiotherapy in patients with locally advanced adenocarcinoma of the esophagogastric junction. J Clin Oncol. 2009;27:851–856. doi: 10.1200/JCO.2008.17.0506. [DOI] [PubMed] [Google Scholar]
- 40.Leong T, Smithers M, Michael M, Gebski V, Boussioutas A, Miller D, Zalcberg JR, Wong R, Haustermans K. TOPGEAR: an international randomized phase III trial of preoperative chemoradiotherapy versus preoperative chemotherapy for resectable gastric cancer (AGITG/TROG/EORTC/NCIC CTG) J Clin Oncol. 2012;30:(suppl; abstr TPS4141). [Google Scholar]
- 41.Lee J, Lim do H, Kim S, Park SH, Park JO, Park YS, Lim HY, Choi MG, Sohn TS, Noh JH, et al. Phase III trial comparing capecitabine plus cisplatin versus capecitabine plus cisplatin with concurrent capecitabine radiotherapy in completely resected gastric cancer with D2 lymph node dissection: the ARTIST trial. J Clin Oncol. 2012;30:268–273. doi: 10.1200/JCO.2011.39.1953. [DOI] [PubMed] [Google Scholar]
- 42.Park SH, Sohn TS, Lee J, Lim do H, Hong ME, Kim KM, Sohn I, Jung SH, Choi MG, Lee JH, et al. Phase III Trial to Compare Adjuvant Chemotherapy With Capecitabine and Cisplatin Versus Concurrent Chemoradiotherapy in Gastric Cancer: Final Report of the Adjuvant Chemoradiotherapy in Stomach Tumors Trial, Including Survival and Subset Analyses. J Clin Oncol. 2015;33:3130–3136. doi: 10.1200/JCO.2014.58.3930. [DOI] [PubMed] [Google Scholar]
- 43.Bamias A, Karina M, Papakostas P, Kostopoulos I, Bobos M, Vourli G, Samantas E, Christodoulou Ch, Pentheroudakis G, Pectasides D, et al. A randomized phase III study of adjuvant platinum/docetaxel chemotherapy with or without radiation therapy in patients with gastric cancer. Cancer Chemother Pharmacol. 2010;65:1009–1021. doi: 10.1007/s00280-010-1256-6. [DOI] [PubMed] [Google Scholar]
- 44.Kim TH, Park SR, Ryu KW, Kim YW, Bae JM, Lee JH, Choi IJ, Kim YJ, Kim DY. Phase 3 trial of postoperative chemotherapy alone versus chemoradiation therapy in stage III-IV gastric cancer treated with R0 gastrectomy and D2 lymph node dissection. Int J Radiat Oncol Biol Phys. 2012;84:e585–e592. doi: 10.1016/j.ijrobp.2012.07.2378. [DOI] [PubMed] [Google Scholar]
- 45.Yu C, Yu R, Zhu W, Song Y, Li T. Intensity-modulated radiotherapy combined with chemotherapy for the treatment of gastric cancer patients after standard D1/D2 surgery. J Cancer Res Clin Oncol. 2012;138:255–259. doi: 10.1007/s00432-011-1085-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kwon HC, Kim MC, Kim KH, Jang JS, Oh SY, Kim SH, Kwon KA, Lee S, Lee HS, Kim HJ. Adjuvant chemoradiation versus chemotherapy in completely resected advanced gastric cancer with D2 nodal dissection. Asia Pac J Clin Oncol. 2010;6:278–285. doi: 10.1111/j.1743-7563.2010.01331.x. [DOI] [PubMed] [Google Scholar]
- 47.Bang YJ, Kim YW, Yang HK, Chung HC, Park YK, Lee KH, Lee KW, Kim YH, Noh SI, Cho JY, et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012;379:315–321. doi: 10.1016/S0140-6736(11)61873-4. [DOI] [PubMed] [Google Scholar]
- 48.Sasako M, Sakuramoto S, Katai H, Kinoshita T, Furukawa H, Yamaguchi T, Nashimoto A, Fujii M, Nakajima T, Ohashi Y. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol. 2011;29:4387–4393. doi: 10.1200/JCO.2011.36.5908. [DOI] [PubMed] [Google Scholar]
- 49.Ychou M, Boige V, Pignon JP, Conroy T, Bouché O, Lebreton G, Ducourtieux M, Bedenne L, Fabre JM, Saint-Aubert B, et al. Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol. 2011;29:1715–1721. doi: 10.1200/JCO.2010.33.0597. [DOI] [PubMed] [Google Scholar]
- 50.Bozzetti F, Marubini E, Bonfanti G, Miceli R, Piano C, Crose N, Gennari L. Total versus subtotal gastrectomy: surgical morbidity and mortality rates in a multicenter Italian randomized trial. The Italian Gastrointestinal Tumor Study Group. Ann Surg. 1997;226:613–620. doi: 10.1097/00000658-199711000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bozzetti F, Marubini E, Bonfanti G, Miceli R, Piano C, Gennari L. Subtotal versus total gastrectomy for gastric cancer: five-year survival rates in a multicenter randomized Italian trial. Italian Gastrointestinal Tumor Study Group. Ann Surg. 1999;230:170–178. doi: 10.1097/00000658-199908000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cho BC, Jeung HC, Choi HJ, Rha SY, Hyung WJ, Cheong JH, Noh SH, Chung HC. Prognostic impact of resection margin involvement after extended (D2/D3) gastrectomy for advanced gastric cancer: a 15-year experience at a single institute. J Surg Oncol. 2007;95:461–468. doi: 10.1002/jso.20731. [DOI] [PubMed] [Google Scholar]
- 53.Sun Z, Li DM, Wang ZN, Huang BJ, Xu Y, Li K, Xu HM. Prognostic significance of microscopic positive margins for gastric cancer patients with potentially curative resection. Ann Surg Oncol. 2009;16:3028–3037. doi: 10.1245/s10434-009-0624-0. [DOI] [PubMed] [Google Scholar]
- 54.Wang SY, Yeh CN, Lee HL, Liu YY, Chao TC, Hwang TL, Jan YY, Chen MF. Clinical impact of positive surgical margin status on gastric cancer patients undergoing gastrectomy. Ann Surg Oncol. 2009;16:2738–2743. doi: 10.1245/s10434-009-0616-0. [DOI] [PubMed] [Google Scholar]
- 55.Jang YJ, Park MS, Kim JH, Park SS, Park SH, Kim SJ, Kim CS, Mok YJ. Advanced gastric cancer in the middle one-third of the stomach: Should surgeons perform total gastrectomy? J Surg Oncol. 2010;101:451–456. doi: 10.1002/jso.21431. [DOI] [PubMed] [Google Scholar]
- 56.Cascinu S, Giordani P, Catalano V, Agostinelli R, Catalano G. Resection-line involvement in gastric cancer patients undergoing curative resections: implications for clinical management. Jpn J Clin Oncol. 1999;29:291–293. doi: 10.1093/jjco/29.6.291. [DOI] [PubMed] [Google Scholar]
- 57.Macdonald JS. Gastric cancer--new therapeutic options. N Engl J Med. 2006;355:76–77. doi: 10.1056/NEJMe068121. [DOI] [PubMed] [Google Scholar]
- 58.Sobin LH, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours. In: Wiley-Blackwell O, editor. 7th ed. USA: Wiley-Blackwell; 2009. [Google Scholar]
- 59.Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ, Welvaart K, Songun I, Meyer S, Plukker JT, Van Elk P, Obertop H, et al. Extended lymph-node dissection for gastric cancer. N Engl J Med. 1999;340:908–914. doi: 10.1056/NEJM199903253401202. [DOI] [PubMed] [Google Scholar]
- 60.Cuschieri A, Weeden S, Fielding J, Bancewicz J, Craven J, Joypaul V, Sydes M, Fayers P. Patient survival after D1 and D2 resections for gastric cancer: long-term results of the MRC randomized surgical trial. Surgical Co-operative Group. Br J Cancer. 1999;79:1522–1530. doi: 10.1038/sj.bjc.6690243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wanebo HJ, Kennedy BJ, Winchester DP, Fremgen A, Stewart AK. Gastric carcinoma: does lymph node dissection alter survival? J Am Coll Surg. 1996;183:616–624. [PubMed] [Google Scholar]
- 62.Dent DM, Madden MV, Price SK. Randomized comparison of R1 and R2 gastrectomy for gastric carcinoma. Br J Surg. 1988;75:110–112. doi: 10.1002/bjs.1800750206. [DOI] [PubMed] [Google Scholar]
- 63.Wu CW, Hsiung CA, Lo SS, Hsieh MC, Chen JH, Li AF, Lui WY, Whang-Peng J. Nodal dissection for patients with gastric cancer: a randomised controlled trial. Lancet Oncol. 2006;7:309–315. doi: 10.1016/S1470-2045(06)70623-4. [DOI] [PubMed] [Google Scholar]
- 64.Wu CW, Hsiung CA, Lo SS, Hsieh MC, Shia LT, Whang-Peng J. Randomized clinical trial of morbidity after D1 and D3 surgery for gastric cancer. Br J Surg. 2004;91:283–287. doi: 10.1002/bjs.4433. [DOI] [PubMed] [Google Scholar]
- 65.Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, Cook P. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. The Surgical Cooperative Group. Lancet. 1996;347:995–999. doi: 10.1016/s0140-6736(96)90144-0. [DOI] [PubMed] [Google Scholar]
- 66.Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, van Elk P, Obertop H, Gouma DJ, Taat CW. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet. 1995;345:745–748. doi: 10.1016/s0140-6736(95)90637-1. [DOI] [PubMed] [Google Scholar]
- 67.Degiuli M, Sasako M, Ponti A; Italian Gastric Cancer Study G. Morbidity and mortality in the Italian Gastric Cancer Study Group randomized clinical trial of D1 versus D2 resection for gastric cancer. Br J Surg. 2010;97:643–649. doi: 10.1002/bjs.6936. [DOI] [PubMed] [Google Scholar]
- 68.Degiuli M, Sasako M, Ponti A, Vendrame A, Tomatis M, Mazza C, Borasi A, Capussotti L, Fronda G, Morino M; Italian Gastric Cancer Study G. Randomized clinical trial comparing survival after D1 or D2 gastrectomy for gastric cancer. Br J Surg. 2014;101:23–31. doi: 10.1002/bjs.9345. [DOI] [PubMed] [Google Scholar]
- 69.Sasako M, Sano T, Yamamoto S, Kurokawa Y, Nashimoto A, Kurita A, Hiratsuka M, Tsujinaka T, Kinoshita T, Arai K, Yamamura Y, Okajima K; Japan Clinical Oncology G. D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med. 2008;359:453–462. doi: 10.1056/NEJMoa0707035. [DOI] [PubMed] [Google Scholar]
- 70.Roviello F, Marrelli D, Morgagni P, de Manzoni G, Di Leo A, Vindigni C, Saragoni L, Tomezzoli A, Kurihara H; Italian Research Group for Gastric C. Survival benefit of extended D2 lymphadenectomy in gastric cancer with involvement of second level lymph nodes: a longitudinal multicenter study. Ann Surg Oncol. 2002;9:894–900. doi: 10.1007/BF02557527. [DOI] [PubMed] [Google Scholar]
- 71.Siewert JR, Böttcher K, Stein HJ, Roder JD. Relevant prognostic factors in gastric cancer: ten-year results of the German Gastric Cancer Study. Ann Surg. 1998;228:449–461. doi: 10.1097/00000658-199810000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Verlato G, Giacopuzzi S, Bencivenga M, Morgagni P, De Manzoni G. Problems faced by evidence-based medicine in evaluating lymphadenectomy for gastric cancer. World J Gastroenterol. 2014;20:12883–12891. doi: 10.3748/wjg.v20.i36.12883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.de Steur WO, Dikken JL, Hartgrink HH. Lymph node dissection in resectable advanced gastric cancer. Dig Surg. 2013;30:96–103. doi: 10.1159/000350873. [DOI] [PubMed] [Google Scholar]
- 74.Dikken JL, van Sandick JW, Allum WH, Johansson J, Jensen LS, Putter H, Coupland VH, Wouters MW, Lemmens VE, van de Velde CJ, et al. Differences in outcomes of oesophageal and gastric cancer surgery across Europe. Br J Surg. 2013;100:83–94. doi: 10.1002/bjs.8966. [DOI] [PubMed] [Google Scholar]
- 75.Memon MA, Khan S, Yunus RM, Barr R, Memon B. Meta-analysis of laparoscopic and open distal gastrectomy for gastric carcinoma. Surg Endosc. 2008;22:1781–1789. doi: 10.1007/s00464-008-9925-9. [DOI] [PubMed] [Google Scholar]
- 76.Haverkamp L, Weijs TJ, van der Sluis PC, van der Tweel I, Ruurda JP, van Hillegersberg R. Laparoscopic total gastrectomy versus open total gastrectomy for cancer: a systematic review and meta-analysis. Surg Endosc. 2013;27:1509–1520. doi: 10.1007/s00464-012-2661-1. [DOI] [PubMed] [Google Scholar]
- 77.Waddell T, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D; European Society for Medical O, European Society of Surgical O, European Society of R, Oncology. Gastric cancer: ESMO-ESSO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24 Suppl 6:vi57–vi63. doi: 10.1093/annonc/mdt344. [DOI] [PubMed] [Google Scholar]
- 78.Hirahara N, Tanaka T, Yano S, Yamanoi A, Minari Y, Kawabata Y, Ueda S, Hira E, Yamamoto T, Nishi T, et al. Reconstruction of the gastrointestinal tract by hemi-double stapling method for the esophagus and jejunum using EEA OrVil in laparoscopic total gastrectomy and proximal gastrectomy. Surg Laparosc Endosc Percutan Tech. 2011;21:e11–e15. doi: 10.1097/SLE.0b013e31820747f2. [DOI] [PubMed] [Google Scholar]
- 79.Kim YW, Yoon HM, Yun YH, Nam BH, Eom BW, Baik YH, Lee SE, Lee Y, Kim YA, Park JY, et al. Long-term outcomes of laparoscopy-assisted distal gastrectomy for early gastric cancer: result of a randomized controlled trial (COACT 0301) Surg Endosc. 2013;27:4267–4276. doi: 10.1007/s00464-013-3037-x. [DOI] [PubMed] [Google Scholar]
- 80.Takiguchi S, Fujiwara Y, Yamasaki M, Miyata H, Nakajima K, Sekimoto M, Mori M, Doki Y. Laparoscopy-assisted distal gastrectomy versus open distal gastrectomy. A prospective randomized single-blind study. World J Surg. 2013;37:2379–2386. doi: 10.1007/s00268-013-2121-7. [DOI] [PubMed] [Google Scholar]
- 81.Nakamura K, Katai H, Mizusawa J, Yoshikawa T, Ando M, Terashima M, Ito S, Takagi M, Takagane A, Ninomiya M, et al. A phase III study of laparoscopy-assisted versus open distal gastrectomy with nodal dissection for clinical stage IA/IB gastric Cancer (JCOG0912) Jpn J Clin Oncol. 2013;43:324–327. doi: 10.1093/jjco/hys220. [DOI] [PubMed] [Google Scholar]
- 82.Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, Ryu SW, Cho GS, Kim CY, Yang HK, et al. Prospective randomized controlled trial (phase III) to comparing laparoscopic distal gastrectomy with open distal gastrectomy for gastric adenocarcinoma (KLASS 01) J Korean Surg Soc. 2013;84:123–130. doi: 10.4174/jkss.2013.84.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Miao RL, Wu AW. Towards personalized perioperative treatment for advanced gastric cancer. World J Gastroenterol. 2014;20:11586–11594. doi: 10.3748/wjg.v20.i33.11586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shum H, Rajdev L. Multimodality management of resectable gastric cancer: A review. World J Gastrointest Oncol. 2014;6:393–402. doi: 10.4251/wjgo.v6.i10.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Prado CM, Baracos VE, McCargar LJ, Reiman T, Mourtzakis M, Tonkin K, Mackey JR, Koski S, Pituskin E, Sawyer MB. Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Clin Cancer Res. 2009;15:2920–2926. doi: 10.1158/1078-0432.CCR-08-2242. [DOI] [PubMed] [Google Scholar]
- 86.Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, Baracos VE. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008;9:629–635. doi: 10.1016/S1470-2045(08)70153-0. [DOI] [PubMed] [Google Scholar]
- 87.Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE. Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer. 2012;107:931–936. doi: 10.1038/bjc.2012.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, Murphy R, Ghosh S, Sawyer MB, Baracos VE. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013;31:1539–1547. doi: 10.1200/JCO.2012.45.2722. [DOI] [PubMed] [Google Scholar]
- 89.Schulz C, Kullmann F, Kunzmann V, Fuchs M, Geissler M, Vehling-Kaiser U, Stauder H, Wein A, Al-Batran SE, Kubin T, et al. NeoFLOT: Multicenter phase II study of perioperative chemotherapy in resectable adenocarcinoma of the gastroesophageal junction or gastric adenocarcinoma-Very good response predominantly in patients with intestinal type tumors. Int J Cancer. 2015;137:678–685. doi: 10.1002/ijc.29403. [DOI] [PubMed] [Google Scholar]
- 90.Webber EM, Kauffman TL, O’Connor E, Goddard KA. Systematic review of the predictive effect of MSI status in colorectal cancer patients undergoing 5FU-based chemotherapy. BMC Cancer. 2015;15:156. doi: 10.1186/s12885-015-1093-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.An JY, Kim H, Cheong JH, Hyung WJ, Kim H, Noh SH. Microsatellite instability in sporadic gastric cancer: its prognostic role and guidance for 5-FU based chemotherapy after R0 resection. Int J Cancer. 2012;131:505–511. doi: 10.1002/ijc.26399. [DOI] [PubMed] [Google Scholar]
- 92.Oki E, Kakeji Y, Zhao Y, Yoshida R, Ando K, Masuda T, Ohgaki K, Morita M, Maehara Y. Chemosensitivity and survival in gastric cancer patients with microsatellite instability. Ann Surg Oncol. 2009;16:2510–2515. doi: 10.1245/s10434-009-0580-8. [DOI] [PubMed] [Google Scholar]
- 93.Shi J, Qu YP, Hou P. Pathogenetic mechanisms in gastric cancer. World J Gastroenterol. 2014;20:13804–13819. doi: 10.3748/wjg.v20.i38.13804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Aichler M, Luber B, Lordick F, Walch A. Proteomic and metabolic prediction of response to therapy in gastric cancer. World J Gastroenterol. 2014;20:13648–13657. doi: 10.3748/wjg.v20.i38.13648. [DOI] [PMC free article] [PubMed] [Google Scholar]


