Abstract
Background:
In the current scenario pathogenesis of majority of the diseases is deeply linked with the oxidative stress, irrespective of its etiology. Enumerable data suggests that reactive oxygen species play a key role in multistage carcinogenesis. Oral submucous fibrosis (OSMF) is considered as a potentially malignant disorder. Its increased incidence over recent years in the Indian subcontinent is a major health concern to oral physicians. However, the role of oxidative stress has not been widely investigated in OSMF.
Aims:
Is to evaluate both antioxidant and oxidant status in OSMF and to compare with controls.
Settings and Design:
Twenty patients and 20 controls of the same age group were enrolled in the study.
Subjects and Methods:
Five milliliters of blood were collected from each individual and serum was separated. Malondialdehyde (MDA) estimation using thiobarbituric acid (TBA) method, and antioxidant activity (AOA) using principle of TBA reactive substances was done using this serum, with a calorimetric method.
Statistical Analysis Used:
Student's t-test and ANOVA test.
Results:
The mean serum AOA status was seen to significantly decrease in OSMF patients, as compared to controls (P = 0.013). The increase in mean serum MDA level was highly significant in OSMF patients, as compared to controls (P < 0.001).
Conclusion:
The disparity between AOA and MDA levels in the patients clearly demonstrates the role of oxidative stress in the disease process. The results also suggest the use of antioxidants in the management of OSMF.
Keywords: Antioxidant activity, malondialdehyde, oral submucous fibrosis, oxidative stress
Introduction
Oral submucous fibrosis (OSMF) is a chronic, irreversible disease with significant functional morbidity and increased potential for malignant transformation. The pathogenesis is till now unsettled and is believed to be multifactorial in origin. Currently, the focus of pathogenesis is on the oxidative stress. Reactive oxygen species (ROS), concerned with multistage carcinogenesis, are generated in substantial amounts during chewing of areca nut.[1] The role of oxidative stress has not been widely investigated in OSMF. With this view, the present study was undertaken to estimate the total antioxidant activity (AOA) status and malondialdehyde (MDA) levels in OSMF patients and controls.
Subjects and Methods
A total of 20 OSMF patients and 20 age-matched healthy controls, attending the outpatient Department of Oral Medicine and Radiology, in a Dental School in South India were enrolled in the study. Ethical clearance was obtained from the College Ethical Committee and written informed consent was obtained from the patients. Patients were subjected to detailed history regarding systemic condition, psychological status, habit duration, frequency, and quid keeping time. A complete clinical examination was also recorded, on a standard pro forma, followed by a biopsy. Patients with any systemic diseases and significant pathologies in the oral cavity were excluded from the study. Clinical staging was done based on mouth opening into Stage I: >40 mm, Stage II: 31–40 mm, Stage III: 21–30 mm, Stage IV: 11–20 mm, Stage V: 0–10 mm and histopathological grading was done according to Utsunomiya et al.[2]
Five milliliters of blood were collected from each individual, using aseptic measures, and samples were centrifuged at 3000 RPM for 10 min and serum was separated immediately after blood centrifugation. Serum was used immediately for analysis or was stored in small aliquots with caps at − 20°C for a maximum of 1 month until assayed. MDA estimation was done using thiobarbituric acid (TBA) method, and AOA was estimated using the principle of TBA reactive substances, by the calorimetric method.[3,4]
Data analysis was done using Statistical Package for Social Science (SPSS, version 10.5) software manufactured by IBM corporation. Student's t-test and ANOVA test were used for statistical analysis. Results were expressed as mean ± standard deviation (SD), and P < 0.05 was considered as statistically significant.
Results
The mean age of study population was 25.7 years with age range of 18–38 years. All the patients in the study group were males. According to clinical staging based on mouth opening, 4 (20%) were in Stage I, and 6 (30%), 8 (40%), and 2 (10%) were in Stage II, Stage III, and Stage IV, respectively. Based on histopathological grading, 5 (25%) were in the early stage, 7 (35%) and 8 (40%) belonged to the intermediate stage, and advanced stage, respectively.
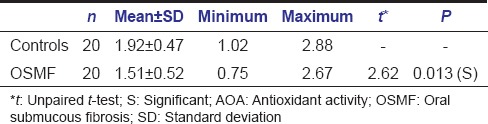
In the present study mean serum AOA status of OSMF patient was 1.51 ± 0.52 mmol/L (mean ± SD) and in control group it was 1.92 ± 0.47 mmol/L (mean ± SD) [Table 1]. The mean serum AOA status was significantly decreased in OSMF patients as compared to controls (P = 0.013). There was no significant difference between mean AOA status among patients with different clinical staging and histopathological grading.
Table 1.
Comparison of serum AOA status (mmol/L) between controls and cases
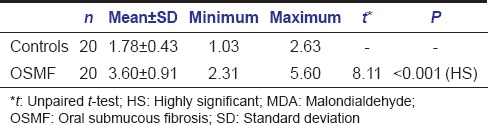
The mean serum MDA levels among OSMF patients were 3.60 ± 0.91 nmol/ml (mean ± SD) and in control group, it was 1.78 ± 0.43 nmol/ml (mean ± SD) [Table 2]. The increase in mean serum MDA level was highly significant in OSMF patients, as compared to controls (P < 0.001). However, no significant difference was noted in serum MDA levels among different clinical staging and histopathological grading.
Table 2.
Comparison of serum MDA levels (nmol/ml) between controls and cases
Discussion
In the present study, mean serum AOA status in OSMF patients were significantly lower than that of the control group, with a mean reduction of 0.41 mmol/L in OSMF patients. Serum AOA status was compared with different clinical and histopathological grading and there was no significant difference noted. Reduced antioxidant status noticed in our patients may be attributed to excessive utilization of antioxidants from the body, in order to scavenge the free radicals, generated during the pathogenesis of the disease. Reduced intake of food due to decreased mouth opening and burning sensation could well be another contributing factor.
To the best of our knowledge, there is no published data where total AOA status has been estimated in OSMF patients. However, observations from the present study were in accordance with other studies where individual antioxidant levels have been estimated.
Gupta et al. observed that serum β carotene and Vitamin E levels were considerably reduced in OSMF as compared to controls.[5] Metkari et al. noticed that superoxide dismutase and Vitamin A levels were reduced in OSMF as compared to controls.[6]
Mean serum MDA levels in OSMF patients were considerably increased as compared to controls, with a mean difference of 1.82 nmol/ml and the difference was statistically highly significant (P < 0.001). Increased MDA noticed in our study can be credited to the oxidative stress taking place in OSMF patients as demonstrated by increased heat shock protein 70, head-out immersion and nitric oxide synthase.[7,8,9] The detection of products of lipid peroxidation in biological materials has provided the basis for several popular assays for ROS and determines the involvement of oxidative stress in the pathogenesis of particular disease.[10] Results from the current study are in accordance with the various other studies like Gupta et al. and Metkari et al. who noticed increase in MDA levels in OSMF patients.[5,6]
Conclusion
From the present study, it is evident that by estimating lipid peroxidation end product and total AOA status in serum of OSMF patients, we can estimate the amount of oxidative stress tissues are undergoing during the process of pathogenesis. Hence, the administration of antioxidant supplements may be helpful in combating the disease. Further trials in this regard should be carried out to investigate the probable mechanisms by which ROS contributes for pathogenesis of OSMF. A long-term follow-up studies have to be carried out in order to draw a link between oxidative stress and malignant transformation in OSMF patients.
Acknowledgment
This work was supported by Department of Biochemistry JJMMC, Davangere, Karnataka and Department of Oral Pathology and Microbiology CODS, Davangere, Karnataka, India. We appreciate the help and suggestions given by Head of the Department and Faculty of Biochemistry Department in conducting this research activity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nair UJ, Obe G, Friesen M, Goldberg MT, Bartsch H. Role of lime in the generation of reactive oxygen species from betel-quid ingredients. Environ Health Perspect. 1992;98:203–5. doi: 10.1289/ehp.9298203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Utsunomiya H, Tilakratne WM, Oshiro K, Maruyama S, Suzuki M, Yonemochi H, et al. Extracellular matrix remodeling in OSMF. J Oral Pathol Med. 2005;34:498–507. doi: 10.1111/j.1600-0714.2005.00339.x. [DOI] [PubMed] [Google Scholar]
- 3.Dillard CJ, Kunert KJ, Tappel AL. Effects of Vitamin E, ascorbic acid and mannitol on alloxan-induced lipid peroxidation in rats. Arch Biochem Biophys. 1982;216:204–12. doi: 10.1016/0003-9861(82)90205-3. [DOI] [PubMed] [Google Scholar]
- 4.Koracevic D, Koracevic G, Djordjevic V, Andrejevic S, Cosic V. Method for the measurement of antioxidant activity in human fluids. J Clin Pathol. 2001;54:356–61. doi: 10.1136/jcp.54.5.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta S, Reddy MV, Harinath BC. Role of oxidative stress and antioxidants in aetiopathogenesis and management of oral submucous fibrosis. Indian J Clin Biochem. 2004;19:138–41. doi: 10.1007/BF02872409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Metkari SB, Tupkari JV, Barpande SR. An estimation of serum malondialdehyde, superoxide dismutase and Vitamin A in oral submucous fibrosis and its clinicopathologic correlation. J Oral Maxillofac Pathol. 2007;11:23–7. [Google Scholar]
- 7.Tsai CH, Yang SF, Lee SS, Chang YC. Augmented heme oxygenase-1 expression in areca quid chewing-associated oral submucous fibrosis. Oral Dis. 2009;15:281–6. doi: 10.1111/j.1601-0825.2009.01523.x. [DOI] [PubMed] [Google Scholar]
- 8.Thubashini M, Malathi N, Kannan L. Expression of heat shock protein 70 in oral submucous fibrosis and oral squamous cell carcinoma: An immunohistochemical study. Indian J Dent Res. 2011;22:256–9. doi: 10.4103/0970-9290.84299. [DOI] [PubMed] [Google Scholar]
- 9.Rajendran R, Varkey S. Inducible nitric oxide synthase expression is upregulated in oral submucous fibrosis. Indian J Dent Res. 2007;18:94–100. doi: 10.4103/0970-9290.33783. [DOI] [PubMed] [Google Scholar]
- 10.Pham-Huy LA, He H, Pham-Huy C. Free radicals, antioxidants in disease and health. Int J Biomed Sci. 2008;4:89–96. [PMC free article] [PubMed] [Google Scholar]


