Abstract
Background:
Oral conditions are known to affect various aspects of quality of life. Similarly, the social consequence of the quality of life in the day to day living is also equally important. Several studies have quantified the social consequences of diseases through activity limitations in people's daily living. The instruments which cover a broad spectrum of life are proposed to be compared with the clinical oral hygiene status of people from different social classes.
Aim:
To assess the validity of dental impact on daily living (DIDL) questionnaire measuring subjective dental problems and their impact in the day to day life among tribes of Wayanad.
Study Design:
Cross-sectional.
Materials and Methods:
DIDL questionnaire developed by Leao and Sheiham was used. We recorded the clinical oral health status using decayed, missing, filled, simplified oral hygiene index, and community periodontal index indices, to correlate the subjective findings of dental impact tribe to obtain construct validity of the questionnaire.
Analysis:
Descriptive statistics and Spearman's correlation using IBM SPSS software version 20.
Results:
In the study population of 250 participants, the majority of the participants were from the age group between 36 and 50 years (40%) and females were in the majority (64%). The clinical status of the participants was poor in the majority while their perceived impact in their day to day living was found to be relatively satisfied. The study results show the DIDL tool had weak validity in relation to the clinical status with relevance to the social status of Indian tribal population.
Conclusion:
The study result shows that there was insignificant and weak validity between the DIDL tool and the oral health status among these tribes who were from a low social class. This might be because their priority in life which is different from what a person from high social class. So the dental problem is ignored at the level of individual depending on his/her priority and at the community level by the policy makers.
Keywords: Dental impact on daily living, oral hygiene of tribes, Paniya tribes, quality of life questionnaire, validation of tool
Introduction
The definition of health quoted for half a centuries ago, states the importance to physical, mental, and social well-being and not the absence of disease or infirmity.[1] However, health is measured in terms of physical entity with clinical indices or pathological stages are being considered and practiced till date.[2] That is health or health status is being measured quantitatively traditionally.[3]
Assessing the dental health status in terms of quality of life has gained importance in recent days. However, the social impact of the dental problems pertaining to the individual and their perceived need for a good quality of life are been ignored. Oral conditions are known to affect various aspects in quality of life.[4] For example, the impact of dental pain or problem affecting the person's ability to work, school attendance, inability to undertake household work, etc., are some of the social problems faced by them. Several studies have quantified the social consequences of diseases through activity limitations in people's daily living.[5] This inadequacy of measuring the health in terms of quality of life has been recognized and lead to the development of measures on oral health-related quality of life and dental impact on daily living.
DIDL was developed by Leao and Sheiham under this context.[4] This included items such as appearance, pain, comfort, eating restrictions, and general performance. The available literature suggests that instruments which cover a broad spectrum of life were proposed and compared with the clinical oral hygiene status.[6,7,8,9,10,11] It has been shown that the DIDL instrument discriminates between different subjective impacts for different groups and also confirms that there are different subjective impacts for different social classes and sexes.[12]
Largest tribal concentrations in the world with various social strata present in India.[13] Among them are the tribe, who experience a low profile in relation to social class and economy. The tribes of India, consist of total population 84 million, belong to around 698 community or clans.[14] These indigenous groups of people are among the poorest and most marginalized population groups experiencing extreme levels of health deprivation.[15] Tribes are usually segregated from modern civilization. The accessibility of these tribes to medical and dental care is minimal.[16] Among the various tribal concentrations in the South India, Paniya is the largest ethnic groups of tribal people found in India. They are tribes who mostly inhabit in Kerala, while some in other parts south India. The Paniya tribes of Wayanad follow their own Paniya language, however they mostly speak, interact and write in Malayalam.[17] The subjective impacts of the oral health status among the tribes are of utmost importance as we understand the psychosocial characteristics of this marginalized population, as they are often segregated from the mainstream population. This study focuses to validate DIDL instrument created by Leao (1993) measuring the DIDL and correlating with clinical status of the tribal population.
Materials and Methods
Study settings
The study was carried out among the tribal populations of Wayanad, Kerala. Wayanad is one among 90 backward districts in India. Wayanad is primarily a rural district with 96.2% living in the rural areas.[18] The tribes dwell in groups known as colonies scattered in different taluks in and around Wayanad like vythiri, mananathawady, and sulthanbathery. Our team comprising of two dental specialists accompanied with a tribal coordinator visited the colonies to collect the data.
Study design
A cross-sectional – household survey of the tribe's in different colonies of Wayanad was done.
Study population
The study was carried out among the tribal population of Wayanad District, Kerala.
Selection of study subjects
Tribes above the age of 18 were only included in the study.
Sample size
We used a convenient sampling since the objective of the study was to test the instrument and since the tribes were scattered around as colonies. The sample size estimated for the study was 250. The questionnaire includes five domains. To validate the questionnaire, 50 samples were suggestive for each domain leading to the total sample size of 250 participants. For which 280 peoples were contacted.
Questionnaire
The questionnaire was originally developed by Leao and Sheiham, which was then linguistically adapted into Malayalam language through back-to-back translation. The translation was done by the language experts. The questionnaire was distributed among five people for translation to Malayalam, which was then given for back translation to English to another five language experts and was checked for validity method. During the pilot study the questionnaire was pilot tested with general population for which 70% of the participants reported feeling uncomfortable for answering three questions which were related to their romantic life and were not forthright with their response to it likewise the cross-cultural adoption was carried out. A pilot study was done to check the adaptation, after which few questions related to personal life was excluded from the main study which was embarrassing for them to answer. Those were the questions related to their personal romantic life.
Proforma
The proforma included consent form, the DIDL questionnaire to be administered and clinical indices which includes decayed, missing, filled (DMF), simplified oral hygiene index (OHI-S), and community periodontal index (CPI). Decayed, missing, filled teeth (DMFT) INDEX were used to assess the caries history, CPI INDEX was used to assess the periodontal status and OHI-S INDEX was used to assess the oral hygiene status of the population.
Data collection
Two dentists visited the colonies where the tribes dwell and as the oral examination and questionnaires were administered by the dental expert. The DIDL questionnaire was used to assess the subjective social-impacts following which the clinical status was examined by another expert separately. The data were collected and recorded, based on the structured questionnaire which had 33 items and also obtained information based on their age, sex, and ethnicity.
Oral examination
Oral examination was carried out for each participant by a dentist following a strict infection control protocol, under sufficient daylight or artificial source when required and collected the demographic details and clinical status of the participants using DMF, OHI-S, and CPI indices.
Statistical plan
The DIDL Scores for answers were given according to whether the impact was positive (+1), neutral (0) or negative (−1). The items within a dimension were then summed and divided by a number of dimension items. A score for each category was obtained. To establish a single total score, the summed weighted dimension scores was calculated. Dimension weights were then combined with dimension scores to obtain a final total score. The single total score ranged from 10 to −10. The DIDL responses were then grouped into three response categories that are, not at all satisfied (scores below 0), relatively satisfied (scores 0–7), and very much satisfied (scores above 7). The clinical status of these subjects was also calculated, and the findings were entered in IBM SPSS software version 20. The variables were tested, and the test showed that the distributions were not significantly different. A spearman correlation between the impact profile and DMF, OHI-S, and CPI was done to test positive and negative significant associations.
Results
Table 1 describes the study characteristic of the study population in which 280 people were contacted, out of which 250 agreed to participate, with the response rate of 89% of 250 participants in which majority of the participants from the age group between 36 and 50 years (40%) and females were in majority (64%) than the males. The chief occupation of the study participants were as agricultural manual laborers (88%).
Table 1.
Characteristics of study population
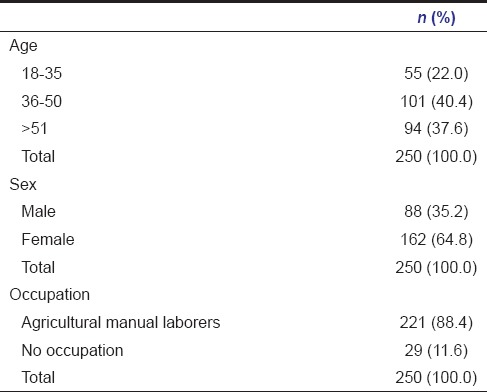
Table 2 describes the clinical status and its impact on their day to day living. The clinical status of the study population was poor for majority of participants, nearly 80% of participants had relatively poor oral hygiene and where nearly 74% of people were having the periodontal problem and more than half (60.8%) of the study population had DMF value greater than seven. However, almost all reported to be relatively satisfied (94.8%) with their dental status.
Table 2.
Characteristics of clinical status and DIDL scale
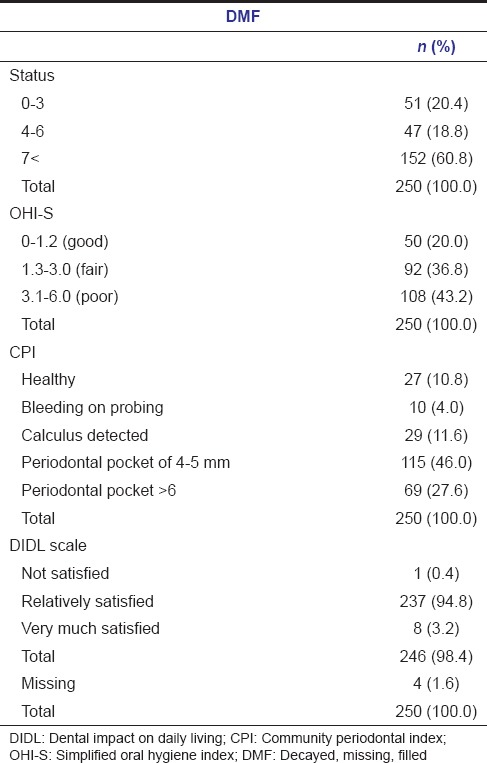
Table 3 describes the characteristic of reported response to specific questions.
Table 3.
Characteristics of response to specific domains
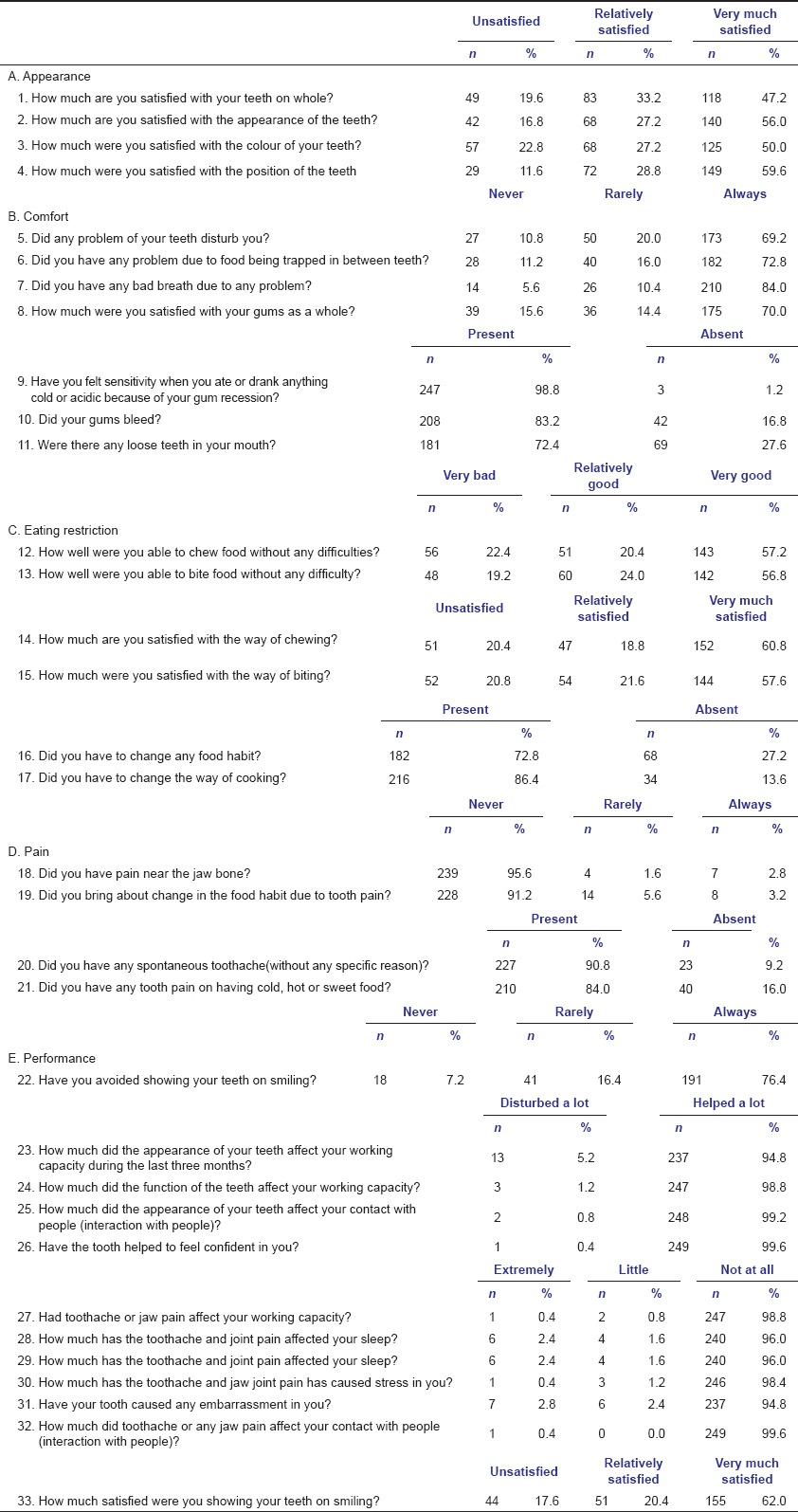
Table 4 describes the proportion of satisfaction of DIDL response. Except for eating restriction (2.4%), for which they were very much satisfied, other domains were relatively satisfied (78%) on an average.
Table 4.
Subjective impacts on five dimensions
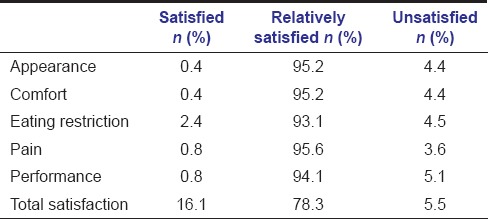
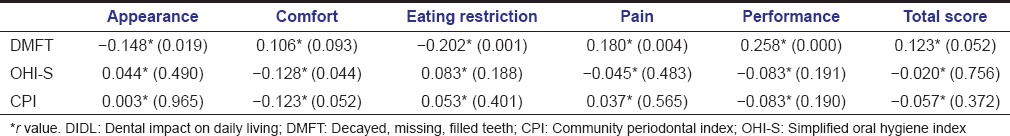
Table 5 describes the correlation between the DIDL questionnaire and the clinical status of the study population. The Spearman correlation between the impact profile and the different clinical oral health status shows that dental caries (P = 0.052) had the major impact on their daily living. DMF had significant and negative correlation with appearance (P = 0.018) and eating restrictions (P = 0.001), while pain (P = 0.004), and performance (P = 0.001) had positive correlation. Oral hygiene status had an insignificant correlation with the DIDL except for comfort (P = 0.044) which had a negative correlation. Periodontal status too had an insignificant correlation to all domains except for comfort (P = 0.052), which too had a negative correlation.
Table 5.
Spearman's correlation among DIDL scale and clinical status
Discussion
Adaptation of a psychosocial instrument requires a rigorous translation and validation to make the adopted instrument culturally relevant for the local nonwestern population.[19] Though the tribal for Wayanad had followed their own Paniya language, they were also familiar with the Malayalam language. Thus, the instrument was checked for adaptation by back-to-back translation. And from the pilot study among the general population of Kerala, it was found that certain questions related to their personal life were excluded. Those were the questions related to the personal romantic life.
Oral conditions are known to affect an individual's quality of life.[20] The impact of oral conditions is based on the perceived feelings or need of an individual which are concerned with their past experience, behavior or attitude and priority in their life.[2] There might be uncertainty in the impact of oral conditions in relation to the social class in which they belong. Literature suggests that there has been a significant difference among the sociopsychological measures with respect to the impact on their day-to-day living.[12] Some studies consider that females are more concerned about dental appearance than males.[21,22,23] But it was found that there were no significant differences between sexes in relation to any domain in the tool. Slightly higher prevalence of dissatisfaction in females (2.4%) than males (0.8%) were similar to the studies of Leao and Sheiham.[12]
The main aim of the study was to check the validation of the DIDL tool whether it can be used unanimously to all people invariably to the social class. So the study population was targeted on the marginalized and indigenous group of the population like the tribes. The study result shows that there was insignificant and weak correlation between the DIDL tool and the oral health status among these tribes who were from a low social class which might be because their priority in life which is different from what a person from high social class has. The DMF (dental caries) had a significant correlation except for comfort which showed a significant but negative correlation with respect to appearance and eating restriction that is, worse the dental caries experience worse the eating restriction and appearance. This was not similar in previous studies where dental caries had a significant difference for all domains except that it had a weak correlation.[2,12] This is suggestive that dental caries had a significant but weak impact on their daily living.
However, they had a poor oral hygiene status with more of periodontal diseases which were found to insignificant except for comfort which was negatively correlated. For example, comfort- which includes questions about bleeding, food packing, halitosis, and satisfaction with gums (periodontal status-CPI) showed a negative correlation that is, when the periodontal problem increases the comfort level decreased. This is not unexpected, given that comfort related problems could be caused by periodontal issues which are not suggestive of the previous study where comfort related issues were attributed to the filled and decayed tooth.[12] The same scenario was been noted with respect to oral hygiene status where respondents had more of debris, stains and calculus (OHI-S) but it had no significant impact on their appearance, pain or performance except for comfort. Thereby it shows that the oral hygiene had no impact on their day to day living. The literature suggest that, hardly any studies that were carried out in adult population assessing the impact with respect to periodontal and oral hygiene status, however in a study involving children's it was found that gum (gingival) related problems had affected children's oral health-related quality of life.[3] Literature also suggests that periodontal diseases are more prevalent in these tribal population.[13] This shows the concern or priority of the respondents toward the oral health status in their day to day life.
The hypothesis regarding the validity were that study results shows; the DIDL tool had weak validity in relation to the clinical status in relevance to the social status. The priorities of the respondents in their day to day life might vary from what is been depicted in the tool. Further qualitative studies are required to assess their priorities and development of the DIDL for different social classes is essential. With which the tool along with sociodemographic profile and clinical examination can serve as a comprehensive social-dental indicator.
Financial support and sponsorship
This study was funded by the Amrita Vishwa Vidyapeetham (University).
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study was funded by the Amrita Vishwa Vidyapeetham (University). We would like to thank all the assistance provided by the interns, PG scholars and staffs from the same university. The aid and assistance from Dr. Iris Valsan and Mukundan are highly appreciated.
References
- 1.WHO | Re-defining “Health”. WHO. [Last cited on 2014 Jun 20]. Available from: http://www.who.int/bulletin/bulletin_board/83/ustun11051/en .
- 2.Ganesh R, John J. A correlation between dental caries and dental impact on daily living: A cross sectional study. Indian J Oral Sci. 2013;4:70. [Google Scholar]
- 3.Gherunpong S, Tsakos G, Sheiham A. The prevalence and severity of oral impacts on daily performances in Thai primary school children. Health Qual Life Outcomes. 2004;2:57. doi: 10.1186/1477-7525-2-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leao A, Sheiham A. Chapel Hill: University of North Carolina, Dental Ecology; 1997. Dental impact on daily living. Measures of Oral Health-Related Quality of Life. [Google Scholar]
- 5.Patrick DL. Constructing social metrics for health status indexes. Int J Health Serv. 1976;6:443–53. doi: 10.2190/C26P-BKVG-WM5Q-UDKU. [DOI] [PubMed] [Google Scholar]
- 6.Reisine ST. Dental health and public policy: The social impact of dental disease. Am J Public Health. 1985;75:27–30. doi: 10.2105/ajph.75.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cushing AM, Sheiham A, Maizels J. Developing socio-dental indicators – The social impact of dental disease. Community Dent Health. 1986;3:3–17. [PubMed] [Google Scholar]
- 8.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 9.Locker D. Measuring oral health: A conceptual framework. Community Dent Health. 1988;5:3–18. [PubMed] [Google Scholar]
- 10.Locker D. Issues in measuring change in self-perceived oral health status. Community Dent Oral Epidemiol. 1998;26:41–7. doi: 10.1111/j.1600-0528.1998.tb01923.x. [DOI] [PubMed] [Google Scholar]
- 11.Leao A, Sheiham A. The development of a socio-dental measure of dental impacts on daily living. Community Dent Health. 1996;13:22–6. [PubMed] [Google Scholar]
- 12.Leao A, Sheiham A. Relation between clinical dental status and subjective impacts on daily living. J Dent Res. 1995;74:1408–13. doi: 10.1177/00220345950740071301. [DOI] [PubMed] [Google Scholar]
- 13.Philip B, Chithresan K, Vijayaragavan VS, Maradi A. Prevalence of periodontal diseases among the adult tribal population in Nilgiris – An epidemiological study. [Last cited on 2014 Feb 10];Int J Public Health Dent. 2013 4:8–12. Available from: http://www.journalgateway.com/ijphd/article/view/446 . [Google Scholar]
- 14.Census of India: Scheduled Castes and Scheduled Tribes. [Last cited on 2014 Feb 06]. Available from: http://www.censusindia.gov.in/Census_And_You/scheduled_castes_and_sceduled_tribes.aspx .
- 15.Paniya People. Wikipedia Free Encycl. 2014. [Last cited on 2014 Feb 06]. Available from: http://www.en.wikipedia.org/w/index.php?title=Paniya_people & oldid=587822746 .
- 16.Pranjali B. Glimpses of adivasi situation in Gudalur, The Nilgiris. Frontier. 2010;43:12–5. [Google Scholar]
- 17.Paniya Tribes | Tribe and Smile. [Last cited on 2014 Feb 06]. Available from: http://www.tribeandsmile.org/paniya .
- 18.Demographics in Wayanad District – Population, Age Group Population, Religion, Scheduled Caste and Scheduled Tribe, Others, Projected Total Population, Projected Rural and Urban Population, Town and Village-wise Total Population in Wayanad District. [Last cited on 2014 Dec 09]. Available from: http://www.districtwayanad.com/demographics/index.aspx .
- 19.Astrøm AN, Okullo I. Validity and reliability of the oral impacts on daily performance (OIDP) frequency scale: A cross-sectional study of adolescents in Uganda. BMC Oral Health. 2003;3:5. doi: 10.1186/1472-6831-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO | Oral Health, General Health and Quality of Life. WHO. [Last cited on 2014 Oct 04]. Available from: http://www.who.int/bulletin/volumes/83/9/editorial30905html/en .
- 21.Kateeb E. Gender-specific oral health attitudes and behaviour among dental students in Palestine. East Mediterr Health J. 2010;16:329–33. [PubMed] [Google Scholar]
- 22.Tin-Oo MM, Saddki N, Hassan N. Factors influencing patient satisfaction with dental appearance and treatments they desire to improve aesthetics. BMC Oral Health. 2011;11:6. doi: 10.1186/1472-6831-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bernabé E, Tsakos G, Messias de Oliveira C, Sheiham A. Impacts on daily performances attributed to malocclusions using the condition-specific feature of the Oral Impacts on Daily Performances Index. Angle Orthod. 2008;78:241–7. doi: 10.2319/030307-111.1. [DOI] [PubMed] [Google Scholar]


