Abstract
Background
Few studies have investigated the association between coronary artery calcium (CAC) progression and arterial stiffness measured by brachial-ankle pulse wave velocity (baPWV). We examined the influence of the severity of baseline baPWV on CAC progression in a large prospective cohort.
Methods
A total of 1600 subjects who voluntarily participated in a comprehensive health-screening program between March 2010 and December 2013 and had baseline baPWV as well as CAC on baseline and serial follow-up computed tomography performed approximately 2.7 ± 0.5 years apart were enrolled in the study.
Results
A total of 1124 subjects were included in the analysis (1067 men; mean age, 43.6 ± 5.1 years). An increased CAC score was found in 318 subjects (28.3 %) during the follow-up period. Baseline higher baPWV was significantly correlated with CAC progression, especially in subjects with third- and fourth-quartile values (adjusted odds ratio [OR] 2.04; 95 % confidence interval [CI] 1.33–3.15 and OR 2.14; 95 % CI 1.34–3.41, respectively) compared with the lowest-quartile values (P for trend <0.001). A similar effect was observed in diabetic subjects. Among the 835 subjects with a baseline CAC score = 0, progression to CAC score >0 was associated with male sex, diabetes, and higher baPWV. However, among the 289 individuals with a baseline CAC score >0, only the presence of CAC itself was predictive of CAC progression.
Conclusions
Higher arterial stiffness measured by baPWV could be significantly associated with CAC progression.
Electronic supplementary material
The online version of this article (doi:10.1186/s12933-015-0311-3) contains supplementary material, which is available to authorized users.
Keywords: Arterial stiffness, baPWV, Cardiometabolic risk factors, Cardiovascular disease (CVD), Coronary arterial calcification
Background
The presence of coronary artery calcium (CAC) is significantly correlated with the risk of coronary heart disease [1] and poor prognosis [2–6]. CAC can be measured using either electron beam computed tomography (CT) or multidetector CT (MDCT) by the Agatston scoring method [7]. In both men and women, CT-measured CAC values are highly sensitive for the presence of ≥50 % angiographic stenosis but only moderately specific (91 and 49 %, respectively) [8]. However, the absence of CAC is highly predictive of the absence of significant coronary artery stenosis and is used to identify individuals at low clinical risk [9].
Although serial measurements of CAC may be useful to assess the activity of the atherosclerotic process or monitor the efficacy of medications used to slow or halt the progression of coronary atherosclerosis, serial CAC studies are of unproven clinical value and are thus not recommended. However, several studies have shown an association between CAC progression and traditional risk factors and increased risk of cardiovascular events [10–12].
Arterial stiffness measured by aortic pulse wave velocity (PWV) is a potential predictor of cardiovascular events [13, 14]. Brachial-ankle pulse wave velocity (baPWV), a promising technique used to assess arterial stiffness, is simple, noninvasive, and nonradiating. BaPWV may provide information similar to that derived from central PWV [15] and is independently associated with the presence and severity of coronary artery disease (CAD) [16–18].
Because few studies have investigated the association between baPWV and CAC progression, it is unclear whether baPWV can be used to identify subjects with progressive subclinical CAC. We examined the influence of the severity of baseline baPWV on CAC progression in a prospective cohort.
Methods
Study subjects
The Kangbuk Samsung Health Study (KSHS) is a Korean cohort study enrolling all men and women 18 years of age or older who voluntarily undergo comprehensive health-screening examinations at the Kangbuk Samsung Hospital Healthcare Centers in Seoul and Suwon, South Korea. Our study included all KSHS participants who had undergone cardiac CT scanning and baPWV measurements as part of their chosen comprehensive health-screening examination from March 2010 to December 2013 (Fig. 1). A total of 2650 subjects had CAC on baseline and serial follow-up scans performed approximately 2.7 ± 0.5 years apart. Among them, 1,600 subjects underwent baseline baPWV during the same period as the first CT scan. We excluded 97 subjects with a history of definite cardio-cerebro-peripheral vascular disease (n = 52), low ankle-brachial index (ABI) (n = 1), or malignancy (n = 44). An additional 379 subjects were excluded because of missing data for the variables included in this study. Finally, total 1124 subjects were included in this analysis (1067 men and 57 women; mean age, 43.6 ± 5.1 years). This study was approved by the Institutional Review Board of the Kangbuk Samsung Hospital.
Fig. 1.
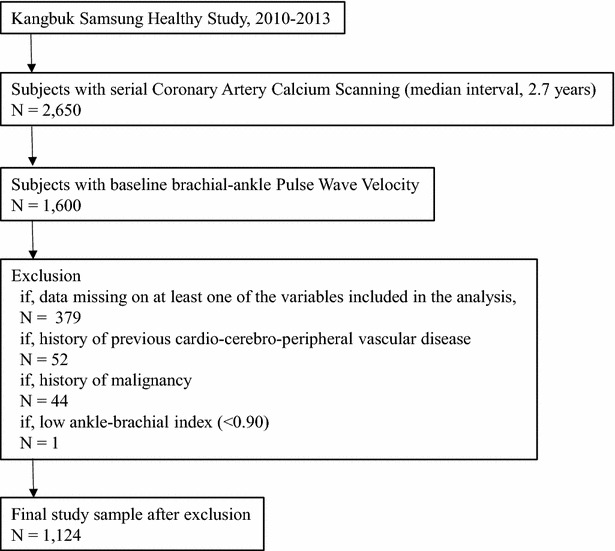
Study population. This flowchart summarizes the source and study population of this study
Data collection
All examinations were conducted at the Kangbuk Samsung Health Screening Center clinics in Seoul and Suwon by trained personnel, following a standardized protocol. A self-administered questionnaire was used to collect information about sociodemographic characteristics, lifestyle factors, medical history, family history, and medication use. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Trained examiners measured blood pressure in the sitting position at least three times using an automated oscillometric device. Blood was drawn from participants after fasting for ≥10 h and analyzed at the Laboratory Medicine Department at the Kangbuk Samsung Hospital. Diabetes was defined as a self-reported history of diabetes, the use of glucose-lowering medications, and/or HbA1c ≥6.5 %.
BaPWV was recorded in the supine position using a VP-1000 (OMRON, Kyoto, Japan), which measures bilateral brachial and posterior tibial artery pressure waveforms using an oscillometric method with cuffs placed on both arms and ankles. BaPWV was calculated automatically for each arterial segment as the path length divided by the corresponding time interval. A validation study of baPWV measurements in an Asian population reported interobserver and intraobserver correlation coefficients of 0.98 and 0.87, respectively [19]. The coefficients of variation in our sample for left and right baPWV were 12.3 and 12.6 %, respectively. The average baPWV was adopted as the mean of the right and left measurements and used for the analyses.
CT scans were obtained using a Lightspeed VCT XTe-64 slice MDCT scanner (GE Healthcare, CA, USA). All scans used the same standard scanning protocol (2.5 mm slice thickness, 400 ms rotation time, 120 kV tube voltage, and 124 mAS ECG-gated dose-modulated tube current (310 mA × 0.4 s)). CAC was scored following the standard Agatston method [20]. CAC measurements had interobserver and intra-observer intraclass correlation coefficients of 0.99 under this protocol. CAC values were scored by a certified CT technologist and were subsequently blindly overread by a board-certified at least two, radiologist with sufficient experience.
Statistical analysis
Demographic characteristics and cardiovascular risk factors of the study participants were calculated and stratified by baPWV quartiles. Categorical variables are presented as number (%) and continuous variables as mean (standard deviation [SD]) or median (interquartile range [IQR]) based on the distribution of data. Differences across quartiles were tested using Chi square or analysis of variance (ANOVA) tests. The distribution of continuous variables was evaluated, and right-skewed variables (triglycerides, alanine transaminase [ALT], gamma-glutamyltransferase [GTP], and high-sensitivity C-reactive protein [hsCRP]) were log transformed for the one-way ANOVA. To test for linear trends, we included the median value of each category as a continuous variable in the regression model. To evaluate the association of CAC progression across baPWV quartiles, we used a binomial logistic regression model to estimate odds ratios (ORs) with 95 % confidence intervals (CIs) for CAC progression. We used three models to progressively adjust for potential confounders. We initially adjusted for age. Model 1 was further adjusted for sex, center, year of screening examination, smoking status, alcohol intake, educational level, BMI, diabetes, hypertension, and high-density lipoprotein (HDL), low-density lipoprotein (LDL), and glucose levels. In model 2, we further adjusted for systolic blood pressure and heart rate. Finally, we analyzed the impact of baPWV and pulse pressure (PP) on CAC progression by dividing subjects into two groups according to median baPWV and PP values.
A two-sided P value <0.05 was considered significant. Statistical analyses were performed using Stata version 12 (Stata Corp. 2011, College Station, TX, USA).
Results
A total of 1124 subjects had CAC on baseline and follow-up scans performed approximately 2.7 ± 0.5 years apart. Their mean age was 43.6 years, and 94.9 % were men; 31.8 % of subjects were current smokers, 8.2 % had diabetes, and 24.6 % had hypertension. Mean CAC scores were 17.8 ± 81.8 at baseline and 29.2 ± 114.9 at follow-up. Study participants in the highest baPWV quartiles were more likely to be older, male, or heavy drinkers and have diabetes or hypertension; higher blood pressure, glucose, total cholesterol, triglyceride, ALT, GTP, and CRP; and lower HDL (Table 1).
Table 1.
Baseline characteristics of study participants by brachial-ankle pulse wave velocity quartiles
| Characteristics | PWV quartiles | P for trend | |||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| PWV (cm/sec) | 977–1256.5 | 1256.5–1345.5 | 1345.5–1441.5 | 1441.5–2397.5 | <0.001 |
| Number | 281 | 281 | 282 | 280 | |
| Age (years)a | 42.3 (4.5) | 43.3 (4.3) | 43.8 (5.2) | 45.0 (6.0) | <0.001 |
| Male (%) | 89.7 | 94.0 | 96.8 | 99.3 | 0.001 |
| BMI (kg/m2) | 25.1(3.3) | 24.9 (2.8) | 25.1 (3.2) | 25.4 (2.9) | 0.155 |
| Obesity (%) | 43.8 | 47.1 | 53.6 | 52.9 | 0.012 |
| Current smoker (%) | 26.3 | 31.0 | 30.9 | 33.9 | 0.065 |
| Alcohol intake (%)b | 28.1 | 32.4 | 32.3 | 40.7 | 0.003 |
| High education level (%)c | 84.2 | 82.3 | 87.7 | 80.8 | 0.655 |
| Diabetes (%) | 5.0 | 6.4 | 9.6 | 16.1 | <0.001 |
| Hypertension (%) | 10.3 | 23.8 | 26.2 | 42.9 | <0.001 |
| Systolic BP (mmHg)a | 113.9 (10.8) | 118.7 (11.5) | 119.3 (11.2) | 126.5 (11.5) | <0.001 |
| Diastolic BP (mmHg)a | 72.6 (8.1) | 76.0 (8.8) | 76.5 (8.0) | 81.5 (9.0) | <0.001 |
| Glucose (mg/dL)a | 94.4 (11.1) | 98.1 (18.3) | 99.2 (18.1) | 105.3 (23.6) | <0.001 |
| Total cholesterol (mg/dL)a | 203.5 (37.4) | 212.0 (35.5) | 213.6 (39.5) | 210.8 (37.5) | 0.020 |
| LDL-C (mg/dL)a | 126.4 (34.1) | 133.5 (32.3) | 134.6 (34.6) | 130.1 (33.8) | 0.174 |
| HDL-C (mg/dL)a | 53.2 (13.8) | 50.5 (10.7) | 49.7 (11.4) | 51.0 (12.0) | 0.022 |
| Triglycerides (mg/dL)d | 114 (80–156) | 138 (98–192) | 139 (99–200) | 163 (114–227.5) | <0.001 |
| ALT (U/l)d | 22 (16–31) | 24 (18–35) | 27 (20–41) | 28 (20–42) | <0.001 |
| GTP (U/l)d | 29 (19–43) | 35 (24–54) | 40 (26–58) | 41 (28.5–68) | <0.001 |
| C-reactive protein (mg/L)d | 0.05 (0.03–0.12) | 0.06 (0.04–0.11) | 0.07 (0.04–0.11) | 0.07 (0.04–0.14) | 0.005 |
Data are a means (standard deviation), d medians (interquartile range), or percentages
SI unit conversion (multiply the conversion factors to obtain the SI unit): glucose, 0.0555 (mmol/L); Total cholesterol, 0.0259 (mmol/L); LDL-C, 0.0259 (mmol/L); HDL-C, 0.0259 (mmol/L); Triglyceride, 0.0113 (mmol/L); C-reactive protein, 10 (mg/L)
ALT alanine aminotransferase, GTP glutamyl transpeptidase, BMI body mass index, BP blood pressure, HDL-C high-density lipoprotein-cholesterol, b ≥20 g/day; c ≥College graduate
During the median 2.7-year follow-up period, 318 subjects (28.3 %) had an increased CAC score at follow-up examination compared with baseline. CAC progression was seen in 76 of 835 subjects (9.1 %) with baseline CAC = 0 but in 242 of 289 subjects (83.7 %) with baseline CAC > 0. Compared with subjects with no change in CAC values, those with an increase in CAC levels were more likely to be older, male, obese, or heavy drinkers and have diabetes or hypertension; higher BMI, blood pressure, fasting glucose, LDL, ALT, GTP, or CRP; and lower HDL cholesterol (Table 2). Study participants in the highest baPWV quartiles were more likely to have more severe progression of CAC compared with those in the lower baPWV quartiles (Table 3).
Table 2.
Baseline characteristics of study participants by Coronary Calcium Score change in serial examination
| Characteristics | CAC change | P for trend | |
|---|---|---|---|
| CAC change = 0 | CAC change >0 | ||
| Number | 806 | 318 | |
| Age (years)a | 42.9 (5.0) | 45.3 (5.2) | <0.001 |
| Male (%) | 93.1 | 99.7 | <0.001 |
| BMI (kg/m2) | 24.9 (3.0) | 25.8 (2.9) | <0.001 |
| Obesity (%) | 45.4 | 59.1 | <0.001 |
| Current smoker (%) | 32.5 | 30.9 | 0.605 |
| Alcohol intake (%)b | 32.3 | 38.7 | 0.018 |
| High education level (%)c | 82.9 | 86.2 | 0.188 |
| Diabetes (%) | 7.1 | 14.5 | <0.001 |
| Hypertension (%) | 21.8 | 35.9 | <0.001 |
| Systolic BP (mmHg)a | 118.9 (12.3) | 121.3 (11.4) | 0.003 |
| Diastolic BP (mmHg)a | 76.1 (9.1) | 77.9 (8.7) | 0.002 |
| Glucose (mg/dL)a | 97.6 (16.4) | 103.4 (23.2) | <0.001 |
| Total cholesterol (mg/dL)a | 206.4 (37.1) | 219.1 (37.6) | <0.001 |
| LDL-C (mg/dL)a | 127.9 (33.0) | 139.5 (34.5) | <0.001 |
| HDL-C (mg/dL)a | 51.7 (12.4) | 49.6 (11.0) | <0.001 |
| Triglycerides (mg/dL)d | 130 (90–191) | 153 (113–215) | <0.010 |
| ALT (U/l)d | 25 (18–37) | 28 (20–40) | <0.001 |
| GTP (U/l)d | 34 (22–54) | 40 (27–65) | <0.001 |
| C-reactive protein (mg/L)d | 0.06 (0.03–0.11) | 0.07 (0.04–0.13) | 0.022 |
Data are ameans (standard deviation), dmedians (interquartile range), or percentages
SI unit conversion (multiply the conversion factors to obtain the SI unit): glucose, 0.0555 (mmol/L); Total cholesterol, 0.0259 (mmol/L); LDL-C, 0.0259 (mmol/L); HDL-C, 0.0259 (mmol/L); Triglyceride, 0.0113 (mmol/L); C-reactive protein, 10 (mg/L)
ALT alanine aminotransferase, GTP glutamyl transpeptidase, BMI body mass index, BP blood pressure, HDL-C high-density lipoprotein-cholesterol; b ≥20 g/day; c ≥College graduate
Table 3.
Degree of change in Coronary Calcium Score according to brachial-ankle pulse wave velocity quartiles
| Characteristics | PWV quartiles | P for trend | |||
|---|---|---|---|---|---|
| Q1 (N = 281) | Q2 (N = 281) | Q3 (N = 282) | Q4 (N = 280) | ||
| Amount of interval change | <0.001 | ||||
| No interval change | 232 | 219 | 184 | 171 | |
| 1–9 | 117 | 19 | 33 | 31 | |
| 10–99 | 29 | 38 | 59 | 60 | |
| ≥100 | 3 | 5 | 6 | 18 | |
In multivariate logistic regression analysis, baseline PWV was significant correlated with CAC progression during follow-up, especially among subjects in the third and fourth quartiles (adjusted OR, 2.04; 95 % CI 1.33–3.15 and OR, 2.14; 95 % CI 1.34–3.41, respectively) compared with those in the lowest quartile (P for trend <0.001) (Table 4). In diabetic patients, these associations remained significant for subjects in the third and fourth quartiles (adjusted OR, 3.50; 95 % CI 1.80–5.20 and OR 3.85; 95 % CI 1.88–5.82, respectively). Another analyses using SQRT method to determine CAC progression and baPWV also showed significant correlation between them (Additional file 1: Tables 1, 2). Using a cutoff point of 10 in CAC change, the progression of CAC was still significantly associated with baseline baPWV (Additional file 1: Table 3).
Table 4.
The risk of progression of Coronary Calcium Score according to baseline brachial-ankle pulse wave velocity quartiles odds ratio (95 % CI) of CAC change >0 by PWV quartiles
| Number | Cases | Age-adjusted ORa (95 % CI) | Multivariate-adjusted ORa
(95 % CI) |
||
|---|---|---|---|---|---|
| Model 1 | Model 2 | ||||
| Total | |||||
| Q1 | 281 | 47 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Q2 | 281 | 63 | 1.29 (0.84–1.98) | 1.12 (0.72–1.75) | 1.16 (0.74–1.82) |
| Q3 | 282 | 99 | 2.31 (1.54–3.47) | 1.95 (1.27–2.99) | 2.04 (1.33–3.15) |
| Q4 | 280 | 109 | 2.34 (1.55–3.52) | 1.90 (1.22–2.95) | 2.14 (1.34–3.41) |
| P for trend | <0.001 | 0.001 | <0.001 | ||
OR odds ratio, CI confidence interval
aEstimated from logistic regression. Multivariable model 1 was adjusted for age, sex, center, year of screening exam, smoking status, alcohol intake, educational level, BMI, diabetes, hypertension, HDL, LDL and glucose; model 2: model 1 plus adjustment for sbp and heart rate
Among study subjects with baseline CAC = 0, higher baPWV could better predict the likelihood of CAC progression compared with lower baPWV quartile values (Table 5), although baseline PP could not predict CAC progression (higher PP group, adjusted hazard ratio [HR], 0.92; 95 % CI 0.63–1.27, compared with lower half of PP). After analyzing the interaction between PP and PWV, PP was still not a significant predictor or CAC progression. Only higher PWV (>50 %), regardless of PP, was significantly associated with CAC progression (Table 6).
Table 5.
Risk of progression of Coronary Calcium Score according to baseline brachial-ankle pulse wave velocity quartiles odds ratio (95 % CI) of CAC change >0 by PWV quartiles among subjects with baseline CAC = 0
| Number | Cases | Age-sex-adjusted ORa (95 % CI) | Multivariate-adjusted ORa
(95 % CI) |
||
|---|---|---|---|---|---|
| Model 1 | Model 2 | ||||
| Total | |||||
| Q1 | 236 | 8 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Q2 | 219 | 17 | 1.22 (0.93–5.27) | 2.28 (0.94–5.51) | 1.26 (0.93–5.50) |
| Q3 | 202 | 30 | 4.38 (1.95–9.83) | 4.21 (1.83–9.68) | 1.15 (1.79–9.61) |
| Q4 | 178 | 21 | 3.05 (1.31–7.12) | 3.16 (1.29–7.70) | 3.04 (1.20–7.73) |
| P for trend | 0.003 | 0.004 | 0.006 | ||
OR odds ratio, CI confidence interval
aEstimated from logistic regression. Multivariable model 1 was adjusted for age, sex, center, year of screening exam, smoking status, alcohol intake, educational level, BMI, diabetes, hypertension, HDL, LDL and glucose; model 2: model 1 plus adjustment for sbp and heart rate
Table 6.
Risk of progression of Coronary Calcium Score according to pulse pressure and brachial-ankle pulse wave velocity odds ratioa (95 % CI) of CAC change >0 by PWV50 % and pulse pressure 50 %
| Number | Cases | Age and sex-adjusted ORa (95 % CI) | Multivariate-adjusted ORa (95 % CI) | ||
|---|---|---|---|---|---|
| Model 1 | Model 2 | ||||
| Pulse pressure | |||||
| Pulse pressure <50 % | 574 | 159 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Pulse pressure ≥50 % | 550 | 159 | 1.01 (0.77–1.32) | 0.91 (0.68–1.21) | 0.90 (0.63–1.28) |
| Pulse Pressure and Pulse Wave Velocity | |||||
| PWV <50 % and pulse pressure <50 % | 322 | 66 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| PWV <50 % and pulse pressure ≥50 % | 240 | 44 | 0.90 (0.58–1.39) | 0.85 (0.54–1.33) | 0.90 (0.55–1.46) |
| PWV ≥50 % and pulse pressure <50 % | 252 | 93 | 2.01 (1.37–2.95) | 1.82 (1.22–2.72) | 1.88 (1.26–2.82) |
| PWV ≥50 % and pulse pressure ≥50 % | 310 | 115 | 1.88 (1.30–2.72) | 1.57 (1.06–2.32) | 1.75 (1.09–2.80) |
| P for trend | <0.001 | 0.002 | <0.001 | ||
OR odds ratio, CI confidence interval
aEstimated from logistic regression. Multivariable model 1 was adjusted for age, sex, center, year of screening exam, smoking status, alcohol intake, educational level, BMI, diabetes, hypertension, HDL, LDL and glucose; model 2: model 1 plus adjustment for sbp and heart rate
In multivariate analysis, progression to CAC > 0 among 835 subjects with CAC = 0 was associated with male sex (OR 3.10; 95 % CI 2.25–3.95; P < 0.001), diabetes (OR 1.90; 95 % CI 1.05–2.85; P = 0.004), and higher PWV (OR 1.85; 95 % CI 1.20–2.45; P = 0.001). However, among the 289 individuals with baseline CAC > 0, only the presence of CAC itself (OR, 14.85; 95 % CI 12.10–17.25; P < 0.001) rather than other CAD risk factors was predictive of CAC progression.
Discussion
Our study clearly demonstrates that arterial stiffness, measured by baPWV, can predict progression of CAC in Korean adults and suggests that noninvasive, nonradiating, and readily available baPWV could be a better surrogate marker of CAC progression than PP. The findings of our study are consistent with those of other studies showing a significant association between several surrogate markers of arterial stiffness (measured using various parameters) and CAC [14, 16, 17, 21, 22].
Several clinical risk factors including microalbuminuria or statin use are related to CAC incidence and progression, especially in patients with diabetes mellitus [23–26]. CAC nearly inevitably progress, with limited influence of traditional risk factors, so prediction or calculation of progression of CAC might be important [25, 27]. Because CAC scanning using MDCT is a test commonly used in clinical practice as a single examination rather than serial examinations, performance of multiple CAC tests in the same setting might be impracticable and hazardous owing to radiation exposure. Although serial measurements of CAC might be meaningful, no intervention, including statin therapy [28], has been shown to slow CAC progression, and serial measurements of CAC are of unproven clinical value. On the other hand, baPWV is a relatively simple, noninvasive, nonradiating, and readily available combined measure of central and peripheral arterial stiffness. Unlike carotid–femoral pulse wave velocity, which is a measure of central arterial stiffness, baPWV is a combined measure of central and peripheral arterial stiffness. BaPWV may provide information similar to that derived from central PWV [15] and is independently associated with the presence and severity of CAC [16, 17, 29]. Our study shows a significant correlation between baPWV and CAC progression in apparently healthy subjects. From a clinical perspective, this convenient, nonradiating, and easily available tool may help identify CAC progression, irrespective of CAC presence.
Several plausible mechanisms may be responsible for the association between baPWV and coronary atherosclerosis as expressed by CAC. First, some common risk factors possibly contribute to arterial stiffness and atherosclerosis, and this is more likely in the peripheral arteries. ABI is also associated with the incidence and severity of coronary atherosclerosis [30]. Secondly, given that the aorta forms a large portion of the arterial tree over which baPWV is measured, 58 % of the variation in baPWV can be explained by aortic PWV [15]. Thus, baPWV is not only a marker of peripheral arterial stiffness but also an indirect marker of central arterial stiffness. Thirdly, arterial stiffness could increase the mechanical shear stress on the arterial wall side and cardiac afterload. This can trigger the initial pathophysiologic cascade, which leads to atherosclerotic changes and cardiac remodeling.
Diabetes mellitus is associated with an increased risk of arterial stiffness and atherosclerotic cardiovascular disease. [31] Vascular calcification, including coronary artery calcification, significantly improved the prediction of outcome compared with the consideration of traditional risk factors, [32, 33] and baPWV improved the ability to identify diabetic individuals at high risk of future cardiovascular events. [34] The combined assessment of CAC and baPWV also could more effectively predict cardiac events than the CAC score alone [35]. Therefore, to predict future events, baPWV might have the potential for wide clinical applications, especially in diabetic patients.
Our study showed that PP, a surrogate marker of arterial stiffness, could not predict CAC progression, unlike baPWV. Generally, increases in PP result from factors that increase and/or decrease systolic and diastolic pressure, respectively. Changes in PP are mostly related to changes in systolic blood pressure, particularly among the elderly, and are usually the result of stiffness in the large arteries as well as an early pulse wave reflection. Although increases in peripheral vascular resistance appear to be a relatively more important component of hypertension in younger patients (younger than 50 years), the role of peripheral vascular resistance in hypertension diminishes progressively with age [36, 37]. Given the known effects of aging on vessel stiffness, increases in PP in older patients result from aortic stiffening, whereas increases in younger patients are more likely to result from increases in stroke volume. Subjects in our cohort had an average age of 43.6 years, which means that higher PP is not likely related to higher arterial stiffness and as a result is not associated with CAC progression.
In our study, during the follow-up period of 2.7 ± 0.5 years, approximately 9.1 % of subjects (76/835) with CAC = 0 at baseline had increases in CAC, whereas CAC progression was observed in 83.7 % of subjects (242/289) with a baseline CAC > 0. This conversion rate is very similar to that reported in a previous study [38]. In that study, 106 of 422 subjects (25.1 %) with no baseline CAC had a positive CAC score during the follow-up period. Conversion from a CAC score of 0 to >0 occurred in 2 (0.5 %), 5 (1.2 %), 24 (5.7 %), 26 (6.2 %), and 49 (11.6 %) subjects after 1, 2, 3, 4, and 5 years of follow up, respectively [38]. Our study also showed that the presence of diabetes, male sex, and higher baPWV were associated with CAC progression in subjects with baseline CAC = 0 whereas in subjects with baseline CAC > 0, only the presence of CAC could predict CAC progression. So far, no clinical factor seems to mandate repeat CAC scanning, but baPWV is able to help predict CAC progression.
Limitations
The chief limitation of our study was a lack of data regarding how patients with normal CAC values were treated by their physicians. The treatment of risk factors such as hypertension, diabetes, or dyslipidemia was left to the discretion of the physicians and subjects, which could have resulted in significant treatment bias. Thus, it is difficult to determine the magnitude of any confounding effects of treatment for risk factors that may have altered the natural course of CAC progression. Additional unmeasured confounders that can modify calcification processes, such as fetuin A, novel inflammatory markers, and additional risk factors (e.g., renal failure, thyroid status, or family history), may mediate this accelerated risk. This study did not evaluate such markers but instead limited its evaluation to the association between baPWV and CAC progression. Secondly, the study design was cross-sectional, which might preclude casual correlation. Thirdly, arterial stiffness was measured using baPWV, for which there is a relative lack of scientific evidence compared with carotid-femoral PWV, the gold standard of arterial stiffness measurement. However, previous studies have shown a high correlation between baPWV and aortic PWV [39]. Currently, baPWV is widely used in Asia, and evidence of its value is growing with time. Fourthly, our study comprised Korean adults voluntarily attending a health-screening program and was primarily performed in men, a small proportion of whom had diabetes. Fifthly, a CAC score between 0 and 10 is likely to represent noise. Although the reproducibility of CAC scores is high, the reproducibility of scores between 0 and 9 is an issue. As compared to those who scored 10 or greater, variation was very high among subjects who scored between 0 and 9, which might have had a significant impact on our results. Finally, our follow-up period was relatively short, without evaluation of clinical outcomes, which gives our findings limited generalizability.
Conclusions
Higher arterial stiffness measured by baPWV could be significantly associated with CAC progression.
Authors’ contributions
KS takes full responsibility for the data collection and integrity of the analyses. JY contributed to the hypothesis, participated in its design and drafted the manuscript. SR participated in the design of the study and performed the statistical analysis. SL, BK1, BK2, JK1, EC, JK2, JP reviewed/edited the manuscript and contributed to discussion. KS is the guarantor for the article and all authors have read and agreed the manuscript as written. All authors read and approved the final manuscript.
Acknowledgements
We acknowledge the efforts of the health screening group at Kangbuk Samsung Hospital, Korea.
Competing interests
The authors declare that they have no competing interests.
Abbreviations
- ABI
ankle-brachial index
- ALT
alanine transaminase
- baPWV
brachial-ankle pulse wave velocity
- BMI
body-mass index
- CAC
coronary artery calcium
- CAD
coronary artery disease
- CI
confidence interval
- CT
computed tomography
- GTP
gamma-glutamyltransferase
- hsCRP
high-sensitivity C-reactive protein
- HDL
high-density lipoprotein
- LDL
low-density lipoprotein
- MDCT
multidetector computed tomography
- OR
odds ratio
- PP
pulse pressure
- PWV
pulse wave velocity
Additional file
10.1186/s12933-015-0311-3 Table 1. The Risk of Progression of Coronary Calcium Score According to Baseline Brachial-Ankle Pulse Wave Velocity: Odds Ratio (95 % Confidence Interval) of Difference [√CAC(follow-up) − √CAC(baseline)] >2.5 by Pulse Wave Velocity quartiles—The SQRT Analysis. Table 2. The Risk of Progression of Coronary Calcium Score According to Pulse Pressure and Brachial-ankle Pulse Wave Velocity: Odds ratio (95 % Confidence Interval) of Difference [√CAC(follow-up) − √CAC(baseline)] >2.5 by Pulse Wave Velocity 50 % and pulse pressure 50 %—The SQRT Analysis. Table 3. The Risk of Progression of Coronary Calcium Score According to Baseline Brachial-Ankle Pulse Wave Velocity: Odds ratio (95 % Confidence Interval) of Coronary Calcium Score Change change >=10 by Pulse Wave Velocity Quartiles.
Contributor Information
Jong-Young Lee, Email: jyleeheart.lee@samsung.com.
Seungho Ryu, Email: sh703.yoo@samsung.com.
Sung Ho Lee, Email: shsh96.lee@samsung.com.
Byung Jin Kim, Email: bjjake.kim@samsung.com.
Bum-Soo Kim, Email: bsmed.kim@samsung.com.
Jin-Ho Kang, Email: jinho2.kang@samsung.com.
Eun Sun Cheong, Email: eunsun.cheong@samsung.com.
Jang-Young Kim, Email: kimjy@yonsei.ac.kr.
Jeong Bae Park, Email: mdparkjb@gmail.com.
Ki-Chul Sung, Phone: 82 2 2001 2001, Email: kcmd.sung@samsung.com.
References
- 1.Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed Tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a Report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the society of atherosclerosis imaging and prevention and the society of cardiovascular computed tomography. J Am Coll Cardiol. 2007;49(3):378–402. doi: 10.1016/j.jacc.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Margolis JR, Chen JT, Kong Y, Peter RH, Behar VS, Kisslo JA. The diagnostic and prognostic significance of coronary artery calcification. A report of 800 cases. Radiology. 1980;137(3):609–616. doi: 10.1148/radiology.137.3.7444045. [DOI] [PubMed] [Google Scholar]
- 3.Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49(18):1860–1870. doi: 10.1016/j.jacc.2006.10.079. [DOI] [PubMed] [Google Scholar]
- 4.Raggi P, Gongora MC, Gopal A, Callister TQ, Budoff M, Shaw LJ. Coronary artery calcium to predict all-cause mortality in elderly men and women. J Am Coll Cardiol. 2008;52(1):17–23. doi: 10.1016/j.jacc.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Raggi P, Shaw LJ, Berman DS, Callister TQ. Prognostic value of coronary artery calcium screening in subjects with and without diabetes. J Am Coll Cardiol. 2004;43(9):1663–1669. doi: 10.1016/j.jacc.2003.09.068. [DOI] [PubMed] [Google Scholar]
- 6.Shaw LJ, Giambrone AE, Blaha MJ, Knapper JT, Berman DS, Bellam N, et al. Long-Term prognosis after coronary artery calcification testing in asymptomatic patients a cohort study long-term prognosis after cac testing in asymptomatic patients. Ann Intern Med. 2015;163(1):14–21. doi: 10.7326/M14-0612. [DOI] [PubMed] [Google Scholar]
- 7.Rumberger JA. Tomographic plaque imaging with CT: technical considerations and capabilities. Prog Cardiovasc Dis. 2003;46(2):123–134. doi: 10.1016/S0033-0620(03)00082-3. [DOI] [PubMed] [Google Scholar]
- 8.O’Rourke RA, Brundage BH, Froelicher VF, Greenland P, Grundy SM, Hachamovitch R, et al. American College of Cardiology/American Heart Association Expert Consensus document on electron-beam computed tomography for the diagnosis and prognosis of coronary artery disease. Circulation. 2000;102(1):126–140. doi: 10.1161/01.CIR.102.1.126. [DOI] [PubMed] [Google Scholar]
- 9.Haberl R, Becker A, Leber A, Knez A, Becker C, Lang C, et al. Correlation of coronary calcification and angiographically documented stenoses in patients with suspected coronary artery disease: results of 1764 patients. J Am Coll Cardiol. 2001;37(2):451–457. doi: 10.1016/S0735-1097(00)01119-0. [DOI] [PubMed] [Google Scholar]
- 10.Budoff MJ, Young R, Lopez VA, Kronmal RA, Nasir K, Blumenthal RS, et al. Progression of coronary calcium and incident coronary heart disease events: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2013;61(12):1231–1239. doi: 10.1016/j.jacc.2012.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Budoff MJ, Hokanson JE, Nasir K, Shaw LJ, Kinney GL, Chow D, et al. Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovasc Imaging. 2010;3(12):1229–1236. doi: 10.1016/j.jcmg.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 12.Wong ND, Nelson JC, Granston T, Bertoni AG, Blumenthal RS, Carr JJ, et al. Metabolic syndrome, diabetes, and incidence and progression of coronary calcium: the Multiethnic Study of Atherosclerosis study. JACC Cardiovasc Imaging. 2012;5(4):358–366. doi: 10.1016/j.jcmg.2011.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55(13):1318–1327. doi: 10.1016/j.jacc.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 14.Oberoi S, Schoepf UJ, Meyer M, Henzler T, Rowe GW, Costello P, et al. Progression of arterial stiffness and coronary atherosclerosis: longitudinal evaluation by cardiac CT. AJR Am J Roentgenol. 2013;200(4):798–804. doi: 10.2214/AJR.12.8653. [DOI] [PubMed] [Google Scholar]
- 15.Sugawara J, Hayashi K, Yokoi T, Cortez-Cooper MY, DeVan AE, Anton MA, et al. Brachial-ankle pulse wave velocity: an index of central arterial stiffness? J Hum Hypertens. 2005;19(5):401–406. doi: 10.1038/sj.jhh.1001838. [DOI] [PubMed] [Google Scholar]
- 16.Cainzos-Achirica M, Rampal S, Chang Y, Ryu S, Zhang Y, Zhao D, et al. Brachial-ankle pulse wave velocity is associated with coronary calcium in young and middle-aged asymptomatic adults: the Kangbuk Samsung Health Study. Atherosclerosis. 2015;241(2):350–356. doi: 10.1016/j.atherosclerosis.2015.05.031. [DOI] [PubMed] [Google Scholar]
- 17.Liu CS, Li CI, Shih CM, Lin WY, Lin CH, Lai SW, et al. Arterial stiffness measured as pulse wave velocity is highly correlated with coronary atherosclerosis in asymptomatic patients. J Atheroscler Thromb. 2011;18(8):652–658. doi: 10.5551/jat.7021. [DOI] [PubMed] [Google Scholar]
- 18.Seo WW, Chang HJ, Cho I, Yoon YY, Suh JW, Kim KI, et al. The value of brachial-ankle pulse wave velocity as a predictor of coronary artery disease in high-risk patients. Korean Circ J. 2010;40(5):224–229. doi: 10.4070/kcj.2010.40.5.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, et al. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res. 2002;25(3):359–364. doi: 10.1291/hypres.25.359. [DOI] [PubMed] [Google Scholar]
- 20.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–832. doi: 10.1016/0735-1097(90)90282-T. [DOI] [PubMed] [Google Scholar]
- 21.Sung KC, Lim YH, Park S, Kang SM, Park JB, Kim BJ, et al. Arterial stiffness, fatty liver and the presence of coronary artery calcium in a large population cohort. Cardiovasc Diabetol. 2013;12:162. doi: 10.1186/1475-2840-12-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park JS, Choi UJ, Lim HS, Choi BJ, Choi SY, Yoon MH, et al. The Relationship between coronary artery calcification as assessed by multi-detector computed tomography and arterial stiffness. Clin Exp Hypertens. 2011;33(8):501–505. doi: 10.3109/10641963.2011.601376. [DOI] [PubMed] [Google Scholar]
- 23.Kronmal RA, McClelland RL, Detrano R, Shea S, Lima JA, Cushman M, et al. Risk factors for the progression of coronary artery calcification in asymptomatic subjects: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2007;115(21):2722–2730. doi: 10.1161/CIRCULATIONAHA.106.674143. [DOI] [PubMed] [Google Scholar]
- 24.DeFilippis AP, Kramer HJ, Katz R, Wong ND, Bertoni AG, Carr J, et al. Association between coronary artery calcification progression and microalbuminuria: the MESA study. JACC Cardiovasc Imaging. 2010;3(6):595–604. doi: 10.1016/j.jcmg.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huynh K. Coronary artery disease: predicting the progression of coronary artery calcification. Nat Rev Cardiol. 2014;11(10):557. doi: 10.1038/nrcardio.2014.117. [DOI] [PubMed] [Google Scholar]
- 26.Pandey AK, Blaha MJ, Sharma K, Rivera J, Budoff MJ, Blankstein R, et al. Family history of coronary heart disease and the incidence and progression of coronary artery calcification: multi-Ethnic Study of Atherosclerosis (MESA) Atherosclerosis. 2014;232(2):369–376. doi: 10.1016/j.atherosclerosis.2013.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Erbel R, Lehmann N, Churzidse S, Rauwolf M, Mahabadi AA, Mohlenkamp S, et al. Progression of coronary artery calcification seems to be inevitable, but predictable—results of the Heinz Nixdorf Recall (HNR) study. Eur Heart J. 2014;35(42):2960–2971. doi: 10.1093/eurheartj/ehu288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McEvoy JW, Blaha MJ, Defilippis AP, Budoff MJ, Nasir K, Blumenthal RS, et al. Coronary artery calcium progression: an important clinical measurement? A review of published reports. J Am Coll Cardiol. 2010;56(20):1613–1622. doi: 10.1016/j.jacc.2010.06.038. [DOI] [PubMed] [Google Scholar]
- 29.Torii S, Arima H, Ohkubo T, Fujiyoshi A, Kadota A, Takashima N, et al. Association between pulse wave velocity and coronary artery calcification in Japanese men. J Atheroscler Thromb 2015. doi:10.5551/jat.30247. [DOI] [PubMed]
- 30.Papanas N, Tziakas D, Maltezos E, Kekes A, Hatzinikolaou E, Parcharidis G, et al. Peripheral arterial occlusive disease as a predictor of the extent of coronary atherosclerosis in patients with coronary artery disease with and without diabetes mellitus. J Int Med Res. 2004;32(4):422–428. doi: 10.1177/147323000403200412. [DOI] [PubMed] [Google Scholar]
- 31.Won KB, Chang HJ, Kim HC, Jeon K, Lee H, Shin S, et al. Differential impact of metabolic syndrome on subclinical atherosclerosis according to the presence of diabetes. Cardiovasc Diabetol. 2013;12:41. doi: 10.1186/1475-2840-12-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cox AJ, Hsu FC, Agarwal S, Freedman BI, Herrington DM, Carr JJ, et al. Prediction of mortality using a multi-bed vascular calcification score in the Diabetes Heart Study. Cardiovasc Diabetol. 2014;13:160. doi: 10.1186/s12933-014-0160-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shemesh J, Tenenbaum A, Fisman EZ, Koren-Morag N, Grossman E. Coronary calcium in patients with and without diabetes: first manifestation of acute or chronic coronary events is characterized by different calcification patterns. Cardiovasc Diabetol. 2013;12:161. doi: 10.1186/1475-2840-12-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Katakami N, Osonoi T, Takahara M, Saitou M, Matsuoka TA, Yamasaki Y, et al. Clinical utility of brachial-ankle pulse wave velocity in the prediction of cardiovascular events in diabetic patients. Cardiovasc Diabetol. 2014;13:128. doi: 10.1186/s12933-014-0128-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Iino R, Yokoyama N, Konno K, Naito K, Isshiki T. Impact of combined assessment of coronary artery calcium score, carotid artery plaque score, and brachial-ankle pulse wave velocity for early coronary revascularization in patients with suspected coronary artery disease. Int Heart J. 2012;53(3):154–159. doi: 10.1536/ihj.53.154. [DOI] [PubMed] [Google Scholar]
- 36.Franklin SS, Wt Gustin, Wong ND, Larson MG, Weber MA, Kannel WB, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997;96(1):308–315. doi: 10.1161/01.CIR.96.1.308. [DOI] [PubMed] [Google Scholar]
- 37.Messerli F, Ventura H, Glade L, Sundgaard-Riise K, Dunn F, Frohlich E. essential hypertension in the elderly: haemodynamics, intravascular volume, plasma renin activity and circulating catecholamine levels. Lancet. 1983;322(8357):983–986. doi: 10.1016/S0140-6736(83)90977-7. [DOI] [PubMed] [Google Scholar]
- 38.Min JK, Lin FY, Gidseg DS, Weinsaft JW, Berman DS, Shaw LJ, et al. Determinants of coronary calcium conversion among patients with a normal coronary calcium scan: what is the “warranty period” for remaining normal? J Am Coll Cardiol. 2010;55(11):1110–1117. doi: 10.1016/j.jacc.2009.08.088. [DOI] [PubMed] [Google Scholar]
- 39.Tsuchikura S, Shoji T, Kimoto E, Shinohara K, Hatsuda S, Koyama H, et al. Brachial-ankle pulse wave velocity as an index of central arterial stiffness. J Atheroscler Thromb. 2010;17(6):658–665. doi: 10.5551/jat.3616. [DOI] [PubMed] [Google Scholar]


