Abstract
Background and aim
Irritable bowel syndrome (IBS) has been associated with high prevalence of psychological and psychiatric disorders. However, the association between IBS and each of its subtypes (diarrhea IBS-D, constipation IBS-C, mixed IBS-M) with anxiety still remains unclear. The purpose of this study was to perform a comparative analysis of the association between anxiety and IBS on a period of ten years.
Methods
PubMed was searched for studies analyzing IBS and anxiety, published at 10 years interval. The study presents a comparative analysis of the articles that were published between 2003–2005 and 2013–2015, investigating the correlation between anxiety and IBS.
Results
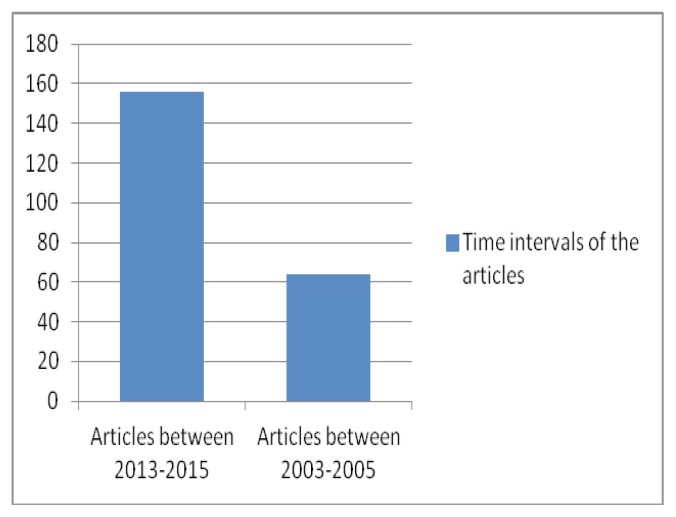
The initial search identified 220 articles, from which 156 were published between 2013 and 2015, and 64 were published between 2003 and 2005. Of these articles, 15 articles were included in the review. Out of these 15 articles, 10 articles analyzed the correlation between anxiety-depression status in IBS patients using specific questionnaires, 2 articles analyzed genetic variables in IBS, 1 article analyzed serotonin and monoamine oxidase levels in IBS, 1 article analyzed serum levels of IL-1β and IL-10 in IBS, 1 article analyzed somatostatin and vasoactive intestinal peptide levels in IBS. The result was a review of 15 studies that analyzed the association between IBS and anxiety.
Conclusions
IBS is a heterogeneous disorder caused by numerous psychological, immunological, infectious, endocrine and genetic factors. In recent years, the number of studies concentrating on genetic factors, cytokines and hormones has increased in comparison with the 2003–2005 period, when clinical investigation, using mainly questionnaires was the essential method. Also, the total number of papers investigating anxiety and IBS, considerably increased. The recent studies have confirmed the fact that IBS symptoms are often exacerbated during stressful events and the psychiatric treatment has a positive effect on gastro-intestinal symptomatology.
Keywords: anxiety, irritable bowel syndrome
Introduction
Irritable bowel syndrome (IBS) is a functional disorder which affects about 20% of the population and is the result of an interaction between genetic predisposition and environmental factors. According to the Rome III criteria, the syndrome is defined as recurrent abdominal pain or discomfort for at least 3 days per month, during the previous 3 months, associated with two or more of the following symptoms: improvement with defecation, onset associated with a change in the frequency of stool and/or onset associated with a change in form or appearance of stool. IBS can be classified as diarrhea-predominant (IBS-D), constipation-predominant (IBS-C), alternating stool pattern (IBS-A) or IBS-M (mixed diarrhea and constipation) [1].
Anxiety is defined as the response to prolonged, unpredictable threat, a response which encompasses physiological, affective, and cognitive changes. According to this definition, anxiety is distinct from fear: a response to acute predictable threats. The DSM-IV definitions of anxiety disorders, prominently feature “difficulty concentrating” as a key symptom. DSM-IV defines a number of different anxiety disorders including generalized anxiety disorder (GAD), phobias, panic disorder, post-traumatic stress disorder (PTSD), and obsessive–compulsive disorder (OCD). Because the rates of co-occurrence with depression are very high, rarely a patient who suffers a “pure” anxiety disorder is found [2].
Comorbidity between IBS and anxiety disorders is high. Moreover, anxiety and depression contribute to inefficient therapies in IBS. IBS symptoms are often exacerbated during periods of stressful events. Numerous investigations have reported comorbidity between IBS and stress-related psychiatric disorders as high as 30–50% [3]. The aim of this study was to carry out a comparative analysis of selected genetic, immunological, endocrine and psychopathological variables in patients with anxiety and IBS.
Methods
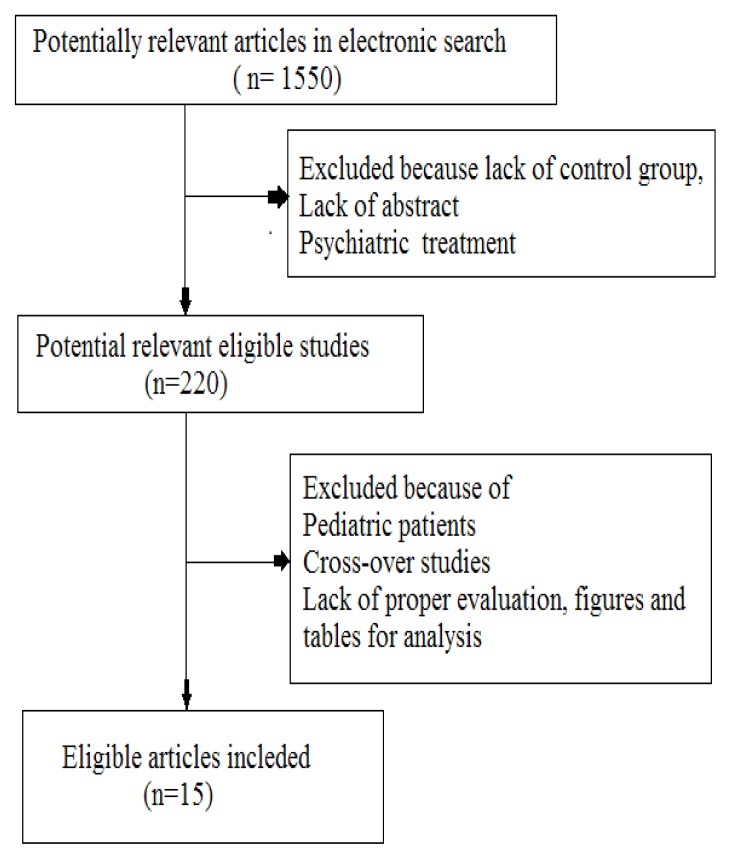
PubMed was searched for studies analyzing the association between IBS and anxiety, published at 10 years interval. The study presents a comparative analysis of the articles that were published between 2003–2005 and 2013–2015, investigating the correlation between anxiety and IBS. Search keywords were: anxiety, etiology, irritable bowel syndrome. The inclusion criteria were: full papers that included patients with anxiety, depression and IBS, concentrating on psychological, immunological, endocrine factors in IBS patients. Exclusion criteria were: reviews, absence of abstract, absence of control group, pediatric patients, lack of proper evaluation, figures and tables, psychiatric treatment.
Results
The result was a review of 15 studies that analyzed the association between IBS and anxiety. The initial search identified 220 articles, from which 156 were published between 2013 and 2015, and 64 were published between 2003 and 2005. Of these articles, 15 articles were included in the review. Out of these 15 articles, 10 articles analyzed the correlation between anxiety-depression status in IBS patients using specific questionnaires, 2 articles analyzed genetic variables in IBS, 1 article analyzed serotonin and monoamine oxidase levels in IBS, 1 article analyzed serum levels of IL-1β and IL-10 in IBS, 1 article analyzed somatostatin and vasoactive intestinal peptide levels in IBS.
2003–2005
Beginning with the fact that patients with IBS have a positive response to psychiatric medication, and also the presence of family history of anxiety and depression led to speculations about the inclusion of this syndrome in the affective spectrum disorder [4].
A clinical study that included 40 IBS patients from clinics of a university hospital and state hospital, 32 controls with inflammatory bowel disease and 34 healthy hospital showed that the prevalence of psychiatric disorders and mood disorders was higher in the IBS group. The interviews were done using SCID-NP (Structured Clinical Interview for DSM-Non-patients) and psychological factors were obtained by the SCL-90-R (Symptom Checklist-90-Revised), the Beck Depression Inventory, the Beck Anxiety Scale and the Hamilton Rating Scale for Depression, family histories were obtained by FH-RDC (Family History Research Diagnostic Criteria). The IBS group rated higher on anxiety and depression scales, and also presence of positive family history for psychiatric disorders was higher in the IBS group [5].
Because IBS has a psychogenic component in its physiopathology, the role of serotonin (5-hydroxytryptamine; 5-HT) and monoamine oxidase (MAO) was studied, in an effort of clarify the correlation between IBS-D and anxiety. The healthy control group was represented by 20 subjects (aged 18–25 years; all men), the IBS-D group included 57 patients with diarrhea-predominant IBS (30–60 years; all men). The concentrations of 5-HT and MAO, the anxiety level score were significantly higher (p<0.001) in study patients than in healthy volunteers, proving the role of serotonin in the physiopathology of IBS [6].
University training has been properly documented, as a time of anxiety, depression and high stress, especially in the examination period. A study on students analyzed the relationships between the presence of irritable bowel syndrome (IBS) and generalized anxiety disorder (GAD), chronic worry, neuroticism, anxiety sensitivity and anxiety about visceral sensations. The data was obtained using the Penn State Worry Questionnaire (PSWQ), the Neuroticism subscale of the Eysenck Personality Questionnaire, the Anxiety Sensitivity Index (ASI) and five additional items designed to measure visceral anxiety. IBS was correlated with a higher frequency of anxiety, GAD and greater worry, neuroticism and visceral anxiety. Moreover, logistic regression analyses showed that the measure of anxiety specific to visceral sensations was the strongest predictor of IBS diagnostic [7].
Traditionally IBS has no serious consequences. However, because of the relation with anxiety and depression, a study that compared one hundred follow-up, tertiary care IBS (tIBS) patients, with 100 secondary IBS (sIBS), 100 primary IBS (pIBS) care patients, and 100 patients with active inflammatory bowel disease (IBD) evidenced that 38% of tIBS patients had contemplated suicide because of their symptoms compared with 16% and 4% in the sIBS and pIBS groups (tIBS vs. sIBS vs. pIBS, P= .002, P< .001). Five tIBS and 1 IBD patient had attempted suicide for reasons related with gastrointestinal symptoms. Hopelessness because of symptom severity, interference with professional life, and inefficient treatment were emphasized as main issues for IBS patients [8].
2013–2015
Using the Symptom Checklist-90-Revised(SCL-90-R), as an instrument for the assessment of psychological distress, patients with IBS were evaluated; 163 controls and 153 patients that met the Rome III criteria were analyzed. Univariate (t-test and Chi-square) and multivariate (logistic regression) methods were used. A significant association of IBS with three global indices including global severity index (GSI), positive symptom distress index (PSDI), and positive symptom total (PST) of the SCL-90-R were present.
Patients with IBS reported significantly higher levels of anxiety, poor appetite, trouble falling asleep, thoughts of death or dying, disturbed sleep, and feelings of guilt compared to the controls. The analysis indicated that anxiety, somatization, paranoid ideation, depression subscales, and PST, PSDI, and GSI global indices were significantly associated with IBS [9].
Furthermore, the relation between anxiety status and cytokines was investigated in patients with IBS-D. Patients with IBS-D were divided into an anxiety-depression IBS-D group and a non anxiety-depression IBS-D group. Patients with IBS and anxiety were included in the control group. The self-rating anxiety scale (SAS) and self-rating depression scale (SDS) were used for scoring. The serum levels of IL-1β and IL-10 but also from colon mucosa were detected. Finally, it was demonstrated that the scores for anxiety and depression were significantly higher than in the control group(P<0.05). Moreover, the levels of cytokines in the blood and sigmoid colon mucosa in the IBS-D group were also significantly higher than in the control group (P<0.05). The results prove that the imbalance of the proinflammatory and anti-inflammatory cytokines leads to the onset or aggravation of IBS [10].
A clinical based study using Hamilton Anxiety rating scale and Hamilton Depression rating scale respectively, evidenced the prevalence of anxiety and depression in IBS patients recruited from a gastroenterology clinic in Mumbai, India. Prevalence rates of anxiety and depression were established and Odds Ratio (OR) were calculated to determine the correlation between depression and anxiety disorders with IBS. In patients with IBS the OR for depression was 6.3 (95% CI 1.6–24.74, P=0.009) and the OR for anxiety disorder was 7.56 (95% CI 1.53–37.29, P=0.01). The result was that the prevalence of depression and anxiety disorder in IBS is very high.[11]. Another clinical based study in a Gastroenterology Clinic of Taleghani Hospital, Tehran province, Iran, designed as cross-sectional study, analyzed anxiety in IBS patients. The most frequent psychiatric symptoms were reported by the constipation-predominant IBS (IBS-C) patients and the least rate was seen in IBS-D. There was a significant difference regarding the mean age of diarrhea-predominant IBS (IBS-D) patients with history of psychiatric symptoms (26.8 years) and without such history (37.9 years)(p<0.05) [12].
The nerve-endocrine network connecting the gastrointestinal tract and the central nervous system is known as the brain-gut axis, the brain-gut interaction is represented by the transmission of gastrointestinal tract activity information to the central nervous system, and the regulation of gastrointestinal tract activity by the central nervous system [13].
In recent years, the way that the neuro-endocrine network is influenced by psychological disorders was studied, especially the interaction of gastrointestinal hormones. The correlation between anxiety and IBS was analyzed using serum concentrations of somatostatin (SS) and vasoactive intestinal peptide (VIP). The hormones were measured by immunohistochemistry and radioimmunoassay methods. Patients with IBS were divided into IBS with normal emotional state ratings and IBS with anxiety states groups. The two groups were then subdivided into (IBS-C) and (IBS-D) groups. Non-IBS patients with normal anxiety ratings were recruited as controls. The anxiety-depression scores of patients with IBS were significantly different from those of the control group (P<0.05), and the expression levels of SS and VIP in the serum and colonic mucosa of the patients with IBS were higher compared with those of the control group. Moreover, the level of SS in the IBS-C group was increased compared with the IBS-D group (P<0.05). The results lead to the conclusion that anxiety states increase the secretion of SS and VIP, and subsequently lead to changes in gastrointestinal motility and function [14].
In order to understand the role of genetic factors but also the environment, the analysis of a population-based twin cohort using the Norwegian national birth registry, showed that low birth weight increased the risk for development of IBS, with environmental influences in utero as the most relevant contributing factor to the co-occurrence between anxiety and IBS [15].
Discussion
The present review identified articles, most of them prospective clinical studies, on the relation between anxiety and IBS during natural evolution or after therapy. Most studies are represented by clinical investigations using questionnaires as the Penn State Worry Questionnaire (PSWQ), the Neuroticism subscale of the Eysenck Personality Questionnaire, the Anxiety Sensitivity Index (ASI) in the effort of correlating anxiety with IBS. The conclusion was that approximately half of IBS patients reported anxiety and/or depression and the IBS-D patients with history of psychiatric symptoms reached the disease in early ages. Other frequent complaints were linked with poor appetite, thoughts of death or dying, trouble falling asleep, disturbed sleep, and feelings of guilt. These data recommend that detection and treatment of psychiatric disorders related to IBS is essential. Differential diagnosis between somatic illness and anxiety disorder is hard and requires long term cooperation between the internal medicine specialist, gastroenterologist and the psychiatrist. The investigation of IBS is intractable because somatic symptoms and psychological status interact and promote one other, resulting that somatic symptoms aggravate the patients’ psychological load, leading to the aggravation of anxiety.
In the recent years consistent attempts have been made to establishthe relation between cytokines, hormones, genetic polymorphism and brain-gut axis dysfunction, functional gastro-intestinal disorders and IBS. Because immunohistochemistry and radioimmunoassay techniques were used, the results revealed a precise correlation between the clinical background and immunological status.
Mental stress may lead to basic immune dysfunction. IL-1β is one of the most important pro-inflammatory factors, which cause an inflammatory reaction and breaks down the integrity of the mucosal barrier and also stops the absorption sodium, resulting in the occurence of diarrhea. The imbalance of the proinflammatory and anti-inflammatory cytokines (IL-1β and IL-10) leads to the onset or aggravation of IBS, if the anxiety-depression status is present. Moreover, the increased secretion of SS and VIP subsequently lead to changes in gastrointestinal motility and function. The genetic susceptibility of certain IBS patients to inflammation can be the effect of insufficient secretion of the inflammation-suppressing factor IL-10. Because pro-inflammatory factors may induce mental disorders and mental disorders interact with the immunological status, functional gastro-intestinal disorders are a difficult topic of study. Study limitations were represented by the low number of patients involved in each study. A reason for excluding articles was the association of other disorders with IBS and the insufficient comparative studies on a particular cytokines or other specific molecules involved in the physiopathology of IBS. A limitation of those studies is represented by the lack of accurate drug history. Consequently constipation may occur as a result of anticholinergic properties of psychotropic drugs.
Conclusions
IBS is a heterogeneous disorder caused by numerous psychological, immunological, infectious, endocrine and genetic factors. In recent years, the number of studies concentrating on genetic factors, cytokines, hormones increased, in comparison with the 2003–2005 period, when clinical investigation, using mainly questionnaires was the essential method. Also the total number of papers investigating anxiety and IBS, considerably increased.
The recent studies confirmed the fact that IBS symptoms are often exacerbated during stressful events and the psychiatric treatment has a positive effect on gastro-intestinal symptomatology. The present data add novel information showing that distinctive interleukins, IL receptors, neuro-endocrine factors and genetic background are directly involved in IBS physiopathology. Presence of low grade inflammation, combined with altered intestinal permeability, may lead to malfunctions of the adaptative neuro-imunological response, as a result of longstanding effects of depression-anxiety status.
One step further was the major focus of attention on the characterization of protein-coding genes and the correlation with clinical manifestations.
Further investigations into the etiology and pathogenesis of IBS are required, in order to improve the diagnosis and treatment of IBS.
Figure 1.
Flow diagram for study selection.
Figure 2.
Time intervals for the selected articles.
Acknowledgement
This paper was presented and published under the frame of European Social Fund, Human Resources Development Operational Programme 2007–2013, project no. POSDRU/159/1.5/S/138776.
References
- 1.Spiegel BM, Farid M, Esrailian E, Talley J, Chang L. Is irritable bowel syndrome a diagnosis of exclusion?: a survey of primary care providers, gastroenterologists, and IBS experts. Am J Gastroenterol. 2010;105(4):848–858. doi: 10.1038/ajg.2010.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gerson CD, Gerson MJ, Chang L, Corazziari ES, Dumitrascu D, Ghoshal UC, et al. A cross-cultural investigation of attachment style, catastrophizing, negative pain beliefs, and symptom severity in irritable bowel syndrome. Neurogastroenterol Motil. 2015;27(4):490–500. doi: 10.1111/nmo.12518. [DOI] [PubMed] [Google Scholar]
- 3.Vandvik PO, Lydersen S, Farup PG. Prevalence, comorbidity and impact of irritable bowel syndrome in Norway. Scand J Gastroenterol. 2006;41(6):650–656. doi: 10.1080/00365520500442542. [DOI] [PubMed] [Google Scholar]
- 4.Folks DG. The interface of psychiatry and irritable bowel syndrome. Curr Psychiatry Rep. 2004;6(3):210–215. doi: 10.1007/s11920-004-0066-0. [DOI] [PubMed] [Google Scholar]
- 5.Solmaz M, Kavuk I, Sayar K. Psychological factors in the irritable bowel syndrome. Eur J Med Res. 2003;8(12):549–556. [PubMed] [Google Scholar]
- 6.Singh R, Pandey H, Singh R. Correlation of serotonin and monoamine oxidase levels with anxiety level in diarrhea-predominant irritable bowel syndrome. Indian J Gastroenterol. 2003;22(3):88–90. [PubMed] [Google Scholar]
- 7.Hazlett-Stevens H, Craske MG, Mayer EA, Chang L, Naliboff BD. Prevalence of irritable bowel syndrome among university students: the roles of worry, neuroticism, anxiety sensitivity and visceral anxiety. J Psychosom Res. 2003;55(6):501–505. doi: 10.1016/s0022-3999(03)00019-9. [DOI] [PubMed] [Google Scholar]
- 8.Miller V, Hopkins L, Whorwell PJ. Suicidal ideation in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2004;2(12):1064–1068. doi: 10.1016/s1542-3565(04)00545-2. [DOI] [PubMed] [Google Scholar]
- 9.Farbod F, Farzaneh N, Bijan M, Mehdi G, Nosratollah N. Psychological features in patients with and without irritable bowel syndrome: A case-control study using Symptom Checklist-90-Revised. Indian J Psychiatry. 2015;57(1):68–72. doi: 10.4103/0019-5545.148526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gao J. Correlation between anxiety-depression status and cytokines in diarrhea-predominant irritable bowel syndrome. Exp Ther Med. 2013;6(1):93–96. doi: 10.3892/etm.2013.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kabra N, Nadkarni A. Prevalence of depression and anxiety in irritable bowel syndrome: A clinic based study from India. Indian J Psychiatry. 2013;55(1):77–80. doi: 10.4103/0019-5545.105520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farzaneh N, Ghobakhlou M, Moghimi-Dehkordi B, Naderi N, Fadai F. Anxiety and depression in a sample of Iranian patients with irritable bowel syndrome. Iran J Psychiatry Behav Sci. 2013;7(1):30–36. [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao Y, Ke M, Wang Z, Wei J, Zhu L, Sun X, et al. Pathophysiplogical and psychosocial study in patients with functional vomiting. J Neurogastroenterol Motil. 2010;16:274–280. doi: 10.5056/jnm.2010.16.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han B. Correlation between gastrointestinal hormones and anxiety-depressive states in irritable bowel syndrome. Exp Ther Med. 2013;6(3):715–720. doi: 10.3892/etm.2013.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bengtson MB, Aamodt G, Vatn M, Harris J. Co-occurrence of IBS and symptoms of anxiety or depression, among Norwegian twins, is influenced by both heredity and intrauterine growth. BMC Gastroenterol. 2015;15:9. doi: 10.1186/s12876-015-0237-y. [DOI] [PMC free article] [PubMed] [Google Scholar]