Abstract
Several cases of acquired resistance in patients with activating epidermal growth factor receptor (EGFR) mutation have been reported. However, rare clinical cases exist of a transformation to small cell lung cancer (SCLC) following treatment with EGFR-tyrosine kinase inhibitors (TKIs). We report a case of non-small cell lung cancer (NSCLC) with L858R mutation at the time of diagnosis. After failure of EGFR-TKI therapy, we performed additional histopathologic examinations. We confirmed that the patient had a histological transformation from NSCLC to SCLC. We performed chemotherapy with etoposide and cisplatin against the SCLC and radiologic findings were improved.
Keywords: Drug resistance, epidermal growth factor receptor, small cell carcinoma, transformation
Introduction
In patients with non-small cell lung carcinoma (NSCLC) harboring active mutations of epidermal growth factor receptor (EGFR), there is a high rate of therapeutic response to EGFR-tyrosine kinase inhibitors (TKIs). Therefore, according to recent treatment guidelines, EGFR-TKIs are recommended for use as first line treatment. It is also well known that 90% of active mutations arise from exon 19 deletion and exon 21 L858R point mutation.1,2 Although there are good responses to the initial EGFR-TKI treatment, drug resistance is inevitable and occurs on average within a year.1,3 The emergence of a secondary mutation of T790M and activation of the bypass signal transduction pathway through the amplification of MET are mechanisms of acquired resistance. Epithelial-mesenchymal transition and morphological transformation to small cell lung carcinoma (SCLC) are also rare mechanisms.1
We report a case of histological transformation from NSCLC to SCLC following treatment with EGFR-TKI. We treated the SCLC with etoposide and cisplatin chemotherapy and found that radiologic findings improved.
Case description
A 73-year-old man presented after three weeks of exertional dyspnea and a week of chest pain (aggravation of the left pleuritic). The patient had also experienced a day of hoarseness. He had a 50 pack-year smoking history and was taking drugs for atrial fibrillation. In January 2013, the patient was incidentally diagnosed as stage IV lung adenocarcinoma accompanied by multiple brain and spine metastases. At the time, the patient had an L858R point mutation of EGFR exon 21 and was treated with gefitinib as first line therapy. However, approximately two months later the cancer had progressed and he received four cycles of chemotherapy with gemcitabine and cisplatin.
At the time of admission, the patient had stable vital signs and laboratory parameters were within normal limits. The levels of tumor markers, such as carcinoembryonic antigen (3.48 ng/mL) and progastrin releasing peptide (24.76 pg/mL), were within normal ranges. Chest X-ray revealed that the size of the mass in the left upper lobe had increased compared to one month before admission (Fig 1a, b). Computed tomography showed a 6.5-cm heterogeneously enhanced mass and bronchoscopic biopsy, which was performed before admission, showed that the mass was suggestive of SCLC (Figs 2, 3). In addition, we performed an EGFR mutation test using the same specimens, revealing that the patient had L858R point mutation, as shown at the time of diagnosis.
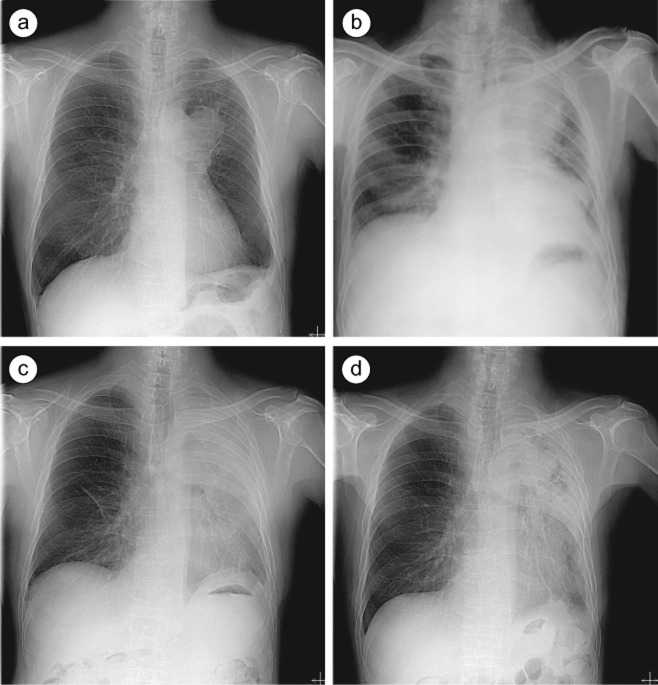
Figure 1.
Chest X-ray findings. (a) One month before admission, the patient had a 6 cm ovoid mass in the left upper lobe. (b) On admission, the left upper lobar mass increased and the patient developed obstructive pneumonia. (c) Immediately before chemotherapy, there is a marked aggravation of left lung haziness. (d) Two weeks after chemotherapy, the left upper lung fields are more aerated.
Figure 2.
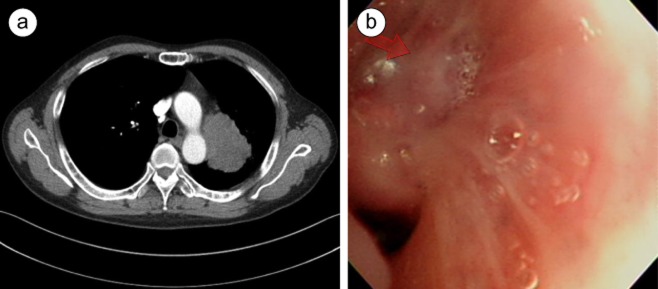
Chest computed tomography scan and bronchoscopy. (a) One month before admission, the patient had a 6.5 cm heterogeneously enhanced mass in the left upper lobe. (b) The patient had multiple polypoid nodular lesions (arrow), accompanied by total obstruction of the apical segment of the left upper lobe.
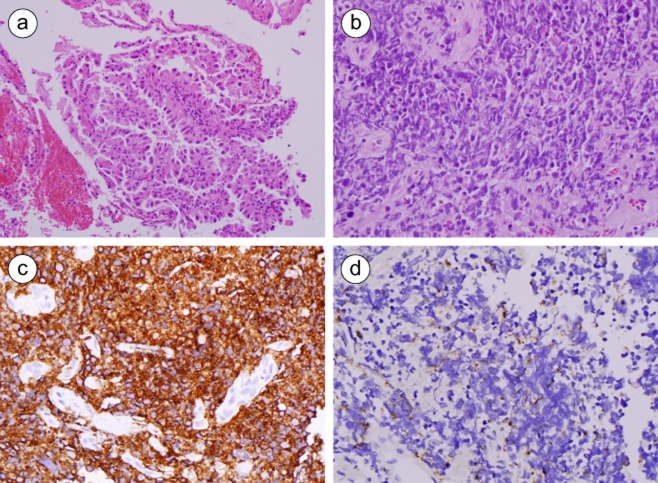
Figure 3.
Histopathologic findings. (a) On initial biopsy, the tumor was composed of atypical large cells with glandular differentiation; this is suggestive of adenocarcinoma (hematoxylin and eosin [H & E], ×200). (b) On subsequent biopsy after gefitinib therapy, the tumor was composed of hyperchromatic cells; this is suggestive of small cell lung carcinoma (H & E, ×400). (c) Immunohistochemical staining for CD56 showed a membranous staining pattern of the tumor cells (×400). (d) Immunohistochemical staining for CK7 showed the tumor cells in a dot-like pattern (×400).
The patient’s respiratory symptoms were aggravated as a result of the cancer progression and were accompanied by delirium, for which the he received conservative treatments. One week thereafter, he achieved an improvement in Eastern Cooperative Oncology Group (ECOG) performance status to 2. On plain chest radiography, however, the patient had an aggravated haziness in the left lung field (Fig 1c). Therefore, we performed chemotherapy with etoposide and carboplatin for the management of SCLC. Two weeks later, a follow-up X-ray showed that there was a slight improvement (Fig 1d). However, the patient presented with neutropenia and septic shock. With conservative treatments, such as antibiotics and granulocyte colony-stimulating factor, the patient recovered and was transferred to a hospice care clinic as per his wishes.
Discussion
Most cases of acquired resistance to EGFR-TKI arise from the emergence of T790M mutation or activation of the bypass signal transduction pathway.1 The current case is of significance in that we confirmed a resistance arising from the morphological transformation to SCLC by histopathologic examination and then attempted to treat it. According to a review of the literature, similar instances have been reported,4–6 with an acquired resistance arising from the histological transformation to SCLC accounting for up to 3% of total cases.7
In patients who have marked changes in clinical presentation after the failure of EGFR-TKIs, clinicians should consider the possibility of a histological transformation to SCLC. In the current case, we compared plain chest radiographic findings between the time point of tissue biopsy and that of hospitalization. These showed that the patient had rapid cancer progression, which is indicative of the prompt progression of SCLC. However, little is known about the exact mechanisms by which acquired resistance arises from the histological transformation to SCLC, for which two major hypotheses have been proposed. These include the alteration of morphological phenotype from NSCLC to SCLC and the predominant presence of SCLC following treatment with EGFR-TKI, although there was a combined presence of NSCLC and SCLC. In the current case, SCLC was confirmed by the second tissue biopsy. An EGFR mutation test using the same specimens confirmed an L858R mutation, as shown at the time of diagnosis. Therefore, it can be inferred that there is a high possibility that cancers of the same origin may undergo histological transformation. However, a small biopsy by bronchoscopy could not represent the entire tumor and moreover, only two months elapsed since the patient received gefitinib treatment. This indicates that we cannot completely rule out the possibility that the patient might initially have a mixed type of tumor or primary resistance to EGFR-TKI.
Currently, there are no established treatment guidelines for patients diagnosed with a histological transformation to SCLC. Experimental studies have been conducted to clarify the mechanisms of acquired resistance to EGFR-TKI using cell lines, showing that there are therapeutic responses to etoposide and cisplatin.8 To date, however, there are cases in which there was no response to chemotherapy against SCLC.5 In the current case, the patient had a radiologic improvement, however, clinicians should not overlook the possibility of complications. Further studies are therefore warranted to examine treatments for NSCLC in patients who have acquired resistance arising from a histological transformation to SCLC. Moreover, after the failure of EGFR-TKIs, an additional biopsy of the tumor should be performed where the acquired resistance occurred. This is essential for clarifying the mechanisms underlying acquired resistance and establishing treatment guidelines in relevant cases.
Disclosure
No authors report any conflict of interest.
References
- Lee JC, Jang SH, Lee KY, Kim YC. Treatment of non-small cell lung carcinoma after failure of epidermal growth factor receptor tyrosine kinase inhibitor. Cancer Res Treat. 2013;45:79–85. doi: 10.4143/crt.2013.45.2.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pao W, Miller VA. Epidermal growth factor receptor mutations, small-molecule kinase inhibitors, and non-small-cell lung cancer: current knowledge and future directions. J Clin Oncol. 2005;23:2556–2568. doi: 10.1200/JCO.2005.07.799. [DOI] [PubMed] [Google Scholar]
- Kobayashi S, Boggon TJ, Dayaram T, et al. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N Engl J Med. 2005;352:786–792. doi: 10.1056/NEJMoa044238. [DOI] [PubMed] [Google Scholar]
- Morinaga R, Okamoto I, Furuta K, et al. Sequential occurrence of non-small cell and small cell lung cancer with the same EGFR mutation. Lung Cancer. 2007;58:411–413. doi: 10.1016/j.lungcan.2007.05.014. [DOI] [PubMed] [Google Scholar]
- Watanabe S, Sone T, Matsui T, et al. Transformation to small-cell lung cancer following treatment with EGFR tyrosine kinase inhibitors in a patient with lung adenocarcinoma. Lung Cancer. 2013;82:370–372. doi: 10.1016/j.lungcan.2013.06.003. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Li XY, Tang Y, et al. Rapid increase of serum neuron specific enolase level and tachyphylaxis of EGFR-tyrosine kinase inhibitor indicate small cell lung cancer transformation from EGFR positive lung adenocarcinoma? Lung Cancer. 2013;81:302–305. doi: 10.1016/j.lungcan.2013.04.005. [DOI] [PubMed] [Google Scholar]
- Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res. 2013;19:2240–2247. doi: 10.1158/1078-0432.CCR-12-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Y, Kim SY, Choi YJ, et al. Neuroendocrine differentiation in acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitor. Tuberc Respir Dis. 2013;75:95–103. doi: 10.4046/trd.2013.75.3.95. [DOI] [PMC free article] [PubMed] [Google Scholar]