Abstract
Purpose
To examine the association of depressive symptoms with coronary heart disease (CHD) endpoints by race and income.
Methods
Study participants were Blacks and Whites (n=24,443) without CHD at baseline from the national REasons for Geographical and Racial Differences in Stroke (REGARDS) cohort. Outcomes included acute CHD and CHD or revascularization. We estimated race-stratified multivariable Cox proportional hazards models of incident CHD and incident CHD or revascularization with the 4-item Center for Epidemiological Studies-Depression scale, adjusting for risk factors.
Results
Mean follow-up was 4.2+1.5 years, CHD incidence was 8.3 events per 1000 person years (n=366) among Blacks and 8.8 events per 1000 person years (n=613) among Whites. After adjustment for age, sex, marital status, region, and socioeconomic status, depressive symptoms were significantly associated with incident CHD among Blacks [HR 1.39 (95%CI 1.00-1.91)], but not among Whites [HR 1.10 (95%CI 0.74-1.64)]. In the fully-adjusted model, compared to Blacks who reported no depressive symptoms, those reporting depressive symptoms had greater risk for the composite endpoint of CHD or revascularization [HR 1.36 (95%CI 1.01-1.81)]. Depressive symptoms were not associated with incident CHD endpoints among Whites.
Conclusions
High depressive symptoms were associated with higher risk of CHD or revascularization for Blacks but not Whites.
Keywords: coronary disease, epidemiology, depressive symptoms, myocardial infarction
Coronary heart disease (CHD) affects about 14 million men and women in the US.1,2 Although mortality from CHD has declined over the last few decades due to improved quality of care and primary prevention efforts,3 Blacks continue to have markedly higher risk for CHD mortality than Whites.2,4 This disparity is in part due to differences in risk factors such as hypertension, diabetes, chronic kidney disease and smoking, which are a greater burden among Blacks than Whites.5,6,7 Less clear is the role of non-traditional risk factors such as depressive symptoms, which also influence CHD incidence and mortality.8,9
Depressive symptoms is considered a non-traditional risk factor, in that it is usually not considered a primary predictor of CHD risk as are more traditional, clinical risk factors. Clinicians rarely screen their patients for depressive symptoms, which is often viewed as a modifiable risk factors for heart disease, and thus a non-traditional risk factor.10 Research has reported that the prevalence of self-report depressive symptoms is higher among non-Hispanic Blacks than non-Hispanic Whites in the general adult population,11-13 and that depressive symptoms is more severe among Blacks than Whites, though the lifetime prevalence of major depressive disorder is higher among Whites.14 In older adults there is no clear understanding of the existence of racial disparities in depressive symptoms. While some researchers have reported that older Whites have higher symptom levels than do Blacks,15 others have found little evidence that there is a disparity in depressive symptoms among older Blacks and Whites.16 Clearly, Black-White disparities in depressive symptoms is not as conclusive as evidence for disparities among young-to-middle-age Blacks and Whites.12
The majority of published reports have examined the associations of depressive symptoms and cardiovascular disease (CVD) endpoints (e.g., total mortality, incident ischemic heart disease and stroke) among Whites.4,9,17,18 Little is known about the association of depressive symptoms with incident CHD among Blacks,8 and results are mixed. One report concluded that depressive symptoms were more strongly associated with CVD risk among Blacks than Whites.9 Another study found that there are no racial differences in the association of depressive symptoms and CVD risk factors such as hypertension risk.19 Studies have reported a stronger association of depressive symptoms with CVD risk factors (hypertension, diabetes and subclinical disease) among Blacks than among Whites.20-24 Clearly, much of the work on Blacks has centered around the association between depressive symptoms and CVD risk factors. This demonstrates why the role of depressive symptoms in the etiology of CHD risk among Blacks and Whites is important.
High depressive symptoms among Blacks may stem from multiple sources, including earning low income, psychological stress, and living in residentially segregated neighborhoods that may limit access to quality mental health care, which also leads to less treatment of mental illness.14,25-27 These factors are more prevalent among Blacks than Whites and are critical to explaining the role depressive symptoms play in the race-CHD pathway. While findings have shown associations of depressive symptoms with CHD among both Blacks and Whites, the burden of depressive symptoms may be more severe among Blacks and low-income families since their depressive symptoms are not treated as often as those among Whites and high-income families.14,28
Depressive symptoms may also impact CHD through a number of possible pathways. Depressed persons more likely engage in unhealthy behaviors such as eating high fat diets, drink alcohol, become physically inactive and smoke, thereby increasing their risk for CHD.29,30 Other research suggest that depressive symptoms impact CHD through poor treatment adherence and more underlying disease severity.31 Depressive symptoms may also affect CHD incidence through neuroendocrine changes that trigger physiological responses involving the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic-parasympathetic systems, which play a central role in the pathophysiology of CHD.32,33 Other pathophysiological effects of negative emotional states that may contribute to atherogenesis include autonomic imbalance, serotonergic dysfunction, secretion of proinflammatory cytokines, and platelet activation.8,34-36 Another line of work proposes that the mechanism by which depressive symptoms contributes to CHD is due to treatment where anti-depressant medications may contribute to cardiotoxicity.37
Few studies have examined the association of depressive symptoms with incident CHD and revascularization (or coronary artery bypass surgery), and the extent to which that association is impacted by income in a large sample of Blacks and Whites. The objective of this study was to examine the association of depressive symptoms with incident acute CHD or coronary revascularization in the national REasons for Geographical and Racial Differences in Stroke (REGARDS) study. We hypothesized that depressive symptoms at baseline would be associated with incident CHD or revascularization for Blacks more so than for Whites, and that associations would vary by income.
Methods
Design and Procedures
REGARDS is a national population-based, cohort study of US community-dwelling adults aged >45 years recruited from January 2003 to October 2007 to determine the causes of racial and geographical differences in stroke mortality. REGARDS recruited 30,239 participants (42% Black and 55% women). Race was self-reported. Data for this study were collected by REGARDS-MI, an ancillary study of REGARDS that adjudicates all heart-related events and merges these data with the existing REGARDS data. Participants were recruited from a commercial list of US residents using mail and telephone contacts. Baseline data were collected on participants’ demographic characteristics, medical history, stroke symptom history, health behaviors, functional status and psychological measures using computer-assisted telephone interviews (CATI). In-home examinations were conducted by trained health care professionals utilizing standardized protocols to collect clinical measures (i.e., blood pressure, height and weight, waist circumference), blood and urine samples, electrocardiograms (ECGs), and medication use by pill bottle review. Blood and urine samples were centrally analyzed at the University of Vermont, and ECGs were read centrally at the Wake Forest University ECG reading center.
Participants or their proxies were followed up every 6 months by telephone interview with retrieval of medical records for reported hospitalizations. Deaths were detected by report of next of kin or through online sources (e.g., Social Security Death Index) and the National Death Index. Proxies or next of kin were interviewed about the circumstances surrounding death, including the presence of chest pain. Death certificates and autopsy reports also were obtained to adjudicate cause of death and cardiovascular outcomes were adjudicated using methods previously described.6 Myocardial infarctions (MIs) were classified as definite, probable or possible. Definite MIs were those with diagnostic cardiac enzymes or ECG. Probable MIs were those with elevated but not diagnostic (i.e., equivocal) enzymes with a positive but no diagnostic ECG; or, if enzymes were missing, with a positive ECG in the presence of ischemic signs or symptoms. Only definite or probable MIs were incorporated as events in this study. Cases were assigned to 2 adjudicators and disagreements were adjudicated by committee. The test for agreement between adjudicators produced a level greater than 0.80 for the presence of definite or probable MI or definite or probable acute CHD death.6 Further discussion of the methodological details and procedures are available elsewhere.38 This study excluded REGARDS participants with baseline CHD defined as a self-reported history of myocardial infarction, coronary artery bypass surgery, percutaneous coronary intervention, or evidence of myocardial infarction by ECG. REGARDS was approved by the Institutional Review Boards of all participating institutions and study participants provided informed consent.
Outcome Measures
The dependent variables included incident acute CHD and a composite endpoint consisting of incident acute CHD or coronary revascularization. Incident acute CHD was defined as a definite or probable MI or acute CHD death. Acute CHD death is a death that is judged to be due to myocardial infarction within the past 28 days, or sudden cardiac death, based on review of medical records, death certificates, interviews with proxies and autopsy reports, where available. Our definition was derived from following an American Heart Association position statement that provided guidance for the definition of acute CHD in epidemiologic and clinical studies.39 Coronary revascularization, the process of restoring the flow of blood to the heart, included percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). The follow-up time for each participant was calculated from the date of the in-home visit to the date of first acute CHD event, for the first endpoint, or the date of first revascularization/acute CHD event, for the second endpoint, or date of death or last follow-up date. Events through December 31, 2009 were included in this analysis. At that time, 9.5% of the original sample was lost to follow-up.
Main exposure variable
The primary independent variable was derived from the Center for Epidemiological Studies-Depression (CES-D)–4-item scale (version 17) to evaluate depressive symptoms. This measure was derived from the 20-item CES-D scale. Scores range from 0 to 12; a score ≥4 indicates an elevated level of psychologic distress.40 Scores were categorized as normal (<4) or depressed (≥4). The internal consistency of the 4-item scale was high in this sample (α=0.80) when compared to that of the 20-item scale measured across studies which ranges from 0.85 to 0.90.41
Other Covariates
Other covariates included demographic, socioeconomic status (SES), health behaviors, and physiological variables. Demographic characteristics included age (continuous variable), sex [male=1; female=0 (referent)], race [black=1; white=0 (referent)], marital status [single=0 (referent); divorced=1; widowed=2; other=3; married=4], and region of residence [stroke belt=1; stroke buckle=2; other=0 (referent)]. The “stroke belt” is a region of states in the southeast with stroke mortality rates 1.3-1.5 times greater than the rest of the US; the “stroke buckle” is a region of counties in North and South Carolina and Georgia with stroke mortality rates higher than the rest of the nation;42 and the “other” category includes states where stroke rates are lower than those found in the stroke belt or buckle. SES included educational attainment [<HS diploma=0 (referent); ≥HS diploma=1], annual family income [<$35,000/year=0 (referent); $35,000 or more/year=1], and residence in a census tract with poverty level of 30% or more [poverty level <30%=0 (referent); poverty level 30% or more=1].43 Health behaviors included physical activity [no exercise=0 (referent); any weekly exercise=1], smoking [none=0 (referent); current smoker=1] and alcohol consumption [past or never=0 (referent); current use=1]. Physiological variables included systolic blood pressure [SBP<120=0 (referent); 120-139=1; >140 mmHg=2], total cholesterol [<200=0 (referent); 200-239=1; >240 mg/dL=2], high density lipoprotein (HDL) cholesterol [men: <40=1; >40 mg/dL=0 (referent); women: <50=1; >50 mg/dL=0 (referent)], albuminuria [<30=0 (referent); 30-300=1; >300 mg/g=2], triglycerides [<150=0 (referent); >150 mg/dL=1], natural log-transformed high sensitivity C-reactive protein (hs-CRP) [<3=0 (referent); >3 mg/dL=1], diabetes status [defined as fasting blood sugar >126 mg/dL, a non-fasting blood sugar >200 mg/dL, a self-reported history of diabetes, or treatment with a diabetes medication (referent is not diabetic)], body mass index [BMI: < 25=0 (referent), 25-29.9=1, ≥ 30 kg/m2=2], use of statins or hydroxymethylglutaryl-coenzyme A (HMG CoA) reductase inhibitors [no=0 (referent); yes=1], use of anti-hypertensive medications [no=0 (referent); yes=1] and use of antidepressant medications [no=0 (referent); yes=1].
Statistical analysis
Longitudinal associations of depressive symptoms with incident acute CHD (acute CHD death, nonfatal MI, or coronary revascularization) by race were examined among participants free of CHD at baseline. Baseline characteristics of REGARDS participants were calculated for those who did not report elevated depressive symptoms (CES-D < 4) and those who did (CES-D ≥ 4). Associations of depressive symptoms with CHD endpoints were examined by estimating hazard ratios (HR, 95% Confidence Interval–CI) for the two endpoints (incident CHD and incident CHD or revascularization) in sequential Cox proportional hazards models. Model 1 adjusted for age, sex, marital status and geographic region of residence. Model 2 adjusted for variables in model 1 plus family income, educational attainment, US census tract level of poverty. Model 3 adjusted for model 2 covariates plus physical activity, smoking, and alcohol consumption. Model 4 adjusted for model 3 variables plus diabetes status, BMI, natural log-transformed hs-CRP, systolic blood pressure, total and HDL cholesterol, urinary albumin, triglycerides, use of statins, use of anti-hypertensive medications, and use of anti-depressants.
Because of our interest in racial differences in depressive symptoms and CHD endpoints,9 race-stratified multivariable analyses were conducted a priori. A test for interaction between race and depressive symptoms was calculated in fully-adjusted models to examine effect modification by race. The results of the significant p-values for interaction are presented in race-stratified models below. The Kaplan-Meier method was used to calculate the cumulative incidence of each endpoint by depressive symptoms (CES-D < 4 vs. CES-D ≥ 4) among Blacks and Whites. A test for interaction between income status (<$35,000 vs. ≥$35,000) and depressive symptoms status was also calculated to assess effect modification by income. This interaction was a significant threshold for psychosocial influences in a prior analysis.44 The results of the significant p-values for interaction are presented in income-stratified models below.
A total of 5,914 study participants were missing one or more covariates, with the highest number of missing data for income (n=3,016), hs-CRP (n=1,519) and urinary albumin (n=1,117). Therefore, multiple imputation of missing data by chained equations was conducted using 5 datasets. All statistical analyses were performed using SAS version 9.2 (SAS Institute, Inc. Cary, NC) and STATA version 12 (STATA Corp, College Station, TX).
Results
Sample Characteristics
Five hundred sixty nine participants were missing any follow up data and 182 participants were missing the CES-D scale; after excluding 5,227 participants with CHD at baseline, the study sample included 24,261 participants (Blacks = 10,265; Whites = 13,996). Depressive symptoms were more prevalent among Blacks (13.1%) than Whites (8.5%), p<0.001. Baseline characteristics by depressive symptoms among participants without CHD at baseline are presented in Table1. Participants who reported CES-D≥4 were more likely to be younger (mean age 62.5 years), female, Black, reside in the stroke belt, have less than a high school education, and earn income less than $35,000 than those who reported CES-D<4. A greater percentage of participants who reported higher depressive symptoms scores had BMI≥30, SBP≥140 mmHg, hsCRP ≥3 mg/dL (49.5%), and diabetes (26.7%) than those who reported normal scores. A greater percentage of those with elevated depressive symptoms reported smoking and fewer reported getting any exercise.
Table 1.
Baseline Characteristics by Depressive Symptoms among REGARDS Participants Without Coronary Heart Disease at Baseline (N=24,261)a
| CES-D < 4 (n =21,731) | CES-D ≥ 4 (n =2,530) | P-value | |
|---|---|---|---|
| Demographics: | n (%) | n (%) | |
| Age, years, M±SD | 64.3±9.3 | 62.5±9.7 | <.001 |
| Female | 12,330(56.7) | 1,848(73.0) | <.001 |
| Black | 8,923(41.0) | 1,342(53.0) | <.001 |
| Marital status | <.001 | ||
| Married | 13,185(60.7) | 988(39.1) | |
| Single | 1,151(5.3) | 204(8.1) | |
| Divorced | 3,189(14.7) | 524(20.7) | |
| Widowed | 3,754(17.3) | 705(27.9) | |
| Other | 452(2.1) | 109(4.3) | |
| Region of residence | <.001 | ||
| Non-belt | 9,789(45.1) | 984(38.9) | |
| Belt | 7,439(34.2) | 958(37.9) | |
| Buckle | 4,503(20.7) | 588(23.2) | |
| Socioeconomic status: | |||
| Education < HS | 2,245(10.3) | 570(22.6) | <.001 |
| Income < $35 ,000/yr | 8,415(44.1) | 1,507(69.7) | <.001 |
| Residence in a census tract with poverty level of 30% or more, |
2,793(14.2) | 484(21.4) | <.001 |
| Physiological Variables: | |||
| BMI (kg/m2): | <.001 | ||
| < 25 | 5,516(25.6) | 550(21.9) | |
| 25-29 | 8,020(37.2) | 815(32.5) | |
| ≥ 30 | 8,048(37.3) | 1,143(45.6) | |
| SBP (categories): | 0.003 | ||
| <120 mmHg | 6,869(31.7) | 779(30.9) | |
| 120-139 mmHg | 10,553(48.7) | 1,178(46.7) | |
| ≥140 mmHg | 4,251(19.6) | 567(22.5) | |
| Total cholesterol (categories): | 0.03 | ||
| <200 mg/dL | 12,013(57.6) | 1,318(54.9) | |
| 200-239 mg/dL | 6,322(30.3) | 767(32.0) | |
| ≥240 mg/dL | 2,510(12.0) | 316(13.2) | |
| Physiological Variables: | n (%) | n (%) | |
| HDL-cholesterol (<40 mg/dL in men or <50 mg/dL in women) |
7,114(34.3) | 899(37.7) | 0.001 |
| Urine Albumin to Creatinine Ratio, median [25th, 75th percentile], log-transformed |
1.95[1.50-2.66] | 2.03[1.57-2.84] | <.001 |
| Triglycerides (≥150 mg/dL) | 5,565(26.7) | 721(30.1) | 0.0005 |
| Highly sensitive C-reactive protein (≥3 mg/dL) |
8,003(39.3) | 1,165(49.5) | <.001 |
| Diabetes | 3,908(18.7) | 650(26.7) | <.001 |
| Current Medication use | |||
| Statins | 6,043(28.1) | 760(30.4) | 0.02 |
| Anti-hypertensives | 10,330(48.0) | 1,372(54.9) | <.001 |
| Health Behaviors: | |||
| Current smoker | 2,832(13.1) | 602(23.9) | <.001 |
| Exercise (any) | 14,525(67.9) | 1,369(54.9) | <.001 |
| Current Alcohol Use | 11,600(53.4) | 1,168(46.2) | <.001 |
Abbreviations: REGARDS - Reasons for Geographic And Racial Differences in Stroke Study, CES-D - Center for Epidemiological Studies-Depression, CHD - coronary heart disease, HS - high school, BMI - body mass index, SBP - systolic blood pressure, DBP - diastolic blood pressure HDL - high-density lipoprotein.
Baseline CHD is defined as history of self-reported myocardial infarction (MI), coronary artery bypass graft, angioplasty, stenting, or evidence of MI via electrocardiograph. Participants missing follow-up (n=513) or baseline CES-D (n=182) are excluded.
Incidence Rates
Overall mean follow-up was 4.2+1.5 years, CHD incidence was 8.3 events per 1000 person-years (n=366 events) among Blacks and 8.8 events per 1000 person-years (n=613 events) among Whites (p=0.0015). Table 2 present the associations of baseline depressive symptoms with incident acute CHD alone and the composite measure of incident acute CHD or revascularization stratified by race. Among Whites, depressive symptoms were not associated with incident acute CHD in any of the models. Among Blacks, the HR for incident acute CHD was 1.54 (95% CI 1.12-2.12) for participants who reported CES-D scores ≥ 4 compared to those who reported CES-D scores < 4 adjusting for age, sex, marital status and region (Model 1). After adjustment for SES, the HR for incident CHD attenuated but remained significant (HR, 1.39; 95% CI 1.00-1.91) (Model 2). After adjustment for the remaining covariates, the HR was attenuated further and no longer significant. Depressive symptoms were not associated with the composite measure acute CHD or revascularization in any of models for Whites. Among Blacks, however, after full adjustment, the HR for the composite outcome acute CHD or revascularization was 1.36 (95% CI 1.01-1.81) for participants who reported CES-D scores ≥ 4 compared to those who reported CES-D scores < 4. From Model 1 to Model 4, there was modest attenuation but the HR remained statistically significant.
Table 2.
Association of incident cardiac events with depressive symptoms at baseline by race among REGARDS participants free of CHD at baseline (N=24,261)a
| Nb | Eventsc | Model 1d HR (95% CI) |
Model 2e HR (95% CI) |
Model 3f HR (95% CI) |
Model 4g HR (95% CI) |
|
|---|---|---|---|---|---|---|
| Incident Acute Coronary Heart Disease - Whites | ||||||
| CES-D < 4(ref) | 12808 | 340 | 1.0 | 1.0 | 1.0 | 1.0 |
| CES-D≥4 | 1188 | 27 | 1.21 (0.81-1.81) | 1.10 (0.74-1.64) | 1.03 (0.69-1.54) | 0.99 (0.66-1.48) |
| Incident Acute Coronary Heart Disease - Blacks | ||||||
| CES-D < 4(ref) | 8923 | 242 | 1.0 | 1.0 | 1.0 | 1.0 |
| CES-D≥4 | 1342 | 46 | 1.54 (1.12-2.12) | 1.39 (1.00-1.91) | 1.32 (0.95-1.83) | 1.29 (0.93-1.79) |
| Incident Acute Coronary Heart Disease or Coronary Revascularization - Whites | ||||||
| CES-D < 4(ref) | 12808 | 575 | 1.0 | 1.0 | 1.0 | 1.0 |
| CES-D≥4 | 1188 | 38 | 1.11 (0.80-1.56) | 1.02 (0.73-1.42) | 0.96 (0.69-1.35) | 0.92 (0.66-1.29) |
| Incident Acute Coronary Heart Disease or Coronary Revascularization - Blacks | ||||||
| CES-D < 4(ref) | 8923 | 307 | 1.0 | 1.0 | 1.0 | 1.0 |
| CES-D≥4 | 1342 | 59 | 1.57 (1.18-2.09) | 1.43 (1.07-1.90) | 1.37 (1.03-1.83) | 1.36 (1.01-1.81) |
Abbreviations: REGARDS - Reasons for Geographic And Racial Differences in Stroke Study, CHD - coronary heart disease, HR – hazard ratio, CI – confidence interval, CES-D - Center for Epidemiological Studies-Depression, ref – referent.
Persons with baseline CHD excluded. 182 participants, missing baseline CES-D assessment are excluded. Multiple imputation for missing data in covariates, including “refused’ category in income and based on 5 models.
Average number across 5 imputation models
Average number of events across 5 imputation models
Model1 adjusts for age, gender, marital status, region.
Model2 adjusts for Model1+ education, income, residence in census tract with poverty level of 30% or more
Model3 adjusts for Model 2 + physical activity, smoking, alcohol consumption
Model4 adjusts for Model3 + diabetes, Body Mass Index, log transformed hsCRP, systolic blood pressure, total cholesterol, HDL, log transformed urinary albumin to creatinine ratio, triglycerides, use of anti-hypertensive medication, use of statins
Bolded p-values < 0.05.
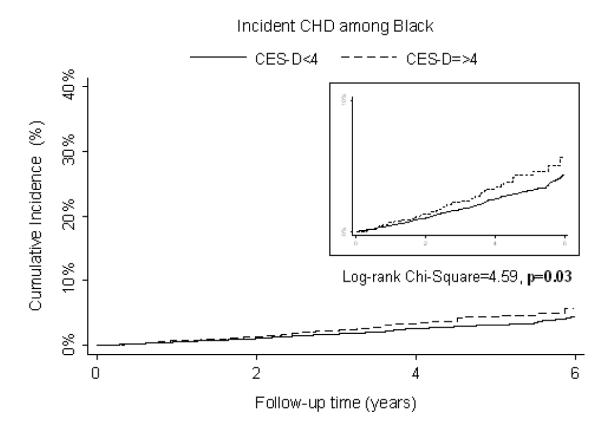
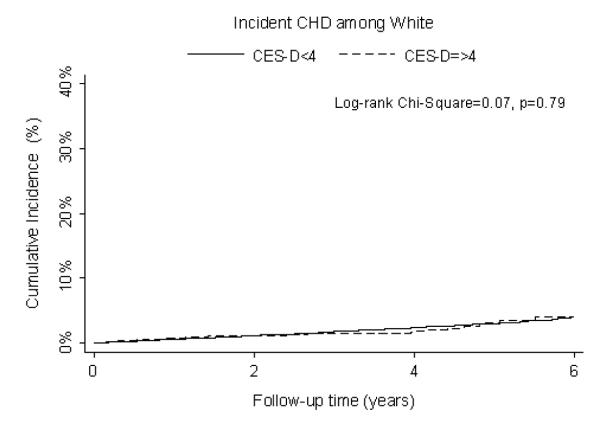
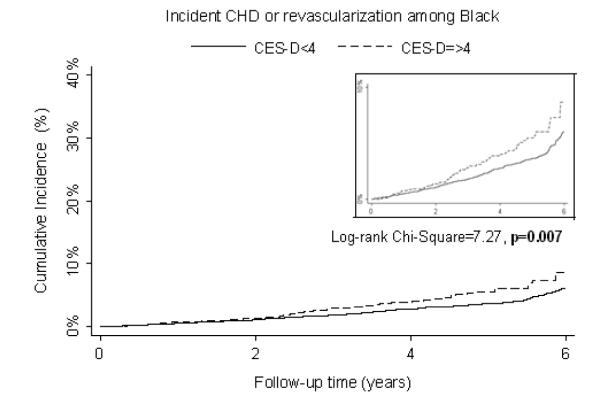
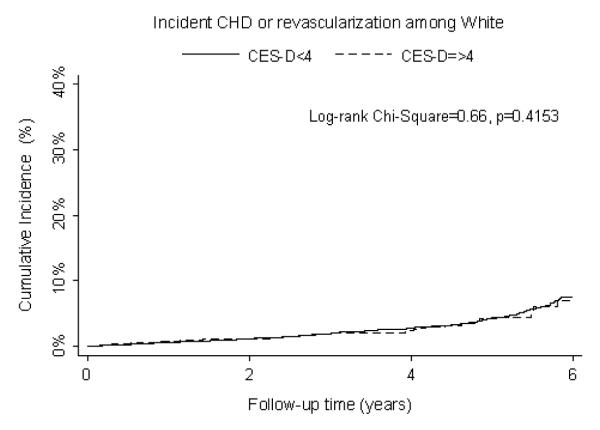
The cumulative incidence of acute CHD and, separately, acute CHD or revascularization, with depressive symptom levels by race are presented in Figure 1. Figure 1a shows Blacks who reported CES-D scores ≥ 4 had a greater cumulative incidence of CHD than Blacks who reported CES-D scores < 4 (p=0.03). Whites had similar cumulative incidence of CHD regardless of CES-D status (Figure 1b). Blacks who reported CES-D scores ≥ 4 had a significantly greater cumulative incidence of CHD or revascularization than Blacks who reported CES-D scores <4 (p=0.007) (Figure 1c). Whites had similar cumulative incidence of CHD or revascularization regardless of CESD status (Figure 1d).
Figure 1.
Cumulative incidence Kaplan-Meier graphs for (A) incident acute CHD among Blacks, (B) incident acute CHD among Whites, (C) incident acute CHD or revascularization among Blacks, and (D) incident acute CHD or revascularization among Whites comparing participants that reported elevated depressive symptoms (CES-D ≥ 4) to participants that reported no depressive symptoms (CES-D <4). A log-rank test was performed and the p-value is reported. CHD indicates coronary heart disease; CES-D, Center for Epidemiological Studies-Depression.
In models stratified on income (Table 3), we found that among participants with an annual income < $35,000, the HR for incident CHD was 1.38 (95% CI1.03-1.83) for those who reported CES-D scores ≥ 4 compared to those reported CES-D scores < 4 adjusting for demographics, SES and behaviors (Model 3). After adjustment for the physiological factors, the HR attenuated and was of marginal statistical significance. Among participants with an annual income ≥ $35,000, depressive symptoms were not associated with incident CHD in any of the models. Depressive symptoms were associated with acute CHD or revascularization in fully-adjusted models for participants who earned <$35,000 (HR, 1.34; 95% CI 1.04-1.72). From Model 1 to Model 4, there was some modest attenuation, but the HR remained statistically significant. Among participants who earned ≥$35,000, depressive symptoms were not associated with incident CHD or revascularization in any of the models.
Table 3.
Association of incident cardiac events with depressive symptoms at baseline by income among REGARDS participants free of CHD at baseline (N=24,261)a
| Nb | Events c |
Model 1d HR (95% CI) |
Model 2e HR (95% CI) |
Model 3f HR (95% CI) |
Model 4g HR (95% CI) |
|
|---|---|---|---|---|---|---|
| Incident Acute Coronary Heart Disease – Annual Income < $35,000 | ||||||
| CES-D < 4(ref) | 9,796 | 325 | 1.0 | 1.0 | 1.0 | 1.0 |
| CES-D≥4 | 1,754 | 63 | 1.41 (1.07-1.86) | 1.43 (1.07-1.90) | 1.38 (1.03-1.83) | 1.33 (1.00-1.77) |
| Incident Acute Coronary Heart Disease – Annual income ≥ $35,000 | ||||||
| CES-D < 4(ref) | 11,935 | 257 | 1.0 | 1.0 | 1.0 | 1.0 |
| CES-D≥4 | 776 | 10 | 0.86 (0.45-1.67) | 0.70 (0.33-1.47) | 0.63 (0.30-1.33) | 0.58 (0.27-1.23) |
| Incident Acute Coronary Heart Disease or Coronary Revascularization - Annual Income < $35,000 | ||||||
| CES-D < 4(ref) | 9,806 | 445 | 1.0 | 1.0 | 1.0 | 1.0 |
| CES-D≥4 | 1,752 | 84 | 1.42 (1.12-1.80) | 1.42 (1.11-1.83) | 1.38 (1.08-1.77) | 1.34 (1.04-1.72) |
| Incident Acute Coronary Heart Disease or Coronary Revascularization - Annual Income ≥ $35,000 | ||||||
| CES-D < 4(ref) | 11,925 | 437 | 1.0 | 1.0 | 1.0 | 1.0 |
| CES-D≥4 | 778 | 13 | 0.73 (0.41-1.29) | 0.56 (0.29-1.09) | 0.53 (0.28-1.03) | 0.54 (0.28-1.02) |
Abbreviations: REGARDS - Reasons for Geographic And Racial Differences in Stroke Study, CHD - coronary heart disease, HR – hazard ratio, CI – confidence interval, CES-D - Center for Epidemiological Studies-Depression, ref – referent.
Persons with baseline CHD excluded. 182 participants, missing baseline CES-D assessment are excluded. Multiple imputation for missing data in covariates, including “refused’ category in income and based on 5 models.
Average number across 5 imputation models
Average number of events across 5 imputation models
Model1 adjusts for age, gender, marital status, region. race
Model2 adjusts for Model1+ education, residence in census tract with poverty level of 30% or more
Model3 adjusts for Model 2 + physical activity, smoking, alcohol consumption
Model4 adjusts for Model3 + diabetes, Body Mass Index, log transformed hsCRP, systolic blood pressure, total cholesterol, HDL, log transformed urinary albumin to creatinine ratio, triglycerides, use of anti-hypertensive medication, use of statins Bolded p-values < 0.05.
Discussion
In this contemporary national study, depressive symptoms were associated with incident acute CHD among Blacks but not Whites. Depressive symptoms were also associated with incident acute CHD or revascularization among Blacks but not Whites. Depressive symptoms were also associated with the CHD/revascularization endpoint for low-income but not high-income individuals. Our findings highlight that many Blacks, who are at greater risk for low-income status, may incur risk for CHD because of depressive symptoms, contributing to long-standing disparities in CHD in the US.
Previous studies have examined the associations of depressive symptoms and CVD.4,9,17,18,45 One study examined depressive symptoms (CES-D 10-item scale) and overall CVD mortality (ischemic heart disease-IHD and stroke) in Blacks and Whites aged 65 and older in a Chicago area study, and found that elevated depressive symptoms were associated with CVD mortality among Blacks but not Whites.9 Another study examined the association of depressive symptoms (CES-D 8-item scale) with CVD mortality (IHD and stroke) in Blacks and Whites age 50 years and older using the Health and Retirement Study, and found that depressive symptoms were associated with overall CVD mortality in Blacks but not Whites.4 Similarly, we found in fully-adjusted models that depressive symptoms were predictive of incident acute CHD among Blacks, but not Whites. Our study is distinct from previous studies in that it is a national study with a large sample of Blacks (n=10,265), and younger age range (adults aged >45).
To our knowledge, no study has examined the association of depressive symptoms with a composite endpoint of CHD or revascularization among Blacks and Whites. Though there was some attenuation from Model 1 to 4, we found that elevated depressive symptoms were significantly associated with incident CHD or revascularization among Blacks. Depressive symptoms are associated with behaviors (physical inactivity, smoking) that may contribute to artery blockage and the need for CABG to restore the flow of blood to the heart. However, even after adjustment for exercise and smoking, associations were significant for Blacks. Research has also shown that a bi-directional association exists between CABG and depression and depressive symptoms, in that knowledge of bypass surgery predicts depression.46 Studies have also reported that patients with elevated depressive symptoms are at risk for CHD mortality and cardiac events after CABG.47-50 These and other factors may explain the robust associations of depressive symptoms with incident CHD or revascularization among Blacks. To our knowledge, no study has examined depressive symptoms as the primary predictor of revascularization among a large sample of Blacks. This gap in the literature demonstrates the need for further understanding this association among Blacks and Black-White differences and how they contribute to racial disparities.
In our examination of the effect modification of income, we found that depressive symptoms had differing effects for those with high and low income, suggesting that depressive symptoms are more important for low-income (than high-income) persons in predicting CHD. Unfortunately, the study had insufficient numbers of events to further explore race differences among low- and high-income participants with high and low depressive symptoms separately. Even in the income-stratified analyses, there were few events among those with depressive symptoms, and we urge caution in interpreting results therein. This level of detail must be examined in future work in order to better understand the social, economic and psychological contributors to racial disparities in CHD.51
Limitations of this study include the inability to draw causal inferences, although REGARDS-MI is a prospective study that allowed for the measurement of depressive symptoms and other covariates as antecedents to CHD endpoints. Second, using self-report measures such as depressive symptoms, SES, and behaviors may misclassify the domain of interest and potentially bias results. The CES-D scale we used is a screening measure to identify depressive symptomatology and not to diagnose clinical depressive symptoms.41 Third, we used the 4-item CES-D scale, whereas the 20-item CES-D scale is more widely used, and depressive symptoms either in the past or during follow-up were not available. Fourth, possible selection bias may have occurred due to the imputation of missing income data. Persons with missing income data may have had a pre-clinical disease or depressive symptoms prior to baseline (not captured in our study). Finally, the relatively small number of events may have contributed to the lack of a dose-response effect of depressive symptoms on CHD risk.
This study makes contributions to understanding CHD disparities by race. First, REGARDS-MI is a large, national cohort of Blacks and Whites that examines the role depressive symptoms play in explaining CHD disparities. Previous studies have used older, smaller samples to examine associations of depressive symptoms and CVD endpoints. Second, this study adds revascularization as a clinical endpoint. Previous studies mainly examine the manner in which CABG contributes to depressive symptoms and not the reverse association. Third, to our knowledge, this is first study that found significant associations of depressive symptoms (using the 4-item CES-D scale) with CHD risk in a large sample of Blacks. Therefore, this shorter scale may be appropriate for testing depressive symptomatology in Black populations. Finally, this study explored in depth how race, income and depressive symptoms contribute to CHD disparities.
Conclusion
Understanding the extent to which depressive symptoms are associated with incident acute CHD and incident CHD or revascularization and how it varies by race and income may provide a better understanding of racial disparities in CHD. Much research has been devoted to understanding this disparity by examining traditional biological and behavioral factors; however, more research is needed that link this disparity to non-traditional psychosocial factors such as depressive symptoms and income, in a large sample of Blacks and Whites.
Acknowledgements
The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Sources of Funding: REGARDS is supported by cooperative agreement U01NS041588 from the National Institute of Neurological Disorders and Stroke (NINDS, Dr. G. Howard, PI). Dr. Safford is supported by grant R01HL080477 and K24 HL111154 from the National Heart, Lung, and Blood Institute (NHLBI). Dr. Safford is also supported by investigator-initiated grant-in-aid from Amgen Corporation. At the time of this work, Dr. Sims was supported by Career Development Award K01 HL08468-05 from the NHLBI, and grants P60MD002249 and U54MD008176 from the National Institute on Minority Health and Health Disparities (NIMHD). At the time of this work, Dr. Redmond was supported by a Minority Investigator Research Supplement R01HL080477-07S1 from NHLBI and grants 1CMS331071-01-00 and 1CMS331300-01-00 from the Centers for Medicare & Medicaid Services.
Abbreviations
- REGARDS
Reasons for Geographic And Racial Differences in Stroke Study
- CHD
coronary heart disease
- CVD
cardiovascular disease
- CATI
computer-assisted telephone interview
- ECG
electrocardiogram
- MI
myocardial infarction
- PCI
percutaneous coronary intervention
- CABG
coronary artery bypass grafting
- CES-D
Center for Epidemiological Studies-Depression
- SES
socioeconomic status
- HS
high school
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- HDL
high density lipoprotein
- hs-CRP
high sensitivity C-reactive protein
- BMI
body mass index
- HMG CoA
hydroxymethylglutaryl-coenzyme A
- HR
hazard ratio
- CI
confidence interval
- SAS
Statistical Analysis System
- IHD
ischemic heart disease
Footnotes
Disclosures: The authors have no competing interests to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115(5):e69–171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 2.Sidney S, Rosamond WD, Howard VJ, Luepker RV. The “heart disease and stroke statistics--2013 update” and the need for a national cardiovascular surveillance system. Circulation. 2013;127(1):21–23. doi: 10.1161/CIRCULATIONAHA.112.155911. [DOI] [PubMed] [Google Scholar]
- 3.Hunink MG, Goldman L, Tosteson AN, et al. The recent decline in mortality from coronary heart disease, 1980-1990. The effect of secular trends in risk factors and treatment. JAMA. 1997;277(7):535–542. [PubMed] [Google Scholar]
- 4.Capistrant BD, Gilsanz P, Moon JR, Kosheleva A, Patton KK, Glymour MM. Does the association between depressive symptoms and cardiovascular mortality risk vary by race? Evidence from the Health and Retirement Study. Ethn Dis. 2013;23(2):155–160. [PMC free article] [PubMed] [Google Scholar]
- 5.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117(4):e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 6.Safford MM, Brown TM, Muntner PM, et al. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308(17):1768–1774. doi: 10.1001/jama.2012.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gutierrez OM, Khodneva YA, Muntner P, et al. Association between urinary albumin excretion and coronary heart disease in black vs white adults. JAMA. 2013;310(7):706–714. doi: 10.1001/jama.2013.8777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 9.Lewis TT, Guo H, Lunos S, et al. Depressive symptoms and cardiovascular mortality in older black and white adults: evidence for a differential association by race. Circ Cardiovasc Qual Outcomes. 2011;4(3):293–299. doi: 10.1161/CIRCOUTCOMES.110.957548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pickering TG. Effects of Stress and Behavioral Interventions in hypertension - Headache and Hypertension: Something Old, Something New. Journal of clinical hypertension. 2000;2(5):345–347. [PubMed] [Google Scholar]
- 11.Pratt LA, Brody DJ. Depression in the United States household population, 2005-2006. NCHS data brief. 2008;(7):1–8. [PubMed] [Google Scholar]
- 12.Skarupski KA, Mendes de Leon CF, Bienias JL, et al. Black-white differences in depressive symptoms among older adults over time. The journals of gerontology. Series B, Psychological sciences and social sciences. 2005;60(3):P136–142. doi: 10.1093/geronb/60.3.p136. [DOI] [PubMed] [Google Scholar]
- 13.Knox S, Barnes A, Kiefe C, et al. History of depression, race, and cardiovascular risk in CARDIA. International journal of behavioral medicine. 2006;13(1):44–50. doi: 10.1207/s15327558ijbm1301_6. [DOI] [PubMed] [Google Scholar]
- 14.Williams DR, Gonzalez HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 15.Gallo JJ, Cooper-Patrick L, Lesikar S. Depressive symptoms of whites and African Americans aged 60 years and older. The journals of gerontology. Series B, Psychological sciences and social sciences. 1998;53(5):P277–286. doi: 10.1093/geronb/53b.5.p277. [DOI] [PubMed] [Google Scholar]
- 16.Blazer DG, Landerman LR, Hays JC, Simonsick EM, Saunders WB. Symptoms of depression among community-dwelling elderly African-American and white older adults. Psychol Med. 1998;28(6):1311–1320. doi: 10.1017/s0033291798007648. [DOI] [PubMed] [Google Scholar]
- 17.Ariyo AA, Haan M, Tangen CM, et al. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Cardiovascular Health Study Collaborative Research Group. Circulation. 2000;102(15):1773–1779. doi: 10.1161/01.cir.102.15.1773. [DOI] [PubMed] [Google Scholar]
- 18.Surtees PG, Wainwright NW, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Depression and ischemic heart disease mortality: evidence from the EPIC-Norfolk United Kingdom prospective cohort study. Am J Psychiatry. 2008;165(4):515–523. doi: 10.1176/appi.ajp.2007.07061018. [DOI] [PubMed] [Google Scholar]
- 19.Yan LL, Liu K, Matthews KA, Daviglus ML, Ferguson TF, Kiefe CI. Psychosocial factors and risk of hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) study. JAMA. 2003;290(16):2138–2148. doi: 10.1001/jama.290.16.2138. [DOI] [PubMed] [Google Scholar]
- 20.Davidson K, Jonas BS, Dixon KE, Markovitz JH. Do depression symptoms predict early hypertension incidence in young adults in the CARDIA study? Coronary Artery Risk Development in Young Adults. Arch Intern Med. 2000;160(10):1495–1500. doi: 10.1001/archinte.160.10.1495. [DOI] [PubMed] [Google Scholar]
- 21.Jonas BS, Lando JF. Negative affect as a prospective risk factor for hypertension. Psychosom Med. 2000;62(2):188–196. doi: 10.1097/00006842-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Boyle SH, Surwit RS, Georgiades A, et al. Depressive symptoms, race, and glucose concentrations: the role of cortisol as mediator. Diabetes care. 2007;30(10):2484–2488. doi: 10.2337/dc07-0258. [DOI] [PubMed] [Google Scholar]
- 23.Everson-Rose SA, Meyer PM, Powell LH, et al. Depressive symptoms, insulin resistance, and risk of diabetes in women at midlife. Diabetes care. 2004;27(12):2856–2862. doi: 10.2337/diacare.27.12.2856. [DOI] [PubMed] [Google Scholar]
- 24.Lewis TT, Everson-Rose SA, Colvin A, Matthews K, Bromberger JT, Sutton-Tyrrell K. Interactive effects of race and depressive symptoms on calcification in African American and white women. Psychosom Med. 2009;71(2):163–170. doi: 10.1097/PSY.0b013e31819080e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marshall GL, Hooyman NR, Hill KG, Rue TC. Association of socio-demographic factors and parental education with depressive symptoms among older African Americans and Caribbean Blacks. Aging Ment Health. 2013;17(6):732–737. doi: 10.1080/13607863.2013.777394. [DOI] [PubMed] [Google Scholar]
- 26.George LK, Lynch SM. Race differences in depressive symptoms: a dynamic perspective on stress exposure and vulnerability. Journal of health and social behavior. 2003;44(3):353–369. [PubMed] [Google Scholar]
- 27.Dinwiddie GY, Gaskin DJ, Chan KS, Norrington J, McCleary R. Residential segregation, geographic proximity and type of services used: evidence for racial/ethnic disparities in mental health. Soc Sci Med. 2013;80:67–75. doi: 10.1016/j.socscimed.2012.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jo SJ, Yim HW, Bang MH, et al. The Association between Economic Status and Depressive Symptoms: An Individual and Community Level Approach. Psychiatry Investig. 2011;8(3):194–200. doi: 10.4306/pi.2011.8.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ruuskanen JM. Physical activity and psychological well-being among people aged 65-84 years. Age Aging. 1995;24:292–296. doi: 10.1093/ageing/24.4.292. [DOI] [PubMed] [Google Scholar]
- 30.Barefoot JC, Schroll M. Symptoms of depression, acute myocardial infarction, and total mortality in a community sample. Circulation. 1996;93(11):1976–1980. doi: 10.1161/01.cir.93.11.1976. [DOI] [PubMed] [Google Scholar]
- 31.Goldston K, Baillie AJ. Depression and coronary heart disease: a review of the epidemiological evidence, explanatory mechanisms and management approaches. Clinical psychology review. 2008;28(2):288–306. doi: 10.1016/j.cpr.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 32.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 33.Diez Roux AV, Ranjit N, Powell L, et al. Psychosocial factors and coronary calcium in adults without clinical cardiovascular disease. Ann Intern Med. 2006;144(11):822–831. doi: 10.7326/0003-4819-144-11-200606060-00008. [DOI] [PubMed] [Google Scholar]
- 34.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45(5):637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 35.Whooley MA, de Jonge P, Vittinghoff E, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300(20):2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carney RM, Blumenthal JA, Freedland KE, et al. Low heart rate variability and the effect of depression on post-myocardial infarction mortality. Arch Intern Med. 2005;165(13):1486–1491. doi: 10.1001/archinte.165.13.1486. [DOI] [PubMed] [Google Scholar]
- 37.Carney RM, Freedland KE, Rich MW, Jaffe AS. Depression as a risk factor for cardiac events in established coronary heart disease: a review of possible mechanisms. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 1995;17(2):142–149. doi: 10.1007/BF02895063. [DOI] [PubMed] [Google Scholar]
- 38.Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25(3):135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 39.Luepker RV, Apple FS, Christenson RH, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation. 2003;108(20):2543–2549. doi: 10.1161/01.CIR.0000100560.46946.EA. [DOI] [PubMed] [Google Scholar]
- 40.Melchior LA, Huba GJ, Brown VB, Reback CJ. A short depression index for women. Educational and Psychological Measurement. 1993;53:1117–1125. [Google Scholar]
- 41.Radloff LS. CES-D scale: A self report depression scale for research in the general populations. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 42.Shrira I, Christenfeld N, Howard G. Exposure to the US Stroke Buckle as a risk factor for cerebrovascular mortality. Neuroepidemiology. 2008;30(4):229–233. doi: 10.1159/000128102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jargowsky PA. Poverty and Place: Ghettos, Barrios, and the American City. Russell Sage Foundation; New York: 1997. [Google Scholar]
- 44.Redmond N, Richman J, Gamboa CM, et al. Perceived stress is associated with incident coronary heart disease and all-cause mortality in low- but not high-income participants in the Reasons for Geographic And Racial Differences in Stroke study. J Am Heart Assoc. 2013;2(6):e000447. doi: 10.1161/JAHA.113.000447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Whang W, Kubzansky LD, Kawachi I, et al. Depression and risk of sudden cardiac death and coronary heart disease in women: results from the Nurses’ Health Study. J Am Coll Cardiol. 2009;53(11):950–958. doi: 10.1016/j.jacc.2008.10.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dias CC, Mateus PS, Mateus C, et al. Myocardial revascularization surgery, depressive symptoms and labeling effect. Rev Port Cir Cardiotorac Vasc. 2004;11(4):201–204. [PubMed] [Google Scholar]
- 47.Mallik S, Krumholz HM, Lin ZQ, et al. Patients with depressive symptoms have lower health status benefits after coronary artery bypass surgery. Circulation. 2005;111(3):271–277. doi: 10.1161/01.CIR.0000152102.29293.D7. [DOI] [PubMed] [Google Scholar]
- 48.Burg MM, Benedetto MC, Soufer R. Depressive symptoms and mortality two years after coronary artery bypass graft surgery (CABG) in men. Psychosom Med. 2003;65(4):508–510. doi: 10.1097/01.psy.0000077509.39465.79. [DOI] [PubMed] [Google Scholar]
- 49.Burg MM, Benedetto MC, Rosenberg R, Soufer R. Presurgical depression predicts medical morbidity 6 months after coronary artery bypass graft surgery. Psychosom Med. 2003;65(1):111–118. doi: 10.1097/01.psy.0000038940.33335.09. [DOI] [PubMed] [Google Scholar]
- 50.Saur CD, Granger BB, Muhlbaier LH, et al. Depressive symptoms and outcome of coronary artery bypass grafting. Am J Crit Care. 2001;10(1):4–10. [PubMed] [Google Scholar]
- 51.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4 Pt 1):1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]