Abstract
Background and Purpose
Little is known about the distribution of National Institutes of Health Stroke Scale (NIHSS) scores from ischemic stroke patients sampled from population-based studies. We describe the distribution of NIHSS in ischemic stroke cases from the Cincinnati/Northern Kentucky Stroke Study.
Methods
Within a biracial population of 1.3 million, all strokes among area residents in 2005 were ascertained by screening discharge records at local hospitals and out-patient clinics. A sampling scheme was developed to ascertain additional cases presenting to physician offices and nursing homes, not identified through the other sources. All confirmed ischemic stroke cases underwent chart abstraction and a retrospective NIHSS (rNIHSS) score (range 0–42) was generated based on initial physician examination findings.
Results
There were 2233 ischemic stroke cases identified during the 12-month study. The overall median rNIHSS score was 3 (IQR 1-7). Median rNIHSS score was 3, 7, and 1, respectively, for stroke cases ascertained through the admitted, inhospital, and out-of-hospital sources. Median rNIHSS was significantly higher in subjects ≥80 years old compared to younger cases (4 vs. 3).
Conclusions
More than half of all ischemic stroke cases have mild symptom severity upon initial presentation (i.e., rNIHSS ≤3). Monitoring trends in NIHSS represents a legitimate target for population-based surveillance efforts.
Keywords: Acute Stroke, NIHSS, severity
Introduction
The National Institutes of Health Stroke Scale (NIHSS) is widely used as a measure of stroke severity and is a strong predictor of patient outcome.1-3 However, NIHSS data from representative samples of acute ischemic stroke patients are lacking; NIHSS is frequently missing in clinical registries,3 and more complete data is usually limited to clinical trial settings. Thus, there are few sources of data that illustrate the distribution of NIHSS in representative population-based samples of ischemic stroke patients. We therefore describe the distribution of NIHSS in ischemic stroke cases from a nationally representative population-based stroke study.
Methods
Details of the design and conduct of the Greater Cincinnati/Northern Kentucky (GCNK) Stroke Study have been described elsewhere.4 Briefly, in calendar year 2005 all acute ischemic stroke events among the 1.3 million residents of the GCNK region were ascertained by identifying inpatient discharge ICD-9 codes 430-436 at 17 area hospitals. Additional screenings for stroke-related visits occurred in all area hospital emergency departments, hospital-based outpatient clinics, and public health clinics, and in sample of 51 of 832 physician offices and 25 of 126 nursing.4 Trained research nurses then undertook an extensive chart abstraction of all suspected stroke cases that included a retrospective NIHSS (rNIHSS) score (0 – 42) based on physician findings at the initial physical examination.5,6 Final confirmation of acute ischemic stroke was based on physician review of the complete medical record and neuroimaging results.
Descriptive statistics of rNIHSS (median, IQR) were generated by demographic subgroups and location of case ascertainment i.e., hospital admission, in-hospital stroke, or out-of-hospital. Out-of-hospital data were weighted to account for the different sampling fractions used in physician offices and nursing homes. To account for the sampling design and multiple stroke events within some subjects, significant differences in log transformed rNIHSS were tested using age-adjusted generalized linear models.
Results
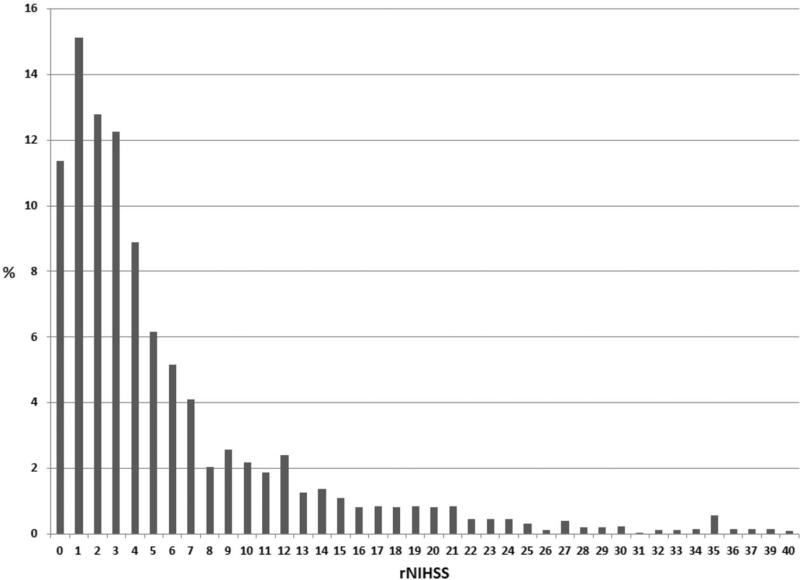
There were 2233 ischemic stroke cases identified during the 12-month study period. The overall distribution of the retrospective rNIHSS is shown in the Figure. The overall median rNIHSS score was 3 (IQR 1-7). The distribution of rNIHSS by age, sex, race, and location of ascertainment are summarized in the Table. The rNIHSS scores were statistically significantly higher in older age groups, and they also differed according to ascertainment location; in-hospital strokes had higher rNIHSS scores (median = 7), while out-of-hospital strokes had lower scores (median = 1), compared to cases admitted to the hospital (median= 3). There were no significant differences by sex or race.
Figure.
Distribution of retrospective NIHSS in 2233 acute ischemic strokes
Table.
Distribution of retrospective NIHSS scores by demographic sub-group and location of ascertainment (n= 2233).
| Sub-group | N | Median | 25 % tile | 75 % tile | P-value* |
|---|---|---|---|---|---|
| Total | 2233 | 3.0 | 1.0 | 7.0 | |
| Age (years) | <0.001 | ||||
| < 65 | 720 | 3.0 | 1.0 | 6.0 | |
| 65-79 | 833 | 3.0 | 1.0 | 7.0 | |
| >= 80 | 680 | 4.0 | 2.0 | 9.0 | |
| Sex | 0.88 | ||||
| Female | 1229 | 3.0 | 1.0 | 8.0 | |
| Male | 1004 | 3.0 | 1.0 | 7.0 | |
| Race | 0.10 | ||||
| White | 1737 | 3.0 | 1.0 | 7.0 | |
| Black | 485 | 4.0 | 2.0 | 8.0 | |
| Other | 11 | 3.0 | 1.0 | 7.0 | |
| Ascertainment Location | 0.02 | ||||
| Hospital admit† | 1932 | 3.0 | 2.0 | 7.0 | |
| In-hospital onset‡ | 271 | 7.0 | 4.0 | 15.0 | |
| Out-of-hospital+ | 30 | 1.0 | 0.0 | 3.0 |
Generated from age-adjusted generalized linear models.
Cases admitted from the community.
Cases developed in patients hospitalized for another reason.
Cases found in out-patient clinics, physician offices and nursing homes.
Discussion
In this population-based representative sample of acute ischemic strokes, more than half had mild symptom severity at initial presentation (i.e., rNIHSS ≤3). We believe this mild spectrum of stroke severity in contemporary ischemic stroke patients is not widely recognized, in part, because most published studies that report NIHSS data are based on selected patient populations enrolled in randomized trials or case-series from academic settings. Our findings are in general agreement with the handful of other reports that have presented NIHSS data from community- or population-based stroke studies. For example, the Northern Manhattan Study demonstrated that just over 50% of ischemic stroke cases had a NIHSS of 0-5.7 In a community-based acute stroke study in Corpus Christi, Texas, the median NIHSS was 3 in a population of almost 1800 ischemic stroke and TIA cases admitted to one of 6 area hospitals.8 The NIHSS will typically be higher in reports where cases are enrolled on the basis of specific clinical inclusion criteria, or where there is incomplete (i.e., selective) reporting of NIHSS. For example, in a report from the Get-With-the-Guidelines(GWTG)-Stroke registry, NIHSS was documented in 40% of hospitalized cases, and the median NIHSS score was 5 (IQR 2-12).9 In GWTG-Stroke, NIHSS scores were more likely to be documented in patients who were younger, male, and arrive by ambulance.3
As expected, stroke severity varied markedly depending on the location where cases were first identified; rNIHSS scores of patients with in-hospital strokes were substantially higher than those of patients who were admitted to the hospital through the emergency department, a finding that has been reported previously.10,11 Unsurprisingly, the severity of stroke cases identified in the out-of-hospital setting was noticeably milder than those admitted to the hospital. Fifteen percent of the cases in this study had a rNIHSS score of 1, while 11% had a rNIHSS of 0 which is much higher than previous estimates.12
The strengths of this study include its population-based approach that is based on well-validated methods that include both in-hospital and out-of-hospital case ascertainment. One limitation is that NIHSS data were collected using retrospective methods which, although shown to be valid across the entire spectrum of scores,5,6 is not as preferable as data collected in real-time by clinical experts; however, such data are difficult to collect across multiple different clinical settings. We also note that it should not be assumed that patients with low NIHSS scores achieve a full recovery; studies show important long-term deficits in function and quality-of-life following mild stroke events.13
In summary, based on a representative population-based sampling of ischemic stroke cases, the spectrum of stroke severity as measured by the NIHSS is surprisingly mild. Given the potential for secular changes in the both the natural history and clinical history of ischemic stroke,4,14 the monitoring of secular trends in NIHSS scores in stroke populations represents a legitimate target for future population-based surveillance efforts. In addition, awareness of the underlying distribution of NIHSS scores may be useful in the planning of future clinical studies.
Acknowledgments
Funding:
Funding for this research was provided by the NIH, NINDS, R01- NS30678.
Footnotes
Disclosures:
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kasner SE. Clinical interpretation and use of stroke scales. Lancet Neurol. 2006;5:603–612. doi: 10.1016/S1474-4422(06)70495-1. [DOI] [PubMed] [Google Scholar]
- 2.Adams HP, Jr., Davis PH, Leira EC, Chang KC, Bendixen BH, Clarke WR, et al. Baseline NIH Stroke Scale score strongly predicts outcome after stroke: A report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology. 1999;53:126–131. doi: 10.1212/wnl.53.1.126. [DOI] [PubMed] [Google Scholar]
- 3.Smith EE, Shobha N, Dai D, Olson DM, Reeves MJ, Saver JL, et al. Risk score for in-hospital ischemic stroke mortality derived and validated within the Get With the Guidelines-Stroke Program. Circulation. 2010;122:1496–1504. doi: 10.1161/CIRCULATIONAHA.109.932822. [DOI] [PubMed] [Google Scholar]
- 4.Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, et al. Stroke incidence is decreasing in whites but not in blacks: a population-based estimate of temporal trends in stroke incidence from the Greater Cincinnati/Northern Kentucky Stroke Study. Stroke. 2010;41:1326–1331. doi: 10.1161/STROKEAHA.109.575043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams LS, Yilmaz EY, Lopez-Yunez AM. Retrospective assessment of initial stroke severity with the NIH stroke scale. Stroke. 2000;31:858–862. doi: 10.1161/01.str.31.4.858. [DOI] [PubMed] [Google Scholar]
- 6.Lindsell CJ, Alwell K, Moomaw CJ, Kleindorfer DO, Woo D, Flaherty ML, et al. Validity of a retrospective National Institutes of Health Stroke Scale scoring methodology in patients with severe stroke. J Stroke Cerebrovasc Dis. 2005;14:281–283. doi: 10.1016/j.jstrokecerebrovasdis.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Dhamoon MS, Moon YP, Paik MC, Boden-Albala B, Rundek T, Sacco RL, et al. Long-term functional recovery after first ischemic stroke: the Northern Manhattan Study. Stroke. 2009;40:2805–2811. doi: 10.1161/STROKEAHA.109.549576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown DL, Lisabeth LD, Garcia NM, Smith MA, Morgenstern LB. Emergency department evaluation of ischemic stroke and TIA - The BASIC Project. Neurology. 2004;63:2250–2254. doi: 10.1212/01.wnl.0000147292.64051.9b. [DOI] [PubMed] [Google Scholar]
- 9.Fonarow GC, Saver JL, Smith EE, Broderick JP, Kleindorfer DO, Sacco RL, et al. Relationship of national institutes of health stroke scale to 30-day mortality in medicare beneficiaries with acute ischemic stroke. J Am Heart Assoc. 2012;1:42–50. doi: 10.1161/JAHA.111.000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farooq MU, Reeves MJ, Gargano J, Wehner S, Hickenbottom S, Majid A. Inhospital stroke in a statewide stroke registry. Cerebrovascular Diseases. 2008;25:12–20. doi: 10.1159/000111494. [DOI] [PubMed] [Google Scholar]
- 11.Kimura K, Minematsu K, Yamaguchi T. Characteristics of in-hospital onset ischemic stroke. Eur Neurol. 2006;55:155–159. doi: 10.1159/000093574. [DOI] [PubMed] [Google Scholar]
- 12.Martin-Schild S, Albright KC, Tanksley J, Pandav V, Jones EB, Grotta JC, et al. Zero on the NIHSS does not equal the absence of stroke. Ann Emerg Med. 2011;57:42–45. doi: 10.1016/j.annemergmed.2010.06.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edwards DF, Hahn M, Baum C, Dromerick AW. The impact of mild stroke on meaningful activity and life satisfaction. J Stroke Cerebrovasc Dis. 2006;15:151–157. doi: 10.1016/j.jstrokecerebrovasdis.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Carandang R, Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Kannel WB, et al. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. Jama-Journal of the American Medical Association. 2006;296:2939–2946. doi: 10.1001/jama.296.24.2939. [DOI] [PubMed] [Google Scholar]