Introduction
Academic medical centers across the United States are facing a crisis. Educational methods are shifting away from didactics and toward labor-intensive problem-based learning. Medical centers are also experiencing lower payments leading to staff layoffs, hiring freezes, limited raises, and faculty and staff salary cuts. (1, 2) Many faculty physicians are asked to work additional half-days in the clinic or see more patients despite efficiency constraints imposed by Electronic Health Records (EHR) and limited staff support.(3) The result has been a growing cadre of faculty who feel over-worked, under-appreciated, and powerless to impact their health care systems. Department Chairpersons caught in this maelstrom find themselves challenged by faculty without the bandwidth to see additional patients and an unwillingness to accept salary cuts. Faculty members point to demands of their research and educational activities and the fact that academic salaries are already 20–30% lower than their cohorts in private practice.(2) It is common to hear complaints about a lack of control over practice and personnel.(2)
Solutions are not easy. Chairpersons are frustrated dealing with unhappy faculty, their own increasing work demands, and turf battles with other departments. Attention to business principles, putting the interests of “our customers” first, and maintaining a focus on our research and education missions can lead to effective solutions.
Methods
The University of Mississippi Medical Center (UMMC) is the only major medical center in the state of Mississippi. The Department of Dermatology is a small department with eight faculty physicians and two nurse practitioners. While the Department is responsible for clinic operations and employing physicians, all other support staff are hired and paid by UMMC’s Ambulatory Operations Department. Traditionally, the university provides one LPN or RN per physician.
While the department is able to apportion 2–3 rooms per dermatologist, one clinical support person cannot efficiently call patients to the exam room, take vitals, perform a history and physical, educate the patient, and record the relevant data into the EHR. A faculty incentive plan (FIP) to reward faculty for “working hard” can do little to improve productivity when faculty are limited by an inefficient system.
During a one-on-one meeting with the chairperson, one faculty member reported frustration with his inability to meet targets in the FIP. He agreed to add six slots to each half day of clinic in exchange for a second LPN/RN. The Department paid for this second “helper” while the Ambulatory Operations Department continued to support one employee. The hypothesis: productivity as measured by completed visits, charges, work relative value units (wRVUs), and collections would increase significantly, creating surplus income greater than the cost of an additional employee.
Results
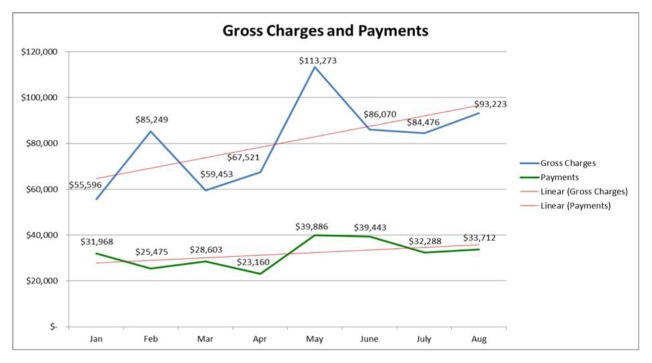
Data was collected over eight months, with the physician having one assistant during the first four months and two assistants during the second four months. Information regarding the above components was recorded and analyzed. The results were impressive: there was a 30% increase in completed visits, 39% increase in wRVU’s, and 33% increase in gross payments received with an annual increase of $144,492 in payments (see figure 1). The faculty member began to consistently reach targets to gain incentive pay while enjoying his work more and minimizing time spent at home completing charts.
Figure 1. Gross charges and gross payments over an 8 month period, with a second assistant present from May until August.
Gross charges increased by 41% and gross payments by 33% during the four months with a second assistant for a gross increase in payments of $36,123 over four months.
Discussion
It is critical to address the financial realities of academic medical centers and departments/divisions in a way that improves physician satisfaction and retention. It is logical that following well-accepted business/leadership principles can lead to improved procedures that are summarized as follows.
Approach the clinic enterprise problems scientifically
A scientific approach in the clinic enterprise requires the formulation of testable hypotheses and obtaining outcomes data. In the case above, the chairman was able to develop scientific support for a business decision made within the department to gain leverage with UMMC leadership. The return on investment (ROI) produced by adding a second assistant to the care team was impressive (net increase annual income of $144,492). The average annual salary of an LPN ($41,540) was covered in the first four months of hire.
Empower individual faculty members by providing the tools they need to succeed
Job burnout and dissatisfaction are often rooted in feelings of hopelessness caused by the inability to exert control on forces that impact one’s professional life. When permitted structural input, physicians predictably can see more patients and generate more income. (5) Job satisfaction also promotes departmental success through increased faculty retention. In the case study above, the “one support person per physician rule” was incompatible with achieving maximal charges or income, especially considering the inefficiencies related to meaningful use of EHRs. (3) While hiring additional support staff served the needs of one physician, other faculty experimented with wave scheduling, working through lunch, controlling the number of new patients per hour, and staggering nursing schedules to ensure rooms are full at the start of each day. Regularly scheduled individual faculty-chairperson meetings permit additional adjustments.
Align incentives and engage mechanisms for self-motivation
Four aspects of a physician’s job provide positive motivation: job attributes, relationships with fellow co-workers, achievement, and remuneration. (6) Remuneration is a difficult issue in cash-strapped academic medical centers. Salaries are generally below the level of private practice. Bonuses and incentive pay are not always available. (4) In fact, poor monetary compensation is a commonly cited reason for academic physicians leaving their jobs. (2) In the case presented, the department established a pilot clinical productivity-based incentive plan. Reachable targets were chosen based on patient charges. Once the target was met, 25% of net patient revenue was returned to the physician.
Putting patients, medical students, and residents first
Academic dermatology departments are ivory towers of education, research centers, and medical care providers for some of the most complex patients in our health care system. The secret for making our academic enterprises a success were nicely distilled in a book: Three Rules for Making a Company Truly Great. (7) The rules are in line with the ethical basis of the medical profession. They are: #1: Put the interests of patients, medical students, and residents ahead of all else (Better before Cheaper). Focusing on quality patient care, teaching, and research is not difficult for academic leaders who stand on the shoulders of those who came before them. #2 Revenue before cost. It costs more today to run a clinical practice considering complex technical treatments, legal and regulatory requirements, and general over-head expenses. It is often more prudent to invest in staff, new technology, education, and training that will pay dividends in the future rather than saving money today.#3: Don’t follow any other rules. Chairpersons must focus on a simple strategic vision for their department and empower administrative staff to manage the process while avoiding overly complex algorithms. (7)
Conclusion
Academic departments/divisions provide patient care, education, and research programs in a complex economic, legal, and regulatory environment. The most difficult aspect is building trust among faculty to accept necessary changes in procedures and policies that impact the department. Ultimately, a strategic vision, good communication with faculty to promote transparency, policies that are simple, and attention to business principles increase the probability of success.
Acknowledgements
None
Footnotes
Author Attribution: Dr. K. Jade Kindley, MD, wrote the first draft of this manuscript. Robert Brodell reviewed and approved the content of the final draft. This article has not been previously published in the literature.
Conflict of Interest: Robert Brodell, MD, discloses the following potential conflicts of interest: honoraria have been received from presentations for Allergan, Galderma Laboratories, L.P, and PharmaDerm, a division of Nycomed US Inc. Consultant fees have been received from Galderma Laboratories, L.P., and Hoffman LaRoche. Clinical trials have been performed for Genentech and Janssen Biotech, Inc. Jeremy Jackson discloses honoraria for presentations from Celgene. K. Jade Kindley, MD, and Taylor Sisson have no conflicts of interest. There was no financial support for the preparation of this manuscript.
References
- 1.Fuchs VR. Current challenges to academic health centers. Journal of American Medical Association. 2013;310(10):1021–1022. doi: 10.1001/jama.2013.227197. [DOI] [PubMed] [Google Scholar]
- 2.Jesitus J. Academia struggles to recruit, retain dermatologists. Dermatology Times. [Accessed October 24, 2014]. http://dermatologytimes.modernmedicine.com/dermatologytimes/news/modernmedicine/modernmedicine-news/academia-strugglesrecruit-retain-dermato?page=fullPublished February 1, 2011.
- 3.Lo HG, Newmark LP, Yoon C, et al. Electronic health records in specialty care: A time-motion study. Journal of the American Medical Informatics Association. 2007;14(5):609–615. doi: 10.1197/jamia.M2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bunton SA, Corrice AM, Mallon WT. Clinical faculty satisfaction with the academic medicine workplace. Association of American Medical Colleges. 2010:1–32. [Google Scholar]
- 5.Westgate A. How practices can add incentives to physician pay: Conference report. Physicians Practice. [Accessed November 7 , 2014]. http://www.physicianspractice.com/mgma/how-practices-can-add-incentivesphysician-payPublished October 24, 2011.
- 6.Lambrou P, Kontodimopoulos N, Niakas D. Motivation and job satisfaction among medical and nursing staff in a Cyprus public general hospital. Human Resources for Health. 2010;8:26–34. doi: 10.1186/1478-4491-8-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raynor ME, Ahmaed M. Three Rules for Making a Company Truly Great. Harvard Business Review. 2013 Apr;:108–117. [Google Scholar]