Abstract
Objective: Although only licensed professionals should be performing cosmetic procedures for patients, there are often news stories of unlicensed individuals performing procedures with serious consequences. This brief report seeks to determine the scope and magnitude of the problem by determining the number of cases of unlicensed procedures and determining the people, procedures, and states that are involved. Design: Various databases were used to find lawsuits and United States English-language news reports from January 1, 2013, through December 31, 2013, which described cosmetic procedures performed by unlicensed individuals. Setting: The United States. Participants: All publicly reported cases. Measurements: Number of cases, case location, type of procedures and injuries, and demographics of the victims and perpetrators. Results: Twenty-eight unique cases were found. The three states with the highest number of cases were Florida (35.7%; n=10), Texas (14.3%; n=4), and California (10.7%; n=3). The type of procedures (n=28) performed were buttocks injections (n=1), face injections (n=7), laser facial procedures (n=2), liposuctions (n=4), and other cosmetic surgeries (n=4). The reported injuries (n=16) were hospitalization (n=8), death (n=4), amputation (n=1), burn (n=1), ptosis (n=1), and scar (n=1). Women and minorities appeared to be disproportionately affected by these illegal procedures. Conclusion: This study likely only provides a small snapshot of a much larger problem, as many cases are presumably not taken to the news or courts. The availability of illegal cosmetic procedures can be diminished with complementary efforts carried out both by law enforcement and the communities themselves.
The American Academy of Dermatology (AAD) defines cosmetic dermatology as treatment of the skin, hair, or nails “that is meant to improve a patient’s appearance rather than treat a disease.” Such treatments include injection of fillers to add fullness; injection of botulinum toxin for wrinkles; laser surgery for blemishes, scars, and hair removal; chemical peels for acne scars; and tumescent liposuction for fat removal.1 In their 2012 Position Statement on the Practice of Dermatology, the AAD writes that “medical aesthetic services should only be delegated to an aesthetician, cosmetologist, or electrologist when competency can be established based on theoretical and didactic education, and clinical training and experience. These licensed professionals should only perform delegated medical aesthetic services under the direct, on-site supervision of a board-certified dermatologist.” The guidelines go further to say that even “licensed and unlicensed medical assistants should only assist a board-certified dermatologist with basic, specific tasks under the dermatologist’s direct, personal supervision.”2
The actual laws in each state vary in their exact language, but the general theme is that professionals who are competent and qualified should be performing the above cosmetic procedures for patients.2 Nonetheless, there are repeated news stories of unlicensed professionals performing these procedures with poor consequences for the patients. This brief report seeks to determine the scope and magnitude of the problem by determining the number of cases of unlicensed procedures and determining who, what, and where is involved.
METHODOLOGY
Lexis Nexis Next, Lexis Nexis Academic, Google News, and Google Advanced Search were used to find lawsuits and US English-language news reports from January 1, 2013, through December 31, 2013, herein termed “cases,” which described cosmetic procedures performed by unlicensed individuals (persons not licensed to practice medicine, such as those without an MD, DO, NP, RN, PA, LVN, or esthetician certification). The following search terms were used: cosmetic, laser, filler, inject, injection, peel, unlicensed, illegal, nonmedical, non-physician. Cases were excluded based on the relevance of titles, and if unclear, based on the case content. Duplicate cases (i.e., articles on the same occurrence of an unlicensed procedure) were excluded. Institutional Review Board approval was not sought because this study did not involve human subjects or private medical records.
RESULTS
A total of 28 unique cases were found. The cases occurred in both 2012 and 2013. The cases spanned 13 states. The three states with the highest number of cases were Florida (35.7%; n=10), Texas (14.3%; n=4), and California (10.7%; n=3). The state of Washington had two cases, and the following states each had one: Arizona, Georgia, Louisiana, Michigan, Mississippi, New Jersey, Nevada, New York, and Tennessee. The type of procedures performed (n=28; Figure 1) were 39.3 percent buttocks injections (n=1l; usually involving industrial-grade silicone or another foreign substance such as cement), 25 percent face injections (n=7; involving legal or illegal botulinum toxin injections), 7.1 percent laser facial procedures (n=2), 14.3 percent liposuctions (n=4), and 14.3 percent other cosmetic surgery (n=4; breast augmentation or other unspecified plastic surgery). The reported injuries (n=16; Figure 1) were 50 percent hospitalization (n=8), 25 percent death (n=4), 6.3 percent amputation (n=1), 6.3 percent burn (n=1; face), 6.3 percent ptosis (n=1; eyelid droop), and 6.3 percent scar (n=1; face). The locations for the procedures (n=20) were 35 percent salon/spa (n=7), 30 percent office (n=6), 20 percent hotel/motel (n=4), and 15 percent home/ apartment (n=3). All cases where victim gender was listed (n=25) involved women. The victim’s age was listed in only four of the cases and ranged from 28 to 42 years. The victim’s race was only listed in six of the cases; five of the six were Hispanic or black. The average age of the perpetrators was 48 years (range 31-59; n=17). The racial breakdown of perpetrators (n=23; Figure 1) was 4.3 percent Asian (n=1), 13.0 percent African American (n=3), 47.8 percent Hispanic (n=1l), 34.8 percent Caucasian (n=8). The perpetrator gender breakdown (n=23) was 43.5 percent men (n=10), 43.5 percent women (n=10), and 13.0 percent transgender (n=3). Four cases involved additional co-perpetrators (e.g., an assistant) who were not counted in the above primary statistics. The perpetrators included (but are not limited to) family members, such as a husband-wife duo or a mother and her two adult daughters; healthcare personnel practicing outside their scope, such podiatrist doing a facial procedure; lay persons posing as licensed doctors/nurses; and persons openly offering cheap illegal procedures.
Figure 1.
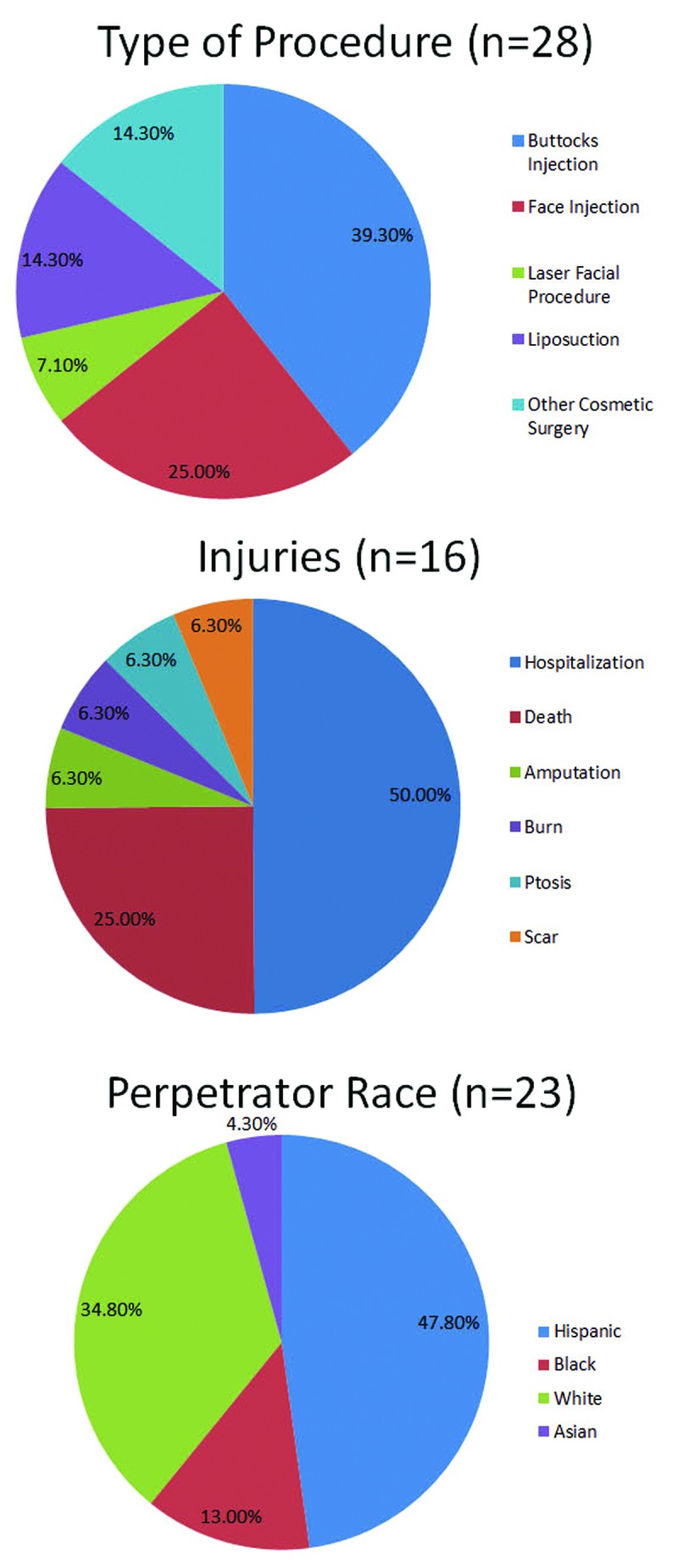
Pie charts illustrating the type of procedures, injuries, and perpetrator race. Several types of procedures were performed by the unlicensed individuals, with buttocks injections the most common. Injuries ranged from scarring to death. The race of the perpetrators varied; however, almost half were Hispanic.
CONCLUSION
This study provides a sampling of injuries due to unlicensed, nonmedical, and non-trained personnel performing elective cosmetic procedures. However, this study likely only provides a small snapshot of a much larger problem, as many cases are presumably not taken to the news or the perpetrator is never found. In addition, the above cases most likely represent only the worst outcomes and do not cover less life-threatening injuries. Although this study provides only a small number of cases, several trends have emerged that can provide hypotheses for future research.
Because many of the victims agree to unlicensed procedures due to the cheaper price tag offered by the perpetrators, the victims are most likely of lower socioeconomic status. In addition, the burden of this issue may be disproportionately carried by minorities, because the majority of both victims and perpetrators in this study were either Hispanic or African American. This could explain the large number of cases in Florida, which has large Hispanic and African American populations. The very high percentage of buttocks injection procedures may relate to cultural focuses on curvy figures and large buttocks. Additionally, the relatively high percentage of transgender perpetrators perhaps reflects the demand of transgender women for feminine figures.3 Finally, the diverse locations for the illegal procedures implies that efforts to combat this problem should not be restricted only to conventional medical offices.
One of the key advocacy areas taken up by the American Society for Dermatologic Surgery Association (ASDSA) is patient safety, especially in regard to use only by licensed medical professionals of dermal fillers and injectables, laser procedures, botulinum toxin, and chemical peels. The ASDS tracks bills being considered by state and federal legislators that pertain to scope of practice for cosmetic procedures, and as of March 2014, they list bills in all but 18 states.4 Proposals have included spelling out full titles on name badges and requiring indication of level of licensure in advertisements. A survey of 1,765 patients found that only 33 percent of patients understand medical title abbreviations, 86 percent want to see a provider’s full title spelled out on name badges, and 89 percent want level of licensure to be required in print ads.5
However, the above proposals pertain to licensed medical professionals performing procedures outside of their expertise; none of the bills address this alarming problem of nonmedical persons performing medical procedures. For unlicensed individuals practicing in offices and spas, the best approach may involve systematic searches by law enforcement for suspicious advertisements on the Internet with subsequent undercover stings. However, for “rogue cosmetic surgeons” utilizing personal networks to practice out of motels and homes, policies will require attention toward the communities and groups that are most affected. For these at-risk people, more education is needed about the risks of unsafe procedures and the avenues available to obtain licensed care. The communities themselves thus will be critical to protecting their own members from utilizing unsafe procedures. Similar to the idea of not letting a friend drink and drive, these communities should take an approach of not letting their friends and loved ones put their lives at risk for procedures done by untrained personnel.
In summary, while the cultures and norms of beauty may be difficult to change, the availability of illegal cosmetic procedures can be diminished with complementary efforts carried out both by law enforcement and the communities themselves.
Footnotes
DISCLOSURE:The authors report no relevant conflicts of interest.
REFERENCES
- 1.American Academy of Dermatology. What is a cosmetic dermatologist? [March 9, 2014]. http://www.aad.org/dermatology-a-to-z/about-dermatology/what-is-a-cosmetic-dermatologist
- 2.American Academy of Dermatology. Position Statement on the Practice of Dermatology: Protecting and Preserving Patient Safety and Quality Care. 2012. [March 9, 2014]. https://www.aad.org/forms/policies/uploads/ps/ps%20practice%20of%20dermatology%20protecting%20and%20preserving.pdf
- 3.Styperek A, Bayers S, Beer M, Beer K. Nonmedical-grade injections of permanent fillers: medical and medicolegal considerations. J Clin Aesthet Dermatol. 2013;6(4):22–29. [PMC free article] [PubMed] [Google Scholar]
- 4.American Society for Dermatologic Surgery Association. Scope of Practice Bill Tracking. [March 9, 2014]. http://asdsa.asds.net/patient-safety.aspx?id=5477
- 5.Smith A, Brod B. https://www.asds.net/_Media.aspx?id=7862 ASDS Future Leaders Network Survey. ASDSA Podcasts: Truth in Advertising: Who’s Behind the White Coat Podcast. 2013.


