Abstract
Background
Scant longitudinal data exists about the interplay between specific substances of abuse, the achievement of abstinence, and clinical outcomes in the treatment of dually diagnosed veterans with post-traumatic stress disorder (PTSD).
Methods
As part of a national program evaluation, veterans admitted from the community to specialized intensive PTSD programs were assessed at intake and 4 months after discharge. Seven mutually exclusive groups were identified from admission self-report data (N=22,948): no substance use, exclusive use of alcohol, opiates, sedatives, cocaine, marijuana, and use of three or more substances. Analysis of covariance, adjusting for potentially confounding baseline variables was used to compare changeamong these seven groups in non-substance use outcomes (PTSD symptoms, violent behavior, suicidality, medical problems, and employment). The effect of abstinence on specific groups was evaluated as the interaction of group membership by abstinence.
Results
All outcome measures except for employment showed significant improvement, with few differences between the groups. Although rate of abstinence differed markedly between the groups, abstinence achievement was associated with greater improvement on all the outcomes except employment in every group. No significant differences in the effect of abstinence across the substance abuse groups were observed.
Conclusion
The specific type of substance used prior to entry into treatment among dually diagnosed PTSD patients seems to have limited effect on treatment outcomes. However, attainment of abstinence at 4 months after treatment, irrespective of the substances abused, was strongly associated with improvement in PTSD symptoms, violence, suicidality and medical problems.
Keywords: Stress Disorders, Post-Traumatic; Substance Use Disorders; Dual Diagnosis; Psychotherapy; Treatment Outcome
1. INTRODUCTION
Posttraumatic stress disorder (PTSD) is associated with frequent comorbid substance use disorder (SUD; McCauley et al., 2012). Clinical morbidity and treatment response have been reported to be worse among PTSD patients with comorbid SUD (McCauley et al., 2012), supporting the general assumption that concurrent substance use worsens the severity of psychiatric disorders. However, in an analysis of data from national program evaluation of Veteran Health Administration (VHA) specialized intensive PTSD treatment programs providing almost daily treatment that included PTSD focused psychotherapy and medication management for many weeks, often with a programmatic expectation of abstinence, Fontana et al (2012) paradoxically reported that Veterans with PTSD and current SUD diagnosis (using any substance and meeting the diagnostic criteria in 30 days prior to the qualifying period for admission to treatment program) showed greater improvement in PTSD symptoms and other outcomes four months after treatment completion in comparison to Veterans with PTSD and no current SUD diagnosis. This difference in treatment effect was accounted for to a substantial extent by decreased days of substance use after treatment. In a subsequent analysis of these data focused on any marijuana use, patients who reported abstinence from marijuana 4 months following discharge showed greater improvement in PTSD symptoms and reduction in violent behavior compared to those who initiated or continued previous use of marijuana (Wilkinson et al., 2014). However, a comparison of the effects of marijuana with other addictive substances regarding PTSD outcomes was not conducted. In a single center study with similar settings, Bonn-Miller et al (2013) showed that veterans with PTSD and cannabis use disorder showed lesser improvement in symptoms compared to others at the completion of treatment. Prior studies have suggested that “hard” drugs like opioids (heroin) and cocaine may have more deleterious psychological effects compared to substances like marijuana in both the general population (Nutt et al., 2010) and in patents diagnosed with PTSD (Cottler et al., 1992; Goldenberg et al., 1995). These studies together raise the questions whether PTSD treatment evokes differential response depending on the specific substances used prior to the treatment episode, and how achievement of abstinence influences the outcome with different types of substance use (SU).
Hien et al (2010a) have suggested that results of outcomes studies pertaining to PTSD and SUD are limited by the tendency to collapse SU categories due to small sample sizes, and that identifying the specific types of substances used at treatment entry may be valuable in predicting treatment response, and should, perhaps, shape treatment processes for these veterans. In this study, we use data from the entire large national VHA program evaluation data set that formed the basis for the studies published by Fontana et al (2012) and by Wilkinson et al (2014) to explore differences in the PTSD and other clinical outcomes among Veterans who did not report any substance use in the 30 days prior to being admitted to specialized intensive PTSD treatment programs as compared to five groups of Veterans who reported use of a single specific addictive substance, and a final group who used three or more classes of substance. We then compare the association of abstinence after treatment for PTSD with outcomes across the seven SU groups. The particular focus of our study was on the impact of recent use and short-term changes in daily use of specific substances rather than SUD diagnoses.
2. METHOD
This study was approved by VACT HCS Institutional Review Board, and followed standard privacy protection protocols, especially regarding SU related data.
2.1. Programs and participants
The data were drawn from an administrative program evaluation developed by VHA Northeast Program Evaluation Center (NEPEC) to evaluate treatment outcomes for Veterans admitted to specialized intensive PTSD programs from 1992- 2011. These programs included inpatient, residential (i.e., halfway house) and day programs that provided services virtually every day of the week for many weeks and generally had programmatic expectation of abstinence prior to entry and during treatment. SU data address self-reported days of substance use during the 30 days prior to the qualifying period before admission; urine toxicology data was not collected.
All patients were evaluated at entry and 4 month after discharge using a standardized set of socio-demographic and clinical measures. The analytic sample excluded veterans who entered treatment on transfer from another inpatient or residential program (who thus would likely have had artificially restricted access to alcohol or drugs). From the entire sample of 47, 310 veterans with a clinical diagnosis of PTSD 35,330 were admitted directly from the community. Veterans were followed up through face-to-face interviews or by phone four months following discharge. Only veterans who completed follow up evaluations were included in the analyses (N=24,160).
From this sample, we identified seven mutually exclusive categories of patients based on their self-reported substance use in 30 days prior to the admission: non-users who did not report any use of alcohol to intoxication or illicit drugs (N=18,719), Veterans who only abused alcohol to intoxication (N=2,542) but no other substances; Veterans who abused opioids only (N=252); who abused sedatives or anxiolytics only N=(113); cocaine/crack or stimulants only (N=159); marijuana only (N=623); and polysubstance users who reported using 3 or more of these substances (N=540). Within this last group reported use rates were 90.17% for alcohol, 58.81% for opiates, 39.15% for sedatives, 74.21% for cocaine, and 81.63% for cannabis. The final analytic sample included 22,948 patients. Toxicological confirmation of substance use was not available. However, available literature suggests that self-report have high correlation with urine toxicology reports in general substance use and dual diagnosis among veterans with PTSD (Calhoun et al., 2000; Darke, 1998; Weiss et al., 1998).
2.2. Measures
Socio-demographic, clinical and military service data were derived from a structured clinical interview conducted by a clinician/research assistant located in individual sites at the time of admission to the program using standardized forms. Research assistant recorded self-report data from veterans in response to structured questions. Since ratings were not based on the judgment of research assistants, the lack of test-retest reliability data (impractical to gather in a large ongoing national program evaluation) does not jeopardize that quality of the data. These data included age, gender, marital status, race/ethnicity, highest year of education, employment, income from work prior to the time of admission, history of incarceration, Axis I psychiatric diagnoses in addition to PTSD or SUD, personality disorder diagnosis, and service connection for PTSD, for another psychiatric disorder, or for a medical disorder. Psychiatric symptom severity and use of alcohol or illicit drugs was assessed by items from composite subscales of the Addiction Severity Index (ASI; McLellan et al., 1985).
Measures of PTSD symptoms and days of substance use were obtained from self-report questionnaires completed by Veterans upon admission and four months following discharge. The admitting clinician clinically determined the diagnoses of PTSD, other psychiatric disorders, and substance use disorders (SUD). The Short Form of the Mississippi Scale (Fontana and Rosenheck, 1994) for PTSD was used to measure current PTSD symptom severity. This is an 11-item version of the full Mississippi Scale that correlates between 0.90 and 0.95 with the full version and that has high sensitivity to change in treatment (Fontana and Rosenheck, 1994). Symptoms assessed by this scale include feeling numb and emotionally distant from others, avoiding reminders of the war, intrusive thoughts, sleep disturbances, flashbacks and nightmares, and symptoms of irritability and hyperarousal. These symptoms mapped on well to DSM-IIR criteria for PTSD, and the full MISSISSIPPI scale was actually derived from DSM-IIIR criteria for PTSD (Fontana and Rosenheck, 1994; Keane et al., 1988).
Evidence of substance use of various kinds was based on items from the Addiction Severity Index reporting any days of use of the following substances in the 30 days prior entry assessment: drinking alcohol to the point of feeling drunk or intoxicated; using opioid narcotics; barbiturates or other sedatives (“downers”); cocaine, crack or amphetamines; or marijuana. The ASI also assesses patient status using composites composed of multiple measures. We used composite scores in the following five areas: medical problems, employment, drug use, and alcohol use (McLellan et al., 1980). The items are standardized and summed to produce a mathematically derived composite score, which ranges from 0.00 to 1.00 for each ASI problem area. Employment status was assessed as the average number of days a veteran had worked for pay in the previous 30 days as well as the composite employment score from the ASI (McLellan et al., 1985). Violent behavior was assessed using a 4-item scale (range 0-4) from the National Vietnam Veterans Readjustment Study (Kulka, 1990). All measures of psychopathology had reasonable internal consistency as represented standardized Cronbachs alphas of 0.69 for short MISSISSIPPI, 0.84 for violence score, 0.95 for ASI Medical index, and 0.78 for ASI Employment index.
2.3. Data Analysis
A seven level nominal variable of mutually exclusive categories was created reflecting substance use at the time of program entry as described above. Baseline characteristics of the 7 SU groups were compared using Chi-square technique for categorical variables, and analysis of variance (ANOVA) for continuous variables. Due to the large sample size, statistical significance testing with p values would be of limited use to detect meaningful differences between the groups. For categorical variables, we compared the SU groups with the largest and smallest proportions using risk ratios with a criterion of risk ratio <0.5 or >2.0 as clinically substantial. For continuous variables, we compared the largest and smallest mean group values using Cohen's d (the difference between means divided by the pooled baseline standard deviation) with a criterion of ≥0.41 as the indicator of substantial clinical difference (Ferguson, 2009).
Variables that were found to be substantially different by the above criteria and had a base rate of more than 10% were included as covariates in analysis of covariance (ANCOVA) to compare change in non-substance use outcomes 4 months after discharge between the seven groups. The outcome variables studied were change in severity of PTSD symptoms on the Short Mississippi PTSD Scale score, the violent behavior score, days of employment, and an item reflecting suicidality from the Mississippi scale.
Next, we identified those who reported no substance use (i.e., abstinence) and any substance use (i.e., non-abstinence) 4 months after discharge in each of the seven SA groups and used chi square tests to compare the proportion. For descriptive purposes, we further describe substances that were involved in the continued use among users in each category.
We then compared change in outcomes between abstinent and non-abstinent veterans 4 months after discharge within each SA group using ANCOVA to control for the same covariates identified previously, but adding a term representing the interaction of SA group and abstinence. T-tests were again used to compare differences in outcomes among abstinent and non-abstinent veterans within each baseline SA group. We thus sought to compare the association of abstinence within each SA group with non-substance use outcomes.
3. RESULTS
3.1. Baseline demographics
Veterans were of similar age across the SU categories, and overwhelmingly of male gender (Table 1). Cocaine only users had largest and Sedative/hypnotic users had the lowest proportions of Veterans identifying as Black (Risk Ratio [RR]=4.84). Veterans belonging to the cocaine only, marijuana only, and polysubstance groups were less often married and working, more often divorced and incarcerated, and earned lower income from employment. Veterans belonging to the alcohol only and sedative/hypnotics only categories had higher proportions identifying as whites (RR 2.56) and were more often working (RR 2.71).
Table 1.
Baseline demographic characteristics at presentation by Substance Use groups
| No Alcohol/Drugs | Alcohol only | Opioids only | Sedative/Hypnotic Only | Cocaine Only | Marijuana only | Poly substance | Risk Ratio/Cohen's d* | |
|---|---|---|---|---|---|---|---|---|
| Number | 18719 | 2542 | 252 | 113 | 159 | 623 | 540 | ¥ |
| Age in years | 53.70 (8.49) | 50.67 (10.71) | 52.73 (8.42) | 52.12 (8.93) | 50.89 (8.66) | 49.65 (10.17) | 48.49 (9.93) | 0.59* |
| Male gender (%) | 96.27 | 95.9 | 89.29 | 87.34 | 91.82 | 95.78 | 96.06 | 1.10 |
| MARITAL STATUS (%) | ||||||||
| Married | 46.96 | 43.71 | 44.05 | 47.79 | 28.3 | 38.36 | 22.96 | 2.08 |
| Remarried | 8.37 | 8.58 | 11.11 | 7.96 | 5.03 | 6.58 | 3.7 | 3.00 |
| Widowed | 1.88 | 1.97 | 1.59 | 2.65 | 1.89 | 2.73 | 3.52 | 2.21 |
| Separated | 6.43 | 6.49 | 8.73 | 7.08 | 11.95 | 6.58 | 12.22 | 1.90 |
| Divorced | 29.39 | 29.78 | 26.98 | 22.12 | 35.85 | 34.51 | 42.59 | 1.93 |
| Never Married | 6.97 | 9.48 | 7.54 | 12.39 | 16.98 | 11.24 | 15 | 2.44 |
| RACE/ETHNICITY (%) | ||||||||
| White | 63.6 | 72.62 | 62.3 | 78.95 | 30.82 | 71.29 | 54.44 | 2.56 |
| Black | 23.77 | 14.83 | 23.41 | 12.28 | 59.12 | 16.13 | 36.3 | 4.84 |
| Hispanic | 7.77 | 7.00 | 8.33 | 4.39 | 7.55 | 6.13 | 5.18 | 1.90 |
| Other | 4.92 | 5.54 | 5.95 | 4.38 | 2.52 | 6.44 | 4.08 | 2.56 |
| Service connected (%) | ||||||||
| PTSD | 53.37 | 51.32 | 47.22 | 59.29 | 53.46 | 51.13 | 39.56 | 1.50 |
| Other Psych | 4.61 | 3.47 | 28.17 | 3.54 | 6.29 | 4.51 | 5.56 | 8.12 |
| Medical | 48.80 | 50.61 | 50.60 | 34.51 | 41.51 | 45.57 | 41.04 | 1.47 |
| SOCIAL MEASURES | ||||||||
| Highest school year | 12.91 (0.02) | 13.15 (0.04) | 12.98 (0.14) | 13.10 (0.20) | 12.92 (0.17) | 13.01 (0.09) | 12.82 (0.09) | 0.15* |
| Working now (%) | 31.44 | 45.40 | 16.27 | 39.47 | 20.75 | 25.04 | 23.66 | 2.71 |
| Ever incarcerated (%) | 44.95 | 43.41 | 49.21 | 41.23 | 59.75 | 53.13 | 67.68 | 1.64 |
| Valid drivers license (%) | 85.39 | 83.06 | 82.47 | 87.71 | 62.89 | 81.15 | 663.59 | 1.39 |
| Car Available (%) | 79.08 | 79.28 | 74.50 | 75.44 | 43.40 | 76.97 | 54.90 | 1.83 |
| Employment income past 30 days (SD) | $286.50 (792.58) | $456.83 (1007.71) | $189.78 (595.89) | $478.80 (1084.70) | $255.88 (717.80) | $213.22 (655.48) | $228.26 (601.78) | 0.36* |
| Days worked: last 30 days (SD) | 3.51 (8.23) | 5.13 (9.45) | 2.26 (6.49) | 5.23 (9.80) | 3.71 (8.64) | 2.86 (7.12) | 3.80 (8.30) | 0.36* |
| SERVICE ERA (%) | ||||||||
| WW II | 3.80 | 2.13 | 1.98 | 0.88 | 1.92 | 0.48 | 0.92 | 7.91 |
| Vietnam | 81.16 | 70.66 | 79.37 | 80.70 | 74.36 | 73.19 | 68.76 | 1.18 |
| Post Vietnam | 4.24 | 4.65 | 7.54 | 5.26 | 9.62 | 7.22 | 8.32 | 2.26 |
| Gulf war | 10.80 | 22.57 | 11.11 | 13.16 | 14.10 | 19.10 | 22.00 | 2.08 |
Comparison of highest to lowest value among substance use groups.
Cohen's d (not Risk Ratio)
3.2. Clinical history at presentation
A clinical diagnosis of alcohol or drug abuse/dependence had the highest prevalence in the polysubstance group (Table 2, RR >2). No substantial difference in the proportions of other psychiatric diagnoses was observed between groups (RR <2). The vast majority of the veterans in every group served in a war zone during their military service, and a substantial proportion observed or participated in what they considered to have been atrocities. Symptom burden (Short MISSISSIPPI, Violence and Suicidality scores) was highest in the polysubstance group at the time of admission (Cohens d 0.96 and 2.10 respectively representing large effect sizes). The opiate only and polysubstance group had the highest levels of medical problems on the ASI medical problems composite score (Cohens d 0.79).
Table 2.
Clinical history at presentation by Substance Use groups
| No Alcohol/Drugs | Alcohol only | Opioids only | Sedative/hypnotic Only | Cocaine Only | Marijuana only | Poly substance | Risk Ratio/*Cohen's d | |
|---|---|---|---|---|---|---|---|---|
| Number | 18719 | 2542 | 252 | 113 | 159 | 623 | 540 | ¥ |
| Clinical Diagnoses (%) | ||||||||
| Alcohol Abuse/Dependence | 35.91 | 52.98 | 36.73 | 36.96 | 46.27 | 40.72 | 72.48 | 2.02 |
| Drug abuse/dependence | 20.03 | 13.53 | 31.87 | 21.05 | 64.15 | 47.59 | 72.46 | 5.36 |
| Anxiety disorder NOT PTSD | 11.34 | 11.25 | 12.7 | 11.4 | 10.06 | 12.38 | 13.52 | 1.34 |
| Affective disorder not bipolar | 29.32 | 25.3 | 29.76 | 25.44 | 29.56 | 29.35 | 25.79 | 1.18 |
| Bipolar disorder | 4.13 | 3.93 | 5.16 | 6.14 | 6.29 | 5.64 | 5.19 | 1.60 |
| Schizophrenia | 1.04 | 0.83 | 0.79 | 0 | 3.14 | 0.81 | 2.22 | |
| Personality disorders | 7.15 | 6.06 | 7.54 | 14.91 | 6.92 | 9.18 | 10.39 | 2.46 |
| Military Trauma Factors (%) | ||||||||
| War zone service | 90.25 | 88.65 | 91.67 | 90.27 | 90.57 | 85.39 | 82.00 | 1.12 |
| Observed/participated in atrocities | 62.96 | 62.03 | 56.72 | 72.92 | 59.38 | 67.45 | 77.70 | 1.37 |
| Sexual Trauma during active duty | 4.40 | 4.15 | 8.71 | 9.00 | 9.15 | 5.92 | 5.37 | 2.20 |
| Non-combat military trauma | 7.58 | 7.70 | 7.05 | 9.00 | 12.42 | 8.55 | 13.32 | 1.89 |
| Symptom Burden | ||||||||
| Short MISSISSIPPI Score (SD) | 39.31 (5.84) | 40.21 (5.49) | 39.85 (5.62) | 40.30 (5.69) | 39.07 (6.40) | 39.81 (5.52) | 41.65 (5.39) | 0.96* |
| Violence Score (1-4) | 1.37 (1.31) | 1.62 (1.30) | 1.48 (1.32) | 1.42 (1.33) | 1.57 (1.32) | 1.60 (1.33) | 2.33 (1.36) | 2.10* |
| ASI Employment score (SD) | 0.59 (0.26) | 0.61 (0.27) | 0.56 (0.26) | 0.61 (0.26) | 0.41 (0.30) | 0.56 (0.26) | 0.45 (0.31) | 0.45* |
| ASI Medical condition score (SD) | 0.57 (0.35) | 0.56 (0.34) | 0.69 (0.32) | 0.55 (0.34) | 0.59 (0.38) | 0.57 (0.35) | 0.63 (0.33) | 0.79* |
| Suicidal [Scored 1 to 4]: Mean (SD) | 2.26 (1.23) | 2.33 (1.23) | 2.42 (1.25) | 2.47 (1.24) | 2.25 (1.28) | 2.32 (1.21) | 2.56 (1.23) | 0.01* |
| Violent behavior in past 30 days (%) | 30.00 | 33.73 | 30.95 | 27.19 | 27.04 | 32.42 | 38.96 | 1.44 |
| Psychiatric medications prescribed in last 30 days (%) | 87.07 | 83.77 | 89.68 | 92.04 | 84.81 | 85.05 | 84.81 | 1.10 |
Comparison of highest to lowest value among substance use groups.
Cohen's d (not Risk Ratio)
3.3. Change in clinical measures 4 months after discharge
After adjusting for variables showing substantial baseline differences, four of the five change measures showed improvement in every SU group (p<0.01), with no significant difference in the magnitude of change between SU groups (p>0.01), except for the ASI medical score (p<0.01) that showed the greatest improvement in the polysubstance group in paired comparisons (Table 3). The ASI employment score showed no significant change in any group.
Table 3.
Change in clinical measures, admission to 4 month after discharge from treatment, least square means by Substance Use groups
| 1- No Alc./Drugs | 2- Alcohol only | 3- Opioids only | 4- Sedative/hypnotics Only | 5- Cocaine Only | 6-Marijuana only | 7- Poly substance | Statistics& | |
|---|---|---|---|---|---|---|---|---|
| Short MISSISSIPPI Score change [SE]^ | −1.70 [0.05] | −1.91 [0.13] | −1.56 [0.40] | −2.12 [0.63] | −2.47 [0.51] | −1.98 [0.26] | −2.59 [0.29] | F 2.38 P=0.03 |
| Violence Score change [SE]^ | −0.56 [0.01] | −0.53 [0.02] | −0.62 [0.07] | −0.57 [0.11] | −0.54 [0.09] | −0.59 [0.04] | −0.52 [0.05] | F 0.73 P=0.62 |
| Suicidality score (1-4) change [SE]^ | −0.21 [0.01] | −0.28 [0. 02] | −0.23 [0.06] | −0.35 [0.10] | −0.31 [0.08] | −0.26 [0.04] | −0.27 [0.05] | F 2.11 P=0.05 |
| ASI Medical condition score Change [SE]* | −0.05 [0.00] | −0.07 [0.01] | −0.01 [0.02] | −0.07 [0.04] | −0.10 [0.03] | −0.05 [0.02] | −0.11 [0.02] | F 4.09 P<0.01 |
| ASI Employment score change [SE]^ | −0.001 | +0.0001 | −0.003 | +0.032 | +0.003 | −0.003 | −0.024 | F 1.77 P=0.10 |
SE: Standard Error (not provided for ASI employment score change as values are too small)
Statistics for comparison between the groups
Significant paired comparisons: Not applicable
Significant paired comparisons: 7>1,3,6
Model adjusted for variables found relevant in baseline analysis (age, marital status, race/ethnicity, service connected status for other psychiatric issues, current employment, possession of car, sexual trauma in military), and baseline measures of ASI indices & outcome variables.
Self-reported abstinence at 4 months varied substantially among the SU groups (Table 4). Among those using alcohol or drugs at baseline, the lowest rates of abstinence were found in marijuana only group (44%) and the highest in the opioid only group (72%). Even among those who did not report using any alcohol or drugs at base line, nearly 18% were using some substance 4 months after discharge. Among those who were using a specific substance at baseline, most were using the same substance 4 months after discharge. Alcohol abuse was frequent at 4 months after discharge in all the SU groups.
Table 4.
Self-reported substance use patterns at 4 months after discharge in Substance Use groups at baseline
| No Alcohol/Drugs | Alcohol only | Opioids only | Sedatives/hypnotics Only | Cocaine Only | Marijuana only | Polysubstance | |
|---|---|---|---|---|---|---|---|
| Abstinent (%) | 82.1 | 48.7 | 72.4 | 69.3 | 68.4 | 43.3 | 59.6 |
| Any substance/alcohol (%) | 17.9 | 51.3 | 27.6 | 30.7 | 31.6 | 56.7 | 40.4 |
| Alcohol use (%) | 13.1 | 45.8 | 13.1 | 13.2 | 21.5 | 17.7 | 28.3 |
| Opioids use (%) | 2.8 | 3.4 | 14.0 | 8.8 | 2.6 | 5.3 | 12.0 |
| Sedatives & Hypnotics use (%) | 1.8 | 2.2 | 4.0 | 15.7 | 3.9 | 2.4 | 8.5 |
| Cocaine use (%) | 1.4 | 1.5 | 2.0 | 0.9 | 14.3 | 2.9 | 11.8 |
| Cannabis use (%) | 4.6 | 6.4 | 4.0 | 3.5 | 5.8 | 49.1 | 22.2 |
3.4. Association of abstinence with change in clinical measures
Analysis of the association of abstinence with change in clinical measures 4 months after discharge showed highly significant main effects for abstinence which was associated with greater improvement on 4 of the five measures (Table 5). A significant main effect was also found for SU groups (with the exception of ASI employment index). However, there was no significant interaction between SU group and abstinence on any measures of change from admission to 4 months after discharge. In other words, abstinence was associated with greater improvement on all the outcomes except for ASI employment index score, but there were no significant differences in the degree of improvement associated with abstinence across SU groups.
Table 5.
Changes in clinical measures stratified by abstinence at 4 months after discharge by substance use groups
| 1 No Alcohol/drugs | 2 Alcohol only | 3 Opioids only | 4 Sedative/hypnotic only | 5 Cocaine only | 6 Marijuana only | 7 Polysubstance | |
|---|---|---|---|---|---|---|---|
| Short MISSISSIPPI Score change* | |||||||
| Not Abstinent | +0.57 [0.11] | −0.28 [0.18] | +0.35 [0.74] | −1.41 [1.09] | −0.40 [0.90] | −0.77 [0.34] | −0.21 [0.43] |
| Abstinent | −2.21 [0.05] | −3.37 [0.18] | −2.31 [0.47] | −2.44 [0.76] | −3.10 [0.61] | −3.57 [0.39] | −4.13 [0.37] |
| Violence Score change** | |||||||
| Not Abstinent | −0.21 [0.02] | −0.27 [0.03] | −0.36 [0.13] | −0.34 [0.19] | −0.17 [0.15] | −0.47 [0.06] | −0.10 [0.07] |
| Abstinent | −0.64 [0.01] | −0.75 [0.03] | −0.71 [0.08] | −0.63 [0.13] | −0.67 [0.10] | −0.75 [0.07] | −0.79 [0.06] |
| Suicidality score change*** | |||||||
| Not Abstinent | +0.07 [0.02] | −0.11 [0.03] | +0.07 [0.12] | −0.12 [0.18] | −0.02 [0.14] | −0.08 [0.06] | −0.08 [0.07] |
| Abstinent | −0.28 [0.01] | −0.43 [0.03] | −0.34 [0.08] | −0.43 [0.12] | −0.40 [0.10] | −0.50 [0.06] | −0.39 [0.06] |
| ASI Medical score change**** | |||||||
| Not Abstinent | −0.01 [0.007] | −0.04 [0.01] | +0.07 [0.05] | −0.04 [0.07] | −0.04 [0.05] | −0.03 [0.02] | −0.07 [0.03] |
| Abstinent | −0.06 [0.003] | −0.09 [0.01] | −0.04 [0.03] | −0.09 [0.05] | −0.12 [0.04] | −0.07 [0.02] | −0.14 [0.02] |
| ASI Employment score change***** | |||||||
| Not Abstinent | −0.001 | −0.010 | −0.002 | −0.0066 | −0.028 | +0.005 | −0.031 |
| Abstinent | −0.0004 | −0.009 | −0.005 | −0.016 | +0.017 | −0.012 | −0.018 |
All values with [Standard Error]: not provided for ASI employment score change as values are too small.
Model adjusted for baseline variables (age, marital status, race/ethnicity, service connected for other psychiatric issues, employment, possession of car, sexual trauma in military), baseline ASI indices & outcome variables, abstinence achievement at 4 months, and interaction between abstinence achievement and SA group.
Main effects and paired comparisons:
SU groups: F Value 14.69, p <0.0001; Abstinence: F-value 81.83, p<0.0001; Interaction of abstinence and SU groups: F value 1.11, p=0.3535. Abstinent Vs not abstinent paired comparison: 1,2,6&7- p<0.0001; 3- p<0.01; 4- p=0.43; 5- p=0.013. Significant paired comparison for SU group main effect (p<0.01): 1 Vs 2,6&7
SU groups: F Value 4.79, p <0.0001; Abstinence: F-value 72.08, p<0.0001; Interaction of abstinence and SU groups: F value 1.92, p=0.0743. Abstinent Vs not abstinent paired comparison: 1,2,&7- p<0.0001; 5&6- p<0.001; 3- p=0.02; 4- p=0.20. Significant paired comparison for SU group main effect (p<0.01): 1 Vs 2&6
SU groups: F Value 11.50, p <0.0001; Abstinence: F-value 52.74, p<0.0001; Interaction of abstinence and SU groups: F value 0.27, p=0.9518. Abstinent Vs not abstinent paired comparison: 1,2&6- p<0.001; 3- p=0.004; 4- p=0.156; 5- p=0.034; 7- p=0.0009. Significant paired comparison for SU group main effect (p<0.01): 1Vs 2,6&7.
SU groups: F Value 5.84, p <0.0001; Abstinence: F-value 12.45, p=0.0004; Interaction of abstinence and SU groups: F value 0.45, p=0.8446 Abstinent Vs not abstinent paired comparison: 1- p<0.0001; 2- p<0.001; 3- p=0.05; 4,5&6- p>0.1; 7- p=0.02. Significant paired comparison for SU group main effect (p<0.01): 1 Vs 2&7; 3 Vs 2&7.
SU groups: F Value 2.05, p =0.0552; Abstinence: F-value 0.32, p=0.5717; Interaction of abstinence and SU groups: F value 1.95, p=0.687. Paired comparison not applicable.
With respect to the Short MISSISSIPPI scale, and measures of violence, suicidality and medical status, paired comparison between abstinent and non-abstinent categories within each SU group showed significant differences with two exceptions. The groups using only sedative/hypnotics and only cocaine at baseline showed no significant abstinence effects, perhaps because these groups had relatively small numbers. Paired comparison was significant for change in the ASI medical score, but abstinent-non-abstinent difference were significant on this measure only for the group that was abstinent at baseline or who used only alcohol.
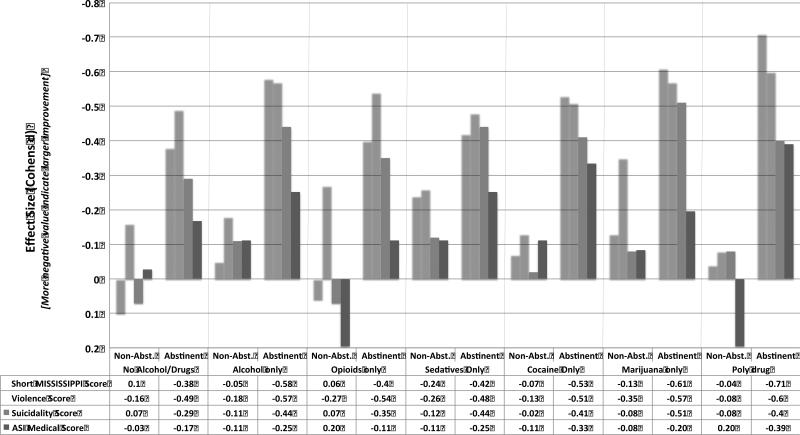
Figure 1 presents a graphic illustration of the improvement in outcomes expressed as effect size (Cohen's d) associated with abstinent and non-abstinent status 4 months after discharge across the SU groups. In general, paired comparison for most outcomes showed substantial improvement with abstinence, most dramatically among the alcohol only and polysubstance groups. Overall the association of abstinence with improvement in each SU group seemed to be statistically stronger than the differences between SU groups.
Figure 1.
Effect size (Cohens d) of PTSD treatment in different substance use groups stratified by abstinence
4. DISCUSSION
This study of Veterans admitted from community settings to specialized intensive residential/inpatient/day treatment PTSD programs in VHA nationally, explored the differences in non-substance abuse clinical outcomes between those who did not report any substance use, five other categories of patients who reported use of a single specific addictive substance and a seventh group who reported polysubstance use in the 30 days prior to admission. We found substantial baseline differences between Veterans in the various substance abuse categories that could potentially confound our analysis of change from baseline to four months after discharge. These variables were thus included as covariates in subsequent analyses. Four months after discharge from treatment, PTSD symptom burden uniformly improved in every SU category with few differences in the magnitude of improvement across these seven groups.
Rates of reported abstinence at 4 months after discharge varied substantially between the groups and, most importantly, abstinence was strongly associated with substantially greater improvement in all outcomes except employment. In contrast, very little change was observed among Veterans who were not abstinent. Notably, the magnitude of the effect of abstinence on PTSD symptom burden improvement was not significantly different across the seven groups. To best of our knowledge this is the first study to explore the differences in outcome with PTSD treatment across different alcohol and drug use categories and to describe the strong association of abstinence with improvement with few differences in abstinence effect across the different groups.
We built upon the previous 2 studies from subsamples of the same database that explored the influence of substance abuse on the clinical outcomes of Veterans with PTSD symptoms severe enough to merit treatment in specialized intensive settings. Fontana et al selected a “pure” subsample of PTSD patients with and without dual diagnosis enrolled between the period between 2003 to 2008 in our data set (n=8,452) using a strict criteria for SU as defined by a clinical diagnosis of SUD and active use of substances in 30 days prior to admission, and unexpectedly showed that PTSD patients with SU had better outcomes than those without SU problems, mainly driven by the decrease of substance use by SU patients (Fontana et al., 2012). In analysis of a specialized subset of Veterans from our dataset composed of those who used marijuana only and randomly selected PTSD patients who never used any substance (n=2,276), Wilkinson et al further showed that abstinence from marijuana use, specifically, was associated with better PTSD outcomes and reduced violence (Wilkinson et al., 2014). Results of the current broader analysis provides an additional layer of information, showing that abstinence at 4 months after discharge from treatment was associated with marked improvement of non-substance use related symptoms, regardless of the specific substance or substances used immediately prior to entering specialized PTSD treatment. While the prior 2 studies used limited specialized data subsets from the same program evaluation effort, we analyzed the entire set of data representing exclusive use of various individual substances, polysubstance use (3 or more substances) and no substance use among community dwelling veterans with severe PTSD who were admitted to the treatment programs (n=22,948). There is thus limited overlap between the data involved in the 3 studies.
Although not the main focus of the study, we also found that achievement of abstinence varied substantially between SU categories, with more socially acceptable, soft drugs like alcohol and cannabis associated with lower rates of abstinence at 4 months and more “deviant” or “illegal” hard drugs like opiates and cocaine showing high levels of abstinence. Marijuana is considered one of the least harmful of substances of abuse (Nutt et al., 2010) and is even considered by some to be helpful in PTSD symptom relief compared to alcohol and other drugs (Bremner et al., 1996; Passie et al., 2012), especially in studies based on self-report judgments from Veterans themselves (Elliott et al., 2015). Probably reflective of this, “marijuana only” users at baseline in our study had the lowest abstinence rate at 4 months. However, marijuana use seems to be associated with similar symptom burden at baseline, and abstinence from marijuana was associated with similar benefit compared to abstaining from alcohol or other substance use. On the other hand, “hard” substances like opioids and cocaine have been reported in previous studies to be associated with poorer outcomes (Cottler et al., 1992; Goldenberg et al., 1995; Nutt et al., 2010). Surprisingly, use of these hard substances was not associated with significantly greater risk for poor outcomes as compared to users of other substances in the present study. The rate of abstinence achievement appeared to be higher among opioid and cocaine users compared to alcohol and marijuana users. A single-site study of Veterans in VA residential treatment for PTSD (marijuana use in 35 of 432 patients before treatment and 59 patients at 4 month follow up) suggested that in contrast to alcohol and cocaine use, marijuana use 4 months after treatment was associated with less improvement of PTSD symptoms (Bonn-Miller et al., 2011). Our larger study, using a far larger national sample, showed limited differences between substance use groups in outcomes 4 months after discharge and particularly that abstinence at 4 months after treatment was associated with markedly better non-substance use outcomes uniformly in all groups with few differences between specific substances used prior to admission. Some prior studies have suggested that with treatment of PTSD in dually diagnosed patients, improvement in PTSD symptom burden precedes reduction in substance use and less evidence that substance use improvement resulted in PTSD improvement (Back et al., 2006; Coffey et al., 2002; Hien et al., 2010b; McCauley et al., 2012; Read et al., 2004). The nature of our study does not allow for such causal conclusions in either direction. The lack of significant improvement in employment outcomes with PTSD treatment may be reflective of the greater age of our sample (predominantly in their 50's), high rates of receipt of disability payments, and high severity and chronicity of PTSD symptoms.
The results of this study lend further support to the assertion that clinicians treating Veterans for PTSD should not be reluctant to treat dually diagnosed Veterans for fear that their substance use will necessarily prove to be an impediment to successful treatment of PTSD symptoms (Foa et al., 2013; Fontana et al., 2012; Kaysen et al., 2014), especially as this study suggests that concurrent reduction of SU comorbidity appears to be notably associated with substantially increased clinical benefits. In addition, previous studies have noted that veterans with PTSD and SUD may themselves prefer an integrative approach to treatment (Back et al., 2014; Brown et al., 1998). In addition, findings from this study, suggest that clinicians may be assured that the outcomes of such treatment may not influenced by the nature of the specific substance used, and can thus have greater confidence in advising patients that abstinence from any specific addictive substances carries a better prognosis for PTSD treatment, violent behavior, suicidality and medical status. PTSD focused psychotherapy interventions are reported to have only modest effects in improving PTSD related symptoms and no effect on substance use outcome in dually diagnosed patients (Roberts et al., 2015). Our data suggests that a focus on reducing the substance use may improve the benefits related to PTSD treatments substantially.
4.1. Limitations
Although the large sample size and multi-site nature of our study renders robustness to our findings, several limitations require comment. Clustering of patients within similar treatment settings could have biased our results. We repeated all the analyses using mixed models with site as a random effect, thus adjusting for the potential correlatedness of data from within sites and minimizing the risk that large sites would unduly dominate the results. The overall results remained the similar on mixed model analysis (data available on request).
Despite the standard intake and evaluation process, variation across sites and providers in diagnostic procedures leave their reliability and consistency unknown. Our study also lacked urine toxicology to confirm substance use. With self-report alone, underreporting of substance use may have occurred due to the expectation of a period of abstinence prior to admission to some programs. However, self reports have been found to have high reliability and validity in substance abuse in general population (Darke, 1998), among dual diagnosis patients (Calhoun et al., 2000), and among veterans with PTSD (Weiss et al., 1998) with only 4-8% of users mis-identified. Moreover, self-reports are often not confirmed by urine toxicology, reflecting the temporal limitations of such measures (Darke, 1998). Under reporting at worst may have diluted our results minimally, but it is unlikely to change the overall conclusions. Because of the observational, non-experimental study design we can only draw conclusions concerning the associations between substance use and PTSD treatment outcomes, and causal relationships, while suggestive, are not conclusive. Length of stay (LOS) of individual patients within programs can be expected to be associated with abstinence. However, data on LOS was not uniformly available at all the sites in our dataset and lack of this data could be a limitation. However, even if LOS data were available, it would be difficult to disentangle the causal relations between LOS and abstinence achievement as they can be expected to go both ways, with abstinence leading to longer LOS and longer LOS leading to greater likelihood of abstinence. Finally, the results of this study may not be generalizable to non-VA settings as the majority of enrollees were older Veterans with long standing history of PTSD and war-zone combat exposure.
4.2. Conclusions and future directions
In conclusion, the specific type of substance used prior to entry into residential treatment among dually diagnosed PTSD patients seems to have only minimal effect on treatment outcomes, whereas attainment of abstinence at 4 months after treatment, irrespective of the addictive substance used, was strongly associated with improvement in PTSD symptom, violent behavior, suicidality, and medical status. Dual diagnosis PTSD patients with comorbid addictive substance use may benefit from more attention to achievement and maintenance of abstinence while engaged in PTSD focused psychotherapies.
*Highlights (for review).
Study pertains to the treatment outcomes of dual diagnosis PTSD patients
Does the type of substance and abstinence achievement influence treatment outcomes?
Type of substance abused was not associated with difference in outcomes
Abstinence achievement from any substance was strongly associated with better outcomes
Non-abstinent patients showed minimal improvement
Acknowledgements
Project supported by VA New England Mental Illness, Research, Education and Clinical Center. Ajay Manhapra supported by VA/OAA Interprofessional Advanced Fellowship in Addiction Treatment, and the Research in Addiction Medicine Scholars (RAMS) Program, R25DA033211 from the National Institute on Drug Abuse
Role of the funding source
No funders had any role in the design of this study, the data analysis or interpretation, the writing of the manuscript, or the decision to submit for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
*Conflict of interest statement
Ajay Manhapra
There are no conflicts of interests to report.
Elina Stefanovics
There are no conflicts of interests to report
Robert Rosenheck
There are no conflicts of interests to report
Contributors
Ajay Manhapra and Robert Rosenheck defined the research questions. Elina Stefanovics conducted the statistical analyses. Ajay Manhapra drafted the manuscript. Robert Rosenheck and Elina Stefanovics reviewed and commented on manuscript drafts.
Conflict of interest
There are no conflicts of interests for any of the authors to report.
All authors have approved the final article.
Ajay Manhapra
Defined research question, reviewed the data, and drafted the manuscript with revisions.
Elina Stefanovics
Conducted the statistical analyses, reviewed the data, and reviewed and commented on manuscript drafts.
Robert Rosenheck
Defined the research questions, reviewed the data, and reviewed and commented on manuscript drafts.
REFERENCES
- Back SE, Brady KT, Sonne SC, Verduin ML. Symptom improvement in co-occurring PTSD and alcohol dependence. J. Nerv. Ment. Dis. 2006;194:690–696. doi: 10.1097/01.nmd.0000235794.12794.8a. [DOI] [PubMed] [Google Scholar]
- Back SE, Killeen TK, Teer AP, Hartwell EE, Federline A, Beylotte F, Cox E. Substance use disorders and PTSD: an exploratory study of treatment preferences among military veterans. Addict. Behav. 2014;39:369–373. doi: 10.1016/j.addbeh.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Boden MT, Vujanovic AA, Drescher KD. Prospective investigation of the impact of cannabis use disorders on posttraumatic stress disorder symptoms among veterans in residential treatment. Psychol. Trauma Theory Res. Pract. Policy. 2013;5:193–200. [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Drescher KD. Cannabis use among military veterans after residential treatment for posttraumatic stress disorder. Psychol. Addict. Behav. 2011;25:485–491. doi: 10.1037/a0021945. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick SM, Darnell A, Charney DS. Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. Am. J. Psychiatry. 1996;153:369–375. doi: 10.1176/ajp.153.3.369. [DOI] [PubMed] [Google Scholar]
- Brown PJ, Stout RL, Gannon-Rowley J. Substance use disorder-PTSD comorbidity. Patients’ perceptions of symptom interplay and treatment issues. J. Subst. Abuse Treat. 1998;15:445–448. doi: 10.1016/s0740-5472(97)00286-9. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Sampson WS, Bosworth HB, Feldman ME, Kirby AC, Hertzberg MA, Wampler TP, Tate-Williams F, Moore SD, Beckham JC. Drug use and validity of substance use self-reports in veterans seeking help for posttraumatic stress disorder. J. Consult. Clin. Psychol. 2000;68:923–927. [PubMed] [Google Scholar]
- Coffey SF, Saladin ME, Drobes DJ, Brady KT, Dansky BS, Kilpatrick DG. Trauma and substance cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug Alcohol Depend. 2002;65:115–127. doi: 10.1016/s0376-8716(01)00157-0. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Compton WM, 3rd, Mager D, Spitznagel EL, Janca A. Posttraumatic stress disorder among substance users from the general population. Am. J. Psychiatry. 1992;149:664–670. doi: 10.1176/ajp.149.5.664. [DOI] [PubMed] [Google Scholar]
- Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. discussion 267-258. [DOI] [PubMed] [Google Scholar]
- Elliott L, Golub A, Bennett A, Guarino H. PTSD and cannabis-related coping among recent veterans in New York City. Contemp. Drug Probl. 2015;42:60–76. doi: 10.1177/0091450915570309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof. Psychol. Res. Pr. 2009;40:532–538. [Google Scholar]
- Foa EB, Yusko DA, McLean CP, Suvak MK, Bux DA, Jr., Oslin D, O'Brien CP, Imms P, Riggs DS, Volpicelli J. Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: a randomized clinical trial. JAMA. 2013;310:488–495. doi: 10.1001/jama.2013.8268. [DOI] [PubMed] [Google Scholar]
- Fontana A, Rosenheck R. A short form of the Mississippi Scale for measuring change in combat-related PTSD. J. Trauma Stress. 1994;7:407–414. doi: 10.1007/BF02102785. [DOI] [PubMed] [Google Scholar]
- Fontana A, Rosenheck R, Desai R. Comparison of treatment outcomes for veterans with posttraumatic stress disorder with and without comorbid substance use/dependence. J. Psychiatr. Res. 2012;46:1008–1014. doi: 10.1016/j.jpsychires.2012.05.004. [DOI] [PubMed] [Google Scholar]
- Goldenberg IM, Mueller T, Fierman EJ, Gordon A, Pratt L, Cox K, Park T, Lavori P, Goisman RM, Keller MB. Specificity of substance use in anxiety-disordered subjects. Compr. Psychiatry. 1995;36:319–328. doi: 10.1016/s0010-440x(95)90112-4. [DOI] [PubMed] [Google Scholar]
- Hien DA, Campbell AN, Ruglass LM, Hu MC, Killeen T. The role of alcohol misuse in PTSD outcomes for women in community treatment: a secondary analysis of NIDA's Women and Trauma Study. Drug Alcohol Depend. 2010a;111:114–119. doi: 10.1016/j.drugalcdep.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Jiang H, Campbell AN, Hu MC, Miele GM, Cohen LR, Brigham GS, Capstick C, Kulaga A, Robinson J, Suarez-Morales L, Nunes EV. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA's Clinical Trials Network. Am. J. Psychiatry. 2010b;167:95–101. doi: 10.1176/appi.ajp.2009.09091261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Schumm J, Pedersen ER, Seim RW, Bedard-Gilligan M, Chard K. Cognitive processing therapy for veterans with comorbid PTSD and alcohol use disorders. Addict. Behav. 2014;39:420–427. doi: 10.1016/j.addbeh.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane TM, Caddell JM, Taylor KL. Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: three studies in reliability and validity. J. Consult. Clin. Psychol. 1988;56:85–90. doi: 10.1037//0022-006x.56.1.85. [DOI] [PubMed] [Google Scholar]
- Kulka RA. Trauma And The Vietnam War Generation: Report Of Findings From The National Vietnam Veterans Readjustment Study. Brunner/Mazel; New York: 1990. [Google Scholar]
- McCauley JL, Killeen T, Gros DF, Brady KT, Back SE. Posttraumatic stress disorder and co-occurring substance use disorders: advances in assessment and treatment. Clin. Psychol. Sci. Pr. 2012;19:283–304. doi: 10.1111/cpsp.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr HL, O'Brien CP. New data from the Addiction Severity Index. Reliability and validity in three centers. J. Nerv. Ment. Dis. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O'BRIEN CP. An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. J. Nerv. Ment. Dis. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–1565. doi: 10.1016/S0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- Passie T, Emrich HM, Karst M, Brandt SD, Halpern JH. Mitigation of posttraumatic stress symptoms by Cannabis resin: a review of the clinical and neurobiological evidence. Drug Testing Anal. 2012;4:649–659. doi: 10.1002/dta.1377. [DOI] [PubMed] [Google Scholar]
- Read JP, Brown PJ, Kahler CW. Substance use and posttraumatic stress disorders: symptom interplay and effects on outcome. Addict. Behav. 2004;29:1665–1672. doi: 10.1016/j.addbeh.2004.02.061. [DOI] [PubMed] [Google Scholar]
- Roberts NP, Roberts PA, Jones N, Bisson JI. Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: a systematic review and meta-analysis. Clin. Pyschol. Rev. 2015;38:25–38. doi: 10.1016/j.cpr.2015.02.007. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Najavits LM, Greenfield SF, Soto JA, Shaw SR, Wyner D. Validity of substance use self-reports in dually diagnosed outpatients. Am. J. Psychiatry. 1998;155:127–128. doi: 10.1176/ajp.155.1.127. [DOI] [PubMed] [Google Scholar]
- Wilkinson ST, Stefanovics E, Rosenheck RA. Marijuana Use is Associated with Worse Outcomes in Symptom Severity and Violent Behavior in Patients with PTSD. 2014 doi: 10.4088/JCP.14m09475. (personal communication, In press) [DOI] [PMC free article] [PubMed] [Google Scholar]