Abstract
We conducted a meta-analysis on the effects of mobile technology on treatment outcome for psychotherapy and other behavioral interventions. Our search of the literature resulted in 26 empirical articles describing 25 clinical trials testing the benefits of smartphone applications, PDAs, or text messaging systems either to supplement treatment or substitute for direct contact with a clinician. Overall, mobile technology use was associated with superior treatment outcome across all study designs and control conditions, ES = .34, p < .0001. For the subset of 10 studies that looked specifically at the added benefit of mobile technology using a rigorous “Treatment” versus “Treatment + Mobile” design, effect sizes were only slightly more modest (ES = .27) and still significant (p < .05). Overall, the results support the role of mobile technology for the delivery of psychotherapy and other behavioral interventions.
Keywords: mobile technology, psychotherapy, treatment outcome, meta-analysis
Technological innovations have been used to deliver and supplement psychotherapy and other behavioral interventions for decades. Phone calls, for example, have been integrated into treatment delivery for anxiety treatment and addictions since at least the 1960s (e.g. Kahn & Baker, 1968; Koumans, Muller, & Miller, 1967). Since the advent of affordable hand-held mobile devices, however, the integration of technology and treatment delivery has become ubiquitous (Jones, 2014). Currently, there is a small but rapidly growing literature describing clinical trials that have been conducted to test the benefits of mobile devices, either as substitutes for regular contact with a clinician (e.g., Bauer, Okon, Meermann, & Kordy, 2012; Watts, et al., 2013) or to supplement face-to-face time with a clinician (e.g., Gustafason, et al., 2014; Oerlemans, van Cranenburgh, Herremans, Spreeuwenberg, & van Dulmen, 2011).
eHealth and mHealth Interventions
Electronic health (eHealth) interventions include internet interventions, video-games, and other computer-based interventions (e.g., Teachman, 2014). Mobile health (mHealth) interventions, in contrast, are a subset of eHealth interventions that involve the use of mobile devices such as personal digital assistants (PDA), text messaging systems, and smartphone applications. mHealth technologies have tremendous potential to augment treatment delivery, particularly to assist in the delivery of skills-based therapies such as cognitive-behavioral treatments. Such approaches are beginning to be used successfully. Palmtop computers have been effectively used to facilitate self-statements, breathing control practice, and exposure exercises, as a supplement to CBT for panic disorder (Kenardy, Dow, Johnston, Newman, Thomson, & Taylor, 2003). PDAs have been used to monitor daily behaviors, mood, and symptom change, provide feedback, and schedule tasks and goals (e.g., Burke et al., 2011; Gentry, Kriner, Sima, McDonough, & Wehman, 2014; Piasecki, Hufford, Solhan, & Trull, 2007). Text messaging systems have been used to increase medication compliance, provide encouragement to practice skills, and remind clients of upcoming sessions. (e.g., de Niet et al., 2012; Louch, Dalking, Bodansky, & Conner, 2013; Whittaker et al., 2011; Ybarra, Holtrop, Prescott, Rahbar, & Strong, 2012). More recently, smartphone apps have been used to administer momentary assessments and diaries, monitor medication use, model effective skill use through video and audio recordings, and provide general diagnostic information. Information collected through smartphone apps is often reviewable by treatment providers. (e.g., Jones, Forehand, McKee, Cuellar, & Kincaid, 2010; Gustafson, McTavish, Chih, Atwood, Johnson, & Boyle, 2014; Kirwan, Vandelanotte, Fenning, & Duncan, 2013; Kristjánsdóttir et al., 2013; Pramana, Parmanto, Kendall, & Silk, 2014). As is evident from these examples, mHealth interventions are changing rapidly with emerging technology.
Related Meta-analyses and Reviews
Few studies have tested the benefits of mobile devices using rigorous research designs. As a result, most reviews of this literature are qualitative. The few meta-analyses and other quantitative reviews include relatively low numbers of articles describing noticeably heterogeneous studies. One of the earlier review articles identified only five studies that tested mobile devices in the context of randomized controlled trials, and zero studies testing the incremental benefit of mobile phones to improve psychotherapy outcome (Boschen, 2009). A meta-analysis (33 studies) on the benefit of pediatric eHealth interventions estimated an overall weighted mean effect size of d = .12, but with slightly larger effects for a subset of 20 studies that included behavioral techniques, d = .35 (Cushing & Steele, 2010). Most of these studies in this meta-analysis, however, involved internet interventions and other computer-based interventions (e.g., CD-ROM) and not the use of mobile technology. A 2011 qualitative review identified eight randomized clinical trials evaluating the effectiveness of mobile devices to enhance the delivery of mental and behavioral health care (Ehrenreich, Righter, Rocke, Dixon, & Himelhoch, 2011). The review concluded that the interventions appeared to be successful but effect sizes were not estimated. The study also highlighted the limited number of rigorous studies that have evaluated interventions for mental health problems using mobile phones, PDAs, or smartphones. Another 2011 review, specific to smartphone apps, reviewed the capabilities and potential benefits of integrating smartphones into the delivery of behavioral healthcare (Luxton, McCann, Bush, Mishkind, & Reger, 2011.) The review did not, however, review actual outcome data or attempt to quantify any benefit. Instead, the review concluded that more studies were needed to evaluate the clinical effectiveness of smartphones to enhance the delivery of behavioral health interventions. A 2013 review, also focusing on smartphone technology, reached similar conclusions (Fiordelli, Diviani, & Schulz, 2013). The review did not include any outcome data on the effectiveness of smartphones to enhance treatment outcome. Rather, the authors noted that while there is no shortage of health-related apps (15,000+ available in app stores), few have been evaluated in terms of outcome. Another study from the same year, described a meta-analysis of 19 text-messaging based clinical trials and estimated an overall weighted mean effect size of d = .33 (Head, Noar, Iannarino, & Harrington, 2013). The study was specific to text-messaging and did not include any studies of PDAs or smartphone apps.
Current Study
In the current study, our aim was to conduct a meta-analysis to estimate the benefits of mobile technology for the delivery of psychotherapy and other behavioral interventions. This meta-analysis differs from prior meta-analyses, described above, in several key ways. First, this meta-analysis focuses exclusively on mobile technologies, including PDAs, texting interventions, and smartphones applications. Second, we chose to examine only clinical trials with at least two groups in order to estimate standardized mean differences at post-treatment. We chose to exclude studies with single-group, pre-post designs which produce significantly inflated effect sizes (e.g., Lindhiem, Higa, Trentacosta, Herschell, & Kolko, 2014). Finally, we coded the studies by research design in order to identify a subset of the most rigorous studies that looked specifically at the added benefit of mobile technology using a rigorous “Treatment” versus “Treatment + Mobile” design.
Method
Procedure
Eligibility criteria
All articles included in this meta-analysis examined the influence of mobile technology on clinical outcome. Inclusion criteria included, 1) a psychotherapy or behavioral intervention outcome study, 2) a clinical trial with at least two groups, 3) at least one group received mobile technology during (or in place of) treatment, 4) written in English or translated into English, and 5) peer review or dissertation.
Study selection
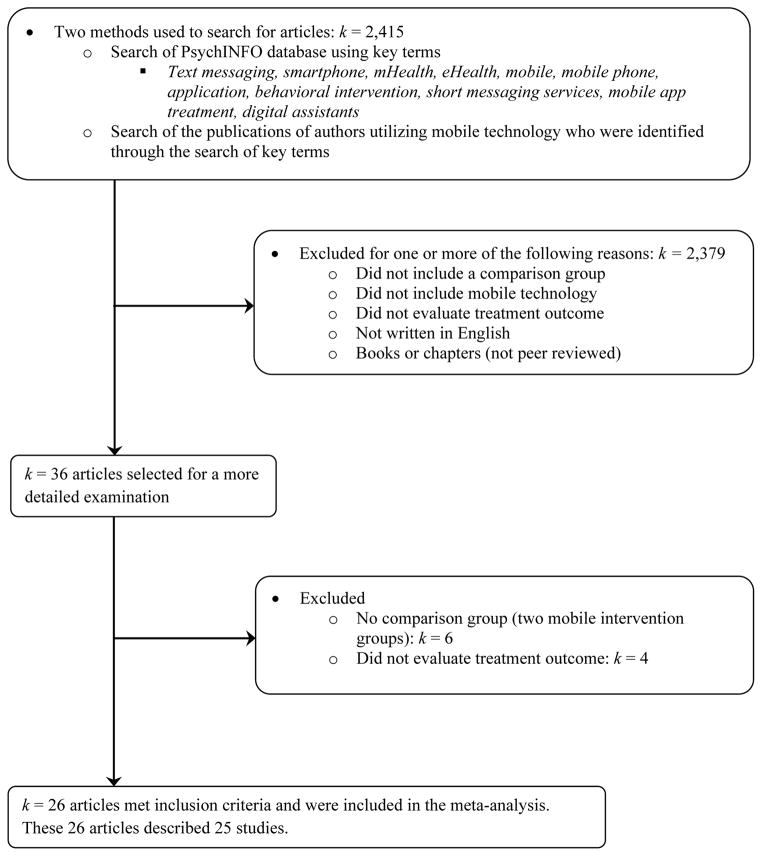
A literature search of the PsycINFO database using the ProQuest search engine was completed on December 8th, 2014. Search terms were text messaging, smartphone, mHealth, eHealth, mobile, mobile phone, application, behavioral intervention, short messaging services, mobile app treatment, and digital assistants. The publications of authors identified through the initial search were then searched for additional articles. These searches yielded 2,415 articles. Articles were excluded for one or more of the following reasons: 1) not evaluating treatment outcome, 2) not including a mobile technology as a supplement or substitute for an intervention, 3) not including a comparison group that did not receive mobile technology, 4) not written in English or translated into English, or 5) not a peer reviewed article or dissertation. Of the 2,415 articles, 36 were examined in greater detail. Ten additional articles were excluded due to not evaluating treatment outcome or not featuring a control group. Overall, 26 articles met inclusion criteria. Two of the articles described the same clinical trial so only one effect size was estimated for this single study. For three studies, the authors were contacted to obtain the statistics needed to calculate the effect sizes. All three authors provided the requested data. In summary, the current meta-analysis included 25 studies (see Figure 1 and Table 1).
Figure 1.
Study selection flow chart.
Table 1.
Description of Studies
| Author | Sample | Diagnosis/Target Problem | Research Design |
|---|---|---|---|
| Askins et al., 2012 | Adults (Mean Age = 36.3 years) | Mothers of Children with Cancer | Problem-Solving Skills Training (PSST) with PDA vs. PSST |
| Bauer et al., 2012 | Adults (Mean Age = 30.0 years) | Eating Disorders | TM treatment vs. TAU |
| Burke et al., 2011 | Adults (Mean Age = 47.0 years) | Obesity/Weight Problems | TAU with PDA vs. TAU |
| de Niet et al., 2012 | Children & Adolescents (Mean Age = 9.9 years) | Obesity/Weight Problems | The Big Friends Club (BFC) treatment with TM vs. BFC. |
| Duncan et al., 2014 | Adults (Mean Age = 44.1 years) | Physical Inactivity and Unhealthy Eating Behaviors | “ManUp” app vs. Educational control |
| Enock, Hofmann, & McNally (2014) | Adults (Mean Age = 34.8 years) | Anxiety | Smartphone app treatment vs. Wait-list |
| Free et al., 2011 | Adults (Mean Age = 36.8 years) | Nicotine Addiction | “txt2stop” TM treatment vs. Attention control |
| Gentry et al., 2014 | Adults (Mean Age = 24.0 years) | Autism | PDA treatment vs. Wait-list |
| Gonzalez et al., 2014 | Children & Adolescents (Age Range = 12–25 years) | Substance Abuse | TM treatment vs. TAU |
| Gustafson et al., 2014 | Adults (Mean Age = 38.3 years) | Alcohol Abuse | TAU with “A-CHESS” app vs. TAU |
| Haug et al., 2013 | Children & Adolescents (Mean Age = 18.2 years) | Nicotine Addiction | “SMS-COACH” TM treatment vs. No treatment |
| Jones et al., 2014 | Children & Adolescents (Mean Age = 5.7 years) | Disruptive Behavior Disorders | Helping the Noncompliant Child (HNC) treatment with app vs. HNC |
| Kirwan et al., 2013 | Adults (Mean Age = 35.2 years) | Type 1 Diabetes | TAU with “Glucose Buddy” app vs. TAU |
| Kristjánsdóttir et al., 2013 | Adults (Mean Age = 44.2 years) | Chronic Pain | Smartphone app treatment vs. No treatment |
| Louch et al., 2013 | Adults (Age Range = 18–30 years) | Type 1 Diabetes | Mobile vs. No Treatment |
| Naughton et al., 2014 | Adults (Mean Age = 41.8 years) | Nicotine Addiction | TAU with “iQuit” TM vs. TAU |
| Oerlemans et al., 2011 | Adults (Mean Age = 38.3 years) | Irritable Bowel Syndrome | TAU with PDA vs. TAU |
| Park et al., 2014 | Adults (Mean Age = 59.2 years) | Heart Disease | TM treatment vs. No treatment |
| Pedersen et al., 2104 | Adults (Age Range = 18–39 years) | Posttraumatic Stress Disorder | PDA treatment vs. No treatment |
| Shapiro et al., 2012 | Adults (Mean Age = 41.9 years) | Obesity/Weight Problems | “Text4Diet” TM treatment vs. No treatment |
| Steinberg et al., 2013 | Adults (Mean Age = 38.3 years) | Obesity/Weight Problems | “Shape Plan” TM treatment vs. Education control |
| Watts et al., 2013 | Adults (Mean Age = 41.0 years) | Depression | “Get Happy Program” App vs. “Sadness Program” treatment |
| Whittaker et al., 2011 | Adults (Mean Age = 27.5 years) | Nicotine Addiction | TM and MMS treatment vs. Attention control |
| Ybarra et al., 2013 | Adults (Mean Age = 21.6 years) | Nicotine Addiction | “Stop My Smoking” TM treatment vs. Attention control |
| Yon et al., 2007 | Adults (Mean Age = 46.8 years) | Obesity/Weight Problems | Behavioral weight loss program with PDA vs. Behavioral weight loss program |
Note. MMS = Multimedia Messaging Service, PDA = Personal Digital Assistant, TAU = Treatment as Usual, TM = Text Messaging
Coding
The following variables were coded:
Sample descriptors: age of sample (adults vs. children and adolescents).
Research design descriptors: Total sample size, treatment group sample size, control group sample size, participant diagnosis (addiction, medical, or psychological), research design (treatment with mobile technology vs. treatment, mobile technology vs. treatment, or mobile technology vs. no treatment), randomization (randomization vs. no randomization), and type of mobile technology (smartphone app, text messaging/short message service, or personal digital assistant).
Standardized mean difference effect sizes (ES) for clinical outcome were calculated according to the procedures outlined in Lipsey and Wilson (2001). All effect sizes were calculated from data collected at post-treatment. When possible, means and standard deviations were used to calculate effect sizes. We use the formulas for calculating Hedges’ g: , where X̄ represents the mean reported for each group, sp is the pooled standard deviation, and n is the number of participants in each condition. Hedges’ g was selected over Cohen’s d as it more accurately estimates effect sizes with small samples. The statistic however, has essentially the same interpretation as Cohen’s d (small = .2; medium = .5; large = .8). When means and standard deviations were unavailable, odds-ratios and F-values were used to calculate effect sizes. Standardized mean difference effect sizes were calculated by using the following formulas: . For four of the studies, failure of randomization yielded groups with baseline scores that were nonequivalent. Consistent with the methodology described in these studies, the effect sizes for these four studies were adjusted to correct for baseline nonequivalence. We examined any outliers which we operationalized as three or more standard deviations from the mean effect size. The current meta-analysis included one outlier, which was “winsorized” to two standard deviations before analyzing the data.
Primary measures, as indicated by the authors, were used to calculate effect sizes. Three studies did not identify a primary measure for clinical outcome. For these studies, we selected a primary outcome measure based on the aims of the study and the psychometrics of each measure. Effect sizes for these three studies were estimated from The Eyberg Child Behavior Inventory (Jones, et al., 2014), Liebowitz Social Anxiety Scale (Enock, Hofmann, & McNally, 2014), and the Body Mass Index (de Niet et al., 2012).
Four studies included three treatment conditions. For these studies, the aims of each study were considered when selecting the most appropriate experimental and control conditions. In addition, groups most similar to the research design codes were selected. Specifically, the monitoring and no monitoring groups (Pedersen, Kaysen, Lindgren, Blayney, & Simpson, 2014), the cognitive bias modification and wait-list groups (Enock, Hofmann, & McNally, 2014), the text messaging and the no text messaging groups (Park, Howie-Esquivel, Chung, & Dracup, 2014), and the personal digital assistant and paper records groups (Burke et al., 2011) were selected for calculating effect sizes. All effect sizes were coded by the second and third authors. The inter-rater agreement was 93%. Discrepancies were resolved through conferencing.
Data Analyses
Analyses were conducted using Lipsey and Wilson’s (2001) macros for SPSS. An aggregate effect sizes was estimated using a random effects model. The Q homogeneity statistic was used to determine whether heterogeneity in effect sizes supported examination of moderators of the overall effect. The Q statistic has a chi-square distribution based on k − 1 degrees of freedom where k represents the number of effect sizes. A homogeneity Q statistic that is statistically significant suggests that the distribution of effect sizes is heterogeneous. We evaluated potential moderator variables individually with the Qbetween statistic using maximum likelihood estimation. A statistically significant Qbetween supports the variable as a moderator of effect size heterogeneity. We examined publication bias using the “fail safe number” based on Orwin’s (1983) formula.
Results
The results of the meta-analysis are summarized in Table 2 and Figure 2. Of the 25 studies, six (24%) involved PDAs, 12 (48%) involved texting interventions, and seven (28%) involved smartphone applications. Twenty-one (84%) of the studies described interventions for adults and four (16%) described interventions for children and adolescents. Seven studies (28%) targeted addictions (e.g., smoking, drinking), 11 (44%) targeted medical/physical conditions (e.g., weight-loss, diabetes), and seven (28%) targeted psychological conditions (e.g., depression, anxiety, PTSD). Ten studies (40%) specifically tested the incremental benefit of mobile technology using a rigorous “Treatment” versus “Treatment + Mobile” design. All but one of the studies used random assignment to treatment condition.
Table 2.
Meta-Analysis of Clinical Outcome
| k | N | d | 95% CI | Q | |
|---|---|---|---|---|---|
| Total | 25 | 8843 | 0.34*** | 0.20 to 0.48 | 125.15*** |
| Age of Sample | 0.20 | ||||
| Adults | 21 | 8090 | 0.33*** | 0.16 to 0.50 | |
| Children & Adolescents | 4 | 753 | 0.43* | 0.03 to 0.83 | |
| Participant Diagnosis | 4.86 | ||||
| Addiction | 7 | 6993 | 0.50*** | 0.26 to 0.73 | |
| Medical | 11 | 1195 | 0.16 | −0.06 to 0.37 | |
| Psychological | 7 | 655 | 0.44** | 0.14 to 0.73 | |
| Study Design | 1.40 | ||||
| Treatment with Mobile vs. Treatment | 10 | 1499 | 0.27* | 0.04 to 0.50 | |
| Mobile vs. Treatment | 4 | 284 | 0.55** | 0.14 to 0.96 | |
| Mobile vs. No Treatment | 11 | 7060 | 0.35** | 0.13 to 0.57 | |
| Randomization | 1.40 | ||||
| Randomized | 24 | 8694 | 0.36*** | 0.21 to 0.51 | |
| Not Randomized | 1 | 149 | - | - | |
| Form of Mobile Intervention | 3.88 | ||||
| Smartphone App | 7 | 943 | 0.57*** | 0.28 to 0.85 | |
| Text Messaging/Short Message Service | 12 | 7211 | 0.31** | 0.11 to 0.53 | |
| Personal Digital Assistant | 6 | 689 | 0.16 | −0.13 to 0.45 |
p < .05;
p <.01;
p < .001
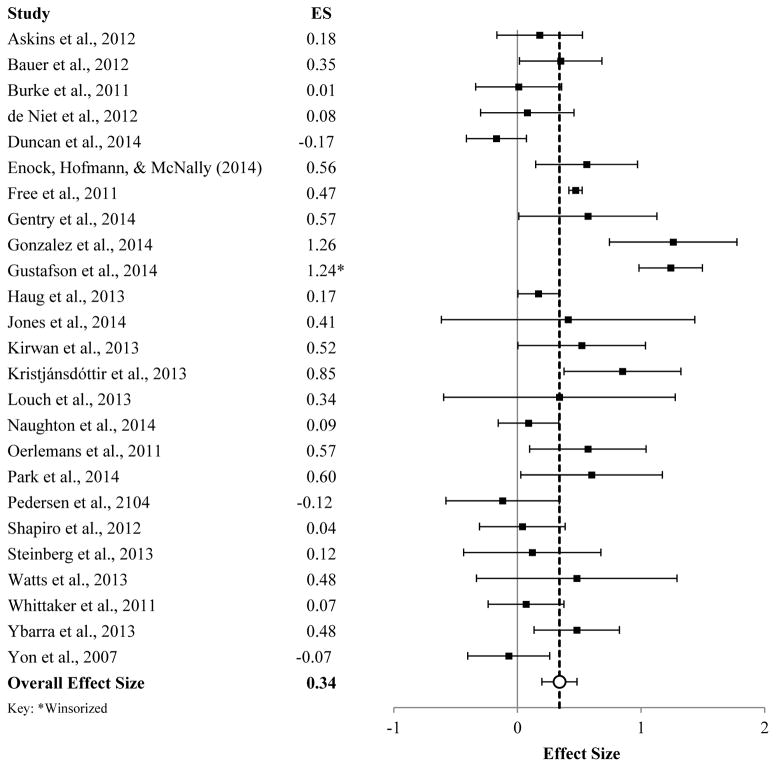
Figure 2.
Effect sizes for clinical outcome. Error bars represent 95% CIs.
Across the 25 independent effect sizes, the aggregate effect size was ES = .34, p < .0001. This falls within the small to medium range based on Cohen’s definitions of “small” (d = .20) and “medium” (d = .50) effect sizes. The homogeneity Q statistic (Q = 125.15, p < .0001) indicated statistically significant variability in the effect sizes between the 25 studies. All but one of the studies used random assignment to treatment condition. The aggregate effect size for these 24 studies was ES = .36, p < .0001. When we examined our study-level variables as potential moderators, none were significant at p < .05. Effect sizes were comparable for studies with children (ES = .43) and adults (ES = .33), between Q = .20, p = .65. Although effect sizes appeared to be substantially smaller for studies of behavioral intervention for medical conditions (ES = .16) than for either treatments for addictions (ES = .50) or psychological disorders (ES = .44), these group differences were not statistically significant, between Q = 4.86, p = .09. Studies using smartphone apps had larger effects effect sizes (ES = .57) than studies using PDAs (ES = .16) or text messaging systems (ES = .31), but these group differences were also not statistically significant, between Q = 3.88, p = .14. As expected, studies specifically testing the additive benefit of mobile technology using a rigorous “Treatment vs. Treatment + Mobile” design had a more modest effect size (ES = .27) relative to studies with other designs, but group differences were again not statistically significant, between Q = 1.40, p = .50. The fail safe N using Orwin’s (1983) formula indicated that 60 additional studies with null findings (ES = .0) would be necessary to reduce the overall aggregate effect size (.34) down to ES = .10.
Discussion
The results of this meta-analysis suggest that mobile technologies benefit the delivery of psychotherapy and other behavioral interventions. Specifically, patients who received mobile technology either to supplement treatment or substitute for direct contact with a clinician experienced better treatment outcome than patients who did not receive any form of mobile technology. These treatment gains remained stable across several potential moderators, including the age of the sample, diagnosis, study design, and the form of mobile technology. These results are consistent with the findings from a meta-analysis that examined the clinical benefit of text-messaging trials (d = .33; Head et al., 2013). Importantly, the results from the current study support the added benefit of mobile technology based on a subset of studies that used a rigorous “Treatment” versus “Treatment + Mobile” design. The results also support the possibility that mobile-only treatments (i.e., treatments that do not include regular, in-session meetings with a clinician) offer better clinical outcome than no treatment at all. Overall, using mobile technology is a promising method of providing mental health treatment to people who would otherwise go untreated.
Clinical Implications
These results support the integration of mHealth technologies into clinical care. Using mobile technology as a supplement may enhance the delivery of treatments. Through the use of digital behavioral diaries, assessments, and messaging, clinicians can utilize mobile devices to observe and interact with their clients in real-world contexts. For example, one study that used text messaging for the treatment of smoking cessation enabled treatment providers to send motivational and behavioral change messages to participants. In addition, participants were able to send text messages during times when they were experiencing cravings for cigarettes (Free et al., 2011). Another study implemented a smartphone app that was designed to supplement treatment for childrens’ behavior problems. The features of the app included video demonstrations of skills, daily surveys, recordings of how families practice skills in their homes, and text messages to remind parents of mid-week updates, home practice, and upcoming sessions and calls (Jones et al., 2014).
Mobile technologies offer tremendous potential to engage with youth, given children and teens’ comfort with technology and the large amount of time they spend interacting with technology (Rideout, Foehr, & Roberts, 2010). Smartphones, in particular, are small and convenient to carry, have become widely available (Smith, 2012), enjoy widespread network coverage, and have extensive computing abilities that allow them to run mHealth applications. mHealth technologies may also help to improve youths’ engagement in treatment by incorporating motivational messages from therapists, providing fun and interactive ways to learn new skills (i.e. games), and incorporating digital rewards to reinforce skill use and practice.
In addition to offering therapeutic benefits, mHealth technologies offer possibilities for overcoming common barriers to psychological and behavioral health treatment. In a study using data collected during the National Comorbidity Survey-Replication (NCS-R) study, a number of barriers that prevented people with a perceived need for treatment from accessing care were identified. Of particular relevance to this meta-analysis, common barriers that were endorsed by respondents included financial limitations and the lack of availability, transportation, and general inconvenience of accessing care (Mojtabai et al., 2011). For individuals in need of treatment, smartphone apps, text messaging, and PDAs can overcome many of these barriers. With about 90% of American adults owning a cell phone and 58% of American adults owning a smartphone (Pew Research Center, 2014), text messaging and app interventions are widely accessible and convenient. For people who are unable to obtain transportation or live in rural areas with limited access to services, mHealth interventions can provide care without the need for transportation or distant commutes to clinic sites. Many of these interventions also do not impose further financial burden on clients, as many people are already paying for their cell phone service.
Potential Mechanisms
The results of this meta-analysis highlight the need to explore possible mechanisms that may explain how mobile technology can provide therapeutic benefits. One clue as to how mHealth technologies improve clinical outcome is the finding that the largest effect sizes were for smartphone app interventions. Common features of behavioral health apps include clinical information (e.g., text, video, and audio files for skills), behavior diaries, discussion boards (digital forums with which app users can communicate with one another), and pop-up reminders (e.g., Gustafson et al., 2014; Jones et al., 2014; Kirwan, et al., 2013; Kristjánsdóttir et al., 2013). Though speculative, these numerous features suggest multiple possible mechanisms for how mobile technology improves clinical outcome.
Increased contact
Mobile technology can increase contact between client and treatment provider. Text messaging can enable clinicians to send messages to clients between sessions (e.g., reminders for upcoming sessions, encouragement to regularly practice skills) while clients can use text messaging as an additional, convenient method for communicating information to their clinician. Though not as widely used as text messaging, some apps feature a HIPAA compliant messaging system with which clients can communicate with treatment providers via messages (e.g., Pramana et al., 2014). These messages, which are accessed and read through a secure online portal, allow clinicians to implement text messaging into treatment without disclosing personal contact information or requiring the possession an additional cell phone service for professional use. Mobile technology provides a convenient method of contact between client and clinician that may supply therapeutic benefits through more frequent encouragement and aid between sessions.
Alarms and reminders
By interacting with the various features of apps frequently, clients receive regular encouragement and reminders to practice skills between sessions. Furthermore, some apps contain an alarm feature that is specifically designed to send reminders and notifications to clients. These apps let clinicians schedule times at which various messages are automatically sent to clients’ mobile phones. The notifications will often alert clients with a vibration, sound, or flashing light. Examples of prompts or reminders include ecological momentary assessment and cues to encourage the frequent practice of skills (e.g., Pramana et al., 2014; Jones et al., 2014). Text messaging can also enable clinicians to schedule and send basic messages to clients. Along with increased contact with the clinician, mobile technology may further improve client engagement throughout the treatment process through the use of alarms and reminders.
Real-time assessment and data collection
When apps include assessments and behavior diaries, clinicians can use these features to identify regular behavior patterns and experiences for each client. This data can be clinically rich and help clinicians generate hypotheses about factors that are facilitating or hindering change. For example, data can be collected on between-session treatment adherence and skills practice. In one study, children with ADHD and their caregivers were provided with PDAs to assess for daily contexts, behaviors, and mood (Whalen, Henker, Ishikawa, et al., 2006; Whalen, Henker, Jamner, et al., 2006). Such a methodology has the potential to provide very rich data about context, stressors, and behaviors that differentiate treatment responders from non-responders outside of treatment sessions. This information can then guide upcoming sessions to address maladaptive behaviors and provide strategies for responding to difficult situations.
Skill acquisitions and utilization
Previous studies have identified the importance of skill acquisition and utilization for positive treatment outcome for behavioral interventions (e.g., Hundt, Mignogna, Underhill, & Cully, 2013; Lindhiem, Higa, Trentacosta, Herschell, & Kolko, 2014). Although increased contact, motivation, prompts, reminders, and real-time assessment and data collection all likely have independent effects, the combination of these mechanisms may have a combined effect by enhancing skill acquisition and skill utilization. Overall, apps may help clients learn and practice skills that promote healthy behaviors, resulting in improved clinical outcome.
Limitations and Future Directions
The greatest limitation of the current meta-analysis is the relatively small number of studies that met inclusion criteria. With only 25 studies, we lacked the power to analyze potential moderators thoroughly. With moderator groups ranging anywhere from one study to 24 studies, no statistically significant differences were detected. Another limitation is that we only examined the effects of mobile technology on treatment outcome at post-treatment. As such, the results of this meta-analysis do not indicate whether or not there are long-term benefits to implementing mobile technology in psychotherapy and other behavior health services. The present study also does not explore the use of mobile technologies as a method for maintaining treatment gains after services have terminated. We hope that the promising results reported in this meta-analysis will encourage the continued development and use of mHealth interventions, which will allow for a more robust analysis of the benefits of mobile technology.
Summary and Conclusions
In a meta-analysis of 25 studies, the use of mobile technology to deliver or supplement treatment was associated with superior treatment outcome across all study designs and control conditions. Overall, the results support the role of mobile technology for the delivery of psychotherapy and other behavioral interventions. Mobile technology could become a common resource for augmenting current clinical practices and overcoming common barriers to treatment. The continued development of mobile health interventions will allow for a more careful examination of moderators and a more thorough understanding of how mobile technology can improve mental health treatment.
Acknowledgments
This study was supported by a grant from the National Institute of Mental Health (NIMH) to the first author (MH 093508).
References
* denotes articles included in the meta-analysis.
- *.Askins MA, Sahler OJZ, Sherman SA, Fairclough DL, Butler RW, Katz ER, Phipps S. Report from a multi-institutional randomized clinical trial examining computer-assisted problem-solving skills training for English- and Spanish-speaking mothers of children with newly diagnosed cancer. Journal of Pediatric Psychology. 2009;34:551–563. doi: 10.1093/jpepsy/jsn124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Bauer S, Okon E, Meermann R, Kordy H. Technology-enhanced maintenance of treatment gains in eating disorders: Efficacy of an intervention delivered via text messaging. Journal of Consulting and Clinical Psychology. 2012;80:700–706. doi: 10.1037/a0028030. [DOI] [PubMed] [Google Scholar]
- Boschen MJ. Mobile telephones and psychotherapy: II. A review of empirical research. The Behavior Therapist. 2009;32(8):175–181. [Google Scholar]
- *.Burke LE, Conroy MB, Sereika SM, Elci OU, Styn MA, Acharya SD, Glanz K. The effect of electronic self-monitoring on weight loss and dietary intake: A randomized behavioral weight loss trial. Obesity. 2011;19:338–344. doi: 10.1038/oby.2010.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cushing CC, Steele RG. A meta-analytic review of eHealth interventions for pediatric health promoting and maintaining behaviors. Journal of Pediatric Psychology. 2010;35:937–949. doi: 10.1093/jpepsy/jsq023. [DOI] [PubMed] [Google Scholar]
- *.de Niet J, Timman R, Bauer S, van den Akker E, de Klerk C, Kordy H, Passchier J. Short message service reduces dropout in childhood obesity treatment: A randomized controlled trial. Health Psychology. 2012;31:797–805. doi: 10.1037/a0027498. [DOI] [PubMed] [Google Scholar]
- *.Duncan M, Vandelanotte C, Kolt GS, Rosenkranz RR, Caperchione CM, George ES, Mummery WK. Effectiveness of a web- and mobile phone-based intervention to promote physical activity and healthy eating in middle-aged males: Randomized controlled trial of the ManUp study. Journal of Medical Internet Research. 2014;16:40–60. doi: 10.2196/jmir.3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrenreich B, Righter B, Rocke DA, Dixon L, Himelhoch S. Are mobile phones and handheld computers being used to enhance delivery of psychiatric treatment? A systematic review. Journal of Nervous and Mental Disease. 2011;199:886–891. doi: 10.1097/NMD.0b013e3182349e90. [DOI] [PubMed] [Google Scholar]
- *.Enock PM, Hofmann SG, McNally RJ. Attention bias modification training via smartphone to reduce social anxiety: A randomized, controlled multi-session experiment. Cognitive Therapy and Research. 2014;38:200–216. doi: 10.1007/s10608-014-9606-z. [DOI] [Google Scholar]
- Fiordelli M, Diviani N, Schulz PJ. Mapping mHealth research: A decade of evolution. Journal of Medical Internet Research. 2013;15:73–86. doi: 10.2196/jmir.2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W, Roberts I. Smoking cessation support delivered via mobile phone text messaging (txt2stop): A single-blind, randomised trial. The Lancet. 2011;378:49–55. doi: 10.1016/S0140-6736(11)60701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Gentry T, Kriner R, Sima A, McDonough J, Wehman P. Reducing the need for personal supports among workers with autism using an iPod touch as an assistive technology: Delayed randomized control trial. Journal of Autism and Developmental Disorders. 2014;45:669–684. doi: 10.1007/s10803-014-2221-8. [DOI] [PubMed] [Google Scholar]
- *.Gonzales R, Ang A, Murphy DA, Glik DC, Anglin MD. Substance use recovery outcomes among a cohort of youth participating in a mobile-based texting aftercare pilot program. Journal of Substance Abuse Treatment. 2014;47:20–26. doi: 10.1016/j.jsat.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Gustafson DH, McTavish FM, Chih M, Atwood AK, Johnson RA, Boyle MG, Shah D. A smartphone application to support recovery from alcoholism: A randomized clinical trial. JAMA Psychiatry. 2014;71:566–572. doi: 10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Haug S, Schaub MP, Venzin V, Meyer C, John U. Efficacy of a text message-based smoking cessation intervention for young people: A cluster randomized controlled trial. Journal of Medical Internet Research. 2013;15:142–155. doi: 10.2196/jmir.2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Head KJ, Noar SM, Iannarino NT, Harrington NG. Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Social Science & Medicine. 2013;97:41–48. doi: 10.1016/j.socscimed.2013.08.003. [DOI] [PubMed] [Google Scholar]
- Hundt NE, Mignogna J, Underhill C, Cully JA. The relationship between use of CBT skills and depression treatment outcome: A theoretical and methodological review of the literature. Behavior Therapy. 2013;44:12–26. doi: 10.1016/j.beth.2012.10.001. [DOI] [PubMed] [Google Scholar]
- Jones DJ. Future directions in the design, development, and investigation of technology as a service delivery vehicle. Journal of Clinical Child and Adolescent Psychology. 2014;43:128–144. doi: 10.1080/15374416.2013.859082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Jones DJ, Forehand R, Cuellar J, Parent J, Honeycutt A, Khavjou O, Newey GA. Technology-enhanced program for child disruptive behavior disorders: Development and pilot randomized control trial. Journal of Clinical Child and Adolescent Psychology. 2014;43:88–101. doi: 10.1080/15374416.2013.822308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones DJ, Forehand R, McKee LG, Cuellar J, Kincaid C. Behavioral parent training: Is there an “app” for that? Behavior Therapist. 2010;33:72–77. [PMC free article] [PubMed] [Google Scholar]
- Kenardy JA, Dow MGT, Johnston DW, Newman MG, Thomson A, Taylor CB. A comparison of delivery methods of cognitive-behavioral therapy for panic disorder: An international multicenter trial. Journal of Consulting and Clinical Psychology. 2003;71:1068–1075. doi: 10.1037/0022-006X.71.6.1068. [DOI] [PubMed] [Google Scholar]
- *.Kirwan M, Vandelanotte C, Fenning A, Duncan MJ. Diabetes self-management smartphone application for adults with type 1 diabetes: Randomized controlled trial. Journal of Medical Internet Research. 2013;15:53–66. doi: 10.2196/jmir.2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kristjánsdóttir ÓB, Fors EA, Eide E, Finset A, Stensrud TL, van Dulmen S, Eide H. A smartphone-based intervention with diaries and therapist-feedback to reduce catastrophizing and increase functioning in women with chronic widespread pain: Randomized controlled trial. Journal of Medical Internet Research. 2013;15:125–146. doi: 10.2196/jmir.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindhiem O, Higa J, Trentacosta CJ, Herschell AD, Kolko DJ. Skill acquisition and utilization during evidence-based psychosocial treatments for childhood disruptive behavior problems: A review and meta-analysis. Clinical Child and Family Psychology Review. 2014;17:41–66. doi: 10.1007/s10567-013-0136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- *.Louch G, Dalkin S, Bodansky J, Conner M. An exploratory randomised controlled trial using short messaging service to facilitate insulin administration in young adults with type 1 diabetes. Psychology, Health & Medicine. 2013;18:166–174. doi: 10.1080/13548506.2012.689841. [DOI] [PubMed] [Google Scholar]
- Lindhiem O, Higa J, Trentacosta CJ, Herschell AD, Kolko DJ. Skill acquisition and utilization during evidence-based psychosocial treatments for childhood disruptive behavior problems: A review and meta-analysis. Clinical Child and Family Psychology Review. 2014;17:41–66. doi: 10.1007/s10567-013-0136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luxton DD, McCann RA, Bush NE, Mishkind MC, Reger GM. mHealth for mental health: Integrating smartphone technology in behavioral healthcare. Professional Psychology: Research and Practice. 2011;42:505–512. doi: 10.1037/a0024485. [DOI] [Google Scholar]
- Mojtabai R, Olfson M, Sampson NA, Jin R, Druss B, Wang PS, Kessler RC. Barriers to mental health treatment: Results from the national comorbidity survey replication. Psychological Medicine. 2011;41:1751–1761. doi: 10.1017/S0033291710002291. http://dx.doi.org/10.1017/S0033291710002291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Advisory Mental Health Council, Workgroup on Services and Clinical Epidemiology Research. The road ahead: Research partnerships to transform services. Washington, D.C: National Institute of Mental Health; 2006. [Google Scholar]
- *.Naughton F, Jamison J, Boase S, Sloan M, Gilbert H, Prevost AT, Sutton S. Randomized controlled trial to assess the short-term effectiveness of tailored web- and text-based facilitation of smoking cessation in primary care (iQuit in practice) Addiction. 2014;109:1184–1193. doi: 10.1111/add.12556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Oerlemans S, van Cranenburgh O, Herremans P, Spreeuwenberg P, van Dulmen S. Intervening on cognitions and behavior in irritable bowel syndrome: A feasibility trial using PDAs. Journal of Psychosomatic Research. 2011;70:267–277. doi: 10.1016/j.jpsychores.2010.09.018. [DOI] [PubMed] [Google Scholar]
- Orwin RG. A fail-safe N for effect size in meta-analysis. Journal of Educational Statistics. 1983;8:157–159. [Google Scholar]
- *.Park LG, Howie-Esquivel J, Chung ML, Dracup K. A text messaging intervention to promote medication adherence for patients with coronary heart disease: A randomized controlled trial. Patient Education and Counseling. 2014;94:261–268. doi: 10.1016/j.pec.2013.10.027. [DOI] [PubMed] [Google Scholar]
- Pramana G, Parmanto B, Kendall PC, Silk JS. The SmartCAT: An m-Health platform for ecological momentary intervention in child anxiety treatment. Telemedicine and e-Health. 2014;20:419–427. doi: 10.1089/tmj.2013.0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Pedersen ER, Kaysen DL, Lindgren KP, Blayney J, Simpson TL. Impact of daily assessments on distress and PTSD symptoms in trauma-exposed women. Journal of Interpersonal Violence. 2014;29:824–845. doi: 10.1177/0886260513505705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. Mobile technology fact sheet. 2014 Retrieved from http://www.pewinternet.org/fact-sheets/mobile-technology-fact-sheet/
- Piasecki TM, Hufford MR, Solhan M, Trull TJ. Assessing clients in their natural environments with electronic diaries: Rationale, benefits, limitations, and barriers. Psychological Assessment. 2007;19:25–43. doi: 10.1037/1040-3590.19.1.25. [DOI] [PubMed] [Google Scholar]
- Rideout VJ, Foehr UG, Roberts DF. Generation M2: Media in the lives of 8- to 18-year-olds. Menlo Park, California: Henry J. Kaiser Family Foundation; 2010. [Google Scholar]
- *.Shapiro JR, Koro T, Doran N, Thompson S, Sallis JF, Calfas K, Patrick K. Text4Diet: A randomized controlled study using text messaging for weight loss behaviors. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2012;55:412–417. doi: 10.1016/j.ypmed.2012.08.011. [DOI] [PubMed] [Google Scholar]
- Smith A. Cell Internet Use 2012. 2012 Retrieved from Pew Research Center’s Internet & American Life Project website: http://www.pewinternet.org/2012/06/26/cell-internet-use-2012/
- *.Steinberg DM, Levine EL, Askew S, Foley P, Bennett GG. Daily text messaging for weight control among racial and ethnic minority women: Randomized controlled pilot study. Journal of Medical Internet Research. 2013;15:67–77. doi: 10.2196/jmir.2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teachman BA. No appointment necessary: Treating mental illness outside the therapist’s office. Perspectives on Psychological Science. 2014;9:85–87. doi: 10.1177/1745691613512659. [DOI] [PubMed] [Google Scholar]
- *.Watts S, Mackenzie A, Thomas C, Griskaitis A, Mewton L, Williams A, Andrews G. CBT for depression: A pilot RCT comparing mobile phone vs. computer. BMC Psychiatry. 2013;13 doi: 10.1186/1471-244X-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whalen CK, Henker B, Ishikawa SS, Jamner LD, Floro JN, Johnston JA, Swindle R. An electronic diary study of contextual triggers and ADHD: Get ready, get set, get mad. American Academy of Child and Adolescent Psychiatry. 2006;45:166–174. doi: 10.1097/01.chi.0000189057.67902.10. [DOI] [PubMed] [Google Scholar]
- Whalen CK, Henker B, Jamner LD, Ishikawa SS, Floro JN, Swindle R, Johnston JA. Toward mapping daily challenges of living with ADHD: Maternal and child perspectives using electronic diaries. Journal of Abnormal Child Psychology. 2006;34:115–130. doi: 10.1007/s10802-005-9008-5. [DOI] [PubMed] [Google Scholar]
- *.Whittaker R, Dorey E, Bramley D, Bullen C, Denny S, Elley CR, Salmon P. A theory-based video messaging mobile phone intervention for smoking cessation: Randomized control trial. Journal of Medical Internet Research. 2011;13:61–72. doi: 10.2196/jmir.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ybarra ML, Holtrop JS, Prescott TL, Rahbar MH, Strong D. Pilot RCT results of Stop My Smoking USA: A text messaging–based smoking cessation program for young adults. Nicotine & Tobacco Research. 2013;15:1388–1399. doi: 10.1093/ntr/nts339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Yon BA, Johnson RK, Harvey-Berino J, Gold BC, Howard AB. Personal digital assistants are comparable to traditional diaries for dietary self-monitoring during a weight loss program. Journal of Behavioral Medicine. 2007;30:165–175. doi: 10.1007/s10865-006-9092-1. [DOI] [PubMed] [Google Scholar]