Abstract
Background
The purpose of this study was to evaluate the efficacy of buspirone, a partial 5-HT1A agonist, for treatment of cannabis dependence.
Methods
One hundred seventy-five cannabis-dependent adults were randomized to receive either up to 60 mg/day of buspirone (n=88) or placebo (n=87) for twelve weeks combined with a brief motivational enhancement therapy intervention and contingency management to encourage study retention. Cannabis use outcomes were assessed via weekly urine cannabinoid tests; secondary outcomes included cannabis craving, cannabis withdrawal symptoms, and clinician ratings of symptom severity.
Results
Participants in both groups reported reduced cannabis craving over the course of the study; however, buspirone provided no advantage over placebo in reducing cannabis use. Significant gender by treatment interaction were observed, with women randomized to buspirone having fewer negative urine cannabinoid tests than women randomized to placebo (p=0.007), and men randomized to buspirone having significantly lower creatinine adjusted cannabinoid levels as compared to those randomized to placebo (p=0.023). An evaluation of serotonin allelic variations did not find an association with buspirone treatment response.
Conclusions
Buspirone was not more efficacious than placebo in reducing cannabis use. Important gender differences were noted, with women having worse cannabis use outcomes with buspirone treatment. Considerations for future medication trials in this challenging population are discussed.
Keywords: cannabis, motivational enhancement therapy, buspirone, contingency management, gender differences
1. Introduction
The 2013 National Survey on Drug Use and Health indicates that more than 114.7 million Americans 12 years of age or older have tried cannabis at least once in their lifetime and almost 32.9 million have used cannabis in the past year (SAMHSA, 2014). It is estimated that approximately 10% of individuals who ever use cannabis become daily users, and lifetime prevalence rates of cannabis dependence have been estimated at 1-4% of the population (Anthony et al., 1994; Anthony and Helzer, 1991; Stinson et al., 2006). In 2013, nearly one million Americans received treatment for cannabis-related problems (SAMHSA, 2014). Although a high demand for effective interventions exists, few specific treatments have been developed for cannabis use disorders. Further, the treatments that have been examined have limited efficacy, with few individuals achieving abstinence (Compton and Pringle, 2004; Kadden et al., 2007; McRae et al., 2003; Nordstrom and Levin, 2007; Vandrey and Haney, 2009). As such, there is significant interest in exploring new strategies to improve treatment outcomes. In particular, the role that medications may play in the treatment of cannabis use disorders has become an active area of research (Levin et al., 2011; Gray et al., 2012; Mason et al., 2012).
Serotonin (5-HT) is implicated in a variety of neuropsychiatric behaviors, and a growing body of evidence implicates cannabinoid interactions with the serotonin neurotransmitter system. Serotonin release is diminished by cannabinoid receptor agonists (Nakazi et al, 2000); conversely, cannabinoid antagonists stimulate 5-HT release (Darmani et al, 2003). The anxiolytic and antidepressant effects of cannabidiol, a major component of cannabis, have been shown to be mediated by 5-HT1A receptors (Gomes et al, 2011; Zanelati et al, 2010). Administration of a synthetic cannabinoid agonist decreases both pre- and post-synaptic 5-HT1A receptor activity (Hill et al., 2006). Fluoxetine, a serotonin reuptake inhibitor, likely modulates CB1 receptor-mediated inhibition of adenyl cyclase through 5-HT1A receptor-dependent mechanisms (Mato et al, 2010). These findings support that serotonergic medications, and particularly those with activity at the 5-HT1A receptor, may have promise in the treatment of cannabis dependence.
Further, functional polymorphisms of the 5-HT1A receptor may be involved in response to treatment, and, as such, a patient's genotype may serve as a biomarker for treatment outcomes. David et al (2008) studied three major serotonin-related polymorphisms and identified the (-1019) SNP as a major variant. Genotyping of 792 subjects (58% female) identified the CC, CG, and GG allelic variants with a frequency of 23%, 50%, and 27%, respectively. Of clinical relevance, previous reports have identified that the HTR1A-1019G allele is associated with decreased transcriptional efficiency, and have also shown an association with major depression and suicide (Lemonde et al, 2003). Boldrini et al (2008) found an increase in 5-HT1A autoreceptors in postmortem brain samples of depressed suicide patients compared with normal controls. In addition, PET analyses have found decreased 5-HT1A binding potential in depressed patients compared to controls (Drevets et al, 2007). A review of studies of the association of C(-1019)G polymorphism with treatment response to SSRIs or antipsychotics found positive associations in 6 reports (Le Francois et al, 2008). Therefore, as chronic cannabis use has been shown to affect 5-HT neurotransmission and alters 5-HT1A activity and the C(-1019)G variant has been associated with depression and response to treatment, genotyping of the 5-HT1A C(-1019)G variant may provide valuable insight into treatment of cannabis-related disorders.
Buspirone, a partial 5-HT1A agonist, is a nonbenzodiazepine anxiolytic that has little or no abuse potential (Lader et al, 1991). Given this activity, buspirone could be a potential medication candidate for treatment of cannabis use disorders. Further, the anxiolytic effects of buspirone may be helpful in preventing relapse to cannabis use, as high anxiety scores have been correlated with increased cannabis withdrawal (Budney et al., 1999), anxiety has been shown to be related to use of cannabis to cope with negative affect (Buckner et al., 2007; Zvolensky et al., 2009), and reduction in anxiety has been associated with reductions in cannabis use (Buckner and Carroll, 2010). In a pilot study in cannabis-dependent individuals, buspirone reduced the percentage of positive urine cannabinoid tests (UCTs) among treatment completers, and a trend was observed for a lower percentage of positive UCTs in the entire sample (McRae-Clark et al, 2009). The purpose of this study was to further explore these promising preliminary findings and the impact of serotonin allelic variation on buspirone treatment response in a larger clinical trial.
2. Material and Methods
This study was a 12-week, double-blind, placebo-controlled trial (NCT00875836) of a flexible dose of buspirone (up to 60 mg/day) in cannabis-dependent individuals conducted between November, 2009 and March, 2014. Participants were primarily recruited through media and internet advertisements. All procedures were conducted in accordance with Good Clinical Practice Guidelines and the Declaration of Helsinki and received approval from the Medical University of South Carolina Institutional Review Board. All participants gave written, informed consent prior to study participation.
Eligible participants were between 18 and 65 years of age and meet DSM-IV criteria for current cannabis dependence. Exclusion criteria included current dependence on any other substance (with the exception of caffeine and nicotine), history of psychotic, bipolar or eating disorder, current suicidal or homicidal risk, current major depression, current treatment with psychoactive medication (with the exception of stimulants and non-benzodiazepine sedative/hypnotics), major medical illness or disease, significant cognitive impairment, hypersensitivity to buspirone or other product component, current consumption of substances that inhibit or induce CYP3A4, and pregnancy, lactation or inadequate birth control. All potential participants received an evaluation for medical exclusions. The medical evaluation included a medical history, routine physical examination, blood chemistries, urine drug screen, and urine pregnancy test if indicated.
The Structured Clinical Interview for DSM-IV (SCID-IV) (First, et al., 2002) was used to assess for psychiatric exclusions. Self-report cannabis use for the 90 days prior to study entry was estimated using the Time-Line Follow-Back (TLFB; Sobell and Sobell, 1978). Levels of cannabis craving were assessed at screening and weekly using the Marijuana Craving Questionnaire (Heishman et al., 2001). The Hamilton Anxiety Scale (HAM-A; Hamilton, 1959) and was administered at screening and weeks 1, 3, 4, 6, 8, and 12. Semi-quantitative UCTs were administered at screening and weekly throughout the study. UCTs were performed using the AXSSYM® system from Abbott Laboratories.
Both groups received adjunctive motivational enhancement therapy sessions (MET) during the first four weeks of the treatment period. Participants completed a series of initial worksheets (Steinberg et al., 2005) from which personalized feedback reports (PFRs) were prepared. These PFRs were used to initiate session discussion regarding participants' frequency of cannabis use, problems related to use, reasons for quitting use, high risk situations for continued or future use, and short and long-term goals related to reduction of use. The first MET session occurred prior to medication initiation and a second session occurred approximately one week later; a third session occurred at week 4.
Stratified randomization (Stout et al., 1994) was used to determine treatment assignment. The stratified randomization variables used were gender and amount of daily cannabis use (less than one joint or one joint and above). Buspirone and placebo tablets were packaged in identical opaque gelatin capsules with lactose, as well as riboflavin powder to allow for compliance monitoring. Medication dosage was initiated at 5 mg buspirone or placebo twice daily and increased by 5-10 mg every three to four days as tolerated, to a maximum dose of 60 mg daily. Medication side effects were evaluated weekly by a clinician by asking the participant open-ended questions such as “Have you had any problems or side effects since we saw you last (such as cold, flu, nausea, headache, or any other problem)?” The type of adverse event, severity of adverse event, relationship to study medication, action taken, and outcome were recorded. In addition to urine riboflavin measurement, compliance was also reviewed weekly using participant report and pill count.
Participants received nominal weekly compensation for returned medication diaries, pill bottles, and unused pills ($10). In order to improve study retention, contingency management (CM) was used to reward weekly visit attendance. Participants received an escalating cash incentive starting at $5 and increasing by $5 each week, beginning at week 1, with any missed weekly visit resulting in a reset of the cash incentive to $5. In addition, participants received cash bonuses for completing week 1 ($20) and week 12 ($40). A 12 week study period was chosen given the delayed onset of action of buspirone (i.e., a lag time of up to two weeks) in treatment of anxiety disorders (Goa and Ward, 1986).
2.1. Statistical Analysis
The primary hypothesis was that participants randomized to receive buspirone would have increased odds of submitting negative weekly UCTs during study treatment as compared to those randomized to placebo. An intent-to-treat approach including all randomized participants was used as the primary analysis (3 participants are missing genotype data and are not in genotype analysis). In the intent-to-treat analysis, those lost to follow-up or missing study data were coded as having positive UCTs at all missing visits.
The study was powered to detect a 29% rate of negative UCTs in participants receiving buspirone, compared with 11% in participants receiving placebo. These estimates were derived from our prior pilot trial of buspirone (McRae et al., 2009) targeting cannabis dependence. Setting the type I error rate to 0.05, a sample of 88 participants per treatment group was deemed necessary to yield 90% power to detect this effect after accounting for a 20% study attrition rate.
Standard descriptive statistics were used to summarize baseline demographic and clinical data. A Wilcoxon Rank sum test was used to evaluate continuous measures between treatment groups while the normal Pearson Chi-Square test was used to assess the relationship for categorical and ordinal variables (Fisher's exact test was used where appropriate). The efficacy of buspirone versus placebo on abstinence (defined as a negative UCT) from cannabis was analyzed over the 12-week treatment period. A repeated measures logistic regression model using the methods of generalized estimating equations (Zeger and Liang, 1986) was applied to assess the overall effect of buspirone on UCT results during active treatment. Working correlation structures were independently compared and the final model structure was chosen using the quasi-likelihood under the independence model criterion statistic (Pan, 2001). Similarly, creatinine adjusted cannabinoid levels were examined during treatment between groups using a linear mixed effects model. Cannabinoid levels were measured weekly and adjusted for concurrently measured creatinine levels. Due to non-normality of model residuals, cannabinoid-creatinine ratios were natural logarithm transformed. Treatment efficacy models were expanded to assess the effect of 5-HT1A receptor polymorphism on treatment response to buspirone; primarily tested was the effect of the functionally deficient C(-1019)G polymorphism in the promoter region of the human 5-HT1A receptor gene.
Additionally, a pre-planned logistic regression model was used to analyze the odds of a negative UCT at the end of the treatment phase of the study (Week 12 study visit) using the intent-to-treat sample (n=175). Mixed effect regression models were used to assess the longitudinal effect of buspirone treatment on craving (as measured by the MCQ). Design adjusted study models contained randomized treatment assignment and study visit. Baseline demographic and clinical characteristics were independently tested for association with efficacy outcome and those that may be associated were included as initial predictors (p<0.10) in covariate adjusted models.
All statistical analyses were conducted using SAS version 9.3 (SAS Institute Inc. Cary, NC, USA). Results from categorical outcomes are presented as odds ratios/hazard ratios with 95% confidence intervals (CI) while results from continuous outcomes are presented as means and associated standard errors as well as mean group differences. Significance was set at a 2-sided p-value of 0.05.
3. Results
3.1. Enrollment and Baseline Data
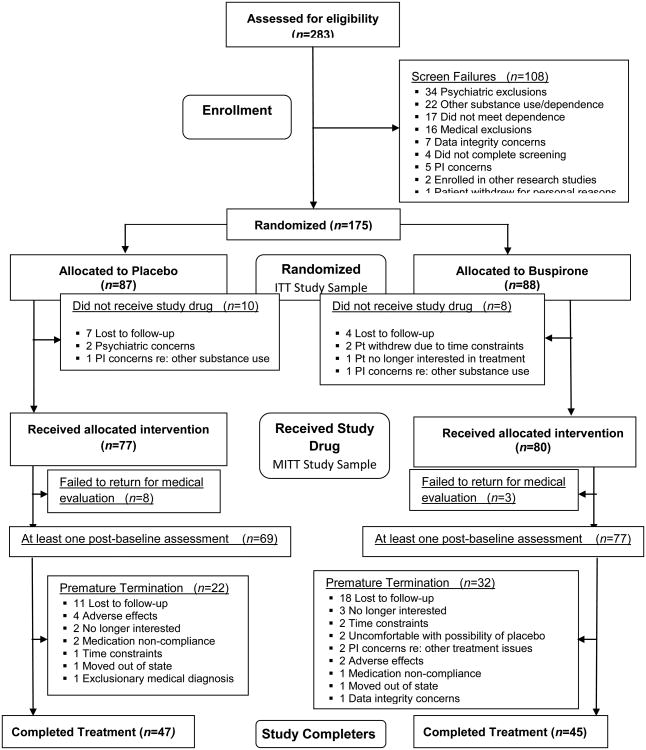
Participants were enrolled between December, 2009 and March, 2014. Two hundred eighty-three individuals were assessed for eligibility, and one hundred eight (38%) were excluded (Figure 1). Demographic and baseline characteristics for randomized participants are presented in Table 1. The randomized participants (n=175) were on average 24 years old (95% CI: 23.1-25.0), were predominately male (n=134, 77%) and Caucasian (n=112, 64%). There were no significant between-group differences in demographics, baseline clinical measures, or cannabis use variables. There was a moderately higher proportion of participants with negative UCTs at baseline in the group randomized to receive buspirone as compared to those randomized to receive placebo (n=8, 9.1% vs. n=2, 2.3%, p=0.053). In the analysis of the association between baseline demographic and clinical characteristics with study abstinence, the reported average cannabis use sessions per day and the average reported number of joints/bowls per day were associated with study outcomes. Participants with an increased number of sessions per day and joints smoked per day prior to study entry were less likely to achieve point prevalence abstinence during the treatment phase of the study [χ21=10.5, p<0.01 and χ21=3.5, p=0.06, respectively]. Additionally, the proportion of days using in the 90 days prior to study entry (via TLFB) was associated with decreased odds of abstinence during the study [χ21=9.7, p<0.01]. Thus, covariate adjusted models contain baseline UCT results, percentage of using days prior to study entry, and baseline sessions of cannabis use per day.
Figure 1. CONSORT Table.
Table 1.
Demographics and clinical characteristics.
| Variable | Overall N=175 | Buspirone N=88 | Placebo N=87 | P Value |
|---|---|---|---|---|
| Demographics and Clinical | ||||
| Characteristics | ||||
| Age | 24.0 (23.1-25.0) | 24.0 (22.7-25.3) | 24.0 (22.6-25.4) | 0.717 |
| Male | 76.6 (134) | 76.1 (67) | 77.0 (67) | 0.891 |
| Caucasian | 64.0 (112) | 65.9 (58) | 62.1 (54) | 0.597 |
| HS Graduate | 90.3 (158) | 89.8 (79) | 90.8 (79) | 0.818 |
| HAM-A | 3.0 (2.5-3.5) | 2.9 (2.3-3.5) | 3.1 (2.4-3.9) | 0.969 |
| 5-HT1A Variant*1 | 0.522 | |||
| C/C | 22.7 (39) | 25.6 (22) | 19.8 (17) | |
| C/G | 49.4 (85) | 45.4 (39) | 53.5 (46) | |
| G/G | 27.9 (48) | 29.1 (25) | 26.7 (23) | |
| 5-HT1A Allele Frequency* | 0.746 | |||
| C Allele | 0.47 (163) | 0.48 (83) | 0.47 (80) | |
| G Allele | 0.53 (181) | 0.52 (89) | 0.53 (92) | |
| Cannabis Use | ||||
| Characteristics | ||||
| Age of Dependence Onset | 19.8 (19.1-20.5) | 19.6 (18.8-20.5) | 20.0 (18.9-21.2) | 0.857 |
| Percent of days Using | 85.2 (82.5-87.8) | 85.0 (81.3-88.8) | 85.3 (81.6-89.1) | 0.964 |
| Sessions Per Day | 3.2 (2.8-3.5) | 2.9 (2.6-3.3) | 3.4 (2.8-3.9) | 0.477 |
| Joints/bowls Per Day | 3.8 (3.5-4.2) | 3.8 (3.3-4.3) | 3.9 (3.3-4.5) | 0.726 |
| MCQ Total Score | 46.1 (43.9-48.3) | 46.4 (43.0-49.9) | 45.8 (42.8-48.7) | 0.777 |
| MCQ Compulsivity Score | 7.9 (7.3-8.6) | 7.8 (7.0-8.7) | 8.1 (7.1-9.0) | 0.817 |
| MCQ Emotionality Score | 10.8 (10.1-11.5) | 11.0 (9.9-12.1) | 10.6 (9.6-11.5) | 0.741 |
| MCQ Expectancy Score | 13.2 (12.5-13.9) | 13.6 (12.6-14.7) | 12.7 (11.8-13.6) | 0.102 |
| MCQ Purposefulness Score | 14.1 (13.3-14.8) | 14.0 (12.9-15.1) | 14.1 (13.1-15.2) | 0.874 |
Continuous characteristics are noted as Mean and associated 95% confidence interval and categorical Characteristics are noted as % (n).
Data available on 172 participants (86 Buspirone and 86 Placebo).
χ21=0.013; p=0.91 for study population consistent with Hardy-Weinberg equilibrium.
3.2. Primary Efficacy Results
The proportion of negative UCTs in the buspirone and placebo groups at each visit is shown in Figure 2a (Intent-to-treat data). The overall proportion of negative weekly UCT was 7.2% (n=76/1056) in the buspirone group and 6.4% (n=64/1044) in the placebo group. A total of 20.6% (36/175) of the randomized participants had at least one negative UCT during the treatment portion of the study. There was no difference in this proportion between the buspirone and placebo groups [Buspirone: 21.6%, n=19 vs. Placebo 19.5%, n=17; χ21=0.1, p=0.74]. In the design adjusted analysis model, there was no significant effect of buspirone on the proportion of negative weekly UCTs [OR (95% CI)=1.09 (0.45-2.61), χ21=0.03, p=0.86] nor was there any differential response over time [Treatment × Visit; χ211=10.4, p=0.49]. In the covariate adjusted models, the treatment effect of buspirone on abstinence from cannabis remained insignificant [OR=0.75 (0.29-1.92), χ21=0.37, p=0.54]. In addition to the intent-to-treat analysis, a sensitivity analysis was performed to examine the effects of attrition and missed study visits imputation methods on study parameter estimates (Table 2). In the two analysis models using imputed data sets (ITT and modified ITT), parameter estimates and confidence intervals were stable across methods. In the two analysis models using data sets with available data (all available and study completers), parameter estimates and confidence intervals were also consistent across methods.
Figure 2.
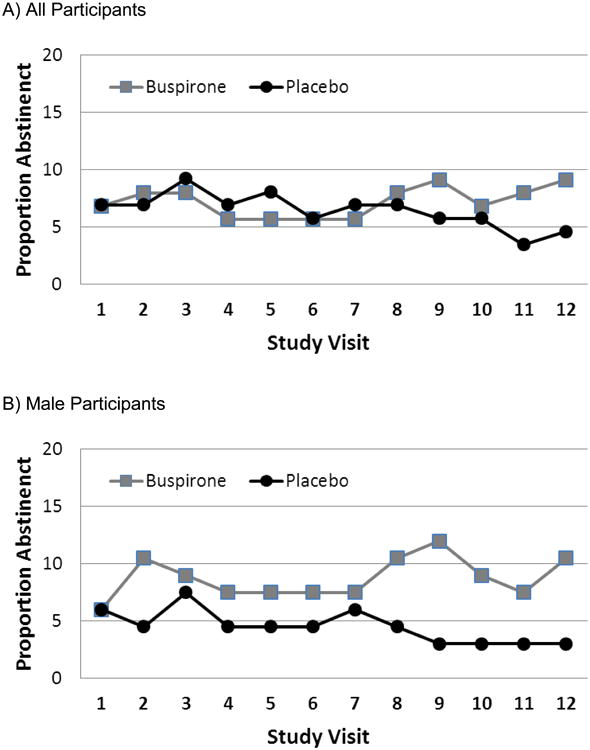
Proportion of randomized participants with negative weekly UCT by treatment assignment for A) all participants B) Male and C) Female participants. Results are shown from the intent to treat (ITT; n=175) data analysis sample (134 Males and 41 Females)
Table 2.
Sensitivity analysis of analytic methods.
| Results | Study Sample | |||
|---|---|---|---|---|
|
| ||||
| Intent to Treat N=175 | Modified Intent to Treat N=157 | Available Data N=143 | Completers N=88 | |
| Statistics | ||||
| OR (95% CI) | 1.09 (0.45-2.61) | 1.06 (0.44-2.54) | 1.11 (0.46-2.65) | 1.66 (0.59-4.64) |
| χ21 | 0.03 | 0.01 | 0.05 | 0.94 |
| P Value | 0.855 | 0.903 | 0.823 | 0.333 |
| % Neg UDS | ||||
| Busprirone | 7.2% (76/1056) | 7.9% (76/960) | 12.2% (76/622) | 13.2% (70/530) |
| Placebo | 6.4% (67/1044) | 7.3% (67/924) | 11.0% (67/607) | 9.9% (49/494) |
Intent to treat analysis: Analysis of all randomized participants. Modified intent to treat analysis: Analysis of ITT sample including only those that received study medication. Available data analysis: Analysis using only available, non-missing data. Completer analysis: Analysis of available data on participants who completed the week 12 study visit. Statistical results are shown from the design adjusted models.
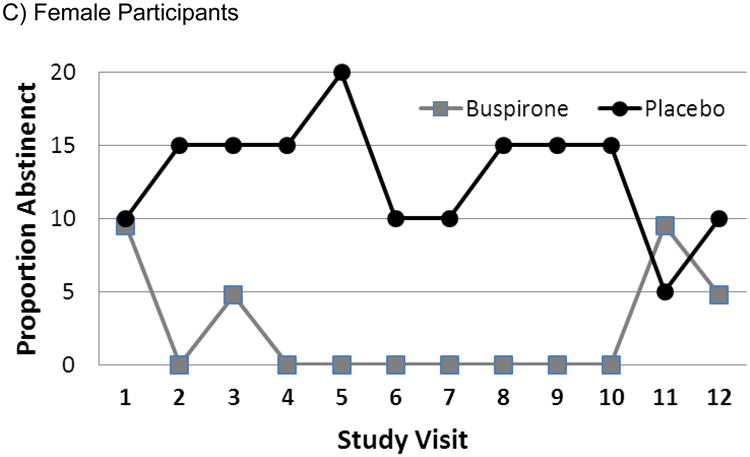
In the analysis of the proportion of negative weekly UCTs in available data from those that completed the study, there was no difference between the buspirone and placebo randomized groups [OR=1.66 (0.59-4.64), χ21=0.9, p=0.33]. End of study abstinence was assessed in all randomized patients at the week 12 study visit. Eight of the 88 randomized participants in the buspirone group and four of the 87 placebo participants submitted negative UCTs [Adjusted OR=2.08 (0.60-7.17), χ21=1.3, p=0.25]. Weekly creatinine adjusted cannabinoid levels are shown in Figure 3a. There was no significant treatment effect on the cannabinoid levels between the participants randomized to buspirone as compared to placebo [ß=-0.24 (-0.57, 0.09), t137=-1.43, p=0.15].
Figure 3.
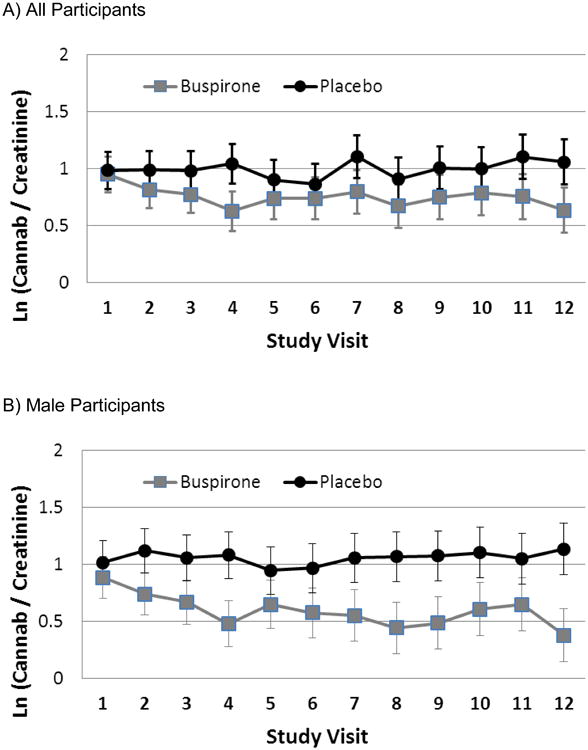
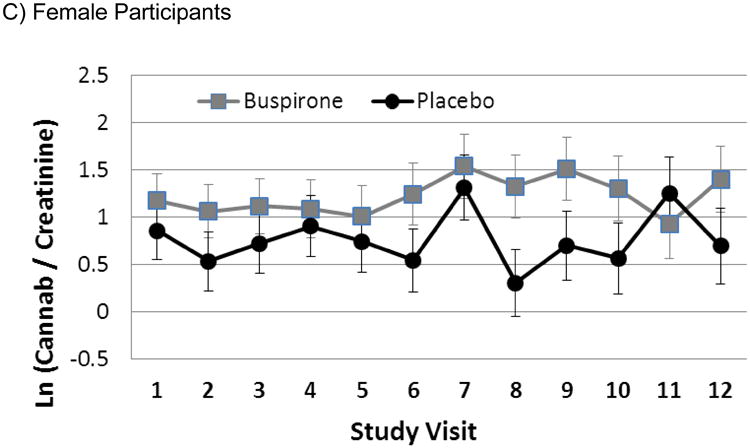
Creatinine adjusted cannabinoid levels by treatment assignment for A) all participants B) Male and C) Female participants. Results are model based means and are shown as the natural logarithm transformed ratio.
The Marijuana Craving Questionnaire (MCQ) was administered at study entry and at all study visits. Data were analyzed on all data from the modified intent to treat sample that had at least one reported measured during study treatment. Craving as measured by the MCQ total score decreased significantly during the course of treatment (Visit 1=36.3±0.9 vs. Visit 12=24.1±1.3; f11,139=10.2; p<0.001) but was not significantly affected by treatment with buspirone as compared to placebo (f1,139=1.64; p=0.20). Participants who attained abstinence from cannabis did have moderately lower reported craving than those who did not attain abstinence (f1,139=8.28; p<0.01).
3.3. Effects of Gender on Efficacy
Following the primary efficacy analysis, the modifying effects of gender on negative UCTs and cannabinoid levels by treatment group were assessed. There was a significant gender by treatment group interaction indicating that the effect of buspirone versus placebo on negative UCTs varied according to gender (ITT sample: χ21=4.5, p=0.034). In males, 8.7% (70/804) of buspirone participant UCTs were negative and 4.5% (36/804) of placebo UCTs were negative [Figure 2b, OR=2.0 (0.71-5.64); p=0.183]. Conversely, in females, 2.4% (6/252) of buspirone participant UCTs were negative and 12.9% (31/240) of placebo UCTs were negative [Figure 2c, OR=0.14 (0.03-0.58); p=0.007]. In the sample of available data, there was a similar interaction between gender and treatment (available sample: χ21=5.6, p=0.018) as well as similar effects stratified by gender [Males: OR=2.1 (0.76-5.98) p=0.149 and Females (OR=0.11 (0.02-0.62) p=0.012]. Although the gender makeup, overall and by treatment group, at the end of the study was similar to that at baseline, the modification of efficacy by gender was not evident in the end of study abstinence proportions by treatment group (End of treatment abstinence: gender by treatment interaction χ21=41.7, p=0.195). Additionally, a gender by treatment interaction indicated that the effect of buspirone versus placebo on creatinine adjusted cannabinoid levels varied according to gender (F1,136=5.3, p=0.023) in concert with the UCT results. In the sample of males, those randomized to buspirone treatment had significantly lower creatinine adjusted cannabinoid levels as compared to those randomized to placebo (Figure 3b; Overall Treatment Difference Ln(Ratio): 0.6±0.1 vs. 1.1±0.1, Δ=-0.47±0.20, p=0.022); this overall effect persisted throughout the study and remained present at the final study visit (0.4±0.2 vs. 1.1±1.2, Δ=-0.76±0.32, F1,105=5.4 p=0.020). The treatment effect size seen in the smaller sample of females was of the same magnitude but numerically opposite from what was seen in males, although it failed to attain statistical significance (Figure 3c, 1.2±0.2 vs. 0.8±0.2, Δ=0.46±0.30 F1,29=2.5, p=0.125).
In light of the evidence of possible differential effects of treatment with buspirone across gender, investigations into differences in baseline clinical and cannabis use characteristics across gender and treatment assignment were conducted. There were no differences noted in any of the baseline cannabis use characteristics between males and females (age of dependence onset, average sessions per day, average joints per day, and ounces used per week; all p>0.10). Although HAM-A scores were low overall, females had higher baseline anxiety symptoms than males in those randomized to receive active buspirone (HAM-A; Males 2.42±0.40 vs. Females 4.43±0.71, t171=2.47, p=0.015) but not so in those randomized to receive placebo (HAM-A; Males 3.13±0.40 vs. Females 3.10±0.73, t171=-0.04, p=0.967). Similarly, females randomized to receive buspirone had higher MCQ purposefulness scores than males randomized to receive buspirone (Males 13.2±0.6 vs. Females 16.5±1.1, t171=2.65, p=0.009). In those randomized to receive placebo, there were no significant differences between females and males (Males 14.3±0.6 vs. Females 13.7±1.1, t171=-0.46, p=0.648). There were no significant differences in the 5-HT1A receptor genotype distribution, education level, or race across genders between the two treatment assignments (χ21=0.01; p=0.912; χ21=1.9; p=0.168; χ21=1.63; p=0.202).
3.4. Role of the Serotonin-1A (5-HT1A) Receptor
The 5-HT1A receptor genotype for the C(-1019)G polymorphism was typed in 172 of the 175 randomized participants (3 subjects were missing genetic sample data and are not included in the ITT analysis). Eighty-five participants (49.4%) were typed as the C/G dysfunctional variant while 87 (50.6%) were typed either C/C or GG. Thirty-nine participants (22.7%) were genotype C/C and 48 (27.9%) were typed G/G). The overall allele frequencies for the study population were 163 (47.4%) for the C and 181 (52.6%) for the G allele. There was no statistical difference in variant distribution or allele frequencies between treatment groups [Variant distribution: χ22=1.3, p=0.52]. When added to the primary efficacy model, there was no significant difference in the proportion of negative UCTs (ITT) between those with the C/G variant and those with other variant types [% negative UCT: C/G=6.4% vs. C/C, G/G=7.1%; OR=1.0 (0.41-2.43), χ21=0.0, p=0.99]. Within the participants randomized to receive placebo, the proportion of negative UCTs during the study was similar between those with the C/G variant and those without [C/G=6.3% vs. C/C, G/G=5.8%; OR=1.05 (0.26-4.32), χ21=0.0, p=0.94]. In the participants randomized to receive buspirone, the proportion of negative UCT during the study was not different in those with the C/G variant as compared to those without [C/G=6.4% vs. C/C, G/G=8.2%; OR=0.81 (0.24-2.73), χ21=0.1, p=0.74, Table 3].
Table 3.
Analysis of the 5-HT1A receptor genotype for the C(-1019)G polymorphism and negative UCT during study treatment; stratified by randomized treatment assignment.
| Results | Study Sample | |||
|---|---|---|---|---|
|
| ||||
| Intent to Treat N=172 | Completers N=87 | |||
| Placebo | Buspirone | Placebo | Buspirone | |
| Statistics | ||||
| OR (95% CI) | 1.05 (0.26-4.32) | 0.81 (0.24-2.73) | 1.45 (0.33-6.37) | 0.92 (0.23-3.63) |
| χ21 | 0.01 | 0.11 | 0.24 | 0.01 |
| P Value | 0.942 | 0.737 | 0.625 | 0.907 |
| % Neg UDS | ||||
| C/G | 6.3% (35/552) | 6.4% (30/468) | 11.6% (31/268) | 11.5% (26/226) |
| C/C G/G | 5.8% (28/480) | 8.2% (46/564) | 8.00% (18/226) | 15.1% (44/292) |
Intent to treat analysis: Analysis of all randomized participants. Completer analysis: Analysis of available data on participants who completed the week 12 study visit. Statistical results are shown from the design adjusted models.
There was no association between the presence of either the C or G allele and proportion of negative UCTs during the study [C allele: χ21=0.2, p=0.88 and G allele: χ21=0.2, p=0.89]. From the group with the dysfunctional C/G variant, 17 (20.0%) participants had at least one negative UCT. In those without the dysfunctional C/G variant, 18 (20.7%) had at least one negative UCT during the study [HR=0.95 (0.49-1.85), χ21=0.2, p=0.89].
3.5. Study Retention and Contingency Management
This study randomized 175 participants to receive either buspirone (n=88) or placebo (n=87). One hundred fifty-seven participants (90%) received at least one dose of study medication and 92 (53%; Buspirone n=45, Placebo n=47) completed the study. The median number of days retained in the study was not significantly different between the two treatment groups (Median (IQR): Buspirone, 79 (18-91); Placebo 84 (14-91); p=0.50). Similarly, the time to study dropout (days to last study visit/LTF) was not different between the two treatment groups [HR = 1.04 (0.54-2.00); χ21=0.0, p=0.91].
In the ITT sample, there was no difference in the CM compensation received between those randomized to receive buspirone as compared to placebo (buspirone 242 +/- 203 vs. placebo 248 +/- 203; p=0.619). Similarly, in those that received at least one dose of study medication (modified ITT sample), there remained no difference in the CM compensation received between those randomized to receive buspirone as compared to placebo (buspirone 283 +/- 192 vs. placebo 316 +/- 175; p=0.625). Additionally, there was a similar proportion of participants that achieved the maximum CM compensation ($450) in each treatment group (buspirone 42.1%, 37/88 vs. placebo 39.1%, 34/87; p=0.690).
3.6. Medication Dosage and Compliance
In participants that received at least one study dose of medication, the maximum dosage received by each participant was tabulated. The mean dose received was 42 (SD=18) mg [39 (17) in the group randomized to receive buspirone and 45(18) in the group randomized to receive placebo]. Of those that received at least one medication dose, 43% (68/157) received the maximum possible dosage (60 mg) and 76% (119/157) received at least 30 mg. Study medication compliance was measured using pill counts at every study visit as well as using a riboflavin marker at every other visit (even numbered). Pill count and self-reported medication usage greater than 80% and riboflavin levels measured greater than 900 ng/ml where considered to be in compliance for the preceding week. Of the weekly recorded pill counts, 88.9% (1094/1230) were in compliance; 87.2% (536/615) in the group randomized to receive buspirone and 90.7% (558/615) in the placebo group [OR (95% CI)=0.73 (0.42-1.29), χ21=1.0, p=0.28]. Of the measured riboflavin levels, 78.8% (477/605) were in compliance; 77.2% (234/303) in the group randomized to receive buspirone and 80.5% (243/302) in the placebo group [OR (95% CI)=1.01 (0.55-1.86), χ21=0.0, p=0.98]. Additionally, medication compliance was not associated with increase concurrent negative UCTs [OR=0.84 (0.51-1.36); χ21=0.5, p=0.47].
3.7. Safety and Tolerability
A thorough safety and tolerability evaluation was conducted at each study visit. A study clinician evaluated adverse events with an open-ended interview and a comprehensive review of clinical measurements. A total of 369 events were reported in 73 participants in the buspirone group and 318 events were reported in 66 participants in the placebo group (χ21=1.34, p=0.25). The most commonly reported adverse events were gastrointestinal in nature or headache, which accounted for 14.7% and 14.0% of all adverse events in the buspirone and placebo treatment groups, respectively. Dizziness and drowsiness additionally accounted for 8.8% and 5.4% of all adverse events in buspirone and placebo treatment groups, respectively. Nearly all reported adverse events were rated mild to moderate (99.6%; 684/687); two participants randomized to the buspirone treatment group and one participant randomized to the placebo group reported severe adverse events that were unrelated to study medication. None of the reported events were considered “definitely related” to the study drug and only a small percentage were considered “probably” related (buspirone 37/369 and placebo 29/318, χ21=1.29, p=0.26). No FDA defined serious events adverse events occurred in either treatment group.
4. Discussion
In this trial, buspirone did not demonstrate an advantage over placebo on cannabis use outcomes. Although cannabis craving (as measured by the MCQ) significantly declined for all participants over the course of the study, no treatment effect was found. These findings add to the growing body of evidence that antidepressants and anxiolytics likely have limited value in the treatment of cannabis use disorders other than potentially for treatment of comorbid conditions (Marshall et al., 2014).
The overall proportion of participants achieving abstinence was low in both groups in the present investigation. A low overall abstinence rate has been observed in other medication trials for cannabis dependence (Carpenter et al., 2009; Levin et al., 2011; McRae-Clark et al., 2010; Weinstein et al., 2014). Although motivational enhancement therapy was provided to all participants, an alternate psychosocial platform may be necessary to encourage sustained abstinence in this population. Contingency management interventions targeting substance use may be more effective in increasing motivation for abstinence (Caroll et al., 2004). A recent promising trial of N-acetylcysteine in cannabis-dependent adolescents (Gray et al., 2012) utilized abstinence-based contingency management; further, there is some evidence in other dependencies that abstinence-based contingency management augments medication efficacy (Gray et al., 2011; Poling et al., 2006; Schmitz et al., 2008). Increasing the duration of the psychosocial intervention may also be necessary. Weekly therapy sessions may have improved attrition and cannabis use outcomes. Given the MET intervention does increase motivation to change substance use behavior, more sessions focusing on effective coping skills may be helpful.
Of note, women randomized to buspirone had worse cannabis use outcomes, while men had a reduction in creatinine corrected cannabinoid levels with buspirone treatment. To our knowledge, this is the first study to demonstrate a gender difference in response to a pharmacological treatment for cannabis dependence. This finding is congruent with a recent study exploring the use of buspirone versus placebo for treatment of cocaine dependence (Winhusen et al., 2014), in which women receiving buspirone had an increase in cocaine use. Previous preclinical work has not demonstrated sex differences in response to the anxiolytic effects of buspirone (Fernandez-Guasti and Picazo, 1990; Fernandez-Guasti and Picazo, 1997); however, sex differences in 5-HT1A receptor and serotonin transporter binding have been reported in a clinical sample (Jovanovic et al., 2008). The present findings, in conjunction with those of Winhusen and colleagues, highlight the importance of including gender as a critical independent variable in the development and evaluation of new treatments for addictive disorders.
Results from our analyses of the impact of serotonergic polymorphisms on UCT prevalence did not reach statistical significance. The inclusion of polymorphisms of the gene coding for the 5-HT1A receptor variants was made on the basis of the known pharmacology of buspirone and documented pathophysiology of 5-HT1A receptors in psychiatric research. The lack of a robust association between a small number of allelic forms and treatment outcomes does not eliminate a genetic contribution for either sustained use of cannabis or potential response to serotonergic or other pharmacologic treatment interventions.
In our previous pilot trial of buspirone for cannabis dependence (McRae-Clark et al., 2009), a reduction in the percentage of positive UCTs was observed in participants that completed the 12-week trial. A post-hoc analysis of completers in the present trial did not find a treatment effect of buspirone. It should be noted that the present sample had a higher percentage of female participants than the previous pilot trial (23.4% vs. 12%, respectively) which, given the gender differential in response observed in the current investigation, may have contributed to these negative findings. Our previous pilot trial also found that anxiety severity over the course of the study was a significant predictor of UCT results, with a treatment main effect. The lower levels of anxiety reported by participants in the current trial preclude the conduct of a similar analysis. Although women randomized to buspirone had higher baseline levels of anxiety than men and worse cannabis use outcomes, it should be noted that the HAM-A scores of both groups were still low (4.43±0.71 and 2.42±0.40, respectively), as the threshold for mild to moderate anxiety is generally accepted as a HAM-A score of 18. As such, we are unable to determine if individuals with clinically significant anxiety may have a greater response to buspirone treatment. This low endorsement of general anxiety symptoms is somewhat unexpected given the reported high comorbidity of cannabis use and anxiety disorders (Stinson et al., 2006); however, it may be reflective of excluding individuals requiring treatment with psychoactive medications or meeting criteria for other major psychiatric disorders, particularly as depression is often comorbid with anxiety.
Limitations of the study included significant attrition during the course of the twelve week study. UCT interpretation is also difficult due to the long excretion half-life of cannabis in urine (Eskridge and Guthrie, 1997). Although creatinine normalization has been proposed as a method to differentiate new cannabis use from residual drug excretion (Huestis and Cone, 1998), the utility of creatinine normalization has not been well established with urine sampling conducted at weekly intervals. Further, as noted above, our analysis of impact of genetic receptor polymorphisms was likely underpowered.
In conclusion, although the sample size in the present investigation was sufficient to detect clinically meaningful differences in cannabis use outcomes, buspirone was not shown to be more efficacious than placebo in the overall sample. Important gender differences were noted, with women having worse cannabis use outcomes with buspirone treatment. Although it is possible that subsets of individuals with cannabis use disorders, such as those with significant anxiety symptoms, may respond more positively to buspirone treatment, the characteristics of participants in this study preclude such analyses. These results underscore the challenges in medication development for cannabis use disorders.
Acknowledgments
Role of Funding Source: Funding for this study was provided by NIDA Grant R01DA026782 (McRae-Clark). NIDA had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Conflicts of Interest: Authors McRae-Clark and Brady have received previous grant support from Bristol-Myers Squibb (none in past seven years).
Contributors: Author McRae-Clark designed the study and wrote the protocol. Authors McRae-Clark, Killeen, Gray, Wagner, and Norton participated in the conduct of the study. Author Baker undertook the statistical analysis. All authors contributed to and have approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anthony JC, Helzer JE. Syndromes of drug abuse and dependence. In: Robins LN, Reiger DA, editors. Psychiatric Disorders in America. Free Press; New York: 1991. pp. 116–154. [Google Scholar]
- Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, controlled substances, and inhalants: basic findings from the National Comorbidity Study. Exp Clin Psychopharmacol. 1994;2:244–268. [Google Scholar]
- Buckner JD, Bonn-Miller MO, Zvolensky MJ, Schmidt NB. Marijuana use and social anxiety among marijuana using young adults. Addict Behav. 2007;32:2238–2252. doi: 10.1016/j.addbeh.2007.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Carroll KM. Effect of anxiety on treatment presentation and outcome: results from the Marijuana Treatment Project. Psychiatry Res. 2010;178:493–500. doi: 10.1016/j.psychres.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney AJ, Novy PL, Hughes JR. Marijuana withdrawal among adults seeking treatment for marijuana dependence. Addiction. 1999;94:1311–1321. doi: 10.1046/j.1360-0443.1999.94913114.x. [DOI] [PubMed] [Google Scholar]
- Carpenter KM, McDowell D, Brooks DJ, Cheng WY, Levin FR. A preliminary trial: double-blind comparison of nefazodone, bupropion-SR, and placebo in the treatment of cannabis dependence. Am J Addict. 2009;18:53–64. doi: 10.1080/10550490802408936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Kosten TR, Rounsaville BJ. Choosing a behavioral therapy platform for pharmacotherapy of substance users. Drug Alcohol Depend. 2004;75:123–134. doi: 10.1016/j.drugalcdep.2004.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Pringle B. Services research on adolescent drug treatment. Commentary on “The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials”. J Subst Abuse Treat. 2004;27:195–196. doi: 10.1016/j.jsat.2004.07.003. [DOI] [PubMed] [Google Scholar]
- Darmani NA, Janoyan JJ, Kumar N, Crim JL. Behaviorally active doses of the CB1 receptor antagonist SR 141716A increase brain serotonin and dopamine levels and turnover. Pharmacol Biochem Behav. 2003;75:777–787. doi: 10.1016/s0091-3057(03)00150-3. [DOI] [PubMed] [Google Scholar]
- David SP, Johnstone EC, Murphy MF, Aveyard P, Guo B, Lerman C, Munafo MR. Genetic variation in the serotonin pathway and smoking cessation with nicotine replacement therapy: new data from the Patch in Practice trial and pooled analyses. Drug Alcohol Depend. 2008;98:77–85. doi: 10.1016/j.drugalcdep.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drevets WC, Thase ME, Moses-Kolko EL, Price J, Frank E, Kupfer DJ, Mathis C. Serotonin-1A receptor imaging in recurrent depression: replication and literature review. Nucl Med Biol. 2007;34:865–877. doi: 10.1016/j.nucmedbio.2007.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eskridge KD, Guthrie SK. Clinical issues associated with urine testing of substances of abuse. Pharmacotherapy. 1997;17:497–519. [PubMed] [Google Scholar]
- Fernandez-Guasti A, Picazo O. The actions of diazepam and serotonergic anxiolytics vary according to the gender and the estrous cycle phase. Pharmacol Biochem Behav. 1990;37:77–81. doi: 10.1016/0091-3057(90)90044-i. [DOI] [PubMed] [Google Scholar]
- Fernandez-Guasti A, Picazo O. Anxiolytic actions of diazepam, but not of buspirone, are influenced by gender and the endocrine stage. Behav Brain Res. 1997;88:213–218. doi: 10.1016/s0166-4328(97)00047-8. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Biometrics Research. New York State Institute; New York: 2002. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) [Google Scholar]
- Goa KL, Ward A. Buspirone. A preliminary review of its pharmacological properties and therapeutic efficacy as an anxiolytic. Drugs. 1986;32:114–129. doi: 10.2165/00003495-198632020-00002. [DOI] [PubMed] [Google Scholar]
- Gomes FV, Resstel LB, Guimaraes FS. The anxiolytic-like effects of cannabidiol injected into the bed nucleus of the stria terminalis are mediated by 5-HT1A receptors. Psychopharmacology (Berl) 2011;213:465–473. doi: 10.1007/s00213-010-2036-z. [DOI] [PubMed] [Google Scholar]
- Gray KM, Carpenter MJ, Baker NL, DeSantis SM, Kryway E, Hartwell KJ, McRae-Clark AL, Brady KT. A double-blind randomized controlled trial of N-acetylcysteine in cannabis-dependent adolescents. Am J Psychiatry. 2012;169:805–812. doi: 10.1176/appi.ajp.2012.12010055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray KM, Carpenter MJ, Baker NL, Hartwell KJ, Lewis AL, Hiott DW, Deas D, Upadhyaya HU. Buproprion SR and contingency management for adolescent smoking cessation. J Subst Abuse Treat. 2011;40:77–86. doi: 10.1016/j.jsat.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. Br J Psychiatry. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Heishman SJ, Evans RJ, Singleton EG, Levin KH, Copersino ML, Gorelick DA. Reliability and validity of a short form of the Marijuana Craving Questionnaire. Drug Alcohol Depend. 2009;102:35–40. doi: 10.1016/j.drugalcdep.2008.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill MN, Sun JC, Tse MT, Gorzalka BB. Altered responsiveness of serotonin receptor subtypes following long-term cannabinoid treatment. Int J Neuropsychopharmacol. 2006;9:277–286. doi: 10.1017/S1461145705005651. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Cone EJ. Differentiating new marijuana use from residual drug excretion in occasional marijuana users. J Anal Toxicol. 1998;22:445–454. doi: 10.1093/jat/22.6.445. [DOI] [PubMed] [Google Scholar]
- Jovanovic H, Lundberg J, Karlsson P, Cerin A, Saijo T, Varrone A, Halldin C, Nordstrom AL. Sex differences in the serotonin 1A receptor and serotonin transporter binding in the human brain measured by PET. NeuroImage. 2008;39:1408–1419. doi: 10.1016/j.neuroimage.2007.10.016. [DOI] [PubMed] [Google Scholar]
- Kadden RM, Litt MD, Kabela-Cormier E, Petry NM. Abstinence rates following behavioral treatments for marijuana dependence. Addict Behav. 2007;32:1220–1236. doi: 10.1016/j.addbeh.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lader M. Can buspirone induce rebound, dependence or abuse? Br J Psychiatry Suppl. 1991;12:45–51. [PubMed] [Google Scholar]
- Le Francois B, Czesak M, Steubl D, Albert PR. Transcriptional regulation at a HTR1A polymorphism associated with mental illness. Neuropharmacology. 2008;55:977–985. doi: 10.1016/j.neuropharm.2008.06.046. [DOI] [PubMed] [Google Scholar]
- Lemonde S, Turecki G, Bakish D, Du L, Hrdina PD, Bown CD, Sequeira A, Kushwaha N, Morris SJ, Basak A, Ou XM, Albert PR. Impaired repression at a 5-hydroxytryptamine 1A receptor gene polymorphism associated with major depression and suicide. J Neurosci. 2003;23:8788–8799. doi: 10.1523/JNEUROSCI.23-25-08788.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin FR, Mariani JJ, Brooks DJ, Pavlicova M, Cheng W, Nunes EV. Dronabinol for the treatment of cannabis dependence: a randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend. 2011;116:142–150. doi: 10.1016/j.drugalcdep.2010.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall K, Gowing L, Ali R, Le Foll B. Pharmacotherapies for cannabis dependence. Cochrane Database System Rev. 2014;12:1–64. doi: 10.1002/14651858.CD008940.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason BJ, Crean R, Goodell V, Light JM, Quello S, Shadan F, Buffkins K, Kyle M, Adusumalli M, Begovic A, Rao S. A proof-of-concept randomized controlled study of gabapentin: effects on cannabis use, withdrawal and executive function deficits in cannabis-dependent adults. Neuropsychopharmacology. 2012;37:1689–1698. doi: 10.1038/npp.2012.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mato S, Vidal R, Castro E, Diaz A, Pazos A, Valdizan EM. Long-term fluoxetine treatment modulates cannabinoid type 1 receptor-mediated inhibition of adenylyl cyclase in the rat prefrontal cortex through 5-hydroxytryptamine 1A receptor-dependent mechanisms. Mol Pharmacol. 2010;77:424–434. doi: 10.1124/mol.109.060079. [DOI] [PubMed] [Google Scholar]
- McRae AL, Budney AJ, Brady KT. Treatment of marijuana dependence: a review of the literature. J Subst Abuse Treat. 2003;24:369–376. doi: 10.1016/s0740-5472(03)00041-2. [DOI] [PubMed] [Google Scholar]
- McRae-Clark AL, Carter RE, Killeen TK, Carpenter MJ, Wahlquist AE, Simpson SA, Brady KT. A placebo-controlled trial of buspirone for the treatment of marijuana dependence. Drug Alcohol Depend. 2009;105:7p. doi: 10.1016/j.drugalcdep.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McRae-Clark AL, Carter RE, Killeen TK, Carpenter MJ, White KG, Brady KT. A placebo-controlled trial of atomoxetine in marijuana-dependent individuals with attention deficit hyperactivity disorder. Am J Addict. 2010;19:481–489. doi: 10.1111/j.1521-0391.2010.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakazi M, Bauer U, Nickel T, Kathmann M, Schlicker E. Inhibition of serotonin release in the mouse brain via presynaptic cannabinoid CB1 receptors. Naunyn Schmiedebergs Arch Pharmacol. 2000;361:19–24. doi: 10.1007/s002109900147. [DOI] [PubMed] [Google Scholar]
- Nordstrom BR, Levin FR. Treatment of cannabis use disorders: a review of the literature. Am J Addict. 2007;16:331–342. doi: 10.1080/10550490701525665. [DOI] [PubMed] [Google Scholar]
- Pan W. Akaike's information criterion in generalized estimating equations. Biometrics. 2001;57:120–125. doi: 10.1111/j.0006-341x.2001.00120.x. [DOI] [PubMed] [Google Scholar]
- Poling J, Oliveto A, Petry N, Sofuoglu M, Gonsai K, Gonzalez G, Martell B, Kosten TR. Six-month trial of bupropion with contingency management for cocaine dependence in a methadone-maintained population. Arch Gen Psychiatry. 2006;63:219–228. doi: 10.1001/archpsyc.63.2.219. [DOI] [PubMed] [Google Scholar]
- SAMHSA. National Household Survey on Drug Use and Health. SAMHSA; Rockville: 2014. [Google Scholar]
- Schmitz JM, Mooney ME, Moeller FG, Stotts AL, Green C, Grabowski J. Levodopa pharmacotherapy for cocaine dependence: choosing the optimal behavioral therapy platform. Drug Alcohol Depend. 2008;94:142–150. doi: 10.1016/j.drugalcdep.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported ethanol consumption. In: Allen J, Litten RZ, editors. Measuring Alcohol Consumption: Psychological And Biological Methods. Humana Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Steinberg KL, Roffman RA, Carroll KM, McRee B, Babor TF, Miller M, Kadden R, Duresky D, Stephens R. Center for Substance Abuse Treatment. Substance Abuse and Mental Health Services Administration; Rockville: 2005. Brief Counseling for Marijuana Dependence: A Manual for Treating Adults (Vol HHS Publication No (SMA) 12-4211) [Google Scholar]
- Stinson FS, Ruan WJ, Pickering R, Grant BF. Cannabis use disorders in the USA: prevalence, correlates and co-morbidity. Psychol Med. 2006;36:1447–1460. doi: 10.1017/S0033291706008361. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Suppl. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Vandrey R, Haney M. Pharmacotherapy for cannabis dependence: how close are we? CNS Drugs. 2009;23:543–553. doi: 10.2165/00023210-200923070-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein AM, Miller H, Bluvstein I, Rapoport E, Schreiber S, Bar-Hamburger R, Bloch M. Treatment of cannabis dependence using escitalopram in combination with cognitive-behavior therapy: a double-blind placebo-controlled study. Am J Drug Alcohol Abuse. 2014;40:16–22. doi: 10.3109/00952990.2013.819362. [DOI] [PubMed] [Google Scholar]
- Winhusen TM, Kropp F, Lindblad R, Douaihy A, Haynes L, Hodgkins C, Chartier K, Kampman KM, Sharma G, Lewis DF, VanVeldhuisen P, Theobald J, May J, Brigham GS. Multisite, randomized, double-blind, placebo-controlled pilot clinical trial to evaluate the efficacy of buspirone as a relapse-prevention treatment for cocaine dependence. J Clin Psychiatry. 2014;75:757–764. doi: 10.4088/JCP.13m08862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanelati TV, Biojone C, Moreira FA, Guimaraes FS, Joca SR. Antidepressant-like effects of cannabidiol in mice: possible involvement of 5-HT1A receptors. Br J Pharmacol. 2010;159:122–128. doi: 10.1111/j.1476-5381.2009.00521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- Zvolensky MJ, Marshall EC, Johnson K, Hogan J, Bernstein A, Bonn-Miller MO. Relations between anxiety sensitivity, distress tolerance, and fear reactivity to bodily sensations to coping and conformity use motives among young adult marijuana users. Exp Clin Psychopharmacol. 2009;17:31–42. doi: 10.1037/a0014961. [DOI] [PMC free article] [PubMed] [Google Scholar]