Abstract
Adult onset Still’s disease (AOSD) is a systemic auto-inflammatory condition of unknown etiology, characterized by high fever, an evanescent, salmon-pink maculopapular skin rash, arthralgia or arthritis and leukocytosis. AOSD can also present with atypical cutaneous manifestations, such as persistent pruritic coalescent papules or plaques and linear lesions that have highly distinctive pathological features and are usually associated with severe disease. Herein, we present a 31-year-old Brazilian man with both typical Still’s rash and atypical persistent polymorphic cutaneous manifestations associated with severe systemic inflammatory response syndrome. Eosinophils that are consistently lacking in the AOSD-associated skin lesions were evident in the skin biopsy of the persistent atypical cutaneous manifestations and were either drug-related or AOSD-associated.
Keywords: AOSD, Systemic inflammatory response syndrome, Eosinophils, Atypical cutaneous manifestations
Introduction
Adult onset Still’s disease (AOSD) is a systemic auto-inflammatory condition of unknown etiology, characterized by intermittent spiking high fever, an evanescent, salmon-pink or erythematous maculopapular skin rash, arthralgia or arthritis and leukocytosis with at least 80 % neutrophils [1]. Other common symptoms include sore throat, lymphadenopathy, hepatomegaly, and splenomegaly [2]. High serum ferritin levels, elevated ESR and high CRP levels, absent antinuclear antibody (ANA) and rheumatoid factors (RF) are the most common laboratory findings [3, 4]. We report a case of AOSD in a 31-year-old Brazilian man presenting with both typical Still’s rash and atypical non-evanescent polymorphic cutaneous manifestations.
Case presentation
A 31-year-old Brazilian male presented with high quotidian fever and night sweats, non-productive cough, lower back pain and erythematous rash for two weeks. The fever occurred almost daily and ranged from 39 to 40 °C. The rash started from both hands and was characterized by multiple erythematous confluent roundish macules and papules that coalesced to form large, irregular erythematous plaques (Fig. 1). The rash lasted for a few days and then appeared with a different morphology on the flexor surfaces of his arms as an extensive erythematous linear urticarial eruption (Fig. 2a). Subsequently the rash appeared on his upper and lower trunk as multiple intensely pruritic linear urticarial streaks (Fig. 2b). Ibuprofen has been used intermittently to alleviate back pain as well as the fever with minimal relief. He denied any contacts with sick individuals, insect or animal bites and his last trip was to Brazil 10 months ago. He has been sexually active in a monogamous relationship.
Fig. 1.

Typical evanescent rash: Multiple non-pruritic confluent erythematous macules and papules on the dorsal surface of both hands that coalesced to form irregular erythematous plaques
Fig. 2.
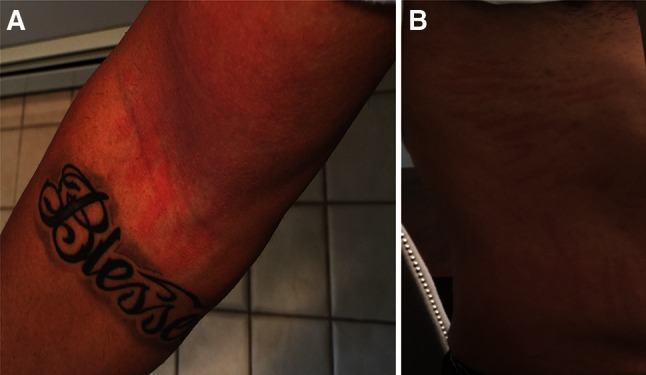
Atypical urticarial rash: a linear urticarial eruption on the flexor surface of arms. b Multiple intensely pruritic linear urticarial streaks on the upper and lower trunk
On admission, his temperature was 39 °C and a persistent pigmented plaque V shaped was evident on his anterior chest extending down the midline to the umbilicus (Fig. 3). Further skin examination revealed a confluent salmon-pink papular eruption on his lower back area and a persistent pigmented plaque on the upper area of his back. Besides mild splenomegaly and a tender right wrist, left second and third proximal interphalangeal joints with no signs of swelling or erythema, the rest of the physical exam was unremarkable. Laboratory profile revealed severe neutrophilic leukocytosis (30,000, normal values 4800–10,800/mcL), and a highly elevated serum ferritin levels (>10,000, normal values 17.90–464.00 ng/mL). Autoantibodies (including ANA, ANCA, RF and anti-CCP) were negative. Blood cultures excluded common viral and bacterial infections and RPR were negative. Serological tests for Hepatitis B and C, HIV, Epstein-Barr and Cytomegalovirus were negative. Borrelia burgdorferi, Bartonella henselae, Rickettsia typhi, RMSF, Typhus and Parvovirus B-19 serologies were negative as well. Parasites for malaria or Babesia microti were undetectable on peripheral blood smear. Transthoracic echocardiogram was negative for vegetations and computed tomography (CT) of the neck, chest and abdomen revealed only borderline mild splenomegaly.
Fig. 3.

Atypical persistent rash: persistent pigmented plaque V shaped on the anterior chest extending down the midline to the umbilicus
The clinical and laboratory findings were consistent with the diagnosis of AOSD according to Yamaguchi criteria [2]. He was started on 50 mg of prednisone. After 2 weeks of treatment, he returned to our hospital with very high daily spiking fever up to 39.5 °C, perfuse sweating, hypotension, elevated liver enzymes and severe leukocytosis with neutrophil predominance. No new skin lesions were noted. The patient was admitted to intensive care unit due to suspected systemic inflammatory response syndrome and was started on broad-spectrum antibiotics and intravenous fluids. Since the blood cultures were negative, antibiotics were discontinued. Anakinra 100 mg daily subcutaneously was added to 50 mg of prednisone with dramatic resolution of his febrile episodes. The patient was discharged with instructions to gradually taper prednisone.
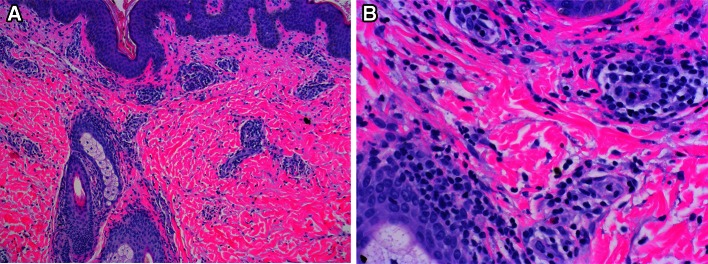
After 1 week of treatment with Anakinra and while on 40 mg of prednisone the patient remained afebrile but new erythematous plaques appeared on lower abdominal quadrants and a skin biopsy was performed (Fig. 4). Skin biopsy showed a normal epidermis, with an inflammatory infiltrate in the dermis surrounding superficial blood vessels and adnexal structures, and the interstitium as well (Fig. 5a). The inflammatory infiltrate composed of lymphocytes, neutrophils and eosinophils (Fig. 5b). Because of the persistent cutaneous manifestations, the patient was advised to apply on the persistent eruptions of his chest and abdomen triamcinolone cream 0.5 % twice daily. After 1-month follow-up, the skin rash on the above areas almost resolved.
Fig. 4.

Atypical persistent pruritic eruption: edematous erythematous plaques on lower abdominal quadrants. Stich denotes the site of skin biopsy
Fig. 5.
a Hematoxylin and eosin (H&E) stain showing periadnexal and perivascular infiltrate of inflammatory cells surrounding blood vessels, hair follicles and the interstitium (in between the vessels and adnexal structures). Original magnification at ×100. b H&E stain showing perivascular inflammatory infiltration of lymphocytes, neutrophils and eosinophils. Original magnification at ×400
Discussion
Review of literature, via the PubMed search, using the terms adult onset Still’s disease, cutaneous manifestations and eruptions from 1985 to 2014 to retrieve data on the diversity in clinical manifestations and histopathological findings of polymorphic Still’s rash, was performed (Table 1). AOSD is a rare young adult systemic autoimmune disorder with diverse clinical manifestations and occasionally unwanted serious organ damage like acute liver failure, adult respiratory distress syndrome, disseminated intravascular coagulation, and hemophagocytic syndrome [5–10]. Thus, early recognition of AOSD is crucial and should be always considered in the differential diagnosis of a systemic inflammatory syndrome, particularly when extensive microbiological workup is negative.
Table 1.
Clinical manifestations and histopathological findings of Still’s disease
| Author/Year | No of patients/ age (range) /Sex | Clinical presentation | Laboratory findings | Cutaneous manifestation | Skin Histology | Treatment |
|---|---|---|---|---|---|---|
| Wouters et al. [12] | 1/66 /F 1/62/M | Polyarthritis, fever, splenomegaly | Leukocytosis, anemia, increased ESRand liver enzymes | Evanescent macular nonpruritic rash on trunk, limbs | - | NSAIDs, Penicillamine |
| Phillips et al. [21] | 1/51/F | Arthralgia, sore throat, lethargy, night sweats | Leukocytosis, anemia, increased ESR, liver enzymes & ferritin | Evanescent erythematous maculopapular pruritic rash on trunk, limbs, face | Perivascular infiltrate in upper dermis and dermal mucin deposition | NSAIDs, Methotrexate |
| Tay et al. [27] | 1/33/F | Fever, arthralgia, malaise, sore throat, headache, lymphadenopathy, hepatomegaly | Leukocytosis, anemia, increased ESR, CRP & immunoglobulins | Evanescent urticarial-like erythematous maculopapular pruritic rash on trunk, limbs | Edema of the upper dermis with perivascular neutrophils and eosinophils | NSAIDs, Prednisolone |
| Setterfield et al. [30] | 1/32/F | Arthralgia, sore throat, fever, anorexia, weight loss | Leukocytosis, anemia, increased ESR, CRP & ferritin | Persistent urticarial annular pruritic lesions on trunk and limbs | Dermal edema, perivascular neutrophilic infiltrate | NSAIDs |
| Lubbe et al. [33] | 1/16/F | Fever, arthritis, sore throat, pericardial effusion, hepatosplenomegaly | Leukocytosis, anemia, increased ESR, CRP & ferritin | Evanescent maculopapular lesions on chest, persistent brownish papules and plaques on face, neck, back | Parakeratosis, acanthosis and scattered intraepithelial keratinocyte necroses | NSAIDs, Prednisone |
| Salaffi et al. [36] | 1/55/F | Fever, arthralgia, fatigue | Leukocytosis, anemia, increased ESR, CRP & ferritin | Urticarial pruritic rash on trunk, limbs and face | Dermal edema with perivascular and interstitial neutrophilic infiltrate | NSAIDs, Prednisone, Methotrexate |
| Suzuki et al. [18] | 1/25/M | Fever, arthralgia, fatigue | Leukocytosis, anemia, increased ESR, CRP, liver enzymes & ferritin | Persistent papules and plaques on trunk, linear pigmentation on chest and back | Mild perivascular infiltration of neutrophils and lymphocytes. | NSAIDs, Prednisolone, Methotrexate |
| Perez et al. [43] | 1/39/M | Polyarthritis, sore throat, fever, chills, lymphadenopathy, hepatosplenomegaly | Leukocytosis, increased ESR, CRP liver enzymes & ferritin | Erythematous papules and plaques on neck, trunk, limbs | Perivascular infiltrate of dermal vessels with eosinophils, histiocytes, lymphocytes and neutrophils within vessels | NSAIDs, Prednisone |
| Lee et al. [25] | 1/46/F | Arthralgia, high fever, headache, nausea, splenomegaly | Anemia, thrombocytopenia, increased ESR, liver enzymes &ferritin | Vesicular and pustular eruption on hands and feet | Fibrin deposit in the vessels, subepidermal bulla and ischemic necrosis of epidermis | NSAIDs, Corticosteroids |
| Elezoglou et al. [42] | 1/47/M | Fever, arthralgia, malaise, sore throat, hepatosplenomegaly glomerulonephritis | Leukocytosis, anemia, increased CRP, liver enzymes & ferritin, cryoglobulinemia | Evanescent maculopapular pruritic rash on head, trunk, buttocks, groin, annular purpuric plaques on ankles and shins | Leuko-cytoclastic vasculitis | Methyl-prednisolone, Methotrexate |
| Thien Huong et al. [17] | 1/23/F | Fever, polyarthralgia, polyadenopathy, myalgia | Leukocytosis, increased ESR & ferritin | Persistent pigmented plaques on trunk | - | Corticosteroids |
| Tomaru et al. [23] | 1/34/F | Fever, polyarthralgia, lymphadenopathy | Leukocytosis, increased CRP, liver enzymes & ferritin | Persistent pruritic erythematous papules with linear arrangement and pigmentary changes on chest and back, evanescent salmon-pink eruption on lower extremities | Mild acanthosis, exocytosis, dyskeratotic cells and liquefaction degeneration in the basal layer, with lichenoid inflammatory reaction | Corticosteroids, Cyclosporine, Methotrexate |
| Criado et al. [31] | 1/52/F | Fever, polyarthralgia, sore throat, mild hepatomegaly, lymphadenopathy | Leukocytosis, increased ESR, CRP, & ferritin, hypergammaglobulinemia | Lenticular urticaria-like rash on face, thorax, abdomen, hands | Interstitial edema in reticular and papillar dermis with neutrophils and leukocytes around vasculitis-free vessels. | NSAIDs, Methotrexate, Thalidomide |
| Yang et al. [35] | 1/47/F | Fever, polyarthralgia, sore throat, myalgia, pleural effusion, splenomegaly | Leukocytosis, elevated liver enzymes & ferritin | Persistent violaceous scaly maculopapular rash with linear lesions on forehead, neck, elbows, knees | Necrotic keratinocytes in the upper epidermis and perivascular infiltrate of lymphocytes and neutrophils | Methyl-prednisolone, Azathioprine |
| Wolgamot et al. [39] | 1/55/F | Fever, polyarthralgia | Leukocytosis, increased ESR, CRP & ferritin |
Pruritic maculopapular rash, plaques on face, extremities, trunk | Pattern with dyskeratotic keratinocytes in upper epidermis and stratum corneum | Prednisone, Methotrexate, Etanercept, Anakinra |
| Yanai et al. [41] | 1/43/M | Fever, arthralgia, myalgia, myositis | Increased fibrinogen CRP, creatine kinase & ferritin | Salmon-pink rash on upper arm | Perivascular lymphocytes infiltration and fragmentation of blood cells compatible with leukocytoclastic vasculitis | NSAIDs, corticosteroids |
| Fortna et al. [40] | 3/15-54/F | Fever, polyarthralgia, myalgia, sore throat | Leukocytosis, increased ESR, CRP, liver enzymes & ferritin | Pruritic erythematous blanchable papules and plaques on back, neck, abdomen, limbs | Hyperkeratosis with patchy parakeratosis, areas of dyskeratosis to upper layers of epidermis, and mild acanthosis. | Methyl-prednisolone, Methotrexate, Anakinra |
| Criado et al. [26] | 2/27-34/F 1/26/M |
Fever, arthritis, sore throat, lymphadenopathy, pleural effusion, splenomegaly | Leukocytosis, anemia, increased ESR, CRP & liver enzymes, hyperferritinemia | Urticarial pruritic rash, linear lesions (dermographism) on trunk, limbs, face | Perivascular and interstitial inflammatory cell infiltrate of lymphocytes and neutrophils with leukocytoclasia. | Prednisone, Chloroquine, Methotrexate, |
| Nagai et al. [34] | 18/16-60/F | Fever, arthralgia, sore throat, splenomegaly, lymphadenopathy | Leukocytosis, increased CRP, liver enzymes & ferritin | Evanescent salmon-pink maculopapular eruption, persistent papules and plaques with linear erythema similar to prurigo pigmentosa, edema of eyelids mimicking dermatomyositis | Parakeratosis and necrotic keratinocytes in epidermis, inflammatory infiltrates of lymphocytes in the papillary and mid-dermis | Corticosteroids, Methotrexate, Mizoribine Cyclosporin, Cyclophosphamide |
| Lee et al. [14] | 30/17-67/F 6/17-67/M |
Fever, arthralgia, sore throat, splenomegaly, lymphadenopathy | Leukocytosis, elevated liver enzymes & ferritin | Evanescent rash, persistent pruritic urticarial, violaceous papules and plaques, dermatographism-like, prurigo pigmentosa-like and dermatomyositis-like eruption on trunk, neck, face, limbs | Normal epidermis with perivascular infiltrate of neutrophils, nectrotic keratinocytes in upper epidermis. | NSAIDs, Corticosteroids, Methotrexate, Azathioprine |
| Yoshifuku et al. [16] | 1/27/F | Fever, polyarthralgia, sore throat, hepatosplenomegaly lymphadenopathy | Leukocytosis, increased CRP, elevated liver enzymes & ferritin | Pruritic pigmented erythematous plaques and dark-reddish papules on abdomen and back | Mild hyperkeratosis, and presence of dyskeratotic keratinocytes in upper epidermis | Corticosteroids, Cyclosporin, |
| Said et al. [37] | 1/23/M | Fever, sore throat, myopericarditis, arthralgia, hepatosplenomegaly | Leukocytosis, increased ESR &CRP, elevated ferritin, raised cardiac enzymes | Urticated and erythematous plaques and papules on the dorsum of right hand and fingers | Superficial and deep perivascular infiltrates of lymphocytes and neutrophils | Corticosteroids, NSAIDs, Azathioprine |
| Cho et al. [24] | 1/38/F | Fever, polyarthralgia, sore throat hepatosplenomegaly lymphadenopathy | Leukocytosis, elevated liver enzymes & ferritin | Prurigo pigmentosa-like persistent papules and plaques on anterior chest, abdomen, back | Parakeratosis, and perivascular infiltrations of lymphocytes, eosinophils and neutrophils in upper dermis | Methyl-prednisolone, Methotrexate, Hydroxychloroquine |
| Sarkar et al. [19] | 1/36/M | Fever, arthritis, hepatosplenomegaly hemophagocytic lymphohistiocytosis | Leukocytosis, anemia, increased ESR, CRP, liver enzymes & ferritin, hypoalbuminemia | Pigmented patches and plaques on chest, dermal and mucosal hyper-pigmentation | Multiple necrotic keratinocytes in aggregates in upper epidermis | Corticosteroids |
| Cossi et al. [38] | 1/35/M | Fever, cough, dyspnea myopericarditis | Increased CRP, liver enzymes & ferritin hypergammaglobulinemia | Pruritic erythematous-edematous plaques on trunk, upper limbs | Epidermal spongiosis, dermal infiltrate of perivascular lymphocytes and histiocytes, intra- vascular CD15+neutrophils | Methyl-prednisolone, Immunoglobulin IV Methotrexate |
The typical skin rash of AOSD is an evanescent salmon-pink non-pruritic or mildly pruritic maculopapular rash, with nonspecific histologic characteristics comprised of a superficial perivascular lymphocytic and scattered neutrophilic infiltrate in the upper epidermis [11–13]. The lesions often develop on the extremities and over the trunk during the peak of the fever and then resolve. AOSD can also present with various atypical cutaneous manifestations and persistent pruritic eruptions (PPEs) are common [14].
PPEs are polymorphic both in morphology and distribution patterns. The more common patterns include lichenoid, linear and dermographism-like eruptions [14], persistent pruritic coalescent papules and plaques [15–17] with linear pigmentation [18], dermal and mucosal hyperpigmentation [19], amyloidosis-like skin eruption [20], generalized peau d’orange appearance of the skin [21], generalized persistent erythema [22], prurigo pigmentosa-like eruption [23, 24], vesiculopustules [25], urticaria [26, 27] and fixed papular lesions [28]. The latter are characterized by atypical wheals, present for more than 24–36 h, with symmetrical distribution [29, 30]. Pruritic lesions are usually evident with the presence of linear dermographism from scratching, as was evident in our patient. The most common atypical rash manifestation in AOSD includes the persistent pruritic coalescent papules and plaques and linear lesions [31].
In addition to the typical maculopapular evanescent Still’s rash, our patient had also an atypical persistent pigmented eruption manifested with different cutaneous morphology and geographic distribution over his body. The linear urticarial streaky and dermographism-like eruptions on upper extremities and torso sequentially gave place to persistent erythematous plaques on his chest and abdomen. We believe that this type of polymorphic cutaneous eruption may be a predictor of severe systemic inflammatory disease like in our case, and could be associated with activation of macrophages and natural killer cells in addition with increased production of IL-2, interferon-γ and tumor necrosis factor (TNF)- α. High levels of IL-8 were demonstrated in Still’s rash and this cytokine is considered as the inducer of the acute phase of inflammatory cascade in AOSD [32]. We believe that the cutaneous response to Anakinra was slower than the systemic one, since the febrile episodes resolved rapidly after initiation of Anakinra whereas the skin lesions persisted. The introduction of Anakinra therapy in our patient may have slightly exacerbated the pre-existing cutaneous lesions and caused new ones at the initiation of the treatment probably due to its immune modulating effects. Anakinra has been shown to cause interstitial granulomatous drug reaction [33, 34]. The application of topical corticosteroids facilitated the resolution of the cutaneous manifestations.
The histological features of persistent eruptions include parakeratosis [35], necrotic keratinocytes in the upper epidermis and a perivascular and interstitial inflammatory infiltrate of lymphocytes and neutrophils in the upper- and mid-dermis [36–39]. In urticarial lesions the histopathologic findings demonstrate an intense infiltrate of mature CD15+ neutrophils between the dermal collagen bundles. This clinicopathological entity has recently been described as neutrophilic urticarial dermatosis (NUD) [40].
Dyskeratosis and dermal mucinosis represent distinctive cutaneous lesions of AOSD [41, 42]. The presence of fibrin thrombi in the small vessel with scarce inflammatory cell infiltration, suggestive of vasculopathy [25] has also been observed in cases of AOSD. Leukocytoclastic cutaneous vasculitis [43, 44] with mixed cryoglobulinemia [44] in AOSD has been described only rare in the literature.
Eosinophils that are commonly seen in drug-induced eruption are consistently lacking in the AOSD-associated skin lesions [14]. Perez et al. described a case of AOSD-related persistent erythematous rash characterized by papules and plaques in which skin biopsy revealed perivascular infiltration of the small vessels in the dermis by eosinophils, histiocytes and lymphocytes [45]. In our case, the histopathology findings of the new persistent cutaneous eruption included the presence of several perivascular eosinophils not just in the dermis but also in the interstitium. The eosinophilic cutaneous manifestation could be either drug-related (i.e. antibiotics, Anakinra) or AOSD-associated.
Treatment of AOSD has been empirical. Non-steroidal anti-inflammatory drugs (NSAIDs), oral corticosteroids, disease modifying anti-rheumatic drugs (DMARDs), methotrexate (MTX), cyclosporine, azathioprine, sulfasalazine and minocycline have been used to treat this rare disease. Recently effective biologic agents including TNF-a, IL-1 and IL-6 antagonist have been used for steroid-resistant AOSD [46]. Laskari et al. provided evidence that Anakinra monotherapy or in combination with a DMARD, such as MTX may be the treatment of choice for patients with refractory Still’s disease [47]. MTX is recommended in patients with polyarthritis and allows for steroid dose sparing in AOSD [48]. Our patient did not respond to corticosteroid treatment, but showed dramatic response to initiation of Anakinra treatment.
In summary, AOSD can manifest with atypical skin lesions that have highly distinctive but non-pathognomonic pathological features and are usually associated with severe disease. Still’s rash can mimic various disorders with maculopapular, urticarial, linear and lichenoid manifestations and skin biopsy of those atypical cutaneous lesions is strongly recommended before or during the treatment course of AOSD because it allows rheumatologists and pathologists to recognize those specific distinctive histopathological characteristics and put the correct diagnosis.
Acknowledgments
We thank Emeritus Professor H.M. Moutsopoulos, MD (Department of Pathophysiology, School of Medicine, National and Kapodistrian University of Athens) for his instructive comments and suggestions.
Compliance with ethical standards
Conflict of interest
There is no conflict of interest. All authors participated in the preparation of this manuscript.
Human and animal rights
For this case report formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Fautrel B. Adult-onset Still disease. Best Pract Res Clin Rheumatol. 2008;22(5):773–792. doi: 10.1016/j.berh.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Yamagushi M, Ohta A, Tsunematsu T, et al. Preliminary criteria for classification of adult Still’s disease. J Rheumatol. 1992;19:424–430. [PubMed] [Google Scholar]
- 3.Appenzeller S, Castro GR, Costallat LT, et al. Adult onset Still disease in southeast Brazil. J Clin Rheumatol. 2005;11:76–80. doi: 10.1097/01.rhu.0000158544.38663.0a. [DOI] [PubMed] [Google Scholar]
- 4.Jaime MAI, Baptista R, Azevedo MNL, et al. Adult onset Still’s disease: study on 25 cases. Rev Bras Rheumatol. 1998;38:285–290. [Google Scholar]
- 5.Crispin JC, Martinez-Banos D, Alcocer-Varela J. Adult-onset Still disease as the cause of fever of unknown origin. Medicine (Baltimore) 2005;84:331–337. doi: 10.1097/01.md.0000188009.47085.76. [DOI] [PubMed] [Google Scholar]
- 6.Bywaters EG. Still’s disease in the adult. Ann Rheum Dis. 1971;30(2):121–133. doi: 10.1136/ard.30.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dino O, Provenzano G, Giannuoli G, et al. Fulminant hepatic failure in adult onset Still’s disease. J Rheumatol. 1996;23(4):784–785. [PubMed] [Google Scholar]
- 8.Hirohata S, Kamoshita H, Taketani T, et al. Adult Still’s disease complicated with adult respiratory distress. Arch Intern Med. 1986;146(12):2409–2410. doi: 10.1001/archinte.1986.00360240157025. [DOI] [PubMed] [Google Scholar]
- 9.Vallianou NG, Kouvidou C, Naxaki A, et al. Acalculous cholecystitis with multiple organ failure and disseminated intravascular coagulation in a patient with adult onset Still’s disease. Ann Gastroenterol. 2014;27(3):289–290. [PMC free article] [PubMed] [Google Scholar]
- 10.Bae CB, Jung JY, Kim HA, et al. Reactive hemophagocytic syndrome in adult-onset Still disease: clinical features, predictive factors, and prognosis in 21 patients. Medicine (Baltimore). 2015;94(4):e451. doi: 10.1097/MD.0000000000000451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee JY, Yang C, Hsu MM. Histopathology of persistent papules and plaques in adult-onset Still’s disease. J Am Acad Dermpath. 2005;52:1003–1008. doi: 10.1016/j.jaad.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 12.Wouters JM, van Rijswijk MH, van de Putte LB. Adult onset Still’s disease in the elderly: a report of two cases. J Rheumatol. 1985;12(4):791–793. [PubMed] [Google Scholar]
- 13.Koga T, Tokunaga N, Ichikawa Y, et al. A 72-year-old female with adult Still’s disease. Intern Med. 1992;31(12):1356–1358. doi: 10.2169/internalmedicine.31.1356. [DOI] [PubMed] [Google Scholar]
- 14.Lee JY, Hsu CK, Liu MF, et al. Evanescent and persistent pruritic eruptions of adult-onset still disease: a clinical and pathologic study of 36 patients. Semin Arthritis Rheum. 2012;42(3):317–326. doi: 10.1016/j.semarthrit.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Kaur S, Bambery P, Dahr S. Persistent dermal plaque lesions in adult onset Still’s disease. Dermatology. 1994;188:241–242. doi: 10.1159/000247150. [DOI] [PubMed] [Google Scholar]
- 16.Yoshifuku A, Kawai K, Kanekura T. Adult-onset Still disease with peculiar persistent plaques and papules. Clin Exp Dermatol. 2014;39(4):503–505. doi: 10.1111/ced.12335. [DOI] [PubMed] [Google Scholar]
- 17.Thien Huong NT, Pitche P, Minh Hoa T et al (2005) Persistent pigmented plaques in adult-onset Still’s disease. Ann Dermatol Venereol. 132(8–9 Pt 1):693–696 (French) [DOI] [PubMed]
- 18.Suzuki K, Kimura Y, Aoki M et al (2001) Persistent plaques and linear pigmentation in adult-onset Still’s disease. Dermatology 202(4):333–335 (Review) [DOI] [PubMed]
- 19.Sarkar RN, Bhattacharya R, Bhattacharyya K, et al. Adult onset Still’s disease with persistent skin lesions complicated by secondary hemophagocytic lymphohistiocytosis. Int J Rheum Dis. 2014;17(1):118–121. doi: 10.1111/1756-185X.12170. [DOI] [PubMed] [Google Scholar]
- 20.Yammamoto M, Sueki H, Fujisawa R, et al. A case of adult Still’s disease with atypical rash. Rinsho Derma. 1999;41:365–368. [Google Scholar]
- 21.Phillips WG, Weller R, Handfield-Johnes SE, et al. Adult Still’s disease. Br J Dermatol. 1994;130:511–513. doi: 10.1111/j.1365-2133.1994.tb03388.x. [DOI] [PubMed] [Google Scholar]
- 22.Fujii K, Kobishi K, Kanno Y, et al. Persistent generalized erythema in adult-onset Still’s disease. Int J Dermatol. 2003;42:824–825. doi: 10.1046/j.1365-4362.2003.01761.x. [DOI] [PubMed] [Google Scholar]
- 23.Tomaru K, Nagai Y, Ohyama N, et al. Adult-onset Still’s disease with prurigo pigmentosa-like skin eruption. J Dermatol. 2006;33(1):55–58. doi: 10.1111/j.1346-8138.2006.00011.x. [DOI] [PubMed] [Google Scholar]
- 24.Cho YT, Liao YH. Prurigo pigmentosa-like persistent papules and plaques in a patient with adult-onset Still’s disease. Acta Derm Venereol. 2014;94(1):102–103. doi: 10.2340/00015555-1615. [DOI] [PubMed] [Google Scholar]
- 25.Lee JB, Kim JW, Lee SS, et al. Adult-onset Still’s disease with vesiculopustules on the hands and feet. J Korean Med Sci. 2002;17(6):852–855. doi: 10.3346/jkms.2002.17.6.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Criado PR, de Carvalho JF, Ayabe LA, et al. Urticaria and dermographism in patients with adult-onset Still’s disease. Rheumatol Int. 2012;32(8):2551–2555. doi: 10.1007/s00296-011-2025-5. [DOI] [PubMed] [Google Scholar]
- 27.Tay YK, Paz RS, Ng SK, et al. A case of adult onset Still’s disease presenting with fever and a rash. Ann Acad Med Singap. 1996;25(2):296–299. [PubMed] [Google Scholar]
- 28.Soy M. A case of adult-onset Still’s disease presenting with angioedema. Clin Rheumatol. 2004;23:92. doi: 10.1007/s10067-003-0822-2. [DOI] [PubMed] [Google Scholar]
- 29.Peroni A, Colato C, Zanoni G, et al. Urticarial lesions: if not urticarial, what else? The differential diagnosis of urticaria: part II. Systemic diseases. J Am Acad Dermatol. 2010;62:557–570. doi: 10.1016/j.jaad.2009.11.687. [DOI] [PubMed] [Google Scholar]
- 30.Setterfield JE, Hughes GRV. Kobza Black A. Urticaria as a presentation of adult Still’s disease. Br J Dermatol. 1998;138:904–927. doi: 10.1046/j.1365-2133.1998.02235.x. [DOI] [PubMed] [Google Scholar]
- 31.Criado RF, Criado PR, Vasconcellos C et al (2006) Urticaria as a cutaneous sign of adult-onset Still’s disease. J Cutan Med Surg 10(2):99–103 [DOI] [PubMed]
- 32.Chen DY, Lan JL, Lin FJ, et al. Proinflammatory cytokine profiles in sera and pathological tissues of patients with active untreated adult onset Still’s disease. J Rheumatol. 2004;31(11):2189–2198. [PubMed] [Google Scholar]
- 33.Regula CG, Hennessy J, Clarke LE, et al. Interstitial granulomatous drug reaction to anakinra. J Am Acad Dermatol. 2008;59:S25–S27. doi: 10.1016/j.jaad.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 34.Michailidou D, Voulgarelis M, Pikazis D (2014) Exacerbation of interstitial granulomatous dermatitis with arthritis by anakinra in a patient with diffuse large B-cell lymphoma. Clin Exp Rheumatol 32(2):259–261 [PubMed]
- 35.Lübbe J, Hofer M, Chavaz P, et al. Adult-onset Still’s disease with persistent plaques. Br J Dermatol. 1999;141(4):710–713. doi: 10.1046/j.1365-2133.1999.03115.x. [DOI] [PubMed] [Google Scholar]
- 36.Nagai Y, Hasegawa M, Okada E, et al. Clinical follow-up study of adult-onset Still’s disease. J Dermatol. 2012;39(11):898–901. doi: 10.1111/j.1346-8138.2012.01600.x. [DOI] [PubMed] [Google Scholar]
- 37.Yang CC, Lee JY, Liu MF et al (2006) Adult-onset Still’s disease with persistent skin eruption and fatal respiratory failure in a Taiwanese woman. Eur J Dermatol 16(5):593–594 [PubMed]
- 38.Salaffi F, Filosa G, Bugatti L, et al. Urticaria as a presenting manifestation of adult-onset Still’s disease. Clin Rheumatol. 2000;19(5):389–391. doi: 10.1007/s100670070034. [DOI] [PubMed] [Google Scholar]
- 39.Said NH, Wong SN, Tan WH. A case of adult-onset Still’s disease presenting with urticated plaques and acute myopericarditis. Indian J Dermatol. 2013;58(5):405. doi: 10.4103/0019-5154.117316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cozzi A, Papagrigoraki A, Biasi D et al (2014) Cutaneous manifestations of adult-onset Still’s disease: a case report and review of literature. Clin Rheumatol. doi:10.1007/s10067-014-2614-2 [DOI] [PubMed]
- 41.Wolgamot G, Yoo J, Hurst S, et al. Unique histopathologic findings in a patient with adult-onset Still disease. Am J Dermatopathol. 2007;29(2):194–196. doi: 10.1097/DAD.0b013e3180332826. [DOI] [PubMed] [Google Scholar]
- 42.Fortna RR, Gudjonsson JE, Seidel G, et al. Persistent pruritic papules and plaques: a characteristic histopathologic presentation seen in a subset of patients with adult-onset and juvenile Still’s disease. J Cutan Pathol. 2010;37(9):932–937. doi: 10.1111/j.1600-0560.2010.01570.x. [DOI] [PubMed] [Google Scholar]
- 43.Yanai H, Furutani N, Yoshida H, et al. Myositis, vasculitis, hepatic dysfunction in adult-onset Still’s disease. Case Rep Med. 2009;2009:504897. doi: 10.1155/2009/504897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Elezoglou AV, Giamarelos-Bourboulis E, Katsilambros N et al (2003) Cutaneous vasculitis associated with mixed cryoglobulinemia in adult Still’s disease. Clin Exp Rheumatol 21(3):405–406 [PubMed]
- 45.Perez C, Montes M, Gallego M, et al. Atypical presentation of adult Still’s disease with generalized rash and hyperferritinaemia. Br J Dermatol. 2001;145(1):187–188. doi: 10.1046/j.1365-2133.2001.04318.x. [DOI] [PubMed] [Google Scholar]
- 46.Franchini S, Dagna L, Salvo F, et al. Efficacy of traditional and biologic agents in different clinical phenotypes of adult-onset Still’s disease. Arthritis Rheum. 2010;62(8):2530–2535. doi: 10.1002/art.27532. [DOI] [PubMed] [Google Scholar]
- 47.Laskari K, Tzioufas AG, Moutsopoulos HM. Efficacy and long-term follow-up of IL-1R inhibitor anakinra in adults with Still’s disease: a case-series study. Arthritis Res Ther. 2011;13(3):R91. doi: 10.1186/ar3366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fautrel B, Borget C, Rozenberg S, et al. Corticosteroid sparing effect of low dose methotrexate treatment in adult Still’s disease. J Rheumatol. 1999;26(2):373–378. [PubMed] [Google Scholar]