Abstract
Background and objectives
Electronic health record (EHR) patient portals allow individuals to access their medical information with the intent of patient empowerment. However, little is known about portal use in nephrology patients. We addressed this gap by characterizing adoption of an EHR portal, assessing secular trends, and examining the association of portal adoption and BP control (<140/90 mmHg).
Design, setting, participants, & measurements
Patients seen between January 1, 2010, and December 31, 2012, at any of four university-affiliated nephrology offices who had at least one additional nephrology follow-up visit before June 30, 2013, were included. Sociodemographic characteristics, comorbidities, clinical measurements, and office visits were abstracted from the EHR. Neighborhood median household income was obtained from the American Community Survey 2012.
Results
Of 2803 patients, 1098 (39%) accessed the portal. Over 87% of users reviewed laboratory results, 85% reviewed their medical information (e.g., medical history), 85% reviewed or altered appointments, 77% reviewed medications, 65% requested medication refills, and 31% requested medical advice from their renal provider. In adjusted models, older age, African-American race (odds ratio [OR], 0.50; 95% confidence interval [95% CI], 0.39 to 0.64), Medicaid status (OR, 0.53; 95% CI, 0.36 to 0.77), and lower neighborhood median household income were associated with not accessing the portal. Portal adoption increased over time (2011 versus 2010: OR, 1.38 [95% CI, 1.09 to 1.75]; 2012 versus 2010: OR, 1.95 [95% CI, 1.44 to 2.64]). Portal adoption was correlated with BP control in patients with a diagnosis of hypertension; however, in the fully adjusted model this was somewhat attenuated and no longer statistically significant (OR, 1.11; 95% CI, 0.99 to 1.24).
Conclusion
While portal adoption appears to be increasing, greater attention is needed to understand why vulnerable populations do not access it. Future research should examine barriers to the use of e-health technologies in underserved patients with CKD, interventions to address them, and their potential to improve outcomes.
Keywords: healthcare disparities, personalized health record, chronic kidney disease, electronic health record, patient portal
Introduction
CKD contributes to substantial morbidity and mortality, particularly among vulnerable populations (1–11). Patient activation (the “knowledge, skills and confidence” needed to actively engage in care) (12) is a critical feature of CKD management, wherein BP self-monitoring, dietary modification, medication adherence, nephrotoxin avoidance, and patient-provider collaboration are essential (13–16). Enabling patients with CKD to easily access their medical information is a novel approach to facilitate patient engagement and activation (17). In other chronic disease settings, empowering patients in this fashion improves disease knowledge, enhances patient-provider communication, and increases adherence to treatment (18–23).
The United States government passed the Health Information Technology for Economic and Clinical Health (HITECH) Act (“meaningful use”) in 2009 to encourage providers to implement electronic health records (EHRs) and to promote EHR capabilities likely to improve care (24). Stage 1 of meaningful use required that providers offer patients timely electronic access to their health information, while stage 2 mandated that providers allow patients to view, download, and transmit their health information and to securely message their providers electronically (24,25). Many providers have adopted patient portals to accomplish these objectives (26). Portals are personalized health record applications tethered to a provider’s EHR. Most portals allow patients to review problem lists, laboratory results, and medications; schedule appointments; request prescription refills; and securely message their providers, thereby facilitating self-monitoring, self-care, and communication (17,20–23,27). However, differences in Internet access (i.e., the digital divide), computer literacy and Internet proficiency, as well as patient attitudes may limit portal adoption (28–31).
Few data characterize the use of EHR portals in nephrology patients. We sought to address this gap by examining portal use, including secular trends, in university-affiliated general nephrology clinics. Given previous literature indicating that underserved groups are less likely to use EHR portals (32–36), we hypothesized that race, neighborhood median household income, and insurance status would be associated with portal use and of particular concern in view of documented CKD disparities in these groups (1–11). In addition, we believed that BP control, a key modifiable outcome that affects CKD progression, would depend on patient adherence, self-monitoring, and patient-provider communication. Thus, we hypothesized that portal adoption would be independently associated with BP control in patients with a diagnosis of hypertension.
Materials and Methods
Portal Implementation
Four university-affiliated nephrology offices in western Pennsylvania with 24 attending providers activated a free patient portal tethered to an existing ambulatory EHR (Epic, Verona, WI) in May 2009. Office staff members routinely invited patients to sign up for the portal during the check-in process and provided access codes and instructions to interested individuals. Fliers and pamphlets written at a fifth- to sixth-grade level advertising the patient portal were displayed. After obtaining an access code, individuals had to go online and follow the short instructions to set up their secure account.
Study Setting and Design
We examined a retrospective cohort of outpatients followed at four general nephrology clinics from January 1, 2010, to December 31, 2012. We excluded the initial 7-month period after portal rollout to ensure familiarity with the portal and resolution of any difficulties encountered during rollout. Patient eligibility criteria were age ≥18 years, one nephrology office visit between January 1, 2010, and December 31, 2012, and at least one additional office visit before June 30, 2013, to ensure nephrologist continuity. The additional 6-month window ensured adequate follow up opportunities for patients first seen near the end of 2012. The University of Pittsburgh institutional review board approved this study.
Portal Use
Portal adoption was defined as one or more logins after the first renal office visit within the cohort period. Portal use was characterized by abstracting electronic patient activity logs and categorizing actions into the following bins: appointment-related tasks (i.e., reviewing, cancelling, confirming, or scheduling appointments), medical information-related tasks (i.e., reviewing the problem list, allergies, family and social history, immunizations, health maintenance schedule, vital signs, or health snapshot which incorporates several of these separate fields), laboratory-related tasks (i.e., reviewing laboratory results or upcoming orders), medication-related tasks (i.e., reviewing the medication list or requesting prescription refills), and requests for medical advice via secure messaging. Patients could perform more than one task per session and could complete multiple distinct activities within a single category during the same session (e.g., reviewing prior laboratory results and upcoming laboratory tests during a single session constituted two laboratory-related tasks). The portal sent alerts to a patient’s email address when new information or test results became available from any university-affiliated provider. Because tests related to a single visit often result over several days, patients may receive multiple alerts for a single set of tests. Alerts were also sent 1 week before scheduled appointments with an affiliated provider.
Covariates
As previously described (37,38), we abstracted sociodemographic characteristics, comorbidities, clinical measurements, laboratory values, and outpatient visit dates from the EHR for the cohort period. Briefly, race was self-reported and categorized as white, black, or other. Because of a limited number of nonwhite, nonblack patients, we dichotomized race as black or nonblack. Insurance status was categorized as private, Medicare, medical assistance/Medicaid, or self-pay. Comorbidities were determined on the basis of their presence on the patient’s problem list, as a billing diagnosis on two outpatient encounters, or active use of a specified medication (Supplemental Table 1) (7,37,39–47). The university-affiliated health system mandates that providers enter all prescriptions electronically and maintain an up-to-date medication list. Comorbidities were used to calculate a Charlson comorbidity index (CCI) score (48). Neighborhood median household income was obtained by linking residential ZIP codes (excluding post office boxes) to the American Community Survey 2012 (49).
CKD stage was categorized according to the National Kidney Foundation’s 2002 staging system (50). The four-variable Modification of Diet in Renal Disease study equation, which was used by local laboratories, was applied to determine baseline eGFR (51,52). Baseline urine dipsticks (performed routinely at each site with each office visit) were used to categorize albuminuria, with values ≥ 1+ deemed positive (7). Baseline values were defined as the earliest available value concurrent with or after a nephrology office visit within the cohort period. In most patients, these values were from the day of the office visit.
Nephrology and non-nephrology outpatient visits (within the university system) were abstracted from the EHR. Because a primary care provider (PCP) within the university setting could affect portal use, this was also included as a covariate.
BP Control
The association between BP control and portal use was examined in patients with a baseline diagnosis of hypertension (HTN). HTN was identified on the basis of two outpatient billing diagnoses, a problem list diagnosis, or the use of an antihypertensive medication (37–39,41–44). For patients with a diagnosis of HTN, all recorded office BP values from the cohort period were abstracted from the EHR. Clinic protocols require staff to record a seated BP upon placing the patient in an examination room. These are overwhelmingly automated cuff readings. If two BP values were recorded on the same day, the mean value was used as the BP for that day. Because optimal BP values in CKD remain controversial (53,54), the less restrictive goal of <140/90 mmHg was used. This ensured a BP goal that all providers could be expected to target.
Statistical Analyses
Sociodemographic characteristics, comorbidities, clinical measurements, and laboratory values were described using standard descriptive statistics. Continuous variables were compared using the Wilcoxon rank-sum test and categorical variables were compared using the chi-square test.
Logistic regression was used to assess the independent association between sociodemographic and clinical factors and portal use. Covariates for adjustment were chosen according to clinical significance and possible effect on portal adoption (1,3–8,10,11,13–15,29,31,33,34,36,54–63). Sociodemographic variables were age, sex, race, marital status, insurance status, neighborhood median household income, tobacco use, and follow-up duration. Clinical factors were HTN, hyperlipidemia, nephrolithiasis, history of kidney transplant, CCI, proteinuria, eGFR, number of nephrology visits, number of non-nephrology visits, and presence of a university-affiliated PCP. Neighborhood median household income and length of follow-up were non-normally distributed and natural log transformed. Age, number of nephrology visits, and number of non-nephrology visits were included in the model as nonlinear terms using restricted cubic splines with knots.
Temporal trends were assessed using logistic regression to examine the association between year of cohort entry and portal use while adjusting for sociodemographic and clinical variables. In addition, interactions between age, race, or insurance status and year of entry were examined to determine whether these variables modified temporal trends.
Mixed-effects logistic regression models were used to assess the independent association of portal adoption and BP control. This approach used repeated BP measures collected over time while using a clinically meaningful BP outcome (above or below the clinical target). This was done by dichotomizing each follow-up BP value for each patient as controlled (i.e., <140/90 mmHg) or uncontrolled. Most patients had multiple follow-up BPs and contributed controlled and uncontrolled BPs to the analysis. The model adjusted for correlated data (due to repeated BP measures by patient), the baseline systolic and diastolic BP value, baseline covariates, provider visits, and follow-up time. Age, number of nephrology visits, and number of non-nephrology visits were included in the model as nonlinear terms using restricted cubic splines with knots. Interaction terms between portal use and age, race, marital status, neighborhood median household income, and insurance status were also tested in the fully adjusted model.
Sensitivity analyses replaced the CCI with its individual components and excluded kidney transplant patients. All analyses used two-sided P values <0.05 for significance. Analyses were performed using R software, version 3.1.2 (64).
Results
Nearly 40% of patients used the EHR portal (Table 1). Portal users were younger and were more likely to be non-black, to be married, to have private insurance, and to have higher neighborhood median household income. Users were less likely to have diabetes, coronary artery disease, or congestive heart failure but were more likely to have had a kidney transplant.
Table 1.
Baseline characteristics
| Characteristic | Overall cohort | Portal user | Nonuser | P Valued |
|---|---|---|---|---|
| Patients, n (%) | 2803 | 1098 (39) | 1705 (61) | |
| Age (yr) | 61±17 | 58±16 | 63±18 | <0.001 |
| Women | 1387 (49) | 549 (50) | 838 (49) | 0.66 |
| Race | ||||
| White | 2200 (78) | 952 (87) | 1248 (73) | <0.001 |
| Black | 519 (19) | 114 (10) | 405 (24) | |
| Other | 84 (3) | 32 (3) | 52 (3) | |
| Married | 1512 (54) | 688 (63) | 824 (48) | <0.001 |
| Insurance | <0.001 | |||
| Private | 1309 (47) | 625 (57) | 684 (40) | |
| Medicaid | 201 (7) | 51 (5) | 150 (9) | |
| Medicare | 1108 (40) | 361 (33) | 747 (44) | |
| Self-pay/uninsured | 185 (7) | 61 (6) | 124 (7) | |
| Median household income ($1000) | 46.8 (38.7–58.3) | 48.7 (39.7–63.2) | 45.6 (37.6–55.6) | <0.001 |
| Diabetes mellitus | 1101 (39) | 395 (36) | 706 (41) | 0.004 |
| Hypertension | 2487 (89) | 977 (89) | 1510 (89) | 0.73 |
| Hyperlipidemia | 1730 (62) | 706 (64) | 1024 (60) | 0.02 |
| Coronary artery disease | 623 (22) | 217 (20) | 406 (24) | 0.01 |
| Congestive heart failure | 342 (12) | 99 (9) | 243 (14) | <0.001 |
| Cerebrovascular disease | 715 (26) | 299 (27) | 416 (24) | 0.09 |
| Peripheral vascular disease | 358 (13) | 134 (12) | 224 (13) | 0.46 |
| Tobacco use | 450 (16) | 131 (12) | 319 (19) | <0.001 |
| CKD stagea | 0.006 | |||
| Preserved eGFR/no proteinuria | 331 (12) | 151 (14) | 180 (11) | |
| 1 and 2 | 320 (12) | 137 (13) | 183 (11) | |
| 3a | 665 (24) | 280 (26) | 385 (23) | |
| 3b | 750 (27) | 291 (27) | 459 (28) | |
| 4 | 499 (18) | 168 (15) | 331 (20) | |
| 5 (non–dialysis-dependent) | 155 (6) | 54 (5) | 101 (6) | |
| Kidney transplant | 376 (13) | 211 (19) | 165 (10) | <0.001 |
| Nephrolithiasis | 300 (11) | 137 (12) | 163 (10) | 0.02 |
| Charlson comorbidity index | 5.7±2.3 | 5.6±2.3 | 5.7±2.3 | 0.25 |
| Systolic BP (mmHg) | 129 (118–142) | 128 (118–140) | 130 (120–142) | 0.002 |
| Diastolic BP (mmHg) | 76 (68–82) | 77 (70–84) | 75 (68–82) | 0.02 |
| Serum creatinineb (mg/dl) | 1.5 (1.1–2.0) | 1.4 (1.0–1.9) | 1.5 (1.1–2.1) | <0.001 |
| eGFRb (ml/min per 1.73 m2) | 44 (30–62) | 47 (32–66) | 42 (29–60) | <0.001 |
| Dipstick proteinuria (≥1+)c | 1032 (37) | 362 (33) | 670 (39) | <0.001 |
| Median follow-up duration (yr) | 2.3 (1.2–3.3) | 2.7 (1.5–3.3) | 2.1 (1.1–3.2) | <0.001 |
| Nephrology office visits/yr | 2.9 (1.8–5.2) | 2.7 (1.8–4.3) | 3.1 (1.9–5.8) | <0.001 |
| University-affiliated PCP | 1375 (49) | 623 (57) | 752 (44) | <0.001 |
| Outpatient visits with a university-affiliated provider (excluding nephrology) | 9 (3–19) | 11 (4–23) | 8 (2–17) | <0.001 |
| Baseline ACEi/ARB use | 1161 (41) | 462 (42) | 699 (41) | 0.57 |
Continuous variables are presented as means±SDs or medians and interquartile ranges. Categorical variables are expressed as frequencies and percentages. ACEi/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker.
n=2720. When CKD staging could not be performed because of missing eGFR/dipstick, International Classification of Diseases, Ninth Revision, billing codes were used to categorize CKD stage if available.
n=2668.
n=2742.
Chi-square or Wilcoxon-Mann-Whitney test used as appropriate.
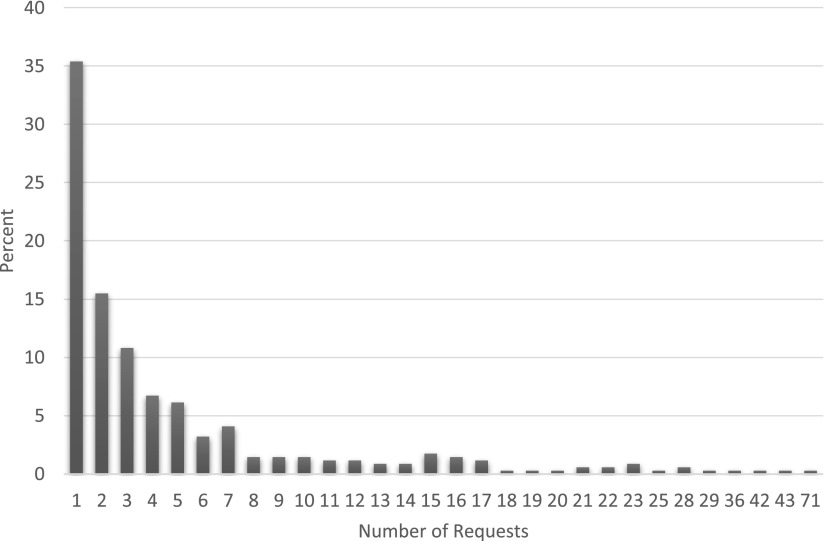
Portal users logged in a median of 18 times per year, and most completed a variety of tasks via the portal (Table 2). For example, 77% of users reviewed their medications, 65% requested medication refills, and 87% reviewed their laboratory results or upcoming laboratory orders, and patients performed these activities repeatedly (Table 2). Requests for medical advice were less common; 416 (38%) users submitted a request for medical advice to a provider within the health system, including 342 (31%) users who submitted a request to their renal provider. Patients requested medical advice from their providers relatively infrequently (Table 2). The median number of medical advice requests directed to a nephrology provider was two per patient (Figure 1).
Table 2.
Tasks performed via the electronic health record portal
| Task | Users Who Performed Task, n (%) | Rate of Task Performance per Yeara |
|---|---|---|
| Login | 1098 (100) | 18.1 (4.4–45.9) |
| Appointment related | 928 (85) | 8.1 (2.6–22.8) |
| Medical information related | 934 (85) | 4.0 (11.0–25.0) |
| Laboratory related | 957 (87) | 21.7 (7.3–51.3) |
| Medication related | 896 (82) | 3.6 (1.2–8.2) |
| Request for medical advice (any provider) | 416 (38) | 1.8 (0.76–5.3) |
Data restricted to portal users.
Data are expressed as median (interquartile range).
Figure 1.
Frequency of medical advice requests to renal providers over median follow-up of 2.5 years.
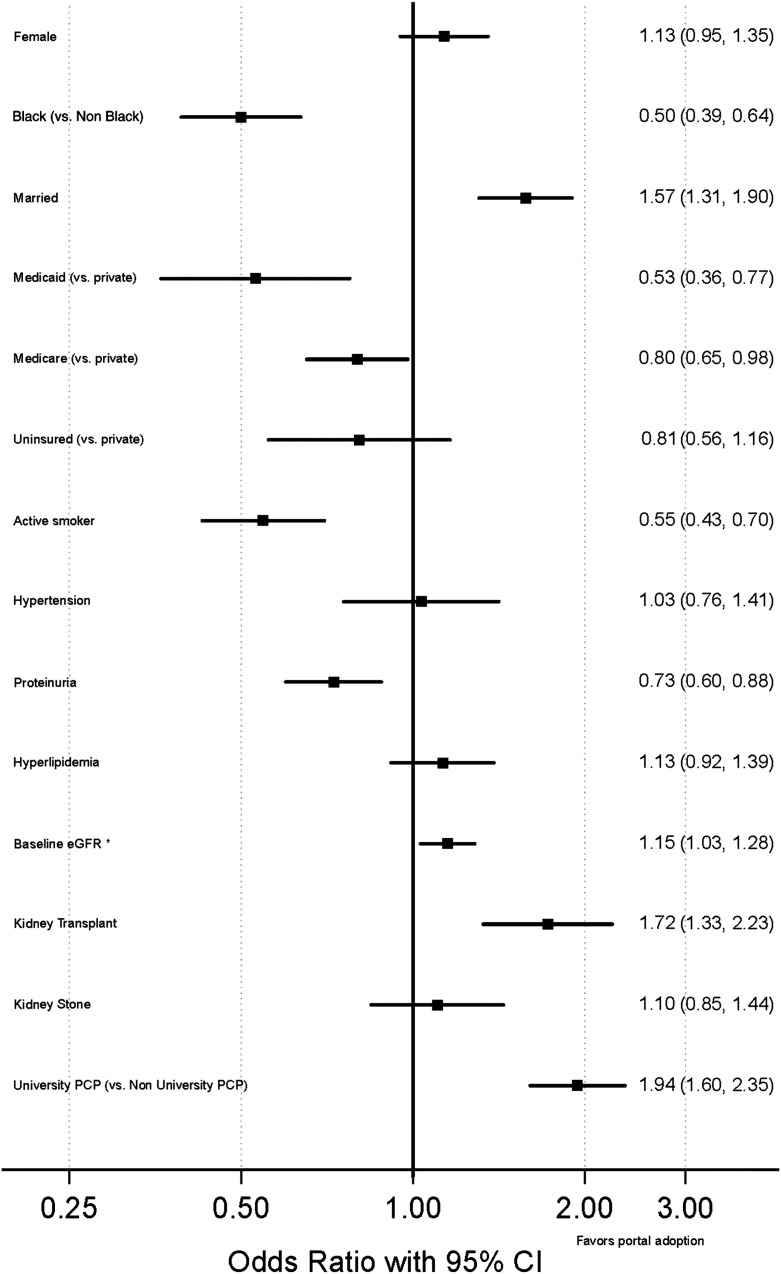
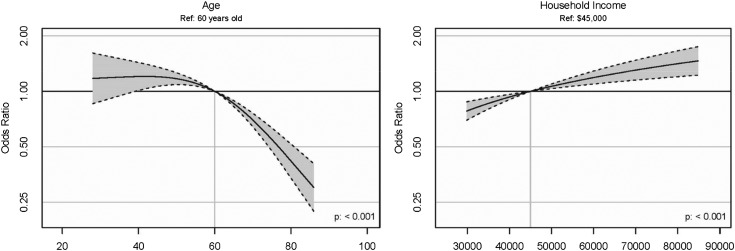
In the multivariable fully adjusted analyses, older age, black race, unmarried status, Medicaid or Medicare insurance (versus private), and lower neighborhood median household income were associated with not using the portal (Figure 2 and Supplemental Table 2). The observed associations were minimally affected by adjustments for confounders (Table 3). A general odds ratio (OR) and 95% confidence interval (95% CI) could not be provided for age and neighborhood median household income (because of nonlinear effects or the need for natural log transformation, respectively); the influence of these variables is depicted in Figure 3. In sensitivity analyses, excluding kidney transplant recipients or replacing the CCI with its components did not qualitatively alter the findings.
Figure 2.
Odds of portal use in fully adjusted model. Proteinuria defined as ≥1+ on dipstick. Model also adjusts for age, neighborhood median household income, Charlson comorbidity index, number of nephrology visits, and duration of follow-up. Because of nonlinear effects or log transformation, a generalized odds ratio cannot be provided for these variables. 95% CI, 95% confidence interval; PCP, primary care provider. *per 30 ml/min per 1.73 m2 increase.
Table 3.
Factors independently associated with electronic health record portal use
| Variable | OR (95% CI) | ||
|---|---|---|---|
| A | B | C | |
| Agea (80 yr versus 40 yr) | 0.35 (0.28 to 0.44) | 0.29 (0.22 to 0.38) | 0.29 (0.21 to 0.38) |
| Sex (female versus male) | 1.14 (0.97 to 1.35) | 1.13 (0.94 to 1.34) | 1.13 (0.95 to 1.35) |
| Black versus nonblack | 0.52 (0.42 to 0.66) | 0.50 (0.39 to 0.64) | 0.50 (0.39 to 0.64) |
| Marital status (married versus unmarried) | 1.50 (1.26 to 1.80) | 1.57 (1.30 to 1.89) | 1.57 (1.31 to 1.90) |
| Insurance status | |||
| Medicaid versus private | 0.56 (0.39 to 0.81) | 0.53 (0.36 to 0.77) | 0.53 (0.36 to 0.77) |
| Medicare versus private | 0.79 (0.65 to 0.96) | 0.80 (0.65 to 0.98) | 0.80 (0.65 to 0.98) |
| Self-pay versus private | 0.76 (0.54 to 1.09) | 0.81 (0.56 to 1.16) | 0.81 (0.56 to 1.16) |
| Median household income (per $40,000 versus $20,000)b | 1.57 (1.30 to 1.90) | 1.53 (1.26 to 1.86) | 1.53 (1.26 to 1.86) |
Model A: adjusted for age, sex, race, marital status, insurance status, neighborhood median household income, tobacco use, and length of follow-up; model B: variables for model A as well as hypertension, hyperlipidemia, nephrolithiasis, history of kidney transplant, proteinuria, eGFR, number of nephrology visits, number of non-nephrology outpatient visits, and university-affiliated primary care provider; model C: variables for models A and B as well as Charlson comorbidity index. OR, odds ratio; 95% CI, 95% confidence interval.
The reported odds ratio is comparison specific because of nonlinear effects.
The reported odds ratio is comparison specific because of natural logarithmic transformation.
Figure 3.
Association of age and neighborhood median household income with portal use in fully adjusted model. Because of nonlinear effects, age incorporates restricted cubic splines and knots. Solid line and shaded region depict point estimate and 95% confidence interval, respectively.
In adjusted models examining for secular trends, portal adoption increased in more recent years (2011 versus 2010: OR, 1.38 [95% CI, 1.09 to 1.75]; 2012 versus 2010: OR, 1.95 [95% CI, 1.44 to 2.64]). This effect did not vary by age, race, or insurance status (data not shown). In analyses stratified by year, disparities in portal adoption by age, race, and insurance status were qualitatively unchanged (data not shown).
To examine the potential health effect of portal use, we examined the association with BP control during the cohort period. We excluded patients without a baseline diagnosis of HTN (n=316) or who had only a single BP measurement during the cohort period (n=14). This left 2473 patients (88% of the cohort) with 38,420 available BP measurements. Patients had a median of 6 BP readings (interquartile range, 3–12). More portal users had BP values available for analysis, especially at longer follow-up intervals (Supplemental Table 3). In general, portal users had a modestly larger number of BP measurements during the study (Supplemental Table 4). Approximately 35% of all BP values were ≥140/90 mmHg; 2075 (84%) patients had at least one BP value ≥140/90 mmHg, while 2342 (94%) patients had at least one BP value <140/90 mmHg. The median of the proportion of patient BP values that were at goal over time is shown in Supplemental Figure 1. Portal use was independently associated with BP control (OR, 1.15; 95% CI, 1.02 to 1.29) after adjustment for age, sex, race, marital status, insurance status, neighborhood median household income, tobacco use, follow-up duration, and baseline systolic and diastolic BP. In the fully adjusted model (also controlling for hyperlipidemia, nephrolithiasis, history of kidney transplant, CCI, proteinuria, eGFR, number of nephrology and outpatient visits, and university-affiliated PCP), the association was somewhat attenuated (OR, 1.11; 95% CI, 0.99 to 1.24) and no longer significant. The association did not vary by age, race, marital status, insurance status, or neighborhood median household income (data not shown). In sensitivity analyses, excluding kidney transplant recipients from the fully adjusted model resulted in a borderline significant association between portal use and BP control (OR, 1.14; 95% CI, 1.00 to 1.29; P=0.05). Replacing the CCI with its components did not meaningfully affect the results (data not shown).
Discussion
Less than half of patients seen in four general nephrology clinics used the EHR-tethered patient portal. Most users accessed the portal many times and completed several tasks, suggesting that they found the portal convenient for reviewing their information and navigating the healthcare system. Although portal adoption increased across all groups in later cohort years, vulnerable groups were still less likely to use the patient portal. For example, Medicaid patients had 47% lower odds (versus the privately insured), blacks had 50% lower odds (versus nonblacks), and 80-year-old patients had 71% lower odds (versus 40-year-old patients) of portal use. In addition, portal adoption showed a borderline association with BP control in patients with HTN.
Although our study confirms significant portal adoption, underserved populations were often left behind. These findings comport with earlier studies in non-nephrology settings (32–36). While the increase in portal adoption across groups in more recent years suggests progress, the continued differences in portal adoption among nephrology patients are disquieting because socioeconomic and racial disparities in CKD outcomes are well documented (1–11). Disparities in the use of patient portals and emerging e-health technologies may reinforce or widen extant disparities. Our results are also notable because they represent a contemporary cohort (2010–2012) that coincides with a decline in the digital divide (57,61).
These findings highlight the need to ensure adequate resource allocation by health systems and government organizations to allow vulnerable populations to benefit from patient portals and other novel e-health applications. Unfortunately, our study design precluded an assessment of potential barriers and facilitators to portal use. However, determinants of portal adoption are likely to include patient comfort and proficiency with use of the Internet, experiences with Internet applications, available features, anticipated benefits, provider enthusiasm, patient engagement/activation, health literacy, communication preferences, and trust in the provider and health system (18,28,33–35,55,58,62,65,66). By anticipating digital deficiencies in older adults and underserved populations, healthcare organizations can develop onsite and remote training activities to enhance uptake of these new technologies (18,21,67–69). Organizations should also consider developing freely available, user-friendly applications that extend access to smartphones early in the rollout period. Frequently, these devices are the primary source of internet access for underserved communities (63). Because portal users frequently reviewed their laboratory results and medical information, studies are needed to understand how to tailor the information provided to optimize patient comprehension, especially in the setting of limited health literacy. In addition, research is needed to understand the features that nonadopters perceive as most beneficial (58,66). Such information could inform targeted marketing efforts and may help ensure more equitable use of portals or other e-health technologies.
Using patient portals to access one’s medical information improves disease knowledge, adherence, and self-efficacy; patient-provider communication; and coordination of care (18–22,60,70,71). These benefits are key aspects of the chronic care model and are critical to the long-term management of CKD (13,16,72,73). Portals may be particularly valuable in complex, chronic disease states, for which they offer patients the opportunity to review medications, laboratory results, and clinical guidance repeatedly and at their convenience (23,74). The ability to query providers and receive written responses may be similarly helpful.
Our study revealed a borderline association between BP control and portal use. This may have been facilitated by improvements in self-monitoring, patient-provider communication, refilling medications, or adherence to lifestyle modifications and antihypertensive medications. Prior studies examining the effect of patient portals on BP have yielded mixed results. A small randomized controlled trial that examined a diabetes patient portal with recommendations that were shared with providers demonstrated that individuals in the portal group were more likely to have an antihypertensive medication initiated or adjusted (59). Yet, the difference in BP between groups was not significant (59). Another small randomized controlled trial examining EHR portals in primary care patients with HTN found no change in BPs; however, only 50% of individuals in the intervention group used the portal at least once (62). Because portal use may itself serve as a marker of patient engagement, additional studies are needed to confirm our findings and to explore other potential health benefits in a nephrology setting. For example, portals can be modified to include CKD educational information (17,75), medication safety checks in the setting of impaired renal function (76), dietary guidance (77), and checklists and reminders regarding kidney transplant evaluation (17). Randomized controlled trials are needed to overcome potential confounding due to patient-level variables (e.g., health literacy, patient activation) that we could not discern.
Two common and related provider concerns regarding portal implementation are the lack of remuneration for time spent and the potential for patient “abuse” (19,78). Although we did not assess the provider burden, the patterns of use suggest that the overwhelming majority of patients are judicious in messaging providers. These findings complement surveys suggesting that providers perceive little change in workload following portal implementation (78,79).
Our findings should be interpreted in light of a few limitations. First, our study design is susceptible to residual confounding (e.g., cognitive deficits, patient activation) and ascertainment bias (e.g., less frequent BP measurements in poorly adherent patients). Second, for most portal functions, we could not determine whether the patient was performing tasks related to their CKD or other health conditions (e.g., diabetes mellitus, HTN). However, we believe CKD self-care should be viewed in the patient-centered context of health self-care. Indeed, patients with CKD frequently have multiple comorbidities that are risk factors for or complications of kidney disease. Third, variables recorded in the EHR, including BP, may be misclassified. However, a prior study demonstrated reasonable agreement between EHR-recorded and research visit BP values (80) and misclassification would be expected to bias toward the null. Fourth, we did not examine whether portal use affected more salient clinical outcomes such as progression to ESRD. Finally, this was a single-center study limiting generalizability. Larger, longer studies with additional clinical outcomes are necessary to delineate the potential benefits of patient portals in a nephrology setting.
In conclusion, nearly 40% of nephrology patients used an EHR portal to perform a variety of tasks, including to schedule appointments, review laboratory results, refill medications, and send a message their renal provider. Portal adoption increased over time in all groups; however, vulnerable groups were substantially less likely to use the portal. These differences in adoption raise concerns of widening disparities in CKD outcomes.
Disclosures
None.
Supplementary Material
Acknowledgments
This work was supported by an American Heart Association grant 11FTF7520014 (M.J.) and National Institutes of Health grants K24DK62849 (T.A.I.) and K23DK090304 (K.A.K.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
An abstract based on these findings was presented at American Society of Nephrology Kidney Week 2014 (Philadelphia, PA).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Electronic Health Record Patient Portals in CKD and Hypertension Management: Meaningfully Used?,” on pages 1897–1899.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.01640215/-/DCSupplemental.
References
- 1.Lipworth L, Mumma MT, Cavanaugh KL, Edwards TL, Ikizler TA, Tarone RE, McLaughlin JK, Blot WJ: Incidence and predictors of end stage renal disease among low-income blacks and whites. PLoS One 7: e48407, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xue JL, Eggers PW, Agodoa LY, Foley RN, Collins AJ: Longitudinal study of racial and ethnic differences in developing end-stage renal disease among aged medicare beneficiaries. J Am Soc Nephrol 18: 1299–1306, 2007 [DOI] [PubMed] [Google Scholar]
- 3.McClellan WM, Warnock DG, Judd S, Muntner P, Kewalramani R, Cushman M, McClure LA, Newsome BB, Howard G: Albuminuria and racial disparities in the risk for ESRD. J Am Soc Nephrol 22: 1721–1728, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martins D, Tareen N, Zadshir A, Pan D, Vargas R, Nissenson A, Norris K: The association of poverty with the prevalence of albuminuria: Data from the Third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis 47: 965–971, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hossain MP, Goyder EC, Rigby JE, El Nahas M: CKD and poverty: A growing global challenge. Am J Kidney Dis 53: 166–174, 2009 [DOI] [PubMed] [Google Scholar]
- 6.Choi AI, Rodriguez RA, Bacchetti P, Bertenthal D, Hernandez GT, O’Hare AM: White/black racial differences in risk of end-stage renal disease and death. Am J Med 122: 672–678, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY: Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351: 1296–1305, 2004 [DOI] [PubMed] [Google Scholar]
- 8.McClellan WM, Newsome BB, McClure LA, Howard G, Volkova N, Audhya P, Warnock DG: Poverty and racial disparities in kidney disease: The REGARDS study. Am J Nephrol 32: 38–46, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Stamler J: End-stage renal disease in African-American and white men. 16-year MRFIT findings. JAMA 277: 1293–1298, 1997 [PubMed] [Google Scholar]
- 10.Nicholas SB, Kalantar-Zadeh K, Norris KC: Socioeconomic disparities in chronic kidney disease. Adv Chronic Kidney Dis 22: 6–15, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johns TS, Estrella MM, Crews DC, Appel LJ, Anderson CAM, Ephraim PL, Cook C, Boulware LE: Neighborhood socioeconomic status, race, and mortality in young adult dialysis patients. J Am Soc Nephrol 25: 2649–2657, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hibbard JH, Stockard J, Mahoney ER, Tusler M: Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Serv Res 39: 1005–1026, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greer R, Boulware LE: Reducing CKD risks among vulnerable populations in primary care. Adv Chronic Kidney Dis 22: 74–80, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson ML: Relationships between and Group Differences in Patient Activation and Knowledge, Skills, Confidence, and Biomarkers in Chronic Kidney Disease, Ann Arbor, University of Nebraska Medical Center, 2014, p 184 [Google Scholar]
- 15.Costantini L, Beanlands H, McCay E, Cattran D, Hladunewich M, Francis D: The self-management experience of people with mild to moderate chronic kidney disease. Nephrol Nurs J 35: 147–155, quiz 156, 2008 [PubMed] [Google Scholar]
- 16.Ong SW, Jassal SV, Porter E, Logan AG, Miller JA: Using an electronic self-management tool to support patients with chronic kidney disease (CKD): A CKD clinic self-care model. Semin Dial 26: 195–202, 2013 [DOI] [PubMed] [Google Scholar]
- 17.Navaneethan SD, Jolly SE, Sharp J, Jain A, Schold JD, Schreiber MJ, Jr, Nally JV, Jr: Electronic health records: A new tool to combat chronic kidney disease? Clin Nephrol 79: 175–183, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferreira A, Correia A, Silva A, Corte A, Pinto A, Saavedra A, Pereira AL, Pereira AF, Cruz-Correia R, Antunes LF: Why facilitate patient access to medical records. Stud Health Technol Inform 127: 77–90, 2007 [PubMed] [Google Scholar]
- 19.van der Vaart R, Drossaert CH, Taal E, van de Laar MA: Giving rheumatology patients online home access to their electronic medical record (EMR): Advantages, drawbacks and preconditions according to care providers. Rheumatol Int 33: 2405–2410, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osborn CY, Mayberry LS, Mulvaney SA, Hess R: Patient web portals to improve diabetes outcomes: A systematic review. Curr Diab Rep 10: 422–435, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nazi KM, Hogan TP, McInnes DK, Woods SS, Graham G: Evaluating patient access to Electronic Health Records: Results from a survey of veterans. Med Care 51[Suppl 1]: S52–S56, 2013 [DOI] [PubMed] [Google Scholar]
- 22.Ross SE, Lin CT: The effects of promoting patient access to medical records: A review. J Am Med Inform Assoc 10: 129–138, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ross SE, Moore LA, Earnest MA, Wittevrongel L, Lin CT: Providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res 6: e12, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wright A, Feblowitz J, Samal L, McCoy AB, Sittig DF: The Medicare Electronic Health Record Incentive Program: Provider performance on core and menu measures. Health Serv Res 49: 325–346, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.HealthIT.gov. Step 5: Achieve Meaningful Use Stage 2. Available at: http://www.healthit.gov/providers-professionals/step-5-achieve-meaningful-use-stage-2 Accessed January 19, 2015
- 26.Turvey C, Klein D, Fix G, Hogan TP, Woods S, Simon SR, Charlton M, Vaughan-Sarrazin M, Zulman DM, Dindo L, Wakefield B, Graham G, Nazi K: Blue Button use by patients to access and share health record information using the Department of Veterans Affairs’ online patient portal. J Am Med Inform Assoc 21: 657–663, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaw RJ, Ferranti J: Patient-provider internet portals–patient outcomes and use. Comput Inform Nurs 29: 714–718, 2011 [DOI] [PubMed] [Google Scholar]
- 28.Wright Nunes JA, Osborn CY, Ikizler TA, Cavanaugh KL: Health numeracy: Perspectives about using numbers in health management from African American patients receiving dialysis. Hemodial Int 19: 287–295, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hsu J, Huang J, Kinsman J, Fireman B, Miller R, Selby J, Ortiz E: Use of e-Health services between 1999 and 2002: A growing digital divide. J Am Med Inform Assoc 12: 164–171, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weingart SN, Rind D, Tofias Z, Sands DZ: Who uses the patient internet portal? The PatientSite experience. J Am Med Inform Assoc 13: 91–95, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fowles JB, Kind AC, Craft C, Kind EA, Mandel JL, Adlis S: Patients’ interest in reading their medical record: Relation with clinical and sociodemographic characteristics and patients’ approach to health care. Arch Intern Med 164: 793–800, 2004 [DOI] [PubMed] [Google Scholar]
- 32.Ketterer T, West DW, Sanders VP, Hossain J, Kondo MC, Sharif I: Correlates of patient portal enrollment and activation in primary care pediatrics. Acad Pediatr 13: 264–271, 2013 [DOI] [PubMed] [Google Scholar]
- 33.Yamin CK, Emani S, Williams DH, Lipsitz SR, Karson AS, Wald JS, Bates DW: The digital divide in adoption and use of a personal health record. Arch Intern Med 171: 568–574, 2011 [DOI] [PubMed] [Google Scholar]
- 34.Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW: Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med 26: 1112–1116, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, López A, Schillinger D: Social disparities in internet patient portal use in diabetes: Evidence that the digital divide extends beyond access. J Am Med Inform Assoc 18: 318–321, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ancker JS, Barrón Y, Rockoff ML, Hauser D, Pichardo M, Szerencsy A, Calman N: Use of an electronic patient portal among disadvantaged populations. J Gen Intern Med 26: 1117–1123, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abdel-Kader K, Fischer GS, Johnston JR, Gu C, Moore CG, Unruh ML: Characterizing pre-dialysis care in the era of eGFR reporting: A cohort study. BMC Nephrol 12: 12, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abdel-Kader K, Fischer GS, Li J, Moore CG, Hess R, Unruh ML: Automated clinical reminders for primary care providers in the care of CKD: A small cluster-randomized controlled trial. Am J Kidney Dis 58: 894–902, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tu K, Campbell NRC, Chen Z-L, Cauch-Dudek KJ, McAlister FA: Accuracy of administrative databases in identifying patients with hypertension. Open Med 1: e18–e26, 2007 [PMC free article] [PubMed] [Google Scholar]
- 40.Singh JA: Accuracy of Veterans Affairs databases for diagnoses of chronic diseases. Prev Chronic Dis 6: A126, 2009 [PMC free article] [PubMed] [Google Scholar]
- 41.Birtwhistle R, Keshavjee K, Lambert-Lanning A, Godwin M, Greiver M, Manca D, Lagacé C: Building a pan-Canadian primary care sentinel surveillance network: Initial development and moving forward. J Am Board Fam Med 22: 412–422, 2009 [DOI] [PubMed] [Google Scholar]
- 42.Kadhim-Saleh A, Green M, Williamson T, Hunter D, Birtwhistle R: Validation of the diagnostic algorithms for 5 chronic conditions in the Canadian Primary Care Sentinel Surveillance Network (CPCSSN): A Kingston Practice-based Research Network (PBRN) report. J Am Board Fam Med 26: 159–167, 2013 [DOI] [PubMed] [Google Scholar]
- 43.de Burgos-Lunar C, Salinero-Fort MA, Cárdenas-Valladolid J, Soto-Díaz S, Fuentes-Rodríguez CY, Abánades-Herranz JC, del Cura-González I: Validation of diabetes mellitus and hypertension diagnosis in computerized medical records in primary health care. BMC Med Res Methodol 11: 146–146, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Szeto HC, Coleman RK, Gholami P, Hoffman BB, Goldstein MK: Accuracy of computerized outpatient diagnoses in a Veterans Affairs general medicine clinic. Am J Manag Care 8: 37–43, 2002 [PubMed] [Google Scholar]
- 45.Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF: Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care 43: 480–485, 2005 [DOI] [PubMed] [Google Scholar]
- 46.Deyo RA, Cherkin DC, Ciol MA: Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45: 613–619, 1992 [DOI] [PubMed] [Google Scholar]
- 47.Tonelli M, Wiebe N, Fortin M, Guthrie B, Hemmelgarn BR, James MT, Klarenbach SW, Lewanczuk R, Manns BJ, Ronksley P, Sargious P, Straus S, Quan H, Alberta Kidney Disease Network : Methods for identifying 30 chronic conditions: Application to administrative data. BMC Med Inform Decis Mak 15: 31, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40: 373–383, 1987 [DOI] [PubMed] [Google Scholar]
- 49.U.S. Census Bureau: American Community Survey, 2012 American Community Survey 5-Year Estimates. S1903 Median Income in the Past 12 Months, using American FactFinder. Available at: http://factfinder.census.gov Accessed September 18, 2014
- 50.National Kidney Foundation : K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39[Suppl 1]: S1–S266, 2002 [PubMed] [Google Scholar]
- 51.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D, Modification of Diet in Renal Disease Study Group : A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann Intern Med 130: 461–470, 1999 [DOI] [PubMed] [Google Scholar]
- 52.Levey AS, Coresh J, Greene T, Marsh J, Stevens LA, Kusek JW, Van Lente F, Chronic Kidney Disease Epidemiology Collaboration : Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem 53: 766–772, 2007 [DOI] [PubMed] [Google Scholar]
- 53.Lewis JB: Blood pressure control in chronic kidney disease: Is less really more? J Am Soc Nephrol 21: 1086–1092, 2010 [DOI] [PubMed] [Google Scholar]
- 54.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Jr, Narva AS, Ortiz E: 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311: 507–520, 2014 [DOI] [PubMed] [Google Scholar]
- 55.Butler JM, Carter M, Hayden C, Gibson B, Weir C, Snow L, Morales J, Smith A, Bateman K, Gundlapalli AV, Samore M: Understanding adoption of a personal health record in rural health care clinics: Revealing barriers and facilitators of adoption including attributions about potential patient portal users and self-reported characteristics of early adopting users. AMIA Annu Symp Proc 2013: 152–161, 2013 [PMC free article] [PubMed] [Google Scholar]
- 56.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS: Prevalence of chronic kidney disease in the United States. JAMA 298: 2038–2047, 2007 [DOI] [PubMed] [Google Scholar]
- 57.File T: Computer and Internet use in the United States: Population characteristics. US Census Bureau. May 2013. Available at: http://www.census.gov/prod/2013pubs/p20-569.pdf, accessed on January 2, 2015
- 58.Goel MS, Brown TL, Williams A, Cooper AJ, Hasnain-Wynia R, Baker DW: Patient reported barriers to enrolling in a patient portal. J Am Med Inform Assoc 18[Suppl 1]: i8–i12, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Grant RW, Wald JS, Schnipper JL, Gandhi TK, Poon EG, Orav EJ, Williams DH, Volk LA, Middleton B: Practice-linked online personal health records for type 2 diabetes mellitus: A randomized controlled trial. Arch Intern Med 168: 1776–1782, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lyles CR, Sarkar U, Ralston JD, Adler N, Schillinger D, Moffet HH, Huang ES, Karter AJ: Patient-provider communication and trust in relation to use of an online patient portal among diabetes patients: The Diabetes and Aging Study. J Am Med Inform Assoc 20: 1128–1131, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Smith A: African Americans and technology use: A demographic portrait. Pew Research Center. January 6, 2014. Available at: http://www.pewinternet.org/files/2014/01/African-Americans-and-Technology-Use.pdf Accessed January 2, 2015
- 62.Wagner PJ, Dias J, Howard S, Kintziger KW, Hudson MF, Seol Y-H, Sodomka P: Personal health records and hypertension control: A randomized trial. J Am Med Inform Assoc 19: 626–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zickuhr K, Smith A: Digital differences. Pew Research Center. April 13, 2012. Available at: http://www.pewinternet.org/files/old-media//Files/Reports/2012/PIP_Digital_differences_041312.pdf Accessed January 2, 2015
- 64.R: A language and environment for statistical computing,Vienna, Austria, R Foundation for Statistical Computing, 2013 [Google Scholar]
- 65.Wade-Vuturo AE, Mayberry LS, Osborn CY: Secure messaging and diabetes management: experiences and perspectives of patient portal users. J Am Med Inform Assoc 20: 519–525, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ronda MC, Dijkhorst-Oei LT, Rutten GE: Reasons and barriers for using a patient portal: Survey among patients with diabetes mellitus. J Med Internet Res 16: e263, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lai AM, Kaufman DR, Starren J: Training digital divide seniors to use a telehealth system: A remote training approach. AMIA Annu Symp Proc 459–463, 2006 [PMC free article] [PubMed] [Google Scholar]
- 68.Sanders MR, Winters P, Fortuna RJ, Mendoza M, Berliant M, Clark L, Fiscella K: Internet access and patient portal readiness among patients in a group of inner-city safety-net practices. J Ambul Care Manage 36: 251–259, 2013 [DOI] [PubMed] [Google Scholar]
- 69.McInnes DK, Solomon JL, Shimada SL, Petrakis BA, Bokhour BG, Asch SM, Nazi KM, Houston TK, Gifford AL: Development and evaluation of an internet and personal health record training program for low-income patients with HIV or hepatitis C. Med Care 51[Suppl 1]: S62–S66, 2013 [DOI] [PubMed] [Google Scholar]
- 70.Otte-Trojel T, de Bont A, Rundall TG, van de Klundert J: How outcomes are achieved through patient portals: A realist review. J Am Med Inform Assoc 21: 751–757, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.McCarrier KP, Ralston JD, Hirsch IB, Lewis G, Martin DP, Zimmerman FJ, Goldberg HI: Web-based collaborative care for type 1 diabetes: A pilot randomized trial. Diabetes Technol Ther 11: 211–217, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wagner EH: Chronic disease management: What will it take to improve care for chronic illness? Eff Clin Pract 1: 2–4, 1998 [PubMed] [Google Scholar]
- 73.Diamantidis CJ, Becker S: Health information technology (IT) to improve the care of patients with chronic kidney disease (CKD). BMC Nephrol 15: 7, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fisher B, Bhavnani V, Winfield M: How patients use access to their full health records: A qualitative study of patients in general practice. J R Soc Med 102: 539–544, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Diamantidis CJ, Zuckerman M, Fink W, Hu P, Yang S, Fink JC: Usability of a CKD educational website targeted to patients and their family members. Clin J Am Soc Nephrol 7: 1553–1560, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Diamantidis CJ, Zuckerman M, Fink W, Aggarwal S, Prakash D, Fink JC: Usability testing and acceptance of an electronic medication inquiry system for CKD patients. Am J Kidney Dis 61: 644–646, 2013 [DOI] [PubMed] [Google Scholar]
- 77.Diamantidis CJ, Fink W, Yang S, Zuckerman MR, Ginsberg J, Hu P, Xiao Y, Fink JC: Directed use of the internet for health information by patients with chronic kidney disease: Prospective cohort study. J Med Internet Res 15: e251, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Keplinger LE, Koopman RJ, Mehr DR, Kruse RL, Wakefield DS, Wakefield BJ, Canfield SM: Patient portal implementation: Resident and attending physician attitudes. Fam Med 45: 335–340, 2013 [PMC free article] [PubMed] [Google Scholar]
- 79.Earnest MA, Ross SE, Wittevrongel L, Moore LA, Lin CT: Use of a patient-accessible electronic medical record in a practice for congestive heart failure: Patient and physician experiences. J Am Med Inform Assoc 11: 410–417, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fishman PA, Anderson ML, Cook AJ, Ralston JD, Catz SL, Carlson J, Larson EB, Green BB: Accuracy of blood pressure measurements reported in an electronic medical record during routine primary care visits. J Clin Hypertens (Greenwich) 13: 821–828, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.