Abstract
Background and objectives
Prompt recognition of severe renal impairment could improve the early management of critically ill patients. We compared the value of kinetic eGFR, plasma neutrophil gelatinase–associated lipocalin (NGAL), and urine tissue inhibitor of metalloproteinase-2 and urine insulin-like growth factor–binding protein 7 ([TIMP-2]*[IGFBP7]) in predicting short-term recovery from AKI and major adverse kidney events.
Design, setting, participants, & measurements
During the 6-month study period, 245 patients were admitted to our intensive care unit. This study included 57 consecutive patients presenting with AKI within the first 24 hours after admission. AKI markers were evaluated at inclusion (day 0) and 24 hours later (day 1). Kinetic eGFR was calculated on day 1 according to serum creatinine evolution. Renal recovery was defined as normalization of serum creatinine with reversal of oliguria within 48 hours. Major adverse kidney events included death, need for RRT, or persistence of renal dysfunction at hospital discharge.
Results
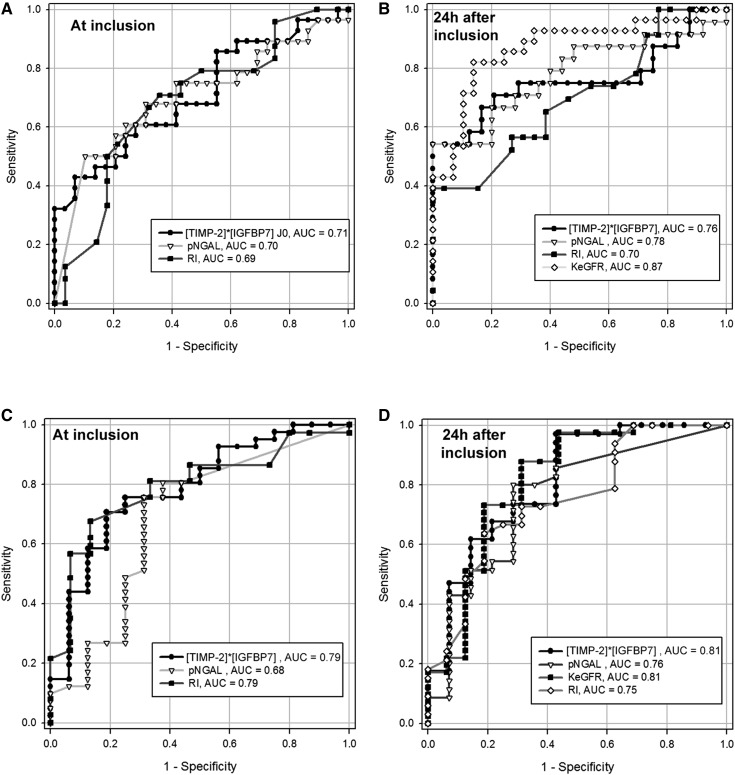
Plasma NGAL and [TIMP-2]*[IGFBP7] predicted renal recovery, with area under the receiver-operating characteristic curve (AUC-ROC) values between 0.70 and 0.79 at inclusion. Although plasma NGAL values frequently reached the maximal measurement range, their decrease on day 1 predicted recovery. The kinetic eGFR calculation after initial resuscitation provided the best AUC-ROC value for renal recovery, at 0.87. The best predictions for major adverse kidney events were provided by [TIMP-2]*[IGFBP7] and kinetic eGFR (equal AUC-ROCs of 0.81). Combining AKI markers in addition to clinical prediction models improved the discrimination and reclassification of patients who will recover from AKI or suffer from major adverse kidney events.
Conclusions
Biomarkers of kidney damage predicted short-term renal recovery and major adverse kidney events for an unselected cohort of critically ill patients. Calculating the kinetic eGFR imposed a delay after initial resuscitation but provided a good diagnostic and prognostic approach. The utility of functional and damage AKI marker combinations in addition to clinical information requires validation in larger prospective studies.
Keywords: AKI, biomarkers, neutrophil gelatinase–associated lipocalin, NGAL, [TIMP-2]*[IGFBP7], Doppler ultrasonography
Introduction
Renal failure is a common clinical problem in critically ill and high-risk surgical patients (1), and it remains associated with markedly worse outcomes (2–4). The most recent definition of AKI proposed by the Kidney Disease Improving Global Outcomes (KDIGO) Clinical Practice Work Group details three stages of severity according to changes in serum creatinine (sCr) and urine output (5). However, oliguria is poorly specified in renal dysfunction as it can be realted to normal kidney function, whereas sCr is recognized as a delayed indicator of renal-filtration function (6). Neutrophil gelatinase–associated lipocalin (NGAL) and the recent combination of tissue inhibitor of metalloproteinase-2 and urine insulin-like growth factor–binding protein 7 ([TIMP-2]*[IGFBP7]) are two novel biomarkers that can be utilized to assess kidney structural damage and predict AKI before sCr increases (7–10). However, critically ill patients often suffer from AKI at the time of intensive care unit (ICU) admission. We conducted an observational study to (1) test the hypothesis that these markers could also estimate the severity of renal injury at admission and (2) assess the predictive value of plasma neutrophil gelatinase–associated lipocalin (NGAL), [TIMP-2]*[IGFBP7], and kinetic eGFR on short-term renal recovery and major adverse kidney events in critically ill patients.
Materials and Methods
Setting and Patients
Our institutional review board (Comité de Protection des Personnes Sud-Ouest et Outre Mer III, Bordeaux, France Pellegrin Hospital, Bordeaux, France, agreement number DC2013/21) approved this noninterventional study. Because data and blood samples were collected in accordance with standard procedures currently used in patient care at our institute, authorization was granted to waive informed consent for this study.
During the 6-month study period (November 2012–April 2013), consecutive patients diagnosed with AKI in the first 24 hours after admission to our 12-bed mixed medical and surgical ICU (thoracic or abdominal surgery) were prospectively included. Exclusion criteria were pregnancy, age <18 years, obstructive renal disease, known ESRD, CKD defined by a GFR <30 ml/min per 1.73 m2, or a presumed life expectancy of <24 hours. The attending physician treated the selected cohort according to international recommendations and standards of care. Antibiotics were administered within the first hours after admission if requested. Initial management included fluid resuscitation with crystalloids (NaCl 0.9%, Ringer’s lactate, or Ringer’s acetate-malate solutions) to achieve rapid hemodynamic stabilization (mean arterial pressure >65 mmHg), lactate normalization, and improved urine output. Transfusion of albumin and blood products was considered if large amounts of crystalloid solution were needed. If fluid resuscitation was insufficient, NE was rapidly introduced. We used an arterial line and echocardiography to monitor hemodynamics in all patients. The PiCCO system (Pulsion Medical Systems, Munich, Germany) was proposed to continuously monitor cardiac output for the most severe patients. Under mechanical ventilation, the tidal volume was set to maintain an inspiratory plateau pressure <30 cm H2O. Daily fluid balance was calculated as the difference between total input and output. Patient outcomes on the 30th day after enrollment were recorded.
Definitions
According to the KDIGO staging system, AKI was defined as urine volume <0.5 ml/kg per hour for 6 hours, an sCr increase ≥0.35 mg/dl within 48 hours, or an sCr increase of 1.5 times the baseline value known to have occurred within the prior 7 days (5). The lowest sCr level measured in blood samples within the prior 7 days before inclusion was used as the sCr baseline.
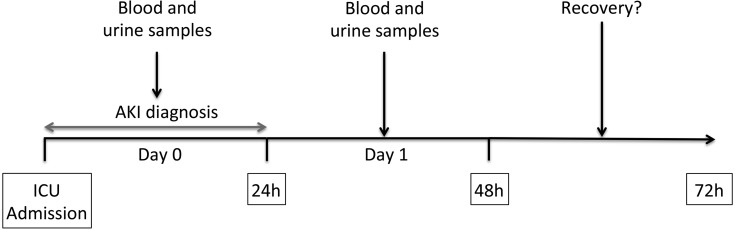
The primary end point was AKI recovery within 48 hours after inclusion, which was defined as a return to a sCr value <1.5 times the baseline value or <0.35 mg/dl above the baseline value with reversal of oliguria (in the absence of diuretic treatment; Figure 1) (11,12). For patients who had both oliguria and changes in sCr defining AKI, both corrections were required to define recovery. Nonrecovery was defined as a steady or higher AKI stage according to the KDIGO classification. The secondary end point was the occurrence of major adverse kidney events, which were defined as death, need for RRT, or persistence of renal dysfunction (defined by a sCr of ≥200% above reference) at hospital discharge truncated at 30 days (8,13).
Figure 1.
The study protocol. Patients diagnosed with AKI in the first 24 hours after ICU admission according to the KDIGO definition were included. Blood and urine samples were collected at inclusion and 24 hours later. AKI recovery was defined as a return to a sCr value <1.5 times the baseline value or <0.35 mg/dl above the baseline value with reversal of oliguria within 48 hours. ICU, intensive care unit; KDIGO, Kidney Disease Improving Global Outcomes; sCr, serum creatinine.
Data Collection
Blood and urine samples were collected at inclusion and 24 hours later (days 0 and 1, respectively). We analyzed plasma levels of urea, creatinine, and sodium, as well as urine concentrations of protein, sodium, potassium, creatinine, and urea. Fractional excretion of urea and sodium (FEUrea and FENa, respectively) was also calculated.
Patients who received RRT within 24 hours after inclusion were excluded from the FEUrea and FENa calculations. Certified intensivists (C.S. and A.D.) performed renal echography at the study inclusion and 24 hours later with a Vivid S6 ultrasound machine and a 4-MHz curved-array multifrequency transducer (GE Healthcare, Little Chalfont, Buckinghamshire, UK). Intrarenal Doppler signals were obtained from two to three representative proximal interlobar arteries. Peak systolic velocity and minimal diastolic velocity were determined by pulsed wave Doppler ultrasonography. The Doppler renal resistive index (RI) was calculated as follows (14): (peak systolic velocity − end diastolic velocity)/peak systolic velocity. Results from three consecutive measurements of both kidneys were averaged.
Blood samples for plasma NGAL were collected in EDTA anticoagulated tubes and were immediately analyzed using the Triage NGAL test (Alere, San Diego, CA) (15). For patients with a plasmal NGAL level exceeding the measurable range (>1300 ng/ml), a value of 1300 ng/ml was retained. Fresh urine samples taken during the last hour of collection were placed in dry tubes and were immediately analyzed for [TIMP-2]*[IGFBP7] using the NephroCheck point-of-care fluorescence immunoassay (Astute Medical, San Diego, CA). All measurements were made in our institution’s biochemistry department.
Because current eGFR equations evaluate kidney function when sCr is stable, we also evaluated kinetic eGFR calculated from sCr evolution between days 0 and 1 using a recently formulated equation (16). This was derived from the initial sCr, the volume of distribution, the creatinine production rate, and the quantitative difference between consecutive sCr over a given time. Kinetic eGFR was calculated as follows:
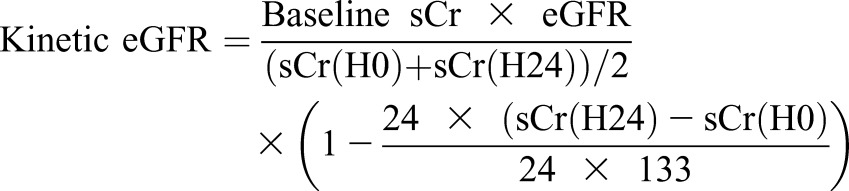 |
Going from the sCr at inclusion (H0) to the sCr 24 hours later (H24), we used the maximal increase in sCr that could occur if renal function was completely lost (1.7 mg/dl per day), as described by Chen (16). The other necessary variables for this formula included baseline sCr (the lowest sCr level measured during the patient’s hospital stay before inclusion in this study) and the corresponding GFR calculated by the Chronic Kidney Disease Epidemiology Collaboration study equation (17). Because the maximum increase in sCr per day must be greater than any observed change in plasma creatinine, the subtracted ratio can never exceed 1, and the lowest possible value is 0 (16). Data from patients undergoing RRT in the 24-hour period after inclusion were excluded from this calculation.
Statistical Analyses
Quantitative parameters are reported as medians with interquartile ranges (IQRs), and qualitative parameters are expressed as numbers and percentages. Categorical variables were compared using the chi-squared test or Fisher’s exact test, as appropriate. Continuous variables were compared using the Mann–Whitney U test. Matched sets of variables were compared with Wilcoxon’s signed-rank test. A two-factor ANOVA for repeated measurements was performed to assess the interaction between time (days 0 and 1) and group (patients with persistent or transient AKI). Receiver-operating characteristic curves (ROCs) were plotted to determine the prognostic values of the AKI markers, and area under the curve (AUC) values were compared using the nonparametric method of DeLong et al. (18). The optimal cutoff point was determined using the Youden index. The following values were used to describe AUC-ROCs: 0.90–1.0, excellent; 0.80–0.89, good; 0.70–0.79, fair; 0.60–0.69, poor; and 0.50–0.59, no (useful) performance (19). Clinical prediction models were constructed by logistic regression with backward elimination. The Hosmer–Lemeshow goodness-of-fit test was used to evaluate the model. Multivariable logistic regression analyses were conducted to assess the performance of predictive models when AKI markers and clinical models were combined. Finally, we calculated the integrated discrimination improvement and the category-free net reclassification improvement (NRI) (20). All tests were two sided, and P<0.05 was considered statistically significant. Statistical analyses were performed using SAS (version 9.3; SAS Institute, Cary, NC) and GraphPad Prism (version 6.00; GraphPad Software, La Jolla, CA) software.
Results
Study Population
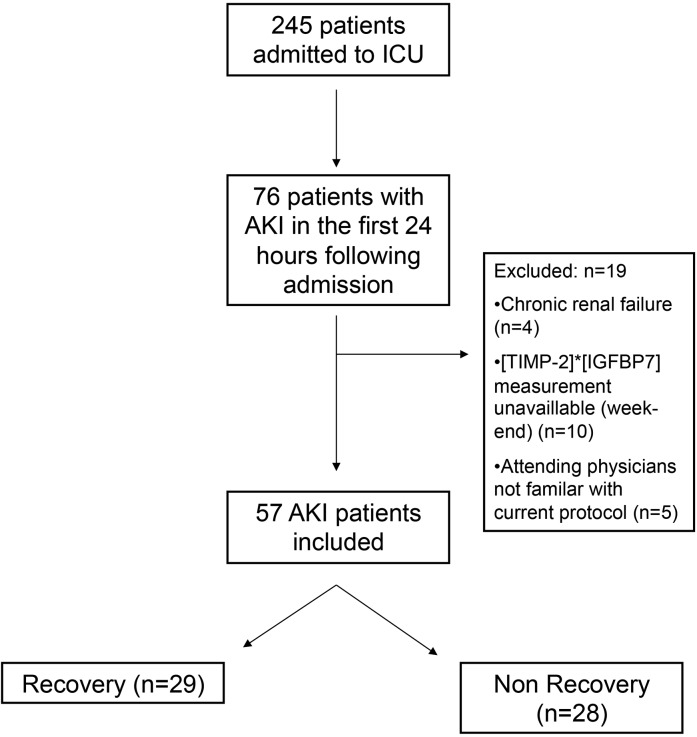
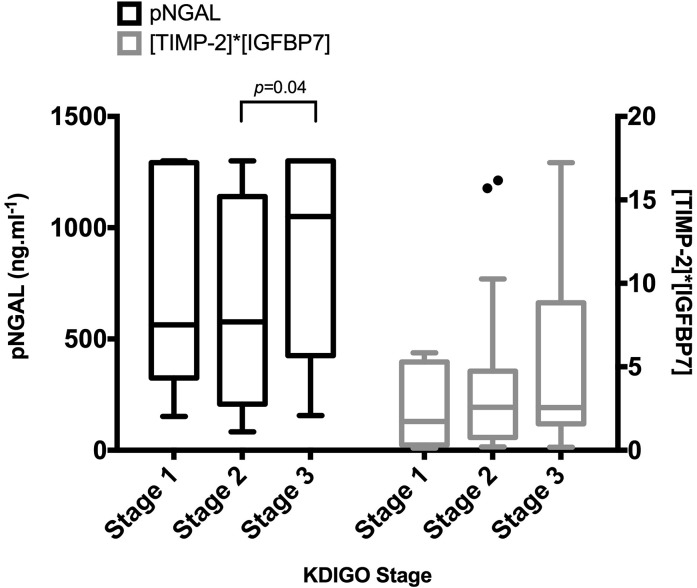
During the study period, 245 patients were admitted to our ICU. Of these patients, 76 (31%) presented with AKI in the first 24 hours after admission and 57 were included in this study (Figure 2). Table 1 summarizes the main patient characteristics. Risk factors for AKI were sepsis (42%), exposure to contrast agents (26%), aminoglycoside therapy (28%), and diabetes mellitus (18%). NE was the only vasoactive drug used in this study. According to our definition, 29 patients (51%) recovered from AKI, whereas 28 patients (49%) did not. RRT was initiated during the study period for three patients. Figure 3 presents plasma NGAL and [TIMP-2]*[IGFBP7] values according to AKI stage at inclusion.
Figure 2.
Flowchart of patients included in the study. During the study period, 245 patients were admitted to our ICU. Seventy-six (31%) patients were diagnosed with AKI in the first 24 hours after admission and 57 were included in this study. Twenty-nine patients (51%) recovered from AKI within 48 hours, whereas 28 patients (49%) did not. ICU, intensive care unit; [TIMP-2]*[IGFBP7], tissue inhibitor of metalloproteinase-2 and urine insulin-like growth factor–binding protein 7.
Table 1.
Characteristic of patients in the study (N=57)
| Characteristic | Recovery Group (n=29) | Nonrecovery Group (n=28) | P Value |
|---|---|---|---|
| Patient characteristics at inclusion | |||
| Age (yr) | 66 (60–74) | 70 (61–79) | 0.22 |
| Men | 15 (52) | 21 (75) | 0.10 |
| Weight (kg) | 72 (62–83) | 75 (66–95) | 0.42 |
| Body mass index (kg/m2) | 26 (23–30) | 26 (23–32) | 0.74 |
| SOFA score | 5 (3–6) | 8 (4–12) | 0.01 |
| SOFA without renal component | 4 (3–6) | 7 (2–11) | 0.08 |
| SAPS-II score | 40 (26–47) | 59 (35–72) | 0.003 |
| Mechanical ventilation | 7 (24) | 12 (43) | 0.17 |
| Mean arterial pressure (mmHg) | 76 (68–90) | 75 (67–85) | 0.68 |
| NE infusion | 6 (21) | 12 (43) | 0.09 |
| Dose of NE (μg/kg per minute) | 0.43 (0.13–0.67) | 0.37 (0.16–0.79) | >0.99 |
| Lactate (mg/dl) | 13.5 (9–16.2) | 18 (13.5–31.5) | 0.02 |
| PaO2/FiO2 ratio | 247 (205–303) | 239 (145–319) | 0.61 |
| Reasons for ICU admission | 0.29 | ||
| Severe sepsis/septic shock | 5 (17)/6(21) | 2 (7)/10 (36) | |
| Major surgery | 11 (38) | 8 (29) | |
| Acute respiratory failure | 5 (17) | 3 (11) | |
| Acute hemorrhage | 1 (3) | 2 (7) | |
| Acute pancreatitis | 1 (3) | 1 (4) | |
| Acute liver failure | 0 (0) | 2 (7) | |
| Infection source | 0.81 | ||
| Intra-abdominal | 6 (46) | 7 (64) | |
| Pulmonary | 3 (23) | 2 (18) | |
| Mediastinal | 2 (15) | 1 (9) | |
| Biliary | 2 (15) | 1 (9) | |
| Prior kidney function | |||
| Baseline creatinine (mg/dl) | 0.8 (0.6–0.9) | 0.9 (0.7–1.1) | 0.02 |
| eGFR (ml/min per 1.73 m2)a | 95 (79–99) | 78 (59–98) | 0.05 |
| Renal function at inclusion | |||
| Diuresis (ml/h) | 0.46 (0.33–0.61) | 0.24 (0.12–0.37) | <0.001 |
| Serum urea (mg/dl) | 24.6 (15.7–31.9) | 32.2 (28.3–52.9) | 0.004 |
| Serum creatinine (mg/dl) | 1.2 (0.7–1.5) | 1.9 (1.3–2.9) | <0.001 |
| KDIGO stage at inclusion | <0.001 | ||
| 1 | 7 (24) | 1 (4) | |
| 2 | 20 (69) | 10 (36) | |
| 3 | 2 (7) | 17 (61) | |
| Fluid balance (ml)b | 1910 (1300–2700) | 2670 (1860–3270) | 0.04 |
| Evolution | |||
| Maximum KDIGO stage reached | <0.001 | ||
| 1 | 6 (21) | 1 (4) | |
| 2 | 21 (72) | 5 (18) | |
| 3 | 2 (7) | 22 (79) | |
| RRT | 0 (0) | 9 (32) | <0.001 |
| ICU, length of stay (d) | 6 (4–8) | 8 (6–20) | 0.01 |
| Hospital, length of stay (d) | 15 (13–25) | 27 (13–52) | 0.17 |
| ICU mortality | 2 (7) | 6 (21) | 0.14 |
| Hospital mortality | 2 (7) | 12 (43) | 0.004 |
| Major adverse kidney eventsc | 2 (7) | 14 (50) | <0.001 |
Data are expressed as medians (interquartile ranges) or n (%). SOFA, Sequential Organ Failure Assessment; SAPS, Simplified Acute Physiology Score; ICU, intensive care unit; KDIGO, Kidney Disease Improving Global Outcomes.
Calculated using the Chronic Kidney Disease Epidemiology Collaboration formula.
Calculated the day of admission.
Major adverse kidney events at hospital discharge truncated at 30 days.
Figure 3.
Plasma NGAL and [TIMP-2]*[IGFBP7] values according to AKI stage at inclusion. Only patients with stage 3 AKI diagnosed in the first 24 hours after ICU admission had significantly higher plasma NGAL values in comparison with patients with stage 2 AKI. Plasma NGAL frequently reached the maximal measurement range provided (1300 ng/ml). ICU, intensive care unit; KDIGO, Kidney Disease Improving Global Outcomes; NGAL, neutrophil gelatinase–associated lipocalin; pNGAL, plasma neutrophil gelatinase–associated lipocalin; [TIMP-2]*[IGFBP7], tissue inhibitor of metalloproteinase-2 and urine insulin-like growth factor–binding protein 7.
AKI Markers at Inclusion and 24 Hours Later
FENa, RI, plasma NGAL, and [TIMP-2]*[IGFBP7] markers measured at inclusion were significantly increased in the nonrecovery group (Table 2). RI, plasma NGAL, and [TIMP-2]*[IGFBP7] values still differed significantly across groups on day 1. Seventeen patients (30%) had a plasma NGAL level that exceeded the measurable range provided by the Alere Triage test at inclusion (value >1300 ng/ml), including 13 patients (46%) in the nonrecovery group. Plasma NGAL remained above the detection range for 13 patients (23%) on day 1 (all in the nonrecovery group). Poor-quality images without detectable arterial flow made obtaining Doppler measurements for any lobar arteries impossible for four patients. Intraobserver and interobserver variations were 4.2% and 7.2%, respectively.
Table 2.
Values of AKI markers at inclusion and 24 hours later
| Marker | Recovery Group (n=29) | Nonrecovery Group (n=28) | P Valuea |
|---|---|---|---|
| At inclusion | |||
| FENa (%) | 0.08 (0.06–0.16) | 0.19 (0.09–0.51) | 0.03 |
| FEUrea (%) | 16 (10–26) | 13 (7–27) | 0.16 |
| Proteinuria (g/dl) | 0.08 (0.04–0.11) | 0.09 (0.05–0.17) | 0.14 |
| RI | 0.66 (0.60–0.72) | 0.75 (0.67–0.78) | 0.02 |
| Plasma NGAL (ng/ml) | 536 (210–919) | 1175 (463–1300) | 0.01 |
| [TIMP-2]*[IGFBP7] ([ng/ml]2/1000) | 1.8 (0.6–3.5) | 3.8 (1.6–9.9) | 0.01 |
| 24h after inclusion | |||
| FENa (%) | 0.37 (0.18–0.75) | 0.34 (0.17–1.18) | 0.61 |
| FEUrea (%) | 29 (23–38)b | 28 (20–37)b | 0.41 |
| Proteinuria (g/dl) | 0.05 (0.04–0.08) | 0.08 (0.04–0.16) | 0.16 |
| RI | 0.68 (0.63–0.75) | 0.75 (0.66–0.79) | 0.02 |
| Plasma NGAL (ng/ml) | 378 (203–661)b | 1300 (512–1300) | <0.001 |
| [TIMP-2]*[IGFBP7] ([ng/ml]2/1000) | 0.62 (0.30–0.80)b | 2.2 (0.5–4.2)b | 0.002 |
| Kinetic eGFR (ml/min per 1.73 m2) | 62 (49–87) | 30 (14–40) | <0.001 |
Data are expressed as medians (interquartile ranges). FENa, fractional excretion of sodium; FEUrea, fractional excretion of urea; RI, renal resistive index; NGAL, neutrophil gelatinase–associated lipocalin; [TIMP-2]*[IGFBP7], tissue inhibitor of metalloproteinase-2 and urine insulin-like growth factor–binding protein 7.
P<0.05 for comparison between renal recovery and nonrecovery groups (Mann–Whitney U test).
P<0.05 for comparison between AKI markers at inclusion and 24 hours later (Wilcoxon signed-rank test).
AKI Marker Evolution between Days 0 and 1 and Calculation of Kinetic eGFR
Patients who recovered from AKI had decreased sCr values between days 0 and 1 (1.2 [IQR, 0.7–1.5] versus 1 [IQR, 0.75–1.44], P=0.01), whereas patients who did not recover had stable sCr values (1.9 [IQR, 1.3–2.9] versus 2.3 [IQR, 1.6–3.9], P=0.60). Table 2 shows AKI marker evolution during the first 24 hours. Decreasing [TIMP-2]*[IGFBP7] values were observed in the recovery and nonrecovery groups (P=0.002 and P=0.03, respectively). An increase in FEUrea was also observed in both groups of patients (P=0.004 and P=0.001, respectively). Plasma NGAL significantly decreased in the recovery group (P=0.01). Interaction analysis revealed that changes in plasma NGAL between inclusion and day 1 significantly differed between the groups (P=0.01), but sCr (P=0.08), RI (P=0.90), and [TIMP-2]*[IGFBP7] (P=0.40) did not.
Performance of AKI Markers in Predicting AKI Recovery and Major Adverse Kidney Events
Table 3 summarizes the predictive performance of the AKI markers. RI, plasma NGAL, and [TIMP-2]*[IGFBP7] predicted AKI recovery, with AUC-ROC values between 0.70 and 0.79. The cutoff value for plasma NGAL was very close to the maximal measurable value provided by the Alere Triage test. Values on day 1 were slightly better, but the AUC-ROC value remained below 0.8. Calculation of the creatinine ratio between days 0 and 1 did not show better predictive performance. The best performance was given by the kinetic eGFR calculation, with an AUC-ROC of 0.87. A pairwise comparison of AUC-ROC values generated for RI, plasma NGAL, [TIMP-2]*[IGFBP7], creatinine ratio, and kinetic eGFR showed no statistical differences, except for the AUC-ROC values generated for RI on day 1 and for kinetic eGFR (P=0.02).
Table 3.
Performance of AKI markers
| Marker | Renal Recovery | Major Adverse Kidney Events | ||||||
|---|---|---|---|---|---|---|---|---|
| AUC-ROC | Cutoff Value | Sensitivity | Specificity | AUC-ROC | Cutoff Value | Sensitivity | Specificity | |
| At inclusion | ||||||||
| FENa (%) | 0.65 (0.50 to 0.78) | 0.08 | 0.62 (0.42 to 0.79) | 0.82 (0.63–0.94) | 0.64 (0.50 to 0.76) | 0.09 | 0.81 (0.54 to 0.96) | 0.51 (0.35 to 0.67) |
| FEUrea (%) | 0.61 (0.47 to 0.74) | 8 | 0.96 (0.82 to 0.99) | 0.32 (0.16 to 0.52) | 0.66 (0.51 to 0.79) | 9 | 0.44 (0.20 to 0.70) | 0.85 (0.71 to 0.94) |
| Proteinuria (g/dl) | 0.62 (0.47 to 0.74) | 0.08 | 0.55 (0.36 to 0.74) | 0.69 (0.48 to 0.86) | 0.71 (0.57 to 0.82) | 0.08 | 0.81 (0.54 to 0.96) | 0.54 (0.37 to 0.70) |
| RI | 0.69 (0.56 to 0.81) | 0.70 | 0.64 (0.44 to 0.81) | 0.71 (0.49 to 0.87) | 0.79 (0.65 to 0.89) | 0.71 | 0.87 (0.59 to 0.98) | 0.68 (0.50 to 0.82) |
| Plasma NGAL (ng/ml) | 0.70 (0.57 to 0.82) | 1290 | 0.90 (0.73 to 0.98) | 0.50 (0.31 to 0.69) | 0.68 (0.55 to 0.80) | 1032 | 0.69 (0.41 to 0.89) | 0.76 (0.60 to 0.88) |
| (TIMP-2)*(IGFBP7) ([ng/ml]2/1000) | 0.71 (0.57 to 0.82) | 5.4 | 0.93 (0.77 to 0.99) | 0.43 (0.24 to 0.63) | 0.79 (0.66 to 0.88) | 2.6 | 0.81 (0.54 to 0.96) | 0.71 (0.54 to 0.84) |
| 24 h after inclusion | ||||||||
| FENa (%) | 0.54 (0.39 to 0.69) | 0.76 | 0.81 (0.61 to 0.94) | 0.41 (0.21 to 0.64) | 0.63 (0.48 to 0.76) | 0.74 | 0.58 (0.28 to 0.85) | 0.78 (0.61 to 0.90) |
| FEUrea (%) | 0.57 (0.42 to 0.71) | 21 | 0.92 (0.75 to 0.99) | 0.27 (0.11 to 0.50) | 0.64 (0.47 to 0.78) | 30 | 0.83 (0.52 to 0.98) | 0.53 (0.36 to 0.70) |
| Proteinuria (g/dl) | 0.57 (0.41 to 0.73) | 0.11 | 0.92 (0.75 to 0.99) | 0.39 (0.20 to 0.61) | 0.54 (0.39 to 0.68) | 0.16 | 0.29 (0.08 to 0.58) | 0.97 (0.85 to 0.99) |
| Creatinine ratioa | 0.70 (0.56 to 0.84) | 0.97 | 0.6 (0.39 to 0.79) | 0.76 (0.56 to 0.90) | 0.61 (0.42 to 0.80) | 1.02 | 0.73 (0.57 to 0.86) | 0.62 (0.32 to 0.86) |
| RI | 0.70 (0.55 to 0.82) | 0.77 | 1 (0.87 to 1) | 0.39 (0.2 to 0.61) | 0.75 (0.61 to 0.86) | 0.69 | 0.81 (0.54 to 0.96) | 0.64 (0.45 to 0.80) |
| Plasma NGAL (ng/ml) | 0.78 (0.64 to 0.88) | 1190 | 1 (0.86 to 1) | 0.54 (0.33 to 0.74) | 0.76 (0.61 to 0.87) | 902 | 0.71 (0.42 to 0.92) | 0.80 (0.63 to 0.92) |
| (TIMP-2)*(IGFBP7) ([ng/ml]2/1000) | 0.76 (0.62 to 0.87) | 1.4 | 1 (0.86 to 1) | 0.54 (0.33 to 0.74) | 0.81 (0.67 to 0.91) | 2.3 | 0.57 (0.29 to 0.82) | 0.97 (0.85 to 1) |
| Kinetic eGFR (ml/min per 1.73 m2) | 0.87 (0.73 to 0.94) | 41 | 0.86 (0.68 to 0.96) | 0.80 (0.59 to 0.93) | 0.81 (0.67 to 0.96) | 39 | 0.77 (0.46 to 0.95) | 0.73 (0.57 to 0.86) |
Data are presented with 95% confidence intervals in parentheses. Major adverse kidney events were defined as death, use of RRT, or persistence of renal dysfunction (defined by serum creatinine ≥200% of the reference) at hospital discharge truncated at 30 days. FENa, fractional excretion of sodium; FEU, fractional excretion of urea; RI, renal resistive index; NGAL, neutrophil gelatinase–associated lipocalin; [TIMP-2]*[IGFBP7], tissue inhibitor of metalloproteinase-2 and urine insulin-like growth factor–binding protein 7; AUC-ROC, area under the receiver-operating characteristic curve.
Ratio of value at inclusion and 24 hours later.
RI and [TIMP-2]*[IGFBP7] on days 0 and 1 showed a good ability to predict major adverse kidney events, with AUC-ROC values close to 0.8 (Figure 4). The kinetic eGFR calculation showed equal performance. Pairwise comparisons of AUC-ROC values generated for RI, plasma NGAL, and [TIMP-2]*[IGFBP7] on days 0 and 1 and for kinetic eGFR showed no statistical differences.
Figure 4.
ROCs showing the ability of the Doppler RI, plasma NGAL, [TIMP-2]*[IGFBP7], and kinetic eGFR to predict renal recovery and major adverse kidney events. (A and B) Renal recovery at inclusion (A) and 24 hours later (B). (C and D) Major adverse kidney events at inclusion (C) and 24 hours later (D). RI, plasma NGAL, and [TIMP-2]*[IGFBP7] showed a fair performance in predicting short-term renal recovery. The best performance was given by the kinetic eGFR calculation on day 1. [TIMP-2]*[IGFBP7] on day 0 and kinetic eGFR and [TIMP-2]*[IGFBP7] on day 1 were the best predictors for major adverse kidney events. AUC, area under the curve; ICU, intensive care unit; KDIGO, Kidney Disease Improving Global Outcomes; KeGFR, kinetic eGFR; pNGAL, plasma neutrophil gelatinase–associated lipocalin; RI, renal resistive index; ROC, receiver-operating characteristic curve; [TIMP-2]*[IGFBP7], tissue inhibitor of metalloproteinase-2 and urine insulin-like growth factor–binding protein 7.
Combination of Clinical Prediction Models and AKI Markers
Clinical prediction models for AKI recovery and major adverse kidney events were constructed by including all variables shown in Table 1 (including Sequential Organ-Failure Assessment scores without the renal component, as well as sCr and diuresis to assess renal function at inclusion). Table 4 shows the retained significant variables that performed well in predicting recovery and major adverse kidney events. The performance of various combinations of AKI markers on day 0 in addition to clinical models was then determined (Table 5). No statistical differences between AUC-ROCs were found. A combination of our clinical model for recovery with RI, plasma NGAL, [TIMP-2]*[IGFBP7], or kinetic eGFR significantly improved the category-free NRI. A combination of our clinical model for major adverse kidney events with [TIMP-2]*[IGFBP7] or kinetic eGFR also significantly improved the category-free NRI. The best performance was obtained with the combination of our clinical model, plasma NGAL, [TIMP-2]*[IGFBP7], and RI for renal recovery as well as the combination of our clinical model, plasma NGAL, [TIMP-2]*[IGFBP7], RI, and kinetic eGFR for major adverse kidney events.
Table 4.
Significant variables at inclusion after logistic regression analysis used to construct a clinical prediction model for renal recovery and major adverse kidney events
| Clinical Variable | Renal Recovery | Major Adverse Kidney Events |
|---|---|---|
| SOFA without renal component | 0.77 (0.63 to 0.95) | 1.44 (1.15 to 1.80) |
| Serum creatinine at inclusion | 0.98 (0.97 to 0.99) | 1.01 (1.00 to 1.03) |
| Fluid balancea | 0.99 (0.99 to 1) | |
| Prior eGFR (ml/min per 1.73 m2) | 1.06 (1.00 to 1.12) | |
| Age | 1.15 (1.04 to 1.28) |
Data are presented as odds ratios (95% confidence intervals). Major adverse kidney events were defined as death, use of RRT, or persistence of renal dysfunction (defined by serum creatinine ≥200% of the reference) at hospital discharge truncated at 30 days. SOFA, Sequential Organ Failure Assessment.
Calculated the day of admission.
Table 5.
Combination of clinical model and AKI markers at inclusion for predicting renal recovery and major adverse kidney events
| Combination | AUC-ROC | P Value | Integrated Discrimination Improvement | P Value | Category-Free Net Reclassification Improvement | P Value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Events | Nonevents | Overall | Events | Nonevents | Overall | |||||
| Renal recovery | ||||||||||
| Clinical model | 0.87 (0.78 to 0.96) | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Clinical model + RI | 0.90 (0.82 to 0.99) | 0.39 | 0.06 (0.02 to 0.11) | 0.003 (−0.04 to 0.04) | 0.07 (0.004 to 0.13) | 0.04 | 0.57 (0.27 to 0.88) | 0.50 (0.15 to 0.84) | 1.07 (0.61 to 1.53) | <0.001 |
| Clinical model + plasma NGAL | 0.88 (0.79 to 0.96) | 0.75 | 0.01 (−0.02 to 0.04) | 0.01 (−0.02 to 0.04) | 0.02 (−0.02 to 0.07) | 0.29 | 0.43 (0.09 to 0.76) | 0.36 (0.09 to 0.76) | 0.79 (0.30 to 1.27) | 0.003 |
| Clinical model + [TIMP-2]*[IGFBP7] | 0.89 (0.81 to 0.97) | 0.36 | 0.02 (−0.01 to 0.06) | 0.02 (−0.02 to 0.06) | 0.04 (−0.02 to 0.10) | 0.15 | 0.50 (−0.03 to 0.07) | 0.07 (−0.30 to 0.44) | 0.57 (0.08 to 1.06) | 0.03 |
| Clinical model + kinetic eGFR (ml/min per 1.73 m2) | 0.87 (0.78 to 0.96) | 0.57 | 0.02 (−0.01 to 0.04) | 0.01 (−0.04 to 0.06) | 0.03 (−0.03 to 0.08) | 0.32 | 0.43 (0.09 to 0.76) | 0.12 (−0.27 to 0.51) | 0.55 (0.04 to 1.06) | 0.05 |
| Clinical model + plasma NGAL + [TIMP-2]*[IGFBP7] | 0.89 (0.81 to 0.97) | 0.41 | 0.03 (−0.02 to 0.08) | 0.03 (−0.01 to 0.07) | 0.06 (−0.008 to 0.13) | 0.09 | 0.50 (−0.01 to 0.07) | 0.36 (0.01 to 0.70) | 0.86 (0.39 to 1.33) | 0.001 |
| Clinical model + RI + plasma NGAL + [TIMP-2]*[IGFBP7] | 0.92 (0.84 to 0.99) | 0.18 | 0.07 (0.01 to 0.12) | 0.008 (−0.04 to 0.06) | 0.07 (0.004 to 0.15) | 0.04 | 0.43 (0.09 to 0.76) | 0.33 (−0.04 to 0.71) | 0.76 (0.26 to 1.27) | 0.01 |
| Clinical model + RI + plasma NGAL + [TIMP-2]*[IGFBP7] + kinetic eGFR | 0.89 (0.80 to 0.98) | 0.48 | 0.07 (0.01 to 0.13) | 0.008 (−0.05 to 0.07) | 0.08 (−0.003 to 0.16) | 0.06 | 0.50 (0.18 to 0.82) | 0.24 (−0.18 to 0.65) | 0.74 (0.21 to 1.26) | 0.01 |
| Major adverse kidney events | ||||||||||
| Clinical model | 0.89 (0.79 to 0.99) | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Clinical model + RI | 0.91 (0.83 to 0.98) | 0.36 | 0.04 (−0.03 to 0.11) | 0.005 (−0.03 to 0.04) | 0.04 (−0.04 to 0.12) | 0.29 | 0.20 (−0.30 to 0.70) | 0.30 (−0.01 to 0.60) | 0.50 (−0.09 to 1.08) | 0.10 |
| Clinical model + plasma NGAL | 0.88 (0.78 to 0.98) | 0.76 | 0.005 (−0.03 to 0.04) | 0.002 (−0.01 to 0.01) | 0.007 (−0.03 to 0.04) | 0.67 | 0.12 (−0.36 to 0.61) | 0.07 (−0.36 to 0.61) | 0.20 (−0.38 to 0.77) | 0.50 |
| Clinical model + [TIMP-2]*[IGFBP7] | 0.89 (0.80 to 0.98) | 0.65 | 0.01 (−0.03 to 0.05) | 0.004 (−0.01 to 0.02) | 0.02 (−0.03 to 0.06) | 0.49 | 0.25 (−0.22 to 0.72) | 0.32 (−0.22 to 0.72) | 0.57 (0.01 to 1.12) | 0.05 |
| Clinical model + kinetic eGFR | 0.87 (0.76 to 0.99) | 0.71 | 0.02 (−0.05 to 0.08) | 0.02 (−0.01 to 0.04) | 0.03 (−0.04 to 0.10) | 0.36 | 0.23 (−0.30 to 0.76) | 0.41 (0.14 to 0.69) | 0.65 (0.05 to 1.24) | 0.04 |
| Clinical model + plasma NGAL + [TIMP-2]*[IGFBP7] | 0.89 (0.80 to 0.98) | 0.67 | 0.01 (−0.03 to 0.06) | 0.005 (−0.01 to 0.02) | 0.02 (−0.03 to 0.07) | 0.47 | 0.25 (−0.22 to 0.72) | 0.07 (−0.23 to 0.3 8) | 0.32 (−0.24 to 0.89) | 0.27 |
| Clinical model + RI + plasma NGAL + [TIMP-2]*[IGFBP7] | 0.91 (0.83 to 0.98) | 0.41 | 0.05 (−0.03 to 0.12) | 0.009 (−0.03 to 0.05) | 0.06 (−0.03 to 0.14) | 0.18 | 0.20 (−0.30 to 0.70) | 0.35 (0.05 to 0.65) | 0.55 (−0.03 to 1.13) | 0.07 |
| Clinical model + RI + plasma NGAL + [TIMP-2]*[IGFBP7] + kinetic eGFR (ml/min per 1.73 m2) | 0.93 (0.86 to 1) | 0.13 | 0.15 (−0.03 to 0.33) | 0.05 (0.01 to 0.09) | 0.20 (0.02 to 0.38) | 0.03 | 0.33 (−0.20 to 0.87) | 0.51 (0.24 to 0.79) | 0.85 (0.25 to 1.45) | 0.01 |
Data are presented with 95% confidence intervals in parentheses. P values are compared with the clinical model. Major adverse kidney events were defined as death, use of RRT, or persistence of renal dysfunction (defined by serum creatinine ≥200% of the reference) at hospital discharge truncated at 30 days. RI, renal resistive index; NGAL, neutrophil gelatinase–associated lipocalin; [TIMP-2]*[IGFBP7], tissue inhibitor of metalloproteinase-2 and urine insulin-like growth factor–binding protein 7; AUC-ROC, area under the receiver-operating characteristic curve; NA, not available.
Discussion
The main findings of our study are as follows. First, biomarkers of kidney damage showed fair performance in predicting short-term renal recovery and major adverse kidney events. Second, after initial resuscitation, changes in sCr, RI, and [TIMP-2]*[IGFBP7] did not improve predictive performance, whereas the kinetic eGFR calculation according to sCr evolution was a good marker of renal recovery. [TIMP-2]*[IGFBP7] and kinetic eGFR were the best predictors for major adverse kidney events. Third, although plasma NGAL values provided by a commercialized point-of-care immunoassay frequently reached the maximal measurement range, their decrease at day 1 also predicted recovery. Finally, combinations of AKI markers in addition to clinical models improved prediction of renal recovery and major adverse kidney events, as measured by the NRI and integrated discrimination improvement indices.
During the last decade, many studies have explored utilizing biomarkers for kidney structural damage to diagnose AKI. However, only a few studies have tested the ability of biomarkers to predict AKI recovery. The limited interest in urinary biochemistry in critically ill patients was confirmed in our study (21–24). Doppler ultrasonography may be a useful tool, and its ability to predict major adverse kidney events was interesting. However, RI measurements are subjective and are influenced by many extrarenal factors, resulting in interobserver variations close to the differences observed between patients (25,26). NGAL, acting as a siderophore/iron-binding protein and a growth factor, has been extensively studied in AKI and was described as an early biomarker for AKI in large unselected cohorts of ICU patients (27,28). Urinary NGAL has been described as a strong indicator of the severity and duration of AKI in emergency departments, with an AUC-ROC of 0.94; urinary NGAL has also been used to distinguish between patients with intrinsic and prerenal AKI (29,30). In the ICU, plasma and urinary NGAL have been shown to predict severe AKI and the need for RRT, with an AUC-ROC close to 0.9 (7). Modest increases in urinary NGAL have also been detected in patients with prerenal AKI, suggesting that mild renal tubular injury could be recognized (31). Decreasing urinary NGAL was associated with greater odds for renal recovery (32). However, sCr and GFR achieved similar performance levels, and both plasma and urinary NGAL had only a minor role in predicting hospital mortality (31). In a recent study, urinary NGAL failed to classify the prerenal versus intrinsic renal state based on fluid responsiveness in 25% of cases (33). A systematic review also demonstrated similar mortality rates and lengths of stay for patients with NGAL-positive/creatinine-negative AKI versus NGAL-negative/creatinine-positive AKI (34). Urinary NGAL was also not associated with a composite outcome of death or RRT, and it exhibited poor discrimination for AKI development in a recent study (35). Despite our finding that plasma NGAL measurements clearly exceeded the Triage range in this study, their decrease after initial resuscitation was significant in patients recovering from AKI.
[TIMP-2]*[IGFBP7], a combination of two urinary markers of cycle cell arrest, seems to improve the identification of patients at risk for imminent AKI compared with previous biomarkers (8,9). The risk of major adverse kidney events elevated sharply with [TIMP-2]*[IGFBP7] values >0.3, and they almost doubled for values >2.0 in a validation study (8). The relationship between a decline in [TIMP-2]*[IGFBP7] between 4 and 24 hours after cardiac surgery in renal recovery had an AUC-ROC of 0.79 (95% confidence interval, 0.65 to 0.92); by contrast, the AUC-ROC curve for NGAL was 0.48 (95% confidence interval, 0.31 to 0.64) (10). In a recent study in surgical patients at high risk for AKI, the addition of [TIMP-2]*[IGFBP7] to clinical models improved the prediction of early use of RRT and 28-day mortality (36). Our study confirmed the prognostic value of this biomarker and showed an elevated value at inclusion with a cutoff <5 for predicting AKI recovery.
One of the main aims of our study was to compare multiple AKI markers and test the recently redefined kinetic eGFR formula in an unselected cohort of critically ill patients. However, several points must be considered when assessing the clinical relevance of our study. First, although our study represents the clinical context in which biomarkers could be used in an ICU, our patient cohort was small. Second, our definition of renal recovery does not address the origin of the pathophysiologic state of the kidney at the time of diagnosis. Several studies have identified that transient AKI is also associated with adverse outcomes (11,37). Finally, because the theoretical daily changes in sCr depend on various factors and because sCr is part of the definition of AKI, the kinetic eGFR calculation may have several limitations in ICUs. However, the kinetic eGFR is a good reflection of sCr kinetics, as confirmed by the lower predictive value of a simple sCr ratio.
Being able to appreciate the severity of kidney damage and the capacity for recovery is clinically relevant, because it can improve the ability to make specific management decisions. As a clinical syndrome, AKI has many causes, results in multiple insults, and relies on a diagnosis of impaired filtration function in the ICU. There is no evidence that acute tubular necrosis is the culprit for nonrecovery after AKI (38,39) and tubular regeneration mechanisms remain poorly understood. In the future, biomarkers may allow appreciation of the site, mechanism, and phase of injury. This study confirms that combinations of functional and damage markers in addition to clinical information could improve our understanding of AKI.
Biomarkers for kidney damage fairly predicted recovery and major adverse kidney events in unselected ICU patients who presented with AKI in the first 24 hours after admission. Estimation of a kinetic eGFR according to sCr evolution imposed a delay after initial resuscitation but provided a good diagnostic and prognostic approach. Combinations of functional and damage markers in addition to clinical prediction models improved the discrimination and reclassification of patients who will recover from AKI or suffer from major adverse kidney events. Larger prospective studies are needed to validate the predictive value of these biomarker combinations.
Disclosures
None.
Acknowledgments
This study was supported solely by the Department of Anesthesiology and Intensive Care. No funds were received to support this study.
The authors thank Astute Medical for providing the NephroCheck tests and Newmed Publishing Services and Erwan Floch for revising the English text.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Lameire NH, Bagga A, Cruz D, De Maeseneer J, Endre Z, Kellum JA, Liu KD, Mehta RL, Pannu N, Van Biesen W, Vanholder R: Acute kidney injury: An increasing global concern. Lancet 382: 170–179, 2013 [DOI] [PubMed] [Google Scholar]
- 2.Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, Kellum JA: RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: A cohort analysis. Crit Care 10: R73, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hobson CE, Yavas S, Segal MS, Schold JD, Tribble CG, Layon AJ, Bihorac A: Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation 119: 2444–2453, 2009 [DOI] [PubMed] [Google Scholar]
- 4.Bagshaw SM: Short- and long-term survival after acute kidney injury. Nephrol Dial Transplant 23: 2126–2128, 2008 [DOI] [PubMed] [Google Scholar]
- 5.Kellum JA, Lameire N, KDIGO AKI Guideline Work Group : Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (Part 1). Crit Care 17: 204, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coca SG, Yalavarthy R, Concato J, Parikh CR: Biomarkers for the diagnosis and risk stratification of acute kidney injury: A systematic review. Kidney Int 73: 1008–1016, 2008 [DOI] [PubMed] [Google Scholar]
- 7.de Geus HR, Bakker J, Lesaffre EM, le Noble JL: Neutrophil gelatinase-associated lipocalin at ICU admission predicts for acute kidney injury in adult patients. Am J Respir Crit Care Med 183: 907–914, 2011 [DOI] [PubMed] [Google Scholar]
- 8.Kashani K, Al-Khafaji A, Ardiles T, Artigas A, Bagshaw SM, Bell M, Bihorac A, Birkhahn R, Cely CM, Chawla LS, Davison DL, Feldkamp T, Forni LG, Gong MN, Gunnerson KJ, Haase M, Hackett J, Honore PM, Hoste EA, Joannes-Boyau O, Joannidis M, Kim P, Koyner JL, Laskowitz DT, Lissauer ME, Marx G, McCullough PA, Mullaney S, Ostermann M, Rimmelé T, Shapiro NI, Shaw AD, Shi J, Sprague AM, Vincent JL, Vinsonneau C, Wagner L, Walker MG, Wilkerson RG, Zacharowski K, Kellum JA: Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care 17: R25, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bihorac A, Chawla LS, Shaw AD, Al-Khafaji A, Davison DL, Demuth GE, Fitzgerald R, Gong MN, Graham DD, Gunnerson K, Heung M, Jortani S, Kleerup E, Koyner JL, Krell K, Letourneau J, Lissauer M, Miner J, Nguyen HB, Ortega LM, Self WH, Sellman R, Shi J, Straseski J, Szalados JE, Wilber ST, Walker MG, Wilson J, Wunderink R, Zimmerman J, Kellum JA: Validation of cell-cycle arrest biomarkers for acute kidney injury using clinical adjudication. Am J Respir Crit Care Med 189: 932–939, 2014 [DOI] [PubMed] [Google Scholar]
- 10.Meersch M, Schmidt C, Van Aken H, Martens S, Rossaint J, Singbartl K, Görlich D, Kellum JA, Zarbock A: Urinary TIMP-2 and IGFBP7 as early biomarkers of acute kidney injury and renal recovery following cardiac surgery. PLoS One 9: e93460, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nejat M, Pickering JW, Devarajan P, Bonventre JV, Edelstein CL, Walker RJ, Endre ZH: Some biomarkers of acute kidney injury are increased in pre-renal acute injury. Kidney Int 81: 1254–1262, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uchino S, Bellomo R, Bagshaw SM, Goldsmith D: Transient azotaemia is associated with a high risk of death in hospitalized patients. Nephrol Dial Transplant 25: 1833–1839, 2010 [DOI] [PubMed] [Google Scholar]
- 13.Palevsky PM, Molitoris BA, Okusa MD, Levin A, Waikar SS, Wald R, Chertow GM, Murray PT, Parikh CR, Shaw AD, Go AS, Faubel SG, Kellum JA, Chinchilli VM, Liu KD, Cheung AK, Weisbord SD, Chawla LS, Kaufman JS, Devarajan P, Toto RM, Hsu CY, Greene T, Mehta RL, Stokes JB, Thompson AM, Thompson BT, Westenfelder CS, Tumlin JA, Warnock DG, Shah SV, Xie Y, Duggan EG, Kimmel PL, Star RA: Design of clinical trials in acute kidney injury: Report from an NIDDK workshop on trial methodology. Clin J Am Soc Nephrol 7: 844–850, 2012 [DOI] [PubMed] [Google Scholar]
- 14.Lerolle N, Guérot E, Faisy C, Bornstain C, Diehl JL, Fagon JY: Renal failure in septic shock: Predictive value of Doppler-based renal arterial resistive index. Intensive Care Med 32: 1553–1559, 2006 [DOI] [PubMed] [Google Scholar]
- 15.Dent CL, Ma Q, Dastrala S, Bennett M, Mitsnefes MM, Barasch J, Devarajan P: Plasma neutrophil gelatinase-associated lipocalin predicts acute kidney injury, morbidity and mortality after pediatric cardiac surgery: A prospective uncontrolled cohort study. Crit Care 11: R127, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen S: Retooling the creatinine clearance equation to estimate kinetic GFR when the plasma creatinine is changing acutely. J Am Soc Nephrol 24: 877–888, 2013 [DOI] [PubMed] [Google Scholar]
- 17.Matsushita K, Selvin E, Bash LD, Astor BC, Coresh J: Risk implications of the new CKD Epidemiology Collaboration (CKD-EPI) equation compared with the MDRD Study equation for estimated GFR: The Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis 55: 648–659, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeLong ER, DeLong DM, Clarke-Pearson DL: Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 44: 837–845, 1988 [PubMed] [Google Scholar]
- 19.Haase-Fielitz A, Bellomo R, Devarajan P, Story D, Matalanis G, Dragun D, Haase M: Novel and conventional serum biomarkers predicting acute kidney injury in adult cardiac surgery--a prospective cohort study. Crit Care Med 37: 553–560, 2009 [DOI] [PubMed] [Google Scholar]
- 20.Pencina MJ, D'Agostino RB, Sr, D'Agostino RB, Jr, Vasan RS: Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond. Stat Med 27: 157–172; discussion 207–212, 2008 [DOI] [PubMed] [Google Scholar]
- 21.Pons B, Lautrette A, Oziel J, Dellamonica J, Vermesch R, Ezingeard E, Mariat C, Bernardin G, Zeni F, Cohen Y, Tardy B, Souweine B, Vincent F, Darmon M: Diagnostic accuracy of early urinary index changes in differentiating transient from persistent acute kidney injury in critically ill patients: Multicenter cohort study. Crit Care 17: R56, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Darmon M, Vincent F, Dellamonica J, Schortgen F, Gonzalez F, Das V, Zeni F, Brochard L, Bernardin G, Cohen Y, Schlemmer B: Diagnostic performance of fractional excretion of urea in the evaluation of critically ill patients with acute kidney injury: A multicenter cohort study. Crit Care 15: R178, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dewitte A, Biais M, Petit L, Cochard JF, Hilbert G, Combe C, Sztark F: Fractional excretion of urea as a diagnostic index in acute kidney injury in intensive care patients. J Crit Care 27: 505–510, 2012 [DOI] [PubMed] [Google Scholar]
- 24.Bagshaw SM, Bennett M, Devarajan P, Bellomo R: Urine biochemistry in septic and non-septic acute kidney injury: A prospective observational study. J Crit Care 28: 371–378, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Darmon M, Schortgen F, Vargas F, Liazydi A, Schlemmer B, Brun-Buisson C, Brochard L: Diagnostic accuracy of Doppler renal resistive index for reversibility of acute kidney injury in critically ill patients. Intensive Care Med 37: 68–76, 2011 [DOI] [PubMed] [Google Scholar]
- 26.Dewitte A, Coquin J, Meyssignac B, Joannès-Boyau O, Fleureau C, Roze H, Ripoche J, Janvier G, Combe C, Ouattara A: Doppler resistive index to reflect regulation of renal vascular tone during sepsis and acute kidney injury. Crit Care 16: R165, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Devarajan P: Neutrophil gelatinase-associated lipocalin: A troponin-like biomarker for human acute kidney injury. Nephrology (Carlton) 15: 419–428, 2010 [DOI] [PubMed] [Google Scholar]
- 28.Schmidt-Ott KM, Mori K, Li JY, Kalandadze A, Cohen DJ, Devarajan P, Barasch J: Dual action of neutrophil gelatinase-associated lipocalin. J Am Soc Nephrol 18: 407–413, 2007 [DOI] [PubMed] [Google Scholar]
- 29.Nickolas TL, O’Rourke MJ, Yang J, Sise ME, Canetta PA, Barasch N, Buchen C, Khan F, Mori K, Giglio J, Devarajan P, Barasch J: Sensitivity and specificity of a single emergency department measurement of urinary neutrophil gelatinase-associated lipocalin for diagnosing acute kidney injury. Ann Intern Med 148: 810–819, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nickolas TL, Schmidt-Ott KM, Canetta P, Forster C, Singer E, Sise M, Elger A, Maarouf O, Sola-Del Valle DA, O’Rourke M, Sherman E, Lee P, Geara A, Imus P, Guddati A, Polland A, Rahman W, Elitok S, Malik N, Giglio J, El-Sayegh S, Devarajan P, Hebbar S, Saggi SJ, Hahn B, Kettritz R, Luft FC, Barasch J: Diagnostic and prognostic stratification in the emergency department using urinary biomarkers of nephron damage: A multicenter prospective cohort study. J Am Coll Cardiol 59: 246–255, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Doi K, Katagiri D, Negishi K, Hasegawa S, Hamasaki Y, Fujita T, Matsubara T, Ishii T, Yahagi N, Sugaya T, Noiri E: Mild elevation of urinary biomarkers in prerenal acute kidney injury. Kidney Int 82: 1114–1120, 2012 [DOI] [PubMed] [Google Scholar]
- 32.Srisawat N, Wen X, Lee M, Kong L, Elder M, Carter M, Unruh M, Finkel K, Vijayan A, Ramkumar M, Paganini E, Singbartl K, Palevsky PM, Kellum JA: Urinary biomarkers and renal recovery in critically ill patients with renal support. Clin J Am Soc Nephrol 6: 1815–1823, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singer E, Elger A, Elitok S, Kettritz R, Nickolas TL, Barasch J, Luft FC, Schmidt-Ott KM: Urinary neutrophil gelatinase-associated lipocalin distinguishes pre-renal from intrinsic renal failure and predicts outcomes. Kidney Int 80: 405–414, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haase M, Devarajan P, Haase-Fielitz A, Bellomo R, Cruz DN, Wagener G, Krawczeski CD, Koyner JL, Murray P, Zappitelli M, Goldstein SL, Makris K, Ronco C, Martensson J, Martling CR, Venge P, Siew E, Ware LB, Ikizler TA, Mertens PR: The outcome of neutrophil gelatinase-associated lipocalin-positive subclinical acute kidney injury: A multicenter pooled analysis of prospective studies. J Am Coll Cardiol 57: 1752–1761, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Siew ED, Ware LB, Bian A, Shintani A, Eden SK, Wickersham N, Cripps B, Ikizler TA: Distinct injury markers for the early detection and prognosis of incident acute kidney injury in critically ill adults with preserved kidney function. Kidney Int 84: 786–794, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gocze I, Koch M, Renner P, Zeman F, Graf BM, Dahlke MH, Nerlich M, Schlitt HJ, Kellum JA, Bein T: Urinary biomarkers TIMP-2 and IGFBP7 early predict acute kidney injury after major surgery. PLoS One 10: e0120863, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coca SG, King JT, Jr, Rosenthal RA, Perkal MF, Parikh CR: The duration of postoperative acute kidney injury is an additional parameter predicting long-term survival in diabetic veterans. Kidney Int 78: 926–933, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rosen S, Heyman SN: Difficulties in understanding human “acute tubular necrosis”: Limited data and flawed animal models. Kidney Int 60: 1220–1224, 2001 [DOI] [PubMed] [Google Scholar]
- 39.Takasu O, Gaut JP, Watanabe E, To K, Fagley RE, Sato B, Jarman S, Efimov IR, Janks DL, Srivastava A, Bhayani SB, Drewry A, Swanson PE, Hotchkiss RS: Mechanisms of cardiac and renal dysfunction in patients dying of sepsis. Am J Respir Crit Care Med 187: 509–517, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]