Abstract
Young women with polycystic ovary syndrome (PCOS) have a high risk of developing endometrial cancer (EC). There is an urgent need for non-surgical prevention and treatment strategies for these patients who fail to respond to progesterone treatment and wish to preserve their fertility. Recently, we have reported that the combined treatment with metformin and progesterone-based oral contraceptives has successfully reversed the early-stage EC into normal endometria in addition to improvement of insulin resistance in women with PCOS. More importantly, one of these treated women has successfully delivered a healthy newborn baby. However, before such treatment can be recommended to the clinical practice, the molecular basis of metformin in the endometrium under physiological and pathological conditions must be elucidated.
Keywords: Metformin, PCOS, Endometrial carcinoma, Fertility
Polycystic ovary syndrome (PCOS), a worldwide health problem, is a heterogeneous hormone-imbalance disorders [1], [2] and occurs in approximately 4%–18% of reproductive-aged women (approximately 12 to 45 years old), depending on the definition [3]. While the etiology and clinical characteristics of PCOS have been well recognized [4], the underlying molecular mechanisms are under active investigation.
Endometrial cancer (EC) is the most common life-threatening gynecological malignancy [5], and young women with PCOS have a high risk of developing EC [6], [7]. It has been reported that women with PCOS and endometrial hyperplasia have four times greater risk of developing EC than women without PCOS [8]. Epidemiological studies have implicated steroid hormonal imbalance in the development of EC [9]. In humans, continuous exposure of the endometrium to estrogens can lead to endometrial overgrowth and hyperplasia [10], and progesterone acts as a protective factor against estrogen-driven uterine cell growth and proliferation [11]. Women with PCOS often present with an abnormal menstrual cycle and anovulation that result in a persistent progesterone deficiency [12]. Thus, the endometrium in women with PCOS tends to remain in an estrogen dominant proliferative state due to the lack of counterbalance by progesterone [5], [13]. In the clinic, progesterone-based oral contraceptives are used to inhibit endometrial hyper-proliferation and improve menstrual dysfunction [14]. However, approximately 30% of women with PCOS fail to respond to such treatment [15]. This results in the development and progression of atypical hyperplasia and further transformation to EC. Although EC can be detected at an early stage, surgery is currently the only truly effective means of treating EC in women with PCOS who have progesterone resistance [12]. Furthermore, surgical treatment may negatively affect future fertility. Therefore, there is an urgent need for non-surgical prevention and treatment strategies for young women with PCOS who wish to preserve their fertility [16].
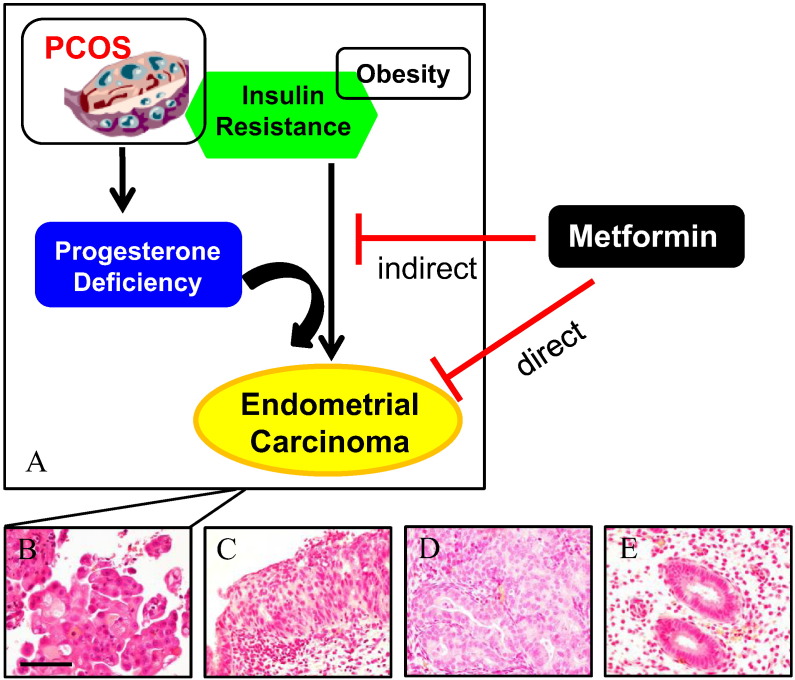
Insulin resistance and hyperinsulinemia appear to be one of major contributors to the pathophysiology of PCOS in women [17]. For example, it has been reported that 50%–70% of women with PCOS exhibit insulin resistance [18]. It is well known that metformin (N,N-dimethylbiguanide), an oral biguanide insulin-sensitizing drug, is used as first-line treatment for type 2 diabetes mellitus worldwide [19]. We and other investigators have previously shown that the combinational therapy of metformin and progesterone-based oral contraceptives such as Diane-35 is sufficient to not only change the insulin resistance state but also reverse atypical endometrial hyperplasia in women with PCOS who fail to respond to progesterone treatment and preserve their fertility [20], [21]. Multiple lines of evidence support that treatment with metformin results in decreased incidence, progression, and even cancer-related mortality of different human cancers [22], [23] including EC [24]. That brings us to the question: does metformin have a beneficial effect on the endometrium in women with PCOS and EC? Very recently, we have reported that the similar combined treatment is capable of reversing the early-stage EC into normal endometria (Fig. 1 B to D) in addition to improvement of insulin resistance in women with PCOS [25].
Fig. 1.
Hypothetical models of metformin actions in women with PCOS and early-stage endometrial cancer. On the basis of the evidence accumulated in other metformin-target tissues, we propose that the systemic and/or local endometria actions of metformin (A) revert the endometrial cancer into normal endometrial cells in women with PCOS and early-stage endometrial cancer. Representative microscopic photomicrographs of early endometrial carcinoma (B, clinical stage 1a, grade 1), complex hyperplasia with atypia (C), complex hyperplasia (D), and normal endometria (E) in women with PCOS and early-stage endometrial cancer before, during, and after co-treatment with metformin and Diane-35. Microscopic images stained with hematoxylin and eosin. Scale bar: 100 μm.
In our early phase human study [25], women with PCOS and EC were co-treated with metformin and Diane-35 for 6 months. After the combination treatment, all patients were requested to continuously measure and record their basal body temperature and to record whether ovulation occurs. If we find that the ovulation did not occur, the patients would receive progesterone-based oral contraceptive therapy during the secretary phase of their menstrual cycle to prevent the endometria from becoming atypical hyperplasia again. In addition, B-ultrasound is used for regular follow-up observations in these patients. Regarding the nature of the disease [1], [2], women with PCOS who have previous EC and atypical hyperplasia often relapse if there is no follow-up treatment. Therefore, if we observe any abnormal changes, for example, in endometrial thickness or shape, the patients must be examined using hysteroscopy. Because the purpose of combination treatment with metformin and oral contraceptives in women with PCOS and EC is to preserve their uterus for future pregnancy [25], it is best to help patients obtain regulated ovulation and subsequent normal uterine pregnancy as early as possible after co-treatment. The good news is that one of these treated women has successfully delivered a healthy newborn baby (our unpublished data). Altogether, our work has suggested that such treatment not only improves various endocrine and metabolic symptoms, but also preserves the fertility in women with PCOS and EC.
As clinicians, we notice that our preliminary reports [25] must be carefully weighed and further research is certainly needed before co-treatment with metformin and oral contraceptives can be recommended as routine clinical practice. Having said that, this raises the question as to how a positive effect of metformin combined with oral contraceptives at the molecular level could inhibit the development of atypical endometrial hyperplasia and EC, whether metformin individually affects endometrial function in women with PCOS, and how our findings affect treatment guidelines for PCOS women with and without insulin resistance. It is important to await the full analysis of the complete findings before reaching definitive conclusions. In fact, we have started a new randomized trial with a larger sample size and longer follow-up period. The cellular and molecular mechanisms behind the treatment effect will also be further investigated in greater detail.
The primary function of metformin is to inhibit hepatic gluconeogenesis and decrease glucose production in the liver that causes decreased circulating glucose and insulin levels, while it improves insulin sensitivity and enhance glucose uptake and utilization in peripheral tissues such as skeletal muscle and adipocytes [23]. However, the identified mechanism of anti-diabetic and anti-cancer actions for metformin in women with PCOS and EC has remained largely unknown [17], [26]. Organic cation transporters (OCTs) and multidrug/toxin extrusion proteins (MATEs) are crucial for the cellular uptake and excretion of metformin. We reported that specific OCTs and MATEs were expressed in the human endometrium [27]. Therefore, future studies are needed to clarify whether metformin has direct and/or indirect effects on the endometrium in women with PCOS and EC (Fig. 1A). Because clinical and epidemiological investigations suggest that obesity and type 2 diabetes are strong risk factors for increased EC incidence and mortality [28], understanding the effects of metformin in the endometrium will take us one step closer to understanding the molecular mechanisms of EC inhibition, and may be beneficial in finding out ways to prevent and treat the EC development and progression in women with PCOS and/or obesity.
Acknowledgments
This work was supported by the Swedish Medical Research Council (5859 and 10380), the Swedish federal government under the LUA/ALF agreement (ALFGBG-147791), Jane and Dan Olsson's Foundation, the Åke-Wiberg Foundation, and Clas Groschinsky's Foundation.
References
- 1.Norman R.J., Dewailly D., Legro R.S., Hickey T.E. Polycystic ovary syndrome. Lancet. 2007;370:685–697. doi: 10.1016/S0140-6736(07)61345-2. [DOI] [PubMed] [Google Scholar]
- 2.Ehrmann D.A. Polycystic ovary syndrome. N. Engl. J. Med. 2005;352:1223–1236. doi: 10.1056/NEJMra041536. [DOI] [PubMed] [Google Scholar]
- 3.Moran L.J., Hutchison S.K., Norman R.J., Teede H.J. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst. Rev. 2011:CD007506. doi: 10.1002/14651858.CD007506.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Sirmans S.M., Pate K.A. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clin. Epidemiol. 2013;6:1–13. doi: 10.2147/CLEP.S37559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim J.J., Kurita T., Bulun S.E. Progesterone action in endometrial cancer, endometriosis, uterine fibroids, and breast cancer. Endocr. Rev. 2013;34:130–162. doi: 10.1210/er.2012-1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haoula Z., Salman M., Atiomo W. Evaluating the association between endometrial cancer and polycystic ovary syndrome. Hum. Reprod. 2012;27:1327–1331. doi: 10.1093/humrep/des042. [DOI] [PubMed] [Google Scholar]
- 7.Barry J.A., Azizia M.M., Hardiman P.J. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum. Reprod. Update. 2014;20(5):748–758. doi: 10.1093/humupd/dmu012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fearnley E.J., Marquart L., Spurdle A.B., Weinstein P., Webb P.M. Polycystic ovary syndrome increases the risk of endometrial cancer in women aged less than 50 years: an Australian case–control study. Cancer Causes Control. 2010;21:2303–2308. doi: 10.1007/s10552-010-9658-7. [DOI] [PubMed] [Google Scholar]
- 9.Setiawan V.W., Yang H.P., Pike M.C., McCann S.E., Yu H., Xiang Y.B., Wolk A., Wentzensen N., Weiss N.S., Webb P.M., van den Brandt P.A., van de Vijver K., Thompson P.J., Strom B.L., Spurdle A.B., Soslow R.A., Shu X.O., Schairer C., Sacerdote C., Rohan T.E., Robien K., Risch H.A., Ricceri F., Rebbeck T.R., Rastogi R., Prescott J., Polidoro S., Park Y., Olson S.H., Moysich K.B., Miller A.B., McCullough M.L., Matsuno R.K., Magliocco A.M., Lurie G., Lu L., Lissowska J., Liang X., Lacey J.V., Jr., Kolonel L.N., Henderson B.E., Hankinson S.E., Hakansson N., Goodman M.T., Gaudet M.M., Garcia-Closas M., Friedenreich C.M., Freudenheim J.L., Doherty J., De Vivo I., Courneya K.S., Cook L.S., Chen C., Cerhan J.R., Cai H., Brinton L.A., Bernstein L., Anderson K.E., Anton-Culver H., Schouten L.J., Horn-Ross P.L. Type I and II endometrial cancers: have they different risk factors? J. Clin. Oncol. 2013;31:2607–2618. doi: 10.1200/JCO.2012.48.2596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horn L.C., Meinel A., Handzel R., Einenkel J. Histopathology of endometrial hyperplasia and endometrial carcinoma: an update. Ann. Diagn. Pathol. 2007;11:297–311. doi: 10.1016/j.anndiagpath.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Yang S., Thiel K.W., Leslie K.K. Progesterone: the ultimate endometrial tumor suppressor. Trends Endocrinol. Metab. 2011;22:145–152. doi: 10.1016/j.tem.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li X., Feng Y., Lin J.F., Billig H., Shao R. Endometrial progesterone resistance and PCOS. J. Biomed. Sci. 2014;21:2. doi: 10.1186/1423-0127-21-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hardiman P., Pillay O.C., Atiomo W. Polycystic ovary syndrome and endometrial carcinoma. Lancet. 2003;361:1810–1812. doi: 10.1016/s0140-6736(03)13409-5. [DOI] [PubMed] [Google Scholar]
- 14.Vrbikova J., Cibula D. Combined oral contraceptives in the treatment of polycystic ovary syndrome. Hum. Reprod. Update. 2005;11:277–291. doi: 10.1093/humupd/dmi005. [DOI] [PubMed] [Google Scholar]
- 15.Aghajanova L., Velarde M.C., Giudice L.C. Altered gene expression profiling in endometrium: evidence for progesterone resistance. Semin. Reprod. Med. 2010;28:51–58. doi: 10.1055/s-0029-1242994. [DOI] [PubMed] [Google Scholar]
- 16.Lee W.L., Lee F.K., Su W.H., Tsui K.H., Kuo C.D., Hsieh S.L., Wang P.H. Hormone therapy for younger patients with endometrial cancer. Taiwan. J. Obstet. Gynecol. 2012;51:495–505. doi: 10.1016/j.tjog.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Li X., Shao R. PCOS and obesity: insulin resistance might be a common etiology for the development of type I endometrial carcinoma. Am. J. Cancer Res. 2014;4:73–79. [PMC free article] [PubMed] [Google Scholar]
- 18.Gambineri A., Pelusi C., Vicennati V., Pagotto U., Pasquali R. Obesity and the polycystic ovary syndrome. Int. J. Obes. Relat. Metab. Disord. 2002;26:883–896. doi: 10.1038/sj.ijo.0801994. [DOI] [PubMed] [Google Scholar]
- 19.Nestler J.E. Metformin for the treatment of the polycystic ovary syndrome. N. Engl. J. Med. 2008;358:47–54. doi: 10.1056/NEJMct0707092. [DOI] [PubMed] [Google Scholar]
- 20.Shen Z.Q., Zhu H.T., Lin J.F. Reverse of progestin-resistant atypical endometrial hyperplasia by metformin and oral contraceptives. Obstet. Gynecol. 2008;112:465–467. doi: 10.1097/AOG.0b013e3181719b92. [DOI] [PubMed] [Google Scholar]
- 21.Session D.R., Kalli K.R., Tummon I.S., Damario M.A., Dumesic D.A. Treatment of atypical endometrial hyperplasia with an insulin-sensitizing agent. Gynecol. Endocrinol. 2003;17:405–407. doi: 10.1080/09513590312331290298. [DOI] [PubMed] [Google Scholar]
- 22.Dowling R.J., Niraula S., Stambolic V., Goodwin P.J. Metformin in cancer: translational challenges. J. Mol. Endocrinol. 2012;48:R31–R43. doi: 10.1530/JME-12-0007. [DOI] [PubMed] [Google Scholar]
- 23.Del Barco S., Vazquez-Martin A., Cufi S., Oliveras-Ferraros C., Bosch-Barrera J., Joven J., Martin-Castillo B., Menendez J.A. Metformin: multi-faceted protection against cancer. Oncotarget. 2011;2:896–917. doi: 10.18632/oncotarget.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nevadunsky N.S., Van Arsdale A., Strickler H.D., Moadel A., Kaur G., Frimer M., Conroy E., Goldberg G.L., Einstein M.H. Metformin use and endometrial cancer survival. Gynecol. Oncol. 2014;132:236–240. doi: 10.1016/j.ygyno.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li X., Guo J.R., Lin J.F., Feng Y., Billig H., Shao R. Combination of Diane-35 and metformin to treat early endometrial carcinoma in PCOS women with insulin resistance. J. Cancer. 2014;5:173–181. doi: 10.7150/jca.8009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shafiee M.N., Khan G., Ariffin R., Abu J., Chapman C., Deen S., Nunns D., Barrett D.A., Seedhouse C., Atiomo W. Preventing endometrial cancer risk in polycystic ovarian syndrome (PCOS) women: could metformin help? Gynecol. Oncol. 2014;132:248–253. doi: 10.1016/j.ygyno.2013.10.028. [DOI] [PubMed] [Google Scholar]
- 27.Shao R., Li X., Feng Y., Lin J.F., Billig H. Direct effects of metformin in the endometrium: a hypothetical mechanism for the treatment of women with PCOS and endometrial carcinoma. J. Exp. Clin. Cancer Res. 2014;33:41. doi: 10.1186/1756-9966-33-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmandt R.E., Iglesias D.A., Co N.N., Lu K.H. Understanding obesity and endometrial cancer risk: opportunities for prevention. Am. J. Obstet. Gynecol. 2011;205:518–525. doi: 10.1016/j.ajog.2011.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]