Abstract
The goal of the present study was to determine whether pre-hospital 25-hydroxyvitamin D (25(OH)D) levels are associated with the risk of hospital-acquired new-onset delirium (HANOD). We performed a retrospective cohort study of 4508 adult inpatients at two teaching hospitals in Boston from 1993 to 2006. All patients had 25(OH)D levels measured before hospital admission. The main outcome measure was HANOD, defined as the onset of delirium during an acute care hospitalisation. Patients with a history of delirium or dementia, or those with a diagnosis of delirium or dementia upon acute care hospitalisation were excluded from the analysis. To test the association of pre-hospital 25(OH)D levels with HANOD, we constructed a multivariable logistic regression model to adjust for clinically relevant covariates. Among our patient cohort, the mean 25(OH)D level was 22 (SD 13) ng/ml and approximately 4 % of patients met the criteria for HANOD. Following adjustment for age, sex, race (non-white v. white), patient type (medical v. surgical) and Deyo–Charlson Index, patients with 25(OH)D levels , 10, 10–19·9 and 20–29·9 ng/ml had higher odds of HANOD than patients with 25(OH)D levels ≥ 30 ng/ml: OR 2·15 (95 % CI 1·32, 3·50), OR 1·54 (95 % CI 0·98, 2·43) and OR 1·23 (95 % CI, 0·76, 1·99), respectively. These data support the rationale for randomised, controlled trials to test the role of vitamin D supplementation in the prevention of HANOD.
Keywords: Vitamin D, 25-Hydroxyvitamin D, Delirium, Nosocomial infections, Hospital-acquired new-onset delirium
Delirium is a complex neuropsychiatric syndrome defined by five key elements: (1) a disturbance of attention; (2) a change in cognition; (3) a rapid onset; (4) a fluctuating course; (5) history, physical examination or laboratory findings which suggest that the disturbance is caused by a direct physiological consequence of a general medical condition, an intoxicating substance, medication use or more than one cause(1). It is commonly encountered in health care settings and has an occurrence rate between 11 and 56 % in hospitalised patients(2,3). While many patients may have a pre-existing history of delirium or another neurocognitive disorder (e.g. dementia) that significantly increases the risk of delirium in an institutionalised setting(4–6), the incidence of hospital-acquired new-onset delirium (HANOD) in other wise ‘low-risk’ individuals is estimated to be between 3 and 29 %(2). On average, patients who develop HANOD remain hospitalised 4–13 d longer than their non-delirious counterparts(7). There is also a 2-fold increased risk of mortality at 12 months when patients who develop HANOD are compared with those who remain free of delirium(2). In the USA, annual health care expenditures attributable to HANOD are estimated to be $38–152 billion(8).
The underlying cause of delirium is often multifactorial(9). Age, sex, medical comorbidities, recent surgery and history of cognitive impairment are all known risk factors for delirium in hospitalised patients(7,9). Recently, with the discovery of vitamin D receptors in the human cortex and hippocampus (areas critical for intact cognition)(10), the role of vitamin D status in neuropsychiatric disorders has become an area of active investigation(11,12). Indeed, levels of the best serum marker of vitamin D status, 25-hydroxyvitamin D (25(OH)D), have been shown to be associated with the risk of dementia(13), Alzheimer’s disease(14) and depression(15). Given the high prevalence of suboptimal 25(OH)D levels in the general population of the USA(16–20), we performed a two-centre observational study of hospitalised adult patients. The objective of the present study was to investigate whether vitamin D status before hospital admission is associated with an increased risk of developing HANOD.
Materials and methods
Source population
We abstracted administrative and laboratory data from individuals who were hospitalised at one of two teaching hospitals in Boston, Massachusetts: Brigham and Women’s Hospital, with777 beds, and Massachusetts General Hospital, with 902 beds. These two hospitals provide primary and tertiary care to an ethnically and socioeconomically diverse population within and around Eastern Massachusetts.
Data sources
We obtained data on all patients admitted to Brigham and Women’s Hospital or Massachusetts General Hospital between August 1993 and November 2006 through the Research Patient Data Registry (RPDR). RPDR is a computerised registry, which serves as a central data warehouse for allinpatient and outpatient records at Partners HealthCare facilities (including Brigham and Women’s Hospital and Massachusetts General Hospital). The registry has been used for multiple clinical research studies(21–25). The Institutional Review Board approval for the study was granted by the Partners Human Research Committee.
Study population
We identified 5341 individual patient admissions (age ≥ 18 years) over the study period that were assigned a Diagnostic Related Group and that had documented serum 25(OH)D measurements between 7 and 365 d before hospitalisation. The Diagnostic Related Group is a nationwide classification system used by hospitals in the USA to categorise the expected resource utilisation for a specific medical case (e.g. heart failure exacerbation, appendectomy). We then excluded five foreign patients without Social Security Numbers since vital status in the present study was determined by the Social Security Administration Death Master File, and 828 patients who had existinghistory of delirium or dementia, or a diagnosis of delirium or dementia upon hospitalisation. Thefinal study cohort was therefore composed of 4508 patients.
Exposure and outcome of interest
The exposure of interest was pre-admission serum 25(OH)D level obtained 7–365 d before the date of hospitalisation. 25(OH)D levels were categorised a priori as<10, 10–19·9, 20–29·9 and ≤30ng/ml. All cut points were adapted from the Endocrine Society clinical practice guidelines(26). Serum 25(OH)D in all cohort subjects was determined by RIA utilising the DiaSorin Corporation 25-Hydroxyvitamin D 125I RIAkit(27). Inter- and intra-assay CV were both<10 %. The primary outcome of interest was the presence of HANOD. HANOD was defined as the new presence of International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM) codes related to delirium: 290.11, 290.3, 290.41, 291.–9,292.81, 293.0 – 293.0 293.9, 300.11, 308.09, 780.02 or780.09 during hospitialisation.
Comorbidities
Data specific to age, sex and race for each patient was directly abstracted from the RPDR. We utilised the ICD-9-CM coding algorithms, which are well studied and validated(30,31), to derive the Deyo–Charlson Index to assess the burden of chronic illness in our study cohort(32). ‘Patient Type’ was defined as ‘Medical’ or ‘Surgical’ and incorporated the Diagnostic Related Group methodology(33).Recent surgery data were obtained from operating room schedule records and was defined as a surgical procedure performed in the operating room before delirium diagnosis. Intensive care unit admission was determined by the assignment of Current Procedural Terminology code 99 291 (critical care, first 30–74 min) during hospitalisation. The use of Current Procedural Terminologycode 99 291 in this manner has been previously validated in the RPDR database(25). Chronic liver disease was determined by ICD-9-CM codes 571.xx, 70.54 and 70.32 (34). Sepsis was defined by the hospitalisation: 038.0–038.9; 020.0; 790.7; 117.9; 112.5 112.8(35), with exclusion of sepsis occurring after a diagnosis of delirium. We have validated ICD-9-CM identification of sepsis in the RPDR database(36). History of major depressive disorder was defined by the presence of ICD-9-CM codes 296.2x or 296.3x before hospital admission(37). Antipsychotic medication use was determined via pharmacy data of haloperidol, risperidone or olanzapine prescriptions during hospitalisation, since these were the antipsychotic medications on the hospital formularies over the study period.
Assessment of mortality
Information on vital status for the study cohort was obtained from the Social Security Administration Death Master File, which has a reported sensitivity for mortality up to 92 % and a specificity of . 99 %(38–41). Utilisation of the Death Master File allows for long-term follow-up of patients after hospital discharge.
Power calculations and statistical analysis
Based on previous studies on HANOD susceptibility among hospitalised patients(2), we assumed that delirium incidence would decrease from 10 % in patients with pre-hospital 25(OH)D<20 ng/ml to 5 % in those with pre-hospital 25(OH)D ≥ 20 ng/ml. With an a error level of 5 % and a power of 80 %, the minimum sample size thus required for our primary end point (HANOD) is 1242 total patients.
Categorical variables were described by frequency distributions, and compared across 25(OH)D groups using contingency tables and χ2 testing. Continuous variables were examined graphically (e.g. histogram and box plot) and in terms of summary statistics, i.e. mean and standard deviation for normally distributed data or median and interquartile range for nonparametric data, and then compared across exposure groups using one-way ANOVA. The outcome considered was HANOD.
Unadjusted associations between 25(OH)D groups and HANOD were estimated by bivariable logistic regression models. Adjusted OR were estimated by multivariable logistic regression models, including a priori covariate terms considered to plausibly associate with both 25(OH)D levels and HANOD(8) to avoid unnecessarily adjusting for variables that do not affect bias or the causal relationship between exposure and outcome(42). For the primary model (HANOD), specification of each continuous covariate (as a linear v. categorical term) was adjudicated by theempiric association with the primary outcome using Akaike’s Information Criterion; overallmodel fit was assessed using the Hosmer–Lemeshow test. Models for secondary analyses were specified identically to the primary model. Unadjusted event rates were calculated with the useof the Kaplan–Meier methods and compared with the use of the log-rank test. Locally weighted scatter plot smoothing(43,44) was used to graphically represent the relationship between pre-hospital 25(OH)D level and the risk of HANOD. All P-values are two-tailed, with values , 0<0.05 considered statistically significant. All analyses were performed using Stata 12.0MP statistical software (Stata Corporation).
Results
Most patients were female, white and had a medical-related Diagnostic Related Group (Table 1). The mean age at hospital admission was 59 (SD 18) years. Approximately 4 % of the cohort patients (n 198) met the criteria for HANOD. The mean 25(OH)D level was 22 (SD 13) ng/ml (to convert to nmol/l, multiply by 2·496). The 45 % of the 25(OH)D measurements occurred in the 3 months before hospital admission.
Table 1.
Baseline demographic characteristics of the study population (Number of subjects and percentages; mean values and standard deviations)
| Non- HANOD |
HANOD |
Total |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Total number of cases | 4309 | 199 | 4508 | |||
| Age (years) | ||||||
| Mean | 59 | 67 | 59 | |||
| SD | 18 | 18 | 18 | |||
| Sex | ||||||
| Female | 2836 | 66 | 125 | 63 | 2961 | 66 |
| Male | 1473 | 34 | 74 | 37 | 1547 | 34 |
| Race | ||||||
| White | 3606 | 84 | 168 | 84 | 3774 | 84 |
| Non-white | 703 | 16 | 31 | 16 | 734 | 16 |
| Patient type | ||||||
| Medical | 2517 | 58 | 138 | 69 | 2655 | 59 |
| Surgical | 1792 | 42 | 61 | 31 | 1853 | 41 |
| Deyo–Charlson Index | ||||||
| 0–3 | 1969 | 46 | 48 | 24 | 2017 | 45 |
| 4–6 | 1103 | 26 | 62 | 31 | 1165 | 26 |
| ≥7 | 1237 | 29 | 89 | 45 | 1326 | 29 |
| Recent surgery | 150 | 4 | 9 | 5 | 159 | 4 |
| Psychiatric primary diagnosis |
62 | 1·4 | 3 | 1·5 | 65 | 1·4 |
| Antipsychotic medications | 174 | 4 | 72 | 36 | 246 | 5 |
| Major depressive disorder history |
134 | 3 | 14 | 7 | 148 | 3 |
| 25(OH)D (ng/ml) | ||||||
| Mean | 22 | 19 | 22 | |||
| SD | 13 | 11 | 13 | |||
| Season of 25(OH)D draw | ||||||
| Autumn | 925 | 21 | 57 | 29 | 982 | 22 |
| Spring | 1096 | 25 | 38 | 19 | 1134 | 25 |
| Summer | 1035 | 24 | 61 | 31 | 1096 | 24 |
| Winter | 1253 | 29 | 43 | 22 | 1296 | 29 |
| Vitamin D supplemental use* |
501 | 12 | 36 | 18 | 537 | 12 |
| 90 d mortality | 284 | 7 | 47 | 24 | 331 | 7 |
HANOD, hospital-acquired new-onset delirium; 25(OH)D, 25-hydroxyvitamin D.
Vitamin D supplemental use refers to vitamin D supplementation in the year before hospitalisation.
Patient characteristics of the study cohort were stratified according to pre-admission 25(OH)D levels (Table 2). Factors that significantly differed between stratified groups included age,sex, race, patient type (medical v. surgical), Deyo–Charlson Index and vitamin D supplementation use. 25(OH)D levels, age and Deyo–Charlson Index were found to be significant predictors of HANOD (Table 3). In-hospital, 30-d and 90-d mortality rates were 3, 4 and 7 %, respectively.
Table 2.
Patient characteristics by pre-hospital vitamin D status (Number of subjects and percentages; mean values and standard deviations)
| Pre-hospital 25(OH)D |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| <10 ng/ml |
10–199 ng/ml |
20–299 ng/ml |
≥30 ng/ml |
||||||
| n | % | n | % | n | % | n | % | P * | |
| Number of cases | 742 | 1542 | 1342 | 882 | |||||
| Age (years) | 0·012† | ||||||||
| Mean | 59 | 58 | 60 | 61 | |||||
| SD | 18 | 18 | 18 | 18 | |||||
| Sex | 0·001 | ||||||||
| Female | 472 | 64 | 980 | 64 | 879 | 66 | 630 | 71 | |
| Male | 270 | 36 | 562 | 36 | 463 | 35 | 252 | 29 | |
| Race | < 0·001 | ||||||||
| White | 567 | 76 | 1248 | 81 | 1161 | 87 | 798 | 90 | |
| Non-white | 175 | 24 | 294 | 19 | 181 | 13 | 84 | 10 | |
| Patient type | <0·001 | ||||||||
| Medical | 511 | 69 | 909 | 59 | 759 | 57 | 476 | 54 | |
| Surgical | 231 | 31 | 633 | 41 | 583 | 43 | 406 | 46 | |
| Deyo–Charlson Index | <0·001 | ||||||||
| 0–3 | 250 | 34 | 683 | 44 | 660 | 49 | 424 | 48 | |
| 4–6 | 202 | 27 | 415 | 27 | 325 | 24 | 223 | 25 | |
| ≥7 | 290 | 39 | 444 | 29 | 357 | 27 | 235 | 27 | |
| Chronic liver disease | 182 | 25 | 403 | 26 | 324 | 24 | 184 | 21 | 0·036 |
| Psychiatric primary diagnosis | 11 | 2 | 24 | 2 | 19 | 1 | 11 | 1 | 0·85 |
| Major depressive disorder history | 25 | 3 | 51 | 3 | 53 | 4 | 19 | 2 | 0·14 |
| Antipsychotic medications | 47 | 6 | 87 | 6 | 73 | 5 | 39 | 4 | 0·39 |
| Vitamin D supplemental use‡ | 126 | 17 | 194 | 13 | 121 | 9 | 96 | 11 | <0·001 |
| Sepsis | 59 | 8 | 77 | 5 | 57 | 4 | 26 | 3 | <0·001 |
| Bloodstream infection§ | 38 | 17 | 65 | 17 | 39 | 13 | 29 | 14 | 0·38 |
| Leucocytes (×103/μl)∥ | 0·061 | ||||||||
| 0–3·9 | 36 | 5 | 44 | 3 | 37 | 3 | 25 | 3 | |
| 4·0–9·9 | 354 | 48 | 705 | 46 | 649 | 48 | 432 | 49 | |
| >10 | 352 | 47 | 793 | 51 | 656 | 49 | 425 | 48 | |
| Creatinine (>133 μmol/l) | 261 | 35 | 350 | 23 | 256 | 19 | 152 | 17 | <0·001 |
| ICU admission | 63 | 8 | 105 | 7 | 107 | 8 | 69 | 8 | 0·47 |
| HANOD | 51 | 7 | 71 | 5 | 50 | 4 | 27 | 3 | 0·001 |
| 90 d mortality | 78 | 11 | 133 | 9 | 76 | 6 | 44 | 5 | <0·001 |
25(OH)D, 25-hydroxyvitamin D; ICU, intensive care unit; HANOD, hospital-acquired new-onset delirium.
P values were determined by Kruskal–Wallis test.
P value determined by χ2 test.
Vitamin D supplemental use refers to vitamin D supplementation in the year before hospitalisation.
1116 patients with blood cultures drawn.
Leucocyte count measured at hospital admission.
Table 3.
Multivariable-adjusted associations between covariates and hospital-acquired new-onset delirium (HANOD)* (Odds ratios and 95% confidence intervals)
| OR | 95% CI | P | |
|---|---|---|---|
| Age (per 1 year) | 1·02 | 1·01, 1·03 | <0·001 |
| Sex | 0·55 | ||
| Female | 1·00 | Reference | |
| Male | 1·10 | 0·81, 1·48 | |
| Race | 0·60 | ||
| Non-white | 1·00 | Reference | |
| White | 0·90 | 0·60, 1·34 | |
| Patient type | |||
| Medical | 1·00 | Reference | 0·13 |
| Surgical | 0·61 | 0·32, 1·15 | |
| Deyo–Charlson Index | |||
| 0–3 | 1·00 | Reference | |
| 4–6 | 1·77 | 1·19, 2·62 | 0·005 |
| ≥7 | 2·12 | 1·46, 3·09 | <0·001 |
| Pre-hospital 25(OH)D (ng/ml) | |||
| <10 | 2·15 | 1·32, 3·50 | 0·002 |
| 10–19·9 | 1·54 | 0·98, 2·43 | 0·063 |
| 20–29·9 | 1·23 | 0·76, 1·99 | 0·39 |
| ≥30 | 1·00 | Reference |
25(OH)D, 25-hydroxyvitamin D.
Adjusted OR were estimated by a multivariable logistic regression model with inclusion of covariate terms considered to plausibly associate with vitamin D status and HANOD. Estimates for each variable are adjusted for all other variables in the table.
Primary outcome
Low pre-admission vitamin D status was a strong predictor of HANOD after adjustment for age, sex, race, Deyo–Charlson Index and patient type (Table 4). The adjusted odds of HANOD in patients with 25(OH)D levels<10 ng/ml and in those with levels 10–19·9 ng/ml were 2·2- and 1·5-fold higher than in patients with 25(OH)D levels ≥30 ng/ml,respectively (Table 4). Additional individual adjustment for potential confounders such as recent surgery, sepsis, history of major depression, antipsychotic drug medication use, leucocyte count or calcium on admission, chronic liver disease, season of 25(OH)D draw, the timing of the 25(OH)D draw relative to admission and intensive care unit admission did not materially alter these point estimates (Table 5).
Table 4.
Unadjusted and adjusted associations between pre-hospital vitamin D status and hospital-acquired new-onset delirium (HANOD)* (Odds ratios and 95% confidence intervals, n 4508)
| Pre-hospital 25(OH)D |
||||
|---|---|---|---|---|
| <10 ng/ml | 10–199 ng/ml | 20–299 ng/ml | ≥30 ng/ml | |
| Unadjusted | ||||
| OR | 2·34 | 1·53 | 1·23 | 1·00 |
| 95% CI | 1·45, 3·77 | 0·97, 2·40 | 0·76, 1·97 | Referent |
| P | <0·001 | 0·065 | 0·40 | |
| Adjusted | ||||
| OR | 2·15 | 1·54 | 1·23 | 1·00 |
| 95% CI | 1·32, 3·50 | 0·98, 2·43 | 0·76, 1·99 | Referent |
| P | 0·002 | 0·063 | 0·39 | |
25(OH)D, 25-hydroxyvitamin D.
Unadjusted associations between 25(OH)D groups and HANOD were estimated by bivariable logistic regression models. Adjusted OR were estimated by multi-variable logistic regression models with inclusion of covariate terms considered to plausibly associate with both 25(OH)D concentrations and HANOD. Estimates adjusted for age, sex, race (non-white v. white), patient type (medical v. surgical) and Deyo–Charlson Index.
Table 5.
Adjusted associations between pre-hospital vitamin D status and hospital-acquired new-onset delirium (HANOD)* (Odds ratios and 95 % confidence intervals, n 4508)
| Pre-hospital 25(OH)D |
||||
|---|---|---|---|---|
| <10 ng/ml | 10–199 ng/ml | 20–299 ng/ml | ≥30 ng/ml | |
| Adjusted+recent surgery | ||||
| OR | 2·13 | 1·51 | 1·21 | 1·00 |
| 95% CI | 1·30, 3·48 | 0·96, 2·39 | 0·75, 1·96 | Referent |
| P | 0·003 | 0·078 | 0·44 | |
| Adjusted+sepsis | ||||
| OR | 2·04 | 1·51 | 1·21 | 1·00 |
| 95% CI | 1·25, 3·33 | 0·96, 2·39 | 0·75, 1·96 | Referent |
| P | 0·004 | 0·076 | 0·43 | |
| Adjusted+ depression | ||||
| OR | 2·14 | 1·53 | 1·20 | 1·00 |
| 95% CI | 1·32, 3·48 | 0·97, 2·42 | 0·74, 1·94 | Referent |
| P | 0·002 | 0·067 | 0·45 | |
| Adjusted+ antipsychotics | ||||
| OR | 2·01 | 1·45 | 1·15 | 1·00 |
| 95% CI | 1·21, 3·35 | 0·91, 2·33 | 0·70, 1·90 | Referent |
| P | 0·007 | 0·12 | 0·57 | |
| Adjusted+leucocyte count | ||||
| OR | 2·15 | 1·52 | 1·23 | 1·00 |
| 95% CI | 1·32, 3·49 | 0·97, 2·41 | 0·76, 1·99 | Referent |
| P | 0·002 | 0·069 | 0·40 | |
| Adjusted+Ca | ||||
| OR | 2·15 | 1·55 | 1·24 | 1·00 |
| 95% CI | 1·33, 3·50 | 0·98, 2·44 | 0·77, 2·01 | Referent |
| P | 0·002 | 0·061 | 0·38 | |
| Adjusted+liver disease | ||||
| OR | 2·16 | 1·54 | 1·23 | 1·00 |
| 95% CI | 1·33, 3·51 | 0·98, 2·43 | 0·76, 1·99 | Referent |
| P | 0·002 | 0·063 | 0·39 | |
| Adjusted+season of 25(OH)D draw |
||||
| OR | 2·14 | 1·51 | 1·21 | 1·00 |
| 95% CI | 1·30, 3·49 | 0·96, 2·40 | 0·75, 1·96 | Referent |
| P | 0·003 | 0·076 | 0·43 | |
| Adjusted+timing of 25(OH)D draw | ||||
| OR | 2·09 | 1·52 | 1·23 | 1·00 |
| 95% CI | 1·28, 3·41 | 0·97, 2·40 | 0·76, 1·99 | Referent |
| P | 0·003 | 0·071 | 0·39 | |
| Adjusted+ICU admission | ||||
| OR | 2·22 | 1·61 | 1·23 | 1·00 |
| 95% CI | 1·36, 3·62 | 1·01, 2·55 | 0·76, 2·00 | Referent |
| P | 0·001 | 0·043 | 0·40 | |
25(OH)D, 25-hydroxyvitamin D; ICU, intensive care unit.
Adjusted associations between 25(OH)D groups and HANOD were estimated by multivariable logistic regression models with the inclusion of covariate terms considered to plausibly associate with both 25(OH)D concentrations and HANOD. Adjusted estimates adjusted for age, sex, race (non-white v. white), patient type (medical v. surgical) and Deyo–Charlson index.
Secondary outcomes
To assess the discrimination of 25(OH)D for HANOD, we used receiver-operating characteristic curve analysis and determined the AUC. Estimating the AUC showed that 25(OH)D had poor discriminative power for HANOD: AUC = 0.57 (95 % CI 0.53, 0.61). Locally weighted scatter plot smoothing plot (Fig. 1) showed a near inverse linear association between 25(OH)D level and the risk of HANOD up to 25(OH)D levels near 30 ng/ml. Beyond 25(OH)D of 40 ng/ml, thecurve appears flat.
Fig. 1.
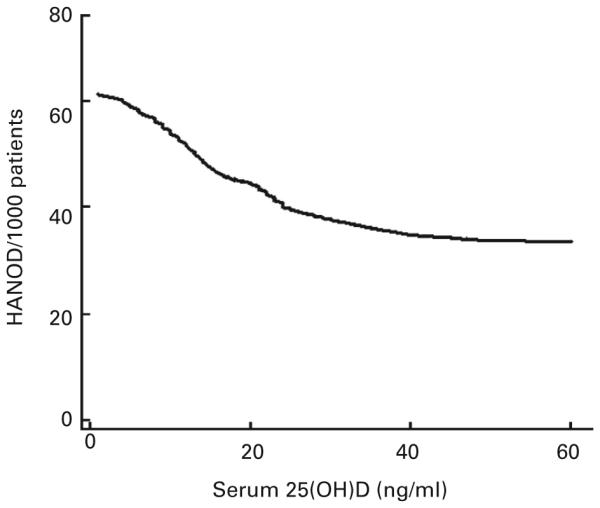
Vitamin D status v. the risk of hospital-acquired new-onset delirium. Locally weighted scatter plot smoothing utilised to represent the near inverse linear association between pre-hospital 25-hydroxyvitamin D (25(OH)D) level and the risk of hospital-acquired new-onset delirium(HANOD). Plot constructed with data from inpatients (n 4508) with pre-hospital vitamin D status excluding patients with existing history of delirium or dementia, and those with the diagnosis of delirium or dementia on admission.
In the study cohort (n 4508), the HANOD rate in patients with pre-hospital 25(OH)D , 10, 10–19·9, 20–29·9 or ≥ 30 ng/ml was determined to be approximately 69, 46, 37 and 31 per 1000 inpatients, respectively; the overall incidence was determined to be forty-four per 1000 inpatients. Finally, HANOD is associated with all-cause mortality (Fig. 2). When HANOD is considered as the exposure and all-cause mortality the outcome, HANOD is associated with 90 d mortality: OR for 90-d mortality in patients with HANOD 3·26 (95 % CI 2·27, 4·69) relative to those without HANOD adjusted for age, sex, race, patient type and Deyo–Charlson Index. When further adjusted for 25(OH)D status, the OR for 90-d mortality in patients with HANOD is 3·12 (95 % CI 2·17, 4·50) relative to those without HANOD adjusted for age, sex, race, patient type, Deyo–Charlson Index and 25(OH)D level.
Fig. 2.
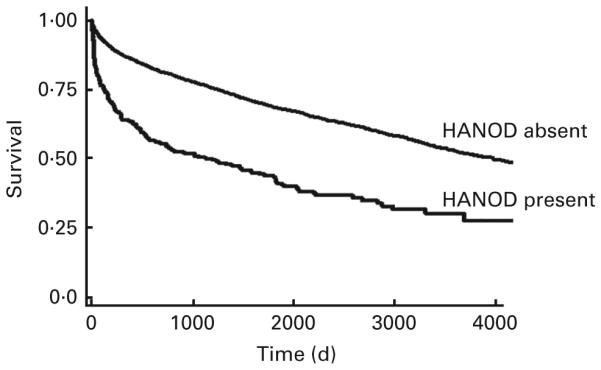
Time-to-event curves for the secondary end point (mortality). Unadjusted event rates were calculated with the use of Kaplan–Meier methods and compared with the use of the log-rank test. The global comparison log rank P value is , 0·0001 (n 4508).HANOD, hospital-acquired new-onset delirium. Vitamin D status and new-onset delirium.
Effect modification
Analyses based on fully adjusted models were performed to evaluate the 25(OH)D–HANOD association, and P for interaction was determined to explore for any evidence of effect modification. We individually tested for effect modification by creatinine, season of 25(OH)D draw, time between 25(OH)D draw and hospital admission or hospital of care by adding an interaction term to the multivariate models. None of these variables emerged as an effect modifier of the association between 25(OH)D and HANOD (P for interaction: HANOD . 0·20 for all variables tested).
Discussion
In the present study, we investigated whether vitamin D status before hospitalisation was associated with the risk of HANOD. We demonstrated that pre-hospital 25(OH)D < 10 ng/ml is indeed associated with a significant increase in the odds of delirium in patients during hospitalisation. While others have reported that vitamin D status may play an important protectiverole against various neuropsychiatric disorders(11–15), the present study presents important evidence to suggest that vitamin D supplementation may provide a novel approach to lowering HANOD risk. However, due to the observational nature of the present study, causal inference of the relationship between vitamin D status and delirium is limited.
The observed association between 25(OH)D and HANOD is biologically plausible. Purkinje cells as well as other neurons in the cerebral cortex and hippocampus (the primary cognitive centres in the human brain) express the vitamin D receptors(13). Binding of the 25(OH)D–vitamin D receptor complex to the nuclear vitamin D response element induces the synthesis of 1-a-hydroxylase(45), which is critical for the paracrine conversion of 25(OH)D to 1,25-dihydroxyvitamin D. As the most biologically active vitamin D metabolite in the central nervous system, 1,25-dihydroxyvitamin D upregulates hippocampal expression of neurotrophins(46). Neurotrophins are a family of proteins that are critical for regulating the survival, differentiation and maintenance of nerve cells(47). Brain-derived neurotrophic factor and nerve growth factor, two key members of the neurotrophin family, have both been shown to be directly associated with delirium following acute stress(48,49). In addition, vitamin D may contribute to neuro protection by modulating the production of glial cell-derived neurotrophic factor, NO synthase and choline acetyl transfer ase(13). Since it is evident that derangements in the cognitive pathways of the brain predispose patients to HANOD, and that vitamin D status is essential for both optimal nerve function and recovery following stress, the present findings raise a number of questions that merit further investigation.
The present study is not without potential limitations. Cohort studies may not provide the highest level of clinical evidence, but may direct future research by illustrating the existence or absence of a true effect(50). Observational studies may also be limited by confounding, reverse causation and/or the lack of a randomly distributed exposure. Since the patient cohort under the study had vitamin D status measurements related to an unknown reason (e.g. work-up for malnutrition, comprehensive immunological work-ups and monitoring for endocrine disorders), which may be absent in other hospitalised patients, ascertainment bias may exist in the present study. These differences may decrease the generalisability of the present results to all hospitalised patients. Despite adjustment for multiple potential confounders, there may still be residual confounding that contributed to the observed differences in outcomes. Specifically, low 25(OH)D levels may be a marker for the general condition of patients (i.e. the combined effect of nutritional status, functional mobility and chronic systemic diseases), for which we are unable to fully adjust.
A further potential limitation is related to the fact that we utilised 25(OH)D measurements between 7 and 365 d before hospitalisation as a reflection of pre-hospital vitamin D status. Others have shown that the intra-person Pearson correlation coefficient for 25(OH)D in outpatients following adjustments for age, race and season is 0·70 at 3 years between blood draws(51). In our cohort, there was no interaction of the 25(OH)D–HANOD association withregard to when 25(OH)D was obtained. Despite this observation, vitamin D status at the time of hospitalisation may be different than when prehospital values were drawn. Indeed, inflammatory changes, intravenous fluid administration and renal wasting may significantly contribute to rapid drops (approximately 30–40 %) in circulating 25(OH)D levels during acute stress(52). And although sunlight exposure, nutritional status (beyond the use of BMI), frailty/functional status and alcohol consumption are all potentially important confounders that may affect the 25(OH)D–HANOD relationship, given the limitations of our present electronicdatabase, we are unable to adjust for these covariates. These issues will need to be addressed byother groups as they try to replicate and extend our finding.
The present study has several strengths. We have sufficient statistical power to detect a clinically relevant difference in HANOD. We were able to control for several well-known risk factors for HANOD such as age, sex, recent surgery, use of antipsychotic medications, serious infections and a history of major depression. In addition, the Deyo–Charlson Index allowed us toaccount for chronic medical comorbidities. Moreover, by our design of measuring vitamin D status before hospitalisation, we attempted to uncouple the influence of illness and inflammation on 25(OH)D levels; we did not include 25(OH)D levels drawn in the 7 d before hospitalisation to avoid any potential alterations of vitamin D status related to acute illness or inflammation.
Conclusion
In conclusion, the present results suggest that pre-hospital vitamin D status may be a modifiable risk factor for HANOD. We hypothesise that serum 25(OH)D levels are associated with optimal expression of endogenous proteins involved with the maintenance of neuronal health in the areasof the central nervous system responsible for cognition. In turn, this may attenuate the effect of acute stressors that may increase the risk of HANOD. Prospective studies are needed to validateour findings, to assess the potential benefit of optimising pre-hospital 25(OH)D levels, and to identify the mechanism by which vitamin D may confer protection against neuropsychiatric disorderssuch as HANOD.
Acknowledgements
This manuscript is dedicated to the memory of our dear friend and colleague Nathan Edward Hellman, MD, PhD.
S. A. Q. was financially supported by the US National Institutes of Health 5T32GM007592 andUL1 RR025758. C. A. C. was supported by the US National Institutes of Health R01 AI093723 and U01AI087881. K. B. C. was supported by the US National Institutes of Health K08AI060881.
Abbreviations
- 25(OH)D
25-hydroxyvitamin D
- HANOD
hospital-acquired new-onset delirium
- RPDR
Research Patient Data Registry
Footnotes
The authors declare that there are no conflicts of interest.
The authors’ contributions are as follows: S. A. Q. and K. B. C. jointly conceived the study as well as designed and implemented the analysis with assistance from C. A. C.; K. B. C. and K. M. E. assembled the input data, wrote the code, ran the model and analysed the output data; S. A. Q.,C. A. C. and K. B. C. wrote the manuscript; S. A. Q., A. A. L., K.M. E., F. K. G., E. G., C. A. C. and K. B. C. edited the manuscript and provided conceptual advice.
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th American Psychiatric Association; Washington, DC: 2006. [Google Scholar]
- 2.Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35:350–364. doi: 10.1093/ageing/afl005. [DOI] [PubMed] [Google Scholar]
- 3.Reston JT, Schoelles KM. In-facility delirium prevention programs as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158:375–380. doi: 10.7326/0003-4819-158-5-201303051-00003. [DOI] [PubMed] [Google Scholar]
- 4.Inouye SK, Viscoli CM, Horwitz RI, et al. A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Intern Med. 1993;119:474–481. doi: 10.7326/0003-4819-119-6-199309150-00005. [DOI] [PubMed] [Google Scholar]
- 5.Marcantonio ER, Goldman L, Mangione CM, et al. JAMA. 271:134–139. [PubMed] [Google Scholar]
- 6.Rudolph JL, Jones RN, Levkoff SE, et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation. 2009;119:229–236. doi: 10.1161/CIRCULATIONAHA.108.795260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCusker J, Cole M, Dendukuri N, et al. Delirium in older medical inpatients and subsequent cognitive and functional status: a prospective study. CMAJ. 2001;165:575–583. [PMC free article] [PubMed] [Google Scholar]
- 8.Leslie DL, Marcantonio ER, Zhang Y, et al. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168:27–32. doi: 10.1001/archinternmed.2007.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siddiqi N, House A. Delirium: an update on diagnosis, treatment and prevention. Clin Med. 2006;6:540–543. doi: 10.7861/clinmedicine.6-6-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalueff AV, Tuohimaa P. Neurosteroid hormone vitamin D and its utility in clinical nutrition. Curr Opin Clin Nutr Metab Care. 2007;10:12–19. doi: 10.1097/MCO.0b013e328010ca18. [DOI] [PubMed] [Google Scholar]
- 11.Buell JS, Dawson-Hughes B. Vitamin D and neurocognitive dysfunction: preventing “D”ecline? Mol Aspects Med. 2008;29:415–422. doi: 10.1016/j.mam.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Annweiler C, Allali G, Allain P, et al. Vitamin D and cognitive performance in adults: a systematic review. Eur J Neurol. 2009;16:1083–1089. doi: 10.1111/j.1468-1331.2009.02755.x. [DOI] [PubMed] [Google Scholar]
- 13.Balion C, Griffith LE, Strifler L, et al. Vitamin D, cognition, and dementia: a systematic review and meta-analysis. Neurology. 2012;79:1397–1405. doi: 10.1212/WNL.0b013e31826c197f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Annweiler C, Llewellyn DJ, Beauchet O. Low serum vitamin D concentrations in Alzheimer’s disease: a systematic review and meta-analysis. J Alzheimers Dis. 2013;33:659–674. doi: 10.3233/JAD-2012-121432. [DOI] [PubMed] [Google Scholar]
- 15.Anglin RE, Samaan Z, Walter SD, et al. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. Br J Psychiatry. 2013;202:100–107. doi: 10.1192/bjp.bp.111.106666. [DOI] [PubMed] [Google Scholar]
- 16.Kuriacose R, Olive KE. Prevalence of vitamin D deficiency and insufficiency in northeast Tennessee. South Med J. 2008;101:906–909. doi: 10.1097/SMJ.0b013e318181881b. [DOI] [PubMed] [Google Scholar]
- 17.Pellicane AJ, Wysocki NM, Schnitzer TJ. Prevalence of 25-hydroxyvitamin D deficiency in the outpatient rehabilitation population. Am J Phys Med Rehabil. 2010;89:899–904. doi: 10.1097/PHM.0b013e3181f71112. [DOI] [PubMed] [Google Scholar]
- 18.Fish E, Beverstein G, Olson D, et al. Vitamin D status of morbidly obese bariatric surgery patients. J Surg Res. 2010;164:198–202. doi: 10.1016/j.jss.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 19.Bogunovic L, Kim AD, Beamer BS, et al. Hypovitaminosis D in patients scheduled to undergo orthopaedic surgery: a single-center analysis. J Bone Joint Surg Am. 2010;92:2300–2304. doi: 10.2106/JBJS.I.01231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ginde AA, Liu MC, Camargo CA, et al. Demographic differences and trends of vitamin D insufficiency in the US population, 1988–2004. Arch Intern Med. 2009;169:626–632. doi: 10.1001/archinternmed.2008.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Braun A, Chang D, Mahadevappa K, et al. Association of low serum 25-hydroxyvitamin D levels and mortality in the critically ill. Crit Care Med. 2011;39:671–677. doi: 10.1097/CCM.0b013e318206ccdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hivert MF, Grant RW, Shrader P, et al. Identifying primary care patients at risk for future diabetes and cardiovascular disease using electronic health records. BMC Health Serv Res. 2009;9:170. doi: 10.1186/1472-6963-9-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hug BL, Lipsitz SR, Seger DL, et al. Mortality and drug exposure in a 5-year cohort of patients with chronic liver disease. Swiss Med Wkly. 2009;139:737–746. doi: 10.4414/smw.2009.12686. [DOI] [PubMed] [Google Scholar]
- 24.Linder JA, Bates DW, Williams DH, et al. Acute infections in primary care: accuracy of electronic diagnoses and electronic antibiotic prescribing. J Am Med Inform Assoc. 2006;13:61–66. doi: 10.1197/jamia.M1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zager S, Mendu ML, Chang D, et al. Neighborhood poverty rate and mortality in patients receiving critical care in the academic medical center setting. Chest. 2011;139:1368–1379. doi: 10.1378/chest.10-2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 27.Hollis BW, Kamerud JQ, Selvaag SR, et al. Determination of vitamin D status by radioimmunoassay with an 125I-labeled tracer. Clin Chem. 1993;39:529–533. [PubMed] [Google Scholar]
- 28.Inouye SK, Leo-Summers L, Zhang Y, et al. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. 2005;53:312–318. doi: 10.1111/j.1532-5415.2005.53120.x. [DOI] [PubMed] [Google Scholar]
- 29.Swan JT, Fitousis K, Hall JB, et al. Antipsychotic use and diagnosis of delirium in the intensive care unit. Crit Care. 2012;16:R84. doi: 10.1186/cc11342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 31.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–682. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 32.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 33.Rapoport J, Gehlbach S, Lemeshow S, et al. Resource utilization among intensive care patients. Managed care vs traditional insurance. Arch Intern Med. 1992;152:2207–2212. [PubMed] [Google Scholar]
- 34.Glasgow RE, Showstack JA, Katz PP, et al. The relationship between hospital volume and outcomes of hepatic resection for hepatocellular carcinoma. Arch Surg. 1999;134:30–35. doi: 10.1001/archsurg.134.1.30. [DOI] [PubMed] [Google Scholar]
- 35.Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. New Engl J Med. 2003;348:1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 36.Moromizato T, Litonjua AA, Braun AB, et al. Association of low serum 25-hydroxyvitamin d levels and sepsis in the critically ill. Crit Care Med. 2014;42:97–107. doi: 10.1097/CCM.0b013e31829eb7af. [DOI] [PubMed] [Google Scholar]
- 37.Busch SH. Specialty health care, treatment patterns, and quality: the impact of a mental health carve-out on care for depression. Health Serv Res. 2002;37:1583–1601. doi: 10.1111/1475-6773.11092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cowper DC, Kubal JD, Maynard C, et al. A primer and comparative review of major US mortality databases. Ann Epidemiol. 2002;12:462–468. doi: 10.1016/s1047-2797(01)00285-x. [DOI] [PubMed] [Google Scholar]
- 39.Sohn MW, Arnold N, Maynard C, et al. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr. 2006;4:2. doi: 10.1186/1478-7954-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schisterman EF, Whitcomb BW. Use of the Social Security Administration Death Master File for ascertainment of mortality status. Popul Health Metr. 2004;2:2. doi: 10.1186/1478-7954-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Newman TB, Brown AN. Use of commercial record linkage software and vital statistics to identify patient deaths. J Am Med Inform Assoc. 1997;4:233–237. doi: 10.1136/jamia.1997.0040233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–495. doi: 10.1097/EDE.0b013e3181a819a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cleveland W. Robust locally weighted regression and smoothing scatterplots. J Am Stat Assoc. 1979;74:829–836. [Google Scholar]
- 44.Cleveland W, Devlin S. Locally-weighted regression: an approach to regression analysis by local fitting. J Am Stat Assoc. 1988;83:596–610. [Google Scholar]
- 45.Zehnder D, Bland R, Williams MC, et al. Extrarenal expression of 25-hydroxyvitamin D(3)–1α-hydroxylase. J Clin Endocrinol Metab. 2001;86:888–894. doi: 10.1210/jcem.86.2.7220. [DOI] [PubMed] [Google Scholar]
- 46.McCann JC, Ames BN. Is there convincing biological or behavioral evidence linking vitamin D deficiency to brain dysfunction? FASEB J. 2008;22:982–1001. doi: 10.1096/fj.07-9326rev. [DOI] [PubMed] [Google Scholar]
- 47.Glade MJ. A 21st century evaluation of the safety of oral vitamin D. Nutrition. 2012;28:344–356. doi: 10.1016/j.nut.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 48.Grandi C, Tomasi CD, Fernandes K, et al. Brain-derived neurotrophic factor and neuron-specific enolase, but not S100β, levels are associated to the occurrence of delirium in intensive care unit patients. J Crit Care. 2011;26:133–137. doi: 10.1016/j.jcrc.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 49.Jockers-Scherubl MC, Bauer A, Kuhn S, et al. Nerve growth factor in serum is a marker of the stage of alcohol disease. Neurosci Lett. 2007;419:78–82. doi: 10.1016/j.neulet.2007.03.051. [DOI] [PubMed] [Google Scholar]
- 50.Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. New Engl J Med. 2000;342:1887–1892. doi: 10.1056/NEJM200006223422507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Platz EA, Leitzmann MF, Hollis BW, et al. Plasma 1,25-dihydroxy- and 25-hydroxyvitamin D and subsequent risk of prostate cancer. Cancer Causes Control. 2004;15:255–265. doi: 10.1023/B:CACO.0000024245.24880.8a. [DOI] [PubMed] [Google Scholar]
- 52.Quraishi SA, Camargo CA., Jr Vitamin D in acute stress and critical illness. Curr Opin Clin Nutr Metab Care. 2012;15:625–634. doi: 10.1097/MCO.0b013e328358fc2b. [DOI] [PMC free article] [PubMed] [Google Scholar]


