Abstract
Objective
Hazardous alcohol use by HIV-infected women is associated with poor HIV outcomes and HIV transmission risk behaviors. We examined the effectiveness of brief alcohol intervention (BI) among hazardous drinking women receiving care in an urban, HIV clinic.
Methods
Women were randomized to a 2-session BI or usual care. Outcomes assessed at baseline, 3, 6 and 12 months included 90-day frequency of any alcohol use and heavy/binge drinking (≥4 drinks per occasion), and average drinks per drinking episode. Secondary outcomes included HIV medication and appointment adherence, HIV1-RNA suppression, and days of unprotected vaginal sex. We examined intervention effectiveness using generalized mixed effect models and quantile regression.
Results
Of 148 eligible women, 74 were randomized to each arm. In mixed effects models, 90-day drinking frequency decreased among intervention group compared to control, with women in the intervention condition less likely to have a drinking day (OR: 0.42 (95% CI: 0.23–0.75). Heavy/binge drinking days and drinks per drinking day did not differ significantly between groups. Quantile regression demonstrated a decrease in drinking frequency in the middle to upper ranges of the distribution of drinking days and heavy/binge drinking days that differed significantly between intervention and control conditions. At follow-up, the intervention group had significantly fewer episodes of unprotected vaginal sex. No intervention effects were observed for other outcomes.
Conclusions
Brief alcohol intervention reduces frequency of alcohol use and unprotected vaginal sex among HIV-infected women. More intensive services may be needed to lower drinks per drinking day and enhance care for more severely affected drinkers.
Keywords: Brief Alcohol Intervention, Women, HIV, Alcohol, Randomized Controlled Trial
Introduction
Alcohol use is prevalent among women with HIV. Among 2,770 HIV infected women followed over 11 years in the Women’s Interagency HIV Study (WIHS), 14%–24% reported past-year hazardous alcohol consumption. 1 Hazardous alcohol use has consistently been associated with decreased antiretroviral therapy adherence,2 increased sexual risk behaviors3;4 and mortality.5;6 Finally, with nearly 1/3 of HIV infected individuals in the United States co-infected with Hepatitis C, reduction in alcohol use is an essential component to reducing liver related morbidity and mortality among HIV and Hepatitis C co-infected individuals. Given the deleterious relationship between hazardous alcohol use, HIV outcomes and transmission risk behaviors, addressing alcohol use in HIV clinical settings is essential to optimize care.
The delivery of alcohol interventions in HIV primary care settings may be especially important for women. Women are particularly vulnerable to the effects of alcohol use, with greater than one drink per day placing women at risk for negative health consequences.7 In addition, women may be less likely to seek and or engage in alcohol treatment services.8;9 Thus identifying hazardous alcohol use and intervening in primary care HIV settings is an essential component in reducing alcohol related harms in women.
Alcohol screening and brief intervention can significantly impact drinking levels in health care settings.10 Project TREAT, a two-session brief alcohol intervention delivered in primary care offices, significantly reduced weekly alcohol consumption and binge drinking among women of child bearing age.11 Among HIV infected individuals, interventions for alcohol use have varied in intensity and content (alcohol only versus alcohol plus drugs or alcohol plus sex), have included mostly men, and have had mixed results.12;13 In a recent trial in an urban HIV clinic, an alcohol-focused motivational interviewing intervention augmented with alcohol self-monitoring questions delivered through an interactive voice response system reduced drinks per drinking day in the intervention compared with control condition.14 Results were not stratified by sex (22% of the sample were women), thus the efficacy of brief alcohol intervention among HIV-infected women remains unknown.
Given the lower drinking threshold for risk of alcohol-related problems among women compared with men, and the negative impact of hazardous alcohol use on HIV treatment outcomes, testing brief intervention effectiveness among HIV infected women is essential to optimizing their health outcomes. In a randomized controlled trial, we examined the effectiveness of a brief alcohol intervention among hazardous drinking women receiving care in the Johns Hopkins HIV Clinic.
MEHODS
Trial Design
We performed a two arm randomized trial of a brief alcohol intervention versus usual care among HIV infected, hazardous drinking women receiving care in an urban HIV clinic.
Setting and Participants
Participants were recruited between April 2006 and July 2010 from the Johns Hopkins HIV Clinic located in Baltimore, MD. Participants were identified through several methods: clinic flyers advertising a woman’s health study, provider referral, waiting room recruitment and review of drinking data obtained from an audio-computer-assisted self-interview (ACASI) routinely administered to clinic patients at six month intervals. Women were eligible for participation if they were receiving care in the Johns Hopkins HIV Clinic, 18 years old or greater, and either consumed alcohol at hazardous levels or had a current TWEAK score of ≥2.15 We defined hazardous drinking as an average of 8 or more drinks per week or two or more heavy drinking episodes (defined as 4 or more drinks/occasion) in the past 6 months. The rationale for using a low drinking threshold for study enrollment was to optimize the sensitivity of screening. We excluded women if they were actively psychotic, currently enrolled in alcohol treatment, or pregnant. The Johns Hopkins Institutional Review Board approved this study and this study was registered at clinicaltrials.gov: NCT00127231
Randomization
Our randomization sequence was generated using SAS by an independent investigator. Randomization was stratified by the presence or absence of active illegal drug use in blocks of six. Sealed envelopes were used to conceal allocation. Outcome assessors, data analysts and investigators were blinded to participant group assignment. The intervention counselor and patients were not blinded to study condition.
Intervention
The brief alcohol intervention consisted of two 20 minute face to face sessions conducted approximately one month apart with a master’s level counselor; each session was followed by a 5–10 minute booster phone call. With permission, the session content was based on the brief intervention developed by Fleming and colleagues for Project TrEAT, the Trial for Early Alcohol Treatment.16 The intervention was adapted for HIV infected women and included content related to alcohol’s role in HIV medication adherence, HIV transmission risk behaviors and Hepatitis C co-infection.
The first session of the intervention, scheduled as soon as possible after completion of baseline assessments, included 1) patient general health assessment and feedback, and 2) goal setting and contracting. The therapist used a scripted workbook that reviewed general health habits, the prevalence of problem drinking in the United States, adverse effects of alcohol, and reasons to either quit or reduce alcohol consumption. Personalized feedback was provided using drinking data derived from the baseline TimeLine FollowBack.17 At the conclusion of the first session, the participant was given the workbook, drinking diary cards to chart daily alcohol use between sessions, and take home exercises. She was encouraged, though not required, to set a drinking limit with the counselor. Following the first session, women in the intervention group received a scripted booster telephone call from the counselor reinforcing intervention content and reminding them of their second session appointment.
During the second session, the counelor reviewed the drinking diary cards, drinking agreement, and the take home exercises with the participant. If relevant, women reviewed barriers and facilitators to changes in alcohol use since the previous session, and identified individuals who supported their behavior change. Women in the intervention group were contacted by the therapist within 2 – 3 weeks following the second session for a second booster call.
Usual Care
Hazardous drinking women randomized to the usual care condition received the standard care offered by the clinic. This included access to primary care providers, mental health services and social work.
Intervention fidelity
Intervention sessions were audio-taped; 10% of the sessions were randomly selected and reviewed for intervention fidelity by a study co-investigator (HH). We adapted fidelity checklists developed for Project TrEAT, and the Healthy Moms Study18 with the purpose of ensuring that the intervention delivered all of the intended components.
Assessment Visits
Participants underwent assessments at baseline and 3, 6 and 12 months and received $20 at the time of each research interview to compensate for their time and travel. Those completing all four research interviews received a $50 bonus at the end of the trial.
Outcomes
Our main outcomes included number of drinking days and number of heavy/binge drinking days over a 90 day period; and average standard drinks per drinking day. We used the 90-day Time Line Follow Back (TLFB) method to ascertain drinking outcomes.17 Secondary outcomes included change in aspartate aminotransferase (AST) and alanine aminotransferase (ALT), drawn at the time of assessment visits; HIV outcomes, including use of antiretroviral therapy (ART), ART adherence, viral suppression, HIV clinic appointment adherence; and episodes of unprotected vaginal sex. Use of ART was obtained by self-report using an Audio-Computer Assisted Self-Interview (ACASI). ART adherence, assessed using pharmacy refill records, was defined as the ratio of number of months the patient refilled their ART over the twelve months enrolled in the study. Viral suppression, defined as an HIV-1 RNA <50, was obtained through laboratory files and drawn at baseline and follow-up visits. Appointment adherence was obtained through clinic registration records, which capture scheduled visits, completed visits, missed visits. Days of unprotected vaginal sex were assessed using a 90 day TLFB.
Independent Variables
Illegal drug was obtained using the 90 day TLFB. Alcohol use severity was assessed using the Alcohol Use Disorders Identification Test (AUDIT)19 at baseline. In addition, 10% of enrolled women completed the alcohol abuse/dependence module of the Structured Clinical Interview for DSM Disorders (SCID) DSM-420. Age, race, income, housing status, education were obtained via ACASI interview using questions from the Addiction Severity Index.21
Statistical Methods
This is a longitudinal analysis of data collected during baseline and three follow-up visits. We first summarized baseline characteristics, including demographics, drinking measures, socioeconomic measures, HIV related biomarkers, unprotected vaginal sex episodes and illicit drug use. Continuous variables were shown as arithmetic mean and standard deviation. For skewed variables, log-transformation was performed. We checked the balance between study arms using the absolute difference in means standardized by the deviation between treatment arms using propensity score analysis. 22;23 Propensity scores suggested that randomization resulted in balance for the majority of measured potential confounders. However, age, race, and days of illegal drug use had a greater than 0.2 absolute difference in standardized means. Analyses including these potential confounders as covariates did not change inferences from the models described below.
To test the overall intervention effect on number of drinking days and number of heavy/binge drinking days we used a generalized binomial mixed effect model with the logit link function and a random intercept. The use of a binomial distribution was indicated for this analysis because the outcome was assessed using a 90-day TLFB Interview, which has a cap at 90 days. Number of drinks per drinking day was modeled using generalized Poisson mixed effect model with log link function. For each of our drinking outcomes, we also tested whether the intervention effect on alcohol outcomes was modified by baseline severity of alcohol use using a dichotomized AUDIT cut-off score at ≥7.
Given that a mixed effect model assesses a shift in the mean on the transformed scale (i.e., logit scale), it is possible that the expectation is not sensitive enough to detect a shift in the distribution between control and intervention arms. Therefore quantile regression was used to assess where the shifts in the distribution were located to better describe the overall difference in drinking behaviors between control and intervention arms.24 Specifically we used a linear quantile mixed model to account for repeated measures on individuals with a random intercept using the R package lqmm.25–27 Given that outcome data for number of drinking days and number of heavy drinking days are both discrete and bounded between 0 and 90, we applied a smooth transformation that jittered the discrete data and transformed it to a logit scale.28;29 For number of drinks per drinking day which is bounded only by 0, the logit transformation was replaced by a log transformation. For these models, visit was not included as we had observed comparable drinking levels across the three follow-up visits and in the mixed-effect model. Pointwise 95% confidence intervals were calculated by bootstrap and results were transformed back into the original scale for increased ease of interpretation. Results were smoothed across the quantiles using locally weighted scatterplot smoother.
To test the intervention effect on AST, ALT, and HIV viral load over the follow up period, we constructed a mixed effect model, with intervention group, baseline measure, and their interaction as covariates. Due to the skewness of viral load, it was log transformed. Clinic appointment adherence was modeled as a repeated dichotomous outcome with each scheduled visit categorized as either completed or missed. A logistic mixed effect model with random intercept was constructed to test intervention effect and the baseline measure was added to the model. ART adherence was calculated using the medication possession ratio (MPR), defined as the ratio of the number of months the patient was on ART over 12 month period following the baseline visit, excluding any period when the patient was in a controlled environment. The ratio was compared between the intervention group and the control group using two-group t-test. Finally, for our outcome of days of unprotected vaginal sex, we used generalized mixed effect regression models for binomial distribution with random intercept and slope. Study group condition and baseline measure were included as covariates in the model. We also ran a sensitivity analysis by limiting the sample to those women who were sexually active.
This study was powered to detect a difference in alcohol consumption between intervention and control conditions. Original power calculations were based on data from Manwell and colleagues11 and indicated that 78 women in each arm would allow for 80% power to detect a 28% difference in reduction in weekly alcohol use between intervention and control conditions. We targeted recruitment of 200 women to allow for study exclusions and drop-out prior to randomization.
Results
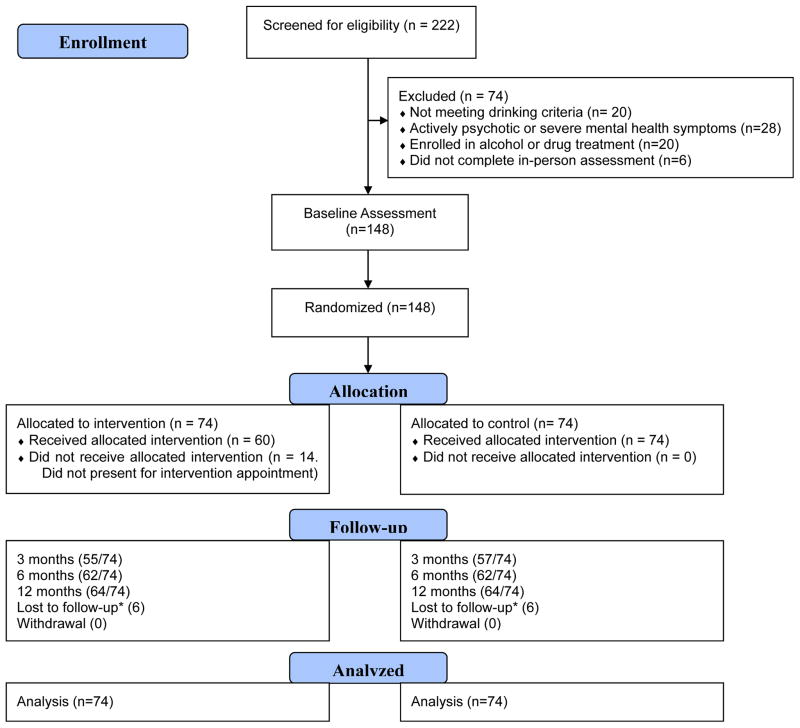
A total of 222 women were screened for eligibility, 148 were eligible and 74 participants were randomized to each arm (Figure 1). Of those randomized to the intervention arm, 14 (18.9%) did not receive the allocated treatment as they did not return for the intervention, 11 (14.9%) attended 1 counseling session, and 49 (66%) attended both in-person counseling sessions and. There were 6 individuals in each arm who were lost to follow-up, which we defined as missing all three follow-up visits at 3, 6, and 12 months. Baseline characteristics of the sample are presented in Table 1. There was no significant difference in audit score, total number of drinking days, drinks per drinking day, and heavy drinking days between the intervention and control arms. At baseline, the typical drinking episode was a binge drinking episode; that is, 80.1% of drinking days were heavy/binge drinking days. Less than 1% of drinking days were days when women consumed only 1 drink. Mean AUDIT scores in both groups were above the clinical cut-off, suggesting a high probability of alcohol related problems in these women. In addition, among the subsample of our study participants in whom we obtained an alcohol diagnosis, 55% had a diagnosis of DSM-IV lifetime alcohol dependence and 10% had subthreshold symptoms.
Figure 1.
Consort Diagram
* Lost to Follow-Up defined as missing all the 3, 6, and 12 month visits.
Table 1.
Baseline characteristics of 148 women in study sample
| Variable | Control (N=74) | Intervention (N=74) | P value3 |
|---|---|---|---|
|
| |||
| Age (Mean, SD) | 44.86 (9.1) | 46.27 (7.07) | 0.196a |
|
| |||
| Race | |||
| African-American/Black | 60 (81.1%) | 67 (90.5%) | 0.099 |
| White and American Indian | 14 (18.9%) | 7 (9.5%) | |
|
| |||
| Employment | |||
| Working part-time or full-time or looking for work | 21 (28.4%) | 28 (37.8%) | 0.222 |
| Working full-time | 53 (71.6%) | 46 (62.2%) | |
|
| |||
| Income ($)(Mean, SD) | 8189.19 (7239.17), N = 73 | 8497.38 (7166.03) | 0.674c |
|
| |||
| HIV1-RNA (copies) (Mean, SD) | 11100.64 (23126.07) | 20851.32 (45884.05), N = 73 | 0.627c |
|
| |||
| Undetectable HIV1-RNA (<50 copies) | 31 (41.9%) | 29 (40.3%) | 0.799 |
|
| |||
| CD4 count (cells/mm) (Mean, SD) | 393.24 (236.78) | 398.11 (269.02) | 0.907a |
|
| |||
| AST (Mean, SD) | 44.80 (34.3) | 44.71 (42.73), N = 73(2) | 0.653b |
|
| |||
| ALT (Mean, SD) | 34.89 (31.08) | 31.14 (24.43), | 0.840b |
|
| |||
| AUDIT Score (Mean, SD) | 12.3 (8.9) | 11.9 (8.7) | 0.827c |
|
| |||
| Total number of drinking days (90day) (Mean, SD) | 30.45 (27.57) | 34.03 (29.47) | 0.525c |
|
| |||
| Total number binge drinking days (90day) (Mean, SD) | 26.71 (28.55) | 24.91 (26.99) | 0.701c |
|
| |||
| # of Drinks per episode(Mean, SD) | 9.55 (6.42) | 9.69 (9.13) | 0.393b |
|
| |||
| Illicit drug use in past 6 months1 | |||
| No | 22 (29.7%) | 24 (32.4%) | 0.722 |
| Yes | 52 (70.3%) | 50 (67.6%) | |
|
| |||
| Injection drug use in past 6 months | |||
| No | 66 (89.2%) | 65 (87.8%) | 0.797 |
| Yes | 8 (10.8%) | 9 (12.2%) | |
|
| |||
| On Antiretroviral Therapy | |||
| No | 24 (32.4%) | 20 (27.0%) | 0.472 |
| Yes | 50 (67.6%) | 54 (73.0%) | |
|
| |||
| Total number of days of unprotected vaginal sex (90 day) (Mean, SD) | 3.23 (9.01) | 2.66 (8.46) | 0.048c |
|
| |||
| HCV | |||
| No | 30 (40.5%) | 36 (48.7%) | 0.321 |
| Yes | 44 (59.5%) | 38 (51.4%) | |
|
| |||
| HAD depression score | 5.78 (4.36) | 6.20 (3.51) | 0.521 |
Marijuana use included
Baseline AST missing in one participant; ALT data available.
a: t-test; b: t-test on log transformed value; c: Wilcoxon test
Effect of Brief Intervention on 90-day Drinking Frequency, Heavy Drinking Days and Drinks per Drinking Day, Generalized Mixed Effect Model
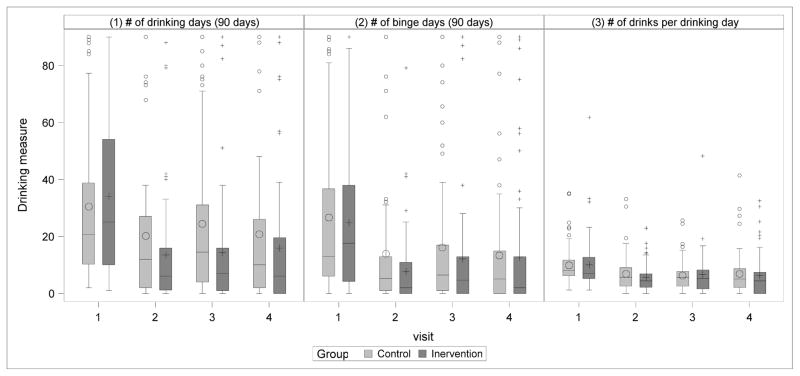
Figure 2 displays the change in alcohol use by intervention and control condition. In mixed effects models (Table 2), 90-day drinking frequency decreased among intervention group compared to control, with women in the intervention condition significantly less likely to have a drinking day (OR: 0.42 (95% CI: 0.23–0.75) (p=0.005). However, neither 90-day frequency of heavy/binge drinking nor number of drinks per drinking day was significantly different between intervention and control groups. There was also no significant difference between study arms in the change in AST or ALT at follow-up. Finally, there was no significant interaction between AUDIT score (as a marker of drinking severity) and the intervention on drinking outcomes.
Figure 2.
Frequency of a) of drinking days ) binge drinking days and c) number of drinks per drinking day by intervention and control conditions at baseline and 3, 6 and 12 month follow-up. The 0 and + symbols indicate the mean of the outcome in the control and intervention conditions, respectively. The horizontal short lines in the boxes are the medians. In panel 1, at baseline, mean drinking days in the intervention group was 34 days. At follow-up, the mean was 14–16 drinking days (depending on visit). Thus drinking days were reduced by 52–59% in the intervention group. The baseline mean drinking days for the control group was 30 and reduced to 20–24 drinking days at follow-up, a reduction of 20–33%. In panel 2, heavy drinking days, the baseline mean in the intervention group was 25, and was reduced to 8 to 13 drinks at follow-up, a 48–68% reduction. In the control group the mean at baseline was 27, and was reduced to 13 to 16 heavy drinking days at follow-up, a reduction between 41–52%. In panel 3, the mean drinks per drinking day at baseline was 10 in both groups, and reduced to 6–7 in both groups, a reduction of 30–40%.
Table 2.
Brief Intervention Effect on Drinking Days, Binge Drinking Days and Drinks Per Drinking Day
| (1) Outcome | Distribution | Comparison | Intervention/Control (95% CI) | P-Value |
|---|---|---|---|---|
| # of drinking days (90 days) | Binomial | Odds ratio | 0.416 (0.230, 0.752) | 0.005 |
| # of binge days (90 days) | Binomial | Odds ratio | 0.603 (0.236, 1.542) | 0.293 |
| # of drinks per drinking day | Poisson | Relative risk | 0.921 (0.684, 1.239) | 0.586 |
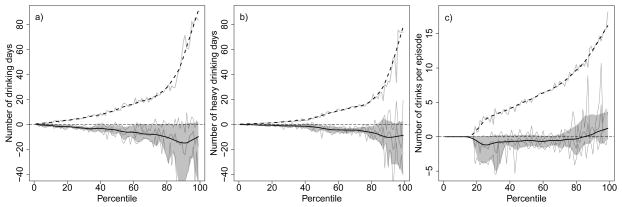
Effect of Brief Intervention on 90-day Drinking Frequency, Heavy Drinking Days and Drinks per Drinking Day, Quantile Regression
Figure 3A displays the results of the quantile regression model for 90-day drinking frequency. The quantile regression shows that the number of drinking days was significantly lower in the intervention compared with control group between the 28th – 90th percentiles of the distribution of drinking days. For example, at the 50th percentile of drinking days, 90-day drinking frequency in the intervention group was 4.6 [95% CI: 0.9, 7.1] drinking days lower than for the control group (estimated at 12 drinking days), a reduction of approximately 39%. These data demonstrate a statistically significant shift that favors the intervention group in the frequency of drinking days that occurs in the middle of the distribution, but not the tails, which is congruent with generalized mixed model results.
Figure 3.
Quantile Regression is used to estimate the treatment effects across a range of the distribution (i.e., quantile such as 10, 25, 50 [median], 75, and 90th percentiles) of the outcomes. For a given percentile (horizontal axis), the vertical axis represents the A) number of drinking days, B) number of heavy/binge drinking days, and C) number of drinks per drinking day. The solid black line represents the treatment effect difference between the control and intervention arms (95% CI represented by gray shaded area). For reference the dashed long line shows the value of the outcome among the controls for a given percentile. For example, at the 80th percentile panel A shows that the 80% of the controls were below 30 drinking days, whereas the intervention effect is 10 drinks less and therefore the 80% of the intervention group were below 20 drinking days. The light grey lines represent the actual estimated values from the quantile regression to which a non-parametric smoother was applied to provide guidance for interpretation.
Figure 3B displays similar results for the number of heavy drinking days. There was a significant difference in the distribution of heavy drinking days in the intervention compared to the control group. Specifically between the 10th–95th percentiles of the distribution, the intervention group had significantly fewer binge days compared with control subjects. For example, the difference at the 50th percentile of heavy/binge drinking days between control and intervention groups was 2.9 [95% CI: 0.8, 4.4]. That is at the 50th percentile the intervention group was nearly 3 heavy drinking days lower than the control group which had 7 heavy drinking days (43% reduction).
There were no significant differences in the distribution of number of drinks per drinking day at each quantile. However, the point estimate of the intervention effect appears to be consistently lower and the confidence interval just includes 0 (Figure 3C).
Unprotected Vaginal Sex
Brief alcohol intervention was significantly associated with a reduction in days of unprotected vaginal sex. After adjustment for baseline number of days of unprotected sex, the intervention group showed a 61.4% reduction in the odds of having unprotected vaginal sex compared with the usual care group (AOR=0.386 with 95% CI (0.156, 0.952), P=0.041). When we restricted the analysis to participants who were sexually active, the intervention showed 60.3% reduction in the odds of having an unprotected vaginal sex on any given day during the follow-up period. The association was marginally significant (AOR= 0.397 with 95% CI (0.153, 1.028), P=0.055).
HIV Outcomes: ART use and adherence, viral suppression, and appointment adherence
Self-reported use of antiretroviral therapy did not differ between intervention and control groups. In addition, neither antiretroviral adherence, (intervention [mean MPR: 0.53, SE: 0.045] and control [mean MPR: 0.58 SE: 0.042] (p=.40) ) nor viral suppression differed between intervention and control across follow-up visits (Odds Ratio: 1.30 95% CI: 0.65–2.61). Finally, appointment adherence (defined as the number of completed visits over total number of scheduled visits) did not differ between study conditions (OR: 1.11 95% CI: (0.853, 1.447) (p=.43)).
Discussion
In hazardous drinking HIV infected women, brief alcohol intervention led to an overall greater reduction in drinking days compared with usual care. Our study yields two important new findings of high relevance to brief alcohol interventions among women in HIV care. First, brief intervention is efficacious in reducing alcohol use across a wide range of self-reported frequency of any and heavy/binge consumption (as reflected by the quantile regression). Secondly, brief intervention can be efficacious among HIV-infected women who are low income and underserved.
Our overall finding of reduced drinking frequency is similar to findings from the Healthy Moms Study18, in which brief alcohol intervention in post-partum women reduced their overall number of drinking days by 33% compared to 12% in controls. Our reduction in drinking days was greater than the Healthy Moms Study, which may be explained by differences in age, (women in our trial were older), or medical comorbidity (presence of HIV, Hepatitis C). In line with other brief alcohol intervention studies, we observed an overall reduction from baseline in drinking frequency in both intervention and control groups. Possible explanations for this finding include assessment reactivity and regression to the mean.30;31 Despite drinking reductions in both groups, the intervention condition significantly decreased frequency of drinking compared to the control condition.
In addition to examining mean treatment effects, we had the opportunity to examine whether differences in drinking behaviors between the intervention and control groups were located over the entirety of their distribution (i.e. a shift in distribution), or only in the low, mid, or high levels of the distribution. Quantile regression analyses of number of drinking days and heavy/binge drinking days demonstrated a decrease in drinking frequency located in the middle to upper ranges of the distribution. By contrast intervention women in the lowest and highest range of drinking frequency did not differ from control women. Lack of an intervention effect in the lowest range of drinking frequency may be due to the small number of subjects in this range or to a floor effect in that there was less room for change among women who drank less frequently. These women may have been less likely to experience drinking-related problems, and therefore were less likely to perceive the need for change. Among intervention women in the highest 10% of the distribution, more intensive intervention may be required to reduce alcohol consumption. In a recent study of HIV-infected patients, Hasin et al. compared MI plus HealthCall (HC) (daily alcohol self-monitoring questions delivered via interactive voice response system) to motivational interviewing (MI) only or advice/education.14 At end of treatment, the MI + HC group significantly reduced their drinks per drinking day compared to control; importantly, a significant treatment effect was observed only among the alcohol-dependent participants. Results suggest that more intensive interventions can be effective in individuals with more severe alcohol use disorder. To reduce alcohol use in more severely impaired patients, it may be necessary to add intervention extenders such as HealthCall, text messaging or other M-Health modalities and/or pharmacotherapy to brief alcohol interventions. Several studies have now demonstrated pharmacotherapy to be effective in reducing heavy drinking days among individuals with alcohol use disorders.32–34 A recent systematic review demonstrated that both naltrexone and acamprosate reduce percent of drinking days and naltrexone also reduces percent of heavy drinking days.32
At baseline in our sample, the typical drinking episode was a binge drinking episode. Thus, the findings of significant reductions in the frequency of drinking and particularly the frequency of heavy drinking in the quantile regression have important clinical implications. Heavy/binge drinking has short- and long-term deleterious effects, including injury, driving accidents, risky sexual behaviors, and alcohol poisoning, particularly among women. Among HIV-infected women, heavy drinking has been associated with decreased antiretroviral therapy adherence,2 increased sexual risk behaviors3;4 and mortality.5;6 Clearly, a reduction in heavy drinking frequency can provide clinical benefit to this high-risk population.
Indeed, we observed an effect of brief alcohol intervention on days of unprotected vaginal sex. To date few studies have examined whether an alcohol-focused intervention can reduce risky sexual behaviors among HIV-infected persons in general, and among HIV infected women in particular.13 Velasquez and colleagues studied a combined 8-session alcohol and sexual risk reduction intervention among hazardous drinking men who have sex with men.35 Intervention compared to control participants had an overall reduction in alcohol use, and, among those at baseline who had sex and consumed alcohol on the same day, a decreased number of days of drinking and unprotected sex. Our finding that a two-session brief alcohol intervention was associated with decreased days of unprotected vaginal sex has implications for reducing HIV transmission risk.
We did not find any effect of brief alcohol intervention on HIV medication adherence, viral suppression or appointment adherence. Reduction in drinking frequency may be inadequate to improve HIV treatment outcomes, and a reduction in drinking quantity is also needed. Among United States veterans, Braithewaite et al found that over a 30 day period, binge drinking episodes were associated with a significantly higher percentage of missed medication doses (14%) compared with non-binge (6%) and non-drinking days (4%).36 It is possible that interventions that specifically reduce drinks per drinking day may be more likely to improve HIV treatment outcomes. To date, results from alcohol intervention studies on medication adherence and viral suppression have been mixed. Parsons et al tested effects of an 8-session motivational interviewing (MI) and cognitive behavioral therapy intervention on alcohol use and ART adherence.37 Though their intervention did not reduce alcohol use, at 3 months, medication adherence and viral suppression improved. In contrast, Samet and colleagues tested a 4-session MI based intervention for alcohol use and ART adherence, and found no significant intervention effect on ART adherence or alcohol use.38 Our intervention was briefer than both of these interventions, and was a single target intervention focused primarily on alcohol reduction, rather than medication adherence or viral suppression, which may explain some differences in our findings.
Our study has limitations. While a major strength of the study is its inclusion of urban HIV infected women, our results may not be generalizable to other settings, to women not engaged in HIV clinical care or HIV infected men. In addition, the intervention was delivered by a counselor, and not integrated directly into the primary care office visit. However, with increased integration of behavioral health specialists into primary care settings through the Affordable Care Act, a two session brief alcohol intervention may now be feasible in an HIV primary care setting. Other limitations include the use of self-reported alcohol use which may be subject to recall bias and social desirability bias. Research assistants who conducted the baseline and follow-up assessments were trained in nonjudgmental interview techniques and blind to intervention condition, limiting the potential impact on group differences. We did not observe a between-group difference in liver function (AST and ALT) as a potential biomarker of alcohol use over the follow-up period. However, despite over half of the sample being co-infected with HCV, these measures were within normal limits at baseline, leading to a floor effect in the data. While newer biomarkers such as phosphatidylethanol (PEth) are now being evaluated among individuals with HIV, at the time of study initiation PEth was not in use.39 Finally, we had limited power to detect differences in HIV treatment outcomes.
In summary, this study demonstrates that brief alcohol intervention can reduce frequency of any alcohol use and heavy/binge drinking among urban women living with HIV. Importantly, women who received the brief alcohol intervention also decreased days of unprotected vaginal sex, a very high risk behavior in this population. Further research is needed to determine whether augmentation of brief intervention with Mhealth modalities or alcohol pharmacotherapy can also reduce drinking intensity (drinks per drinking day), particularly among patients with more severe alcohol use disorders.
Acknowledgments
Funding: This research was funded by the National Institute of Alcohol Abuse and Alcoholism NIAAA R01 AA014500 (McCaul, Chander, Hutton) and K23AA015313 (Chander).
Footnotes
This research was presented at the 35th Annual Conference of the Research Society on Alcoholism June 23–27 2012, in San Francisco, CA.
Registered at ClinicalTrials.gov: NCT00127231
Reference List
- 1.Cook RL, Zhu F, Belnap BH, et al. Longitudinal trends in hazardous alcohol consumption among women with human immunodeficiency virus infection, 1995–2006. Am J Epidemiol. 2009;169:1025–1032. doi: 10.1093/aje/kwp004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52:180–202. doi: 10.1097/QAI.0b013e3181b18b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hutton HE, McCaul ME, Chander G, et al. Alcohol use, anal sex, and other risky sexual behaviors among HIV-infected women and men. AIDS Behav. 2013;17:1694–1704. doi: 10.1007/s10461-012-0191-4. [DOI] [PubMed] [Google Scholar]
- 4.Shuper PA, Joharchi N, Irving H, Rehm J. Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: review and meta-analysis. AIDS Behav. 2009;13:1021–1036. doi: 10.1007/s10461-009-9589-z. [DOI] [PubMed] [Google Scholar]
- 5.Neblett RC, Hutton HE, Lau B, McCaul ME, Moore RD, Chander G. Alcohol consumption among HIV-infected women: impact on time to antiretroviral therapy and survival. J Womens Health (Larchmt ) 2011;20:279–286. doi: 10.1089/jwh.2010.2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeLorenze GN, Weisner C, Tsai AL, Satre DD, Quesenberry CP., Jr Excess mortality among HIV-infected patients diagnosed with substance use dependence or abuse receiving care in a fully integrated medical care program. Alcohol Clin Exp Res. 2011;35:203–210. doi: 10.1111/j.1530-0277.2010.01335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Institute of Alcohol Abuse and Alcoholism. Helping Patients Who Drink Too Much, A Clinician’s Guide. 2005 http://pubs_niaaa_nihgov/publications/Practitioner/CliniciansGuide2005/guide.pdf [serial online]
- 8.Schmidt L, Weisner C. The emergence of problem-drinking women as a special population in need of treatment. Recent Dev Alcohol. 1995;12:309–334. doi: 10.1007/0-306-47138-8_20. [DOI] [PubMed] [Google Scholar]
- 9.Greenfield SF, Pettinati HM, O’Malley S, Randall PK, Randall CL. Gender differences in alcohol treatment: an analysis of outcome from the COMBINE study. Alcohol Clin Exp Res. 2010;34:1803–1812. doi: 10.1111/j.1530-0277.2010.01267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Donnell A, Anderson P, Newbury-Birch D, et al. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol. 2014;49:66–78. doi: 10.1093/alcalc/agt170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manwell LB, Fleming MF, Mundt MP, Stauffacher EA, Barry KL. Treatment of problem alcohol use in women of childbearing age: results of a brief intervention. [PubMed] [Google Scholar]
- 12.Samet JH, Walley AY. Interventions targeting HIV-infected risky drinkers: drops in the bottle. Alcohol Res Health. 2010;33(3):267–79. [PMC free article] [PubMed] [Google Scholar]
- 13.Brown JL, DeMartini KS, Sales JM, Swartzendruber AL, DiClemente RJ. Interventions to reduce alcohol use among HIV-infected individuals: a review and critique of the literature. Curr HIV/AIDS Rep. 2013 Dec;10(4):356–70. doi: 10.1007/s11904-013-0174-8. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasin DS, Aharonovich E, O’Leary A, et al. Reducing heavy drinking in HIV primary care: a randomized trial of brief intervention, with and without technological enhancement. Addiction. 2013;108:1230–1240. doi: 10.1111/add.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan AW, Pristach EA, Welte JW, Russell M. Use of the TWEAK test in screening for alcoholism/heavy drinking in three populations. Alcohol Clin Exp Res. 1993;17:1188–1192. doi: 10.1111/j.1530-0277.1993.tb05226.x. [DOI] [PubMed] [Google Scholar]
- 16.Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers. A randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–1045. [PubMed] [Google Scholar]
- 17.Sobell LC, Sobell MB. Timeline followback: A technique for assessing self-reported alcohol consumption. In: Litten R, Allen J, editors. Measuring Alcohol Consumption: Psychosocial and biological methods. New Jersey: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 18.Fleming MF, Lund MR, Wilton G, Landry M, Scheets D. The Healthy Moms Study: the efficacy of brief alcohol intervention in postpartum women. Alcohol Clin Exp Res. 2008;32:1600–1606. doi: 10.1111/j.1530-0277.2008.00738.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol. 1995 Jul;56(4):423–32. doi: 10.15288/jsa.1995.56.423. [DOI] [PubMed] [Google Scholar]
- 20.First Michael B, Spitzer Robert L, Miriam Gibbon, Williams Janet BW. Structures Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; Nov, 2002. [Google Scholar]
- 21.McLellan AT, Cacciola JC, Alterman AI, Rikoon SH, Carise D. The Addiction Severity Index at 25: origins, contributions and transitions. Am J Addict. 2006;15:113–124. doi: 10.1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- 22.Ho DE, Imai K, King G, Stuart EA. MatchIt: Nonparametric Preprocessing for Parametric Causal Inference. Journal of Statistical Software. 2011;42:1–28. [Google Scholar]
- 23.Stuart EA. Matching methods for causal inference: A review and a look forward. Stat Sci. 2010;25:1–21. doi: 10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koenker R. Quantile Regression. Cambridge University Press; 2005. [Google Scholar]
- 25.Geraci M, Bottai M. Quantile regression for longitudinal data using the asymmetric Laplace distribution. Biostatistics. 2007;8:140–154. doi: 10.1093/biostatistics/kxj039. [DOI] [PubMed] [Google Scholar]
- 26.Geraci M. Linear Quantile Mixed Models: The lqmm Package for Laplace Quantile Regression. Journal of Statistical Software. 2014;57:1–29. [Google Scholar]
- 27.Geraci M, Bottai M. Linear Quantile Mixed Models. Statistics and Computing. 2014;24:461–479. [Google Scholar]
- 28.Bottai M, Cai B, McKeown RE. Logistic quantile regression for bounded outcomes. Stat Med. 2010;29:309–317. doi: 10.1002/sim.3781. [DOI] [PubMed] [Google Scholar]
- 29.Machado JAF, Santos Silva JMC. Quantiles for Counts. Journal of the American Statistical Association. 2005;100:1226–1237. [Google Scholar]
- 30.McCambridge J, Kypri K, McElduff P. Regression to the mean and alcohol consumption: a cohort study exploring implications for the interpretation of change in control groups in brief intervention trials. Drug Alcohol Depend. 2014;135:156–159. doi: 10.1016/j.drugalcdep.2013.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCambridge J, Kypri K. Can simply answering research questions change behaviour? Systematic review and meta analyses of brief alcohol intervention trials. PLoS One. 2011;6:e23748. doi: 10.1371/journal.pone.0023748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jonas DE, Amick HR, Feltner C, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA. 2014;311:1889–1900. doi: 10.1001/jama.2014.3628. [DOI] [PubMed] [Google Scholar]
- 33.Blodgett JC, Del Re AC, Maisel NC, Finney JW. A meta-analysis of topiramate’s effects for individuals with alcohol use disorders. Alcohol Clin Exp Res. 2014;38:1481–1488. doi: 10.1111/acer.12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Erwin BL, Slaton RM. Varenicline in the Treatment of Alcohol Use Disorders. Ann Pharmacother. 2014;48:1445–1455. doi: 10.1177/1060028014545806. [DOI] [PubMed] [Google Scholar]
- 35.Velasquez MM, von Sternberg K, Johnson DH, Green C, Carbonari JP, Parsons JT. Reducing sexual risk behaviors and alcohol use among HIV-positive men who have sex with men: a randomized clinical trial. J Consult Clin Psychol. 2009 Aug;77(4):657–67. doi: 10.1037/a0015519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Braithwaite RS, McGinnis KA, Conigliaro J, et al. A temporal and dose-response association between alcohol consumption and medication adherence among veterans in care. Alcohol Clin Exp Res. 2005;29:1190–1197. doi: 10.1097/01.alc.0000171937.87731.28. [DOI] [PubMed] [Google Scholar]
- 37.Parsons JT, Golub SA, Rosof E, Holder C. Motivational interviewing and cognitive-behavioral intervention to improve HIV medication adherence among hazardous drinkers: a randomized controlled trial. J Acquir Immune Defic Syndr. 2007 Dec 1;46(4):443–50. doi: 10.1097/qai.0b013e318158a461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Samet JH, Horton NJ, Meli S, Dukes K, Tripps T, Sullivan L, Freedberg KA. A randomized controlled trial to enhance antiretroviral therapy adherence in patients with a history of alcohol problems. Antivir Ther. 2005;10(1):83–93. doi: 10.1177/135965350501000106. [DOI] [PubMed] [Google Scholar]
- 39.Hahn JA, Dobkin LM, Mayanja B, Emenyonu NI, Kigozi IM, Shiboski S, Bangsberg DR, Gnann H, Weinmann W, Wurst FM. Phosphatidylethanol (PEth) as a biomarker of alcohol consumption in HIV-positive patients in sub-Saharan Africa. Alcohol Clin Exp Res. 2012 May;36(5):854–62. doi: 10.1111/j.1530-0277.2011.01669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]