Summary:
With a growing national emphasis in data transparency and reporting of public health data, it is essential for researchers to know more about Medicare claims data, the largest and most reliable source of health-care utilization and expenditure for individuals older than 65 years in the United States. This article provides an overview of Medicare claims data for plastic surgery outcomes research. We highlight essential information on various files included in Medicare claims data, strengths and limitations of the data, and ways to expand the use of existing data for research purposes. As of now, Medicare data are limited in providing adequate information regarding severity of diagnosed conditions, health status of individuals, and health outcomes after certain procedures. However, the data contain all health-care utilization and expenditures for services that are covered by Medicare Parts A, B, and D (inpatient, outpatient, ambulatory-based and physician-based services, and prescription drugs). Additionally, Medicare claims data can be used for longitudinal analysis of variations in utilization and cost of health-care services at the patient level and provider level. Linking Medicare claims data with other national databases and utilizing the ICD-10 coding system would further expand the use of these datasets in health services research.
The number and proportion of individuals of the age 65 years or older are rapidly increasing. According to the 2010 census, there were 40.3 million people aged 65 years or older in the United States, representing 13% of the total population and 36% of the total health-care expenditure.1 It is, therefore, important to study health-care use and cost among this population. Medicare is a federally funded and administered program that provides health insurance for approximately 47 million individuals who aged 65 years and older. Medicare claims data offer a unique opportunity for researchers to analyze the trends in plastic surgery treatment options, variations in treatment and expenditures, and comparative effectiveness of treatments and surgical procedures.
Medicare claims data are derived from the payment or reimbursement of medical bills. Therefore, they are regularly audited and are of the highest quality. These data have increasingly been used for research purposes because of the wealth of information they provide for a nationally representative population of adults aged 65 years and older. However, Medicare data are complex and “highly susceptible to misleading conclusions”2 that could compromise the quality of patient care. This article comes at a time of increased national emphasis on health services research and heightened transparency of Medicare claims. In this article, we discuss plastic surgery research applications, major pros and cons of using Medicare data for research, and how to further expand the use of claims data for research purposes. This article will assist practicing plastic surgeons in better understanding the literature that is derived from Medicare data and to promote original plastic surgery research using Medicare data.
HISTORICAL BACKGROUND
The Medicare program has been amended and has grown more complex over the decades since its 1965 launch. Today, people aged 65 years or older comprise the majority (85%) of Medicare beneficiaries, followed by younger individuals with certain disabilities (15%) and people of all ages with end-stage renal disease (<1%). Part A now covers inpatient hospital care, skilled nursing facilities, and home health care and hospice care. To be eligible for Part B, people must also be eligible for or have bought into Medicare Part A.3 Premiums and coverage caps for inpatient and outpatient settings change on a yearly basis and are publicly available.4 Medicare Part C, also known as Medicare Advantage, is a health plan that is offered by private companies that are in contract with Medicare and provides Part A, Part B, and possibly prescription drug coverage benefits to those enrolled.5,6 Cost sharing under Medicare Advantage plans vary depending on geographic location and the specific plan.6,7 Finally, Part D, implemented in 2006, is an optional federally funded and privately administered program, which provides prescription drug coverage for those enrolled3; cost and coverage caps may vary depending on geographic location and the Part D plan.8
PROCUREMENT AND USE OF MEDICARE CLAIMS DATA IN RESEARCH
Although Medicare claims data were originally created for payment, reimbursement, and administrative purposes, it did not take long for the data to be used for various research initiatives. The Research Data Assistance Center assists researchers to identify files needed for their research and is the liaison between them and the Center for Medicare and Medicaid Services (CMS).9 Medicare claims data are considered Research identifiable files, containing beneficiary-level protected health information.10 After identifying the required Medicare files, the Research Data Assistance Center submits a researcher’s data request to CMS. The CMS Privacy Board reviews the submitted research proposal and requires an Institutional Review Board approval and Data Use Agreement to ensure that patient privacy is protected and the need for data is justified.
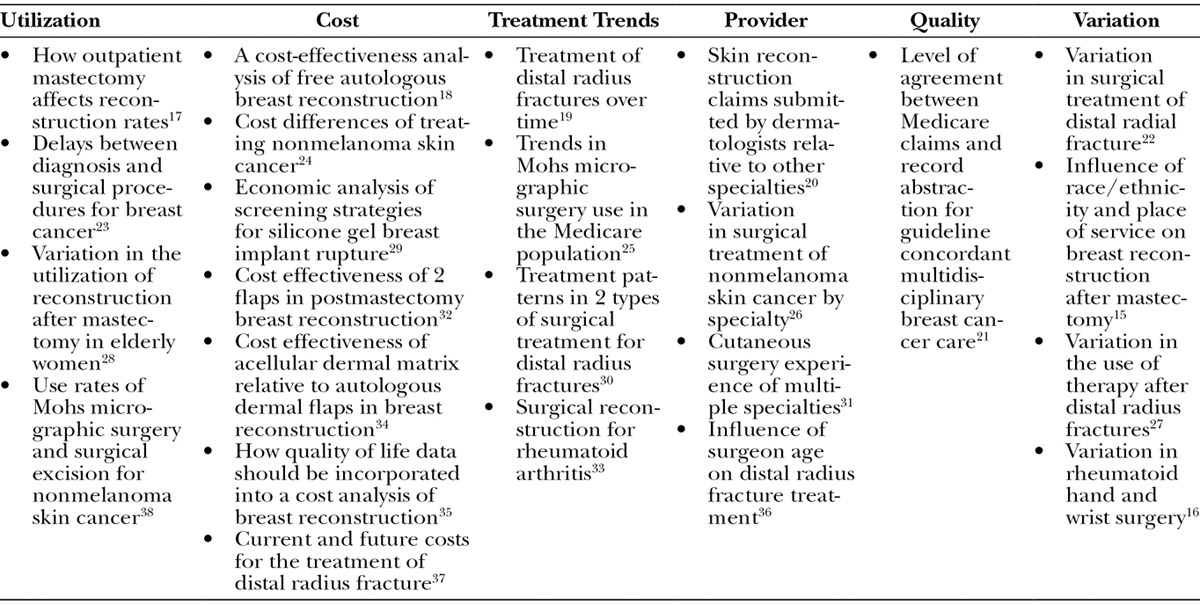
Many of the earlier investigations using Medicare claims data focused on analyzing the retrospective and prospective payment system11–13 and assessing the sensitivity and specificity of the data.11,14 Over the last decade, however, researchers have increasingly used Medicare claims data for various issues in surgical outcomes research. Investigations of the factors influencing variation in breast reconstruction15 and in rheumatoid hand and wrist surgery16 are examples of how data have recently been used in plastic surgery outcomes research (Table 1). The data can be analyzed according to different units of analysis, such as patient, provider, location of care, diagnosis, procedure, or geographic area.
Table 1.
Use of Medicare Data in Plastic Surgery Outcomes Research
MEDICARE CLAIMS FILES
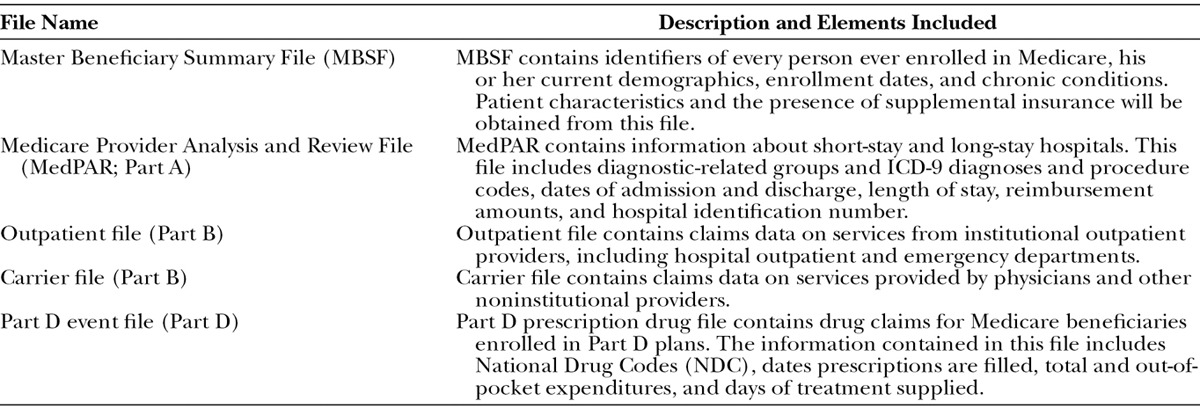
Table 2 shows a list of commonly used Medicare data files. Part A (Medicare Provider and Analysis Review), Part B (Carrier File), and Part D are all available for purchase. Most researchers exclude Part C recipients from their analysis because Medicare Managed Care (MMC) participants do not have any inpatient and outpatient claims data. Medicare data files can be used for research in 3 ways: (1) as identifiable data files, containing beneficiary-specific and physician-specific information, (2) as limited dataset files with no identifying information, and (3) as nonidentifiable data files within the public domain. It is essential to get the denominator file, also known as the Master Beneficiary Summary File, if demographic information is needed. For example, the Master Beneficiary Summary File can be used to verify a beneficiary’s age, sex, race, and other important demographic and insurance information; it also allows researchers to track patients over time if several years of data are obtained. The costs in obtaining data vary depending on which database is used and the amount of data that is abstracted.
Table 2.
Description of Medicare Claims Files
STRENGTHS AND WEAKNESSES OF MEDICARE DATA
Medicare claims data contain reliable demographic information including age, sex, race, and place of residence for all individuals who are enrolled in Medicare. Furthermore, claims data contain information regarding utilization of various health services that are covered, and information about services that are to be paid and the providers of these services. Beneficiaries’ identification is encrypted but patient factors can be identified in aggregate.
Claims data contain information about covered services used by beneficiaries. Therefore, researchers can obtain the exact place of care, dates of admission and discharge, diagnosis, procedures performed, prescriptions received, and detailed expenditures related to the services and procedures received. Because Medicare claims data report on a large population base, researchers can use these datasets for detailed longitudinal subgroup analysis or cost-effectiveness of surgical treatment options without being concerned about loss of statistical power.
Unlike survey or clinical data, administrative claims data do not include any self-reported conditions. Therefore, conditions must be diagnosed before individuals can be included in the selected cohort. As a result, chronic conditions such as hypertension or depression are most often underdiagnosed. Diagnosis can be found as International Classification of Diseases, ninth revision (ICD-9) codes; however, these codes do not define the severity or history of the disease. This can pose a problem for researchers who are assessing 30-day postoperative complications because ICD-9 codes do not specify whether a diagnosis is related to a preoperative comorbidity or a postoperative complication. Thus, complication rates may be overestimated or underestimated if relying on ICD-9 codes. Lawson et al39 found that agreement between the American College of Surgeons National Surgical Quality Improvement Program and Medicare data for 10 postoperative complications ranged from poor to moderate.
Some components of treatments may not be included in bills if reimbursement rates are relatively inexpensive. Thus, it can be difficult to know whether these components of treatment are being uniformly provided to all patients in the dataset. In addition, different care settings use different coding systems for procedures. The American Medical Association registered and continues to add/modify the Current Procedure Terminology (CPT) codes.40 On the other hand, the Centers for Medicare & Medicaid Services created and regularly change the Healthcare Common Procedure Coding System (HCPCS) codes.41 Therefore, there is no universal coding system in place. For instance, inpatient care is coded using 4-digit ICD-9 procedure codes; Carrier and Durable Medical Equipment files usually use 5-digit CPT and HCPCS codes; hospital outpatient care uses a mix of CPT and hospital billing center codes. Also, there are many discrepancies between CPT and HCPCS codes, making it a challenging task for providers or researchers to investigate an exact condition or procedure.42 Finally, both CPT and HCPCS codes change regularly, on a year-to-year basis. Therefore, researchers have to check the accuracy of these codes regularly.43
Claims data do not include clinical information about the health status of individuals. Medicare claims indicate records of health services received, not the care needed based on individuals’ health conditions. Additionally, because test results are not included, there is no direct way to assess the results of the services received.
Another limitation is that data are limited to covered benefits. Before 2006, Medicare had no pharmacy benefit so outpatient medications before 2006 cannot be studied using Medicare data. Also, covered services for which claims are not submitted are not included in the data. Thus, there would be no record of immunizations or prescription drugs if Medicare was not the payer of the service.
Finally, a growing number of Medicare beneficiaries have chosen to join an MMC plan as a cost saving measure.6 Today, about 30% of all Medicare beneficiaries are enrolled in an MMC plan.6 This is an important issue, which severely undermines the representativeness of Medicare data. As a result of the 2003 Medicare Modernization and Improvement Act, starting in 2004, Medicare began subsidizing payments to MMC plans.6 Therefore, many MMC plans expanded their benefits, without additional cost to enrollees. For example, many MMC enrollees had prescription drug coverage before the implementation of Part D in 2006.44 Because MMC plans have offered lower premium and copayment, and have provided additional services (such as preventive care), their enrollment increased significantly over time.5 During the past decade, MMC enrollment increased by more than 50% from about 6 to 15 million.5 With the exception of Medicare Part D event files, Medicare claims data do not have any information about health-care utilization and expenditure for these individuals.
WORKING AROUND THE LIMITATIONS OF MEDICARE CLAIMS DATA
One of the main challenges in using Medicare claims data for health outcome research is their lack of granularity in measuring health outcomes. Administrative claims data, by nature, are limited in providing health outcome measures. Researchers who are studying surgical outcomes are often limited to using mortality and hospital readmission rates as proxies for health outcome measures. Part of this issue, however, has to do with the outdated ICD-9 coding system that is still in use by the Centers for Medicare & Medicaid Services.
In 1992, the World Health Organization, after a decade of work, published the ICD-10 diagnostic and procedure codes. During the 1990s, most developed nations switched to the ICD-10 coding system.45 Today, the United States is one of the few developed nations that have not yet adopted the new coding system.46 ICD-10 codes would dramatically improve the quality of the data from clinical and surgical research perspectives. For example, the set of available codes has expanded from 13,000 codes in ICD-9 to 68,000 codes in ICD-10. Additionally, the code set has expanded from 5 digits in ICD-9 to 7 digits in ICD-10. These enhancements not only allow the coding system to reflect new advancements in the world of medicine and technology, but they also make it possible to report laterality, symptoms, severity, and related complications of procedures undertaken. Although using the ICD-10 codes in Medicare claims data would provide more detailed information and expand the potential range of outcome research, the transition from ICD-9 to ICD-10 codes will require a learning curve for physicians, coders, and researchers. Instead of using 1 code that encompasses all aspects of a procedure, the ICD-10 requires that each distinct portion of a procedure is coded separately.47 It will be difficult to conduct and interpret studies that use Medicare data from both before and after the transition to ICD-10.
Researchers can limit some of the drawbacks of Medicare claims data by linking the data with various national datasets (Fig. 1). This can be accomplished by using various fields (such as beneficiary ID, beneficiary zip code, and provider ID) included in Medicare data files. The following are just a few examples:
Fig. 1.
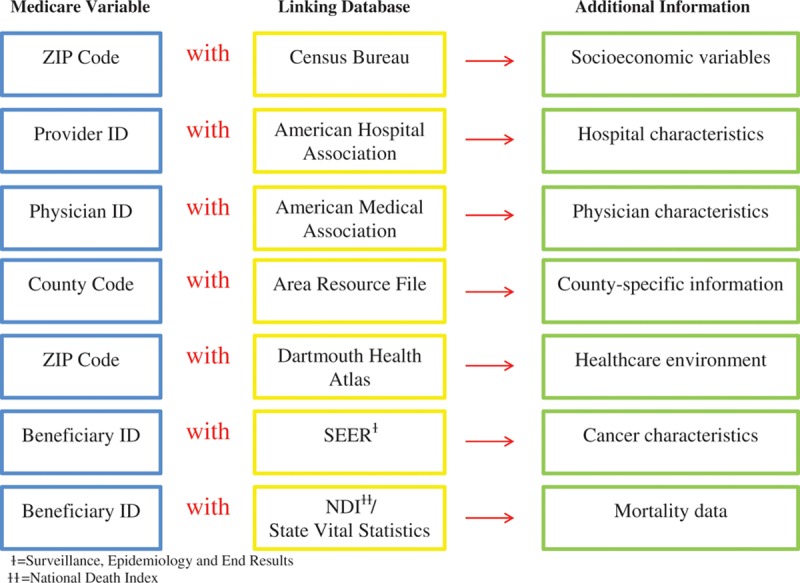
Information that may be obtained by linking Medicare claims data variables with other databases.
Census Bureau Data
Using a beneficiary’s place of residence ZIP code available in the master beneficiary file, researchers can link Medicare data with ZIP code level socioeconomic variables such as mean household income, education level, and median household value. There are no socioeconomic variables available in the Medicare claims data. Therefore, the ZIP code level variables obtained from the Census Bureau Data can be utilized as proxies for socioeconomic variables.48 In their study of postmastectomy breast reconstruction, Onega et al15 controlled for income as a potential confounder by using the median household income for tract of residence at the time of breast cancer diagnosis.
Provider Data (Hospitals and Physicians)
Researchers investigating health care delivered by different institutions may be interested in evaluating the influence of hospital characteristics such as their teaching status, bed size, nurse-to-patient ratio, and average daily census.49,50 Such information can be accessed through the American Hospital Association Annual Survey Database. Medicare inpatient claims data can be linked to American Hospital Association data by Medicare provider ID, recorded in both datasets.51 Furthermore, measuring surgeons’ characteristics is becoming increasingly important in health services research. Researchers were previously limited to studying associations between hospital volume and surgical outcomes, but they are now able to specify the surgeon within the institution to evaluate his or her personal surgical volume. Waljee et al36 found an association between surgeon age and surgical treatment chosen after distal radius fracture. Attending physicians are identifiable using the Unique Identification Number of Physicians and National Provider Identifier. Using these 2 physician IDs, Medicare outpatient claims can be linked to the American Medical Association physician master file, which contains primary and secondary specialty, age, year of graduation from medical school, geographic location, and other important physician characteristics.36,52
Area Resource File
The National Bureau of Standards, U.S. Department of Commerce, established the county codes used in the Area Resource File (ARF) and the Health Resource and Services Administration, Bureau of Health Professions makes the ARF available.53 The county-specific ARF is a database containing more than 6000 variables on health facilities, health professions, and measures of resource scarcity, economic activity, and socioeconomic and environmental characteristics.53 The ARF can be merged with Medicare data files at a county level. Additional information such as density of physicians or hospitals, stratified by patients’ sex, age, and race/ethnicity; physician and hospital characteristics; and county-level population density information can be merged with Medicare data. For example, in a study of postmastectomy breast reconstruction, Bian et al17 used the Surveillance, Epidemiology, and End Results (SEER)-Medicare database linked to the ARF to determine county-level health care resources such as the number of specialty surgeons per 1000 population.
Dartmouth Health Atlas Data
For the past 2 decades, the Dartmouth Atlas Working Group has used Medicare data to provide a wealth of comprehensive information on the health-care market. Dartmouth Atlas Working Group provides a variety of publicly available datasets that can expand researchers’ understanding of the health-care environment. These data are available at different levels (state, hospital referral region, hospital service area, or county) and can be linked to Medicare data via a beneficiary’s place of residence zip code. For example, using these datasets, researchers can include availability of certain specialists or family practitioners where beneficiaries reside.54
Surveillance, Epidemiology, and End Results Data
The SEER data collected by the National Cancer Institute cover cancer incidence and survival data of approximately 28% of the U.S. population. The SEER program began in 1973 and has been collecting and releasing data each year on patient demographics; tumor characteristics such as primary tumor site, tumor morphology, and stage at diagnosis; and treatment and vital status of patients (provided by the National Center for Health Statistics).55 This database includes cancer data such as histology, stage, and grade, which are not otherwise available in the Medicare database. However, the SEER program only follows each cancer case for 4 months; thus, the data do not capture treatments provided after 4 months beyond the primary diagnosis, and there is no information on recurrence or metastasis. Additionally, the sample size will be smaller when compared with the case in which the Medicare data alone are used. Furthermore, each case enters the system on the initial diagnosis of cancer without morbidity and health services utilization information before the diagnosis. Lastly, there are no expenditure-related variables in the SEER datasets to allow for economic analysis. Compared with SEER data, Medicare claims data reflect use and expenditure of health-care services utilized by beneficiaries for the whole period between enrollment in Medicare plans and death or disenrollment; however, they do not provide any cancer characteristics or time of initial diagnosis of cancer. The 2 databases are complementary, and the linkage of SEER and Medicare data provides comprehensive episodes of cancer care. The merged data can enable researchers to identify diagnosis of cancer, severity of the condition, other comorbidities, and finally health services use and their corresponding expenditure before, during, and after cancer diagnosis.56–58 In et al28 used the linked SEER-Medicare database to identify elderly patients with early-stage breast cancer who subsequently underwent mastectomy and reconstruction. Linking SEER data to Medicare data not only provides a longitudinal perspective, but it also enhances the identification of treatment procedures provided to cancer patients (as SEER only records the most invasive surgeries or cancer therapies). For example, 18% of breast cancer patients identified as receiving radiation therapy in Medicare data were not recorded accordingly in the SEER data.59 Furthermore, research on complications after cancer treatment, readmissions, and recurrences also becomes possible using the combined data.60–63
CONCLUSIONS
This article provides an overview regarding Medicare claims data, their use in plastic surgery outcomes research, their strengths and weaknesses, and how to work with some of their inherent limitations. It is important for investigators to understand Medicare data before initiating a project using Medicare claims. Likewise, it is important to see what others have been able and unable to do using this database to critically evaluate published research and to embark upon original research. Compared with expensive and lengthy clinical trials, use of Medicare claims data for longitudinal population-based studies seems to be a cost-effective approach for various surgical outcomes analyses among the older population.
Footnotes
Disclosure: This work was supported by the Midcareer Investigator Award in Patient-Oriented Research (2 K24-AR053120-06) to Dr. Kevin C. Chung. All other authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.National Institute for Health Care Management (NIHCM) The Concentration of Healthcare Spending. 2012. Available at: http://www.nihcm.org/pdf/DataBrief3Final.pdf. Accessed March 15, 2015. [Google Scholar]
- 2.Department of Health and Human Services (DHHS) Centers for Medicare and Medicaid Services. Request for Public Comments on the Potential Release of Medicare Physician Data. 2013. Available at: http://www.aafp.org/dam/AAFP/documents/advocacy/payment/medicare/LT-CMS-MedicarePhysicianData-090513.pdf. Accessed August 15, 2014. [Google Scholar]
- 3.Medicare Payment Advisory Commision (MedPAC) Status Report on Part D. 2012. Available at: http://www.medpac.gov/documents/reports/chapter-14-status-report-on-part-d-(march-2015-report).pdf. Accessed March 15, 2015. [Google Scholar]
- 4.California Health Advocates. Medicare: Policy, Advocacy and Education. 2014. Available at: https://www.cahealthadvocates.org/basics/benefits-summary.html. Accessed March 15, 2015. [Google Scholar]
- 5.Kaiser Family Foundation (KFF) Medicare Advantage Fact Sheet. 2014. Available at: http://kff.org/medicare/fact-sheet/medicare-advantage-fact-sheet/. Accessed August 15, 2014. [Google Scholar]
- 6.McGuire TG, Newhouse JP, Sinaiko AD. An economic history of Medicare part C. Milbank Q. 2011;89:289–332. doi: 10.1111/j.1468-0009.2011.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.California Health Advocates. Costs and Benefits of Medicare Advantage Plans. 2014. Available at: https://www.cahealthadvocates.org/advantage/costs-benefits.html. Accessed March 15, 2015. [Google Scholar]
- 8.California Health Advocates. Prescription Drugs (Medicare Part D) 2014. Available at: http://www.cahealthadvocates.org/drugs/index.html. Accessed March 15, 2015. [Google Scholar]
- 9.Research Data Assistance Center. 2015. Available at: http://www.resdac.org. Accessed March 15, 2015.
- 10.Research Data Assistance Center. Research Identifiable Files (RIF) Request. 2015. Available at: http://www.resdac.org/cms-data/request/research-identifiable-files. Accessed March 15, 2015. [Google Scholar]
- 11.Calore KA, Iezzoni L. Disease staging and PMCs. Can they improve DRGs? Med Care. 1987;25:724–737. doi: 10.1097/00005650-198708000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Pettengill J, Vertrees J. Reliability and validity in hospital case-mix measurement. Health Care Financ Rev. 1982;4:101–128. [PMC free article] [PubMed] [Google Scholar]
- 13.Sloan FA, Morrisey MA, Valvona J. Effects of the Medicare prospective payment system on hospital cost containment: an early appraisal. Milbank Q. 1988;66:191–220. [PubMed] [Google Scholar]
- 14.Hebert PL, Geiss LS, Tierney EF, et al. Identifying persons with diabetes using Medicare claims data. Am J Med Qual. 1999;14:270–277. doi: 10.1177/106286069901400607. [DOI] [PubMed] [Google Scholar]
- 15.Onega T, Weiss J, Kerlikowske K, et al. The influence of race/ethnicity and place of service on breast reconstruction for Medicare beneficiaries with mastectomy. Springerplus. 2014;3:416. doi: 10.1186/2193-1801-3-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhong L, Chung KC, Baser O, et al. Variation in rheumatoid hand and wrist surgery among medicare beneficiaries: a population-based cohort study. J Rheumatol. 2015;42:429–436. doi: 10.3899/jrheum.140658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bian J, Krontiras H, Allison J. Outpatient mastectomy and breast reconstructive surgery. Ann Surg Oncol. 2008;15:1032–1039. doi: 10.1245/s10434-007-9762-4. [DOI] [PubMed] [Google Scholar]
- 18.Chatterjee A, Krishnan NM, Van Vliet MM, et al. A comparison of free autologous breast reconstruction with and without the use of laser-assisted indocyanine green angiography: a cost-effectiveness analysis. Plast Reconstr Surg. 2013;131:693e–701e. doi: 10.1097/PRS.0b013e31828659f4. [DOI] [PubMed] [Google Scholar]
- 19.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91:1868–1873. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Donaldson MR, Coldiron BM. Dermatologists perform the majority of cutaneous reconstructions in the Medicare population: numbers and trends from 2004 to 2009. J Am Acad Dermatol. 2013;68:803–808. doi: 10.1016/j.jaad.2013.01.026. [DOI] [PubMed] [Google Scholar]
- 21.Fleming ST, Kimmick GG, Sabatino SA, et al. Patterns of Care Study Group. Defining care provided for breast cancer based on medical record review or Medicare claims: information from the Centers for Disease Control and Prevention Patterns of Care Study. Ann Epidemiol. 2012;22:807–813. doi: 10.1016/j.annepidem.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 22.Fanuele J, Koval KJ, Lurie J, et al. Distal radial fracture treatment: what you get may depend on your age and address. J Bone Joint Surg Am. 2009;91:1313–1319. doi: 10.2106/JBJS.H.00448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bleicher RJ, Ruth K, Sigurdson ER, et al. Preoperative delays in the US Medicare population with breast cancer. J Clin Oncol. 2012;30:4485–4492. doi: 10.1200/JCO.2012.41.7972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chirikov VV, Stuart B, Zuckerman IH, et al. Physician specialty cost differences of treating nonmelanoma skin cancer. Ann Plast Surg. 2015;74:93–99. doi: 10.1097/SAP.0b013e31828d73f0. [DOI] [PubMed] [Google Scholar]
- 25.Donaldson MR, Coldiron BM. Mohs micrographic surgery utilization in the Medicare population, 2009. Dermatol Surg. 2012;38:1427–1434. doi: 10.1111/j.1524-4725.2012.02464.x. [DOI] [PubMed] [Google Scholar]
- 26.Manternach T, Housman TS, Williford PM, et al. Surgical treatment of nonmelanoma skin cancer in the Medicare population. Dermatol Surg. 2003;29:1167–1169; discussion 1169. doi: 10.1111/j.1524-4725.2003.29381.x. [DOI] [PubMed] [Google Scholar]
- 27.Waljee JF, Zhong L, Shauver M, et al. Variation in the use of therapy following distal radius fractures in the United States. Plast Reconstr Surg Glob Open. 2014;2:e130. doi: 10.1097/GOX.0000000000000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.In H, Jiang W, Lipsitz SR, et al. Variation in the utilization of reconstruction following mastectomy in elderly women. Ann Surg Oncol. 2013;20:1872–1879. doi: 10.1245/s10434-012-2821-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chung KC, Malay S, Shauver MJ, et al. Economic analysis of screening strategies for rupture of silicone gel breast implants. Plast Reconstr Surg. 2012;130:225–237. doi: 10.1097/PRS.0b013e318254b43b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Farner S, Malkani A, Lau E, et al. Outcomes and cost of care for patients with distal radius fractures. Orthopedics. 2014;37:e866–e878. doi: 10.3928/01477447-20140924-52. [DOI] [PubMed] [Google Scholar]
- 31.Shaffer CL, Feldman SR, Fleischer AB, Jr, et al. The cutaneous surgery experience of multiple specialties in the Medicare population. J Am Acad Dermatol. 2005;52:1045–1048. doi: 10.1016/j.jaad.2005.03.049. [DOI] [PubMed] [Google Scholar]
- 32.Krishnan NM, Purnell C, Nahabedian MY, et al. The cost effectiveness of the DIEP flap relative to the muscle-sparing TRAM flap in postmastectomy breast reconstruction. Plast Reconstr Surg. 2015;135:948–958. doi: 10.1097/PRS.0000000000001125. [DOI] [PubMed] [Google Scholar]
- 33.Waljee J, Zhong L, Baser O, et al. The incidence of upper and lower extremity surgery for rheumatoid arthritis among Medicare beneficiaries. J Bone Joint Surg Am. 2015;97:403–410. doi: 10.2106/JBJS.N.00802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krishnan NM, Chatterjee A, Van Vliet MM, et al. A comparison of acellular dermal matrix to autologous dermal flaps in single-stage, implant-based immediate breast reconstruction: a cost-effectiveness analysis. Plast Reconstr Surg. 2013;131:953–961. doi: 10.1097/PRS.0b013e3182865a24. [DOI] [PubMed] [Google Scholar]
- 35.Preminger BA, Pusic AL, McCarthy CM, et al. How should quality-of-life data be incorporated into a cost analysis of breast reconstruction? A consideration of implant versus free TRAM flap procedures. Plast Reconstr Surg. 2008;121:1075–1082. doi: 10.1097/01.prs.0000304246.66477.cd. [DOI] [PubMed] [Google Scholar]
- 36.Waljee JF, Zhong L, Shauver MJ, et al. The influence of surgeon age on distal radius fracture treatment in the United States: a population-based study. J Hand Surg Am. 2014;39:844–851. doi: 10.1016/j.jhsa.2013.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shauver MJ, Yin H, Banerjee M, et al. Current and future national costs to medicare for the treatment of distal radius fracture in the elderly. J Hand Surg Am. 2011;36:1282–1287. doi: 10.1016/j.jhsa.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 38.Viola KV, Jhaveri MB, Soulos PR, et al. Mohs micrographic surgery and surgical excision for nonmelanoma skin cancer treatment in the Medicare population. Arch Dermatol. 2012;148:473–477. doi: 10.1001/archdermatol.2011.2456. [DOI] [PubMed] [Google Scholar]
- 39.Lawson EH, Louie R, Zingmond DS, et al. A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg. 2012;256:973–981. doi: 10.1097/SLA.0b013e31826b4c4f. [DOI] [PubMed] [Google Scholar]
- 40.American Medical Association (AMA) Current ProceduralTerminology. 2014. Available at: http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/coding-billing-insurance/cpt.page. Accessed September 15, 2014. [Google Scholar]
- 41.Centers for Medicare and Medicaid Services (CMS) HCPCS General Information. 2014. Available at: http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html?redirect=/medhcpcsgeninfo/. Accessed September 15, 2014. [Google Scholar]
- 42.Health Information Management (HIM) Note similarities and differences between HCPCS, CPT® codes. 2012. Available at: http://www.hcpro.com/HIM-284009–8160/Note-similarities-and-differences-between-HCPCS-CPT-codes.html. Accessed September 15, 2014. [Google Scholar]
- 43.Centers for Medicare and Medicaid Services (CMS) HCPCS Quarterly Updates. 2014. Available at: http://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/HCPCS-Quarterly-Update.html. Accessed August 14, 2014. [Google Scholar]
- 44.Mahmoudi E, Jensen GA. Has Medicare Part D reduced racial/ethnic disparities in prescription drug use and spending? Health Serv Res. 2014;49:502–525. doi: 10.1111/1475-6773.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 46.Meyer H. Coding complexity: US Health Care gets ready for the coming of ICD-10. Health Aff (Millwood) 2011;30:968–974. doi: 10.1377/hlthaff.2011.0319. [DOI] [PubMed] [Google Scholar]
- 47.Utter GH, Cox GL, Owens PL, et al. Challenges and opportunities with ICD-10-CM/PCS: implications for surgical research involving administrative data. J Am Coll Surg. 2013;217:516–526. doi: 10.1016/j.jamcollsurg.2013.04.029. [DOI] [PubMed] [Google Scholar]
- 48.CB. Department of Commerce; US Census Bureau. American FactFinder. 2014. Available at: http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml. March 26, 2015. [Google Scholar]
- 49.Nathan H, Shore AD, Anders RA, et al. Variation in lymph node assessment after colon cancer resection: patient, surgeon, pathologist, or hospital? J Gastrointest Surg. 2011;15:471–479. doi: 10.1007/s11605-010-1410-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schootman M, Jeffe DB, Lian M, et al. The role of poverty rate and racial distribution in the geographic clustering of breast cancer survival among older women: a geographic and multilevel analysis. Am J Epidemiol. 2009;169:554–561. doi: 10.1093/aje/kwn369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schrag D, Bach PB, Dahlman C, Warren JL. Identifying and measuring hospital characteristics using the SEER-Medicare data and other claims-based sources. Med Care. 2002;40(8 Suppl):IV-96–IV-103. doi: 10.1097/00005650-200208001-00013. [DOI] [PubMed] [Google Scholar]
- 52.Baldwin L-M, Adamache W, Klabunde CN, et al. Linking physician characteristics and Medicare claims data: issues in data availability, quality, and measurement. Med Care. 2002;40(8 Suppl):IV-82–IV-95. doi: 10.1097/00005650-200208001-00012. [DOI] [PubMed] [Google Scholar]
- 53.Department of Health and Human Services (DHHS) Health Resources and Services Administration. 2010. Available at: http://arf.hrsa.gov. March 26, 2015. [Google Scholar]
- 54.DAHC. The Dartmouth Atlas of Health Care. 2014. Available at: http://www.dartmouthatlas.org/. March 26, 2015. [Google Scholar]
- 55.Hankey BF, Ries LA, Edwards BK. The surveillance, epidemiology, and end results program: a national resource. Cancer Epidemiol Biomarkers Prev. 1999;8:1117–1121. [PubMed] [Google Scholar]
- 56.Du X, Freeman JL, Warren JL, et al. Accuracy and completeness of Medicare claims data for surgical treatment of breast cancer. Med Care. 2000;38:719–727. doi: 10.1097/00005650-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 57.Warren JL, Harlan LC, Fahey A, et al. Utility of the SEER-Medicare data to identify chemotherapy use. Med Care. 2002;40(8 Suppl):IV-55–IV-61. doi: 10.1097/01.MLR.0000020944.17670.D7. [DOI] [PubMed] [Google Scholar]
- 58.Welzel TM, Graubard BI, Zeuzem S, et al. Metabolic syndrome increases the risk of primary liver cancer in the United States: a study in the SEER-Medicare database. Hepatology. 2011;54:463–471. doi: 10.1002/hep.24397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Du X, Freeman JL, Goodwin JS. Information on radiation treatment in patients with breast cancer: the advantages of the linked Medicare and SEER data. J Clin Epidemiol. 1999;52:463–470. doi: 10.1016/s0895-4356(99)00011-6. [DOI] [PubMed] [Google Scholar]
- 60.Warren JL, Klabunde CN, Schrag D, et al. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40(8 Suppl):IV-3–IV-18. doi: 10.1097/01.MLR.0000020942.47004.03. [DOI] [PubMed] [Google Scholar]
- 61.Potosky AL, Warren JL, Riedel ER, et al. Measuring complications of cancer treatment using the SEER-Medicare data. Med Care. 2002;40(8 Suppl):IV-62. doi: 10.1097/00005650-200208001-00009. [DOI] [PubMed] [Google Scholar]
- 62.Reddy DM, Townsend CM, Jr, Kuo YF, et al. Readmission after pancreatectomy for pancreatic cancer in Medicare patients. J Gastrointest Surg. 2009;13:1963–1974; discussion 1974. doi: 10.1007/s11605-009-1006-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stokes ME, Thompson D, Montoya EL, et al. Ten-year survival and cost following breast cancer recurrence: estimates from SEER-medicare data. Value Health. 2008;11:213–220. doi: 10.1111/j.1524-4733.2007.00226.x. [DOI] [PubMed] [Google Scholar]


