Background:
Since the first successful hand transplantation in 1998, there have been multiple reports about surgical technique, transplant survival, and immunosuppression. However, very limited published data exist on psychosocial outcomes following hand transplantation.
Methods:
We report psychosocial outcomes in a patient with bilateral hand transplants at the midforearm level with serial follow-ups over 3.5 years. Different metrics used to study psychosocial outcomes included the following: SF-12, CES-D, Dyadic Adjustment Scale, Rosenberg SE, and EQ-5D.
Result:
Preoperatively, our patient did not have any evidence of depression (CES-D = 3), had a nonstressful relationship with his spouse (Dyadic Adjustment Scale = 100), and self-esteem was in the normal range (Rosenberg SE = 21). These metrics and his additional scales (SF-12 MCS, EQ-5D, and EQ-VAS) did not change appreciably and were within the normal range for the entire duration of 3.5-year follow-up at all different time points.
Conclusion:
With the increasing popularity of hand transplantation and the increasing awareness of the importance of psychosocial parameters in overall success, appropriate, comprehensive, and standardized measurements are important. These should be an integral part of patients’ screening and follow-up.
Since the first successful hand transplantation in 1998,1 multiple reports exist about surgical technique, transplant survival, and immunosuppression.2–4 However, very limited reports describe psychosocial outcomes after hand transplantation.5–11 As hand transplantation becomes more popular with successful long-term survival, measurement and critical evaluation of psychosocial outcomes gain importance.
We report a combination of psychosocial metrics in our first successful patient and justify standardized measurement of psychosocial domains. We aim to establish a baseline for others to study using a common set of standardized scales.
We have performed 3 bilateral hand transplantations at our institution. Our index patient, a 68-year-old formerly left-handed man, lost all 4 limbs in 2002 due to sepsis and disseminated intravascular coagulation related to a renal stone. He underwent bilateral hand transplantation at the midforearm level on October 5, 2011.
METHODS
We describe psychosocial metrics with serial follow-ups over 3.5 years. Psychosocial self-reported measures included the following: Medical Outcomes Survey Short Form 12 (SF-12),12,13 Center for Epidemiological Studies Depression (CES-D),14,15 Dyadic Adjustment Scale (DAS),16,17 Rosenberg Self-Esteem Scale (Rosenberg SE),18 and EuroQOL 5-Dimension Questionnaires (EQ-5D).19,20 Preoperative social desirability was measured using Marlowe-Crowne Social Desirability Scale (MC-SDS).21
The SF-12 assesses 8 domains, namely general health, physical functioning, physical role, bodily pain, vitality, social functioning, emotional role, and mental health. The first 4 components constitute physical component summary (PCS), whereas the latter 4 provide mental component summary (MCS).12 Scores range from 0 (lowest level of health) to 100 (highest level of health).13
The CES-D is a 20-item scale measuring depressive symptoms among general population. The CES-D employs 4-point scales ranging from “rarely or none of the time” (0 point) to “most or all of the times” (3 points). The total score ranges from 0 to 60, with increasing scores indicating increasing depressive symptom severity.14 CES-D score of >15 is indicative of depression.15
The 32-item DAS measures relationship adjustment and consists of 4 subscales: dyadic consensus, dyadic satisfaction, dyadic cohesion, and affectional expression.16 Scores range from 0–151 with higher scores reflecting a less stressful relationship with a partner.17 Scores >97 indicate “nonstressful” relationship.
The 10-item Rosenberg-SE scale assesses global self-worth by measuring both positive and negative feelings about the self. Items are answered using a 4-point Likert scale ranging from “strongly agree” to “strongly disagree.” Total scores range from 0–30. Scores <15 suggest low self-esteem.18
The EQ-5D assesses function in 5 socially relevant domains: mobility, self-care, usual activities, pain-discomfort, and anxiety-depression.19 Based on these 5 domains, an index score is derived ranging from 1 (best possible health) to −0.11 (worse than death).19 It is accompanied by a Visual Analogue Scale (VAS), which provides a self-assessment of one’s health ranging from 0 (worst imaginable health) to 100 (best imaginable health).20
These measures have established reliability and validity and the selected psychosocial domains are established as risk factors for poorer adjustment post transplantation.22,23 Additionally, the SF-12 and EQ-5D are widely used scales for quality of life post transplantation.24–26 Accordingly, this combination of standardized and validated metrics provides the technology and framework for comparisons of psychosocial outcomes.
RESULTS
Psychosocial outcomes were assessed longitudinally as shown in Table 1 and Figure 1. Preoperatively, there was no evidence of depression (CES-D = 3), a nonstressful relationship with his partner (DAS = 101), normal self-esteem (Rosenberg SE = 19), and average social desirability (MC-SDS = 11). Depressive symptom scores fluctuated but remained well below the clinical cut-off for depression. Similarly, relationship adjustment scores fluctuated but, with the exception of 6 weeks post operation, were within the normal range for the 3.5-year follow-up. The SF-12 MCS was often slightly higher than US norms, and the EQ-5D and EQ-VAS scores were generally stable for the duration of the follow-up. The SF-12 PCS scores worsened at 6 weeks post operation, consistent with broad transplantation findings25 of increased disability and dependence during early surgical recovery, and continued to fluctuate around the baseline over the 3.5-year follow-up.
Table 1.
Psychosocial Outcomes Using Standardized Parameters in a Patient with Bilateral Hand Transplantation at the Midforearm Level with Comparison to the Preoperative State
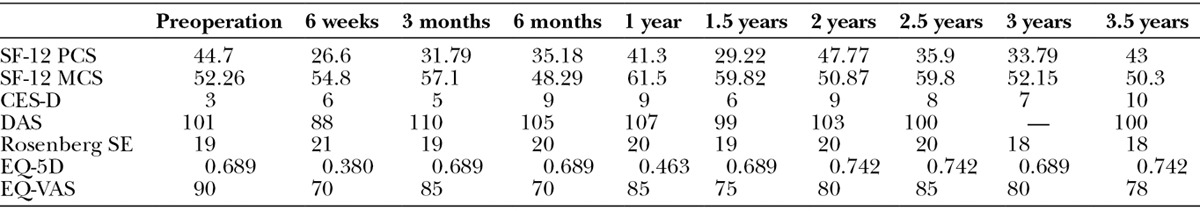
Fig. 1.
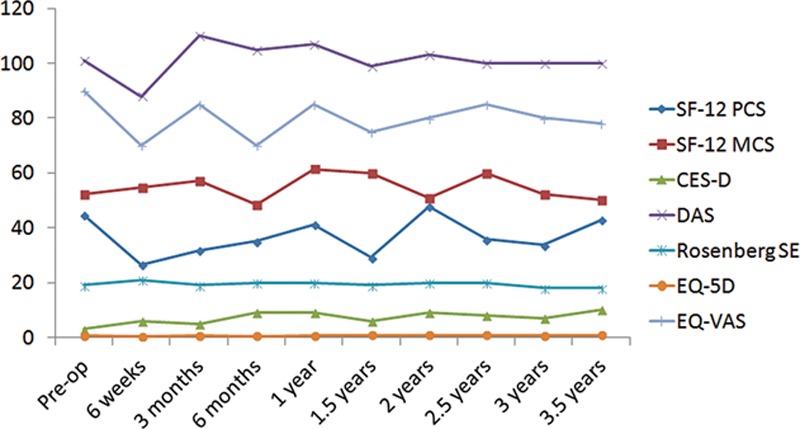
Graphical representation of psychosocial outcomes using standardized parameters in a patient with bilateral hand transplantation at the midforearm level with comparison to the preoperative state.
DISCUSSION
We describe multiple psychosocial outcome metrics and serial long-term follow-up in our first successful patient. To evaluate psychosocial outcomes, we included empirically based risk factors and indicators such as self-esteem, relation with partner, depressive symptoms, and health-related quality of life. These assessments capture a broad cross-section of patients’ psychosocial functioning while being manageable to administer and minimize patient response burden.
Although there are defined parameters for psychological screening of candidates being considered for hand transplant,27–29 there is dearth of literature about psychosocial outcomes following transplant.8–11 Several studies report improved psychosocial outcomes following hand transplantation but such assessment is generally based on personal interviews with patients.9–11
Our findings show that multiple aspects of psychosocial outcomes were largely within normal ranges preoperatively and throughout the postoperative course. There was no apparent sustained improvement among the measured parameters and, consistent with extant transplant literature, a slight transient worsening of well-being in the immediate 6-week postoperative period. These remarkably stable findings may be explained by several possibilities. First, stability in scores may reflect inherent selection bias while considering patients for hand transplantation. Our index patient was well-compensated, both functionally and psychologically, functioning quite independently with prosthesis and with very stable social support. Although this made him an ideal transplantation candidate, it left little room for psychosocial improvement post transplantation. Second, it is possible for patients to falsely improve their scores preoperatively to appear a better candidate for selection. However, the average score on social desirability scale makes it an unlikely possibility in our patient. Third, the extensive follow-up and rehabilitation needed for first few years post transplantation may contribute to limited psychosocial improvement. Patients might have improved objective psychosocial outcomes 5 to 10 years after transplant when follow-up visits are less frequent and their social readjustment is complete.
CONCLUSIONS
With the increasing popularity of hand transplantation and the importance of truly improving our patients’ lives, standardized psychosocial evaluation is an increasingly important part of transplant evaluation. Acknowledging the limitations of data from a single patient, we feel that additional research and increased sample size are needed. However, the psychosocial domains evaluated were chosen based on existing transplant literature and standardized and validated metrics should be an integral part of patients’ screening and follow-up after hand transplantation.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Dubernard JM, Owen E, Herzberg G, et al. Human hand allograft: report on first 6 months. Lancet. 1999;353:1315–1320. doi: 10.1016/S0140-6736(99)02062-0. [DOI] [PubMed] [Google Scholar]
- 2.Kanitakis J, Jullien D, Petruzzo P, et al. Clinicopathologic features of graft rejection of the first human hand allograft. Transplantation. 2003;76:688–693. doi: 10.1097/01.TP.0000079458.81970.9A. [DOI] [PubMed] [Google Scholar]
- 3.Foroohar A, Elliott RM, Kim TW, et al. The history and evolution of hand transplantation. Hand Clin. 2011;27:405–409, vii. doi: 10.1016/j.hcl.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Cavadas PC, Ibáñez J, Thione A, et al. Bilateral trans-humeral arm transplantation: result at 2 years. Am J Transplant. 2011;11:1085–1090. doi: 10.1111/j.1600-6143.2011.03503.x. [DOI] [PubMed] [Google Scholar]
- 5.Dubernard JM, Petruzzo P, Lanzetta M, et al. Functional results of the first human double-hand transplantation. Ann Surg. 2003;238:128–136. doi: 10.1097/01.SLA.0000078945.70869.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hautz T, Engelhardt TO, Weissenbacher A, et al. World experience after more than a decade of clinical hand transplantation: update on the Innsbruck program. Hand Clin. 2011;27:423–431, viii. doi: 10.1016/j.hcl.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Jabłecki J. World experience after more than a decade of clinical hand transplantation: update on the Polish program. Hand Clin. 2011;27:433–442, viii. doi: 10.1016/j.hcl.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Breidenbach WC, 3rd, Tobin GR, 2nd, Gorantla VS, et al. A position statement in support of hand transplantation. J Hand Surg Am. 2002;27:760–770. doi: 10.1053/jhsu.2002.35306. [DOI] [PubMed] [Google Scholar]
- 9.Breidenbach WC, Gonzales NR, Kaufman CL, et al. Outcomes of the first 2 American hand transplants at 8 and 6 years posttransplant. J Hand Surg Am. 2008;33:1039–1047. doi: 10.1016/j.jhsa.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Zhu L, Pei G, Gu L, et al. Psychological consequences derived during process of human hand allograft. Chin Med J (Engl) 2002;115:1660–1663. [PubMed] [Google Scholar]
- 11.Ravindra KV, Buell JF, Kaufman CL, et al. Hand transplantation in the United States: experience with 3 patients. Surgery. 2008;144:638–643. doi: 10.1016/j.surg.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 12.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2nd ed. Boston, MA: The Health Institute, New England; 1998. [Google Scholar]
- 14.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 15.Han M, Jia CX. Reliability and validity of Center for Epidemiological Survey, Depression Scale in different rural populations. Chin J Public Health. 2012;28(10):1265–1267. [Google Scholar]
- 16.Spanier GB. Measuring dyadic adjustment: new scale for assessing the quality of marriage and the similar relationship. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- 17.South SC, Krueger RF, Iacono WG. Factorial invariance of the Dyadic Adjustment Scale across gender. Psychol Assess. 2009;21:622–628. doi: 10.1037/a0017572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenberg M. Society and the adolescent self-image 1965. Available at: http://www.fetzer.org/sites/default/files/images/stories/pdf/selfmeasures/Self_Measures_for_Self-Esteem_ROSENBERG_SELF-ESTEEM.pdf. Accessed on February 22, 2014. [Google Scholar]
- 19. Available at: http://archive.ahrq.gov/professionals/clinicians-providers/resources/rice/EQ5Dscore.html. Accessed February 2005.
- 20.Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 21.Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Psychol. 1960;24:349–354. doi: 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- 22.Dew MA, Simmons RG, Roth LH, et al. Psychosocial predictors of vulnerability to distress in the year following heart transplantation. Psychol Med. 1994;24:929–945. doi: 10.1017/s0033291700029020. [DOI] [PubMed] [Google Scholar]
- 23.Olbrisch ME, Benedict SM, Ashe K, et al. Psychological assessment and care of organ transplant patients. J Consult Clin Psychol. 2002;70:771–783. doi: 10.1037//0022-006x.70.3.771. [DOI] [PubMed] [Google Scholar]
- 24.Anyanwu AC, McGuire A, Rogers CA, et al. Assessment of quality of life in lung transplantation using a simple generic tool. Thorax. 2001;56:218–222. doi: 10.1136/thorax.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang G, Pomahac B. Psychosocial changes 6 months after face transplantation. Psychosomatics. 2013;54:367–371. doi: 10.1016/j.psym.2012.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feurer ID, Russell RT, Pinson CW. Incorporating quality of life and patient satisfaction measures into a transplant outcomes assessment program: technical and practical considerations. Prog Transplant. 2007;17:121–128. doi: 10.1177/152692480701700207. [DOI] [PubMed] [Google Scholar]
- 27.Kumnig M, Jowsey SG, Moreno E, et al. An overview of psychosocial assessment procedures in reconstructive hand transplantation. Transpl Int. 2014;27:417–427. doi: 10.1111/tri.12220. [DOI] [PubMed] [Google Scholar]
- 28.Kumnig M, Jowsey SG, Rumpold G, et al. The psychological assessment of candidates for reconstructive hand transplantation. Transpl Int. 2012;25:573–585. doi: 10.1111/j.1432-2277.2012.01463.x. [DOI] [PubMed] [Google Scholar]
- 29.Carta I, Convertino O, Cornaggia CM. Psychological investigation protocol of candidates for hand transplantation. Transplant Proc. 2001;33:621–622. doi: 10.1016/s0041-1345(00)02171-0. [DOI] [PubMed] [Google Scholar]


