Summary:
Radical parotidectomy often results in complex facial nerve defects involving the main nerve trunk and multiple distal nerve branches. Although cable nerve grafting often leads to good nerve regeneration, severe synkinesis due to aberrant axonal regrowth is inevitable. In such situations, the use of 2 motor sources to differentially reanimate the upper and lower face could minimize synkinesis. Here we describe a method of total facial nerve reconstruction in which the upper and lower face are differentially reconstructed with the hypoglossal nerve and facial nerve, respectively, using 2 interpositional nerve grafts. Reconstruction of the lower face with the facial nerve restored voluntary and coordinated animation, and reconstruction of the upper face with the hypoglossal nerve restored frontalis muscle tone and eye closure. These results suggest that our method could serve as an alternative to conventional techniques that use only the facial or hypoglossal nerve.
In parotid cancer patients, radical parotidectomy often results in complex facial nerve defects, which leave a proximal main nerve stump and multiple distal nerve stumps. Although immediate reconstruction with nerve grafting often leads to good nerve regeneration, severe synkinesis due to misdirected axonal regrowth is inevitable.1 To address this issue, some researchers have used 2 motor sources to differentially reanimate the upper and lower face, ie, the proximal facial nerve for the upper face and the hypoglossal nerve for the lower face.2,3 However, because emotional facial animation such as smiling can only be obtained when the ipsilateral or contralateral facial nerve is used as the motor source,4 we believe the facial nerve should be used for reanimation of the lower face. Here we describe a novel method of total facial nerve reconstruction in which the upper and lower face are differentially reanimated with the hypoglossal nerve and facial nerve, respectively, using 2 interpositional nerve grafts.
CASE REPORT
A 52-year-old man underwent radical right parotidectomy for parotid cancer at Osaka University Medical Hospital. Complete tumor resection resulted in a facial nerve defect with a proximal facial nerve trunk and 6 distal facial nerve stumps (temporal branch, zygomatic branch, 2 buccal branches, and 2 mandibular branches). A 32-cm-long sural nerve graft was harvested and divided into 2 segments.
In one graft, the proximal segment was intraneurally dissected to create 2 5-cm-long branches,5 and the distal segment originally had 4 major branches (Fig. 1). One proximal branch was anastomosed to the facial nerve trunk in an end-to-end fashion and the other proximal branch was anastomosed to the hypoglossal nerve in a side-to-end fashion using the 10% partial neurectomy technique (Fig. 2).6 The distal branches were then anastomosed to the buccal and mandibular branches in an end-to-end fashion. In the other graft, the distal segment was intraneurally dissected to create 2 1.5-cm-long branches (Fig. 1). The proximal stump was anastomosed to the other side of the hypoglossal nerve in a side-to-end fashion using the 30% partial neurectomy technique, and the distal branches were anastomosed to the temporal and zygomatic branches (Fig. 2). After nerve grafting, the soft tissue defect was reconstructed using a free anterolateral thigh flap.
Fig. 1.

A 32-cm-long sural nerve graft was harvested and divided into 2 segments. Upper and lower grafts were used for reanimation of the lower and upper face, respectively.
Fig. 2.
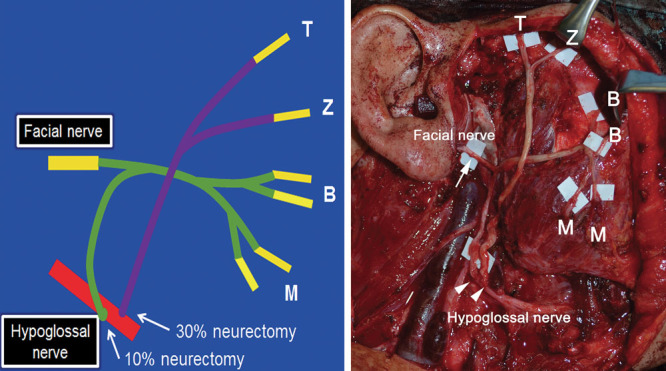
A schematic illustration of the procedure (A) and an intraoperative view (B) are shown. End-to-end anastomotic site between the facial nerve trunk and nerve graft (arrow) and side-to-end anastomotic sites between the hypoglossal nerve and 2 nerve grafts (arrow heads). B indicates buccal branch, M, mandibular branch; T, temporal branch; Z, zygomatic branch.
During the follow-up period, rehabilitation training using mirror visual biofeedback was encouraged. The myogenic tonus of the mimetic muscles started to recover at 4 months postoperatively, followed by spontaneous facial reanimation. There was no synkinesis between the upper and lower face except for the corrugator muscle, which was possibly innervated by the facial nerve, because no movement of the muscle was observed with tongue movement. At 30 months postoperatively, the patient regained a voluntary and coordinated smile. Although there was synkinesis between the frontalis muscle and orbicularis oculi muscle, forehead wrinkles and complete eye closure were restored (Fig. 3) (See video, Supplemental Digital Content 1, which displays the patient 30 months after surgery, http://links.lww.com/PRSGO/A141). No obvious atrophy or dysfunction of the tongue was noted.
Fig. 3.

Smile at 30 months postoperatively.
Video Graphic 1.

See video, Supplemental Digital Content 1, which displays the patient 30 months after surgery, http://links.lww.com/PRSGO/A141.
DISCUSSION
Despite recent advances in microsurgical techniques, in total facial nerve reconstruction, there is no technique to reconstruct all distal branches without synkinesis. In addition to the unreliable fascicular pattern in the facial nerve trunk, aberrant axonal sprouts at the suture line and within the nerve graft increase misdirected reinnervation, even with interfascicular nerve grafting.7 Because synkinesis of the upper and lower face is especially disturbing for patients, use of multiple motor sources to differentially reanimate them is a good solution.2,3
In the present method, we chose the facial nerve as the main motor source for reanimation of the lower face. Voluntary and coordinated animation of the lower face was achieved without major synkinesis of the upper and lower face as shown in the postoperative video. Animation of the lower face is very important not only for emotional expressions such as a spontaneous smile, but also for daily activities such as eating and speaking. Although the results after hypoglossal or masseteric nerve transfer could be improved with rehabilitation therapy such as electromyographic or mirror visual biofeedback,8,9 it is more difficult to reestablish facial animation during emotional expression. In the upper face, which was reinnervated by the hypoglossal nerve, frontalis muscle tone and complete eye closure were restored. Although there was synkinesis between the frontalis muscle and orbicularis oculi muscle as well as absence of spontaneous blink, the patient has no complaints about them in the present case. When speaking and eating, the unpleasant movement of the upper face was minimal (See video, Supplemental Digital Content 1, which displays the patient 30 months after surgery, http://links.lww.com/PRSGO/A141).
In the lower face, the axonal supercharging technique with the hypoglossal nerve was also used.5,10 To minimize synkinesis between the upper and lower face, the anastomotic site on the hypoglossal nerve was different from that on the upper face and only 10% neurectomy was performed. Although there seems to be no obvious synkinesis, further studies will be needed to determine whether the technique positively contributes to the outcome.
CONCLUSIONS
Two interpositional nerve grafts can differentially reanimate the upper and lower face with 2 different motor sources, minimizing synkinesis between them. Reanimation of the lower face with the facial nerve can achieve voluntary and coordinated reanimation, whereas reanimation of the upper face with the hypoglossal nerve can restore frontalis muscle tone and eye closure. Our method may serve as a good alternative to conventional techniques that use only the facial or hypoglossal nerve.
PATIENT CONSENT
The patient provided written consent for the use of his image.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Kerrebijn JD, Freeman JL. Facial nerve reconstruction: outcome and failures. J Otolaryngol. 1998;27:183–186. [PubMed] [Google Scholar]
- 2.Stennert E. I. Hypoglossal facial anastomosis: its significance for modern facial surgery. II. Combined approach in extratemporal facial nerve reconstruction. Clin Plast Surg. 1979;6:471–486. [PubMed] [Google Scholar]
- 3.Volk GF, Pantel M, Streppel M, et al. Reconstruction of complex peripheral facial nerve defects by a combined approach using facial nerve interpositional graft and hypoglossal-facial jump nerve suture. Laryngoscope. 2011;121:2402–2405. doi: 10.1002/lary.22357. [DOI] [PubMed] [Google Scholar]
- 4.Terzis JK, Konofaos P. Nerve transfers in facial palsy. Facial Plast Surg. 2008;24:177–193. doi: 10.1055/s-2008-1075833. [DOI] [PubMed] [Google Scholar]
- 5.Tomita K, Hosokawa K, Yano K. Reanimation of reversible facial paralysis by the double innervation technique using an intraneural-dissected sural nerve graft. J Plast Reconstr Aesthet Surg. 2010;63:e535–e539. doi: 10.1016/j.bjps.2009.11.023. [DOI] [PubMed] [Google Scholar]
- 6.May M, Sobol SM, Mester SJ. Hypoglossal-facial nerve interpositional-jump graft for facial reanimation without tongue atrophy. Otolaryngol Head Neck Surg. 1991;104:818–825. doi: 10.1177/019459989110400609. [DOI] [PubMed] [Google Scholar]
- 7.Witzel C, Rohde C, Brushart TM. Pathway sampling by regenerating peripheral axons. J Comp Neurol. 2005;485:183–190. doi: 10.1002/cne.20436. [DOI] [PubMed] [Google Scholar]
- 8.Brudny J, Hammerschlag PE, Cohen NL, et al. Electromyographic rehabilitation of facial function and introduction of a facial paralysis grading scale for hypoglossal-facial nerve anastomosis. Laryngoscope. 1988;98:405–410. doi: 10.1288/00005537-198804000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Dalla Toffola E, Tinelli C, Lozza A, et al. Choosing the best rehabilitation treatment for Bell’s palsy. Eur J Phys Rehabil Med. 2012;48:635–642. [PubMed] [Google Scholar]
- 10.Fujiwara T, Matsuda K, Kubo T, et al. Axonal supercharging technique using reverse end-to-side neurorrhaphy in peripheral nerve repair: an experimental study in the rat model. J Neurosurg. 2007;107:821–829. doi: 10.3171/JNS-07/10/0821. [DOI] [PubMed] [Google Scholar]


