Abstract
Background
Effectiveness of pandemic plans and community compliance was extensively researched following the H1N1 pandemic. This systematic review examined community response studies to determine whether behavioural responses to the pandemic were related to level of knowledge about the pandemic, perceived severity of the pandemic and level of concern about the pandemic.
Methods
Literature databases were searched from March 2009 to August 2011 and included cross‐sectional or repeated population surveys undertaken during or following the H1N1 pandemic which reported on community response to the pandemic. Studies using population subgroups and other respiratory diseases were excluded, as were mathematical modelling and qualitative studies.
Results
Nineteen unique studies were included. Fourteen reported pandemic knowledge, 14 reported levels of concern and risk perception and 18 reported pandemic behaviours. Awareness of the pandemic was high, and knowledge was moderate. Levels of concern and risk were low moderate and precautionary behavioural actions lower than intentions. The most commonly reported factors influencing adopting recommended behaviours were increased risk perception and older age, increased pandemic knowledge and being female.
Conclusions
Important implications for future pandemic planning were identified. A remarkable lack of intercountry variability in responses existed; however, differences between populations within a single country suggest one‐size‐fits‐all plans may be ineffective. Secondly, differences between reported precautionary intentions and preventive behaviours undertaken may be related to people's perceived risk of infection.
Keywords: H1N1 influenza, pandemic, systematic review
Background
In 2009, the world experienced its first global influenza pandemic since the 1968 outbreak of Hong Kong flu. The 2009 influenza A (H1N1) pandemic tested national and international pandemic plans that had been in preparation for at least a decade. The resultant wave of research on the effectiveness of these pandemic plans provided an opportunity to examine what worked and where plans needed further refinement. This research has included a large number of surveys of the community response to the management of the pandemic. Understanding community compliance with public health measures and acceptance of prolonged use of these measures are important for revising and improving plans, especially with respect to those strategies that are used in the first months of a pandemic when there is much uncertainty about the virulence of the new disease, and before a vaccine can be developed and disseminated.
We conducted a systematic review of studies which had examined the community response to the H1N1 influenza A pandemic in 2009. We specifically sought to determine whether behavioural responses to the pandemic (including adoption of pharmaceutical and non‐pharmaceutical mitigation strategies) were related to level of knowledge about the pandemic, perceived severity of the pandemic and perceived level of concern about the pandemic.
Methods
Search strategies
We searched PubMed and MEDLINE in Process, MEDLINE, Excerpta Medica Database (EMBASE), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Database of Systematic Reviews, American College of Physicians (ACP) Journal Club, Database of Abstracts of Reviews of Effects (DARE), Cochrane Central Register for Controlled Trials (CCTR), Cochrane Methodology Register (CMR), Health Technology Assessment (HTA) and NHS Economic Evaluation Database from March 2009 to August 2011. Search terms used combinations of MESH and free‐text terms for human influenza, swine flu, H1N1, pandemic, community behaviour, attitudes, knowledge, survey, questionnaire, interview and computer‐aided telephone interview (CATI). The reference lists of all included studies were searched for any additional studies not identified via the main search (pearling), and excluded studies were tabulated with reasons for exclusion.
Inclusion and exclusion criteria
We included cross‐sectional or repeated population surveys undertaken during or following the 2009 influenza A (H1N1) pandemic which reported on the community response to the H1N1 pandemic. We excluded studies of subgroups of the general public including health workers; studies of other types of influenza or respiratory disease pandemics (such as avian influenza or SARS); studies incorporating only mathematical modelling; and qualitative research studies. Only English language studies were included. Outcomes of interest were pandemic knowledge, concern, risk perception and recommended and precautionary behaviours. However, we did not include studies in which the main focus of the survey was the H1N1 vaccine (either vaccination intention or uptake) as this is the subject of two recent systematic reviews.1, 2 Studies in which vaccination intention or uptake was reported as part of a broader survey were included; however, we did not extract data (usually from regression analysis) identifying factors associated with vaccination intention or uptake as this replicates the work of the existing systematic reviews.
Data extraction and analysis
Data were extracted into a pre‐specified data extraction form by one researcher (JC) and checked by a second (RT). No data were suitable for statistical pooling or meta‐analysis. Instead, data were narratively synthesised and tabulated by outcome.
Critical appraisal
Included studies were critically appraised to identify factors which may have introduced bias or limited the generalizability of the results, including methods of selecting groups, adequacy of adjustment for confounding in correlational analysis, completeness of the dataset and risk of misclassification bias, according to the methods suggested by the National Health and Medical Research Council (Australia) and the National Institute for Health and Clinical Excellence (UK).3, 4
Results
We identified 60 potentially relevant articles for inclusion in the review. After examination of the full text, we excluded 36 articles; of these, 18 were studies of H1N1 vaccination intention or uptake. We included 19 unique studies after identifying duplicate publications (two studies were reported altogether in six separate papers) (Figure 1).
Figure 1.
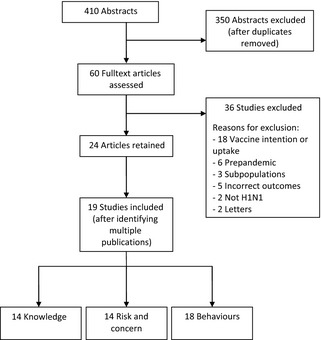
Flow chart of study inclusions.
Included studies were undertaken across a wide range of cultural settings including Australia (n = 5), the US (n = 4), the UK (n = 1), Hong Kong (n = 2), Saudi Arabia (n = 1), China (n = 1) and Mexico (n = 1), and several European countries (n = 5). There were 14 studies reporting pandemic knowledge, 14 reporting levels of concern and risk perception and 18 reporting pandemic behaviours including nine which reported use or intended use of pharmaceuticals (antivirals and vaccines). Included studies differed substantially in the methods of data collection from large computer‐aided telephone interviews of a representative sample of the population (n = 11), to online or web‐based surveys of existing panels of participants (n = 5) and to opportunistic surveys of members of the public in public spaces such as shopping centres (n = 1). There is no standardised survey of pandemic knowledge, attitudes and behaviours. Although there was substantial overlap in the domains of interest that were surveyed in the included studies, there were substantial differences between surveys in how the domains were explored. Questions were framed differently, combinations of domains differed between surveys and the scoring of domains, especially for levels of concern and risk were not standard. None of the included studies used a method to verify self‐reported data. As a consequence, there was considerable heterogeneity between surveys in the size of effects. A particular issue that may have affected the response to these surveys was the timing of the data collection in terms of the spread of the H1N1 pandemic and other factors that may have affected respondents' perceptions of risk and subsequent behaviours. Unfortunately, the data were not reported in such a way that this could be accounted for in statistical pooling of the results. Many different factors were included in correlational analysis. However, there was little consistency between studies. Overall, we judged that the included studies were at moderate risk of bias (Table 1).
Table 1.
Included studies
| Authors | N | PR (%) | Data source | Risk of bias | Outcomes reported |
|---|---|---|---|---|---|
|
Aburto14
Mexico May–Jun 2009 |
2666 | 80–87 | Random household cluster sampling | Low | K, B |
|
Balkhy5
Saudi Arabia Sep 2009 |
1548 | 97 | Shopping malls | Moderate | K, B, RP/C |
|
Brown25
Australia Jul–Aug 2009 |
1292 | 42 | Population phone survey | Moderate | B |
|
Bults12
Netherlands Apr–Aug 2009 |
Apr: 456 Aug: 934 |
59 63 79 |
Cross sectional online survey | Low‐moderate | K, B, RP/C |
|
Eastwood10
Australia Aug–Sep 2009 |
830 | 72 | Population phone survey | Low | K, B, RP/C |
|
Gilles21
Switzerland Mar–Jun 2009 Mar–Jun 2010 |
Wave 1: 950 Wave 2: 601 |
NR (63% of sample in Wave 2) | Two‐wave longitudinal survey | Low | B |
|
Goodwin16
Malaysia & Europe Apr–May 2009 |
328 Malaysia: 200 Europe: 128 |
M: 90 E:NR | Internet or paper based survey | High | K, B, RP/C |
|
Ibuka6
United States Apr–May 2009 |
1290 | 3 | Online panel survey | Moderate‐high | B, RP/C |
|
Kamate7
India Jul–Aug 2009 |
791 | 95 | Random population survey | High | K, B, RP/C |
|
Kiviniemi24
United States Oct–Nov 2009 |
807 | 24 | Population phone survey | Moderate | B, RP/C |
|
Lau11
Hong Kong Jul 2009 |
301 | 80 | Population phone survey | Moderate | K, RP/C |
|
Lau13
Hong Kong May–Jun 2009 |
999 | 62 | Population phone survey | Moderate | K, B, RP/C |
|
Lin15
China Nov 2009–Mar 2010 |
10 669 | 46 | Random household cluster sampling | Low | K, B, RP/C |
|
Marshall8
Australia Aug–Sep 2009 |
1961 | 65 | Population phone survey | Low | K, B, RP/C |
|
Maurer19
United States March 2010 |
3917 | 74 | Population phone survey | Low | K, RP/C |
|
Prati23
Italy Feb 2010 |
1010 | 25 | Population phone survey | Moderate | B |
|
Quinn17
United States Jun–Jul 2009 |
1543 | 62 | Online research panel | Low | RP/C |
|
Rubin18
United Kingdom May 2009 |
997 | NR | Population phone survey | Low | B, RP/C |
|
Seale9
Australia May 2009 |
620 | 85 | Face to face or online | Moderate | K, RP/C |
|
Seale20
Australia Sep–Oct 2009 |
627 | 47 | Face to face | Moderate | K, B, RP/C |
|
Setbon22
France Dec 2009 |
1003 | 46 | Population phone survey | Low‐moderate | B |
K, knowledge; B, behaviour; RP/C, risk perception/concern; PR, participation rate; NR, not reported.
Lau (2010a) includes Lau, Nelson, Yeung (2010) & Lau, Nelson, Choi et al. (2009); Lau (2010b) includes Lau, Griffiths et al. (2010), Lau, Griffiths, Choi (2009) & Lau, Griffiths, Choi (2010); Eastwood (10) includes Eastwood et al., (10).
Bults (2011); surveys conducted in April and June were random samples, and the August survey used participants from either April or June surveys as a follow‐up. Those who responded to survey in April or June but did not participate in the follow‐up in August were excluded from further analysis.
Pandemic knowledge
Pandemic awareness
Awareness of the swine flu pandemic was high, as might be expected, with over 85% of respondents in four studies having heard of H1N1 or swine flu.6, 7, 8, 9
Knowledge of H1N1
Level of knowledge about H1N1 in general and transmission in particular was moderate (Table 2). In three studies, between 30% and 51% of respondents were able to respond correctly to more than two‐thirds of knowledge items.5, 10, 11 In two studies (one conducted in Saudi Arabia and the other in Australia), <15% of respondents were able to respond correctly to all or more than 75% of knowledge items.5, 10 However, in one study from the Netherlands,12 knowledge of H1N1 was higher, with more than 85% of respondents able to correctly respond to more than two‐thirds of knowledge items. In this time series study, this outcome improved over time such that by August of 2009, the proportion of respondents had increased from 85% (as at April of 2009) to over 95%.
Table 2.
Knowledge about H1N1 (n/N,% respondents)
| Study | Low knowledge | Mod knowledge | High knowledge | Incorrect knowledge | Correct knowledge |
|---|---|---|---|---|---|
|
Aburto14
N = 2666 |
– | – | – | <1·5% handling pork products spread infection |
>85% contact with infected people >30% contact with infected surfaces Approximately 10% eating with infected utensils |
|
Balkhy5
N = 1548 |
<10/17 correct, 44% |
10–12/17 correct, 51% |
13+ correct, 5% | – | – |
|
Bults12
N = 1868 |
– | ≥4/7 correct, 88%–96% | – | – | – |
|
Eastwood10
N = 830 |
2/4 correct, 31% | 3/4 correct, 49% | 4/4 correct, 15% | – | – |
|
Goodwin16
N = 328 |
– | – | – |
38/148, 26% Seasonal flu different symptoms to H1N1 |
95/148, 64% Seasonal flu kills >100 K worldwide |
|
Kamate7
N = 791 |
– | – | – |
648/791, 82% Swine flu not equiv to H1N1 474/791, 60% Unaware of length of illness |
144/791, 18% Swine flu caused by H1N1 385/791, 49% Swine flu caused by pigs |
|
Lau11
N = 301 |
1/3 correct, 20% | 2/3 correct, 29% | 3/3 correct, 51% |
178/301, 59·1% At least one incorrect belief about transmission |
123/301, 41% No incorrect beliefs about transmission |
|
Lau13
N = 999 |
– | – | 3/3 correct, 60% |
62% At least one incorrect belief about transmission |
– |
|
Lin15
N = 10 669 |
– | – | – | 30% believed H1N1 could be transmitted via food |
8063/10 669, 76% virus transmitted via coughs 6599/10 669, 62% virus transmitted face‐to‐face 2383/10 669, 22% virus transmitted indirect hand contact 2854/10 669 (27%) virus transmitted by handshake |
|
Marshall8
N = 1961 |
23% don't know what a pandemic is | – | – | 35% incorrect definition of pandemic | 42% correct definition of pandemic |
Percentages are those extracted exactly from included studies.
In two Hong Kong studies,11, 13 over 50% of participants were able to identify 3/3 modes of transmission correctly; however, in both studies, around 60% of respondents also named at least one incorrect mode of transmission. In another study conducted in Mexico,14 more than 85% of respondents were able to correctly identify contact with infected people as a primary source of disease transmission, and <1·5% of people erroneously believed contact with pork products would transmit H1N1. In one Australian study,8 42% of respondents knew the correct definition of pandemic, but 35% provided an incorrect definition. In another study,15 76% of respondents knew at least one correct transmission route, but 30% of respondents believed the virus could be transmitted via food.
Knowledge of prevention methods
Knowledge of prevention methods was reasonable. In one Australian study,10 nearly all respondents knew that hand washing prevented infection. However, in two other studies8, 16 (one Australian and one conducted in Malaysia and Europe), far fewer respondents spontaneously named these methods. In one study, avoiding infected others was the method reported by most respondents,8 and in another study, over a quarter of respondents suggested wearing a mask.16
Level of concern and perception of risk posed by H1N1 pandemic
Level of concern and anxiety about the pandemic
The majority of respondents in seven studies reported either low or moderate levels of concern about the H1N1 pandemic (Table 3).8, 10, 12, 13, 16, 17, 18 In all of these studies, the proportion of respondents reporting high or very high levels of concern ranged from 2%18 to 36%.12 In one Saudi Arabian study,5 the reverse pattern was observed: over half of respondents were very concerned, and only 11% were not at all concerned. When mapped over time (Suppl file 1), level of concern typically reduced between March 2009 and August 2009; however, due to the nature of the data, we were unable to statistically pool findings according to data collection period, and therefore, our figure (Suppl file 1) should be interpreted with caution as it points merely to patterns in the data.
Table 3.
Pandemic concern and disease severity (n/N,% respondents)
| Study | Level of concern or anxiety about the pandemic | ||
|---|---|---|---|
| Not at all concerned (Low) | Somewhat concerned (Moderate) | Very concerned (High) | |
|
Bults12
N = 1868a |
– | – |
36% in April 2009 (n = 456) 19% in June 2009 (n = 478) 14% in Aug 2009 (n = 934) |
|
Balkhy5
N = 1548 |
11% | 34·7% | 54·3% |
|
Goodwin16
N = 328 |
160/328, 50% | 82/328, 25% | 83/328, 26% |
|
Eastwood10
N = 830 |
648/830, 78% | 168/830, 17% | 44/830, 5% |
|
Lau13
N = 999 |
– | – | 100/999, 10·1% |
|
Marshall8
N = 1961 |
– | Mean concern (1–10 ascending scale) 4·8 (95% CI 4·6–4·9) | – |
|
Quinn17
N = 1543 |
– | 46·2%a | – |
|
Rubin18
N = 997 |
– | 237/997, 23·8% | 21/997, 2·1% |
| Perceived severity of disease | |||
|---|---|---|---|
| Not at all severe/moderately severe | Severe/very severe | Don't know/not sure | |
|
Bults12
N = 1868a |
– |
80% in April 2009 (n = 456) 67% in June 2009 (n = 478) 39% in Aug 2009 (n = 934) |
– |
|
Eastwood10
N = 830 |
645/830, 78% | 168/830, 20% | 17/830, 2% |
|
Kamate7
N = 791 |
38·4% | 34·5% | 27·1% |
|
Lau11
N = 301 |
189/301, 62·8% | 76/301, 25·2% | 36/301, 12% |
|
Maurer19
N = 3917 |
6·2% | 71·1% | – |
|
Quinn17
N = 1543 |
874/1524, 58% | 650/1524, 42% | – |
|
Seale20
N = 627 |
234/627, 37·3% | 275/627, 43·9% | 42/627, 6·7% |
% reporting concerned about swine flu.
Percentages are those extracted exactly from included studies.
Perceived severity of disease
In three studies,10, 11, 17 H1N1 was perceived as not severe or moderately severe by the majority of respondents (Table 3). In two studies,19, 20 the majority of respondents regarded H1N1 as either severe or very severe. In one Indian study,7 about as many respondents regarded H1N1 as severe/very severe as considered, it was not at all or moderately severe. Perceived severity of H1N1 declined over time (Suppl file 2).
Perception of personal risk of contracting H1N1
In nine studies, the majority of respondents regarded their personal vulnerability to contracting H1N1 to be low or moderate (Table 4).6, 10, 11, 12, 13, 17, 20, 21 However, between 5% and 25% of respondents in six studies regarded their personal risk of contracting H1N1 as high or very high.9, 10, 11, 12, 13, 20
Table 4.
Perception of risk posed by H1N1 (n/N,% respondents)
| Study | Low riska | Medium risk | High riska |
|---|---|---|---|
| Personal risk of contracting H1N1 | |||
|
Bults12
N = 1868a |
– | – |
5% in April 2009 (n = 456) 5% in June 2009 (n = 478) 15% in Aug 2009 (n = 934) |
|
Eastwood10
N = 830 |
– | – | 211/830, 25·4% |
|
Gilles21
N = 1551 |
Mean 2·29 [0·75] (likert 1–5 scale) | – | – |
|
Ibuka6
N = 1290 |
Approximately 37% on perceived likelihood scale (0–100%) | – | – |
|
Lau11
N = 301 |
237/301, 77·7% | – | 67/301, 22·3% |
|
Lau13
N = 999 |
– | – | 8·6%–11·7% |
|
Quinn17
N = 1543 |
1273/1543, 85·8% | – | – |
|
Seale9
N = 620 |
235/620, 37·9% | 201/620, 32·4% | 133/620, 21·4% |
|
Seale20
N = 627 |
332/627, 52·9% | 175/627, 27·9% | 109/627, 17·4% |
| Community risk from H1N1 | |||
|
Lau11
N = 301 |
– | – |
Family 30/301 (10%) General public 35/301 (12%) |
|
Lau13
N = 999 |
– | – |
Family 8·7% General public 12·5% |
|
Quinn17
n = 1543 |
1148/1543, 75·3% | – | – |
|
Seale20
N = 627 |
272/627, 43·4% | 247/627, 39·4% | 99/627, 15·8% |
Low risk: very unlikely/unlikely to be at risk, high risk: likely/very likely to be at risk.
Percentages are those extracted exactly from included studies.
Perception of community risk posed by H1N1
The threat posed to the community was regarded as low or moderate by the majority of respondents in four studies.11, 13, 17, 20 In three studies, between 8% and 16% of respondents regarded the risk to the community from H1N1 to be high (See Table 4).
Precautionary and recommended behaviours in response to the pandemic
Non‐pharmaceutical mitigation strategies
A range of behavioural intentions to undertake protective behaviours and precautions (listed in Table 5) was reported in the included studies, and in general, intentions to undertake protective behaviours and precautions were expressed by a large proportion of respondents in each study (ranging from 30% to 99%). However, there were significantly lower proportions of respondents reporting that they had actually undertaken any of the recommended behaviours and precautions (Table 5). In nine studies,5, 7, 10, 12, 13, 14, 15, 18, 20, 22 the proportion of respondents, who reported washing hands more frequently, ranged from 28% to 90%. This compares with two studies of behaviour intention which reported 62·5%23 and 98·5%24 of respondents intended to comply with recommendations to wash hands. Similarly, in five studies, between 50% and 96% of respondents reported intending to stay home from work with symptoms of H1N1.8, 10, 12, 24, 25 However, in six studies, the proportion of respondents reporting that they stayed home from work ranged from <1% to 26%.5, 6, 7, 14, 18, 22 Similar patterns were observed for most of the behavioural outcomes reported.
Table 5.
Non‐pharmaceutical mitigation strategies reported (n/N,% respondents)
| Study | Wash hands | Cover coughs & sneezes | Purchase or wear mask | Disinfect objects | Avoid infected others | Avoid crowded places | Stay home from work | Keep kids home from school | Avoid public transport |
|---|---|---|---|---|---|---|---|---|---|
| Intention to undertake behaviours | |||||||||
| Brown25 N = 1292 | – | – | – | – | – | – | 95% | – | – |
|
Bults12
N = 1868a |
– | – |
70% Apr 09 57% Jun 09 44% Aug 09 |
– |
89% Apr 09 81% Jun 09 72% Aug 09 |
76% Apr 09 66% Jun 09 59% Aug 09 |
61% Apr 09 53% Jun 09 50% Aug 09 |
– | – |
|
Eastwood10
N = 830 |
– | – |
601/830 (72·4%) |
– | – |
687/830 (82·8%) |
797/830 (96%) |
– | – |
|
Goodwin16
N = 328 |
– | – |
96/328 (29%) |
– | – | – | – | – | – |
|
Kiviniemi24
N = 807 |
98·5% | 98·4% | – | – | – | – | 87·7% | – | – |
|
Marshall8
N = 1961 |
– | – | 81·1% | – | – | – | 94·1% | 73% | – |
|
Prati23
N = 1010 |
631/1010 (62·5%) |
428/1010 (42·4%) |
– |
322/1010 (31·9%) |
– |
339/1010 (33·6%) |
– | – | – |
| Behaviours undertaken | |||||||||
|
Aburto14
N = 837b |
89·3% | 21·5% | 63·4% | – | 10·4% | 19·5% | 9%c | – | – |
|
Balkhy5
N = 1601 |
893/1601 (57·7%) |
588/1601 (38%) |
870/1601 (56·2%) |
– | – | – |
398/1601 (25·7%) |
– | – |
|
Bults12
N = 1868a |
‐ | ‐ |
0·4% Apr 09 0·7% Jun 09 2% Aug 09 |
– |
4% Jun 09 10% Aug 09 |
3% Apr 09 3% Jun 09 8% Aug 09 |
– | – | – |
|
Eastwood10
N = 830 |
387/830 (46·6%) |
231/830 (27·8%) |
72/830 (8·7%) |
103/830 (12·4%)d |
– | – | – | – | – |
|
Goodwin16
N = 328 |
– | – |
25/328 (8%) |
– | – | – | – | – |
116/328 (36%) |
|
Ibuka6
N = 1290 |
– | – | – | – | – | – | 8% | – | – |
|
Kamate7
N = 791 |
432/791 (54·6%) |
– | – |
288/791 (36·5%) |
– |
375/791 (47·4%) |
208/791 (26·3%) |
128/791 (16·2%) |
256/791 (32·4%) |
|
Lau13
N = 999 |
415/999 (41·5%)e |
– |
215/999 (21·5%) |
– | – | 54·6% | – | – | – |
|
Lin15
N = 10669 |
6049/ 10 669 (56·9%) |
– | – | – |
6119/10 669 (57·4%) |
4574/10 669 (42·9%) |
– | – | – |
|
Rubin18
N = 997 |
278/989 (28·1%) |
169/976 (17·3%) |
35/955 (3·7%) |
5/732 (0·7%) |
2/486 (0·4%) |
20/710 (2·8%) |
|||
|
Seale20
N = 627 |
303/627 (48·3%) |
– | – |
195/627 (31·1%) |
– |
54/627 (8·6%) |
– |
21/627 (3·3%) |
46/627 (7·3%) |
|
Setbon22
N = 1003 |
59·7% | – | 3·3% | – | – | 14·6% | 1·5% | – | 12·8% |
April 2009 (n = 456); June 2009 (n = 478); Aug 2009 (n = 934).
Data for Mexico City only.
Staying away from other people.
More than usual time cleaning the house.
Wash hands >10 times per day.
Percentages are those extracted exactly from included studies.
Pharmaceutical mitigation strategies (use of antivirals and vaccines)
Intention to accept either antiviral medication or a vaccine against H1N1 (when it became available) was reported by more than 50% of respondents in seven studies (Suppl file 3).6, 7, 8, 10, 12, 23, 24 In one US study,17 far fewer respondents indicated intention to vaccinate (8·7%) but in this study, respondents were asked whether they would accept a new, as yet unapproved, vaccine. As with other behavioural outcomes, many fewer respondents reported either buying or using antivirals (<2% of respondents in two studies, one Australian and one conducted in the Netherlands)8, 12 or receiving the H1N1 vaccine when it was available (11–16% in two studies).15, 24
Associations between outcomes and demographic and H1N1 factors
Table 6 summarises the relationship between study outcomes and demographic and H1N1 factors. There was a great deal of consistency in the direction of these findings; however, the actual adjusted odds ratios differed significantly probably due to the variability of outcome measures used and differences in which factors were included in multivariate regression analyses. Consequently, these data are not reported here.
Table 6.
Associations between H1N1 outcomes and demographic and H1N1 factors
| Knowledge | Awareness | Concern | Behaviour | Intentions | Accept antiviral | Pay for antiviral | |
|---|---|---|---|---|---|---|---|
| Demographic factors | |||||||
| Female | ↓7 | ↑10, 13 ↓5 | ↑6 | ↑6 | |||
| Age | ↑↑8 | ↑↑6 | ↑↑5, 10, 13 | ↑↑12 | ↑↑6 | ↑↑6 | |
| Education | ↑↑7, 15 | ↓↑5 | ↑↑5, 10 | ||||
| Employed | ↑7 | ↑13 | |||||
| SES | ↑↑8 | ||||||
| Previous ILI | ↑10 | ||||||
| Married | ↑13 | ||||||
| Household size | ↑↑6 | ↑↑6 | |||||
| Being black (US) | ↓17 | ||||||
| H1N1 factors | |||||||
| Knowledge | ↑↑5, 13 | ↑↑6 | ↑↑6 | ||||
| Risk perception | ↑↑13, 14 | ↑↑10, 12, 13, 14, 18 | ↑↑12 | ↑↑17 | ↑↑6 | ||
| Concern | ↑↑13 | ↓↑17 | |||||
↑↑, direct relationship between outcome and factor; ↓↑, inverse relationship between outcome and factor; ↓, outcome worse if factor present; ↑, outcome better if factor present.
Pandemic knowledge or awareness was higher for older age groups, higher post‐secondary education, higher socioeconomic status and for employed people. In one Indian study, women had lower pandemic knowledge than men.7 Gender differences in knowledge were not reported in any of the other studies. Level of concern and perception of risk were directly related; however, level of education was inversely related to level of concern in one study (Saudi Arabia).5 The most commonly reported factors influencing actually adopting recommended pandemic behaviours were increased risk perception and older age group followed by increased pandemic knowledge and being female. Other factors associated with increased pandemic behaviours were higher post‐secondary education, higher socioeconomic status, being employed, having had a previous influenza‐like illness, being married, and having a higher level of concern. One study reported that women were less likely to adopt recommended behaviours and precautions.5 Older age and increased risk perception were also associated with intention to adopt recommended behaviours. Likelihood of accepting (or purchasing) antivirals was associated with increased age, large household size, higher pandemic knowledge and increased risk perception. Increased acceptance of, and/or willingness to pay for, antivirals in two US studies was associated with being female, Hispanic or Caucasian as opposed to African American, older age, larger household size, higher pandemic knowledge and increased risk perception.6, 17
Discussion
This review of community surveys carried out during or after the 2009 influenza A (H1N1) pandemic included studies from 14 countries, including many developed and some developing countries. Despite significant differences between countries in pandemic planning for and experience with the disease, these surveys resulted in quite a consistent picture of the community response to the pandemic. Awareness of the pandemic was high (much higher than similar surveys conducted prior to the 2009 pandemic)26, 27 but specific pandemic knowledge was only moderate. While respondents were aware of a number of means of transmission and methods for preventing the spread of infection, incorrect beliefs were also held by a number of people across some countries.7, 11, 13 Overall, concerns about the pandemic, its perceived severity and perceived personal and community vulnerability to infection were low to moderate and moderated over the first 6 months of the pandemic presumably as more became known about the low virulence and severity of the virus. However, up to one‐third of respondents in two surveys had a high or very high level of concern.5, 12 The first of these was a small online survey conducted in the Netherlands very early in the pandemic when very little was known about the virulence of the virus.12 The second was a study conducted in Saudi Arabia in late 20095 and may have reflected local concerns related to the influx of visitors associated with the impending Haj pilgrimage.
A wide range of precautionary and preventive behaviours was reported; however, reported intentions to comply with pandemic advice were typically much higher than actual behaviours undertaken, in particular for more onerous or economically costly behaviours such as purchase of antiviral drugs, stockpiling of food and staying home from work. A number of respondent characteristics were associated with the study outcomes which enable the identification of what might be termed an ‘active responder’: older, more highly educated and more socially advantaged people were more likely to have good pandemic knowledge and to undertake recommended behaviours. Older people were also more likely to be concerned about the pandemic and to rate the severity of the illness more highly, and this in turn was related to adoption of recommended behaviours.
Local circumstances and timing are also important in the uptake of preventive behaviours. For example, the surveys describing the lowest (UK)18 and highest (Mexico)14 values for reported hand washing were both undertaken at the same time (May 2009) but the first death in the UK was not until mid‐June, and pandemic impact had been slight, whereas, by this time, in Mexico, there had been numerous deaths attributed to swine flu, and Mexican authorities had implemented social distancing measures for several weeks (see Suppl file 4 for 2009 country case counts). We would conclude that the patterns of behaviour are likely linked, early in the pandemic, to the potentially high degree of risk posed by the virus and, in the longer term, to the mild nature of the pandemic. Our findings suggest that even the best and most clearly communicated plans will be interpreted by the community in the light of how events actually work out and that people will balance the messages and directives provided by health authorities with a personal risk assessment based on real‐life experience. In revising pandemic plans in preparation for the next pandemic, thought could be given to whether it is possible to convert more of the population to ‘active responder’ status but also to more timely responses to rapidly changing understanding and knowledge. Officials involved in pandemic planning may also need to give some consideration to whether they should attempt to increase hazard awareness28 to motivate mitigation behaviours, and how this might impact later perceptions of the early warnings, if the pandemic ends up being less severe than first thought.
It is also apparent that subpopulations within a community (for example younger people or those with lower levels of education) may be slower to respond. At a minimum, future pandemic planning should take into account that plans cannot be one‐size‐fits‐all and should incorporate communication and strategies tailored to local circumstances and to different demographic groups within populations. As the less active responders are also more likely to experience a higher burden of disease, particular emphasis should be placed on plans which access these more vulnerable groups and should emphasise the risk to these groups of not being vaccinated.29
With respect to the nature of the preventive behaviours adopted, it is clear that hand washing was consistently valued and used as a precautionary strategy across populations. In contrast, masks were not used unless there was a perception of high risk. This was the case in Saudi Arabia and Mexico, both of which reported high use of masks, possibly because of the timing of events described above. The only Asian country surveyed about mask use was Hong Kong with 21% indicating that they had used a mask. This compares well with a survey during the early part of the SARS epidemic in Hong Kong when the risk of SARS was seen as moderate.30 In that case, as the number of SARS cases climbed, the percentage of the population reporting that they were wearing masks also increased, probably also related to consistent messages from health authorities about the importance of wearing a mask and masks and the widespread availability of masks. Our findings support the notion that for an individual to adopt protective behaviours, in a pandemic, there need to be both clear and consistent messages and support from health authorities and individual perceptions of high risk from the infectious threat. Similarly, in two recent systematic reviews about the use of vaccines during the H1N1 pandemic, intentions and uptake of vaccinations were often dependent on individual perceptions of risk or their level of concern about contracting the virus.1, 2
Limitations of the review
As with any systematic review, the findings of this review are limited by the nature of the available data. Methodological quality of the included studies was moderate but the data were not sufficiently similar to be pooled statistically. Heterogeneity was introduced by differences in sampling strategy, outcome measures and analyses. There is no standardised survey for the community response to an influenza pandemic, although arguably, given the consistency in direction of findings in this review, there is a set of common outcomes from which a global pandemic response survey could be developed. Preparation of such a survey in advance of a pandemic is essential as pandemics emerge without warning, and both research and practice responses must be rapid. Such a survey or measure would also facilitate cross‐country comparisons and help to pinpoint gaps in pandemic planning and communication plans more quickly and reliably.
Conclusion
Four key implications for communication and community response during a pandemic arose from this review. First, the lack of intercountry variability in responses: people across cultural and geographical boundaries responded surprisingly similarly in terms of levels of concern and intended adherence to precautionary and protective measures. Second, within‐country heterogeneity where different groups in each community respond differently suggests that a one‐size‐fits‐all approach to pandemic planning would not be effective. Third, intention to perform behaviour does not always translate into action; pandemic planning should understand and incorporate this. Lastly, the lack of translation of intention to action may be related to the perceived mildness of the H1N1 pandemic.10, 12 This suggests that people respond more strongly to factors present in their everyday environment than to official messages about what a pandemic is and what they should do. Understanding and integration of these findings are very important to the success of future pandemic planning and communication, particularly in the early stages of the pandemic when severity may not be fully apparent but contagion already an issue.
Supporting information
Suppl file 1: Level of concern about the pandemic over time (determined by date of data collection).
Suppl file 2: Perceptions of disease severity over time (determined by date of data collection).
Suppl file 3: Pharmaceutical mitigation strategies reported (n/N, % respondents).
Suppl file 4: Included studies country of origin H1N1 case counts for 2009.
Acknowledgements
This work was supported by the National Health and Medical Research Council [Grant Number 626867]. Author HM is supported by an NHMRC Career Development Fellowship No. 1016272.
Tooher(2013) Community knowledge, behaviours and attitudes about the 2009 H1N1 Influenza pandemic: a systematic review. Influenza and Other Respiratory Viruses 7(6), 1316–1327.
References
- 1. Nguyen T, Holdt Henningsen K, Brehaut JC, Hoe E, Wilson K. Acceptance of pandemic influenza vaccine: a systematic review of surveys of the general public. Infect Drug Resist 2011; 4:197–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bish A, Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol 2010; 15:797–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. NHMRC guidelines . Available at http://www.nhmrc.gov.au/guidelines/resources-guideline-developers (Accessed 1 May 2011).
- 4. NIHCE UK guidelines . Available at http://www.nice.org.uk/aboutnice/howwework/developingniceclinicalguidelines/clinicalguidelinedevelopmentmethods/GuidelinesManual2009.jsp (Accessed 3 June 2011).
- 5. Balkhy HH, Abolfotouh MA, Al‐Hathlool RH, Al‐Jamah M. Awareness, attitudes, and practices related to the swine influenza pandemic among the Saudi public. BMC Infect Dis 2010; 10:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ibuka Y, Chapman GB, Meyers LA, Li M, Galvani AP. The dynamics of risk perceptions and precautionary behaviour in response to 2009 (H1N1) pandemic influenza. BMC Infect Dis 2010; 10:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kamate SK, Agrawal A, Chaudhary H, Singh K, Mishra P, Asawa K. Public knowledge, attitude and behavioural changes in an Indian population during the Influenza A (H1N1) outbreak. J Infect Dev Ctries 2010; 4:7–14. [DOI] [PubMed] [Google Scholar]
- 8. Marshall H, Tooher R, Collins J et al Awareness, anxiety, compliance: community perceptions and response to the threat and reality of an influenza pandemic. Am J Infect Control 2012; 40:270–272. [DOI] [PubMed] [Google Scholar]
- 9. Seale H, McLaws ML, Heywood AE et al The community's attitude towards swine flu and pandemic influenza. Med J Aust 2009; 191:267–269. [DOI] [PubMed] [Google Scholar]
- 10. Eastwood K, Durrheim D, Butler M et al Responses to pandemic (H1N1) 2009, Australia. Emerg Infect Dis 2010; 16:1211–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lau JTF, Yeung NCY, Choi KC, Cheng MYM, Tsui HY, Griffiths S. Factors in association with acceptability of A/H1N1 vaccination during the influenza A/H1N1 pandemic phase in the Hong Kong general population. Vaccine 2010a; 28:4632–4637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bults M, Beaujean DJMA, deZwart O et al Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: results of three consecutive online surveys. BMC Public Health 2011; 11:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lau JTF, Griffiths S, Choi KC, Tsui HY. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect Dis 2010b; 10:139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aburto NJ, Pevzner E, Lopez‐Ridaura R et al Knowledge and adoption of mitigation efforts in Mexico during the 2009 H1N1 Pandemic. Am J Prev Med 2010; 39:395–402. [DOI] [PubMed] [Google Scholar]
- 15. Lin Y, Huang L, Nie S et al Knowledge, Attitudes and Practices (KAP) related to the pandemic (H1N1) 2009 among Chinese general population: a telephone survey. BMC Infect Dis 2011; 11:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Goodwin R, Haque S, Neto F, Myers LB. Initial psychological responses to Influenza A H1N1 (“Swine Flu”). BMC Infect Dis 2009; 9:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Quinn SC, Kumar S, Freimouth VS, Kidwell K, Musa D. Public willingness to take a vaccine or drug under emergency use authorisation during the 2009 H1N1 pandemic. Biosecur Bioterror 2009; 7:275–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rubin GJ, Amlot R, Page L, Wessely S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. BMJ 2009; 339:b2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maurer J, Uscher‐Pines L, Harris KM. Perceived seriousness of seasonal and A (H1N1) influenzas, attitudes toward vaccination, and vaccine uptake among U.S. adults: does the source of information matter? Prev Med 2010; 51:185–187. [DOI] [PubMed] [Google Scholar]
- 20. Seale H, Heywood AE, McLaws M et al Why do I need it? I am not at risk! Public perceptions towards the pandemic (H1N1) 2009 vaccine. BMC Infect Dis 2010; 10:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gilles I, Bangerter A, Cleménce A et al Trust in medical organisations predicts pandemic (H1N1) 2009 vaccination behaviour and perceived efficacy of protection measures in the Swiss public. Eur J Epidemiol 2011; 26:203–210. [DOI] [PubMed] [Google Scholar]
- 22. Setbon M, Le‐Pape M, Letroublon C, Caille‐Brillet A, Raude J. The public's preventive strategies in response to the pandemic influenza A/H1N1 in France: distribution and determinants. Prev Med 2011; 52:178–181. [DOI] [PubMed] [Google Scholar]
- 23. Prati G, Pietrantoni L, Zani B. Compliance with recommendations for pandemic influenza H1N1 2009: the role of trust and personal beliefs. Health Educ Res 2011; 26:761–769. [DOI] [PubMed] [Google Scholar]
- 24. Kiviniemi MT, Ram PK, Kozlowski LT, Smith KM. Perceptions of and willingness to engage in public health precautions to prevent 2009 H1N1 influenza transmission. BMC Public Health 2011; 11:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Brown LH, Aitken P, Leggat PA, Speare R. Self‐reported anticipated compliance with Physician advice to stay home during pandemic (H1N1) 2009: results from the 2009 Queensland Social Survey. BMC Public Health 2010; 10:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Marshall H, Ryan P, Roberton D, Street J, Watson M. Pandemic influenza and community preparedness. Am J Public Health 2009; 99(Suppl 2):S365–S371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Eastwood K, Durrheim D, Francis JL et al Knowledge about pandemic influenza and compliance with containment measures among Australians. Bull World Health Organ 2009; 87:588–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sandman P. What Kind of Risk Communication Does Pandemic Preparedness Require? Minneapolis, MN: CIDRAP Business Source, 2007. [Google Scholar]
- 29. Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine 2011; 29:6472–6484. [DOI] [PubMed] [Google Scholar]
- 30. Lau JTF, Yang X, Tsui H, Kim JH. Monitoring community responses to the SARS epidemic in Hong Kong: from day 10 to day 62. J Epidemiol Community Health 2003; 57:864–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Suppl file 1: Level of concern about the pandemic over time (determined by date of data collection).
Suppl file 2: Perceptions of disease severity over time (determined by date of data collection).
Suppl file 3: Pharmaceutical mitigation strategies reported (n/N, % respondents).
Suppl file 4: Included studies country of origin H1N1 case counts for 2009.


