Abstract
Background
Seasonal influenza activity varies with geography and time of year.
Objective
To describe how pandemic influenza A(H1N1)2009 [A(H1N1)pdm09] activity varied during the 2009–2010 pandemic.
Methods
We analyzed influenza virological data compiled by the World Health Organization from June 2009–August 2010. We calculated weekly proportions of A(H1N1)pdm09‐positive specimens out of all A(H1N1)pdm09‐positive specimens detected during the study period for each country. We compared parameters of pandemic activity (e.g., peak A[H1N1]pdm09 weekly proportion [peak activity], number of weeks between the 5th and 95th percentiles of A(H1N1)pdm09 cumulative weekly proportion [duration of activity]) between countries in temperate and tropical–subtropical regions. We quantified the proportion of A(H1N1)pdm09 out of all influenza A specimens by country and correlated it with countries' central latitudes.
Results
We analyzed data from 80 countries (47 temperate, 33 tropical–subtropical). The median proportion of cases identified during the peak week was higher in temperate (0·12) than in tropical–subtropical (0·09) regions (P < 0·01). The median duration of activity was longer in tropical–subtropical (27 weeks) than in temperate countries (20 weeks) (P < 0·01). In most temperate countries (98%), peak pandemic activity occurred during the fall–winter period. There was a positive correlation between country central latitude and proportion of A(H1N1)pdm09 out of all influenza A specimens (r: 0·76; P < 0·01).
Conclusions
The transmission of A(H1N1)pdm09 exhibited similarities with seasonal influenza transmission in that activity varied between temperate and tropical–subtropical countries and by time of year. Our findings suggest the potential utility of accounting for these factors during future pandemic planning.
Keywords: 2009 influenza A (H1N1), pandemic influenza, seasonality
Introduction
Seasonal influenza transmission varies throughout the world with time of year and region.1 The mechanisms behind influenza seasonality are not well understood; however, multiple factors, including virological, immunological, environmental, and social factors likely contribute to the observed seasonal patterns of influenza transmission.2, 3 These factors give rise to annual influenza epidemics during the winter months in Northern and Southern Hemisphere temperate climates.4 In tropical and subtropical climates, influenza activity may be detected throughout the year, although there is increasing evidence of a notable seasonal component to influenza activity in some tropical countries.3, 5
Pandemic influenza viruses can emerge at any time of year, but it is not clear whether the factors that drive yearly seasonal influenza transmission influence transmission of a novel virus to which the population has little immunity (resulting in increased population susceptibility, higher attack rates, and prolonged viral shedding in comparison with seasonal influenza). It has been postulated that there were seasonal variations in the transmission of pandemic influenza viruses during the 20th century, as they appeared to have had either a secondary or a tertiary wave of activity at the time of the historical influenza season.6, 7 The A(H1N1)pdm09 pandemic of 2009–2010 also demonstrated a seasonal component to transmission early during the pandemic, in the Americas.8 For example, surveillance during April to August 2009 pointed to higher rates of A(H1N1)pdm09 infection in Southern Hemisphere temperate countries, where the pandemic began at the time that seasonal influenza activity was expected.5, 9, 10
The A(H1N1)pdm09 pandemic provides a unique opportunity to study pandemic influenza transmission dynamics because there were more surveillance data from tropical and subtropical countries obtained during this pandemic than from any previous time in history.11 The objectives of our study are to describe the transmission patterns of the A(H1N1)pdm09 virus throughout the world and to identify whether they varied in relation to geography (i.e., latitude and climatic regions) and time of year when A(H1N1)pdm09 was first detected in relation to countries' historical influenza season. This knowledge could be useful for pandemic preparedness, as it might help identify the best timing for the implementation of public health interventions or the distribution of limited supplies during a pandemic.
Methods
We compiled laboratory‐confirmed influenza virological reports for the influenza A subtypes H3N2, seasonal H1N1, and A(H1N1)pdm09 from recognized sovereign states and other administrative regions (i.e., entities not formally recognized as sovereign states such as New Caledonia) around the world (all referred to as ‘countries’ from now on). The study period included the 62 weeks from June 11, 2009, to August 10, 2010, coinciding with the official start and end date of the pandemic period, as stated by the World Health Organization (WHO). Our data sources included virological influenza data obtained by WHO in FluNet11 as well as regional and national laboratory surveillance Web sites (e.g., http://www.euroflu.org, http://www.nicd.ac.za/). We analyzed influenza virological data from countries that reported laboratory‐confirmed influenza results for ≥70% of weeks in the study period and that reported >120 positive A(H1N1)pdm09 samples during the study period. We obtained 2010 World Population Projections and population density by country.12 In addition, we categorized countries by income groups according to World Bank classifications (high income, upper‐middle income, lower‐middle income and low income)13 to identify whether income groups were equally represented in our study (trend test).
We examined each country's influenza virological data by calculating the proportion of A(H1N1)pdm09‐positive specimens identified each week, out of all A(H1N1)pdm09‐positive samples tested during the study period (weekly proportion). We then graphed the weekly proportions for each country to help us visualize the countries' influenza activity. We used locally weighted scatterplot smoothing (LOESS) to create smoothed curves of influenza activity for each country (Figure 1). Using the smoothed data, we determined the following parameters of A(H1N1)pdm09 activity for each country: week of first detection of the A(H1N1)pdm09 virus, the proportion of A(H1N1)pdm09 specimens detected during the week of highest activity (peak activity), number of weeks from first A(H1N1)pdm09 detection until the week of peak activity (time to peak), number of weeks when 90% of A(H1N1)pdm09 specimens were detected (i.e., time encompassing the 5th and 95th percentiles of cumulative A(H1N1)pdm09 weekly proportion), and number of waves of A(H1N1)pdm09 activity during the study period. We defined a wave as the time period including an increase and subsequent decrease in A(H1N1)pdm09 activity and including a peak week of activity. A peak week was defined as a week during which the LOESS‐smoothed proportion of A(H1N1)pdm09 activity was higher than the week immediately preceding it and immediately following it, and when the weekly proportion was at least 1% higher than in the troughs on either side. For example, Costa Rica showed only one wave of pandemic activity (Figure 1); the proportion of A(H1N1)pdm09‐positive specimens identified during the peak week (week 27) was 6·7%, and it was 0·5% during the trough week that followed (week 43). The smaller increases observed later in the study period did not meet the peak definition. This method helped us to avoid counting spurious fluctuations as peaks and was selected after evaluating a range of thresholds.
Figure 1.
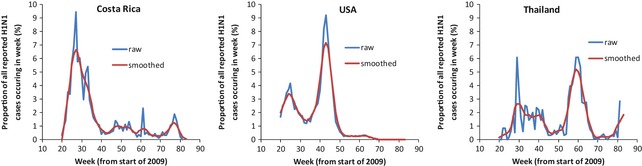
Examples of the weekly proportion of influenza A(H1N1)pdm09‐positive specimens using locally weighted scatterplot smoothing technique in three selected countries.
Countries were then classified into climatic regions by using their central latitude (i.e., the latitude at the center of the country): Northern and Southern temperate (central latitude ≥|30°|), subtropical (central latitude |23·5–29·9| and tropical (central latitude ≤|23·4°|).14 We also classified countries into two other categories: those where A(H1N1)pdm09 was first detected during the start of the country's historical influenza season and those where A(H1N1)pdm09 was detected at any other time. The start of the historical influenza season was defined as the time encompassing the 6 weeks before the start of the influenza season and the first half of the season. The timing of country's historical influenza season (i.e., typical month of start and end of the season) was only known for a subgroup of countries (17 in temperate regions and 22 in tropical–subtropical regions) based on data from a prior study.15 In the case of China, data from mainland temperate and subtropical regions, Chinese Taipei and Hong Kong SAR, were analyzed separately.
We quantified the number of weeks between initial detection of A(H1N1)pdm09 in Mexico and the United States (third week in April 2009) and the first report of A(H1N1)pdm09 in every country. We then calculated the median number of weeks of first A(H1N1)pdm09 detection for each continent. We compared the parameters of A(H1N1)pdm09 activity described above (peak activity, time to peak, number of weeks between the 5 and 95th percentiles of cumulative A(H1N1)pdm09 weekly proportion, and number of waves) between countries in temperate and tropical–subtropical climatic regions. We also compared the same parameters of A(H1N1)pdm09 activity between countries where A(H1N1)pdm09 was first detected during the start of countries' historical influenza season and those where A(H1N1)pdm09 was introduced at any other time of the year. This was made for the subgroup of 39 countries for which we had data on the timing of the historical influenza season, as described above.
In addition, we explored whether there was a correlation between the following variables: peak activity and the proportion of cases within the 12‐week period around the peak; latitude and peak activity; latitude and number of weeks from detection of A(H1N1)pdm09 to countries' peak week; latitude and the proportion of total A(H1N1)pdm09‐positive specimens out of total influenza A‐positive specimens during the pandemic. Lastly, we calculated the minimum doubling time of A(H1N1)pdm09 in each country using the following formula: doubling time = ln(2)/ln(weekly proportion of A(H1N1)pdm09/proportion in the previous week). We compared the mean doubling time in Northern Hemisphere temperate, Southern Hemisphere temperate, and tropical–subtropical countries.
We used sas 9.2 (SAS Institute Inc., Cary, NC, USA) to conduct Wilcoxon rank sum tests and Kruskal–Wallis tests to compare continuous data, chi‐square tests to compare categorical data, Spearman's test to identify correlations, and Cochran–Armitage test to identify trends.
Results
Description of the study population and geographical spread
From surveillance databases, we had access to data from 128 countries. Eighty of these countries provided sufficient laboratory‐confirmed influenza data to meet our inclusion criteria and were included in our analyses (Figure 2) (Table S1). The 80 countries have a cumulative population of 5·5 billion persons or 80% of the world's population. Among these 80 countries, 47 (59%) were classified as temperate (45 from the Northern Hemisphere and two from the Southern Hemisphere) and 33 (41%) were tropical–subtropical. As there were only five subtropical countries, we grouped them with the tropical countries for all analyses. Among 213 countries that had been classified by the World Bank into income group classifications, our sample countries included 31 (45%) of 69 high‐income countries, 21 (44%) of 48 upper‐middle‐income countries, 17 (30%) of 56 lower‐middle‐income countries, and 8 (20%) of 40 low‐income‐countries (test for trend, P < 0·01).
Figure 2.
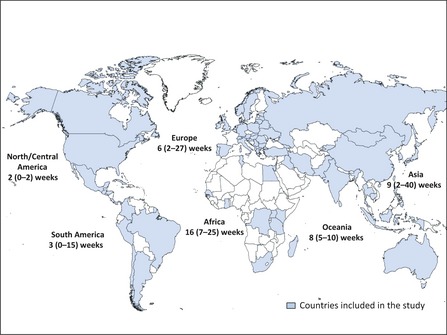
Map of the world highlighting the countries included in our analyses and the number of weeks from the time of first world detection of influenza A(H1N1)pdm09 (third week of April, 2009), until the median week of detection in each continent.
The median number of weeks from first detection of A(H1N1)pdm09 in Mexico and the United States (third week in April 2009) until first detection in countries from each continent was 2 weeks (range 0–20) in North/Central America, 3 weeks (range 0–15) in South America, six weeks (range 2–21) in Europe, 8 weeks (range 5–10) in Oceania, 9 weeks (range 2–40) in Asia, and 16 weeks (range 7–25) in Africa (P < 0·01) (Figure 2).
Parameters of A(H1N1)pdm09 activity by climatic region and latitude
The median proportion of A(H1N1)pdm09 specimens detected during the peak week (peak activity) was significantly higher in temperate (0·12) than in tropical–subtropical (0·09) regions (P < 0·01) (Table 1). We found fewer median number of weeks between the 5th and 95th percentiles of the A(H1N1)pdm09 weekly proportion in temperate countries (20 weeks [13–24 interquartile range (IQR)]) than in tropical–subtropical countries (27 weeks [17–44 IQR], P < 0·01) (Table 1). We also identified a positive correlation between peak activity and the proportion of cases within the 12‐week period around the peak (r s = 0·79, P < 0·01) (Figure 3A). The median number of weeks from first detection of A(H1N1)pdm09 to peak week was 25 weeks (20–27 IQR) in temperate and 9 weeks (6–16 IQR) in tropical–subtropical countries (P < 0·01), consistent with a positive correlation between country latitude and number of weeks from country detection of A(H1N1)pdm09 to country peak week (r s = 0·46, P < 0·01) (Figure 3B).
Table 1.
Parameters of influenza A(H1N1)pdm09 activity by climatic region
| Parameters of A(H1N1)pdm09 activity | Temperate countries (n = 47) | Tropical and subtropical countries (n = 33) | P value |
|---|---|---|---|
| Peak A(H1N1)pdm09 weekly proportiona (peak activity) | 0·12 (0·09–0·14) | 0·09 (0·07–0·12) | <0·01 |
| No. of weeks between the 5th and 95th percentiles of cumulative weekly proportiona | 20 (13–24) | 27 (17–44) | <0·01 |
| No. of weeks from first detection to peak weeka | 25 (20–27) | 9 (6–16) | <0·01 |
| Countries with >1 wave, no. (%) | 16 (34) | 10 (30) | 0·81 |
Wilcoxon rank sum tests and Kruskal–Wallis tests were used to compare continuous data, chi‐square tests to compare categorical data.
Median (interquartile range).
Figure 3.
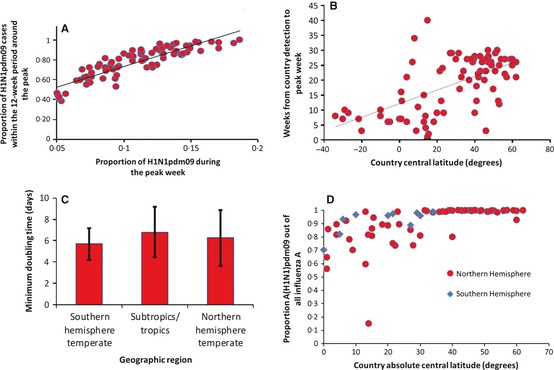
Correlation between countries' influenza A(H1N1)pdm09 weekly proportion in the peak week (peak activity) and the proportion of cases within the 12‐week period around the peak (A). Correlation between country latitude and number of weeks from country detection of influenza A(H1N1)pdm09 until countries' peak week (B). Mean influenza A(H1N1)pdm09 minimum doubling times by geographical region (C). Correlation between countries' central latitude and the proportion of influenza A(H1N1)pdm09‐positive specimens, out of all influenza A‐positive specimens (D).
In 44 (98%) of 45 Northern Hemisphere temperate countries, the peak week occurred within the 12 weeks from the 2nd week of October to the 4th week of December 2009, a time corresponding to the autumn–winter period in the region (Figure 4). This time typically also corresponds to the early part of the countries' historical influenza season. The peak week of the two Southern Hemisphere temperate countries also clustered within their autumn–winter period. However, among the tropical countries, the peak week occurred over a period of 47 weeks, extending from the 3rd week of May 2009 to the 4th week of March 2010. There were 26 countries with more than one wave of activity, but there was no significant difference in the number of waves, by climatic region (Table 1). The mean A(H1N1)pdm09 minimum doubling time was not significantly different in Northern Hemisphere temperate (6·3 days [2·6 SD]), Southern Hemisphere temperate (5·7 days [1·5 SD]), and tropical–subtropical countries (6·2 days [2·3 SD]) (P = 0·4) (Figure 3C).
Figure 4.
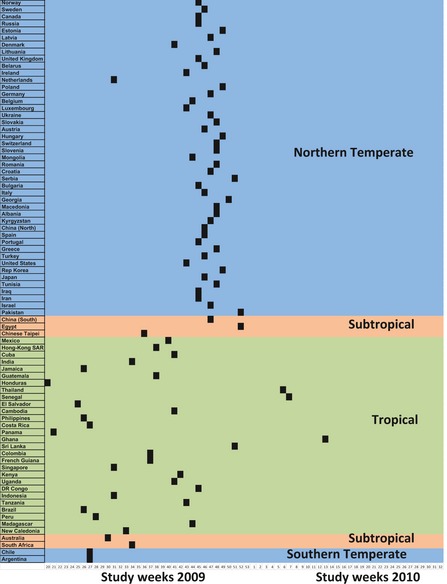
Time course of the peak influenza A(H1N1)pdm09 weekly proportion (peak week) by country and climatic region. The black bars represent the peak week of H1N1pdm09 virus activity for each country during the pandemic.
We found a positive correlation between countries' central latitude and countries' proportion of total A(H1N1)pdm09‐positive specimens out of total influenza A‐positive samples for the pandemic period (r s = 0·76, P < 0·01) (Figure 3D).
Parameters of A(H1N1)pdm09 activity in relation to the start of the historical influenza season
We had data on the timing of the historical influenza season for a subgroup of 39 countries. The median number of weeks from first A(H1N1)pdm09 detection until peak week was 8 weeks (6–13 IQR) in countries where A(H1N1)pdm09 was first identified during the start of their historical influenza season. The median number of weeks from first detection until peak week was 25 weeks (20–27 IQR) in countries where first detection occurred at any other time of the year (P < 0·01). Three of 14 (21%) countries had more than one wave of A(H1N1)pdm09 where A(H1N1)pdm09 was introduced during the start of the historical influenza season, compared with 12 of 25 countries (48%) where it was introduced during any other time, although this difference was not statistically significant (P = 0·17). There was no statistically significant association between peak activity and the median number of weeks between the 5th and 95th percentiles of A(H1N1)pdm09 weekly proportion, among countries where A(H1N1)pdm09 was introduced during the start of the historical influenza season compared with countries where it was introduced at any other time of the year (Table 2).
Table 2.
Parameters of influenza A(H1N1)pdm09 activity in countries where influenza A(H1N1)pdm09 was first detected during the start of countries' historical influenza season and countries where it was first detected at a different time of the year
| Parameters of A(H1N1)pdm09 activity | First detection of A(H1N1)pdm09 | P value | |
|---|---|---|---|
| First half of historical influenza season (n = 14) | Different time of the year (n = 25) | ||
| Peak A(H1N1)pdm09 weekly proportiona (peak activity) | 0·12 (0·09–0·15) | 0·08 (0·07–0·12) | 0·17 |
| No. of weeks between the 5th and 95th percentiles of cumulative weekly proportiona | 24 (14–46) | 25 (18–30) | 0·86 |
| No. of weeks from first detection to peak weeka | 8 (6–13) | 25 (20–27) | <0·01 |
| Countries with >1 wave, no. (%) | 3 (21) | 12 (48) | 0·17 |
Wilcoxon rank sum tests and Kruskal–Wallis tests were used to compare continuous data, chi‐square tests to compare categorical data.
Median (interquartile range).
Discussion
During the 2009–2010 pandemic, A(H1N1)pdm09 activity was associated with latitude; specifically, our analysis demonstrated that temperate countries had higher intensity (higher median peak) but shorter duration of A(H1N1)pdm09 activity (fewer weeks between the 5th and 95th percentiles) than tropical–subtropical countries. The positive correlation between peak activity and the proportion of cases within the 12‐week period around the peak demonstrates that countries with higher peak incidence had more concentrated waves overall. These findings are consistent with our initial hypothesis, as we anticipated that pandemic influenza would show similar behavior to seasonal influenza viruses and readily transmit, during a shorter time period, in temperate climate countries, and demonstrate less intense activity spread out over a longer period of time in tropical climate countries.
We also demonstrate that in Northern and Southern Hemisphere temperate countries, the peak week of pandemic activity was most frequently identified within a 12‐week period during their autumn–winter season (the time of year when seasonal influenza is typically circulating), while in tropical countries, the timing of the peak was heterogeneously distributed over a 47‐week period. These findings may explain why the median number of weeks from first A(H1N1)pdm09 detection until reaching peak week was longer in temperate climate countries, as 45 of 47 temperate countries in our study were in the Northern Hemisphere, and they were experiencing spring when A(H1N1)pdm09 was introduced (a time of year when influenza activity is low in these climatic regions). It is also consistent with our finding that countries where A(H1N1)pdm09 was introduced during the start of their historical influenza season had less time until peak A(H1N1)pdm09 activity was reached, and although not statistically significant, these countries also had lower probabilities of having a second wave of pandemic activity. As the timing of the historical influenza season corresponds to the time of year when the environmental, social, or biological factors responsible for influenza seasonality create a setting for enhanced influenza virus transmission,2, 3 we suggest that these factors might also have a role in the transmission of novel influenza viruses.
The positive correlation between countries' central latitudes and their proportion of A(H1N1)pdm09‐positive specimens out of all influenza A‐positive specimens maybe the result of the emergence of A(H1N1)pdm09 when little to no seasonal influenza was circulating in northern hemisphere temperate countries; hence, A(H1N1)pdm09 would comprise a higher proportion of influenza infections. In contrast, in tropical countries, with more year‐round influenza transmission and seasonal influenza circulating, A(H1N1)pdm09 would comprise a lower proportion of infections.
Our findings have implications for pandemic preparedness, as they could inform the timing when supplies, services, and public health interventions might be most needed during a pandemic. The time from first identification of a novel influenza strain until it is detected in every continent can be weeks, and countries that are not in the epicenter of a pandemic should consider using this time to implement early interventions that may help further delay the spread of pandemic viruses, as recommended by WHO.16 Countries in temperate climates might need to plan for the highest levels of activity during the autumn–winter (despite the fact that some might face an initial wave of activity close to the introduction of the pandemic virus); this is supported by findings from previous pandemics in countries like the United States., where peaks of activity occurred during the autumn/winter months.6, 7, 17 Countries in tropical climates can expect influenza activity to be spread out over a longer period of time, with no evident pattern in the timing of their peak activity. Other investigators have made efforts to use influenza information obtained through current surveillance systems along with morbidity and mortality data from previous pandemics to generate models that may help estimate the burden of a future pandemic.18 There were also several contributions from mathematical modeling during the A(H1N1)pdm09 pandemic.19 Some models have even looked at the role of seasonality in previous pandemics as well as the potential role in future pandemics.20 Our findings suggest the potential utility of accounting for latitude and historical timing of the influenza season when modeling the behavior of pandemic viruses.
This study has several important limitations. Although we analyzed data from 80 countries containing approximately 80% of the world's population, these data might not be representative of all regions within each country, and our data may not be globally representative. This is especially true of lower‐income countries, as these were under‐represented in comparison with higher‐income countries. The number of samples tested, laboratory methods used, sampling criteria, and reporting practices varied by country which might limit the comparability of data between countries. Timing of the historical influenza season was known for less than half of the countries in this study. We were unable to compare the absolute incidence of A(H1N1)2009 between countries, as data available to us did not include rates of illness.
Conclusion
The transmission of pandemic influenza A(H1N1)2009 exhibited important similarities with the transmission of seasonal influenza, despite the fact that it was a novel virus to which the majority of the population had little preexisting immunity. In comparison with tropical and subtropical countries, we found that countries in temperate climates had higher peaks, shorter durations of pandemic activity, and higher proportions of A(H1N1)pdm09 among influenza A‐positive samples. The time of year likely played a role in temperate climate countries, as the peak of pandemic activity occurred during the fall–winter period in most countries. These findings may be useful in future pandemic preparedness planning.
Conflict of interests
The authors declare no conflict of interests.
Disclaimer
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the Centers for Disease Control and Prevention or the institutions with which the authors are affiliated.
Supporting information
Table S1. Countries included in analyses along with their central latitude and climatic region.
Acknowledgements
The authors would like to recognize all of the National Influenza Centers, the WHO Global Influenza Surveillance and Response System and other laboratories who reported their data on FluNet or otherwise made it available to the global community. The free and transparent sharing of data is critical to improving our corporate understanding of influenza transmission dynamics and our ability to appropriately and effectively respond to future pandemics. This work was supported by the Centers for Disease Control and Prevention, the World Health Organization, and Imperial College of London.
Storms et al (2013) Worldwide transmission and seasonal variation of pandemic influenza A(H1N1)2009 virus activity during the 2009–2010 pandemic. Influenza and Other Respiratory Viruses 7(6), 1328–1335.
References
- 1. Dowell SF, Ho MS. Seasonality of infectious diseases and severe acute respiratory syndrome‐what we don't know can hurt us. Lancet Infect Dis 2004; 4:704–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lofgren E, Fefferman NH, Naumov YN, Gorski J, Naumova EN. Influenza seasonality: underlying causes and modeling theories. J Virol 2007; 81:5429–5436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tamerius J, Nelson MI, Zhou SZ, Viboud C, Miller MA, Alonso WJ. Global influenza seasonality: reconciling patterns across temperate and tropical regions. Environ Health Perspect 2011; 119:439–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Finkelman BS, Viboud C, Koelle K, Ferrari MJ, Bharti N, Grenfell BT. Global patterns in seasonal activity of influenza A/H3N2, A/H1N1, and B from 1997 to 2005: viral coexistence and latitudinal gradients. PLoS ONE 2007; 2:e1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moura FE. Influenza in the tropics. Curr Opin Infect Dis 2010; 23:415–420. [DOI] [PubMed] [Google Scholar]
- 6. Cox NJ, Subbarao K. Global epidemiology of influenza: past and present. Annu Rev Med 2000; 51:407–421. [DOI] [PubMed] [Google Scholar]
- 7. Juzeniene A, Ma LW, Kwitniewski M et al The seasonality of pandemic and non‐pandemic influenzas: the roles of solar radiation and vitamin D. Int J Infect Dis 2010; 14:e1099–e1105. [DOI] [PubMed] [Google Scholar]
- 8. Lessler J, dos Santos T, Aguilera X, Brookmeyer R, Group PITW, Cummings DA. H1N1pdm in the Americas. Epidemics 2010; 2:132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oliveira W, Carmo E, Penna G et al Pandemic H1N1 influenza in Brazil: analysis of the first 34,506 notified cases of influenza‐like illness with severe acute respiratory infection (SARI). Euro Surveill 2009; 14: Available at http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19362 (Accessed 14 May 2012) [DOI] [PubMed] [Google Scholar]
- 10. Baker M, Kelly H, Wilson N. Pandemic H1N1 influenza lessons from the southern hemisphere. Euro Surveill 2009; 14: Available at http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19370 (Accessed 14 May 2012) [DOI] [PubMed] [Google Scholar]
- 11. WHO . FluNet Website. Available at http://www.who.int/influenza/gisrs_laboratory/flunet/en/ (Accessed 15 December 2010).
- 12. Division UNP. World Population Prospects: The 2008 Revision Population Database. Available at http://esa.un.org/unpd/wpp/unpp/panel_population.htm (Accessed 1 January 2011).
- 13. Bank TW. World Development Indicators & Global Development Finance. Available at http://data.worldbank.org/data-catalog/world-development-indicators (Accessed 15 October 2010).
- 14. Mobilgistix . Average Latitude & Longitude of Countries. Available at http://web.archive.org/web/20080822000330/http://www.mobilgistix.com/Resources/GIS/Locations/average-latitude-longitude-countries.aspx (Accessed 19 January 2011).
- 15. Azziz Baumgartner E, Dao CN, Nasreen S et al Seasonality, timing, and climate drivers of influenza activity worldwide. J Infect Dis 2012; 206:838–846. [DOI] [PubMed] [Google Scholar]
- 16. WHO . Pandemic influenza preparedness and response. WHO guidance document. 2009: Available at http://www.who.int/influenza/resources/documents/pandemic_guidance_04_2009/en/ (Accessed 21 March 2011). [PubMed]
- 17. Glezen WP. Emerging infections: pandemic influenza. Epidemiol Rev 1996; 18:64–76. [DOI] [PubMed] [Google Scholar]
- 18. Monto AS, Comanor L, Shay DK, Thompson WW. Epidemiology of pandemic influenza: use of surveillance and modeling for pandemic preparedness. J Infect Dis 2006; 194(Suppl. 2):S92–S97. [DOI] [PubMed] [Google Scholar]
- 19. Van Kerkhove MD, Ferguson NM. Epidemic and intervention modelling – a scientific rationale for policy decisions? Lessons from the 2009 influenza pandemic. Bull World Health Organ 2012; 90:306–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shi P, Keskinocak P, Swann JL, Lee BY. Modelling seasonality and viral mutation to predict the course of an influenza pandemic. Epidemiol Infect 2010; 138:1472–1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Countries included in analyses along with their central latitude and climatic region.


