Abstract
Purpose
An earlier randomized controlled trial found that two middle school sexual education programsda risk avoidance (RA) program and a risk reduction (RR) programddelayed initiation of sexual intercourse (oral, vaginal, or anal sex) and reduced other sexual risk behaviors in ninth grade. We examined whether these effects extended into 10th grade.
Methods
Fifteen middle schools were randomly assigned to RA, RR, or control conditions. Follow-up surveys were conducted with participating students in 10th grade (n = 1,187; 29.2% attrition).
Results
Participants were 60% female, 50% Hispanic, and 39% black; seventh grade mean age was 12.6 years. In 10th grade, compared with the control condition, both programs significantly delayed anal sex initiation in the total sample (RA: adjusted odds ratio [AOR], .64, 95% confidence interval [CI], .42–.99; RR: AOR, .65, 95% CI, .50–.84) and among Hispanics (RA: AOR, .53, 95% CI, .31–.91; RR: AOR, .82, 95% CI, .74–.93). Risk avoidance students were less likely to report unprotected vaginal sex, either by using a condom or by abstaining from sex (AOR: .61, 95% CI, .45–.85); RR students were less likely to report recent unprotected anal sex (AOR: .34, 95% CI, .20–.56). Both programs sustained positive impact on some psychosocial outcomes.
Conclusions
Although both programs delayed anal sex initiation into 10th grade, effects on the delayed initiation of oral and vaginal sex were not sustained. Additional high school sexual education may help to further delay sexual initiation and reduce other sexual risk behaviors in later high school years.
Keywords: Adolescents, Sexual behavior, Intervention studies, Health education, Computer-based, Urban populations
Many United States (U.S.) adolescents engage in sexual behaviors that may increase their risk of teen pregnancy and sexually transmitted infections (STIs). Nationally, 47% of high school students have had sex; of these, 40% did not use a condom at last intercourse and 15% had four or more partners [1]. These behaviors may lead to pregnancy and STIs, both of which disproportionately affect minority youth. For instance, Hispanics experience higher teen birth rates than other racial/ethnic groups [2], and African-Americans represent almost two thirds of human immunodeficiency virus (HIV) diagnoses among youth [3]. Early sexual debut, which is more common in minority students than in whites [4], increases the risk of these adverse health outcomes [5,6]. Evidence indicates that sexual health education may help reduce health disparities related to teen pregnancy and STIs.
School-based programs represent an effective strategy to reduce risky sexual behavior [7–9]. Several middle school interventions have shown effects on delayed sexual initiation and reduced risky sexual behavior into ninth grade. These interventions have used both risk avoidance (RA) (abstinence education or abstinence until marriage) [10] and risk reduction (RR) (abstinence-plus or comprehensive sex education) approaches [11,12]. However, few studies have evaluated the sustained impact of middle school sexual health education programs into 10th grade or beyond (i.e., ≥36 months’ follow-up), showing only limited long-term impact. For example, evaluation of My Choice, My Future!, an RA program composed of three curricula delivered in eighth, ninth, and 10th grades, respectively, implemented among predominantly white, non-Hispanic youth, found no sustained significant behavioral impact 4–5 years post-baseline, although some positive psychosocial outcomes were sustained [13]. Evaluation of ReCapturing the Vision, an RA program targeting mostly eighth-grade African-American and Hispanic high-risk girls, found no sustained significant behavioral impact 4–5 years post-baseline, although some significant positive psychosocial outcomes were sustained [13]. Similarly, evaluation of Focus on Youth in the Caribbean, an RR program for Bahamian youth delivered in sixth to eighth grade, found no sustained significant behavioral impact but some positive sustained psychosocial outcomes in 10th grade [14]. Thus, we have a limited understanding of how students retain and apply sexual health education messages received in prepubescence as they enter adolescence. Questions remain whether the retention and application of sexual health education messages received in middle school differ by prevention approach or by sociodemographic characteristics (i.e., by race/ethnicity or gender).
In an earlier randomized, controlled trial, we evaluated the impact of two middle school sexual health education programs delivered in seventh and eighth grades—an RA program and an RR program—on behavioral and psychosocial outcomes in ninth grade [15]. Relative to controls, the RR program delayed sexual initiation (oral, vaginal, or anal sex) in the overall sample. Subgroup analyses showed significant delay in sexual initiation among females and African-Americans. The RR students also reduced unprotected sex at last intercourse, past 3 months’ frequency of anal sex, and unprotected vaginal sex. The RA program delayed sexual initiation among Hispanics and reduced unprotected sex at last intercourse in the overall sample. However, RA students reported a significantly greater number of recent vaginal sex partners relative to controls. Both programs positively affected several psychosocial outcomes related to sexual behavior.
In this follow-up study, we examined whether these behavioral and psychosocial effects extended into 10th grade, to provide additional insight into the long-term impact of these programs. We hypothesized that students who received either the RA or RR intervention in middle school would significantly delay any sexual initiation into 10th grade and report less risky sexual behaviors compared with students in the control condition.
Methods
Study design and participants
Seventh graders from 15 middle schools in a large, urban, south-central U.S. school district were recruited into a randomized, controlled trial in 2006–2007. Schools were randomly assigned to one of three conditions (RA, RR, and control) before the baseline assessment. Overall, 60% of students returned a parental consent, 83% (n = 1,873) with permission to participate; of these, 93% (n = 1,742) provided assent and completed the baseline survey. There were no significant differences in recruitment across study conditions. Additional recruitment information is published elsewhere [15].
Tenth-grade surveys were completed by 1,233 students (29.2% attrition) between October 2009 and July 2010. Students who were lost to follow-up were more likely to be older (p < .001), male (p < .01), and sexually experienced at baseline (p < .001), with no significant differences across conditions.
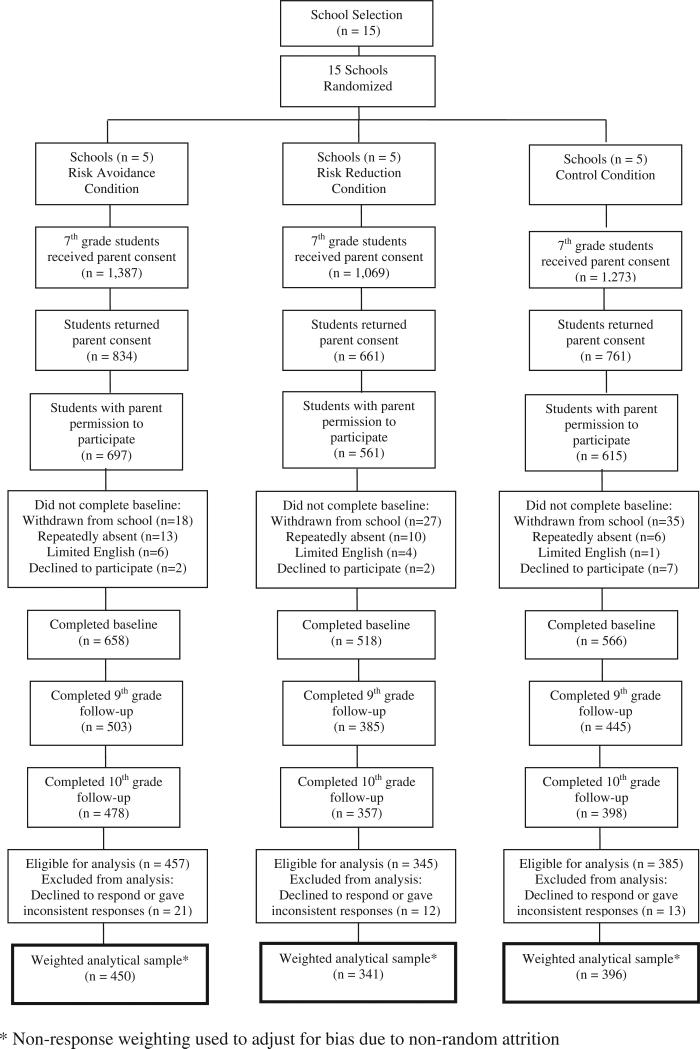
Students who completed baseline and 10th-grade surveys were eligible for analysis. We excluded 46 students because of missing or inconsistent responses, which left 1,187 students for analysis (Figure 1). This study was approved by institutional review boards at the University of Texas Health Science Center and the Centers for Disease Control and Prevention, and by the school district's Office of Research.
Figure 1.
Progress of participants through study and final weighted analytical sample.
Interventions
The RA and RR programs were based on an existing middle school sexual health education program: It's Your Game. Keep It Real (IYG) [11], which is grounded in social cognitive models [16,17]. Both programs targeted psychosocial factors related to healthy relationships and sex (e.g., self-efficacy and beliefs). Both programs were composed of 24 50-minute lessons, with 12 lessons delivered in seventh grade and 12 lessons in eighth grade [15]. Seventy-one percent of RA lessons (17 of 24) contained essentially identical activities to RR lessons but were framed to convey an abstinence-until-marriage message rather than an abstinence-until-older message (age and relationship not spec-ified). Both programs integrated group-based classroom activities with individual computer-based activities, some of which were tailored by gender or sexual experience, journaling, and parent-child take-home assignments. Both programs were implemented by trained facilitators. Neither included booster sessions or additional resources beyond eighth grade. Additional details about both programs are provided elsewhere [15].
The two programs differed in several key aspects. Mainly, RA activities targeted beliefs about the benefits of abstinence until marriage, per federal abstinence education guidelines [18], and incorporated elements of future orientation and character development, whereas RR activities promoted abstinence until older, responsibility, and self-respect, and included computerized skill-based activities to practice steps for correct condom use.
Students in the control condition received the district's regular sexual health education in seventh or eighth grade. Four to 6 hours of instruction included information-based activities on puberty, reproduction, and HIV/STI transmission, excluding information on abstinence until marriage or condoms and contraception.
Data collection
Survey data were collected using audio-computer-assisted self-interviews on laptop computers [15]. Surveys were conducted in a quiet location (e.g., school library); headphones were provided to enhance confidentiality. Five waves of assessments were conducted: one in the fall and spring of seventh grade and one in eighth, ninth, and 10th grades (40 months post-baseline). The current analysis used data from the seventh- and 10th-grade surveys only.
Behavioral measures
For students who were sexually inexperienced at baseline, we assessed the impact of both interventions on delayed sexual initiation by 10th grade (a composite variable composed of initiation of oral, vaginal, or anal sex) and delayed initiation of oral, vaginal, and anal sex specifically. Other sexual behaviors assessed included unprotected sex at last vaginal intercourse, number of lifetime sexual partners, and other recent (i.e., in the past 3 months) behaviors including frequency of oral, vaginal, and anal sex; frequency of vaginal or anal sex without a condom; and number of sexual partners. All measures have been used previously with urban youth [11,12,19].
Psychosocial measures
Items assessed intermediate factors targeted by the RA or RR interventions. These included behavioral knowledge, perceived self-efficacy, behavioral and normative beliefs, behavioral intentions, environmental factors, and character traits (i.e., future orientation). These measures are described elsewhere [15]. All measures have been previously used with urban youth [11,12,19].
Covariates
Sociodemographic factors recognized to influence sexual behavior (i.e., gender, age, race/ethnicity, and family structure) [20–22] were included in analytical models. Race/ethnicity was collapsed into three categories: African-American, Hispanic, and other, including white, Asian, Native American, and non-Hispanic multiracial youth.
Analysis approach
Nonresponse weighting was used to adjust for bias resulting from nonrandom attrition. Significant baseline differences between treatment conditions were observed for all sociodemographic factors (excluding gender) and for sexual behavior. At baseline, control condition students were more likely to be sexually experienced than either RA or RR students (Table 1). All subsequent analyses controlled for these baseline differences via inclusion of covariates in the regression models.
Table 1.
Baseline comparability of risk avoidance, risk reduction, and control conditions at 10th-grade follow-up among the analyzed cohort (n = 1,187)a
| Demographic characteristics | RA (n = 450) |
RR (n = 341) |
C (n = 396) |
Total sample (n = 1,187) |
RA versus C p-value | RR versus C p-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||
| Female | 279 | 62.0 | 195 | 57.1 | 233 | 59.0 | 707 | 59.5 | .38 | .61 |
| Race/ethnicity | .07 | .04 | ||||||||
| African-American | 164 | 36.5 | 122 | 35.9 | 174 | 44.1 | 461 | 38.9 | ||
| Hispanic | 224 | 49.9 | 186 | 54.5 | 179 | 45.3 | 590 | 49.7 | ||
| Other | 61 | 13.6 | 33 | 9.6 | 42 | 10.6 | 136 | 11.5 | ||
| Age, years (mean [SD]) | 446 | 12.6 (.76) | 338 | 12.7 (.72) | 394 | 12.7 (.81) | 1,178 | 12.6 (.77) | .01 | .34 |
| Family structure | <.01 | .10 | ||||||||
| Living with two parents | 163 | 37.1 | 102 | 30.7 | 98 | 25.3 | 362 | 31.3 | ||
| Living with one parent and one step-parent | 175 | 39.9 | 152 | 45.8 | 212 | 54.8 | 538 | 46.5 | ||
| Living with one parent | 40 | 9.1 | 20 | 5.9 | 23 | 6.0 | 83 | 7.1 | ||
| Living with someone other than parent | 61 | 13.9 | 58 | 17.6 | 54 | 13.0 | 173 | 15.0 | ||
| Ever had sex (any sex) | 38 | 8.9 | 30 | 9.3 | 63 | 17.2 | 130 | 11.8 | <.01 | <.01 |
| Sex in past 3 months (any sex) | 20 | 4.5 | 15 | 4.3 | 48 | 12.1 | 83 | 7.0 | <.01 | <.01 |
| Type of sex: | ||||||||||
| Oral sexb | ||||||||||
| Ever had oral sex | 18 | 4.1 | 11 | 3.5 | 33 | 9.0 | 62 | 5.5 | .05 | <.01 |
| Oral sex in past 3 months | 8 | 1.7 | 8 | 2.4 | 27 | 6.7 | 42 | 3.6 | <.01 | <.01 |
| Vaginal sexc | ||||||||||
| Ever had vaginal sex | 33 | 7.5 | 27 | 8.2 | 59 | 15.8 | 119 | 10.3 | <.01 | <.01 |
| Vaginal sex in past 3 months | 18 | 4.0 | 14 | 4.0 | 43 | 10.8 | 74 | 6.3 | <.01 | <.01 |
| Vaginal sex without condom in past 3 months | 6 | 1.3 | 9 | 2.5 | 21 | 5.4 | 36 | 3.0 | <.01 | .05 |
| Anal sexd | ||||||||||
| Ever had anal sex | 10 | 2.3 | 7 | 2.1 | 17 | 4.2 | 34 | 3.0 | .11 | .09 |
| Anal sex in past 3 months | 3 | .7 | 4 | 1.2 | 13 | 2.3 | 21 | 1.7 | .01 | .04 |
| Anal sex without condom in past 3 months | 3 | .7 | 4 | 1.2 | 13 | 3.3 | 21 | 1.7 | .07 | .47 |
C = control; RA = risk avoidance; RR = risk reduction; SD = standard deviation.
Analyzed cohort was composed of students who completed baseline and 10th-grade follow-up surveys. All analyses presented were adjusted for nonresponse.
Oral sex was defined as “When someone puts his or her mouth on their partner's penis, vagina, or anus/butt or lets their partner put his or her mouth on their penis, vagina, or anus/butt.”
Vaginal sex was defined as “When a boy puts his penis inside a girl's vagina; some people call this ‘making love’ or ‘doing it.’”
Anal sex was defined as “When a boy puts his penis in his partner's anus or butt.”
Based on the principle of intent-to-treat [23], all students were analyzed according to their randomized condition regardless of intervention exposure. A standard set of covariates was entered into each model for all comparisons: gender, race/ethnicity, age at baseline, family structure, time between measures, and school-level sexual experience at baseline. For psychosocial outcomes, the baseline measure was included for all comparisons. Observations from students within the same school were assumed to be correlated [11,15]; therefore, multilevel models for continuous and binary data were used to compare treatment conditions. The estimated standard errors from these models were adjusted for any intra-class correlation present in the data. We used Wald tests to determine statistical significance, set at p < .05. All analyses were conducted using STATA, version 12 [24].
Separate models were fit comparing RA students with control students, and RR students with control students, for the total sample and stratified by gender and race/ethnicity. Students who were sexually experienced at baseline were excluded from analyses of sexual initiation. Students who were sexually inexperienced in 10th grade were coded as protected for other sexual behavior analyses [25].
For unexpected outcomes (i.e., outcomes that we did not anticipate to see as a result of the two interventions), such as an increased frequency of sex, post-hoc exploratory analyses were conducted to adjust for the dose of intervention received, not accounted for in primary analyses that used an intent-to-treat approach. Intervention dose for RA and RR students was assessed via lesson-specific student rosters and ranged from 0 to 24 lessons. Four additional models were run for each unexpected outcome, controlling for different levels of intervention dosage versus having received no intervention exposure (received at least one lesson, received four or more lessons, received eight or more lessons, and received ≥12 lessons).
Results
Participant characteristics
At baseline, participants were 60% female, 39% were African-American, and 50% were Hispanic, with a mean age of 12.6 years (standard deviation, .77); 12% had ever had sex (Table 1).
Intervention exposure
Risk avoidance and RR implementation occurred concurrently, ranging from 4 to 6 weeks per grade. Student attendance was documented per lesson. Students attended approximately 16 or 17 lessons (RA: range, 0–24, median, 16, mode, 22; RR: range, 0–24, median, 17, mode, 22). There was no significant difference in intervention exposure between RA and RR students.
Intervention effects
Delayed sexual initiation
For students in the RA and RR conditions, each compared separately with students in the control condition, there were no significant differences in delaying sexual initiation (analyzed as a composite variable) or in delaying oral or vaginal sex specifically in the total sample or among the subgroups. However, RA students were less likely to have initiated anal sex specifically in the total sample and among Hispanics (adjusted odds ratio [AOR], .64, 95% confidence interval [CI], .42–.99; and AOR, .53, 95% CI, .31–.91, respectively) compared with control students (both p < .05). Similarly, RR students were less likely to have initiated anal sex specifically in the total sample and among Hispanics (AOR, .65, 95% CI, .50–.84; and AOR, .82, 95% CI, .74–.93, respectively) compared with control students (both p < .01). Female RR students were also less likely to have initiated anal sex specifically (AOR, .66, 95% CI, .57–.76; p < .01) (Table 2).
Table 2.
Adjusted odds ratios at 10th-grade follow-up for risk avoidance and risk reduction interventions versus control condition for delayed sexual initiation, by total sample and by gender and race/ethnicity, and for other sexual behaviors
| Risk avoidance versus control |
Risk reduction versus control |
|||||
|---|---|---|---|---|---|---|
| na | AORb | 95% confidence interval | na | AORb | 95% confidence interval | |
| Delayed any sexual initiation | ||||||
| Total sample | 686 | .87 | 59–1.28 | 586 | .92 | 66–1.29 |
| Hispanicc | 352 | 1.19 | 72–1.99 | 307 | .94 | 75–1.18 |
| African-Americanc | 260 | .61 | .31–1.21 | 230 | .85 | .54–1.34 |
| Males | 223 | 1.20 | 71–2.03 | 208 | 1.02 | 87–1.18 |
| Females | 463 | .73 | 49–1.09 | 378 | .91 | 73–1.13 |
| Delayed initiation of specific types of sex | ||||||
| Oral sex | ||||||
| Total sample | 685 | .84 | 47–1.49 | 586 | .93 | 80–1.07 |
| Hispanicc | 352 | .85 | 51–1.41 | 307 | .94 | 75–1.18 |
| African-Americanc | 259 | .79 | 37–1.70 | 230 | .97 | 69–1.36 |
| Males | 222 | 1.19 | 68–2.11 | 208 | 1.01 | 79–1.29 |
| Females | 463 | .66 | 33–1.31 | 378 | .88 | 74–1.07 |
| Vaginal sex | ||||||
| Total sample | 681 | .92 | 63–1.33 | 585 | .89 | 63–1.27 |
| Hispanicc | 349 | 1.29 | 87–1.93 | 307 | .94 | 70–1.25 |
| African-Americanc | 259 | .63 | 29–1.35 | 229 | .83 | 55–1.25 |
| Males | 220 | 1.42 | 83–2.43 | 207 | 1.03 | 78–1.35 |
| Females | 461 | .74 | 49–1.11 | 378 | .89 | 74–1.07 |
| Anal sex | ||||||
| Total sample | 683 | .64 | 42–.99* | 585 | .65 | 50–.84** |
| Hispanicc | 350 | .53 | 31–.91* | 307 | .82 | 74–.93** |
| African-Americanc | 259 | .46 | 17–1.25 | 229 | .80 | 53–1.20 |
| Males | 221 | .75 | 36–1.55 | 207 | .97 | 75–1.25 |
| Females | 462 | .56 | 29–1.07 | 378 | .66 | 57–.76** |
| nd,e | AORf | 95% confidence interval | nd,e | AORf | 95% confidence interval | |
|---|---|---|---|---|---|---|
| Other sexual behaviorsg | ||||||
| Unprotected sex at last vaginal intercourseh | 777 | .61 | .45–.85** | 677 | .71 | .38–1.34 |
| Number of lifetime partners: two or more versus one or none | ||||||
| Oral sex | 755 | 1.29 | .74–2.25 | 653 | 1.30 | .77–2.25 |
| Vaginal sex | 765 | 1.12 | .79–1.57 | 668 | 1.13 | .80–1.60 |
| Anal sex | 817 | .83 | .49–1.42 | 707 | .98 | .60–1.59 |
| Number of times having sex in the past 3 months: two or more versus one or none | ||||||
| Oral sex | 753 | .96 | .51–1.82 | 651 | .89 | .70–1.13 |
| Vaginal sex | 767 | 1.04 | .82–1.31 | 667 | 1.34 | .96–1.86 |
| Anal sex | 749 | .65 | .29–1.42 | 645 | .19 | .11–.33** |
| Number of times having sex in the past 3 months without a condom: one or more versus none | ||||||
| Vaginal sex | 638 | .66 | .44–1.00 | 550 | .98 | .66–1.47 |
| Anal sex | 702 | .68 | .35–1.31 | 596 | .34 | .20–.56** |
| Number of sex partners in the past 3 months: two or more versus one or none | ||||||
| Vaginal sex | 641 | 2.80 | 1.52–5.14** | 551 | 2.14 | 1.37–3.35 ** |
AOR = adjusted odds ratio.
Excludes students who reported any sex at baseline.
An odds ratio <1 indicates that more participants in the intervention condition delayed sexual initiation relative to participants in the control condition. Each analysis was adjusted for gender, race/ethnicity, age, family structure, time between measures, and school-level sexual experience at baseline.
Because of small sample sizes, the racial/ethnic comparisons did not include the “other” subgroup.
Analyses included students who were not sexually experienced, coded as 0 (protected).
Sample sizes vary owing to missing data.
An odds ratio >1 indicates that more participants in the intervention condition engaged in the sexual behavior compared with participants in the control condition. Each analysis was adjusted for gender, race/ethnicity, age, family structure, school-level sexual experience at baseline, and baseline measure of outcome.
Because of small sample sizes, subgroup analyses were not conducted by gender and race/ethnicity for other sexual behaviors.
0 = used a condom at last vaginal intercourse or abstained from sex.
p < .05
p < .01.
Other sexual behaviors
Compared with control students, RA students were less likely to have engaged in unprotected sex at last vaginal intercourse either by using a condom or by abstaining from sex (AOR, .61, 95% CI, .45–.85; p < .01) (Table 2). Risk avoidance students reported a significantly greater number of recent vaginal sex partners (AOR, 2.80, 95% CI, 1.52–5.14; p < .01). However, after adjusting for intervention dose, there was no significant difference in the number of recent vaginal sex partners between students who received at least four RA lessons and control students (Table 3). There were no significant differences between RA students and control students for any other sexual behaviors.
Table 3.
Psychosocial outcomes for risk avoidance and risk reduction interventions versus control condition at 10th-grade follow-up among the analyzed cohort (n = 1,187)a
| Psychosocial variablesb | No. items | Range of scores | Cronbach αc | Risk avoidance versus control |
Risk reduction versus control |
||
|---|---|---|---|---|---|---|---|
| nd | Beta coefficiente | nd | Beta coefficiente | ||||
| Behavioral knowledge | |||||||
| STI signs and symptoms knowledge | 6 | 0–1 | .60 | 732 | .01 | 646 | .01 |
| HIV/STI knowledge | 5 | 0–2 | .49 | 806 | .09* | 698 | .08* |
| General condom knowledge | 6 | 0–2 | .65 | 833 | .03 | 717 | .10** |
| Perceived self-efficacy | |||||||
| Self-efficacy to refuse sex | 7 | 1–4 | .86 | 806 | .10* | 698 | .11** |
| Self-efficacy to use condoms | 3 | 0–3 | .63 | 803 | .09** | 693 | .10 |
| Self-efficacy to negotiate condom use | 2 | 0–3 | .75 | 821 | .06** | 707 | .08 |
| Behavioral and normative beliefs | |||||||
| General beliefs about waiting to have sex | 4 | 0–3 | .78 | 838 | –.7 | 720 | –.05 |
| Beliefs about abstinence until marriage | 6 | 0–3 | .84 | 820 | .13** | 702 | .05* |
| Reasons for not having sexf | 16 | 0–16 | NA | 834 | .04** | 719 | –.02 |
| Friends’ perceived beliefs about waiting to have sex | 3 | 0–3 | .75 | 838 | –.05 | 718 | .01 |
| Friends’ perceived sexual behavior | 4 | 0–3 | .76 | 816 | .02 | 700 | .01 |
| Perceived parental beliefs about waiting to have sex | 3 | 1–5 | .57 | 833 | –.01 | 715 | .06** |
| Beliefs about condoms | 3 | 0–3 | .87 | 817 | .11** | 704 | –.03 |
| Behavioral intentions | |||||||
| Intention to have oral sex in next year | 1 | 1–5 | NA | 842 | .06 | 719 | .09 |
| Intention to have vaginal sex in next year | 1 | 1–5 | NA | 838 | .04 | 719 | .27* |
| Intention to remain abstinent until end of high school | 1 | 1–5 | NA | 841 | .11 | 719 | .07 |
| Intention to remain abstinent until marriage | 1 | 1–5 | NA | 837 | .06 | 719 | –.00 |
| Intention to use condom in next 3 months | 1 | 1–5 | NA | 823 | –.06 | 719 | –.09 |
| Environmental factors | |||||||
| Exposure to risky situations that could lead to sex | 5 | 0–3 | .83 | 813 | –.03 | 704 | .03 |
| Parental communication about sexual topics | 3 | 0–2 | .87 | 789 | .08* | 674 | .14** |
| Character traits | |||||||
| Character qualities | 5 | 0–4 | .78 | 822 | .03 | 707 | .06* |
| Future orientation | 4 | 0–3 | .80 | 806 | –.06 | 686 | –.00 |
HIV = human immunodeficiency virus; NA = not applicable; STI = sexually transmitted infection.
All models were adjusted for gender, race/ethnicity, age, family structure, time between measures, school-level sexual experience at baseline, and baseline measure of outcome.
All psychosocial variables are coded as protective factors except for perceived friends’ sexual behavior, exposure to risky situations, oral sex intentions, and vaginal sex intentions.
Reliability indices were calculated using baseline data.
Sample sizes vary because of missing data.
Beta coefficients for these models are interpreted as the difference in adjusted means for each psychosocial variable.
Score reflects number of reasons chosen.
p < .05.
p < .01.
Compared with control students, RR students were less likely to have engaged in recent anal sex (AOR, .19, 95% CI, .11–.33) and unprotected anal sex (AOR, .34, 95% CI, .20–.56), respectively (both p < .01), either by using a condom or by abstaining from sex. Conversely, RR students were 2.14 times (95% CI, 1.37–3.35) as likely to have had two or more recent vaginal sex partners compared with control students (p < .01) (Table 2). However, after adjusting for intervention dose, there was no significant difference in the number of recent vaginal sex partners between students who received at least four RR lessons and control students (data not shown). There were no significant differences between RR students and control condition students for any other sexual behaviors.
Psychosocial outcomes
Among RA students, eight of 22 psychosocial outcomes were statistically significant in a positive direction (greater HIV/STI knowledge; greater self-efficacy for sex refusal, condom use, and condom use negotiation; more positive beliefs about abstinence until marriage; more reasons for not having sex; more positive beliefs about condoms; and more frequent parent–child communication about sexual topics). No outcomes were statistically significant in a negative direction (Table 3).
Among RR students, seven of 22 psychosocial outcomes were statistically significant in a positive direction (greater HIV/STI and general condom knowledge; greater self-efficacy for sex refusal; more positive beliefs about abstinence until marriage; more positive perceived parental beliefs about waiting to have sex; more frequent parent–child communication about sexual topics; and greater character qualities). One outcome was statistically significant in a negative direction: RR students reported greater intentions to engage in vaginal sex in the next year compared with control condition students (Table 3). However, after adjusting for intervention dose, students who received one or more RR lessons reported no greater vaginal sex intentions than control condition students (data not shown).
Discussion
We examined whether the behavioral and psychosocial effects of two middle school sexual health education programs extended into 10th grade. Similar to previous studies examining the long-term effect of middle school programs [13,14], we found no sustained impact on delayed sexual initiation or on delayed initiation of oral or vaginal sex specifically in the total sample, for either the RA or RR program relative to the control condition. Thus, our hypothesis that these programs would delay any sexual initiation into 10th grade was not supported. However, we found that compared with students in the control condition, students in both programs were significantly less likely to have initiated anal sex specifically from seventh to 10th grade in the total sample and among Hispanics. Female RR students were also less likely to have initiated anal sex specifically compared with control students. Both programs defined anal sex and provided repeated messages about the increased risk of STI/HIV transmission, which may have countered students’ perception that anal sex is a safer alternative to vaginal sex. These findings are encouraging regarding possible long-term health benefits of middle school sexual health education regardless of prevention approach.
Despite the positive impact on delayed anal sexual initiation among Hispanics (both programs) and females (the RR program), no sustained effects on delayed anal sexual initiation were found for African-Americans or males. This warrants further investigation to determine how different subgroups process and apply sexual health education messages received in middle school. This information could lead to the development of activities that resonate more effectively with most urban students or, conversely, to the development of more tailored approaches.
Our hypothesis that both sexual health education programs would have a sustained impact on other sexual behaviors was partially supported. Risk avoidance students were less likely to have had unprotected sex at last vaginal intercourse, either by using a condom or by abstaining from sex, or to have engaged in recent unprotected vaginal sex. Risk reduction students were less likely to have engaged in recent anal sex and unprotected anal sex, either by using a condom or by abstaining from sex. These outcomes indicate that middle school sexual health education programs may have some sustained effect on reducing specific sexual risk behaviors into 10th grade. In contrast, both programs had a significant unexpected effect on the number of recent vaginal sex partners. In post-hoc exploratory analyses adjusting for the dose of intervention received, which was not adjusted for in the primary models, this difference was no longer significant. However, these findings highlight the need to enhance activities in middle school programs to address the risks of having multiple sexual partners. This was not a major behavioral focus in either program.
Similar to previous studies [13,14], both interventions, relative to the control condition, had a sustained positive impact on some psychosocial factors: HIV/STI knowledge, refusal self-efficacy, beliefs about abstinence until marriage, and parent–child communication on sexual topics. Risk avoidance students also reported more reasons for not having sex, greater self-efficacy for condom use and negotiation, and more positive beliefs about condoms relative to controls. Risk reduction students also reported greater general condom knowledge, more positive perceived parental beliefs about waiting to have sex, and greater global character qualities. The findings that RA students reported more positive psychosocial outcomes related to condom use, whereas RR students reported more positive beliefs about abstinence until marriage, were unexpected because these topics were not explicitly covered in each respective program. Some students may have received additional sexual health education after this primary intervention, (i.e., some RA students may have received an RR program in ninth or 10th grade). We analyzed data regarding students’ exposure to other sexual health education programs in ninth and 10th grades; however, the data did not explain these findings. Similar findings were found at eighth- and ninth-grade follow-up [15], increasing the likelihood that they may be attributable to the programs themselves. As hypothesized previously [15], this may be because both programs presented abstinence as the healthiest choice for middle school students, provided medically accurate information about condoms, and reiterated messages about responsible sexual behavior. Regardless, these findings are noteworthy because they may allay concerns that RA programs negatively affect condom use intentions [26] and that RR programs undermine an abstinence message and endorse sexual activity [27].
Although these findings are promising, several limitations exist. First, requiring parental consent may have excluded students who were most at risk of early sexual initiation; thus, our findings generalize to students who would participate in an opt-in sexual health education program. Second, the large number of statistical tests may have led to some outcomes being significant by chance. However, we used two-tailed significance tests for all comparisons, all analyses were stated a priori, and multiple outcomes were significant at p < .01, strengthening the likelihood that significant outcomes were attributable to intervention effects. Third, baseline imbalances in sociodemographic characteristics and sexual behavior between treatment conditions may have biased outcomes away from the null hypothesis. However, multilevel modeling and inclusion of a school-level sexual prevalence covariate helped to adjust for this school-level impact. Finally, the study was conducted in one school district. Because it is the seventh largest school district in the U.S., findings may generalize to other large, urban districts.
Despite these limitations, our findings are important for researchers and practitioners in school-based sexual health education. The sustained delay of anal sex initiation and the reduction of some sexual behaviors into 10th grade suggest the potential long-term benefits of middle school sexual health education programs, irrespective of prevention approach. These data indicate that middle school sexual health education programs have the potential to develop responsible sexual behavior among high school students. However, because effects on any sexual initiation and on the initiation of oral and vaginal sex specifically were not sustained, there is a need for additional evidence-based sexual health education early in high school. Previous programs delivered in ninth and 10th grades, such as Reducing the Risk [28] and Safer Choices [29], both of which emphasized abstinence but included condom and contraceptive skill training, have shown positive outcomes regarding delayed sexual initiation and increased condom and contraceptive use among high school students. Thus, development of a contiguous middle through high school sexual health education program that builds on knowledge and skills developed in middle school may have a positive, synergistic effect on sexual behavior in high school. Our findings also highlight the need to address additional topics in middle school programs (e.g., avoiding multiple sexual partners), to impart messages about responsible sexual behavior before sexual initiation.
Evidence-based, middle school sexual health education programs can have positive short-term effects on adolescent behavior. Although they may be necessary to support healthy adolescent behavior, they are not sufficient over the long term to prevent many sexual risky behaviors. When considering how best to support adolescent sexual health within a school setting, school officials may want to consider implementing additional sexual health education in ninth and 10th grades to further delay sexual initiation and reduce risky sexual behavior in later high school years.
IMPLICATIONS AND CONTRIBUTION.
Findings extend our understanding of the sustained impact of sexual health education programs delivered in middle school. Although middle school programs can support healthy adolescent sexual behavior, additional education in ninth and 10th grades may help to further delay sexual initiation and reduce risky behavior in later high school years.
Acknowledgments
The study is registered at www.clinicaltrials.gov (#U48/DP000057). The authors thank their Expert Advisory Group, including Elaine Borawski, Karin Coyle, Ralph DiClemente, Patricia Goodson, Gale Grant, Doug Kirby, Joneen Mackenzie, Rebecca Maynard, Anita Smith, Shepherd Smith, Freya Sonenstein, Kate Walters, and Gina Wingood, for their input and support throughout the study; Mary Ann Mosack and Peggy Pecchio, for their input and guidance in developing the risk avoidance curriculum; school district personnel and students, for their participation; and Lionel Santibáñez, for editorial assistance.
Funding Sources
This study was funded by Centers for Disease Control and Prevention Grant 5U48DP000057 and by United States Department of Health and Human Services, Adolescent Family Life, Grant 90XF0036.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflicts of Interest: No authors have any potential conflicts of interest.
References
- 1.Centers for Disease Control and Prevention (CDC) Youth Risk Behavior Surveillance—United States, 2011. MMWR. 2012;61:1–162. [PubMed] [Google Scholar]
- 2.Hamilton B, Ventura S. Birth rates for U.S. teenagers reach historic lows for all age and ethnic groups. National Center for Health Statistics; Hyattsville (MD): 2012. p. 89. [PubMed] [Google Scholar]
- 3.CDC. [January 31, 2013];Diagnoses of HIV infection and population among young adults aged 20-24 years, by race/ethnicity, 2010-46 states. Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/slides/adolescents/index. htm.
- 4.CDC Division of Adolescent and School Health [January 31, 2013];Youth online: High school YRBS. Available at: http://apps.nccd.cdc.gov/youthonline/App/Default.aspx.
- 5.Flanigan CM. Sexual activity among girls under age 15: Findings from the National Survey of Family Growth. In: Albert B, Brown S, Flanigan CM, editors. 14 and younger: The sexual behavior of young adolescents. National Campaign to Prevent Teen Pregnancy; Washington, DC: 2003. pp. 57–64. [Google Scholar]
- 6.Kaestle CE, Halpern CT, Miller WC, et al. Young age at first sexual intercourse and sexually transmitted infections in adolescents and young adults. Am J Epidemiol. 2005;161:774–80. doi: 10.1093/aje/kwi095. [DOI] [PubMed] [Google Scholar]
- 7.Chin HB, Sipe TA, Elder R, et al. The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: Two systematic reviews for the Guide to Community Preventive Services. Am J Prev Med. 2012;42:272–94. doi: 10.1016/j.amepre.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 8.United Nations Educational, Scientific and Cultural Organization . School-based sexuality education programmes: a cost and cost-effectiveness analysis in six countries. Section of Education and HIV & AIDS; Paris, France: [November 22, 2013]. Available at: http://www.unesco.org/aids; 2011. [Google Scholar]
- 9.Advocates for Youth . Sex education and other programs that work to prevent teen pregnancy, HIV and sexually transmitted infections. Washington, DC: p. 2008. [Google Scholar]
- 10.Denny G, Young M. An evaluation of an abstinence-only sex education curriculum: An 18-month follow-up. J Sch Health. 2006;76:414–22. doi: 10.1111/j.1746-1561.2006.00135.x. [DOI] [PubMed] [Google Scholar]
- 11.Tortolero S, Markham CM, Peskin MF, et al. It's Your Game: Keep It Real: Delaying sexual behavior with an effective middle school program. J Adolesc Health. 2010;46:169–79. doi: 10.1016/j.jadohealth.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coyle KK, Kirby DB, Marin BV, et al. Draw the Line/Respect the Line: A randomized trial of a middle school intervention to reduce sexual risk behaviors. Am J Public Health. 2004;94:843–51. doi: 10.2105/ajph.94.5.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trenholm C, Devaney B, Fortson K, et al. Impacts of four Title V, Section 510 abstinence education programs: Final report. Mathematica Policy Research, Inc; Princeton (NJ): 2007. pp. 8549–110. MPR Ref. [Google Scholar]
- 14.Stanton B, Chen X, Koci V, et al. Effect of a grade 6 HIV risk reduction intervention four years later among students who were and were not enrolled in the study trial. J Adolesc Health. 2012;50:243–9. doi: 10.1016/j.jadohealth.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Markham C, Tortolero S, Peskin M, et al. Sexual risk avoidance and sexual risk reduction interventions for middle school youth: A randomized controlled trial. J Adolesc Health. 2012;50:279–88. doi: 10.1016/j.jadohealth.2011.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice-Hall; Englewood Cliffs (NJ): 1986. [Google Scholar]
- 17.McGuire W. Social psychology. In: Dodwell PC, editor. New horizons in psychology. Penguin Books; Middlesex, UK: 1972. pp. 219–42. [Google Scholar]
- 18.Section 510 of Title V of the Social Security Act. Section 912 of the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (Public Law 104–193) ed. 1996 [Google Scholar]
- 19.Centers for Disease Control and Prevention [April 28, 2008];Youth Risk Behavior Surveillance—comprehensive results, 1991-2005, sexual behaviors. Available at: http://apps.nccd.cdc.gov/yrbss/. [Google Scholar]
- 20.Blum RW, Beuhring T, Shew ML, et al. The effects of race/ethnicity, income, and family structure on adolescent risk behaviors. Am J Public Health. 2000;90:1879–84. doi: 10.2105/ajph.90.12.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kirby D, Lepore G, Ryan J. Sexual risk and protective factors: Factors affecting teen sexual behavior, pregnancy, childbearing and sexually transmitted disease: Which are important? Which can you change? ETR Associates for National Campaign to Prevent Teen Pregnancy: Putting What Works to Work Project; Washington, DC: Aug, 2005. [Google Scholar]
- 22.Miller BC, Benson B, Galbraith KA. Family relationships and adolescent pregnancy risk: A research synthesis. Dev Rev. 2001;21:1–38. [Google Scholar]
- 23.Gross D, Fogg L. A critical analysis of the intent-to-treat principle in prevention research. J Primary Prev. 2004;25:475–89. [Google Scholar]
- 24.Stata statistical software. Release 12. StataCorp LP; College Station (TX): 2011. [Google Scholar]
- 25.Mathematica Policy Research . Identifying programs that impact teen pregnancy, sexually transmitted infections, and associated sexual risk behaviors: Review protocol. Mathematica Policy Research; Washington, DC: 2012. Child Trends. Version 2.0. [Google Scholar]
- 26.Borawski E, Trapl E, Lovegreen L, et al. Effectiveness of abstinence-only intervention in middle school teens. Am J Health Behav. 2005;29:423–34. doi: 10.5555/ajhb.2005.29.5.423. [DOI] [PubMed] [Google Scholar]
- 27.Martin S, Rector R, Pardue M. Comprehensive sex education vs. authentic abstinence: A study of competing curricula. Heritage Foundation; Washington, DC: 2004. [Google Scholar]
- 28.Kirby D, Barth R, Leland N, et al. Reducing the Risk: Impact of a new curriculum on sexual risk-taking. Fam Plann Perspect. 1991;23:253–63. [PubMed] [Google Scholar]
- 29.Coyle K, Basen-Engquist K, Kirby D, et al. Safer choices: Reducing teen pregnancy, HIV, and STDs. Public Health Rep. 2001;116:82–93. doi: 10.1093/phr/116.S1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]