Abstract
Musculoskeletal diagnostic ultrasound imaging (MSK-DUSI) has been growing outside the traditional radiology speciality. Increased use of this technology has been reported in several healthcare settings, however an apparent gap in the knowledge of the accuracy of this diagnostic technology indicated a review was warranted. We undertook a structured review of the literature to assess the accuracy of MSK-DUSI for the diagnosis of musculoskeletal soft tissue pathology of the extremities. An electronic search of the National Library of Medicine’s PubMed database (1972 to mid-2014) was conducted. All relevant systematic reviews of diagnostic studies, all diagnostic studies published after the date of the latest systematic reviews and relevant diagnostic studies outside the scope the systematic reviews that directly compared the accuracy of MSK-DUSI (the index test) to an appropriate reference standard for the target condition were included. A fundamental appraisal of the methodological quality of studies was completed. The individual sensitivity, specificity and likelihood ratio data were extracted and entered into diagnostic accuracy tables. A total of 207 individual studies were included. The results show that MSK-DUSI has acceptable diagnostic accuracy for a wide spectrum of musculoskeletal conditions of the extremities. However, there is a lack of high quality prospective experimental studies in this area and as such clinicians should interpret the results with some caution due to the potential for overestimation of diagnostic accuracy.
Electronic supplementary material
The online version of this article (doi:10.1186/s12998-015-0076-5) contains supplementary material, which is available to authorized users.
Background
Musculoskeletal ultrasound (MSK-US) is a non-ionizing imaging modality, which is relatively inexpensive, portable, safe and rapid [1–4]. MSK-US should be considered in two distinct sub-categories. 1) Musculoskeletal diagnostic ultrasound imaging (MSK-DUSI) which primarily focuses on the morphological characteristics and structural integrity of the neuromusculoskeletal system [5–7]. 2) Rehabilitative ultrasound imaging (RUSI) which evaluates muscle and related soft tissue morphology and function during exercise and physical tasks [8, 9].
Historically, diagnostic ultrasound imaging (DUSI) has been utilised in medicine since the early 1950’s [5, 7]. In the following decades, DUSI became well-established in clinical obstetrics, gynaecology and cardiology [5]. In 1972, the first clinically significant application of DUSI was used in musculoskeletal medicine; where it was used to differentiate Baker’s cysts from thrombophlebitis [10]. This paper led to the logical extension of DUSI in musculoskeletal medicine seen today. The primary use of MSK-US continues to be used for traditional diagnostic imaging purposes, allowing real-time, dynamic evaluation of neuromusculoskeletal structures, including but not limited to joints, tendons, ligaments, muscles and nerves [5–7].
In the 1980’s, a new branch of MSK-US was developing. Young and colleagues used MSK-US to accurately measure muscle atrophy post-injury, aging on muscle size and the relationship between muscle size and strength in different populations [11–13]. This work established RUSI [7]. In the past two decades, a series of studies highlighted the use of RUSI to detect abnormal lumbar multifidus and transverse abdominus muscle morphology and activation patterns in patients with acute and chronic lower back pain [7]. In addition, researchers utilising RUSI found that recovery of these muscles was not automatic when pain subsided, but required specific training to re-activate them [7]. This has cemented RUSI, particularly in physiotherapy practice, where RUSI has been used to monitor the recovery of these muscles [7]. Concurrently, adult spinal MSK-DUSI created a high degree of interest among groups of chiropractors for the evaluation of spinal canal diameters, facet, intervertebral disc and nerve root pathology [14–21]. However, this was soon abandoned due to technological factors such as inadequate depth of penetration, lack of penetration of spinal structures and poor image resolution resulting in limited accuracy and clinical utility [14, 22–30].
In the past decade, interest in MSK-DUSI among non-radiologists has made a resurgence [31] and has attracted the attention of many chiropractic practitioners. The use of MSK-DUSI in clinical practice has nearly quadrupled in the United States since the 2000’s and is also an expanding area in Europe, driven primarily by increased utilisation by non-radiologists [3, 31]. This can be attributed to recent advances in conventional two-dimensional (2D) ultrasound technology [32–36]. Recent refinements in 2D ultrasound technology, such as broadband transducers are now available at frequencies greater than 15 MHz that allow visualization of superficial and deep structures with resolutions approaching that of standard T1 and T2 magnetic resonance imaging (MRI) sequences [33]. Ultrasound machines are now available as compact, portable systems (typically the size of a notebook computer), which are on average available at less cost than the conventional cart-based systems. [32, 33] Although the cart-based systems allow for extra features including: greater image and patient information archive capacity and more ultrasound mode options (i.e. 2D, Doppler, harmonic mode etc.), the mid-range compact, portable systems are cheaper and have similar image resolution [32, 34]. Reduced machine cost, portability, improved image resolution and increased diagnostic accuracy have influenced MSK-DUSI growth among non-radiologists and interest among chiropractors.
A review of the literature revealed a current paucity of studies examining the utility of MSK-DUSI within chiropractic environments. The majority consist of experimental studies assessing the normal or abnormal sonographic appearance of anatomy [37–42]; several case reports demonstrating the importance of subsequent MSK-DUSI when plain films are unremarkable [43–46]; and a few commentaries [14, 16]. One pilot study by Hung et al. [47] showed that it may be feasible to teach senior chiropractic students an area of normal sonographic anatomy. This is consistent with other professions demonstrating an ability to train novice interpreters to a standard of that of an experienced interpreter [48–51]. Extrapolations of these studies suggest it may be feasible to teach the sonographic appearance of other body regions to novice interpreters. Although the literature on the topic is limited, current observational trends of increasing accessibility to MSK-DUSI training for chiropractors suggest that a growing body of literature may emerge.
MSK-DUSI has been reported as a valid technique for imaging a wide variety of neuromusculoskeletal conditions [52]. However, it is important to emphasise with the current state of the technology the utility of MSK-DUSI is typically limited to the diagnosis of superficial pathology of the extremities. MSK-DUSI has little use in the spine other than landmark identification for injection purposes by medical professionals and research. Nonetheless, a high percentage of chiropractic patients undergoing diagnosis and treatment have musculoskeletal complaints of the extremities [53, 54]. Improving patient care is pivotal in all healthcare professions and by developing the utility of MSK-DUSI in the chiropractic profession may allow for earlier, accurate diagnosis and therefore, better patient management and outcomes. MSK-DUSI involves no ionising radiation, meaning it is safe for patients. Accessibility is increasing as costs of the systems diminish. Portability allows efficient and accurate ‘in office’ scanning as a potential extension to physical examination for certain anatomic areas. MSK-DUSI has become an accurate, prompt, relatively inexpensive and readily available method of imaging the neuromusculoskeletal system. This presents new opportunities within the chiropractic profession to improve patient care and research.
The growing appeal of MSK-DUSI among the chiropractic profession can be observed from the recent accessibility to tailored courses and through the growing number of published research papers [14–16, 37–46]. The appropriate use of imaging is essential in all healthcare professions for accurate patient diagnosis and management as well as optimising the use of healthcare resources. However, the instrument of measurement needs to be reliable and valid. Therefore, this review investigated the evidence currently available on the accuracy of diagnostic ultrasound for the diagnosis of musculoskeletal soft tissue pathology of the extremities.
Review
Identification and selection of studies
The anatomical areas selected included: shoulder, elbow, hand/wrist, hip, knee and ankle/foot. These areas corresponded to the MSK-DUSI guidelines identified by the European Society of Musculoskeletal Radiology (ESMR) and the American College of Radiology (ACR) [3, 55]. All clinically indicated musculoskeletal soft-tissue conditions identified by the ESMR and ACR MSK-DUSI guidelines were included this review [3, 55]. Therefore, for the purpose of this article ‘soft tissue pathology’ was defined to mean musculoskeletal conditions of muscle, tendon, ligament, and certain joint and peripheral nerve structures.
The conclusions of the report are based on the results of relevant systematic reviews of diagnostic studies, all diagnostic studies published after the date of the latest systematic reviews and relevant diagnostic studies outside the scope the systematic reviews. Articles included in the systematic reviews were not treated individually in this review but were included as a whole review. While critical appraisal of the included reviews and diagnostic studies would be ideal, it is beyond the scope of the present report.
A review of the literature was performed using the National Library of Medicine’s PubMed data base (1972 to mid-2014). The term ‘index test’ was defined to mean the test whose performance was being evaluated. The reference test or ‘gold standard’ was the standard against which the index test was compared. All systematic reviews and diagnostic studies that assessed the accuracy of MSK-DUSI (the index test) to an appropriate reference test for musculoskeletal soft tissue pathology of the extremities were included. The reference test is dependent on the target condition and includes: MRI, surgical findings (arthroscopy or open surgery), arthrography and electromyography (EMG), or nerve conduction studies (NCS). The search strategy used three important ‘search term sets’ including: index test set, target condition set, and diagnostic accuracy set. Additional file 1 shows the full electronic search strategy. The search was restricted to articles published in English or languages for which a full translation to English was also published. The titles and abstracts retrieved were screened by one reviewer (RH) to identify potentially relevant studies for inclusion and duplicates removed. Full-text manuscripts were obtained and evaluated for final inclusion against a predetermined criteria (Table 1). The reference lists of each potentially relevant paper were reviewed to identify any omitted studies missed by the search strategy.
Table 1.
Inclusion
| • Published as full-text article, published in English and languages for which a full translation could be obtained. |
| • Human studies only (no cadaveric studies). |
| • Index test: MSK-DUSI. |
| • Target condition(s): musculoskeletal soft tissue pathology. |
| • Reference tests: MRI, surgical findings (arthroscopy or open surgery), arthrography and electromyography or nerve conduction studies. |
| • Interpreted by radiolo |
| • Individual diagnostic studies not included in prior systematic review/meta-analysis. |
| • Sufficient quantitative data provided (minimum: two-by-two tables) |
Data extraction and analysis
A fundamental appraisal of the methodological quality of studies was completed by the reviewer (RH), as outlined by the Users’ Guide to the Medical Literature: A Manual for Evidence-Based Clinical Practice [56]. The following items were assessed:
Was the patient sample appropriate? (i.e. representative of clinical practice; uncertain diagnosis; wide spectrum – age, gender, severity; patients with disease/with similar presenting disease/ without disease)
Was there an independent, blinded comparison to an appropriate reference standard?
Did all patients, regardless of index test results, undergo the reference standard?
The following data were extracted:
Publication details.
Sample size.
Baseline characteristics: age, duration of symptoms between injury and MSK-DUSI and diagnosis.
Target condition as reported.
Index test: ultrasound transducer frequency, ultrasound operator and reviewer.
Reference standard.
Quantitative Data: Sensitivity (SnS), Specificity (SpC) and likelihood ratios (LR).
Two-by-two tables containing the number of true positives, true negatives, false positives and false negatives were the minimum quantitative data necessary for inclusion of individual diagnostic studies and systematic reviews. Articles that did not provide the required minimum quantitative data were excluded from this review. SnS, SpC and LRs were calculated from the two-by-two tables using a web-based diagnostic test calculator when they were not provided outright. [57] When SnS and SpC were provided outright without LRs, the LRs were calculated manually using an excel spreadsheet. Pooled SnS and SpC data provided from systematic reviews were extracted if provided. The authors did not pool the data. When pooled data was not provided, the data range was extracted.
The extracted data were entered into two types of tables.
Study characteristics tables containing: target condition; publication details; sample size; age; duration of symptoms between injury and MSK-DUSI; ultrasound transducer frequency; ultrasound operator and reviewer.
MSK-DUSI accuracy tables containing: target condition; publication details; reference standard; quantitative data.
Accuracy summary tables
These tables were developed with the purpose of providing the best available evidence-based recommendations for when diagnostic ultrasound is clinically indicated for musculoskeletal soft tissue pathology. The tables are based on the results relating to each anatomical area. The Accuracy Summary is based on a five scale determination as follows. Unknown: No diagnostic accuracy studies found. Grade 0: Not indicated. Grade 1: Conflicting evidence (test results should be interpreted with caution). Grade 2: Equivalent to other imaging techniques (other techniques might provide significant information). Grade 3: First choice technique (other techniques rarely provide more information). A clinical condition received a grade 0 recommendation if the data or the majority of studies reported SnS and SpC values less than 0.60. A Grade 1 recommendation was given if there was a relatively even number of studies reporting conflicting SnS and SpC data (e.g. the positive supportive evidence does not significantly out-weigh the negative supportive evidence, and vice versa). A Grade 2 recommendation was given if the data or the majority of studies reported SnS and SpC values greater than 0.60 and less than 0.85. A Grade 3 recommendation was given if the data or the majority of studies reported SnS and SpC values greater than 0.85. The grading system was adapted from the four scale determination used in Clinical indications for musculoskeletal ultrasound: A Delphi-based consensus paper of the European society of musculoskeletal radiology [3].
Data interpretation
In text, the collective diagnostic findings are classified as low, moderate and high diagnostic accuracy. There is currently no reported classification for what is considered poor, low, moderate or high diagnostic accuracy [58–60]. As such the following ranges were used to classify the collective diagnostic findings. Low (SnS and SpC: less than 0.60), moderate (SnS and SpC: 0.60 to 0.85) and high (SnS and SpC: greater than 0.85) diagnostic accuracy. These ranges reflect those of the accuracy summary tables to maintain consistency throughout the article.
It is worth remembering that tests with high SnS and small negative likelihood ratios (LR–) are most useful for ruling out disease. That is, a negative result indicates that disease is not likely to be present. Tests with high SpC and high positive likelihood ratios (LR+) are most useful for ruling in disease. That is, a positive test indicates that disease is likely to be present [61]. LRs summarise how many times more (or less) likely patients with the disease are to have a particular test result than patients without the disease. A LR+ above 10 and a LR– below 0.1 are considered to provide strong evidence to rule a diagnosis in or out, respectively [62].
Results
In total, the search strategy identified 6321 citations. After removing duplicates, there were 3894 potentially eligible titles and abstracts. Once the titles and abstracts of these citations were screened, 332 potentially eligible articles remained. These full-text articles were reviewed for eligibility, 95 studies (12 systematic reviews and 83 diagnostic studies) were included in the final review. The individual studies in the systematic reviews totalled 124 and when added to the other 83 diagnostic studies amounted to 207 individual studies. The full results of the search strategy are presented in a flow chart (Fig. 1).
Fig. 1.
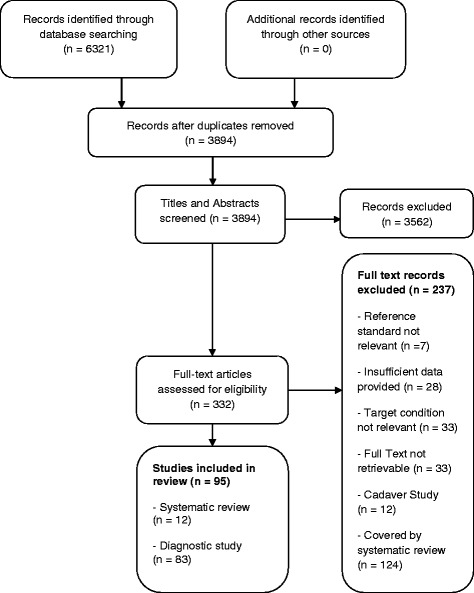
Flow chart: search strategy results
Shoulder
A total of 13 clinical conditions were identified (Table 2). Seventy-two diagnostic studies and five systematic reviews relevant to the accuracy of MSK-DUSI for diagnosing soft-tissue pathology of the shoulder were found. Four of the systematic reviews investigated rotator cuff tears [63–66] and one was a systematic review investigating subacromial disorders [67]. The systematic reviews contained 63 of the same articles found in this review. These articles were not treated individually in this review as they were included by way of each systematic review (refer to systematic reviews for these references). This left four relevant diagnostic studies published after the date of the latest systematic review [49, 68–70] and five relevant diagnostic studies outside the scope the systematic reviews [71–75]. Therefore, a total of 14 relevant articles were used in this review (nine diagnostic studies and five systematic reviews) [49, 63–75], amounting to 72 individual studies in all. The study characteristics are presented in Table 3.
Table 2.
Identified clinical conditions of the shoulder
| Identified clinical conditions of the shoulder | Relevant studies found (Yes/No) |
|---|---|
| Full thickness cuff tears | Y |
| Partial thickness cuff tears | Y |
| Bursitis | Y |
| Calcific tendinitis (Supraspinatus and long head the biceps) | Y |
| Rotator cuff tendinopathy (includes tendinitis and tendinosis) | Y |
| Rotator cuff muscle atrophy | Y |
| Subacromial impingement | Y |
| Long head of biceps: tears | Y |
| Long head of biceps: dislocation | Y |
| Long head of biceps: tendinopathy \(includes tendinitis and tendinosis) | Y |
| Adhesive capsulitis | N |
| Pectoralis tears | N |
| Deltoid tears | N |
Table 3.
Shoulder: Study Characteristics
| Study | Target Condition | Number of studies (Systematic Review) | Subjects | Mean Age (years) | Mean time from injury to ultrasound | Ultrasound transducer frequency (MHz) | Ultrasound reviewers |
|---|---|---|---|---|---|---|---|
| Systematic Review | |||||||
| Lenza et al., 2013 [65] | RC FTT/PTT | 10 | 654 | N/S | <1 year | 5.0 to 15 | RAD |
| Smith et al., 2011 [66] | RC FTT/PTT | 62 | 6007 | 52.2 | 1 year | 5.0 to 13 | RAD and Non-RAD |
| Ottenheijm et al., 2010 [67] | RC FTT/PTT; Bursitis; CT; RCT | 23 | 1377 | 52 | <3 months | >7.5 | RAD and Non-RAD |
| Kelly et al., 2009 [64] | RC FTT/PTT | 67 | N/S | N/S | N/S | N/S | RAD and Non-RAD |
| de Jesus et al., 2009 [63] | RC FTT/PTT | 65 | N/S | N/S | N/S | N/S | RAD |
| Diagnostic Study | |||||||
| Alavekios et al., 2013 [68] | RC FTT | - | 200 | N/S | N/S | 12 to 15 | Non-RAD |
| Le Corroller et al., 2008 [69] | RC FTT/PTT; Bursitis; RCT; LHB | - | 65 | 52.4 | N/S | 5.0 to 12 | RAD |
| Murphey et al., 2013 [49] | RC FTT | - | 156 | N/S | 1 day | 4.7 to 13 | RAD and Non-RAD |
| Ok et al., 2013 [70] | RC FTT/PTT | - | 51 | N/S | N/S | 12 | Non-RAD |
| Khoury et al., 2008 [72] | RC Atrophy | - | 39 | 61 | N/S | 5.0 to 12 | RAD |
| Strobel et al., 2005 [75] | RC Atrophy | - | 65 | 53.1 | N/S | 7.5 to 9 | RAD |
| Armstrong et al., 2006 [71] | LHB | - | 71 | 59 | N/S | 7.5 to 9 | RAD |
| Read et al., 1998 [73] | LHB; Impingement | - | 42 | 44 | 8.8 weeks | 7.5 | RAD |
| Skendzel et al., 2011 [74] | LHB | - | 66 | 55 | <6.5 months | 10 to 17 | RAD |
| - | AC | - | - | - | - | - | - |
| - | Pec/Delt Tears | - | - | - | - | - | - |
N/S not stated; RAD Radiologist; RC rotator cuff; FTT full tendon tear; PTT partial tendon tear; CT calcific tendonitis; RCT rotator cuff tendinopathy (includes tendinosis and tendinitis); LHB long head of the biceps tendon; AC adhesive capsulitis; Pec/Delt pectoralis/deltoid
Table 3 reports, the five systematic reviews included a total of 227 diagnostic studies [63–67]. The number of patients was not stated in two studies [63, 64]. The other 12 studies reviewed a total of 8739 patients [49, 65–75]. The mean age was not stated in six studies [49, 63–65, 68, 70]. In the eight studies where it was stated, the mean age of the cohorts was 53.6 (SD 5.1) [66, 67, 69, 71–75]. Mean time from injury to imaging was not stated in eight studies [63, 64, 68–72, 75]. In the six studies where this was stated [49, 65–67, 73, 74], this ranged from 1 day [49] to less than 200 days [74]. All studies documented the job titles of the people who performed and reviewed the ultrasound images. In eight studies, a radiologist performed and interpreted the images [63, 65, 69, 71–75]; in four studies a radiologist and non-radiologist were involved [49, 64, 66, 67]; in two studies only a non-radiologist was involved [68, 70]. Non-radiologists were either a sonographer, physician or orthopaedic surgeon [49, 64, 66–68, 70].
The individual SnS, SpC and LRs for the ultrasound diagnosis of musculoskeletal soft-tissue pathology of the shoulder are presented in Table 4. Overall, both systematic reviews and diagnostic studies consistently demonstrated high diagnostic accuracy for full-thickness rotator cuff tears [49, 63–70]. Therefore, a positive test provides convincing evidence that a full-thickness tear is present, because it increases the odds of a full tear being present 6 to 30-fold (LR + = 6.0 to 30.0), well above the arbitrary threshold of 10 [62]. In addition, a negative test rules out a full-thickness tear, because it decreases the odds 0.04 to 0.23-fold (LR- = 0.04 to 0.23), below the 0.1 value commonly used for exclusion [62]. For partial thickness-tears, both systematic reviews and diagnostic studies results show that it is easier to rule in or diagnose patients with partial thickness tears (SpC: 0.75 to 0.98; LR + = 1.84 to 35.5) than to rule it out (SnS: 0.46 to 0.84; LR- = 0.18 to 0.72) [63–67, 69, 70].
Table 4.
Accuracy of MSK-DUSI for detecting soft-tissue pathology of the shoulder
| Target Condition | Study | Reference Standard | Sensitivity | Specificity | LR+ | LR- |
|---|---|---|---|---|---|---|
| Systematic Review | ||||||
| RC FTT | Lenza 2013 [65] | Arthroscopy or open surgery | 0.92 | 0.93 | 13.1 | 0.09 |
| Smith 2011 [66] | Arthroscopy or open surgery | 0.96 | 0.93 | 13.7 | 0.04 | |
| Ottenheijm 2010 [67] | Arthroscopy or MRI | 0.95 | 0.96 | 23.8 | 0.05 | |
| Kelly 2009 [64] | MRI | 0.87 | 0.96 | 21.8 | 0.14 | |
| de Jesus 2009 [63] | Arthroscopy or open surgery | 0.92 | 0.94 | 16.5 | 0.08 | |
| Diagnostic Study | ||||||
| Alavekios 2013 [68] | MRI | 0.95 | 0.90 | 9.50 | 0.06 | |
| Le Corroller 2008 [69] | MRA | 0.91 | 0.91 | 10.1 | 0.10 | |
| Murphey 2013 [49] | Arthroscopy | 0.90 | 0.97 | 30.0 | 0.10 | |
| Ok 2013 [70] | Arthroscopy | 0.80 | 0.86 | 5.71 | 0.23 | |
| Systematic Review | ||||||
| RC PTT | Lenza 2013 [65] | Arthroscopy or open surgery | 0.52 | 0.93 | 7.43 | 0.52 |
| Smith 2011 [66] | Arthroscopy or open surgery | 0.84 | 0.89 | 7.64 | 0.18 | |
| Ottenheijm 2010 [67] | Arthroscopy or MRI | 0.72 | 0.93 | 10.3 | 0.30 | |
| Kelly 2009 [64] | MRI | 0.67 | 0.94 | 11.2 | 0.35 | |
| de Jesus 2009 [63] | Arthroscopy or open surgery | 0.67 | 0.94 | 11.2 | 0.35 | |
| Diagnostic Study | ||||||
| Le Corroller 2008 [69] | MRA | 0.71 | 0.98 | 35.5 | 0.30 | |
| Ok 2013 [70] | Arthroscopy | 0.46 | 0.75 | 1.84 | 0.72 | |
| Systematic Review | ||||||
| Bursitis | Ottenheijm 2010 [67] | Arthroscopy or MRI | 0.79–0.81 | 0.94–0.98 | 12.8–41.5 | 0.20–0.22 |
| Diagnostic Study | ||||||
| Le Corroller 2008 [69] | MRA | 0.96 | 0.90 | 9.60 | 0.04 | |
| Systematic Review | ||||||
| CT | Ottenheijm 2010 [67] | Arthroscopy or MRI | 1.00 | 0.85–0.98 | 6.5–51.8 | 0.02–0.06 |
| Systematic Review | ||||||
| RCT | Ottenheijm 2010 [67] | Arthroscopy or MRI | 0.67–0.93 | 0.88–1.00 | 5.73–41.5 | 0.07–0.38 |
| Diagnostic Study | ||||||
| Le Corroller 2008 [69] | MRA | 0.89 | 0.96 | 22.3 | 0.12 | |
| RC atrophy | Khoury 2008 [72] | MRI | 0.84 | 1.00 | - | 0.16 |
| Strobel 2005 [75] | MRI | 0.78 | 0.81 | 4.11 | 0.27 | |
| Subacromial impingement | Read 1998 [73] | Clinical Diagnosis | 0.97 | 0.63 | 2.62 | 0.05 |
| LHB | ||||||
| Full rupture | Armstrong 2006 [71] | Arthroscopy | 1.00 | 1.00 | - | - |
| Le Corroller 2008 [69] | MRA | 0.86 | 0.98 | 43.0 | 0.14 | |
| Read 1998 [73] | Arthroscopy | 0.75 | 1.00 | - | 0.25 | |
| Skendzel 2011 [74] | Arthroscopy | 0.88 | 0.98 | 44.0 | 0.12 | |
| Dislocation | Armstrong 2006 [71] | Arthroscopy | 0.96 | 1.00 | - | 0.04 |
| Le Corroller 2008 [69] | MRA | 0.86 | 0.98 | 43.0 | 0.14 | |
| Read 1998 [73] | Arthroscopy | 1.00 | 1.00 | - | - | |
| Tendinitis | Le Corroller 2008 [69] | MRA | 0.86 | 0.98 | 43.0 | 0.14 |
| Read 1998 [73] | Arthroscopy | 1.00 | 1.00 | - | - |
MRA magnetic resonance arthrography; RC rotator cuff; FTT full tendon tear; PTT partial tendon tear; CT calcific tendonitis; RCT rotator cuff tendinopathy (includes tendinosis and tendinitis); LHB long head of the biceps tendon
The results showed that ultrasound has a high diagnostic value for calcific tendinitis (supraspinatus), full-thickness tears and dislocation of the long head of the biceps [67, 69, 71, 73, 74]. Ultrasound can rule in and out subacromial bursitis with moderate to high accuracy [67, 69], and appeared to be able to rule in rotator cuff tendinopathy accurately, however the SnS results conflicted [67, 69]. One study included in Ottenheijm’s et al. 67] review reported a low SnS (0.67), which was possibly explained by a small population and out-dated ultrasound technology. Ultrasound can rule in rotator cuff atrophy with moderate to high accuracy but is less sensitive in ruling it out [72, 75]. Refer to Table 4 for the individual SnS, SpC and LR outcomes for each of the above conditions. This review found no diagnostic studies assessing the accuracy of ultrasound diagnosis of adhesive capsulitis, pectoralis tears, deltoid tears or partial-tears, tendinosis, calcific tendinitis of the long head of the biceps.
In the shoulder region, the results suggest the use of MSK-DUSI is indicated for any rotator cuff tear, however is less sensitive in ruling out partial-thickness tears. To a lesser extent ultrasound is indicated to diagnose bursitis, calcific tendinitis, rotator cuff tendinopathy, rotator cuff atrophy, subacromial impingement syndrome and long head of the biceps pathology. A summary of recommendations are presented in Table 5. It is important to emphasise that this information is a summary of the results and should be interpreted with consideration of the full results table (Table 4).
Table 5.
Accuracy Summary – Musculoskeletal Clinical Indications for the use of Diagnostic Ultrasound for the Shoulder Region
| Target Condition | Recommendation |
|---|---|
| Tendons and soft tissue | Grade |
| Calcific Tendinitis | 3 |
| Full thickness rotator cuff tears | 3 |
| LHB: dislocation | 3 |
| LHB: full thickness tears | 3 |
| LHB: tendinitis | 3 |
| Rotator cuff tendinopathy | 3 |
| Subacromial bursitis | 3 |
| Partial thickness rotator cuff tears | 2 |
| Rotator cuff atrophy | 2 |
| Subacromial Impingement | 2 |
| Adhesive capsulitis | Unknown |
| Deltoid tears | Unknown |
| LHB: partial thickness tears | Unknown |
| Pectoralis tears | Unknown |
LHB long head of biceps
Unknown: No diagnostic accuracy studies found
Grade 0: Not indicated
Grade 1: Conflicting evidence (test results should be interpreted with caution)
Grade 2: Equivalent to other imaging techniques (other techniques might provide significant information)
Grade 3: First choice technique (other techniques rarely provide more information)
Elbow
A total of 11 clinical conditions were identified (Table 6). Eight diagnostic studies and two systematic reviews relevant to the accuracy of MSK-DUSI for diagnosing soft-tissue pathology of the elbow were found. One systematic review investigated lateral epicondylalgia [76] and one was a systematic review investigating cubital tunnel syndrome [77]. The systematic reviews contained six of the same articles found in this review. These articles were not treated individually in this review as they were included by way of each systematic review (refer to systematic reviews for these references). No other relevant diagnostic studies published after the date of the latest systematic review were found. Two relevant diagnostic studies outside the scope the systematic reviews were found [78, 79]. Therefore, a total of four relevant articles were used in this review (two diagnostic studies and two systematic reviews) [76–79], amounting to 8 individual studies in all. The study characteristics are presented in Table 7.
Table 6.
Identified clinical conditions of the elbow
| Identified clinical conditions of the elbow | Relevant studies found (Yes/No) |
|---|---|
| Cubital tunnel syndrome | Y |
| Lateral epicondylalgia (itis/osis) | Y |
| Medial epicondylalgia (itis/osis) | Y |
| Biceps tendon injury | Y |
| Ulnar nerve subluxation | N |
| Radial nerve compression | N |
| Median nerve entrapment/pronator syndrome | N |
| Lateral collateral ligament injury | N |
| Medial collateral ligament injury | N |
| Triceps tendon injury | N |
| Bursitis | N |
Table 7.
Elbow: Study Characteristics
| Study | Target Condition | Number of studies (Systematic Review) | Subjects | Mean Age (years) | Mean time from injury to ultrasound | Ultrasound transducer frequency (MHz) | Ultrasound reviewers |
|---|---|---|---|---|---|---|---|
| Systematic Review | |||||||
| Beekman et al., 2003 [80] | UNN/CTS | 7 | 542 | 39.2 | N/S | 5.0 to 12 | RAD and Non-RAD |
| Dones et al., 2014 [76] | LE | 7 | 211 | 50 | >6 weeks | 5.0 to 15 | RAD and Non-RAD |
| Diagnostic Study | |||||||
| Lobo et al., 2013 [78] | BTI | - | 45 | 44 | 34.5 days | 6.0 to 17.5 | RAD |
| Park et al., 2008 [79] | ME | - | 18 | 50 | 17.6 months | 7.5 to 15 | RAD |
| - | UNS | - | - | - | - | - | - |
| - | RNC | - | - | - | - | - | - |
| - | MNE/PS | - | - | - | - | - | - |
| - | LCL | - | - | - | - | - | - |
| - | MCL | - | - | - | - | - | - |
| - | Bursitis | - | - | - | - | - | - |
| - | TTI | - | - | - | - | - | - |
N/S not stated; RAD Radiologist; LE lateral epicondylalgia; ME medial epicondylalgia; BTI biceps tendon injury; UNN/CTS ulnar nerve neuropathy/cubital tunnel syndrome; UNS ulnar nerve subluxation; RNC radial nerve compression; MNE/PS median nerve entrapment/pronator syndrome; LCL lateral collateral ligament; MCL medial collateral ligament; TTI triceps tendon injury
Table 7 reports, the two systematic reviews included 14 diagnostic studies [76, 77]. The included studies reviewed 816 patients [76–79]. The mean age of the cohorts was 45.8 (SD 5.2). Mean time from injury to imaging was not stated in one study [77]. In the three studies where this was stated [76, 78, 79], the time varied from 34.5 days [78] to 17.6 months [79]. All studies documented the job title of the person who performed and reviewed the ultrasound images. In two studies [78, 79], a radiologist performed and interpreted the images and in the remaining two studies [76, 77] a radiologist and non-radiologist were involved. Non-radiologists were either a sonographer or physician [76, 77].
The individual SnS, SpC and LRs for the ultrasound diagnosis of musculoskeletal soft-tissue pathology of the elbow are presented in Table 8. Ulnar nerve thickening at the elbow (the cross-sectional area) is the most common sonographic characteristic used to diagnose cubital tunnel syndrome [77]. Therefore, the results reflect the SnS and SpC of this sonographic characteristic to diagnose cubital tunnel syndrome. One systematic review assessed the accuracy of ultrasound detection for ulnar nerve neuropathy (cubital tunnel syndrome) at the elbow [77]. This review demonstrated that ultrasound can be helpful in the diagnosis of cubital tunnel syndrome, with moderate diagnostic accuracy in demonstrating ulnar nerve thickening and also by detecting underlying abnormalities [77]. One systematic review assessed the accuracy of ultrasound detection for lateral epicondylalgia [76]. This review demonstrated the use of grey-scale ultrasound has moderate diagnostic accuracy in objectively diagnosing lateral epicondylalgia [76].
Table 8.
Accuracy of MSK-DUSI for detecting soft tissue pathology of the elbow
| Target Condition | Study | Reference Standard | Sensitivity | Specificity | LR+ | LR- |
|---|---|---|---|---|---|---|
| Systematic Review | ||||||
| UNN/CTS | Beekman 2003 [80] | EMG or NCS | 0.46–1.00 | 0.71–0.97 | 2.88–14.3 | 0.00–0.64 |
| LE | Dones 2014 [76] | Clinical Diagnosis | 0.64 | 0.82 | 3.56 | 0.44 |
| Diagnostic Study | ||||||
| ME | Park 2008 [79] | Clinical Diagnosis | 0.95 | 0.92 | 11.9 | 0.05 |
| BTI | ||||||
| Full Rupture | Lobo 2013 [78] | Clinical Diagnosis or open surgery | 0.95 | 0.71 | 3.28 | 0.07 |
LE lateral epicondylalgia; ME medial epicondylalgia; BTI biceps tendon injury; UNN/CTS ulnar nerve neuropathy/cubital tunnel syndrome
The results showed that ultrasound has a high diagnostic value for detecting medial epicondylalgia [79] and that ultrasound can rule out full rupture of the distal biceps with high diagnostic accuracy but is only moderately accurate in ruling it in [78]. Refer to Table 8 for the individual SnS, SpC and LR outcomes for each of the above conditions. This review found no diagnostic studies assessing the accuracy of ultrasound diagnosis of partial distal bicep tendon tears, bursitis, lateral or medial collateral ligament injury, triceps tendon injury (tears and snapping triceps syndrome), ulnar nerve subluxation, radial nerve compression or median nerve entrapment/pronator syndrome.
In the elbow region, the results suggest the use of MSK-DUSI is indicated for assisting in the diagnosis of cubital tunnel syndrome and objectively diagnosing lateral epicondylalgia. To a lesser extent, ultrasound is indicated to diagnose medial epicondylalgia and full rupture of the distal biceps tendon. A summary of recommendations are presented in Table 9. It is important to emphasise that this information is a summary of the results and should be interpreted with consideration of the full results table (Table 8).
Table 9.
Accuracy Summary – Musculoskeletal Clinical Indications for the use of Diagnostic Ultrasound for the Elbow Region
| Target Condition | Recommendation |
|---|---|
| Tendons and soft tissue | |
| Medial epicondylalgia | 3 |
| Lateral epicondylalgia | 3 |
| BTI: full thickness tears | 2 |
| BTI: partial thickness tears | Unknown |
| Bursitis | Unknown |
| LCL and MCL injury | Unknown |
| Triceps tendon injury | Unknown |
| Nerves | |
| Cubital tunnel syndrome | 2 |
| Median nerve entrapment | Unknown |
| Radial nerve compression | Unknown |
| Ulnar nerve subluxation | Unknown |
BTI biceps tendon injury; LCL lateral collateral ligament; MCL medial collateral ligament
Unknown: No diagnostic accuracy studies found
Grade 0: Not indicated
Grade 1: Conflicting evidence (test results should be interpreted with caution)
Grade 2: Equivalent to other imaging techniques (other techniques might provide significant information)
Grade 3: First choice technique (other techniques rarely provide more information)
Wrist/hand
A total of 10 clinical conditions were identified (Table 10). Sixty-three diagnostic studies and four systematic reviews relevant to the accuracy of MSK-DUSI for diagnosing soft-tissue pathology of the wrist/hand were found. The four systematic reviews investigated idiopathic carpal tunnel syndrome [80–83]. The systematic reviews contained 48 of the same articles found in this review. These articles were not treated individually in this review as they were included by way of each systematic review (refer to systematic reviews for these references). This left five relevant diagnostic studies published after the date of the latest systematic review [84–88] and 10 relevant diagnostic studies outside the scope the systematic reviews [89–98]. Therefore, a total of 19 relevant articles were used in this review (15 diagnostic studies and four systematic reviews) [80–98], amounting to 63 individual studies in all. The study characteristics are presented in Table 11.
Table 10.
Identified clinical conditions of the wrist/hand
| Identified clinical conditions of the wrist/hand | Relevant Studies Found (Yes/No) |
|---|---|
| Carpal tunnel syndrome | Y |
| Ligament Injury | Y |
| de Quervains | Y |
| Ganglion Cyst | Y |
| Guyons canal neuropathy | N |
| Wartenberg syndrome | N |
| Intersection syndrome | N |
| Rugby/Jersey finger | N |
| Trigger finger | N |
| Tendinopathy (other) | N |
Table 11.
Wrist/Hand: Study Characteristics
| Study | Target Condition | Number of studies (Systematic Review) | Subjects | Mean Age (years) | Mean time from injury to ultrasound | Ultrasound transducer frequency (MHz) | Ultrasound reviewers |
|---|---|---|---|---|---|---|---|
| Systematic Review | |||||||
| Cartwright et al., 2012 [81] | CTS | 45 | 1450 | N/S | N/S | N/S | RAD and Non-RAD |
| Descatha et al., 2012 [82] | CTS | 13 | 456 | N/S | N/S | 3.0 to 13 | RAD and Non-RAD |
| Roll et al., 2011 [83] | CTS | 23 | 890 | 48 | N/S | 5.0 to 18 | RAD and Non-RAD |
| Beekman et al., 2003 [80] | CTS | 7 | 268 | N/S | N/S | 7.0 to 10 | RAD and Non-RAD |
| Diagnostic Study | |||||||
| Deniz et al., 2012 [84] | CTS | - | 54 | 46 | N/S | 10 | RAD |
| Kim et al., 2012 [85] | CTS | - | 135 | 53 | N/S | N/S | N/S |
| Moghtaderi et al., 2012 [86] | CTS | - | 79 | 43 | N/S | 10 to 13 | RAD |
| Ooi et al., 2014 [87] | CTS | - | 51 | 55 | N/S | 5.0 to 17 | Non-RAD |
| Tajika et al., 2013 [88] | CTS | - | 79 | 58.6 | N/S | 6.0 to 14 | Non-RAD |
| Chuter et al., 2009 [90] | Ligament Injury | - | 127 | 40 | N/S | N/S | N/S |
| Dao et al., 2004 [91] | Ligament Injury | - | 32 | 29 | N/S | 5.0 to 10 | RAD |
| Finlay et al., 2004 [92] | Ligament Injury | - | 26 | 34 | N/S | 9.0 to 13 | RAD |
| Hergan et al., 1995 [93] | Ligament Injury | - | 17 | N/S | N/S | N/S | N/S |
| Melville et al., 2013 [96] | Ligament Injury | - | 26 | 40 | 33 days | 10 to 17 | RAD |
| Taljanovic et al., 2008 [98] | Ligament Injury | - | 16 | 36.4 | <12 months | 9.0 to 12 | RAD |
| Choi et al., 2011 [89] | DQ | - | 13 | 52.4 | 19 months | 5.0 to 17 | RAD |
| Kwon et al., 2010 [95] | DQ | - | 40 | 51 | 7.5 months | 12 to 15 | RAD |
| Kuwano et al., 2009 [94] | Ganglion | - | 183 | N/S | N/S | 8.5 | N/S |
| Osterwalder et al., 1997 [97] | Ganglion | - | 83 | N/S | N/S | 7.5 | RAD |
| - | Guyons canal | - | - | - | - | - | - |
| - | WS | - | - | - | - | - | - |
| - | Rugby/jersey finger | - | - | - | - | - | - |
| - | Trigger Finger | - | - | - | - | - | - |
| - | IS | - | - | - | - | - | - |
| - | T (O) | - | - | - | - | - | - |
N/S not stated; RAD Radiologist; DQ de Quervains; IS intersection syndrome; T (O) tendinopathy (other); CTS carpal tunnel syndrome; WS Wartenberg syndrome
Table 11 reports, the four systematic reviews included a total of 88 diagnostic studies [80–83]. The 19 included studies reviewed 4025 patients [80–98]. The mean age was not stated in six studies [80–82, 93, 94, 97]. In the 13 studies where it was stated the mean age of the cohorts was 45.1 (SD 8.9) [83–92, 95, 96, 98]. Mean time from injury to imaging was not stated in 15 studies [80–88, 90–94, 97]. In the four studies where this was stated [89, 95, 96, 98], this ranged from 33 days [96] to 19 months [89]. The ultrasound reviewers were not stated in four studies [85, 90, 93, 94]. In the 15 studies where this was stated; nine studies documented a radiologist performed and interpreted the images [84, 86, 89, 91, 92, 95–98]; four studies documented a radiologist and non-radiologist were involved [80–83]; in the remaining two studies only non-radiologists were involved [87, 88]. Non-radiologists were either a sonographer or physician [80–83, 87, 88].
The individual SnS, SpC and LRs for the ultrasound diagnosis of musculoskeletal soft-tissue pathology of the wrist/hand are presented in Table 12. The quantitative measure commonly reported to support the diagnosis of idiopathic carpal tunnel syndrome was median nerve thickening at the wrist (cross-sectional area) [80]. Therefore, the results reflect the SnS and SpC of this sonographic characteristic to diagnose carpal tunnel syndrome. The four reviews demonstrate that ultrasound has low to moderate diagnostic value in detecting idiopathic carpal tunnel syndrome and had the potential to be used as a screening tool or as a complementary examination to electrodiagnostic studies, however not as an isolated alternative [80–83]. The five diagnostic studies dated after the systematic reviews reported ultrasound has a moderate to high diagnostic value in the detection of carpal tunnel syndrome [84–88]. The presence of discordance between the results of the systematic reviews and diagnostic studies may be the result of severity of disease, operator-interpreter experience, quality of ultrasound equipment and the cut-off measurement used to determine median nerve thickening. Currently, ultrasound scanning technique and measurements for median nerve thickening are not fully standardised [82].
Table 12.
Accuracy of MSK-DUSI for detecting soft tissue pathology of the wrist/hand
| Target Condition | Study | Reference Standard | Sensitivity | Specificity | LR+ | LR- |
|---|---|---|---|---|---|---|
| Systematic Review | ||||||
| CTS | Cartwright 2012 [81] | Clinical and NCS | 0.65–1.00 | 0.50–0.98 | 1.66–48.5 | 0.00–0.38 |
| Descatha 2012 [82] | Clinical and NCS | 0.84 | 0.78 | 3.82 | 0.21 | |
| Roll 2011 [83] | Clinical and NCS | 0.29 to 1.00 | 0.47 to 1.00 | 1.89–∞ | 0.00–0.71 | |
| Beekman 2003 [80] | NCS | 0.70–0.88 | 0.57–0.96 | 1.70–27.3 | 0.13–0.48 | |
| Diagnostic Study | ||||||
| Deniz 2012 [84] | Clinical and NCS | 0.84 | 0.79 | 4.00 | 0.20 | |
| Kim 2012 [85] | Clinical and NCS | 0.89 | 0.90 | 8.90 | 0.12 | |
| Moghtaderi 2012 [86] | Clinical and NCS | 0.83 | 0.91 | 9.22 | 0.19 | |
| Ooi 2014 [87] | NCS | 0.92 | 0.90 | 9.20 | 0.09 | |
| Tajika 2013 [88] | NCS | 1.00 | 0.99 | 100 | - | |
| Ligament Injury | ||||||
| UCL (displaced) | Chuter 2009 [90] | Surgical Findings | 0.92 | N/S | - | - |
| Hergan 1995 [93] | MRI | 0.88 | 0.83 | 5.18 | 0.15 | |
| Melville 2013 [96] | Surgical Findings | 1.00 | 1.00 | - | - | |
| UCL (non-displaced) | Hergan 1995 [93] | MRI | 0.88 | 0.91 | 9.78 | 0.13 |
| Melville 2013 [96] | Surgical Findings | 1.00 | 1.00 | - | - | |
| Scapholunate | Dao 2004 [91] | Arthroscopy | 0.46 | 1.00 | - | 0.54 |
| Finley 2004 [92] | Arthrography | 1.00 | 1.00 | - | - | |
| Taljanovic 2008 [98] | MRA | 1.00 | 0.92 | 12.5 | - | |
| Lunotriquetral | Finley 2004 [92] | Arthrography | 0.25 | 1.00 | - | 0.75 |
| Taljanovic 2008 [98] | MRA | 0.50 | 0.90 | 5.00 | 0.56 | |
| TFCC | Finley 2004 [92] | Arthrography | 0.64 | 1.00 | - | 0.36 |
| Taljanovic 2008 [98] | MRA | 0.86 | 1.00 | - | 0.14 | |
| de Quervains | Choi 2011 [89] | Surgical Findings | 1.00 | N/S | - | - |
| Kwon 2010 [95] | Surgical Findings | 1.00 | 0.96 | 25.0 | - | |
| Ganglion Cyst | Kuwano 2010 [94] | Surgical Findings | 0.39 | 1.00 | - | 0.61 |
| Osterwalder 1997 [97] | Histology and surgical findings | 0.93 | 0.86 | 6.64 | 0.08 |
UCL ulnar collateral ligament; TFCC triangular fibrocartilage complex; CTS carpal tunnel syndrome
The results showed that ultrasound had high diagnostic value for ulnar collateral ligament (UCL) injury (displaced and non-displaced) [90, 93, 96] and high diagnostic value for ruling in triangular fibrocartilage complex (TFCC) injury, but is less sensitive at ruling it out [92, 98]. The results showed ultrasound had a high accuracy in ruling in scapholunate ligament (SLL) and lunotriquetral ligament (LTL) injury (SpC: >0.90), but there was conflicting SnS for SLL injury and low SnS for LTL injury (<0.50) [91, 92, 98]. This indicates that ultrasound may be no better than chance in excluding injury to the LTL. Dao et al. [91] reported a low SnS (0.46) of ultrasound for detecting SLL injury and although the methodological quality the study was strong it might be explained by the small sample size and difficulty in reproducing dynamic manoeuvres . Refer to Table 12 for the individual SnS, SpC and LR values for the above conditions. This review found no diagnostic studies assessing the accuracy of ultrasound for detecting Guyons canal neuropathy, Wartenberg syndrome, Intersection syndrome, rugby/jersey finger, trigger finger or other tendinopathy.
In the wrist/hand region, the results suggest that MSK-DUSI has moderate diagnostic value for detecting idiopathic carpal tunnel syndrome and is indicated as a screening tool or complementary test to electrodiagnostic studies. To a lesser extent ultrasound is indicated to: rule in and out displaced and non-displaced ulnar collateral ligament tears and de Quervains; rule in ganglions cysts and scapholunate ligament tears, however conflicting results are present for the ability of ultrasound to rule them out; rule in TFCC injury and lunotriquetral ligament tears but not to rule them out. A summary of recommendations are presented in Table 13. It is important to emphasise that this information is a summary of the results and should be interpreted with consideration of the full results table (Table 12).
Table 13.
Accuracy Summary – Musculoskeletal Clinical Indications for the use of Diagnostic Ultrasound for the Wrist/Hand Region
| Target Condition | Recommendation |
|---|---|
| Tendons and soft tissue | Grade |
| de Quervains | 3 |
| Ganglion cyst | 3 |
| Lunotriquetral ligament injury | 2 |
| Ulnar collateral ligament (displaced) | 2 |
| Ulnar collateral ligament (non-displaced) | 2 |
| Scapholunate ligament injury | 1 |
| TFCC injury | 1 |
| Intersection syndrome | Unknown |
| Rugby/jersey finger | Unknown |
| Trigger finger | Unknown |
| Other tendinopathy | Unknown |
| Nerves | |
| Carpal tunnel syndrome | 2 |
| Guyons canal neuropathy | Unknown |
| Wartenberg syndrome | Unknown |
TFCC triangular fibrocartilage complex
Unknown: No diagnostic accuracy studies found
Grade 0: Not indicated
Grade 1: Conflicting evidence (test results should be interpreted with caution)
Grade 2: Equivalent to other imaging techniques (other techniques might provide significant information)
Grade 3: First choice technique (other techniques rarely provide more information)
Hip
A total of 6 clinical conditions were identified (Table 14). Eight diagnostic studies and one systematic review relevant to the accuracy of MSK-DUSI for diagnosing soft-tissue pathology of the hip were found. The systematic review investigated gluteal tendon tears [99]. The systematic review contained seven of the same articles found in this review. These articles were not treated individually in this review as they were included by way of the systematic review (refer to systematic reviews for these references). No other relevant diagnostic studies published after the date of the latest systematic review were found. Two relevant diagnostic studies outside the scope the systematic reviews were found [100, 101]. Therefore, a total of three relevant articles were used in this review (two diagnostic studies and one systematic review) [99–101], amounting to nine individual studies in all. The study characteristics are presented in Table 15.
Table 14.
Identified clinical conditions of the hip
| Identified clinical conditions of the hip | Relevant Studies Found (Yes/No) |
|---|---|
| Muscle/tendon injury (gluteal, psoas, hamstrings, quadriceps) | Y |
| Bursitis (trochanteric, iliopsoas) | Y |
| Meralgia paresthetica | Y |
| Snapping hip syndrome (extra-articular) | N |
| Sciatica | N |
| Femoral nerve injury | N |
Table 15.
Hip: Study Characteristics
| Study | Target Condition | Number of studies (Systematic Review) | Subjects | Mean Age (years) | Mean time from injury to ultrasound | Ultrasound transducer frequency (MHz) | Ultrasound reviewers |
|---|---|---|---|---|---|---|---|
| Systematic Review | |||||||
| Westacott et al., 2011 [99] | Muscle/Tendon Injury | 7 | N/S | N/S | N/S | 7.5 to 18 | RAD |
| Diagnostic Study | |||||||
| Fearon et al., 2010 [100] | Bursitis | - | 24 | 56 | 33.8 months | 7.0 | N/S |
| Suh et al., 2013 [101] | LFC/MP | - | 23 | 46 | 4 months | 5.0 to 12 | Non-RAD |
| - | Sciatica | - | - | - | - | - | - |
| - | Femoral Nerve | - | - | - | - | - | - |
| - | Snapping hip (E) | - | - | - | - | - | - |
N/S not stated; RAD Radiologist; LFT/MP lateral femoral cutaneous/meralgia paresthetica; (E) (extra-articular)
Table 15 reports, the one systematic review included seven diagnostic studies [99]. One study did not state the number of subjects [99]. In the two studies where this was stated the studies reviewed 47 patients [100, 101]. The mean age was not stated in one study [99]. In the two studies where this was stated the mean age of the cohorts was 51 (SD 7.1) [100, 101]. Mean time from injury to imaging was not stated in one study [99]. In the two studies where this was stated [100, 101], this ranged from 4 months [101] to 33.8 months [100]. One study did not report on who performed and reviewed the ultrasound images [100]. In the two studies where this was reported, one study recorded that a radiologist performed and interpreted the images [99] and in the remaining study a sonographer performed and interpreted the images [101].
The individual SnS, SpC and LRs for the ultrasound diagnosis of musculoskeletal soft-tissue pathology of the hip are presented in Table 16. The results of the systematic review demonstrate that ultrasound has moderate to high diagnostic accuracy for detecting any tear of the gluteal tendon and may prove to be the investigation of choice [99]. The results show that ultrasound has a moderate diagnostic value for ruling out trochanteric bursitis, but has high diagnostic value of ruling it in [100]. For meralgia paresthetica the results show that ultrasound has a high diagnostic value for detecting meralgia paresthetica [101]. This review found no diagnostic studies assessing the accuracy of ultrasound diagnosis muscle or tendon injury of the psoas, hamstrings and quadriceps; iliopsoas bursitis, snapping hip syndrome (extra-articular), sciatica, or femoral nerve injury.
Table 16.
Accuracy of MSK-DUSI for detecting soft tissue pathology of the hip
| Target Condition | Study | Reference Standard | Sensitivity | Specificity | LR+ | LR- |
|---|---|---|---|---|---|---|
| Systematic Review | ||||||
| Gluteal Tendon Tear | Westacott 2011 [99] | MRI | 0.79–1.00 | 0.95–1.00 | 15.8–∞ | 0.00–0.21 |
| Diagnostic Study | ||||||
| Trochanteric bursitis | Fearon 2010 [100] | Surgical findings and histology | 0.69 | 1.00 | - | 0.31 |
| LFC/MP | Suh 2013 [101] | Clinical and NCS | 0.96 | 0.96 | 24.0 | 0.04 |
LFT/MP lateral femoral cutaneous/meralgia paresthetica
In the hip region, the results suggest the use of MSK-DUSI is indicated for any gluteal tendon tear due to its moderate to high diagnostic accuracy and to a lesser extent for the diagnosis of trochanteric bursitis and meralgia paresthetica. A summary of recommendations are presented in Table 17. It is important to emphasise that this information is a summary of the results and should be interpreted with consideration of the full results table (Table 16).
Table 17.
Accuracy Summary – Musculoskeletal Clinical Indications for the use of Diagnostic Ultrasound for the Hip Region
| Target Condition | Recommendation |
|---|---|
| Tendons and soft tissue | Grade |
| Gluteal tendon tears | 3 |
| Trochanteric bursitis | 2 |
| Iliopsoas bursitis | Unknown |
| Psoas/hamstring/quadriceps injury | Unknown |
| Snapping hip syndrome (extra-articular) | Unknown |
| Nerves | |
| Meralgia paresthetica | 3 |
| Femoral nerve injury | Unknown |
| Sciatica (causes) | Unknown |
Unknown: No diagnostic accuracy studies found
Grade 0: Not indicated
Grade 1: Conflicting evidence (test results should be interpreted with caution)
Grade 2: Equivalent to other imaging techniques (other techniques might provide significant information)
Grade 3: First choice technique (other techniques rarely provide more information)
Knee
A total of 19 clinical conditions were identified (Table 18). Twenty diagnostic studies pertaining to the accuracy of MSK-DUSI for diagnosing musculoskeletal soft-tissue pathology of the knee were found [102–121]. No systematic reviews were found. The study characteristics are presented in Table 19.
Table 18.
Identified clinical conditions of the knee
| Identified clinical conditions of the knee | Relevant studies found (Yes/No) |
|---|---|
| Quadriceps tendon injury | Y |
| Patella tendon injury | Y |
| Popliteus tendon injury | Y |
| Anterior cruciate ligament injury | Y |
| Lateral collateral ligament injury | Y |
| Plica syndrome | Y |
| Baker’s cyst | Y |
| Meniscal tears | Y |
| Meniscal cyst | Y |
| Common peroneal neuropathy | Y |
| Bursitis | N |
| Ganglion | N |
| Iliotibial band friction syndrome | N |
| Hoffer’s fat pad syndrome | N |
| Retinacula pathology | N |
| Medial collateral ligament injury | N |
| Posterior cruciate ligament injury | N |
| Hamstring injury | N |
| Gastrocnemius injury | N |
Table 19.
Knee: Study Characteristics
| Study | Target Condition | Number of studies (Systematic Review) | Subjects | Mean Age (years) | Mean time from injury to ultrasound | Ultrasound transducer frequency (MHz) | Ultrasound reviewers |
|---|---|---|---|---|---|---|---|
| Diagnostic Study | |||||||
| Bianchi et al., 1994 [104] | Tendinopathy/Tear | - | 29 | 41 | N/S | 7.5 | RAD |
| Garrick et al., 2008 [107] | Tendinopathy/Tear | - | 63 | N/S | N/S | 10 to 14 | RAD |
| Sekiya et al., 2010 [114] | Tendinopathy/Tear; Ligament Injury | - | 16 | N/S | N/S | 10 to 14 | RAD |
| Warden et al., 2007 [120] | Tendinopathy/Tear | - | 30 | 27 | N/S | 10 to 14 | RAD |
| Ward et al., 2001 [119] | Baker’s Cyst | - | 36 | 46 | 78 days | 7.0 to 10 | RAD |
| Derks et al., 1986 [105] | Plica syndrome | - | 38 | N/S | N/S | 7.5 | RAD |
| Paczesny et al., 2009 [110] | Plica Syndrome | - | 88 | 20 | 6 months | 12 | Non-RAD |
| Fuchs et al., 2002 [106] | Ligament Injury | - | 193 | N/S | N/S | 10 to 14 | RAD |
| Khan et al., 2006 [108] | Ligament Injury; Meniscal Tear | - | 60 | 35 | N/S | 7.5 | RAD |
| Ptasznik et al., 1995 [112] | Ligament Injury | - | 37 | 27 | 3.3 weeks | 7.5 | RAD |
| Skovgaard et al., 2000 [116] | Ligament Injury | - | 62 | 29.2 | 9 days | 7.0 | RAD |
| Alizadeh et al., 2013 [102] | Meniscal Tear | - | 37 | 43.5 | N/S | 14 | RAD |
| Azzoni et al., 2002 [103] | Meniscal Tear | - | 216 | 27.5 | N/S | 7.5 to 10 | RAD |
| Najafi et al., 2006 [109] | Meniscal Tear | - | 100 | N/S | N/S | 6.5 | RAD |
| Park et al., 2008 [79] | Meniscal Tear | - | 22 | 50.4 | N/S | 7.5 to 15 | RAD |
| Shetty et al., 2008 [115] | Meniscal Tear | - | 35 | 47 | N/S | 5.0 to 13 | RAD |
| Wareluk et al., 2012 [121] | Meniscal Tear | - | 80 | 36.2 | <1 month | 6.0 to 12 | Non-RAD |
| Rutten et al., 1998 [113] | Meniscal cyst/Meniscal Tear | - | 50 | 51 | N/S | 7.5 | N/S |
| Sorrentino et al., 2007 [117] | Meniscal cyst | - | 104 | 43 | N/S | 7 to 12 | RAD |
| Visser et al., 2013 [118] | Nerve Injury | - | 103 | 53 | 5 weeks | 7 to 18 | N/S |
| - | Bursitis | - | - | - | - | - | - |
| - | Ganglion | - | - | - | - | - | - |
| - | ITB friction | - | - | - | - | - | - |
| - | HFPS | - | - | - | - | - | - |
| - | Retinacula | - | - | - | - | - | - |
N/S not stated; RAD Radiologist; ITB iliotibial band; HFPS Hoffer’s fat pad syndrome
Table 19 reports, the 20 included studies reviewed 1399 patients [102–121]. The mean age was not stated in five studies [105–107, 109, 114]. In the 15 studies where it was stated the mean age of the cohorts was 38.5 (SD 10.4) [102–104, 108, 110–113, 115–121]. Mean time from injury to imaging was not stated in 14 studies [102–104, 106–109, 111, 113–115, 117, 119, 120]. In the six studies where this was stated [110, 112, 116, 118, 119, 121], it ranged from 3.3 days [112] to 6 months [110]. Two studies did not report on who performed and reviewed the ultrasound images [113, 118]. In the 18 studies where this was reported, 16 studies recorded a radiologist performed and interpreted the images [102–109, 111, 112, 114–117, 119, 120] and in two studies a non-radiologist performed and interpreted the images [110, 121]. The non-radiologists were a sonographer and a physician [110, 121].
The individual SnS, SpC and LRs for the ultrasound diagnosis of musculoskeletal soft-tissue pathology of the knee are presented in Table 20. The results show that ultrasound has a moderate to high diagnostic value for medial and lateral meniscal tears [102, 103, 108, 109, 111, 113, 115, 121]. The results show that ultrasound has a high diagnostic value for full quadriceps tendons tears [104], moderate for patella tendinopathy [107, 120] and injury to the popliteal tendon [114].. Five studies assessed the accuracy of ultrasound detection of ligamentous injury [106, 108, 112, 114, 116]. The results show that ultrasound has moderate to high diagnostic value for full anterior cruciate ligament tears [106, 108, 112, 116] and high diagnostic value at ruling in lateral collateral ligament tears, but low diagnostic value in ruling them out [114]. Ultrasound had a 100 % false negative rate for detecting partial anterior cruciate ligament tears [108]. The results show that ultrasound has high diagnostic value for Baker’s cysts [119] and meniscal cysts [113, 117], with moderate to high diagnostic value for medial-patella plica syndrome [105, 110]. Ultrasound can rule out common peroneal nerve neuropathy with high accuracy, but in less specific at ruling it in [118]. This review found no diagnostic studies assessing the accuracy of ultrasound for detecting muscle or tendon pathology of the hamstrings, iliotibial band and gastrocnemius; pes anserinus tendinobursitis, medial collateral ligament or posterior cruciate ligament injury, ganglions, retinacula pathology or Hoffa’s fat pad syndrome.
Table 20.
Accuracy of MSK-DUSI for detecting soft tissue pathology of the knee
| Target Condition | Study | Reference Standard | Sensitivity | Specificity | LR+ | LR- |
|---|---|---|---|---|---|---|
| Tendinopathy/Tear | Diagnostic Study | |||||
| Full QTT | Bianchi 1994 [104] | Surgical Findings | 1.00 | 1.00 | - | - |
| Patella Tendinopathy | Garrick 2008 [107] | Clinical and MRI | 0.87 | 0.79 | 4.14 | 0.16 |
| Warden 2007 [120] | Clinical and MRI | 0.87 | 0.82 | 4.83 | 0.16 | |
| Popliteus Tear | Sekiya 2010 [114] | Surgical Findings | 0.67 | 0.75 | 2.68 | 0.44 |
| Ligament Injury | ||||||
| Full ACL Tear | Fuchs 2002 [106] | MRI | 0.91 | 0.80 | 4.55 | 0.11 |
| Khan 2006 [108] | MRI and Arthroscopy | 0.79 | 1.00 | - | 0.21 | |
| Ptasznik 1995 [112] | Arthroscopy | 0.91 | 1.00 | - | 0.09 | |
| Skovgaard 2000 [116] | Arthroscopy | 0.88 | 0.98 | - | - | |
| Partial ACL Tear | Khan 2006 [108] | MRI and Arthroscopy | 0.00 | 0.00 | - | - |
| LCL | Sekiya 2010 [114] | Surgical Findings | 0.33 | 1.00 | -. | 0.67 |
| Plica Syndrome | Derks 1986 [105] | Arthroscopy | 0.92 | 0.73 | 3.41 | 0.11 |
| Paczesny 2009 [110] | Arthroscopy | 0.90 | 0.83 | 5.29 | 0.12 | |
| Baker’s Cyst | Ward 2001 [119] | MRI | 1.00 | 1.00 | - | - |
| Meniscal Tear | ||||||
| Medial Meniscus | Alizadeh 2013 [102] | MRI | 0.83 | 0.71 | 2.86 | 0.24 |
| Azzoni 2002 [103] | MRI | 0.60 | 0.21 | 0.76 | 1.90 | |
| Khan 2006 [108] | MRI and Arthroscopy | 0.93 | 0.93 | 13.3 | 0.08 | |
| Najafi 2006 [109] | Arthroscopy | 1.00 | 0.95 | 20 | 0.00 | |
| Park 2008 [79] | MRI | 0.86 | 0.85 | 5.73 | 0.16 | |
| Rutten 1998 [113] | Surgical Findings | 0.82 | 0.75 | 3.29 | 0.24 | |
| Shetty 2008 [115] | MRI | 0.86 | 0.69 | 2.77 | 0.20 | |
| Wareluk 2012 [121] | Arthroscopy | 0.93 | 0.73 | 3.44 | 0.10 | |
| Lateral Meniscus | Khan 2006 [108] | MRI and Arthroscopy | 0.88 | 1.00 | - | 0.12 |
| Najafi 2006 [109] | Arthroscopy | 0.93 | 1.00 | - | 0.07 | |
| Park 2008 [79] | MRI | 0.86 | 0.85 | 5.73 | 0.16 | |
| Rutten 1998 [113] | Surgical Findings | 0.82 | 0.75 | 3.29 | 0.24 | |
| Wareluk 2012 [121] | Arthroscopy | 0.67 | 0.96 | 16.8 | 0.34 | |
| Meniscal Cyst | Rutten 1998 [113] | Surgical Findings | 0.97 | 0.86 | 6.93 | 0.03 |
| Sorrentino 2007 [117] | MRI | 0.94 | 1.00 | - | 0.06 | |
| Nerve Injury | ||||||
| Common Peroneal Neuropathy | Visser 2013 [118] | NCS | 0.90 | 0.69 | 2.90 | 0.14 |
QTT quadriceps tendon tear; ACL anterior cruciate ligament; LCL lateral collateral ligament
In the knee region, the results suggest MSK-DUSI may be indicated as a screening tool for medial and lateral meniscus tears due to its moderate to high diagnostic accuracy. To a lesser extent ultrasound may be used for the diagnosis of full-thickness quadriceps tendon tears, patella tendinopathy, full-thickness anterior cruciate ligament tears, medial patella plica syndrome, Baker’s cysts and meniscal cysts. Ultrasound can rule in lateral collateral ligament and popliteus tears but is less sensitive at ruling it out and can rule out common peroneal nerve neuropathy but is less sensitive at ruling it in. Ultrasound is not indicated for partial-thickness anterior cruciate ligament tears. A summary of recommendations are presented in Table 21. It is important to emphasise that this information is a summary of the results and should be interpreted with consideration of the full results table (Table 20).
Table 21.
Accuracy Summary – Musculoskeletal Clinical Indication for Diagnostic Ultrasound of the Knee Region
| Target Condition | Recommendation |
|---|---|
| Tendons and soft tissue | Grade |
| Full thickness quadriceps tendon tears | 3 |
| Patella tendinopathy | 3 |
| Baker’s Cyst | 2 |
| Medial patella plica syndrome | 2 |
| Meniscal cyst | 2 |
| Ganglion cyst | Unknown |
| Hamstring/ITB/gastrocnemius injury | Unknown |
| Hoffa’s fat pad syndrome | Unknown |
| Pes anserinus tendinobursitis | Unknown |
| Internal knee derangement and associated injury | |
| Full ACL tears | 0a |
| Partial ACL tears | 0 |
| Medial meniscus tears | 0a |
| Lateral meniscus tears | 0a |
| LCL injury | 0a |
| Popliteal injury | 0a |
| MCL injury | Unknown |
| PCL injury | Unknown |
| Nerves | |
| Common peroneal neuropathy | 2 |
ACL anterior cruciate ligament; PCL posterior cruciate ligament; LCL lateral collateral ligament; MCL medial collateral ligament; ITB iliotibial band
Unknown: No diagnostic accuracy studies found
Grade 0a: Not indicated as a definitive diagnostic tool for ligamentous and meniscal tears of the knee, however may have a role as an on field, point-of-care screening tool
Grade 0: Not indicated
Grade 1: Conflicting evidence (test results should be interpreted with caution)
Grade 2: Equivalent to other imaging techniques (other techniques might provide significant information)
Grade 3: First choice technique (other techniques rarely provide more information)
Ankle/foot
A total of 20 clinical conditions were identified (Table 22). Thirty-five diagnostic articles relevant to the accuracy of MSK-DUSI for diagnosing soft-tissue pathology of the ankle/foot were found [122–156]. No systematic reviews were found. The study characteristics are presented in Table 12.
Table 22.
Identified clinical conditions of the ankle/foot
| Identified clinical conditions of the ankle/foot | Relevant studies found (Yes/No) |
|---|---|
| Plantaris tendon injury | Y |
| Plantar plate injury | Y |
| Peroneal tendon injury | Y |
| Achilles tendon injury | Y |
| Posterior tibial tendon injury | Y |
| Anterior talofibular ligament injury | Y |
| Posterior talofibular ligament injury | Y |
| Calcaneofibular ligament injury | Y |
| Deltoid ligament injury | Y |
| Syndesmotic injury | Y |
| Morton’s neuroma | Y |
| Anterolateral impingement | Y |
| Peroneal subluxation | Y |
| Plantar fasciitis | Y |
| Tarsal tunnel syndrome | N |
| Bursitis | N |
| Retinacula pathology | N |
| Ganglion | N |
| Tibialis anterior injury | N |
| Gastrocnemius tears | N |
Table 23 reports, the 35 included studies reviewed 1713 patients [122–156]. The mean age was not stated in nine studies [133, 137–139, 141, 150, 153, 155, 156]. In the 26 studies where it was stated the mean age of the cohorts was 42.7 (SD 9.9) [122–132, 134–136, 140, 142–149, 151, 152, 154]. Mean time from injury to imaging was not stated in 24 studies [123, 125, 126, 128, 130, 131, 133–140, 144, 145, 147–151, 153, 154, 156]. In the 11 studies where this was stated [122, 124, 127, 129, 132, 141–143, 146, 152, 155], this ranged from <2 days [132] to 14 months [142]. Two studies did not report on who performed and reviewed the ultrasound images [134, 148]. In the 34 studies where this was reported, 24 studies recorded a radiologist performed and interpreted the images [122, 124–127, 131, 133, 135–137, 140–143, 147, 149–156]; in two studies a radiologist and non-radiologist were involved [123, 128]; and in eight studies only a non-radiologist was involved [129, 130, 132, 138, 139, 144–146]. The non-radiologists consisted of either a sonographer or a physician [123, 128–130, 132, 139, 144–146].
Table 23.
Ankle/Foot: Study Characteristics
| Study | Target Condition | Number of studies (Systematic Review) | Subjects | Mean Age (years) |
Mean time from injury to ultrasound | Ultrasound transducer frequency (MHz) | Ultrasound reviewers |
|---|---|---|---|---|---|---|---|
| Diagnostic Study | |||||||
| Bianchi et al., 2011 [122] | Tendinopathy/Tear | - | 5 | 47.2 | 8 days | 12.5 to 17.5 | RAD |
| Carlson et al., 2013 [123] | Tendinopathy/Tear | - | 8 | 51.9 | N/S | N/S | RAD and Non-RAD |
| Grant et al., 2005 [127] | Tendinopathy/Tear | - | 58 | 45.2 | 11.2 months | 11 to 15 | RAD |
| Gregg et al., 2006 [128] | Tendinopathy/Tear | - | 52 | 57 | N/S | 11 | RAD and Non-RAD |
| Hartgerink et al., 2001 [131] | Tendinopathy/Tear | - | 26 | 40 | N/S | 7.5 to 12 | RAD |
| Kainberger et al., 1990 [134] | Tendinopathy/Tear | - | 73 | 38 | N/S | 5.0 to 10 | N/S |
| Kalebo et al., 1992 [135] | Tendinopathy/Tear | - | 37 | 35 | N/S | 7.5 | RAD |
| Kayser et al., 2005 [137] | Tendinopathy/Tear | - | 13 | N/S | N/S | 7.5 | RAD |
| Klein et al., 2012 [138] | Tendinopathy/Tear | - | 42 | N/S | N/S | 15 to 16 | Non-RAD |
| Klein et al., 2013 [139] | Tendinopathy/Tear | - | 50 | N/S | N/S | 15 to 16 | Non-RAD |
| Nallamshetty et al., 2005 [144] | Tendinopathy/Tear | - | 18 | 61 | N/S | 10 | Non-RAD |
| Premkumar et al., 2002 [149] | Tendinopathy/Tear | - | 31 | 43 | N/S | 10 | RAD |
| Rockett et al., 1998 [150] | Tendinopathy/Tear | - | 28 | N/S | N/S | 7.5 to 10 | RAD |
| Waitches et al., 1998 [156] | Tendinopathy/Tear | - | 33 | N/S | N/S | 7.5 to10 | RAD |
| Cheng et al., 2014 [124] | Ligament Injury | - | 120 | 32 | 2.2 years | 5.0 to 17 | RAD |
| Guillodo et al., 2010 [129] | Ligament Injury | - | 56 | 30.1 | 7.6 months | 5.0 to 12 | Non-RAD |
| Gun et al., 2013 [130] | Ligament Injury | - | 65 | 34 | N/S | 7.5 | Non-RAD |
| Henari et al., 2011 [132] | Ligament Injury | - | 12 | 41 | <2 days | N/S | Non-RAD |
| Hua et al., 2012 [133] | Ligament Injury | - | 83 | N/S | N/S | 7.5 | RAD |
| Margetic et al., 2012 [141] | Ligament Injury | - | 30 | N/S | 1 week | 7.0 to 15 | RAD |
| Mei-Dan et al., 2009 [143] | Ligament Injury | - | 47 | 27 | 12 days | 7.5 to 12 | RAD |
| Oae et al., 2010 [146] | Ligament Injury | - | 34 | 29 | 1 week | 9.0 | Non-RAD |
| van Dijk et al., 1996 [155] | Ligament Injury | - | 160 | N/S | <1 week | N/S | RAD |
| Fazal et al., 2012 [126] | Morton’s Neuroma | - | 47 | 46 | N/S | 5.0 t o12 | RAD |
| Kankanala et al., 2007 [136] | Morton’s Neuroma | - | 48 | 52.6 | N/S | 13.5 | RAD |
| Lee et al., 2007 [140] | Morton’s Neuroma | - | 17 | 48.6 | N/S | 9.0 | RAD |
| Oliver et al., 1998 [147] | Morton’s Neuroma | - | 37 | 49.6 | N/S | 7.5 | RAD |
| Pastides et al., 2012 [148] | Morton’s Neuroma | - | 36 | 43.8 | N/S | N/S | N/S |
| Sharp et al., 2003 [152] | Morton’s neuroma | - | 25 | 52 | 8 months | 12 | RAD |
| Sobiesk et al., 1997 [153] | Morton’s Neuroma | - | 20 | N/S | N/S | 7.5 | RAD |
| Torres-Claramunt et al., 2012 [154] | Morton’s Neuroma | - | 37 | 60.6 | N/S | 7.5 to 9.0 | RAD |
| Cochet et al., 2010 [125] | Impingement | - | 41 | 32 | N/S | 5.0 to 12 | RAD |
| McCarthy et al., 2008 [142] | Impingement | - | 17 | 32 | 14 months | 5.0 to 12 | RAD |
| Neustadter et al., 2004 [145] | Peroneal Subluxation | - | 13 | 30.4 | N/S | 12 to 13 | Non-RAD |
| Sabir et al., 2005 [151] | Plantar Fasciitis | - | 77 | 45.9 | N/S | 6.0 to 9.0 | RAD |
| - | TTS | - | - | - | - | - | - |
| - | Bursitis | - | - | - | - | - | - |
| - | Retinacula | - | - | - | - | - | - |
| - | Ganglion | - | - | - | - | - | - |
N/S not stated; RAD Radiologist; TTS tarsal tunnel syndrome
The individual SnS, SpC and LRs for the ultrasound diagnosis of musculoskeletal soft-tissue pathology of the ankle/foot are presented in Table 24. The results show that ultrasound has high diagnostic value for peroneal subluxation [145], anterior talofibular [124, 129, 130, 133, 141, 146, 155], posterior talofibular [124], calcaneofibular [124, 141], deltoid [132] and syndesmotic ligament injury [143]. The high accuracy of posterior talofibular ligament injury was based off one subject, therefore the use of ultrasound for this condition is not recommended due to lack of evidence. Ultrasound has high diagnostic accuracy for ruling in Morton’s neuroma, but is less sensitive at ruling it out [126, 136, 140, 147, 148, 152–154].
Table 24.
Accuracy of MSK-DUSI for detecting soft tissue pathology of the ankle/foot
| Target Condition | Study | Reference Standard | Sensitivity | Specificity | LR+ | LR- |
|---|---|---|---|---|---|---|
| Diagnostic Study | ||||||
| Tendinopathy/Tear | ||||||
| Plantaris Tendon Tear | Bianchi 2011 [122] | MRI | 1.00 | 1.00 | - | - |
| Plantar Plate Tear | Carlson 2013 [123] | Surgical Findings | 1.00 | 0.60 | 2.50 | - |
| Gregg 2006 [128] | MRI | 0.86 | 0.64 | 2.39 | 0.22 | |
| Klein 2013 [139] | MRI | 0.91 | 0.25 | 1.21 | 0.36 | |
| Klein 2012 [138] | MRI | 0.92 | 0.25 | 1.23 | 0.32 | |
| Peroneal Tendon Tear | Grant 2005 [127] | Surgical Findings | 1.00 | 0.85 | 6.67 | - |
| Waitches 1998 [156] | Surgical Findings | 1.00 | 0.79 | 4.76 | - | |
| Achilles Tendinopathy | Hartgerink 2001 [131] | Surgical Findings | 1.00 | 0.83 | 5.88 | - |
| Kainberger 1990 [134] | Clinical and MRI | 0.72 | 0.83 | 4.24 | 0.34 | |
| Kalebo 1992 [135] | Surgical Findings | 0.94 | 1.00 | - | 0.06 | |
| Kayser 2005 [137] | MRI | 0.50 | 0.81 | 2.63 | 0.62 | |
| Posterior Tibial Tendinopathy | Nallamshetty 2005 [144] | MRI | 0.78 | 1.00 | - | 0.22 |
| Premkumar 2002 [149] | MRI | 0.80 | 0.90 | 8.00 | 0.22 | |
| Rockett 1998 [150] | Surgical Findings | 1.00 | 0.90 | 10.0 | - | |
| Waitches 1998 [156] | Surgical Findings | 1.00 | 1.00 | - | - | |
| Ligament Injury | ||||||
| ATF | Cheng 2014 [124] | Surgical Findings | 0.99 | 0.96 | 24.8 | 0.01 |
| Guillodo 2010 [129] | Arthrography | 0.85 | 1.00 | - | 0.15 | |
| Gun 2013 [130] | MRI | 0.94 | 1.00 | - | 0.06 | |
| Hua 2012 [133] | Surgical Findings | 0.98 | 0.92 | 12.3 | 0.02 | |
| Margetic 2012 [141] | MRI | 1.00 | 1.00 | - | - | |
| Oae 2010 [146] | Surgical Findings | 1.00 | 0.33 | 1.49 | - | |
| van Dijk 1996 [155] | Arthrography | 0.92 | 0.64 | 2.56 | 0.13 | |
| PTF | Cheng 2014 [124] | Surgical Findings | 1.00 | 1.00 | - | - |
| CF | Cheng 2014 [124] | Surgical Findings | 0.94 | 0.91 | 10.4 | 0.07 |
| Margetic 2012 [141] | MRI | 1.00 | 1.00 | - | - | |
| Deltoid | Henari 2011 [132] | Arthrography | 1.00 | 1.00 | - | - |
| Syndesmotic | Mei-Dan 2009 [143] | MRI | 1.00 | 1.00 | - | - |
| Morton’s Neuroma | Fazal 2012 [126] | Surgical Findings | 0.96 | 1.00 | - | 0.04 |
| Kankanla 2007 [136] | Surgical and Histology | 0.91 | 1.00 | - | 0.09 | |
| Lee 2007 [140] | Surgical Findings | 0.79 | 1.00 | - | 0.21 | |
| Oliver 1998 [147] | Surgical and Histology | 0.96 | 1.00 | - | 0.04 | |
| Pastides 2012 [148] | Surgical Findings | 0.90 | 1.00 | - | 0.10 | |
| Sharp 2003 [152] | Surgical and Histology | 0.79 | 1.00 | - | 0.21 | |
| Sobiesk 1997 [153] | Surgical Findings | 1.00 | 0.83 | 5.88 | - | |
| Torres-Claramunt 2012 [154] | Surgical and Histology | 0.57 | 1.00 | - | 0.43 | |
| Anterolateral Impingement | Cochet 2010 [125] | Arthrography | 0.77 | 0.57 | 1.79 | 0.40 |
| McCarthy 2008 [142] | Surgical Findings | 1.00 | 1.00 | - | - | |
| Peroneal Subluxation | Neustadter 2004 [145] | Surgical Findings | 1.00 | 1.00 | - | - |
| Plantar Fasciitis | Sabir 2005 [151] | MRI | 0.80 | 0.89 | 7.27 | 0.22 |
ATF anterior talofibular; PTF posterior talofibular; CF calcaneofibular
The results show that ultrasound has high diagnostic value for plantaris tendon tears [122]; moderate to high for peroneal tendon tears [127, 156], Achilles tendinopathy [131, 134, 135, 137] and posterior tibial tendinopathy [144, 149, 150, 156]; moderate for plantar fasciitis [151]. Ultrasound can rule out plantar plate tears with high accuracy, but has low accuracy when ruling them in [123, 128, 138, 139]. The low SpC significantly reduces the overall accuracy of ultrasound for this condition. Two studies assessed the accuracy of ultrasound detection of anterolateral ankle impingement, reporting significant differences in SnS and SpC [125, 142]. The difference in diagnostic accuracy is likely due to the heterogenic study population and study size. Cochet et al. [125] report on 41 subjects from the general population whereas McCarthy et al. [142] reported on 17 subject from a population of elite athletes. This review found no diagnostic studies assessing the accuracy of ultrasound diagnosis for tibialis anterior tendinopathy, gastrocnemius tears, bursitis, retinaculum pathology, ganglion or tarsal tunnel syndrome.
In the ankle/foot region, the results suggest the use of MSK-DUSI is indicated for anterior talofibular ligament injury and Morton’s neuroma due to its high diagnostic accuracy. To a lesser extent ultrasound may be used for the diagnosis of plantaris tendon tears, peroneal tendon tears, posterior tibial tendinopathy; calcaneofibular ligament, deltoid ligament and syndesmotic injury; peroneal subluxation and plantar fasciitis. There is conflicting evidence to indicate ultrasound for the detection of Achilles tendon tendinopathy and anterolateral ankle impingement. Ultrasound can rule out plantar plate tears but it is less sensitive at ruling them in. Ultrasound is not indicated for posterior talofibular ligament injury. A summary of recommendations are presented in Table 25. It is important to emphasise that this information is a summary of the results and should be interpreted with consideration of the full results table (Table 24).
Table 25.
Accuracy Summary - Musculoskeletal Clinical Indications for Diagnostic Ultrasound Imaging in the Ankle/Foot Region
| Target Condition | Recommendation |
|---|---|
| Tendons and soft tissue | Grade |
| Anterior talofibular ligament injury | 3 |
| Calcaneofibular ligament injury | 3 |
| Peroneal tendon tears | 3 |
| Peroneal subluxation | 3 |
| Posterior tibial tendinopathy | 3 |
| Plantaris Tendon tears | 3 |
| Plantar fasciitis | 3 |
| Achilles tendinopathy | 2 |
| Deltoid ligament injury | 2 |
| Plantar plate tears | 2 |
| Syndesmotic Injury | 2 |
| Anterolateral ankle impingement | 0 |
| Posterior talofibular ligament injury | 0 |
| Bursitis | Unknown |
| Ganglion cyst | Unknown |
| Retinaculum pathology | Unknown |
| Tibialis anterior tendinopathy | Unknown |
| Nerves | |
| Morton’s neuroma | 2 |
| Tarsal tunnel syndrome | Unknown |
Unknown: No diagnostic accuracy studies found
Grade 0: Not indicated
Grade 1: Conflicting evidence (test results should be interpreted with caution)
Grade 2: Equivalent to other imaging techniques (other techniques might provide significant information)
Grade 3: First choice technique (other techniques rarely provide more information)
Discussion
Diagnostic ultrasound is a common imaging modality used to assist in the diagnosis of musculoskeletal complaints when the clinical picture is uncertain [34]. The aim of this study was to undertake a comprehensive review of the literature to assess the diagnostic accuracy of MSK-DUSI for the diagnosis of soft tissue pathology of the extremities. All musculoskeletal soft-tissue conditions identified by the ESMR and ACR MSK-DUSI guidelines were included in this review [3, 55]. This review does not cover the entire utility of this technology.
This discussion section is divided into sub-sections. These relate to the anatomical areas discussed in the results section and include shoulder, elbow, wrist/hand, hip, knee, and ankle/foot.
Shoulder
Shoulder complaints are common in primary and secondary care settings [157, 158]. Most shoulder complaints present with similar signs and symptoms, often making a definitive diagnosis difficult. Even following a thorough history and physical examination there is often a significant degree of clinical uncertainty [159]. An accurate diagnosis is essential to ensure that patients receive appropriate and timely treatment and correct information regarding their prognosis. Overall, the results showed that MSK-DUSI was a useful imaging method to accurately detect certain musculoskeletal disorders of the shoulder. Importantly, the results demonstrated high discriminatory ability for detecting any rotator cuff tear and the ability to rule in rotator cuff atrophy with moderate to high accuracy. This is desirable, because surgical repair is sometimes required and positive post-operative outcomes have been correlated with early surgical repair [160, 161] and the absence of rotator cuff atrophy [162]. For partial thickness rotator cuff tears it is important to emphasise that it is easier to rule it in (SpC: 0.75 to 0.98; LR + = 1.84 to 35.5) than to rule it out (SnS: 0.46 to 0.84; LR- = 0.18 to 0.72).
Based on the results for the shoulder region it seemed that the use of MSK-DUSI is indicated for any rotator cuff tear, subacromial bursitis, calcific tendinitis, rotator cuff tendinopathy, rotator cuff atrophy, subacromial impingement syndrome and long head of the biceps pathology.
Elbow
The utility of MSK-DUSI for the elbow has been well-described [3], however this review found limited diagnostic studies in this area, with the exception of lateral epicondylalgia and cubital tunnel syndrome. The results showed that hypoechogenity of the common extensor origin had the best combination of diagnostic SnS and SpC in determining elbows with lateral epicondylalgia. Other ultrasound features found in chronic cases include neovascularity, calcifications and cortical irregularities which show high SpC but very low SnS. There was little clarity on the role of these findings in the diagnosis of lateral epicondylalgia [76]. The use of MSK-DUSI is recommended as an objective tool to complement the clinical reference standard when the diagnosis is uncertain.
For cubital tunnel syndrome, the diagnostic value of MSK-DUSI showed a wide variation between the studies included in Beekman et al. [77] review. The wide range in diagnostic accuracy was likely due to a number of factors. Methodological flaws were present in most of the studies. In addition, there was no consensus on the ideal scanning procedure and no standardised cross-sectional area measurements to determine an abnormal ulnar nerve thickening at the elbow. It is likely that MSK-DUSI may be helpful in the diagnosis by demonstrating ulnar nerve thickening and by detecting underlying abnormalities. However, MSK-DUSI results should be interpreted with some caution due to its wide variation of diagnostic accuracy.
Based on the results for the elbow region it is recommended that the use of MSK-DUSI is indicated for objectively identifying lateral and medial epicondylalgia when the clinical picture is uncertain and full-thickness tears of the distal biceps tendon. It is likely that MSK-DUSI may be helpful in the diagnosis of cubital tunnel syndrome, however it is recommended to clinicians that they do not rely on negative test findings to rule it out and to use appropriate clinical judgement whether or not to follow up with electrodiagnostic studies.
Wrist/hand
The results showed ultrasound diagnosis of carpal tunnel syndrome (CTS) was the most frequently investigated condition of the wrist/hand. CTS is typically diagnosed clinically, with electrodiagnostic studies (NCS and/or EMG) used to confirm its presence [81]. However, electrodiagnostic studies have limitations; they are uncomfortable and cannot directly assess the surrounding anatomy, which is why MSK-DUSI has emerged as a possible alternative diagnostic tool [82]. The results showed a wide variation of the diagnostic accuracy of MSK-DUSI in the assessment of median nerve cross-sectional area at the wrist. This variation might be explained by different scanning protocols and reference ranges for median nerve cross-sectional area, along with differences in study design (e.g. blinding, selection of patients and controls, retrospective or prospective study design). This review did not allow for strong conclusions to be made about the diagnostic accuracy of MSK-DUSI due to the wide variation of results, however the majority of studies demonstrated moderate SnS and SpC. It is the authors’ opinion that MSK-DUSI would appear to be complementary to electrodiagnostic studies rather than an alternative.
de Quervains disease is typically an easy clinical diagnosis with pain and tenderness in the first extensor compartment of the wrist and a positive Finkelstein test. [163] However, the presence of an intracompartmental septum, an anatomical variation, has been reported to increase the risk of non-operative treatment failure and thus prognosis [89]. Therefore, studies assessing the accuracy of MSK-DUSI for detecting this septum were included. The results showed MSK-DUSI had high diagnostic value for detecting the septum and findings associated with de Quervains disease. MSK-DUSI has high diagnostic value for ganglion cysts. However, the size of the lesion can influence the SnS of MSK-DUSI for detecting ganglion cysts. The classic ultrasound diagnostic criteria for ganglion cysts has been described as an anechoic (dark/black) mass with thin, relatively sharp borders and posterior acoustic enhancement (the area behind an anechoic structure appears more echogenic (brighter) than its surroundings) [164]. Recently, researchers have reported that small ganglion cysts (≤10 mm) appear hypoechoic without posterior acoustic enhancement and thus do not fulfil the normal criteria [164]. Future studies in this area should take into account both diagnostic criteria with an aim to minimise the potential of false negative findings.
The intrinsic wrist ligaments and triangular fibrocartilage complex (TFCC) can be assessed at least in part by MSK-DUSI. The two most important intrinsic wrist ligaments are the scapholunate (SLL) and lunotriquetral (LTL), as their disruption may result in significant pain, instability and loss of function [98]. MSK-DUSI can rule in SLL and LTL injury but cannot rule it out. Imaging these structures with MSK-DUSI requires dynamic manoeuvers which are difficult to reproduce which might explain ultrasounds lack of SnS [91]. Ulnar collateral ligament (UCL) ruptures are not uncommon but are easily misdiagnosed and mistreated in the primary care setting [90]. An accurate and safe method of diagnosis is typically required. The results showed MSK-DUSI had high diagnostic value for ulnar collateral ligament (UCL) injury (displaced and non-displaced). Due to the overall paucity of the literature for intrinsic wrist ligament and TFCC injury the results should be interpreted with some caution.
Based on the results for the wrist/hand region it is recommended that MSK-DUSI be used for de Quervains, ganglion cysts and any UCL tear. It is likely that MSK-DUSI might be helpful in the diagnosis of carpal tunnel syndrome and can be used as a screening tool. However, it is recommended to clinicians that they not rely on negative test findings to rule out carpal tunnel syndrome and to use appropriate clinical judgement whether or not to follow up with electrodiagnostic studies. With the current state of the technology the use of MSK-DUSI is not indicated for SLL, LTL or TFCC injury.
Hip
The reported clinical indications for MSK-DUSI of soft tissue structures of the hip are great, varying from tendinopathy and tears to bursitis and snapping hip syndrome [3, 6]. This review found limited studies investigating the diagnostic value of MSK-DUSI for these and other soft tissue conditions of the hip. Hamstring injuries are among the most common in sports that involve sprinting and jumping, but are also common in dancing and water-skiing [165]. Both MSK-DUSI and MRI technologies have been advocated in cases of hamstring injury [166, 167], thus the author found the lack of diagnostic studies for this muscle region a notable gap in the literature. While both imaging modalities are considered useful in identifying hamstring injuries when oedema and haemorrhage are present [167], MRI is considered superior for evaluating injuries to deep portions of the muscles [168], or when a previous hamstring injury is present, as residual scarring can be misinterpreted on an ultrasound image as an acute injury [166]. Due to these factors MRI is considered to provide a more accurate diagnosis than MSK-DUSI [6].
Overall, the deep location of the target structures, complex anatomy, and extensive investigation area is challenging for the current capabilities of MSK-DUSI. Low to medium frequency transducers are required, providing increased image depth at the expense of resolution. In addition, the small field of view provided by the ultrasound exam limits the ability to exclude significant findings beyond the examined region [6]. These technical limitations of MSK-DUSI appear to favour MRI or CT for diagnostic purposes and may explain why a paucity of studies were found.
Based on the results for the hip region it is recommended that the use of MSK-DUSI is indicated for gluteal tendon tears, trochanteric bursitis and meralgia paresthetica.
Knee
The results show MSK-DUSI has a high diagnostic value for full quadriceps tendon tears, Baker’s cysts and meniscal cysts. The medial patella plica (MPP) has been reported as the most commonly injured plica due to its anatomical location [169] and mimics the presentation of other internal derangements of the knee [170]. MSK-DUSI can rule out MPP syndrome with high accuracy and can rule it in with moderate accuracy. Stubbings et al. [170] found that the MPP test (orthopaedic test) and MSK-DUSI possesses superior diagnostic accuracy compared to MRI.
Patellar tendinopathy is typically an easy diagnosis based primarily on clinical examination, where it presents as activity-related anterior knee pain associated with well-localised, palpable patella tendon tenderness [120]. The results show MSK-DUSI has a moderate to high diagnostic value for patellar tendinopathy. However, a clinical question should be asked, ‘is further imaging necessary in the light that it will not change the treatment plan?’ MSK-DUSI may potentially have a role in assessing the severity of disease, thus prognosis and/or patient education, but this is yet to be established.
Posterolateral knee structures (LCL, popliteal tendon and popliteofibular ligament) along with meniscal and other ligament injuries of the knee should be grouped together when assessing the diagnostic value of MSK-DUSI. This is because injury to one of these structures rarely occurs in isolation but rather they occur in combination and often also with osseous involvement (fracture, bone bruise) [171–175]. The results show a wide variation in the capability of MSK-DUSI to detect these structures accurately. This might be explained by a technical factor: the required increased depth of penetration is obtained at the expense of image resolution. It also seems reasonable to assume that the accuracy of MSK-DUSI may be influenced by an expanding haemarthrosis, which is commonly associated with internal knee derangement [116]. This again requires increased depth of penetration and results in decreased image resolution (i.e. ultrasound accuracy may decrease with increasing time between knee injury and the ultrasound examination). A major limitation of MSK-DUSI of the knee menisci is the inability to visualise the entire meniscus, due to the presence of artifacts and difficulty in imaging the inner margins if the meniscus [103]. The diagnostic value of MSK-DUSI for ligamentous and meniscal lesions relies on its ability to visualise all of these structures as they often occur in combination. The results highlight that the diagnostic accuracy of MSK-DUSI varies between each condition thus limiting its usefulness as a primary imaging modality for suspected internal knee derangement. However, this does not mean MSK-DUSI does not have a role to play in assessing internal knee derangement. Its potential use is as a side-line, point-of-care screening tool at sporting events rather than a definitive diagnostic tool in a primary or secondary care setting, but this is yet to be established.
The results show MSK-DUSI has high diagnostic accuracy in ruling common peroneal neuropathy out but is less sensitive in ruling it in. Electrodiagnostic studies have been reported to have a false negative rate of up to 30 % for this condition [118]. However, it is importanto emphasise that MSK-DUSI was not introduced to replace electrodiagnostic investigation of common peroneal neuropathy but to act as a complementary modality to assess nerve cross-sectional area to improve diagnostic accuracy and to assess for potential structural causes [118].
Based on the results for the knee region it is recommended that the use of MSK-DUSI is indicated for full-thickness quadriceps tendon tears, patella tendinopathy, medial patella plica syndrome, Baker’s cysts and meniscal cysts. It is likely that MSK-DUSI may be helpful in the diagnosis of common peroneal nerve neuropathy and can be used as a screening tool. However, it is recommended to clinicians that they do not rely on negative test findings to rule out common peroneal nerve neuropathy and to use appropriate clinical judgement whether or not to follow up with electrodiagnostic studies. With the current state of the technology the author recommends that the use of MSK-DUSI is not indicated as a definitive diagnostic tool for ligamentous and meniscal tears of the knee, however may have a role as a side-line, point-of-care screening tool at sporting events. MSK-DUSI is not indicated for partial-thickness ACL tears.
Ankle/foot
Ligament and syndesmotic injuries are common and some patients develop functional instability, persistent pain and swelling [124, 132]. With prompt, accurate grading of the injury the appropriate conservative or surgical management can be taken. Early, appropriate management has been shown to reduce the risk of developing chronic ankle instability symptoms by 70-90 % [176]. Of the ligamentous structures of the ankle/foot MSK-DUSI has high diagnostic value for anterior talofibular ligament, calcaneofibular ligament, deltoid ligament, posterior talofibular ligament and syndesmotic injury. The high accuracy of posterior talofibular ligament injury was based off one subject, therefore the use of MSK-DUSI for this condition is not recommended due to lack of current evidence.
The results show MSK-DUSI has high diagnostic value for plantaris tendon tears, peroneal tendon tears and posterior tibial tendinopathy. Tendinosis, tendinitis, peritendinitis, and partial or complete tendon rupture are all causes of achilles tendinopathy [137]. The value of MSK-DUSI lies within its ability to differentially diagnose these causes as shown by the results. It has been reported that the chronicity of Achilles tendon tears might impact the SnS of MSK-DUSI because fibrous scarring and granulomatous tissue can mask the defect and is therefore often overlooked [134]. Overall, the results show MSK-DUSI has moderate to high diagnostic value for differentiating Achilles tendinopathy.
The diagnosis of Morton’s neuroma is typically clear with a thorough history and physical examination. Clinical suspicion should arise if the patient gives a history of pain or tingling on the plantar aspect of the foot, made worse whilst wearing tight shoes and relieved by rest. Clinical examination may reveal tenderness on direct palpation, squeezing the metatarsals together or on stretching toes around the affected web space, a feeling of reduced sensation in between the toes of the affected area or a ‘Mulder’s Click’ [126, 148]. However, in cases of doubtful symptomatology and double lesions imaging studies may be indicated [154]. The results show MSK-DUSI has high diagnostic value for Morton’s neuroma. Anterolateral impingement syndrome can occur from a variety of causes including ankle instability, osseous and soft tissue changes [142]. Therefore, MSK-DUSI has emerged has a non-invasive tool to detect the presence of a soft tissue lesion as the cause [125]. There is conflicting evidence for the use of MSK-DUSI, therefore the results should be interpreted carefully. The difference in diagnostic accuracy is likely due to the heterogenic study population and study size. Cochet et al. [125] report on 41 subjects from the general population whereas McCarthy et al. [142] reported on 17 subjects from a population of elite athletes.
Based on the results for the ankle/foot region it is recommended that the use of MSK-DUSI is indicated for anterior talofibular ligament injury and for Morton’s neuroma when the clinical picture is uncertain. To a lesser extent MSK-DUSI can diagnose calcaneofibular and deltoid ligament injury; syndesmotic injury, plantaris tendon tears, peroneal tendon tears, posterior tibial tendinopathy, peroneal subluxation and plantar fasciitis. MSK-DUSI is recommended for differentiating causes of Achilles tendinopathy. However, a negative test may need to be followed up with MRI if the patient fits the clinical picture for a partial tear. With the current state of the technology the author recommends that the use of MSK-DUSI is not indicated for plantar plate tears, posterior talofibular ligament tears and anterolateral ankle impingement.
Comparison with existing reviews
To the authors knowledge this is the first time a review has examined the accuracy of MSK-DUSI to diagnose a full spectrum of musculoskeletal soft-tissue disorders of the upper and lower limb. Only one other study relating to the spectrum of conditions in this review was identified. The paper by Klauser et al. [3] was a combined review and Delphi consensus. Klauser et al. [3] did not report quantitative diagnostic accuracy data (SnS; SpC; LRs). A limitation of Klauser et al. [3] study. Rather, Klauser et al. [3] reported the evidence level (Level A: consistent randomised controlled clinical trial or prospective cohort study; Level B: Consistent retrospective cohort, exploratory cohort or case–control study; Level C: case series study) combined with the final Delphi consensus (grade/strength of recommendation from 0 to 3, with grade 3: ultrasound is the first choice level technique).
In this article, the review was limited to the inclusion to musculoskeletal soft tissue conditions identified by the ESMR and ACR MSK-DUSI guidelines [3, 55]. Whereas Klauser et al. [3] included all clinical indications for MSK-DUSI (i.e. soft tissue, nerve, osseous and joint pathology). A considerable strength of this article was the reported quantitative diagnostic accuracy data for each individual study and when appropriate the provided pooled data. A key comparison of this review and Klauser et al. [3] paper should be emphasised. The clinical conditions where MSK-DUSI was found to have moderate to high diagnostic accuracy in this review consistently matched Klauser et al. [3] final Delphi consensus with a grade/strength of recommendation of 2 or 3.
Strengths and weaknesses of the review
The results were based on a comprehensive and sensitive literature search strategy that aimed to identify all relevant systematic reviews of diagnostic studies, all diagnostic studies published after the date of the latest systematic reviews and relevant diagnostic studies outside the scope the systematic reviews in the National Library of Medicine’s PubMed data base (1972 to mid-2014). Wide search terms, not limited by language were used, and retrieved reference lists were manually searched for relevant primary studies to include in the review. In addition, to the authors knowledge this is the first time a review has examined the accuracy of MSK-DUSI to diagnose a full spectrum of musculoskeletal soft-tissue disorders of the upper and lower extremity. It is the authors’ opinion that the scope and breadth of the review is a strength in itself and most importantly a strength to the reader. In particular, the comprehensive range of accuracy statistics is a significant strength.
It is important to emphasise that this study is not a systematic review and is instead a narrative review. Although we used a comprehensive literature search strategy our search may not have been completely exhaustive, however if relevant studies were missed they were likely few in number and would be unlikely to impact the results with any significance. Clinical indications for which this report concludes the evidence currently shows MSK-DUSI has moderate to high diagnostic accuracy or even low diagnostic accuracy sometimes rests on a single diagnostic study. The quality of the diagnostic study also has a substantial influence on the conclusions.
Other potential weaknesses of this review include that there was only one reviewer in the selection of the studies for inclusion. When two or more independent, blinded reviewers select studies for inclusion and then independently extract data the potential for bias decreases. This review included all types of diagnostic studies, including retrospective studies. It has been shown that retrospective data is associated with an overestimation of results [177]. The reviewer did a fundamental appraisal of the methodological quality of studies, as outlined by the Users’ Guide to the Medical Literature: A Manual for Evidence-Based Clinical Practice but did not use a study quality assessment tool such as the Standards for Reporting Studies of Diagnostic Accuracy (STARD) or the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) criterion lists [178]. While critical appraisal of the included reviews and diagnostic studies would be ideal, it was beyond the scope of the present report. It was noted during this process that the strength of evidence for a large proportion of test comparisons were limited because most studies were small, heterogeneous and had design flaws, thus potentially limiting the reliability of their findings.
In about half the studies not all patients who had an ultrasound scan (index test) underwent the reference test allowing for potential verification bias to affect the results. This often occurs as the reference standard is usually invasive, expensive or both and the issue then becomes ethical in nature. The mean time from injury to ultrasound was poorly reported in about two in three studies, therefore it was not possible to compare between acute and chronic complaints. Consequently, disease progression bias might have influenced the results. However, it has been reported that these design flaws have minimal effect on estimates of diagnostic accuracy [177]. The articles assessing rotator cuff tears did not differentiate between specific structures, as such we could not evaluate each rotator cuff separately. The MSK-DUSI criteria used to consider that there was a full or partial-thickness rotator cuff tear was not reported in all studies and may have differing definitions between studies. It is well-documented that the effective use of diagnostic ultrasound is highly dependent on operator skill and training [14, 179]. Unfortunately, most studies did not state the experience level of non-radiologists. These design flaws of the original studies may have influenced the reliability of their findings.
It is important to emphasise that the vast majority of studies were conducted in a secondary care setting. In addition, about 70 % of the studies had a surgical reference standard. This implies that these studies may have included a high proportion of more severe cases and therefore, it is uncertain whether the diagnostic value of MSK-DUSI will be similar when used in primary care settings. Due to the limitations discussed, clinicians should interpret the results with some caution because of the potential for overestimation of diagnostic accuracy.
Future research
There is a lack of high quality prospective experimental studies that directly compare the accuracy of MSK-DUSI for soft-tissue pathology of the extremities to an appropriate reference standard. Consequently, future research should focus on prospective experimental studies to reduce the potential risk of spectrum and verification bias. The vast majority of studies were conducted in a secondary care setting, thus limiting the ability to generalise the results to a primary care setting. With the growth of MSK-DUSI among non-radiologists in a primary care setting [31] future studies are needed in order to evaluate the accuracy of MSK-DUSI in a primary care setting and with operators and reviewers who are not musculoskeletal radiologists.
It seems apparent that the lack of standardised values of abnormal nerve cross-sectional area impact significantly on MSK-DUSI diagnostic accuracy studies. Consequently, future research should be undertaken to standardise normal and abnormal nerve cross-sectional area values before further research is taken in investigating the diagnostic value of MSK-DUSI. Other areas of research for individual conditions were also noted. For example, MSK-DUSI has high diagnostic value for patella tendinopathy. This condition is a simple clinical diagnosis and is always treated conservatively, thus the value in imaging needs to be questioned if it does not change management. This example applies to several conditions in this review. Research in this area should focus on investigating whether MSK-DUSI can demonstrate the severity of disease, thus potentially determine prognosis and track the response to treatment. Furthermore, research in this area could involve MSK-DUSI imaging for patient education and its effect on clinical outcomes. In addition, this review found over 30 clinically indicated conditions with no diagnostic accuracy studies. Overall, there is a lack of high quality literature on the diagnostic accuracy of MSK-DUSI for a wide variety of clinically indicated conditions and future research should be considered a high priority.
Conclusion
The purpose of this article was to undertake a structured review of the literature to assess the accuracy of diagnostic ultrasound for the diagnosis of musculoskeletal soft tissue pathology of the extremities. The results of this review indicated that MSK-DUSI has good diagnostic accuracy for the detection of a wide spectrum of soft tissue conditions of the extremities. As such, MSK-DUSI is recommended as a non-invasive, relatively cheap, accurate, quick and accessible imaging modality for a variety of soft tissue conditions of the extremities. However, the current evidence base presents with some limitations. Overall, there is a lack of high quality literature on the diagnostic accuracy of MSK-DUSI for a variety of clinically indicated conditions and future research should be considered a high priority.
Abbreviations
- 2D
2-dimensional
- 3D
3-dimensional
- CT
Computed tomography
- EMG
Electromyography
- LCL
Lateral collateral ligament
- LR-
Negative likelihood ratio
- LR+
Positive likelihood ratio
- LTL
Lunotriquetral ligament
- MPP
Medial patella plica
- MRA
Magnetic Resonance Arthrography
- MRI
Magnetic Resonance Imaging
- MSK-DUSI
Musculoskeletal diagnostic ultrasound imaging
- MSK-US
Musculoskeletal ultrasound imaging
- NCS
Nerve conduction study
- PET
Positron emission tomography
- QUADAS
Quality Assessment of Diagnostic Accuracy Studies
- RUSI
Rehabilitative ultrasound imaging
- SLL
Scapholunate ligament
- SnS
Sensitivity
- SpC
Specificity
- STARD
Standards for Reporting Studies of Diagnostic Accuracy
- TFCC
Triangular fibrocartilage complex
- UCL
Ulna collateral ligament
Additional file
Search Terms - full electronic search strategy. (PDF 84 kb)
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RH conceived the study and was the main author who designed the study, performed the review and drafted the manuscript. BW and KY revised the study critically, participated in its design and helped to draft the manuscript. BW also helped perform the statistical analysis. All authors read and approved the final manuscript.
Authors’ information
This review was part of a three chapter thesis entitled Musculoskeletal Diagnostic Ultrasound Imaging and the Chiropractic Profession written by RH for the Honours degree in Science (Chiropractic) at Murdoch University. The project was supervised by BW and KY.
Contributor Information
Rogan E A Henderson, Email: rogan.henderson@yahoo.com.au.
Bruce F. Walker, Email: bruce.walker@murdoch.edu.au
Kenneth J. Young, Email: k.young@murdoch.edu.au
References
- 1.Backhaus M, Burmester G, Gerber T, Grassi W, Machold K, Swen W, et al. Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis. 2001;60(7):641–649. doi: 10.1136/ard.60.7.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacobson JA. Seminars in musculoskeletal radiology: 2005. New York: Copyright© 2005 by Thieme Medical Publishers, Inc; 2005. Musculoskeletal ultrasound and MRI: which do I choose? pp. 135–149. [DOI] [PubMed] [Google Scholar]
- 3.Klauser AS, Tagliafico A, Allen GM, Boutry N, Campbell R, Grainger A, et al. Clinical indications for musculoskeletal ultrasound: a Delphi-based consensus paper of the European Society of Musculoskeletal Radiology. Eur Radiol. 2012;22(5):1140–1148. doi: 10.1007/s00330-011-2356-3. [DOI] [PubMed] [Google Scholar]
- 4.Nazarian LN. The top 10 reasons musculoskeletal sonography is an important complementary or alternative technique to MRI. Am J Roentgenol. 2008;190(6):1621–1626. doi: 10.2214/AJR.07.3385. [DOI] [PubMed] [Google Scholar]
- 5.Kane D, Grassi W, Sturrock R, Balint P. A brief history of musculoskeletal ultrasound:‘From bats and ships to babies and hips’. Rheumatology. 2004;43(7):931–933. doi: 10.1093/rheumatology/keh004. [DOI] [PubMed] [Google Scholar]
- 6.Smith J, Finnoff JT. Diagnostic and interventional musculoskeletal ultrasound: part 2 Clinical applications. PM R. 2009;1(2):162–177. doi: 10.1016/j.pmrj.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Whittaker JL, Teyhen DS, Elliott JM, Cook K, Langevin HM, Dahl HH, et al. Rehabilitative ultrasound imaging: understanding the technology and its applications. J Orthop Sports Phys Ther. 2007;37(8):434–449. doi: 10.2519/jospt.2007.2350. [DOI] [PubMed] [Google Scholar]
- 8.Koppenhaver SL, Hebert JJ, Parent EC, Fritz JM. Rehabilitative ultrasound imaging is a valid measure of trunk muscle size and activation during most isometric sub-maximal contractions: a systematic review. Aust J Physiother. 2009;55(3):153–169. doi: 10.1016/S0004-9514(09)70076-5. [DOI] [PubMed] [Google Scholar]
- 9.Teyhen D. Rehabilitative Ultrasound Imaging Symposium, May 8–10, 2006, San Antonio, Texas. J Orthop Sports Phys Ther. 2006;36(8):A-1–A-17. doi: 10.2519/jospt.2006.0301. [DOI] [PubMed] [Google Scholar]
- 10.McDonald DG, Leopold GR. Ultrasound B-scanning in the differentiation of Baker’s cyst and thrombophlebitis. Br J Radiol. 1972;45(538):729–732. doi: 10.1259/0007-1285-45-538-729. [DOI] [PubMed] [Google Scholar]
- 11.Young A, Hughes I, Russell P, Parker M, Nichols P. Measurement of quadriceps muscle wasting by ultrasonography. Rheumatology. 1980;19(3):141–148. doi: 10.1093/rheumatology/19.3.141. [DOI] [PubMed] [Google Scholar]
- 12.Young A, Stokes M, Crowe M. Size and strength of the quadriceps muscles of old and young women*. Eur J Clin Invest. 1984;14(4):282–287. doi: 10.1111/j.1365-2362.1984.tb01182.x. [DOI] [PubMed] [Google Scholar]
- 13.Young A, Stokes M, Crowe M. The size and strength of the quadriceps muscles of old and young men. Clin Physiol. 1985;5(2):145–154. doi: 10.1111/j.1475-097X.1985.tb00590.x. [DOI] [PubMed] [Google Scholar]
- 14.Barry M, Brandt J, Christensen K. Facts and fallacies of diagnostic ultrasound of the adult spine. Dynamic Chiropractic. 1996;14(9):30. [Google Scholar]
- 15.Chovil AC, Anderson DJ, Adcock DF. Ultrasonic measurement of lumbar canal diameter: a screening tool for low back disorders? South Med J. 1989;82(8):977–980. doi: 10.1097/00007611-198908000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Futoran R. Musculoskeletal diagnostic ultrasound: Non-invasive imaging is here. J Am Chiropractic Assoc. 1995;32(9):28–32. [Google Scholar]
- 17.McCarron RF, Wimpee MW, Hudkins PG, Laros GS. The inflammatory effect of nucleus pulposus: a possible element in the pathogenesis of low-back pain. Spine. 1987;12(8):760–764. doi: 10.1097/00007632-198710000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Moore R. Blind study: comparison of the sonographic results in patients with back pain previously diagnosed by MRI, x-ray and standard orthopedic exam. Am J Clin Chiropractic. 1995;5(2):34–35. [Google Scholar]
- 19.Porter R, Bewley B. A ten-year prospective study of vertebral canal size as a predictor of back pain. Spine. 1994;19(2):173–175. doi: 10.1097/00007632-199401001-00010. [DOI] [PubMed] [Google Scholar]
- 20.Stipkovich L. Musculoskeletal ultrasonographic examination of the cervical spine and surrounding tissues including normal lymph nodes. J Chiropractic. 1994;31:33–3. [Google Scholar]
- 21.Weiss G. Spinal ultrasound: clinical correlation of spinal ultrasound and MRI. Am J Pain Manag. 1996;6:123–126. [Google Scholar]
- 22.American Chiropractic Association. Policy Statement: Diagnostic Ultrasound of the Adult Spine. Adopted by the ACA House of Delegates. 1995. [cited 2014 April]. Available from: https://www.acatoday.org/level2_cfm?T2ID=10&T1ID=10&searchQuery=diagnostic+ultrasound#27.
- 23.Battiæ MC, Hansson T, Bigos S, Zeh J, Fisher L, Spengler D. B-scan ultrasonic measurement of the lumbar spinal canal as a predictor of industrial back pain complaints and extended work loss. J Occup Environ Med. 1993;35(12):1250–1256. [PubMed] [Google Scholar]
- 24.Battiae MC, Hansson TH, Engel JM, Zeh J, Bigos SJ, Spengler DM. The reliability of measurements of the lumbar spine using ultrasound B-scan. Spine. 1986;11(2):144–148. doi: 10.1097/00007632-198603000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Drinkall J, Porter R, Hibbert C, Evans C. Value of ultrasonic measurement of spinal canal diameter in general practice. Br Med J (Clin Res Ed) 1984;288(6411):121–122. doi: 10.1136/bmj.288.6411.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Howie DW, Chatterton BE, Hone MR. Failure of ultrasound in the investigation of sciatica. J Bone Joint Surgery Br. 1983;65(2):144–147. doi: 10.1302/0301-620X.65B2.6826617. [DOI] [PubMed] [Google Scholar]
- 27.Kamei K, Hanai K, Matsui N. Ultrasonic level diagnosis of lumbar disc herniation. Spine. 1990;15(11):1170–1174. doi: 10.1097/00007632-199011010-00016. [DOI] [PubMed] [Google Scholar]
- 28.American Institute of Ultrsound in Medicine. Official Statement Nonoperative Spinal/Paraspinal Ultrasound in Adults. Approved June. 2002 [cited 2014 April]. Available from: https://www.aium.org/officialStatements/18.
- 29.Nazarian LN, Zegel HG, Gilbert KR, Edell SL, Bakst BL, Goldberg BB. Paraspinal ultrasonography: lack of accuracy in evaluating patients with cervical or lumbar back pain. J Ultrasound Med. 1998;17(2):117–122. doi: 10.7863/jum.1998.17.2.117. [DOI] [PubMed] [Google Scholar]
- 30.Raghavendra B, Epstein F. Sonography of the spine and spinal cord. Radiol Clin North Am. 1985;23(1):91–105. [PubMed] [Google Scholar]
- 31.Sharpe RE, Nazarian LN, Parker L, Rao VM, Levin DC. Dramatically increased musculoskeletal ultrasound utilization from 2000 to 2009, especially by podiatrists in private offices. J Am Coll Radiol. 2012;9(2):141–146. doi: 10.1016/j.jacr.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 32.Harvey CJ, Pilcher JM, Eckersley RJ, Blomley MJ, Cosgrove DO. Advances in ultrasound. Clin Radiol. 2002;57(3):157–177. doi: 10.1053/crad.2001.0918. [DOI] [PubMed] [Google Scholar]
- 33.Jacobson JA. Musculoskeletal ultrasound: focused impact on MRI. Am J Roentgenol. 2009;193(3):619–627. doi: 10.2214/AJR.09.2841. [DOI] [PubMed] [Google Scholar]
- 34.Lento PH, Primack S. Advances and utility of diagnostic ultrasound in musculoskeletal medicine. Curr Rev Musculoskelet Med. 2008;1(1):24–31. doi: 10.1007/s12178-007-9002-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patil P, Dasgupta B. Role of diagnostic ultrasound in the assessment of musculoskeletal diseases. Therapeutic Adv Musculoskelet Dis. 2012;4(5):341–55. doi: 10.1177/1759720X12442112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith J, Finnoff JT. Diagnostic and interventional musculoskeletal ultrasound: part 1. Fundamentals. PM R. 2009;1(1):64–75. doi: 10.1016/j.pmrj.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 37.Cho JC-S, Haun DW, Kettner NW. Sonographic evaluation of the greater occipital nerve in unilateral occipital neuralgia. J Ultrasound Med. 2012;31(1):37–42. doi: 10.7863/jum.2012.31.1.37. [DOI] [PubMed] [Google Scholar]
- 38.Cho S, Chin J, Haun DW, Kettner NW, Scali F, Clark TB. Sonography of the normal greater occipital nerve and obliquus capitis inferior muscle. J Clin Ultrasound. 2010;38(6):299–304. doi: 10.1002/jcu.20693. [DOI] [PubMed] [Google Scholar]
- 39.Haun DW, Cho J, Clark TB, Kettner NW. Normative cross-sectional area of the brachial plexus and subclavian artery using ultrasonography. J Manipulative Physiol Ther. 2009;32(7):564–570. doi: 10.1016/j.jmpt.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 40.Haun DW, Cho J, Kettner NW. Normative cross-sectional area of the C5-C8 nerve roots using ultrasonography. Ultrasound Med Biol. 2010;36(9):1422–1430. doi: 10.1016/j.ultrasmedbio.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 41.Haun DW, Cho J, Kettner NW. Symptomatic plantar fibroma with a unique sonographic appearance. J Clin Ultrasound. 2012;40(2):112–114. doi: 10.1002/jcu.20853. [DOI] [PubMed] [Google Scholar]
- 42.Nuzzo JL, Haun DW, Mayer JM. Ultrasound measurements of lumbar multifidus and abdominal muscle size in firefighters. J Back Musculoskelet Rehabil. 2014;27(4):427–33. doi: 10.3233/BMR-140463. [DOI] [PubMed] [Google Scholar]
- 43.Battaglia PJ, Kaeser MA, Kettner NW. Diagnosis and serial sonography of a proximal fifth metatarsal stress fracture. J Chiropractic Med. 2013;12(3):196–200. doi: 10.1016/j.jcm.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cook J. Correlation between musculoskeletal ultrasound, magnetic resonance imaging, arthroscopic and clinical findings in a 30-year-old male with a medial meniscus ganglion: A case report. Clin Chiropractic. 2008;2(11):83–89. [Google Scholar]
- 45.Haun DW: The Utility of Diagnostic Musculoskeletal Ultrasound in a Chiropractic Teaching Clinic. ACC-RAC Case Report 2008
- 46.Moore R: Musculoskeletal Sonography: A Case Report on the Shoulder. Dynamic Chiropractic 1997, 15(24).
- 47.Hung LY, Lucaciu OC, Soave DM. A comparative analysis of sonographic interpretation of peripheral nerves in the anterior compartment of the forearm between an experienced and novice interpreter. J Chiropractic Ed. 2012;26(1):47–50. doi: 10.7899/1042-5055-26.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gellhorn AC, Carlson MJ. Inter-rater, intra-rater, and inter-machine reliability of quantitative ultrasound measurements of the patellar tendon. Ultrasound Med Biol. 2013;39(5):791–796. doi: 10.1016/j.ultrasmedbio.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 49.Murphy RJ, Daines MT, Carr AJ, Rees JL. An independent learning method for orthopaedic surgeons performing shoulder ultrasound to identify full-thickness tears of the rotator cuff. J Bone Joint Surg. 2013;95(3):266–272. doi: 10.2106/JBJS.K.00706. [DOI] [PubMed] [Google Scholar]
- 50.Ozcakar L, Kara M, Tekin L, Karanfil Y, Esen E, Utku B, et al. Effect of supervision on ultrasonographic measurements. A blinded randomized cross-over study. Eur J Phys Rehabil Med. 2013;49(4):527–531. [PubMed] [Google Scholar]
- 51.Singhal R, Dheerendra SK, Charalambous CP, Waseem M. Teaching basic shoulder ultrasonography to orthopaedic postgraduate trainees—effectiveness of a training workshop. Med Ultrason. 2012;14:120–124. [PubMed] [Google Scholar]
- 52.O’Neill J: Musculoskeletal Ultrasound: Springer; 2008
- 53.Brown BT, Bonello R, Fernandez-Caamano R, Graham PL, Eaton S, Green H. Chiropractic in Australia: A survey of the general public. Chiropractic J Aus. 2013;43(3):85. [Google Scholar]
- 54.French SD, Charity M, Forsdike K, Gunn J, Polus B, Walker BF, et al. Chiropractic Observation and Analysis STudy (COAST): providing an understanding of current chiropractic practice. Med J Aust. 2013;10(199):687–691. doi: 10.5694/mja12.11851. [DOI] [PubMed] [Google Scholar]
- 55.American College of Radiology ACR-AIUM-SPR-SRU Practice Guidline for the Performence of the Musculoskeletal Ultrasound Examination. Resolution. 2012;27:1–12. [Google Scholar]
- 56.Straus SE, Glasziou P, Richardson WS, Haynes RB. Evidence-Based Medicine. Edinburgh: Churchill Livingston, Elsevier; 2011. [Google Scholar]
- 57.MedCalc Software: Diagnostic Test Evaluation. 2015 [cited 2014]. Available from: https://www.medcalc.org/calc/diagnostic_test.php
- 58.Florkowski CM. Sensitivity, specificity, receiver-operating characteristic (ROC) curves and likelihood ratios: communicating the performance of diagnostic tests. Clin Biochem Rev. 2008;29(Suppl 1):S83. [PMC free article] [PubMed] [Google Scholar]
- 59.Harper R. Reporting of precision of estimates for diagnostic accuracy: a review. BMJ. 1999;318(7194):1322–1323. doi: 10.1136/bmj.318.7194.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jaeschke R, Guyatt G, Sackett DL, Bass E, Brill-Edwards P, Browman G, et al. Users’ Guides to the Medical Literature: III. How to Use an Article About a Diagnostic Test A. Are the Results of the Study Valid? Jama. 1994;271(5):389–391. doi: 10.1001/jama.1994.03510290071040. [DOI] [PubMed] [Google Scholar]
- 61.Altman DG, Bland JM. Diagnostic tests. 1: Sensitivity and specificity. BMJ. 1994;308(6943):1552. doi: 10.1136/bmj.308.6943.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ. 2004;329(7458):168–169. doi: 10.1136/bmj.329.7458.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. Am J Roentgenol. 2009;192(6):1701–1707. doi: 10.2214/AJR.08.1241. [DOI] [PubMed] [Google Scholar]
- 64.Kelly AM, Fessell D. Ultrasound compared with magnetic resonance imaging for the diagnosis of rotator cuff tears: a critically appraised topic. In: Seminars in roentgenology: 2009: WB Saunders; 2009: 196–200 [DOI] [PubMed]
- 65.Lenza M, Buchbinder R, Takwoingi Y, Johnston RV, Hanchard NC, Faloppa F. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. 2013;9:CD009020. doi: 10.1002/14651858.CD009020.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Smith T, Back T, Toms A, Hing C. Diagnostic accuracy of ultrasound for rotator cuff tears in adults: a systematic review and meta-analysis. Clin Radiol. 2011;66(11):1036–1048. doi: 10.1016/j.crad.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 67.Ottenheijm RP, Jansen MJ, Staal JB, van den Bruel A, Weijers RE, de Bie RA, et al. Accuracy of diagnostic ultrasound in patients with suspected subacromial disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2010;91(10):1616–1625. doi: 10.1016/j.apmr.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 68.Alavekios DA, Dionysian E, Sodl J, Contreras R, Cho Y, Yian EH. Longitudinal analysis of effects of operator experience on accuracy for ultrasound detection of supraspinatus tears. J Shoulder Elbow Surg. 2013;22(3):375–380. doi: 10.1016/j.jse.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 69.Le Corroller T, Cohen M, Aswad R, Pauly V, Champsaur P. Sonography of the painful shoulder: role of the operator’s experience. Skeletal Radiol. 2008;37(11):979–986. doi: 10.1007/s00256-008-0539-z. [DOI] [PubMed] [Google Scholar]
- 70.Ok J-H, Kim Y-S, Kim J-M, Yoo T-W. Learning curve of office-based ultrasonography for rotator cuff tendons tears. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1593–1597. doi: 10.1007/s00167-012-2105-4. [DOI] [PubMed] [Google Scholar]
- 71.Armstrong A, Teefey SA, Wu T, Clark AM, Middleton WD, Yamaguchi K, et al. The efficacy of ultrasound in the diagnosis of long head of the biceps tendon pathology. J Shoulder Elbow Surg. 2006;15(1):7–11. doi: 10.1016/j.jse.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 72.Khoury V, Cardinal É, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. Am J Roentgenol. 2008;190(4):1105–1111. doi: 10.2214/AJR.07.2835. [DOI] [PubMed] [Google Scholar]
- 73.Read JW, Perko M. Shoulder ultrasound: diagnostic accuracy for impingement syndrome, rotator cuff tear, and biceps tendon pathology. J Shoulder Elbow Surg. 1998;7(3):264–271. doi: 10.1016/S1058-2746(98)90055-6. [DOI] [PubMed] [Google Scholar]
- 74.Skendzel JG, Jacobson JA, Carpenter JE, Miller BS. Long head of biceps brachii tendon evaluation: accuracy of preoperative ultrasound. Am J Roentgenol. 2011;197(4):942–948. doi: 10.2214/AJR.10.5012. [DOI] [PubMed] [Google Scholar]
- 75.Strobel K, Hodler J, Meyer DC, Pfirrmann CW, Pirkl C, Zanetti M. Fatty Atrophy of Supraspinatus and Infraspinatus Muscles: Accuracy of US 1. Radiology. 2005;237(2):584–589. doi: 10.1148/radiol.2372041612. [DOI] [PubMed] [Google Scholar]
- 76.Dones VC, 3rd, Grimmer K, Thoirs K, Suarez CG, Luker J. The diagnostic validity of musculoskeletal ultrasound in lateral epicondylalgia: a systematic review. BMC Med Imaging. 2014;14:10. doi: 10.1186/1471-2342-14-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Beekman R, Schoemaker M, Van Der Plas J, Van Den Berg L, Franssen H, Wokke J, et al. Diagnostic value of high-resolution sonography in ulnar neuropathy at the elbow. Neurology. 2004;62(5):767–773. doi: 10.1212/01.WNL.0000113733.62689.0D. [DOI] [PubMed] [Google Scholar]
- 78.Lobo Lda G, Fessell DP, Miller BS, Kelly A, Lee JY, Brandon C, et al. The role of sonography in differentiating full versus partial distal biceps tendon tears: correlation with surgical findings. AJR Am J Roentgenol. 2013;200(1):158–162. doi: 10.2214/AJR.11.7302. [DOI] [PubMed] [Google Scholar]
- 79.Park GY, Lee SM, Lee MY. Diagnostic value of ultrasonography for clinical medial epicondylitis. Arch Phys Med Rehabil. 2008;89(4):738–742. doi: 10.1016/j.apmr.2007.09.048. [DOI] [PubMed] [Google Scholar]
- 80.Beekman R, Visser LH. Sonography in the diagnosis of carpal tunnel syndrome: a critical review of the literature. Muscle Nerve. 2003;27(1):26–33. doi: 10.1002/mus.10227. [DOI] [PubMed] [Google Scholar]
- 81.Cartwright MS, Hobson-Webb LD, Boon AJ, Alter KE, Hunt CH, Flores VH, et al. Evidence-based guideline: neuromuscular ultrasound for the diagnosis of carpal tunnel syndrome. Muscle Nerve. 2012;46(2):287–293. doi: 10.1002/mus.23389. [DOI] [PubMed] [Google Scholar]
- 82.Descatha A, Huard L, Aubert F, Barbato B, Gorand O, Chastang JF. Meta-analysis on the performance of sonography for the diagnosis of carpal tunnel syndrome. Semin Arthritis Rheum. 2012;41(6):914–922. doi: 10.1016/j.semarthrit.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 83.Roll SC, Case-Smith J, Evans KD. Diagnostic accuracy of ultrasonography vs. electromyography in carpal tunnel syndrome: a systematic review of literature. Ultrasound Med Biol. 2011;37(10):1539–1553. doi: 10.1016/j.ultrasmedbio.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 84.Deniz FE, Oksuz E, Sarikaya B, Kurt S, Erkorkmaz U, Ulusoy H, et al. Comparison of the diagnostic utility of electromyography, ultrasonography, computed tomography, and magnetic resonance imaging in idiopathic carpal tunnel syndrome determined by clinical findings. Neurosurgery. 2012;70(3):610–616. doi: 10.1227/NEU.0b013e318233868f. [DOI] [PubMed] [Google Scholar]
- 85.Kim JY, Yoon JS, Kim SJ, Won SJ, Jeong JS. Carpal tunnel syndrome: Clinical, electrophysiological, and ultrasonographic ratio after surgery. Muscle Nerve. 2012;45(2):183–188. doi: 10.1002/mus.22264. [DOI] [PubMed] [Google Scholar]
- 86.Moghtaderi A, Sanei-Sistani S, Sadoughi N, Hamed-Azimi H. Ultrasound evaluation of patients with moderate and severe carpal tunnel syndrome. Prague Med Rep. 2012;113(1):23–32. doi: 10.14712/23362936.2015.34. [DOI] [PubMed] [Google Scholar]
- 87.Ooi CC, Wong SK, Tan AB, Chin AY, Bakar RA, Goh SY, et al. Diagnostic criteria of carpal tunnel syndrome using high-resolution ultrasonography: correlation with nerve conduction studies. Skeletal Radiol. 2014;43(10):1387–1394. doi: 10.1007/s00256-014-1929-z. [DOI] [PubMed] [Google Scholar]
- 88.Tajika T, Kobayashi T, Yamamoto A, Kaneko T, Takagishi K. Diagnostic utility of sonography and correlation between sonographic and clinical findings in patients with carpal tunnel syndrome. J Ultrasound Med. 2013;32(11):1987–1993. doi: 10.7863/ultra.32.11.1987. [DOI] [PubMed] [Google Scholar]
- 89.Choi SJ, Ahn JH, Lee YJ, Ryu DS, Lee JH, Jung SM, et al. de Quervain disease: US identification of anatomic variations in the first extensor compartment with an emphasis on subcompartmentalization. Radiology. 2011;260(2):480–486. doi: 10.1148/radiol.11102458. [DOI] [PubMed] [Google Scholar]
- 90.Chuter GS, Muwanga CL, Irwin LR. Ulnar collateral ligament injuries of the thumb: 10 years of surgical experience. Injury. 2009;40(6):652–656. doi: 10.1016/j.injury.2009.01.107. [DOI] [PubMed] [Google Scholar]
- 91.Dao KD, Solomon DJ, Shin AY, Puckett ML. The efficacy of ultrasound in the evaluation of dynamic scapholunate ligamentous instability. J Bone Joint Surg Am. 2004;86-a(7):1473–1478. doi: 10.2106/00004623-200407000-00016. [DOI] [PubMed] [Google Scholar]
- 92.Finlay K, Lee R, Friedman L. Ultrasound of intrinsic wrist ligament and triangular fibrocartilage injuries. Skeletal Radiol. 2004;33(2):85–90. doi: 10.1007/s00256-003-0698-x. [DOI] [PubMed] [Google Scholar]
- 93.Hergan K, Mittler C, Oser W. Ulnar collateral ligament: differentiation of displaced and nondisplaced tears with US and MR imaging. Radiology. 1995;194(1):65–71. doi: 10.1148/radiology.194.1.7997584. [DOI] [PubMed] [Google Scholar]
- 94.Kuwano Y, Ishizaki K, Watanabe R, Nanko H. Efficacy of diagnostic ultrasonography of lipomas, epidermal cysts, and ganglions. Arch Dermatol. 2009;145(7):761–764. doi: 10.1001/archdermatol.2009.61. [DOI] [PubMed] [Google Scholar]
- 95.Kwon BC, Choi SJ, Koh SH, Shin DJ, Baek GH. Sonographic Identification of the intracompartmental septum in de Quervain’s disease. Clin Orthop Relat Res. 2010;468(8):2129–2134. doi: 10.1007/s11999-009-1199-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Melville D, Jacobson JA, Haase S, Brandon C, Brigido MK, Fessell D. Ultrasound of displaced ulnar collateral ligament tears of the thumb: the Stener lesion revisited. Skeletal Radiol. 2013;42(5):667–673. doi: 10.1007/s00256-012-1519-x. [DOI] [PubMed] [Google Scholar]
- 97.Osterwalder JJ, Widrig R, Stober R, Gachter A. Diagnostic validity of ultrasound in patients with persistent wrist pain and suspected occult ganglion. J Hand surg. 1997;22(6):1034–1040. doi: 10.1016/S0363-5023(97)80044-5. [DOI] [PubMed] [Google Scholar]
- 98.Taljanovic MS, Sheppard JE, Jones MD, Switlick DN, Hunter TB, Rogers LF. Sonography and sonoarthrography of the scapholunate and lunotriquetral ligaments and triangular fibrocartilage disk: initial experience and correlation with arthrography and magnetic resonance arthrography. J Ultrasound Med. 2008;27(2):179–191. doi: 10.7863/jum.2008.27.2.179. [DOI] [PubMed] [Google Scholar]
- 99.Westacott DJ, Minns JI, Foguet P. The diagnostic accuracy of magnetic resonance imaging and ultrasonography in gluteal tendon tears--a systematic review. Hip Int. 2011;21(6):637–645. doi: 10.5301/HIP.2011.8759. [DOI] [PubMed] [Google Scholar]
- 100.Fearon AM, Scarvell JM, Cook JL, Smith PN. Does ultrasound correlate with surgical or histologic findings in greater trochanteric pain syndrome? A pilot study. Clin Orthop Relat Res. 2010;468(7):1838–1844. doi: 10.1007/s11999-009-1174-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Suh DH, Kim DH, Park JW, Park BK. Sonographic and electrophysiologic findings in patients with meralgia paresthetica. Clin Neurophysiol. 2013;124(7):1460–1464. doi: 10.1016/j.clinph.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 102.Alizadeh A, Babaei Jandaghi A, Keshavarz Zirak A, Karimi A, Mardani-Kivi M, Rajabzadeh A. Knee sonography as a diagnostic test for medial meniscal tears in young patients. Eur J Orthopaedic Surg Traumatol. 2013;23(8):927–931. doi: 10.1007/s00590-012-1111-z. [DOI] [PubMed] [Google Scholar]
- 103.Azzoni R, Cabitza P. Is there a role for sonography in the diagnosis of tears of the knee menisci? J Clin Ultrasound. 2002;30(8):472–476. doi: 10.1002/jcu.10106. [DOI] [PubMed] [Google Scholar]
- 104.Bianchi S, Zwass A, Abdelwahab IF, Banderali A. Diagnosis of tears of the quadriceps tendon of the knee: value of sonography. AJR Am J Roentgenol. 1994;162(5):1137–1140. doi: 10.2214/ajr.162.5.8165998. [DOI] [PubMed] [Google Scholar]
- 105.Derks WH, de Hooge P, van Linge B. Ultrasonographic detection of the patellar plica in the knee. J Clin Ultrasound. 1986;14(5):355–360. doi: 10.1002/jcu.1870140505. [DOI] [PubMed] [Google Scholar]
- 106.Fuchs S, Chylarecki C. Sonographic evaluation of ACL rupture signs compared to arthroscopic findings in acutely injured knees. Ultrasound Med Biol. 2002;28(2):149–154. doi: 10.1016/S0301-5629(01)00507-5. [DOI] [PubMed] [Google Scholar]
- 107.Garrick JG. Assessing clinically diagnosed patellar tendinopathy with magnetic resonance imaging and ultrasound. Clin J Sport Med. 2008;18(3):304–305. doi: 10.1097/01.jsm.0000248840.09003.f3. [DOI] [PubMed] [Google Scholar]
- 108.Khan Z, Faruqui Z, Ogyunbiyi O, Rosset G, Iqbal J. Ultrasound assessment of internal derangement of the knee. Acta Orthop Belg. 2006;72(1):72–76. [PubMed] [Google Scholar]
- 109.Najafi J, Bagheri S, Lahiji FA. The value of sonography with micro convex probes in diagnosing meniscal tears compared with arthroscopy. J Ultrasound Med. 2006;25(5):593–597. doi: 10.7863/jum.2006.25.5.593. [DOI] [PubMed] [Google Scholar]
- 110.Paczesny Ł, Kruczynski J. Medial Plica Syndrome of the Knee: Diagnosis with Dynamic Sonography 1. Radiology. 2009;251(2):439–446. doi: 10.1148/radiol.2512081652. [DOI] [PubMed] [Google Scholar]
- 111.Park GY, Kim JM, Lee SM, Lee MY. The value of ultrasonography in the detection of meniscal tears diagnosed by magnetic resonance imaging. Am J Physical Med Rehab. 2008;87(1):14–20. doi: 10.1097/PHM.0b013e31815e643a. [DOI] [PubMed] [Google Scholar]
- 112.Ptasznik R, Feller J, Bartlett J, Fitt G, Mitchell A, Hennessy O. The value of sonography in the diagnosis of traumatic rupture of the anterior cruciate ligament of the knee. AJR Am J Roentgenol. 1995;164(6):1461–1463. doi: 10.2214/ajr.164.6.7754893. [DOI] [PubMed] [Google Scholar]
- 113.Rutten MJ, Collins JM, van Kampen A, Jager GJ. Meniscal cysts: detection with high-resolution sonography. AJR Am J Roentgenol. 1998;171(2):491–496. doi: 10.2214/ajr.171.2.9694482. [DOI] [PubMed] [Google Scholar]
- 114.Sekiya JK, Swaringen JC, Wojtys EM, Jacobson JA. Diagnostic ultrasound evaluation of posterolateral corner knee injuries. Arthroscopy. 2010;26(4):494–499. doi: 10.1016/j.arthro.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 115.Shetty AA, Tindall AJ, James KD, Relwani J, Fernando KW. Accuracy of hand-held ultrasound scanning in detecting meniscal tears. J Bone Joint Surg. 2008;90(8):1045–1048. doi: 10.1302/0301-620X.90B8.20189. [DOI] [PubMed] [Google Scholar]
- 116.Skovgaard Larsen LP, Rasmussen OS. Diagnosis of acute rupture of the anterior cruciate ligament of the knee by sonography. Eur J Ultrasound. 2000;12(2):163–167. doi: 10.1016/S0929-8266(00)00109-9. [DOI] [PubMed] [Google Scholar]
- 117.Sorrentino F, Iovane A, Nicosia A, Vaccari A, Candela F, Cimino PG, et al. High-resolution ultrasonography (HRUS) of the meniscal cyst of the knee: our experience. Radiol Med. 2007;112(5):732–739. doi: 10.1007/s11547-007-0176-y. [DOI] [PubMed] [Google Scholar]
- 118.Visser LH, Hens V, Soethout M, De Deugd-Maria V, Pijnenburg J, Brekelmans GJ. Diagnostic value of high-resolution sonography in common fibular neuropathy at the fibular head. Muscle Nerve. 2013;48(2):171–178. doi: 10.1002/mus.23729. [DOI] [PubMed] [Google Scholar]
- 119.Ward EE, Jacobson JA, Fessell DP, Hayes CW, van Holsbeeck M. Sonographic detection of Baker’s cysts: comparison with MR imaging. AJR Am J Roentgenol. 2001;176(2):373–380. doi: 10.2214/ajr.176.2.1760373. [DOI] [PubMed] [Google Scholar]
- 120.Warden SJ, Kiss ZS, Malara FA, Ooi AB, Cook JL, Crossley KM. Comparative accuracy of magnetic resonance imaging and ultrasonography in confirming clinically diagnosed patellar tendinopathy. Am J Sports Med. 2007;35(3):427–436. doi: 10.1177/0363546506294858. [DOI] [PubMed] [Google Scholar]
- 121.Wareluk P, Szopinski KT. Value of modern sonography in the assessment of meniscal lesions. Eur J Radiol. 2012;81(9):2366–2369. doi: 10.1016/j.ejrad.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 122.Bianchi S, Sailly M, Molini L. Isolated tear of the plantaris tendon: ultrasound and MRI appearance. Skeletal Radiol. 2011;40(7):891–895. doi: 10.1007/s00256-010-1076-0. [DOI] [PubMed] [Google Scholar]
- 123.Carlson RM, Dux K, Stuck RM. Ultrasound imaging for diagnosis of plantar plate ruptures of the lesser metatarsophalangeal joints: a retrospective case series. J Foot Ankle Surg. 2013;52(6):786–788. doi: 10.1053/j.jfas.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 124.Cheng Y, Cai Y, Wang Y. Value of ultrasonography for detecting chronic injury of the lateral ligaments of the ankle joint compared with ultrasonography findings. Br J Radiol. 2014;87(1033):20130406. doi: 10.1259/bjr.20130406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Cochet H, Pele E, Amoretti N, Brunot S, Lafenetre O, Hauger O. Anterolateral ankle impingement: diagnostic performance of MDCT arthrography and sonography. AJR Am J Roentgenol. 2010;194(6):1575–1580. doi: 10.2214/AJR.09.3650. [DOI] [PubMed] [Google Scholar]
- 126.Fazal MA, Khan I, Thomas C. Ultrasonography and magnetic resonance imaging in the diagnosis of Morton’s neuroma. J Am Podiatr Med Assoc. 2012;102(3):184–186. doi: 10.7547/1020184. [DOI] [PubMed] [Google Scholar]
- 127.Grant TH, Kelikian AS, Jereb SE, McCarthy RJ. Ultrasound diagnosis of peroneal tendon tears. A surgical correlation. J Bone Joint Surg Am. 2005;87(8):1788–1794. doi: 10.2106/JBJS.D.02450. [DOI] [PubMed] [Google Scholar]
- 128.Gregg J, Silberstein M, Schneider T, Marks P. Sonographic and MRI evaluation of the plantar plate: A prospective study. Eur Radiol. 2006;16(12):2661–2669. doi: 10.1007/s00330-006-0345-8. [DOI] [PubMed] [Google Scholar]
- 129.Guillodo Y, Varache S, Saraux A. Value of ultrasonography for detecting ligament damage in athletes with chronic ankle instability compared to computed arthrotomography. Foot Ankle Spec. 2010;3(6):331–334. doi: 10.1177/1938640010378531. [DOI] [PubMed] [Google Scholar]
- 130.Gun C, Unluer EE, Vandenberk N, Karagoz A, Senturk GO, Oyar O. Bedside ultrasonography by emergency physicians for anterior talofibular ligament injury. J Emergencies Trauma Shock. 2013;6(3):195–198. doi: 10.4103/0974-2700.115340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hartgerink P, Fessell DP, Jacobson JA, van Holsbeeck MT. Full- versus partial-thickness Achilles tendon tears: sonographic accuracy and characterization in 26 cases with surgical correlation. Radiology. 2001;220(2):406–412. doi: 10.1148/radiology.220.2.r01au41406. [DOI] [PubMed] [Google Scholar]
- 132.Henari S, Banks LN, Radovanovic I, Queally J, Morris S. Ultrasonography as a diagnostic tool in assessing deltoid ligament injury in supination external rotation fractures of the ankle. Orthopedics. 2011;34(10):e639–643. doi: 10.3928/01477447-20110826-11. [DOI] [PubMed] [Google Scholar]
- 133.Hua Y, Yang Y, Chen S, Cai Y. Ultrasound examination for the diagnosis of chronic anterior talofibular ligament injury. Acta Radiol. 2012;53(10):1142–1145. doi: 10.1258/ar.2012.120171. [DOI] [PubMed] [Google Scholar]
- 134.Kainberger FM, Engel A, Barton P, Huebsch P, Neuhold A, Salomonowitz E. Injury of the Achilles tendon: diagnosis with sonography. AJR Am J Roentgenol. 1990;155(5):1031–1036. doi: 10.2214/ajr.155.5.2120931. [DOI] [PubMed] [Google Scholar]
- 135.Kalebo P, Allenmark C, Peterson L, Sward L. Diagnostic value of ultrasonography in partial ruptures of the Achilles tendon. Am J Sports Med. 1992;20(4):378–381. doi: 10.1177/036354659202000402. [DOI] [PubMed] [Google Scholar]
- 136.Kankanala G, Jain AS. The operational characteristics of ultrasonography for the diagnosis of plantar intermetatarsal neuroma. J Foot Ankle Surg. 2007;46(4):213–217. doi: 10.1053/j.jfas.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 137.Kayser R, Mahlfeld K, Heyde CE. Partial rupture of the proximal Achilles tendon: a differential diagnostic problem in ultrasound imaging. Br J Sports Med. 2005;39(11):838–842. doi: 10.1136/bjsm.2005.018416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Klein EE, Weil L, Jr, Weil LS, Sr, Knight J. Magnetic resonance imaging versus musculoskeletal ultrasound for identification and localization of plantar plate tears. Foot Ankle Spec. 2012;5(6):359–365. doi: 10.1177/1938640012463061. [DOI] [PubMed] [Google Scholar]
- 139.Klein EE, Weil L, Jr, Weil LS, Sr, Knight J. Musculoskeletal ultrasound for preoperative imaging of the plantar plate: a prospective analysis. Foot Ankle Spec. 2013;6(3):196–200. doi: 10.1177/1938640013484795. [DOI] [PubMed] [Google Scholar]
- 140.Lee M-J, Kim S, Huh Y-M, Song H-T, Lee S-A, Lee JW, et al. Morton neuroma: evaluated with ultrasonography and MR imaging. Korean J Radiol. 2007;8(2):148–155. doi: 10.3348/kjr.2007.8.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Margetic P, Pavic R. Comparative assessment of the acute ankle injury by ultrasound and magnetic resonance. Coll Antropol. 2012;36(2):605–610. [PubMed] [Google Scholar]
- 142.McCarthy C, Wilson D, Coltman T. Anterolateral ankle impingement: findings and diagnostic accuracy with ultrasound imaging. Skeletal Radiol. 2008;37(3):209–216. doi: 10.1007/s00256-007-0411-6. [DOI] [PubMed] [Google Scholar]
- 143.Mei-Dan O, Kots E, Barchilon V, Massarwe S, Nyska M, Mann G. A dynamic ultrasound examination for the diagnosis of ankle syndesmotic injury in professional athletes: a preliminary study. Am J Sports Med. 2009;37(5):1009–1016. doi: 10.1177/0363546508331202. [DOI] [PubMed] [Google Scholar]
- 144.Nallamshetty L, Nazarian LN, Schweitzer ME, Morrison WB, Parellada JA, Articolo GA, et al. Evaluation of posterior tibial pathology: comparison of sonography and MR imaging. Skeletal Radiol. 2005;34(7):375–380. doi: 10.1007/s00256-005-0903-1. [DOI] [PubMed] [Google Scholar]
- 145.Neustadter J, Raikin SM, Nazarian LN. Dynamic sonographic evaluation of peroneal tendon subluxation. AJR Am J Roentgenol. 2004;183(4):985–988. doi: 10.2214/ajr.183.4.1830985. [DOI] [PubMed] [Google Scholar]
- 146.Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol. 2010;39(1):41–47. doi: 10.1007/s00256-009-0767-x. [DOI] [PubMed] [Google Scholar]
- 147.Oliver TB, Beggs I. Ultrasound in the assessment of metatarsalgia: a surgical and histological correlation. Clin Radiol. 1998;53(4):287–289. doi: 10.1016/S0009-9260(98)80128-1. [DOI] [PubMed] [Google Scholar]
- 148.Pastides P, El-Sallakh S, Charalambides C. Morton’s neuroma: A clinical versus radiological diagnosis. Foot Ankle Surg. 2012;18(1):22–24. doi: 10.1016/j.fas.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 149.Premkumar A, Perry MB, Dwyer AJ, Gerber LH, Johnson D, Venzon D, et al. Sonography and MR imaging of posterior tibial tendinopathy. AJR Am J Roentgenol. 2002;178(1):223–232. doi: 10.2214/ajr.178.1.1780223. [DOI] [PubMed] [Google Scholar]
- 150.Rockett MS, Waitches G, Sudakoff G, Brage M. Use of ultrasonography versus magnetic resonance imaging for tendon abnormalities around the ankle. Foot Ankle Int. 1998;19(9):604–612. doi: 10.1177/107110079801900907. [DOI] [PubMed] [Google Scholar]
- 151.Sabir N, Demirlenk S, Yagci B, Karabulut N, Cubukcu S. Clinical utility of sonography in diagnosing plantar fasciitis. J Ultrasound Med. 2005;24(8):1041–1048. doi: 10.7863/jum.2005.24.8.1041. [DOI] [PubMed] [Google Scholar]
- 152.Sharp RJ, Wade CM, Hennessy MS, Saxby TS. The role of MRI and ultrasound imaging in Morton’s neuroma and the effect of size of lesion on symptoms. J Bone Joint Surg. 2003;85(7):999–1005. doi: 10.1302/0301-620X.85B7.12633. [DOI] [PubMed] [Google Scholar]
- 153.Sobiesk GA, Wertheimer SJ, Schulz R, Dalfovo M. Sonographic evaluation of interdigital neuromas. J Foot Ankle Surg. 1997;36(5):364–366. doi: 10.1016/S1067-2516(97)80038-5. [DOI] [PubMed] [Google Scholar]
- 154.Torres-Claramunt R, Gines A, Pidemunt G, Puig L, de Zabala S. MRI and ultrasonography in Morton’s neuroma: Diagnostic accuracy and correlation. Indian J Orthop. 2012;46(3):321–325. doi: 10.4103/0019-5413.96390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.van Dijk CN, Mol BW, Lim LS, Marti RK, Bossuyt PM. Diagnosis of ligament rupture of the ankle joint. Physical examination, arthrography, stress radiography and sonography compared in 160 patients after inversion trauma. Acta Orthop Scand. 1996;67(6):566–570. doi: 10.3109/17453679608997757. [DOI] [PubMed] [Google Scholar]
- 156.Waitches GM, Rockett M, Brage M, Sudakoff G. Ultrasonographic-surgical correlation of ankle tendon tears. J Ultrasound Med. 1998;17(4):249–256. doi: 10.7863/jum.1998.17.4.249. [DOI] [PubMed] [Google Scholar]
- 157.Bot S, Van der Waal J, Terwee C, Van der Windt D, Schellevis F, Bouter L, et al. Incidence and prevalence of complaints of the neck and upper extremity in general practice. Ann Rheum Dis. 2005;64(1):118–123. doi: 10.1136/ard.2003.019349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Luime J, Koes B, Hendriksen I, Burdorf A, Verhagen A, Miedema H, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33(2):73–81. doi: 10.1080/03009740310004667. [DOI] [PubMed] [Google Scholar]
- 159.Ottenheijm RP, Hesselmans NJ, Kemper A, Moser A, Bie RA, Dinant GJ, et al. GPs’ perspectives on the diagnostic work‐up in patients with shoulder pain: a qualitative study. J Eval Clin Pract. 2014;20(3):239–245. doi: 10.1111/jep.12114. [DOI] [PubMed] [Google Scholar]
- 160.Lähteenmäki HE, Hiltunen A, Virolainen P, Nelimarkka O. Repair of full-thickness rotator cuff tears is recommended regardless of tear size and age: a retrospective study of 218 patients. J Shoulder Elbow Surg. 2007;16(5):586–590. doi: 10.1016/j.jse.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 161.Millett PJ, Wilcox RB, O’Holleran JD, Warner JJ. Rehabilitation of the rotator cuff: an evaluation-based approach. J Am Acad Orthop Surg. 2006;14(11):599–609. doi: 10.5435/00124635-200610000-00002. [DOI] [PubMed] [Google Scholar]
- 162.Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy. 2009;25(1):30–39. doi: 10.1016/j.arthro.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 163.Nagaoka M, Matsuzaki H, Suzuki T. Ultrasonographic examination of de Quervain’s disease. J Orthop Science. 2000;5(2):96–99. doi: 10.1007/s007760050134. [DOI] [PubMed] [Google Scholar]
- 164.Wang G, Jacobson JA, Feng FY, Girish G, Caoili EM, Brandon C. Sonography of Wrist Ganglion Cysts Variable and Noncystic Appearances. J Ultrasound Med. 2007;26(10):1323–1328. doi: 10.7863/jum.2007.26.10.1323. [DOI] [PubMed] [Google Scholar]
- 165.Petersen J, Hölmich P. Evidence based prevention of hamstring injuries in sport. Br J Sports Med. 2005;39(6):319–323. doi: 10.1136/bjsm.2005.018549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. Am J Roentgenol. 2004;183(4):975–984. doi: 10.2214/ajr.183.4.1830975. [DOI] [PubMed] [Google Scholar]
- 167.Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. J Orthop Sports Phys Ther. 2010;40(2):67–81. doi: 10.2519/jospt.2010.3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Koulouris G, Connell D. Hamstring Muscle Complex: An Imaging Review 1. Radiographics. 2005;25(3):571–586. doi: 10.1148/rg.253045711. [DOI] [PubMed] [Google Scholar]
- 169.Nigam A, Shetty VD. The medial plica: a clinical perspective. Eur J Orthop Surg Traumatol. 2012;22(2):97–102. doi: 10.1007/s00590-011-0800-3. [DOI] [Google Scholar]
- 170.Stubbings N, Smith T. Diagnostic test accuracy of clinical and radiological assessments for medial patella plica syndrome: A systematic review and meta-analysis. Knee. 2014;21(2):486–490. doi: 10.1016/j.knee.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 171.Khoshnoodi P, Tehranzadeh AD, Dunn JM, Tehranzadeh J. Semimembranosus tendon avulsion fracture of the posteromedial tibial plateau associated with posterior cruciate ligament tear and capsular rupture. Skeletal Radiol. 2014;43(2):239–242. doi: 10.1007/s00256-013-1719-z. [DOI] [PubMed] [Google Scholar]
- 172.Manoj M, Francis J. Correlation of MRI with arthroscopy in injuries of knee joint. Kerala J Orthop. 2014;27(1):18–21. [Google Scholar]
- 173.Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports Med. 2014;44(2):281–293. doi: 10.1007/s40279-013-0116-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wharton R, Henckel J, Bhattee G, Ball S, Church S: Segond fracture in an adult is not pathognomonic for ACL injury. Knee Surgery, Sports Traumatology, Arthroscopy 2014:1–4 [DOI] [PubMed]
- 175.Wissman RD, England E, Mehta K, Nepute J, Von Fischer N, Apgar J, et al. Patellotibial contusions in anterior cruciate ligament tears. Skeletal Radiol. 2014;43(2):247–250. doi: 10.1007/s00256-013-1721-5. [DOI] [PubMed] [Google Scholar]
- 176.Lynch SA, Renström PA. Treatment of acute lateral ankle ligament rupture in the athlete. Sports Med. 1999;27(1):61–71. doi: 10.2165/00007256-199927010-00005. [DOI] [PubMed] [Google Scholar]
- 177.Rutjes AW, Reitsma JB, Di Nisio M, Smidt N, Van Rijn JC, Bossuyt PM. Evidence of bias and variation in diagnostic accuracy studies. Can Med Assoc J. 2006;174(4):469–476. doi: 10.1503/cmaj.050090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Cook C, Cleland J, Huijbregts P. Creation and critique of studies of diagnostic accuracy: use of the STARD and QUADAS methodological quality assessment tools. J Man Manip Ther. 2007;15(2):93–102. doi: 10.1179/106698107790819945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Farina R, Sparano A: Errors in Sonography. In: Errors in Radiology. edn.: Springer; 2012: 79–85.


