Abstract
Objective
The objective was to evaluate the efficacy of the Revised National Institute for Occupational Safety and Health (NIOSH) lifting equation (RNLE) to predict risk of low-back pain (LBP).
Background
In 1993, NIOSH published the RNLE as a risk assessment method for LBP associated with manual lifting. To date, there has been little research evaluating the RNLE as a predictor of the risk of LBP using a prospective design.
Methods
A total of 78 healthy industrial workers' baseline LBP risk exposures and self-reported LBP at one-year follow-up were investigated. The composite lifting index (CLI), the outcome measure of the RNLE for analyzing multiple lifting tasks, was used as the main risk predictor. The risk was estimated using the mean and maximum CLI variables at baseline and self-reported LBP during the follow-up. Odds ratios (ORs) were calculated using a logistic regression analysis adjusted for covariates that included personal factors, physical activities outside of work, job factors, and work-related psychosocial characteristics.
Results
The one-year self-reported LBP incidence was 32.1%. After controlling for history of prior LBP, supervisory support, and job strain, the categorical mean and maximum CLI above 2 had a significant relationship (OR = 5.1–6.5) with self-reported LBP, as compared with the CLI below or equal to 1. The correlation between the continuous CLI variables and LBP was unclear.
Conclusions
The CLI > 2 threshold may be useful for predicting self-reported LBP. Research with a larger sample size is needed to clarify the exposure–response relationship between the CLI and LBP.
Keywords: Revised NIOSH lifting equation, lifting index, manual lifting, low-back pain, prospective study, job strain
Introduction
Low-back pain (LBP) has been identified as a major workplace health problem in numerous studies (Bernard, 1997; da Costa & Vieira, 2010; Ferguson & Marras, 1997; Hoogendoorn, van Poppel, Bongers, Koes, & Bouter, 2000; National Research Council, 2001). The total health care expenditures incurred by individuals with LBP in the United States have reached $90.7 billion (Luo, Pietrobon, Sun, Liu, & Hey, 2003). Recent data showed that workplace overexertion injuries, primarily linked to LBP, accounted for about 24% of the total workers' compensation costs and were estimated to be $12.7 billion in 2009 (Liberty Mutual Research Institute for Safety, 2009).
The risk factors for LBP are multifactorial, involving personal, physical job factors, and workplace psychosocial characteristics (Davis & Heaney, 2000). Few studies have employed a comprehensive approach to jointly investigate the effects of these risk factors (Bigos et al., 1986; Kerr et al., 2001; Marras, Lavender, et al., 1995; Marras, Lavender, Splittstoesser, & Gang, 2010; Norman et al., 1998). Moreover, prior research has attempted to study these risk factors through the use of a questionnaire (Marras, Lavender, Ferguson, Splittstoesser, & Yang, 2010) or a single job physical exposure variable such as trunk flexion, lifting, or heavy weight (Garg et al., 2013). A recent review (da Costa & Vieira, 2010) of longitudinal studies focusing on musculoskeletal disorders including LBP from 1997 to 2008 revealed that only one longitudinal study (Hoogendoorn, Bongers, et al., 2000) used video recording and force measurements (i.e., objective quantification methods) to quantify physical risk factors. In Hoogendoorn, Bongers, et al.'s (2000) study, however, quantifications of the physical risk exposure were still limited to single posture variables, such as trunk flexion or rotation. Many unclear findings about the effects of physical risk factors on LBP may be attributable to these gross physical risk factors measured by questionnaire or single physical risk exposure variables. Epidemiologic evidence regarding an exposure–response relationship between multiple risk factors and LBP may be better determined when physical risk factors are properly quantified by biomechanical analysis (Boda, Bhoyar, & Garg, 2010; Burdorf, 1992; National Research Council, 2001; Sutherland, Albert, Wrigley, & Callaghan, 2008).
In 1993, the National Institute for Occupational Safety and Health (NIOSH) published the Revised NIOSH Lifting Equation (RNLE) for evaluating the physical demands of two-handed manual lifting tasks (Waters, Putz-Anderson, Garg, & Fine, 1993). The RNLE is a useful method for measuring the physical risk factors for LBP on the basis of research findings from bio-mechanics, psychophysics, and physiology (Waters et al., 1993). The RNLE consists of two equations, the recommended weight limit (RWL) and lifting index (LI), for evaluating a specified manual lifting task. The RWL is computed from a simple mathematical equation requiring measurement of variables that describe the task, such as hand location in relation to the body, frequency of lifting, work-rest duration pattern, and type of hand coupling (Waters et al., 1993). The LI provides an estimate of the relative physical demand for the task and is defined as the ratio of the actual weight of the load lifted divided by the RWL for the task. For multiple lifting tasks, a composite LI (CLI) is calculated using a lifting frequency-weighted method with all the tasks (Waters et al., 1993). An LI or CLI ≤ 1 is the recommended value for safe lifting without an increased risk of LBP. An LI or CLI > 1 has been shown to be associated with LBP in previous studies (Lavender, Oleske, Nicholson, Andersson, & Hahn, 1999; Wang et al., 1998; Waters et al., 1999; Waters, Lu, Piacitelli, Werren, & Deddens, 2011). These studies, however, were cross-sectional in design and thus could not demonstrate a temporal relationship between the CLI and LBP.
To demonstrate a potentially causal relationship between risk factors and work-related LBP, prospective studies are needed (National Research Council, 2001). In response to the recommendation by the National Research Council (2001), two recent prospective studies were conducted in an effort to evaluate the CLI (a quantitative physical risk measure) in association with LBP (Garg et al., 2013; Pinder, Frost, & Hill, 2011). The two studies, however, showed mixed results. A significant exposure–response relationship between the CLI and LBP was found in Garg et al.'s (2013) study, whereas no significant relationship was found in Pinder et al.'s (2011) study. To our knowledge, there is no other published prospective study investigating the relationship between RNLE and LBP.
The purpose of this current study was to add scientific evidence about the relationship between the RNLE and LBP. A prospective design was used for evaluating this relationship, while controlling for personal factors, physical activities outside of work, job factors, and work-related psychosocial characteristics. The exposure–response relationship between baseline CLI and self-reported LBP at one-year follow-up was assessed.
Method
Job Description
Manual materials handling (MMH) jobs at a large dryer manufacturing company in the Midwestern United States were evaluated for inclusion in this study. The investigators were blinded to LBP or injury rates for all jobs. The following criteria were used to select jobs: (a) jobs in which manual lifting was performed as a regular daily task activity, with at least 25 lifts per day; (b) jobs with little or no unpredictable variations in task characteristics; (c) jobs that met the requirements for the application of the RNLE; and (d) jobs that did not involve a significant exposure to whole-body vibration.
The selected jobs involved lifting a number of dryer parts (panels, motors, drums, bulkheads, cabinets, etc.) ranging from 3.2 to 10 kg each in weight. Lifting jobs were selected in build areas for manufacturing parts, transfer areas for moving unfinished parts from one operation to another, and installation areas for assembling finished parts. The jobs involved 3 to 10 rotations with a fixed rotation pattern. The job rotations varied between 15 and 30 min. Two 15-min breaks and one 30-min lunch break were provided during each shift. All the jobs were repetitive with a cycle time of 10 to 50 s. Not all work rotations were lifting tasks. Some were light-duty assembly tasks in either a standing or sitting position.
Subject Recruitment and Study Design
Workers assigned to the selected jobs were asked to participate in the study. During work time, workers were invited to a training room at the plant and were informed by a research team of potential risks and benefits before signing a consent form approved by the NIOSH Human Subjects Review Board. Participants were weighed and measured for height and filled out a self-administered standardized questionnaire (Hurrell & McLaney, 1988). The questionnaire was used for obtaining information on their personal factors, physical activities outside of work, job factors, and work-related psychosocial characteristics. Another research team was assigned to collect physical risk data for subjects' lifting tasks.
To maintain a comparison consistency with two previous studies on RNLE (Waters et al., 1999; Waters, Lu, et al., 2011) and to ensure a cohort of steady risk exposure, we used the following subject inclusion criteria in this paper: (a) full-time employees at least for one year at the time of the subject recruitment, (b) no reported LBP in the preceding year at the time of subject recruitment, (c) no job changes during the one-year follow-up period, and (d) no accidental LBP during the study period.
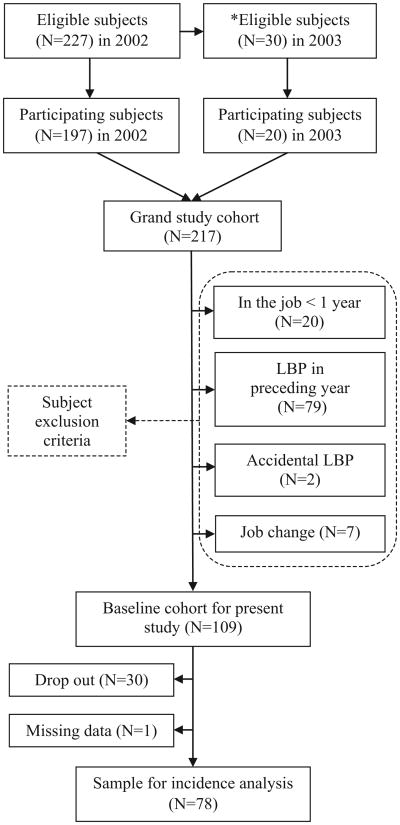
The study was designed to follow subjects for 2 years. A high subject attrition rate (57%) after 2 years of follow-up kept us from performing a meaningful statistical analysis using the second follow-up's data. The current paper focuses on the data available for a one-year follow-up. Among the eligible workers on the selected jobs, 197 and 20 participated in the study in 2002 and 2003, respectively.
Evaluation of Personal Physical Activities Outside of Work and Job Factors
Personal information collected by questionnaire included subjects' gender, education level, age, length of employment, smoking status, alcohol consumption, and self-rated health status. Physical activities outside of work were evaluated by four variables derived from two dichotomous (yes/no) questions (“Do you work at a second job for a different employer?” and “Are there sports and hobbies that you do every week?”) and two gross quantitative questions about frequency levels (<5, 5–9, 10–19, ≥20 hr/week) of manual work (“How many hours on average do you spend on activities in which you bend forward or twist your back?” and “How many hours on average do you spend on activities in which you lift, push, pull or carry moderate to heavy weights?”). Job factors in the questionnaire included job tenure, work shift, work hours per day, work days per week, overtime per week, overtime in the previous year, perceived hand and arm activity level (0–10 scale, 10 as the most rapid), and overall physical efforts (0–10, 10 as the maximal) for their work.
Characterization of Work-Related Psychosocial Factors
Work-related psychosocial factors in the questionnaire were selected primarily from the NIOSH Generic Job Stress Questionnaire (GJSQ; Hurrell & McLaney, 1988) and the Job Content Questionnaire (JCQ; Karasek et al., 1998). The scale measures used in this study included work-related psychological job demands (five items), job control or decision latitude (nine items), supervisor support (three items), and coworker support (three items). These psychosocial factors were the same as those in the GJSQ and JCQ and scored on a 4-point Likert-type scale of strongly disagree, disagree, agree, and strongly agree. Job strain, a derived variable, was evaluated using the job demands and control variables. The quotient and quadrant methods were used to determine job strain (Landsbergis, Schnall, Warren, Pickering, & Schwartz, 1994). The quotient method used the ratio of psychological demands to job control as job strain, whereas the quadrant method grouped the job strain into four exposure levels based on the high/low level of job control (decision latitude) and psychological job demands, dichotomized by their corresponding median values of the subjects' scores (Landsbergis et al., 1994). To determine the coworker social support and supervisory social support variables, the sum of the scores for three JCQ items (concern, pay attention, and helpfulness answered on the earlier-mentioned 4-point Likert-type scale) for each variable was calculated, then dichotomized by the median value of all subjects' data to form two high/low exposure groups. Finally, job security and job satisfaction were evaluated by a single item with a 4-point Likert-type scale of strongly disagree, disagree, agree, and strongly agree (Karasek et al., 1998). The response to each question was then dichotomized as high (grouping agree and strongly agree responses) or low exposure (grouping strongly disagree and disagree responses).
Evaluation of LBP
The status of LBP was evaluated by questions from the standardized Nordic Musculoskeletal Questionnaire, including a reference diagram of the low-back (Dickinson et al., 1992; Guo et al., 1995; Kuorinka et al., 1987). A dichotomous response (yes/no) to the question “In the past 12 months, have you had low-back pain every day for a week (7 days) or more?” was used as the LBP case definition in the current study. Two separate yes/no questions about history of prior self-reported LBP (every day for a week or more) and accidental LBP pain (accident or sudden injury to the back) were also evaluated in the study. These back health questions were identical to those used in the 1988 Health Interview Survey and previous NIOSH studies (Ezzati, Massey, Waksberg, Chu, & Maurer, 1992; Waters, Dick, Davis-Barkley, & Krieg, 2007; Waters, Dick, & Krieg, 2011).
Description of the Human Posture Simulation for Calculating the CLI and Lifting Variables
The physical risk factors for LBP in this study were assessed by the human posture simulation method (Lu, Waters, & Werren, 2012; Lu, Waters, Werren, & Piacitelli, 2010; Waters, Lu, Werren, & Piacitelli, 2010). The method involved measuring the weight of the load for each lifting task and a video analysis of estimating the whole-body posture for the task (Lu et al., 2010; Lu et al., 2012; Waters et al., 2010). The weight of the load for each lift was measured by the researchers using a scale or a dynamometer at the site. Video recording of work posture was collected at approximately 90° from each subject's sagittal plane to minimize posture simulation errors (Lu et al., 2010; Lu et al., 2012). Each video recording lasted for 10 to 20 min for each job rotation to ensure that at least three samples of each lifting task were recorded.
Custom computer software was developed to process simulated posture data for determining the RNLE task variables including horizontal distance, vertical travel distance, asymmetry angle at both origin and destination of the lift, and lifting frequency. Other RNLE task variables (hand coupling, significant control for each task, and work-rest pattern for the entire workday) were manually entered into the custom software program. The program subsequently used all the data to calculate the CLI. A detailed description of the CLI calculation method has been previously provided (Lu et al., 2010; Lu et al., 2012; Waters et al., 2010).
The arithmetic mean and maximum of the CLI values, lifting frequency rates, and loads across all job rotations that required manual lifting were calculated as the final physical risk exposure variables. In addition, the total lift time (sum of the periods of all the lifts) and number of lifts over the 8-hr work shift were included as additional lifting variables.
Statistical Analysis
It was not feasible to completely collect physical risk exposure data for every subject for every lifting task. For subjects with missing data, the mean of the exposure data from other subjects in the identical job were imputed. Descriptive statistics were performed for the frequency response of LBP at the one-year follow-up visit for the covariates at baseline (Table 1), as well as the mean and standard deviation of the lifting variables at baseline and their correlation with the development of LBP during the one-year follow-up period (Table 2). Since the study cohort consisted of subjects' data from two different years, the recruitment/baseline year was examined as a potential covariate. Logistic regression analysis was used to examine the association between each covariate at baseline and LBP (yes/no) at the one-year follow-up. A separate model was used for each covariate. In the logistic regression analysis, an odds ratio (OR) was calculated as the risk estimate for the categorical covariates using the lowest level of exposure as the reference, and for the categorical CLI variables (0 < CLI ≤ 1, 1 < CLI ≤ 2, 2 < CLI ≤ 3, and CLI > 3) using the recommended CLI value ≤ 1.0 as the reference (Waters et al., 1993). In addition, some continuous covariates (age, length of employment, body mass index [BMI], hands/arms activity, overall physical efforts, and job strain ratio) were used in the logistic regression analysis.
Table 1. Results of the Univariate Logistic Regression Analysis for Variables Associated With Self-Reported Low-Back Pain (LBP) at One-Year Follow-Up (N = 78).
| Variables | n | % LBP | M(SD) | OR (CI) | p Value |
|---|---|---|---|---|---|
| Personal factors | |||||
| Sex | |||||
| Male | 59 | 30.5 | — | Ref | — |
| Female | 19 | 36.8 | — | 1.3 (0.4–3.9) | .61 |
| Age (years) | 77 | 31.2 | 39.5(11.2) | 1.0 (0.95–1.04) | .8 |
| Caucasian | 77 | 31.2 | — | — | — |
| Education | |||||
| College graduate or some college | 18 | 33.3 | — | Ref | — |
| High school or some high school | 60 | 27.8 | — | 0.8(0.24–2.16) | .66 |
| Length of employment (years) | 75 | 30.7 | 5.55 (6.42) | 1.0(0.96–1.11) | .32 |
| BMI | 78 | 32.1 | 28 (6.2) | 1.0 (0.92–1.07) | .87 |
| Smoking status | .83 | ||||
| Never smoker | 25 | 36 | — | Ref | — |
| Past smoker | 28 | 32.1 | — | 0.8 (0.27–2.6) | .77 |
| Current smoker | 25 | 28 | — | 0.7 (0.21–2.3) | .55 |
| Alcohol consumption | .73 | ||||
| None | 18 | 28.8 | — | Ref | — |
| Fewer than 12 drinks in past year | 19 | 21.1 | — | 0.7(0.15–3.14) | .63 |
| Fewer than 3 drinks per week | 20 | 45 | — | 2.1 (0.55–8.25) | .28 |
| 3 or >3 drinks per week | 20 | 35 | — | 1.4 (0.35–2.57) | .63 |
| Self-rated health | .64 | ||||
| Excellent | 11 | 11.1 | — | 0.18(0.02–1.5) | .1 |
| Very good | 25 | 36 | — | 1.0 (0.36–2.84) | .98 |
| Good | 40 | 35 | — | Ref | — |
| Fair | 1 | 0 | — | Ref | — |
| Poor | 1 | 100 | — | Ref | — |
| History of prior self-reported LBP (yes) | 20 | 50 | — | 2.87 (0.99–8.2) | .051 |
| Cohort baseline year (2003 vs. 2002) | 16 | 37.5 | — | 1.35 (0.43–4.3) | .6 |
| Physical activities outside of work | |||||
| Second job (yes vs. no) | 7 | 28.5 | — | 0.84(0.15–4.6) | .84 |
| Nonwork bent/twisted back posture | .75 | ||||
| <5 hr per week | 40 | 32.5 | — | Ref | — |
| 5–9 hr per week | 19 | 36.8 | — | 1.2(0.37–3.8) | .74 |
| 10–19 hr per week | 11 | 18.2 | — | 0.48 (0.1–2.44) | .36 |
| 20 or >20 hr per week | 8 | 16.7 | — | 1.25 (0.26–6.0) | .78 |
| Nonwork MMH | .94 | ||||
| <5 hr per week | 42 | 31 | — | Ref | — |
| 5–9 hr per week | 22 | 31.8 | — | 1.0 (0.3–3.2) | .94 |
| 10–19 hr per week | 6 | 33.3 | — | 1.1 (0.18–6.9) | .91 |
| 20 or >20 hr per week | 7 | 42.9 | — | 1.7 (0.33–8.6) | .54 |
| Sports or hobbies (yes vs. no) | 34 | 32.3 | — | 1.0 (0.4–2.67) | .96 |
| Job factors | |||||
| Job tenure with company | .46 | ||||
| 1 to <3 years | 19 | 21.1 | — | Ref | — |
| 3 to <5 years | 10 | 50 | — | 3.7 (0.7–19.7) | .12 |
| 5 to <10 years | 18 | 27.8 | — | 1.4 (0.32–6.5) | .63 |
| ≥ 10 years | 30 | 33.3 | — | 1.85 (0.5–7.2) | .35 |
| Work shift | .98 | ||||
| 1st | 37 | 32.4 | — | Ref | — |
| 2nd | 26 | 30.1 | — | 0.93 (0.31–2.7) | .88 |
| 3rd | 15 | 33.3 | — | 1.04 (0.29–3.7) | .95 |
| Work time per day | |||||
| ≤8 hr | 65 | 32.3 | — | Ref | — |
| 8 hr | 9 | 22.2 | — | 0.6 (0.1–3.13) | .54 |
| Workdays per week | |||||
| ≤5 | 72 | 30.1 | — | Ref | — |
| >5 | 2 | 50 | — | 1.4 (0.32–0.57) | .57 |
| Overtime per week | |||||
| 1–4 hr | 58 | 34.5 | — | Ref | — |
| ≥5 hr | 15 | 33.3 | — | 0.95 (0.3–3.2) | .93 |
| Overtime in previous year | .33 | ||||
| 1–9 weeks | 47 | 40.4 | — | Ref | — |
| 10–19 weeks | 17 | 23.5 | — | 0.45 (0.13–1.6) | .22 |
| ≥20 weeks | 9 | 22.2 | — | 0.42 (0.1–2.25) | .32 |
| Hands and arms activity (0–10, rapidest) | 78 | 32.1 | 7.1 (1.3) | 1.2 (0.81–1.68) | .42 |
| Overall physical efforts (0–10, maximal) | 78 | 32.1 | 5.7 (1.9) | 1.1 (0.85–1.4) | .52 |
| Psychosocial characteristics | |||||
| Job strain (four quadrants) | .76 | ||||
| High DL + low PD | 18 | 33.3 | 0.66 (0.18) | Ref | — |
| Low DL + low PD | 21 | 33.3 | 0.81 (0.22) | 1.0 (0.26–3.8) | 1.0 |
| High DL + high PD | 21 | 38.1 | 0.75 (0.18) | 1.23 (0.33–4.6) | .75 |
| Low DL + high PD | 18 | 22.2 | 0.92 (0.16) | 0.57 (0.13–2.5) | .46 |
| Low supervisor social support | 49 | 36.7 | — | 1.8 (0.65–5.1) | .25 |
| Low coworker social support | 49 | 34.7 | — | 1.3 (0.48–3.65) | .58 |
| Low job security | 20 | 40 | — | 1.6 (0.56–4.63) | .38 |
| Low job satisfaction | 9 | 22.2 | — | 1.75 (0.34–9.1) | .51 |
Note. DL = decision latitude; MMH = manual materials handling related to lifting, pushing, pulling, and carrying; PD = psychological demand.
Table 2. Descriptive Statistics of Lifting Variables at Baseline and Their Correlation With Self-Reported Low-Back Pain (LBP) at One-Year Follow-Up (N = 78).
| All Subjects, M (SD) (n = 78) | Non-LBP, M (SD) (n = 53) | LBP, M (SD) (n = 25) | R (n = 78) | p Value (n = 78) | |
|---|---|---|---|---|---|
| Number of lifts per shifta | 103.6 (135.7) | 94.8 (137) | 122.4 (134.7) | .10 | .4 |
| Lift time per shift (min)a | 192.2 (248.3) | 178.8 (254.8) | 220.7 (236.5) | .08 | .5 |
| Mean lifting frequency (per min) | 7.2 (3.2) | 7.0 (3.1) | 7.8 (3.5) | .12 | .3 |
| Mean load (kg) | 6.3 (2.5) | 6.2 (2.8) | 6.3 (2.0) | .005 | .97 |
| Mean CLI | 1.5 (1.0) | 1.4 (1.1) | 1.7 (0.7) | .12 | .29 |
| Maximum lifting frequency (per min) | 8.4 (4.1) | 8.1 (4.1) | 9 (4.1) | .11 | .36 |
| Maximum load (kg) | 9.0 (6.8) | 9.2 (7.5) | 8.5 (5.0) | –.05 | .67 |
| Maximum CLI | 2.0 (1.6) | 2.0 (1.8) | 2.2 (1.0) | .08 | .5 |
Note: CLI = composite lifting index; r = biserial correlation coefficient.
Derived variable based on analyzed lifts and job rotation pattern during an 8-hr shift.
To form the final multivariable logistic regression model, we used two selection criteria for the covariates: (a) an association with LBP (p < .3) found in the univariate logistic regression analysis or (b) a greater than 10% change in the OR of the mean CLI variable calculated from the logistic regression coefficient when the covariate was added to the model (Harris-Adamson et al., 2013). Selected covariates and each CLI variable (continuous or categorical) were used in the final regression models. All the statistical work was performed with SAS (Version 9.0, SAS Institute Inc., Cary, NC).
Results
Figure 1 shows the results of the subject recruitments in two separate years and the subject exclusion criteria for an incidence analysis at one-year follow-up. In all, 30 subjects who were unavailable for participation or refused to participate in the study in 2002 were reap-proached for study participation in 2003. The overall participation rate for both years was 95.6%. Of 217 participating subjects, 109 met the subject inclusion criteria for the incidence analysis; 30 dropped out of the study, resulting in a dropout rate of 27.5%. One subject had missing job exposure data that could not be imputed. The final sample size for the incidence analysis was 78.
Figure 1.
The study sample for a self-reported low back pain (LBP) incidence analysis based on two subject recruitments in 2002 and 2003 at a large dryer manufacturing plant. *Subjects who were unavailable or refused to participate in the study in 2002.
The one-year incidence rate of self-reported LBP in the study cohort was 32.1%. Results of the univariate analysis for the potential covariates in relation to self-reported LBP are summarized in Table 1. Of the subjects, 74% were male. All were Caucasian except 1 Hispanic subject, with a mean age of 39.5 and a standard deviation of 11.2. The means of the scores for decision latitude and psychological demands were 22.95 (SD = 2.89) and 14.68 (SD = 1.65), respectively. The resulting job strain ratio was 0.75 (SD = 0.24). This continuous job strain ratio was not significantly associated with LBP (OR = 1.0, p = .9). In addition, none of the potentially confounding variables in Table 1 were significantly associated with LBP (p < .05). History of prior LBP and supervisory support were marginally associated with LBP (p = .051 and .25, respectively).
The mean and standard deviation of the number of lifts analyzed in the video recording for each subject were 33 and 24, respectively. Table 2 shows the characteristics of the lifting variables at baseline between the non-LBP and LBP groups and their correlation with LBP during the one-year follow-up period. Of the data in Table 2, 36% were imputed. The subjects in the LBP group had nonsignificantly (p > .05) larger magnitudes of exposure to the lifting variables than the non-LBP group except the maximal load variable.
In addition to history of prior LBP and supervisory support, which both met the first covariate selection criterion for the final multivariate analysis model, job strain met the second selection criterion. These covariates were selected to the final logistic regression model. Results from the logistic regression analyses for the mean and maximum CLI variables are presented in Tables 3 and 4, respectively. There was a borderline significant relationship (p = .08) between the continuous mean CLI in the multivariate model. No clear relationship was found for the continuous maximum CLI in both univariate and multivariate models. Due to the small sample sizes for the categorical mean CLI > 3 (n = 4) and 2 < maximum CLI ≤ 3 (n = 7) variables, data for these two CLI categories were pooled for OR calculations using CLI ≤ 1 as the reference. Results showed that both categorical mean and maximum CLI > 2 had a significant OR for LBP in the multivariate model (p < .05). Their OR and confidence interval (CI) were 5.1 (CI = 1.1–24.5) and 6.5 (CI = 1.4–29.7), respectively. Both categorical mean and maximum between 1 and 2 did not have a significant OR for LBP.
Table 3. Crude and Adjusted Odds Ratios of the Mean Composite Lifting Index (CLI) for Predicting Self-Reported Low-Back Pain (LBP) at One-Year Follow-Up (N = 78).
| CLI Category | n | LBP Cases | M | SD | OR | 95% CI | p | aORa | 95% CI | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Continuous CLI | 78 | 25 | 1.5 | 1.0 | 1.3 | 0.8–2.1 | .3 | 1.6 | 0.9–2.8 | .08 |
| CLI ≤ 1 | 29 | 6 | 0.7 | 0.2 | Ref | Ref | Ref | Ref | Ref | Ref |
| 1 < CLI ≤ 2 | 32 | 12 | 1.4 | 0.3 | 2.3 | 0.7–7.3 | .16 | 3.2 | 0.9–11.2 | .07 |
| 2 < CLI | 17 | 7 | 3.0 | 1.1 | 2.7 | 0.7–10 | .14 | 5.1* | 1.1–24.5 | .04 |
Adjusted for history of prior self-reported LBP, supervisory support, and job strain.
p < .05.
Table 4. Crude and Adjusted Odds Ratios of the Maximum Composite Lifting Index (CLI) for Predicting Self-Reported Low-Back Pain (LBP) at One-Year Follow-Up (N = 78).
| CLI Category | n | LBP Cases | M | SD | OR | 95% CI | p | aORa | 95% CI | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Continuous CLI | 78 | 25 | 2.0 | 1.6 | 1.1 | 0.8–1.4 | .5 | 1.3 | 0.9–1.8 | .13 |
| CLI ≤ 1 | 24 | 5 | 0.8 | 0.2 | Ref | Ref | Ref | Ref | Ref | Ref |
| 1 < CLI ≤ 2 | 28 | 8 | 1.4 | 0.3 | 1.5 | 0.4–5.5 | .52 | 2.3 | 0.6–9.7 | .25 |
| 2 < CLI | 26 | 12 | 3.7 | 1.8 | 3.3 | 0.9–11.4 | .06 | 6.5* | 1.4–29.7 | .02 |
Adjusted for history of prior self-reported LBP, supervisory support, and job strain.
p < .05.
Discussion
The present study is one of the first studies using a prospective design to show a temporal relationship between the CLI and self-reported LBP. Although findings from this study did not provide clear evidence that the continuous CLI variables had a statistically significant exposure–response relationship with LBP across all exposure categories, the trend in this relationship was positive. The CLI > 2 category was significantly associated with LBP in the current study, which agreed with the two previous cross-sectional studies (Waters et al., 1999; Waters, Lu, et al., 2011). It should be noted that the present study did not have a nonexposure group (i.e., no exposure to manual lifting, which was the reference group for the previous studies). If a nonexposure group had been used as the reference group in the present study, the risk estimates likely would have been greater.
It is worth mentioning that the maximum CLI > 2 category seemed to be a stronger predictor than the mean CLI > 2 category in the present study (Tables 3 and 4). This finding agrees with the suggestion in Garg et al.'s (2013) prospective RNLE study that the peak job physical demands are better predictors of LBP than average job demands. An exposure–response relationship between the maximum CLI and self-reported LBP was found in Garg et al.'s study, whereas this relationship was unclear in the present study. The small sample size (N = 78) for the present study is probably the main factor for this unclear relationship. However, different results in Garg et al.'s and the present studies are also likely to be attributable to the different methodologies. In Garg et al.'s study, the LBP case was defined as any self-reported LBP intensity lasting 1 day or longer, whereas the LBP case in the present study was determined by self-reported LBP lasting 1 week or longer. In addition, the subject inclusion criterion (at least 3 months free of LBP vs. at least 1 year free of LBP at baseline) and the risk modeling methods (hazard ratio vs. OR) were different between the studies. Despite the different research methodologies, both studies suggest that the RNLE may be a useful tool for assessing the risk of LBP (Garg et al., 2013).
The one-year LBP incidence (32.1%) found in this study is similar to the one-year prevalence (32%) reported in our previous cross-sectional study (Waters, Lu, et al., 2011), but higher than 26.1% reported for manufacturing jobs in a previous study (Xiao, Dempsey, Lei, Ma, & Liang, 2004) and the 17.6% reported in the 1988 Health Interview Survey (Behrens, Seligman, Cameron, Mathias, & Fine, 1994) using the same survey question asking for LBP lasting a week or more in the preceding year (Guo et al., 1995). The LBP incidence rate found in the present study is also comparable to the rates (33%–34%) for operator/laborer jobs during the Quality of Life Survey from the General Social Survey, a nationally representative survey conducted in 2002 and 2006 in the United States (Waters, Dick, et al., 2011; Waters et al., 2007).
The low correlations of the individual lifting variables with LBP (Table 2) suggest that the risk of developing LBP may be best estimated by the synergetic effects of many lifting variables, rather than one singular lifting factor (Singh & Kumar, 2012; Xiao et al., 2004). The findings agree with the results from a prospective study investigating 40 individual lifting variables in relation to impaired back function at 6-month follow-up (Ferguson, Allread, Deborah, Heaney, & Marras, 2012). Only 3 of the 40 lifting variables in Ferguson et al.'s (2012) study showed a significant relationship with impaired back function. Some of our significant findings concerning the CLI in relation to LBP seem to agree with the suggestion that biomechanical variables (e.g., moment, compressive, and shear forces on the spine), estimated with multiple lifting posture angles and load factors, are important measures for assessing the risk of LBP (Marras, Lavender, et al., 1995; Marras, Lavender, Ferguson, et al., 2010; Marras, Parnianpour, et al., 1995).
Although used in our final regression analysis model, job strain and other psychosocial variables were not significantly associated with LBP in the univariate regression analysis. The findings are in agreement with those in a review paper (Hartvigsen, Lings, Leboeuf-Yde, & Bakketeig, 2004). There is some evidence from both cross-sectional and longitudinal studies to support the link between low job satisfaction and LBP (Bigos et al., 1986; da Costa & Vieira, 2010; Marras et al., 1993; van Poppel, Koes, Deville, Smid, & Bouter, 1998; Waters et al., 1999; Waters, Lu, et al., 2011). In the present study, no significant relationship between low job satisfaction and LBP was found. The relationship may have been affected by a large percentage (88%) of the subjects that reported high to very high job satisfaction.
The adjusted ORs for the categorical CLI variables were affected by the addition of covariates in the regression model, whereas the ORs for the continuous CLI variables were not substantially affected (Tables 3 and 4). The larger changes seen in the models using exposure categories are probably due to the small sample sizes in the higher exposure categories. The CIs are wide. In Table 3, removal of the job strain variable from the final model reduced the adjusted OR from 5.1 to 3.3 in the CLI > 2 category. In Table 4, removal of the supervisory support variable from the final model reduced the adjusted OR from 6.5 to 4.6 in the CLI > 2 category. In Table 4, removal of the job strain variable from the final model reduced the adjusted OR from 6.5 to 4.4 in the CLI > 2 category. Removal of history of prior LBP variable from the final model did not substantially affect the ORs in either table. These additional post hoc analyses suggest that the two psychosocial variables may act as effect modifiers of the CLI.
Several limitations of the study are acknowledged as follows:
Data for ethnicity (99% Caucasian), self-related health status (∼98% for good–excellent), job satisfaction (88% for high to very high), and job security (80% for high to very high) were distributed toward the extreme scale. A lack of data variance across the response levels limits the interpretation of the study findings for these underpowered factors.
Given the large mean (∼7 lifts per minute) of the lifting frequency rates found in this study, the lifting tasks were likely to be dynamic. Dynamic lifting has been shown to increase the spinal loading (i.e., risk of LBP) attributed to co-contractions of back muscles during lifting (Marras, Davis, Kirking, & Granata, 1999). Absence of evaluation criteria for lifting velocity and acceleration in the RNLE presents a limitation of using the CLI for predicting LBP for highly dynamic lifting tasks (Lavender et al., 1999).
Misclassifications of the physical risk exposure data attributable to 36% of the imputed job exposure data may exist. The percentages of the imputed mean CLI data across the CLI categories were comparable (52%, 41%, and 59% for the 0 < CLI ≤ 1, 1 < CLI ≤ 2, and CLI > 2 categories, respectively). In addition, the percentages of the imputed data between the non-LBP (45%) and LBP groups (56%) were not largely different. There was no significant difference (p < .05) in the imputed physical risk exposure data between the different groups for the two comparison analyses. The findings indicate that the imputation may not be statistically problematic due to a possible random distribution of the missing data.
Self-reported LBP in one year is subject to recall errors. Inclusion of other health outcomes (medical records, OSHA 300 logs, sickness absence, and worker health compensation data) for evaluating LBP may reduce the recall errors.
The large subject dropout rate (27.5%), the small sample size (N = 78), one study site, and the short one-year observation period limit the generalizability of the study results.
The finding that the cumulative lift time and number of lifts over a work shift were not related to LBP may have resulted from not adjusting for the effects of recovery time attributable to job rotation. Job rotation is a common work practice in industry, but the effect of job rotation on LBP is unclear and difficult to evaluate (Davis & Jorgensen, 2005).
Conclusions
After controlling for history of prior LBP, supervisory support, and job strain, workers with the mean CLI and maximum CLI greater than 2 were significantly more likely to report LBP after one year compared to workers with the CLIs less than or equal to 1. Although findings from this study did not provide clear evidence that the CLI had a statistically significant exposure–response relationship with LBP across all exposure categories, the trend in this relationship was positive. The predictability of the CLI for LBP needs more research.
Key Points.
The categorical mean and maximum CLI above 2 had a significant effect on self-reported LBP at the one-year follow-up, as compared with the CLI below or equal to 1.
Although findings from this study did not provide clear evidence that the CLI had a statistically significant exposure–response relationship with LBP across all exposure categories, the trend in this relationship was positive.
More research with a larger sample size and a longer follow-up period is needed to explore the temporal relationship between different ranges of the CLI and LBP.
Acknowledgments
The authors would like to thank Laurie Piacitelli, Dale Woods, John Peacock, Lian Luo, Brian Lowe, Yong-Ku Kong, Marisol Barrero, Diane Papes, Ken Crombie, Caitlin Zivkovich, Dennis Roberts, Belinda Johnson, Anne Marie White, Eric McKibben, Jessica Burkhardt, Jessica Streit, Amy Feng, and Tarah Cole for their valuable assistance in collecting and analyzing data. The authors are grateful to Arun Garg, William S. Marras, and Patrick Dempsey for their technical review and suggestions. The findings and conclusions of this study are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
Biographies
Ming-Lun Lu is a certified professional ergonomist and a senior research fellow at the National Institute for Occupational Safety and Health (NIOSH). He holds a PhD in Industrial Hygiene with a concentration on ergonomics from the University of Cincinnati. His primary research interests include occupational biomechanics and ergonomic risk assessments for prevention of work-related musculoskeletal disorders.
Thomas R. Waters, now retired, was a senior research safety engineer at NIOSH at the time this article was developed. He holds a PhD in biomechanics and a master's of science in engineering science from the University of Cincinnati. Dr. Waters has published more than 50 papers and book chapters on manual materials handling and prevention of low-back disorders.
Edward Krieg is a statistician in the Division of Applied Research and Technology at NIOSH in Cincinnati, Ohio. He received a PhD in psychology from Tulane University. He designs and analyzes data from the division's laboratory and field studies.
Dwight Werren received a bachelor's degree in zoology from Miami University and has two years of undergraduate training in computer science from the University of Cincinnati. He works as an IT specialist for NIOSH. He writes software applications for ergonomic and laboratory research. Current software development allows interfacing digital video and lifting task variables with human motion capture data to provide analyses using the Revised NIOSH Lifting Equation and the University of Michigan's 3D Static Strength Prediction Program.
Footnotes
Author(s) Note: The author(s) of this article are U.S. government employees and created the article within the scope of their employment. As a work of the U.S. federal government, the content of the article is in the public domain.
References
- Behrens V, Seligman P, Cameron L, Mathias CG, Fine L. The prevalence of back pain, hand discomfort, and dermatitis in the US working population. American Journal of Public Health. 1994;84:1780–1785. doi: 10.2105/ajph.84.11.1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard B. A critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. Washington, DC: U.S. Department of Health and Human Services, Center for Disease Control and Prevention, National Institute for Occupational Safety and Health; 1997. [Google Scholar]
- Bigos SJ, Spengler DM, Martin NA, Zeh J, Fisher L, Nachemson A, Wang MH. Back injuries in industry: A retrospective study. II. Injury factors. Spine. 1986;11:246–251. doi: 10.1097/00007632-198604000-00011. [DOI] [PubMed] [Google Scholar]
- Boda S, Bhoyar P, Garg A. Validation of revised NIOSH Lifting Equation and 3D SSP model to predict risk of work-related low back pain. Paper presented at the 54th Human Factors and Ergonomics Society annual meeting; San Francisco, CA. 2010. Sep, [Google Scholar]
- Burdorf A. Exposure assessment of risk factors for disorders of the back in occupational epidemiology. Scandinavian Journal of Work, Environment & Health. 1992;18:1–9. doi: 10.5271/sjweh.1615. [DOI] [PubMed] [Google Scholar]
- da Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. American Journal of Industrial Medicine. 2010;53:285–323. doi: 10.1002/ajim.20750. [DOI] [PubMed] [Google Scholar]
- Davis KG, Heaney CA. The relationship between psychosocial work characteristics and low back pain: Underlying methodological issues. Clinical Biomechanics. 2000;15:389–406. doi: 10.1016/s0268-0033(99)00101-1. [DOI] [PubMed] [Google Scholar]
- Davis K, Jorgensen M. Ergonomics. Pros and cons of job rotation as a means of reducing injury costs. Journal of Occupational Environmental Hygiene. 2005;2:D1–D3. doi: 10.1080/15459620590894760. [DOI] [PubMed] [Google Scholar]
- Dickinson CE, Campion K, Foster AF, Newman SJ, O'Rourke AMT, Thomas PG. Questionnaire development: An examination of the Nordic Musculoskeletal Questionnaire. Applied Ergonomics. 1992;23:197–201. doi: 10.1016/0003-6870(92)90225-k. [DOI] [PubMed] [Google Scholar]
- Ezzati TM, Massey JT, Waksberg J, Chu A, Maurer KR. Sample design: Third National Health and Nutrition Examination Survey. Vital and Health Statistics Series 2. 1992;113:1–35. [PubMed] [Google Scholar]
- Ferguson SA, Allread WG, Deborah B, Heaney C, Marras WS. Biomechanical, psychosocial and individual risk factors predicting low back function impairment among furniture distribution employees. Clinical Biomechanics. 2012;27:117–123. doi: 10.1016/j.clinbiomech.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson SA, Marras WS. A literature review of low back disorder surveillance measures and risk factors. Clinical Biomechanics. 1997;12:211–226. doi: 10.1016/s0268-0033(96)00073-3. [DOI] [PubMed] [Google Scholar]
- Garg A, Boda S, Moore JS, Kapellusch JM, Bhoyar P, Thiese M, Merryweather A, Deckow-Schaefer G, Bloswick D, Malloy E. The NIOSH lifting equation and low back pain, part 1: Association with low back pain in the BackWorks prospective cohort study. Human Factors. 2013 doi: 10.1177/0018720813486669. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Guo HR, Tanaka S, Cameron LL, Seligman PJ, Behrens VJ, Ger J, Wild DK, Putz-Anderson V. Back pain among workers in the United States: National estimates and workers at high risk. American Journal of Industrial Medicine. 1995;28:591–602. doi: 10.1002/ajim.4700280504. [DOI] [PubMed] [Google Scholar]
- Harris-Adamson C, Eisen EA, Dale AM, Evanoff B, Hegman KT, Thiese MS, Kapellusch JM, Burt S, Bao S, Silverstein B, Geer F, Merlino L, Rempel D. Personal and workplace psychosocial risk factors for carpel tunnel syndrome: A pooled study cohort. Occupational and Environmental Medicine. 2013 doi: 10.1136/oemed-2013-101365. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartvigsen J, Lings S, Leboeuf-Yde C, Bakketeig L. Psychosocial factors at work in relation to low back pain and consequences of low back pain: A systematic, critical review of prospective cohort studies. Occupational and Environmental Medicine. 2004;61:1–10. [PMC free article] [PubMed] [Google Scholar]
- Hoogendoorn WE, Bongers PM, de Vet HC, Douwes M, Koes BW, Miedema MC, Ariens GA, Bouter LM. Flexion and rotation of the trunk and lifting at work are risk factors for low back pain: Results of a prospective cohort study. Spine. 2000;25:3087–3092. doi: 10.1097/00007632-200012010-00018. [DOI] [PubMed] [Google Scholar]
- Hoogendoorn WE, van Poppel MN, Bongers PM, Koes BW, Bouter LM. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine. 2000;25:2114–2125. doi: 10.1097/00007632-200008150-00017. [DOI] [PubMed] [Google Scholar]
- Hurrell JJ, McLaney MA. Exposure to job stress: A new psychometric instrument. Scandinavian Journal of Work, Environment & Health. 1988;14(Suppl. 1):27–28. [PubMed] [Google Scholar]
- Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. Journal of Occupational Health Psychology. 1998;3:322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- Kerr MS, Frank JW, Shannon HS, Norman RW, Wells RP, Neumann WP, Bombardier C. Biomechanical and psychosocial risk factors for low back pain at work. American Journal of Public Health. 2001;91:1069–1075. doi: 10.2105/ajph.91.7.1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G, Jørgensen K. Standardized Nordic questionnaires for the analysis of musculoskeletal symptoms. Applied Ergonomics. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- Landsbergis PA, Schnall PL, Warren K, Pickering TG, Schwartz JE. Association between ambulatory blood pressure and alternative formulations of job strain. Scandinavian Journal of Work, Environment & Health. 1994;20:349–363. doi: 10.5271/sjweh.1386. [DOI] [PubMed] [Google Scholar]
- Lavender SA, Oleske DM, Nicholson L, Andersson GB, Hahn J. Comparison of five methods used to determine low back disorder risk in a manufacturing environment. Spine. 1999;24:1441–1448. doi: 10.1097/00007632-199907150-00009. [DOI] [PubMed] [Google Scholar]
- Liberty Mutual Research Institute for Safety. Liberty Mutual workplace safety index. Hopkinton, MA: Author; 2009. [Google Scholar]
- Lu M, Waters TR, Werren D. Development of human posture simulation method for assessing posture angles and spinal loads. Human Factors and Ergonomics in Manufacturing & Service Industries. 2012 doi: 10.1002/hfm.20534. Advance online publication. doi:10.1002.hfm.20534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu M, Waters T, Werren D, Piacitelli L. Human posture simulation to assess cumulative spinal load due to manual lifting: Part II—Accuracy and precision. Theoretical Issues in Ergonomics Science. 2010;12:1–15. [Google Scholar]
- Luo X, Pietrobon RX, Sun S, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine. 2003;29:79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- Marras WS, Davis KG, Kirking BC, Granata KP. Spine loading and trunk kinematics during team lifting. Ergonomics. 1999;42:1258–1273. doi: 10.1080/001401399184938. [DOI] [PubMed] [Google Scholar]
- Marras WS, Lavender SA, Ferguson SA, Splittstoesser RE, Yang G. Quantitative biomechanical workplace exposure measures: Distribution centers. Journal of Electromyography and Kinesiology. 2010;20:813–822. doi: 10.1016/j.jelekin.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Marras WS, Lavender SA, Leurgans SE, Fathallah FA, Ferguson SA, Allread WG, Rajulu SL. Bio-mechanical risk factors for occupationally related low back disorders. Ergonomics. 1995;38:377–410. doi: 10.1080/00140139508925111. [DOI] [PubMed] [Google Scholar]
- Marras WS, Lavender SA, Leurgans SE, Rajulu SL, All-read WG, Fathallah FA, Ferguson SA. The role of dynamic three-dimensional trunk motion in occupationally-related low back disorders. The effects of workplace factors, trunk position, and trunk motion characteristics on risk of injury. Spine. 1993;18:617–628. doi: 10.1097/00007632-199304000-00015. [DOI] [PubMed] [Google Scholar]
- Marras WS, Lavender SA, Splittstoesser RE, Gang Y. Quantitative dynamic measures of physical exposure predict low back functional impairment. Spine. 2010;35:914–923. doi: 10.1097/BRS.0b013e3181ce1201. [DOI] [PubMed] [Google Scholar]
- Marras WS, Parnianpour M, Ferguson SA, Kim JY, Crowell RR, Bose S, Simon SR. The classification of anatomic- and symptom-based low back disorders using motion measure models. Spine. 1995;20:2531–2546. doi: 10.1097/00007632-199512000-00013. [DOI] [PubMed] [Google Scholar]
- National Research Council. Musculoskeletal disorders and the workplace. Washington, DC: National Research Council and Institute of Medicine; 2001. [Google Scholar]
- Norman R, Wells R, Neumann P, Frank J, Shannon H, Kerr M. A comparison of peak vs cumulative physical work exposure risk factors for the reporting of low back pain in the automotive industry. Clinical Biomechanics. 1998;13:561–573. doi: 10.1016/s0268-0033(98)00020-5. [DOI] [PubMed] [Google Scholar]
- Pinder ADJ, Frost GA, Hill H. Prospective evaluation of the 1991 NIOSH lifting equation. London, UK: Health and Safety Executive; 2011. RR901 Research Report. [Google Scholar]
- Singh S, Kumar S. Factorial analysis of lifting task to determine the effect of different parameters and interactions. Journal of Manufacturing Technology Management. 2012;23:947–953. [Google Scholar]
- Sutherland CA, Albert WJ, Wrigley AT, Callaghan JP. A validation of a posture matching approach for the determination of 3D cumulative back loads. Applied Ergonomics. 2008;39:199–208. doi: 10.1016/j.apergo.2007.05.004. [DOI] [PubMed] [Google Scholar]
- van Poppel MN, Koes BW, Deville W, Smid T, Bouter LM. Risk factors for back pain incidence in industry: A prospective study. Pain. 1998;77:81–86. doi: 10.1016/S0304-3959(98)00085-2. [DOI] [PubMed] [Google Scholar]
- Wang MJ, Garg A, Chang YC, Shih YC, Yeh WY, Lee CL. The relationship between low back discomfort ratings and the NIOSH lifting index. Human Factors. 1998;40:509–515. doi: 10.1518/001872098779591377. [DOI] [PubMed] [Google Scholar]
- Waters TR, Baron SL, Piacitelli LA, Anderson VP, Skov T, Haring-Sweeney M, Wall DK, Fine LJ. Evaluation of the revised NIOSH lifting equation. A cross-sectional epidemiologic study. Spine. 1999;24:386–394. doi: 10.1097/00007632-199902150-00019. [DOI] [PubMed] [Google Scholar]
- Waters TR, Dick RB, Davis-Barkley J, Krieg EF. A cross-sectional study of risk factors for musculoskeletal symptoms in the workplace using data from the General Social Survey (GSS) Journal of Occupational and Environmental Medicine. 2007;49:172–184. doi: 10.1097/JOM.0b013e3180322559. [DOI] [PubMed] [Google Scholar]
- Waters TR, Dick RB, Krieg EF. Trends in work-related musculoskeletal disorders: A comparison of risk factors for symptoms using quality of work life data from the 2002 and 2006 General Social Survey. Journal of Occupational and Environmental Medicine. 2011;53:1013–1024. doi: 10.1097/JOM.0b013e3181fc8493. [DOI] [PubMed] [Google Scholar]
- Waters TR, Lu M, Piacitelli LA, Werren D, Deddens JA. Efficacy of the revised NIOSH lifting equation to predict risk of low back pain due to manual lifting: Expanded cross-sectional analysis. Journal of Occupational and Environmental Medicine. 2011;53:1061–1067. doi: 10.1097/JOM.0b013e31822cfe5e. [DOI] [PubMed] [Google Scholar]
- Waters TR, Lu M, Werren D, Piacitelli L. Human posture simulation to assess cumulative spinal load due to manual lifting. Part I: Methods. Theoretical Issues in Ergonomics Science. 2010;12:176–188. [Google Scholar]
- Waters TR, Putz-Anderson V, Garg A, Fine LJ. Revised NIOSH equation for the design and evaluation of manual lifting tasks. Ergonomics. 1993;36:749–776. doi: 10.1080/00140139308967940. [DOI] [PubMed] [Google Scholar]
- Xiao GB, Dempsey PG, Lei L, Ma ZH, Liang YX. Study on musculoskeletal disorders in a machinery manufacturing plant. Journal of Occupational and Environmental Medicine. 2004;46:341–346. doi: 10.1097/01.jom.0000121153.55726.95. [DOI] [PubMed] [Google Scholar]