Abstract
Background
Changes in criteria and differences in populations studied and methodology have produced a wide range of prevalence estimates for mild cognitive impairment (MCI).
Methods
Uniform criteria were applied to harmonized data from 11 studies from USA, Europe, Asia and Australia, and MCI prevalence estimates determined using three separate definitions of cognitive impairment.
Results
The published range of MCI prevalence estimates was 5.0%–36.7%. This was reduced with all cognitive impairment definitions: performance in the bottom 6.681% (3.2%–10.8%); Clinical Dementia Rating of 0.5 (1.8%–14.9%); Mini-Mental State Examination score of 24–27 (2.1%–20.7%). Prevalences using the first definition were 5.9% overall, and increased with age (P < .001) but were unaffected by sex or the main races/ethnicities investigated (Whites and Chinese). Not completing high school increased the likelihood of MCI (P ≤ .01).
Conclusion
Applying uniform criteria to harmonized data greatly reduced the variation in MCI prevalence internationally.
Introduction
Mild cognitive impairment (MCI) refers to cognitive decline from a previous level of functioning, both subjectively and by objective evidence. The condition was first conceptualized in the 1980s, at which time it focused on memory impairment and was thought to be a transitional stage between normal cognitive ageing and Alzheimer’s disease (AD) [1], and assigned to corresponding stages on both the Clinical Dementia Rating (CDR; rating of 0.5) [2] and Global Deterioration Scale (stages 2 and 3) [3]. While individuals with MCI due to AD may go on to develop dementia due to AD, others with MCI may develop different subtypes of dementia [4–7]. It has also become apparent that MCI is not necessarily a pre-dementia syndrome, as many individuals with MCI do not show progression of their cognitive deficits, and may in some cases revert to normal cognition [6, 8, 9]. Accordingly, the concept of MCI has evolved to accommodate heterogeneity in outcomes and aetiologies, in part through the development of MCI subtypes with greater potential clinical and prognostic value [1, 10]. The major MCI subtypes are amnestic (aMCI), involving episodic memory impairment (with or without impairment in other cognitive domains), and non-amnestic (naMCI), involving impairment in cognitive domains other than memory. Of these subtypes, aMCI is considered more likely to progress to AD, and naMCI more likely to progress to other types of dementia [10].
The level of cognitive decline associated with MCI is greater than expected for age, but not as severe as that associated with dementia. Another point of difference is retention of independence in activities of daily living (ADLs) with MCI [11, 12]. This can be difficult to establish however, as people with MCI can show impairments in high level or complex functional tasks [11, 13]. A decrease in the ability to perform such tasks can predict a decline from MCI to dementia [8].
Since MCI imposes a health burden of its own and increases the risk of dementia, it is important to reliably estimate the prevalence of MCI around the globe. However, a recent review found that the reported prevalence of MCI varies widely across international studies, from around 3% to 42% [14]. This high level of variability in reported MCI prevalence poses problems for public health policy and planning. Some of the variation may be associated with regional and/or ethnic differences. For example, the prevalence of aMCI in India is reportedly more than five times higher than in China, despite standardization for age, sex and education [15]. Another study found a higher prevalence of naMCI in Blacks than in Whites from a similar geographical location, even when sex and education were controlled [16]. That study also found the prevalence of aMCI to increase with age among men and blacks. Others have found that the prevalence of MCI increased with age [17, 18], or that men had a higher prevalence of either MCI [18] or aMCI [19]. Education also appears to influence the prevalence of MCI [17]. While findings like these suggest that differences in location and demographic make-up may contribute to the wide variation in reported prevalence of MCI, a significant proportion can be attributed to differences in definition and methodology [14]. For example, studies have not been consistent in how they have defined objective cognitive impairment. Small changes to elements of this criterion, such as the threshold for impairment and the number of sub-threshold cognitive test results required, can greatly affect the prevalence of MCI found [20]. A further issue is the use of only global scales by many studies, with limited forms of neuropsychological testing less likely than comprehensive test batteries to reliably identify MCI [21].
We have recently developed an international consortium—Cohort Studies of Memory in an International Consortium (COSMIC) [22]–which has brought together data from cohort studies of cognitive aging internationally. The goal of this study was to harmonize these data and apply uniform diagnostic criteria to more reliably estimate MCI prevalence across different geographical and ethnocultural regions. We present data from three studies in USA, four in Europe, two in Asia, and two in Australia.
Materials and Methods
Contributing studies and participants
Cross-sectional analyses of 11 longitudinal population-based studies of cognitive aging (listed in Table 1, with abbreviations) were performed. Rather than the full population of each study, we used samples comprising individuals aged 60 or more years who were not identified as having dementia and/or did not have a CDR [34] ≥ 1. Any individuals with missing age, sex or dementia status data were excluded. A number of samples did not require exclusions for dementia because individuals with dementia were already omitted during the recruitment phase of the study. Table 2 shows the demographic characteristics of the samples used in our analyses, including the main race or ethnicity represented (White in 7 studies and Chinese in 2 studies). As a project of the COSMIC collaboration, the present study was performed with approval from the University of New South Wales Human Research Ethics Committee (Ref: # HC12446). Each of the 11 extant studies contributing data to the present study had previously obtained ethics approval from their respective institutional review boards, and all participants within the studies provided consent (for details see the references listed in Table 1). The particular use of these data for the present study did not warrant further participant consent, with de-identified health data not considered to be protected health information under current research principles (e.g., as per the Privacy Rule proposed by the National Institute of Health, USA http://privacyruleandresearch.nih.gov/research_repositories.asp).
Table 1. Contributing studies.
| Study | Abbreviation | Country | Reference |
|---|---|---|---|
| Cognitive Function & Ageing Studies | CFAS | UK | Brayne et al. [23] |
| Einstein Aging Study | EAS | USA | Katz et al. [16] |
| Etude Santé Psychologique Prévalence Risques et Traitement | ESPRIT | France | Ritchie et al. [24] |
| Hong Kong Memory and Ageing Prospective Study | HK-MAPS | Hong Kong | Wong et al. [25] |
| Invecchiamento Cerebrale in Abbiategraso | Invece.Ab | Italy | Guaita et al. [26] |
| Monongahela Valley Independent Elders Survey | MoVIES | USA | Ganguli et al. [27] |
| Personality and Total Health Through Life Project | PATH | Australia | Anstey et al. [28] |
| Singapore Longitudinal Ageing Studies | SLAS | Singapore | Feng et al. [29, 30] |
| Sydney Memory and Ageing Study | Sydney MAS | Australia | Sachdev et al. [31] |
| Washington Heights Inwood and Columbia Aging Project | WHICAP | USA | Tang et al. [32] |
| Zaragoza Dementia Depression Project | ZARADEMP | Spain | Lobo et al. [33] |
Table 2. Sample characteristics.
| Characteristic | CFAS | EAS | ESPRIT | HK-MAPS | Invece.Ab | MoVIES | PATH | SLAS | Sydney MAS | WHICAP | ZARADEMP |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (N = 2050) | (N = 1954) | (N = 2189) | (N = 786) | (N = 1267) | (N = 1276) | (N = 1973) | (N = 3950) | (N = 1037) | (N = 3991) | (N = 4415) | |
| Age (yrs) | |||||||||||
| Mean ± SD | 75.8 ± 7.3 | 78.3 ± 5.4 | 73.1 ± 5.6 | 72.3 ± 7.2 | 71.2 ± 1.3 | 74.2 ± 5.4 | 70.6 ± 1.5 | 68.5 ± 6.3 | 78.8 ± 4.8 | 76.4 ± 6.5 | 73.4 ± 9.3 |
| Range | 64–105 | 63–100 | 65–96 | 60–96 | 70–75 | 66–97 | 68–74 | 60–97 | 70–90 | 63–103 | 60–102 |
| Sex | |||||||||||
| Female | 1289 (62.9) | 1191 (61.0) | 1277 (58.3) | 422 (53.7) | 684 (54.0) | 775 (60.7) | 953 (48.3) | 2382 (60.3) | 572 (55.2) | 2684 (67.3) | 2518 (57.0) |
| Male | 761 (37.1) | 763 (39.0) | 912 (41.7) | 364 (46.3) | 583 (46.0) | 501 (39.3) | 1020 (51.7) | 1568 (39.7) | 465 (44.8) | 1307 (32.7) | 1897 (43.0) |
| Education | |||||||||||
| Less than completed high school | 195 (9.5) | 428 (21.9) | 550 (25.1) | 686 (87.3) | 1150 (90.8) | 500 (39.2) | 466 (23.6) | 3449 (87.3) | 437 (42.1) | 2163 (54.2) | 3838 (86.9) |
| Completed high school | 1399 (68.2) | 906 (46.4) | 911 (41.6) | 49 (6.2) | 90 (7.1) | 544 (42.6) | 202 (10.2) | 73 (1.8) | 177 (17.1) | 733 (18.4) | 128 (2.9) |
| Technical/college diploma | 286 (14.0) | 97 (5.0) | 210 (9.6) | 8 (1.0) | NA a | 193 (15.1) | 610 (30.9) | 265 (6.7) | 112 (10.8) | 480 (12.0) | 281 (6.4) |
| University degree | 148 (7.2) | 478 (24.5) | 516 (23.6) | 42 (5.3) | 27 (2.1) | 39 (3.1) | 674 (34.2) | 161 (4.1) | 311 (30.0) | 605 (15.2) | 131 (3.0) |
| Missing data | 22 (1.1) | 45 (2.3) | 2 (0.1) | 1 (0.1) | 0 (0.0) | 0 (0.0) | 21 (1.1) | 2 (0.1) | 0 (0.0) | 10 (0.3) | 37 (0.8) |
| Race/ethnicity | White | White (67%); Black (27%) | White | Chinese | White | White | White | Chinese | White | Hispanic (48%); Black (30%); White (21%) | White |
NA = not applicable. Data are n (%) unless stated otherwise. N is for the contributed sample that includes individuals from the full study sample without dementia and with no missing data on the baseline dementia, age and sex variables. Age corresponds to the assessment wave for which data were provided: baseline for all studies except MoVIES (wave 2) and PATH (wave 3). For race/ethnicity, the sample was comprised entirely or predominantly of that shown unless otherwise indicated.
a Technical/college diploma could not be distinguished from Completed high school for Invece.Ab.
Measures and harmonization
Of the 11 contributing studies, nine provided raw data needed to make classifications of MCI (summarized in S1–S5 Tables). The Sydney team processed these data, which were harmonized, when necessary, and pooled. The other two studies, CFAS and Invece.Ab, conducted analyses in-house using the protocols developed for this report. Baseline or wave 1 data were used for all studies except two that did not have all variables needed to make MCI classifications until later waves: MoVIES [27] provided data for wave 2 (2 years after baseline), and PATH [28] for wave 3 (8 years after baseline). Data for SLAS are for two cohorts, SLAS-1 recruited 2003–2004 and SLAS-2 recruited 2008–2011, and for whom the same core measurements and procedures were used [29, 30].
Demographics
Information included age, sex and education. Education data were harmonized by forming a variable with four categories: Less than high school completion; high school completion; technical or college diploma; university degree (as shown in S6 Table). Note that we use the term college diploma in an international context, referring to courses of less duration and standard than a bachelor’s degree that are typically provided by technical, applied, or more vocationally oriented institutions rather than universities. Each of the contributing studies helped determine how the data representing their local education system was best transformed to the four categories we used.
Functional ability
A variety of instruments assessing ADLs and instrumental ADLs (IADLs) was used across the studies (S7 Table), with the Lawton & Brody IADL Scale [35] used by five studies. Six common and compatible IADL items were chosen for harmonization: telephone, food preparation, medications, shopping, finances, and transport. For each of these items, the Lawton & Brody IADL Scale assigns a score of 0 to dependent responses and 1 to independent responses. We produced a dichotomized variable of 0 (dependence) and 1 (independence) for each item by matching responses from different instruments to this scoring system. The strictness or level of assistance required for a classification of dependence varies between items on the Lawton & Brody Scale, and thus a response from another instrument such as “Yes, some difficulty” could be considered independent on one of the harmonized items but dependent on another. For full details of this procedure see S8 and S9 Tables.
Cognitive ability or status
All studies, except for ZARADEMP, administered a neuropsychological test battery; additionally, all except for EAS and WHICAP used the Mini-Mental State Examination (MMSE). However, EAS administered the Blessed Information-Memory-Concentration test, and a validated formula was used to convert scores for this test to MMSE scores [36]. More than half of the studies administered the CDR Scale (Table 3). There was limited overlap in the neuropsychological tests used between studies, and each test score was allocated to one of five cognitive domains: memory, attention/processing speed, language, executive function, and perceptual-motor. However, the perceptual-motor domain was not used in classifying MCI as scores could not be formed for four studies (ESPRIT, HK-MAPS, Invece.Ab, and PATH). Tests were allocated to domains to be consistent with common practice (as outlined in the S1 Text and S10–S14Tables) [37–39]. Domain scores were calculated separately for each study, using information from within the study only. The first step was to adjust test scores for age, sex and education, and for all interactions between these variables using regression analyses. Such adjustments are standard practice in neuropsychological assessment because these variables may significantly affect test performance [37]. Further, the use of age and education adjusted norms has been particularly recommended when assessing the objective cognitive impairment criterion for MCI [11]. Our use of these adjustments should therefore have yielded prevalences for MCI similar to those found were each study to independently make new classifications of MCI using the same set of recent international guidelines. The adjusted test scores were then transformed to Z-scores using the mean and SD of the study sample as normative values. It has been argued and shown that more equivalent and accurate comparisons of cognitive performance between countries are facilitated by the use of country-specific norms [40]. However, for many countries, including those represented by the studies contributing to this investigation, there are no published normative data available. Indeed, a survey of the COSMIC member studies shows that even when norms for particular cognitive tests are available they are often not age-appropriate for elderly samples. Thus, the largely incomplete availability of external norms helped determine our choice to use study-specific internal norms. After forming Z-scores for the tests on the basis of these internal norms, composite scores for each domain were calculated as the mean of the Z-scores of the relevant component tests. These composite scores were themselves then transformed to Z-scores to ensure that all domains had means of 0 and SDs of 1 within each study. Full details and reasons for how domain scores were calculated are in S1 Text.
Table 3. Prevalence of mild cognitive impairment: subtypes, and as based on Clinical Dementia Ratings and Mini-Mental State Examination scores.
| aMCI | naMCI | MMSE | CDR | |||||
|---|---|---|---|---|---|---|---|---|
| Study | Crude | Standardized | Crude | Standardized | Crude | Standardized | Crude | Standardized |
| CFAS | NA | NA | NA | NA | 11.3 (9.1–13.9) | 13.9 (11.7–16.1) | NA | NA |
| EAS | 1.8 (1.3–2.6) | 1.4 (0.9–1.9) | 2.6 (1.9–3.4) | 2.0 (1.4–2.6) | 10.3 (8.9–11.9) | 6.7 (5.7–7.7) | 6.6 (5.4–8.0) | 5.2 (4.1–6.2) |
| ESPRIT | 1.2 (0.8–1.7) | 1.3 (0.7–1.8) | 3.5 (2.8–4.4) | 3.7 (2.8–4.5) | 9.2 (8.1–10.6) | 9.4 (8.0–10.7) | NA | NA |
| HK-MAPS | 1.0 (0.4–2.6) | 0.5 (0.0–0.9) | 4.4 (2.9–6.9) | 5.2 (2.7–7.6) | 14.4 (11.8–17.3) | 14.5 (11.7–17.3) | 13.6 (11.3–16.2) | 14.9 (12.1–17.8) |
| Invece.Ab | 3.9 (3.0–5.2) | 3.0 (2.3–3.7) | 4.4 (3.3–5.8) | 4.0 (3.1–4.9) | 10.7 (9.0–12.7) | 9.9 (8.5–11.2) | NA | NA |
| MoVIES | 2.6 (1.9–3.6) | 2.6 (1.7–3.5) | 4.7 (3.6–6.0) | 5.1 (3.8–6.4) | 18.5 (16.4–20.8) | 19.1 (16.8–21.4) | 1.5 (1.0–2.3) | 1.8 (1.0–2.6) |
| PATH | 1.0 (0.6–1.6) | 1.0 (0.6–1.5) | 2.3 (1.6–3.1) | 2.4 (1.7–3.0) | 1.3 (0.9–2.0) | 2.1 (1.5–2.7) | NA | NA |
| SLAS | 2.0 (1.4–2.9) | 2.2 (1.3–3.1) | 3.2 (2.4–4.2) | 2.8 (1.7–3.9) | 6.5 (5.5–7.6) | 6.7 (5.5–8.0) | 13.6 (11.3–16.3) | 13.9 (10.5–17.3) |
| Sydney MAS | 4.0 (2.9–5.5) | 3.6 (2.5–4.7) | 6.7 (5.3–8.6) | 6.2 (4.7–7.6) | 16.7 (14.4–19.3) | 17.4 (15.1–19.6) | 9.2 (7.4–11.3) | 9.6 (7.8–11.3) |
| WHICAP | 1.6 (1.3–2.1) | 1.5 (1.1–1.9) | 4.8 (4.0–5.6) | 4.6 (3.8–5.4) | NA | NA | 9.5 (8.6–10.5) | 9.3 (8.3–10.2) |
| ZARADEMP | NA | NA | NA | NA | 19.7 (18.4–21.1) | 20.7 (19.2–22.1) | NA | NA |
| Total | 2.0 (1.7–2.2) | 2.0 (1.7–2.2) | 3.9 (3.6–4.2) | 3.9 (3.6–4.2) | 12.0 (11.5–12.5) | 12.0 (11.5–12.4) | 8.5 (8.0–9.2) | 9.0 (8.4–9.6) |
aMCI = amnestic mild cognitive impairment; naMCI = non-amnestic mild cognitive impairment; CDR = Clinical Dementia Rating; MMSE = Mini-Mental State Examination; NA = not applicable. Values are percentage prevalence (95% confidence interval). The objective cognitive impairment criteria for these classifications was for aMCI: performance in the bottom 6.681% of the relevant study for the memory domain; naMCI: performance in the bottom 6.681% of the relevant study for at least one harmonized cognitive domain other than and excluding memory; CDR: a rating of 0.5; MMSE: a score of 24–27. Standardized prevalence estimates were directly standardized for age group and sex, with the standard population being the total sample of all studies included in the analysis; data were imputed for the missing age ranges within Invece.Ab, PATH and Sydney MAS.
Subjective cognitive complaint or concern
The means by which the contributing studies ascertained the presence or absence of a cognitive complaint or concern varied widely. Some studies asked a single question of the participant, while others used different and sometimes multiple approaches that included clinical impression, standardized instruments, and informant reports. We attempted to minimize any biases associated with these differences, particularly those related to having different numbers of opportunities to endorse a complaint, by choosing to use only the most generalized question asked of the participant (either in isolation or extracted from a longer instrument) from each study (see S15 Table). This was also the default option given that some studies only had one relevant item. All of the questions addressed memory only, except those used by SLAS, which also addressed thinking or other mental abilities. We dichotomized the responses to indicate either the presence or absence of a subjective cognitive complaint or concern.
Classification of MCI
MCI was classified using the four generally accepted criteria: absence of dementia, no or minimal functional impairment, subjective memory/cognitive complaint or concern, and objective cognitive impairment [12]. Most studies reported making classifications of dementia using DSM-IV criteria (see S16 Table). Note that a number of studies excluded any individuals with dementia at the recruitment stage of their study. Functional impairment was defined as dependence in two or more harmonized IADL items (the handling of missing data is detailed in S1 Text). Cognitive complaints or concerns were determined as above. Objective cognitive impairment for each cognitive domain was a score within the bottom 6.681% of the scores for that domain within the relevant study’s sample, which is the equivalent of impairment being defined as scores more than 1.5 SDs below the mean. A classification of MCI required impairment in any of the four domains used. Impairment on the memory domain was needed for aMCI, and impairment on any of the other domains (without memory impairment) for naMCI; individuals with data for fewer than three of the non-memory domains were included if impairment was present in one or more domain, otherwise excluded. For other analyses, objective cognitive impairment was defined as an MMSE score from 24 to 27 (inclusive), or as a CDR of 0.5. An MMSE score of 24–27 has been previously used to define a range of milder forms of cognitive impairment, including MCI [41, 42], mild cognitive decline [43] and mild AD [44], and a CDR of 0.5 is a commonly-used criteria for MCI (e.g., [45, 46]).
Statistical analysis
The Sydney team performed all analyses of the harmonized and pooled data. Five different MCI classifications were made: MCI and its aMCI, and naMCI subtypes using harmonized cognitive domain scores for determining objective cognitive impairment; and MCI using each of MMSE and CDR scores for this criterion. For each type of classification, only individuals with complete data for all four MCI criteria were included. Crude prevalence was determined for men and women in three age groups (60–69, 70–79 and 80–89 yrs). The Wilson score method described, evaluated and endorsed by Newcombe [47] was used to determine 95% confidence intervals (CIs), and chi-square tests were used to make comparisons. Prevalence estimates and CIs directly standardized for age and sex were calculated (for details see S1 Text). For studies with participants in only one or two of the age groups, data for the remaining age group or groups were generated using a multiple imputation procedure (outlined in S1 Text). Associations between educational level and MCI were investigated with logistic regressions that controlled for age and sex. The two studies that provided results rather than raw data (CFAS and Invece.Ab) used the standard protocols developed for this report. The analyses were done using IBM SPSS Statistics 20, and the imputations done using the R-package mice 2.21.
Results
Sample description
The demographic characteristics of the cohorts are provided in Table 2. The samples varied in size from 786 (HK-MAPS) to 4,415 (ZARADEMP), with a median of 2,000, and total sample of 24,888 (59.3% women; mean age 73.6 yrs). The purpose and design of both Invece.Ab [26] and PATH [28] led to them having narrower age cohorts than the other contributing studies. The sample sizes for each approach for classifying MCI are shown in S17 Table.
Prevalence of MCI
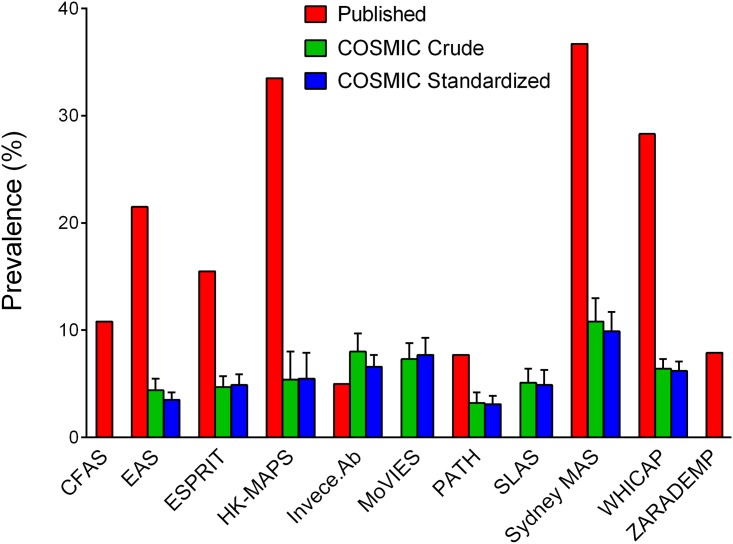
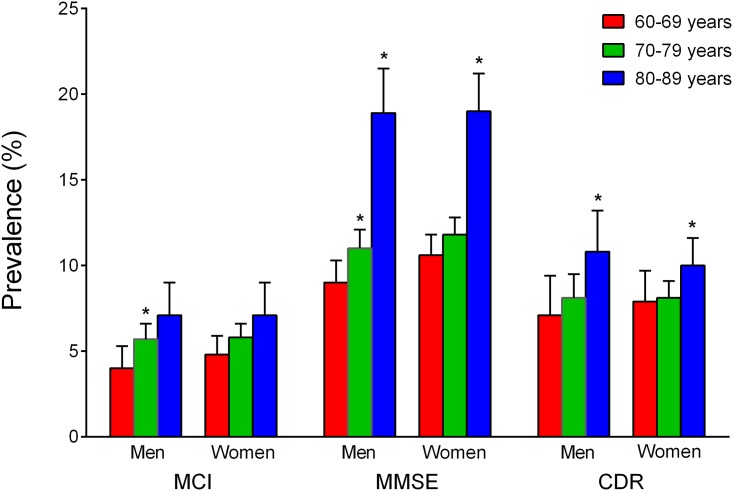
Fig 1 shows the prevalences of MCI previously published by the contributing studies, alongside the crude and standardized prevalences obtained using COSMIC protocols that defined cognitive impairment as performance in the bottom 6.681%. With this criterion, the crude prevalence was 5.9 (5.5–6.3)% overall, and increased with age: from 4.5% among 60–69 year-olds to 5.8% among 70–79 year-olds (χ2 = 6.80, df = 1, P = .009), and to 7.1% among 80–89 year-olds (χ2 = 5.28, df = 1, P = .022 vs. 70–79 year-olds). The crude prevalence for men was higher among 70–79 year-olds than among 60–69 year-olds (χ2 = 4.62, df = 1, P = .032), but not significantly higher among 80–89 year-olds than 70–79 year-olds (see Fig 2). For women, the only increase was from 60–69 year-olds to 80–89 year-olds (χ2 = 7.82, df = 1, P = .005). There were no significant differences between men and women within any of the age groups. The average age- and sex-standardized prevalence for 60–89 year-olds was 5.8 (5.4–6.2)%. The standardized prevalence differed across the studies (χ2 = 94.64, df = 8, P < .001), but not between Chinese (5.2%, 95% CI = 4.1–6.4%) and Whites (5.8%, 5.3–6.3%; χ2 = 0.76, df = 1, P = .383).
Fig 1. Prevalence estimates of mild cognitive impairment previously published and as obtained using COSMIC protocols.
Error bars indicate the upper limits of 95% confidence intervals. For the crude and standardized prevalence estimates obtained using COSMIC protocols, the criterion for objective cognitive impairment was performance in the bottom 6.681% for the study on at least one harmonized cognitive domain. Estimates were directly standardized for age and sex, with the standard population being the total sample of all studies included in the analysis; data were imputed for missing age ranges within Invece.Ab, PATH and Sydney MAS. SLAS had not previously published prevalence estimates of mild cognitive impairment (MCI), and a published estimate for MoVIES was for amnestic MCI only [19]. CFAS and ZARADEMP did not have neuropsychological test data from which harmonized cognitive domain scores could be derived. Published prevalence estimates are for baseline, except for PATH (wave 3, the first assessment when all relevant data for classifying MCI were obtained). References for the published estimates shown are: CFAS [48]; EAS [16]; ESPRIT [24]; HK-MAPS [25]; Invece.Ab [49]; PATH [50]; Sydney MAS [51]; WHICAP [52]; ZARADEMP [53]. Note that the HK-MAPS sample was over-represented by individuals considered to be at increased risk of conversion to dementia, and the prevalence estimates for MCI shown are likely to overestimate those for the broader population [25].
Fig 2. Crude prevalence estimates of mild cognitive impairment (MCI) among men and women of different age groups.
Error bars indicate upper limits of 95% confidence intervals. Asterisks indicate a significant difference from: * 60–69 years; ** 70–79 years. There were no significant differences between men and women of the same age group for any classification approach. The objective cognitive impairment criteria for the classifications was performance in the bottom 6.681% of the relevant study for at least one harmonized cognitive domain (mild cognitive impairment), a Clinical Dementia Rating (CDR) of 0.5, or a Mini-Mental State Examination (MMSE) score 24–27.
Higher figures were obtained when MMSE scores 24–27 were used as the criterion, with an overall total crude prevalence of 12% (see Table 3). Crude prevalence estimates were greater among 70–79 year-olds than 60–69 year-olds for men (χ2 = 5.80, df = 1, P = .016), and greater among 80–89 year-olds than 70–79 year-olds for both men (χ2 = 43.10, df = 1, P < .001) and women (χ2 = 46.07, df = 1, P < .001; Fig 2). There were no significant differences between men and women within any of the age groups. Standardized prevalence estimates were significantly higher for White populations (12.9%, 12.3–13.4%) than for Chinese (8.6%, 7.4–9.7%; χ2 = 42.34, df = 1, P < .001). All studies except WHICAP had MMSE scores, and it is noteworthy that the Spanish study (ZARADEMP), which only had MMSE scores, yielded the highest crude and standardized prevalence figures using this measure, thereby influencing the overall prevalence estimates. The CDR, administered by only six studies, yielded prevalence estimates of 8.5% (overall crude) and 9.0% (overall standardized), which were in between those based on MMSE scores and those based on harmonized cognitive domain scores (see Table 3). CDR-based prevalence estimates were significantly greater among 80–89 year-olds than 70–79 year-olds for both men (χ 2 = 4.74, df = 1, P = .030) and women (χ 2 = 4.46, df = 1, P = .035; Fig 2). The correspondence between the prevalence estimates with MMSE or CDR was low.
The range of MCI prevalence estimates published by the contributing studies was 5.0%–36.7% (see Fig 1). This considerable variation in estimates was reduced with all three of the definitions for cognitive impairment that we used: performance in the bottom 6.681% (3.2%–10.8%); CDR of 0.5 (1.8%–14.9%); MMSE score of 24–27 (2.1%–20.7%).
Prevalence of MCI subtypes
The overall crude prevalence of aMCI was 2.0% and of naMCI 3.9% (see Table 3). Prevalence estimates of aMCI did not differ significantly across age groups or by sex (S1 Fig). Prevalence estimates of naMCI were greater among 70–79 year-olds than 60–69 year-olds for men (χ2 = 5.06, df = 1, P = .024), and greater among 80–89 year-olds than 70–79 year-olds for women (χ2 = 4.95, df = 1, P = .026), but there were no sex differences. On the basis of standardized estimates, there were no differences in the prevalence of either subtype between Whites (2.1%, 1.8–2.4% for aMCI and 3.8%, 3.4–4.2% for naMCI) and Chinese (1.8%, 1.1–2.5% for aMCI and 3.6%, 2.6–4.6% for naMCI; χ2 = 0.19, df = 1, P = .663 and χ2 = 0.39, df = 1, P = .532, respectively).
Education and MCI
Compared to the lowest level (not having completed high school), all higher levels of education conveyed a reduced likelihood of MCI. The odds ratios were 0.58 (P < .001) for having completed high school, 0.55 (P < .001) for technical college or a diploma, and 0.73 (P = .002) for a university degree (S18 Table). Controlling for education however only partially reduced variation in prevalence across studies (further described in S2 Text).
Effects of age on subjective memory complaints, functional independence, and objective cognitive impairment
We conducted supplementary analyses to determine the extent to which effects of age on the harmonized variables used to classify MCI may have contributed to our finding that the prevalence of MCI increased with age (values are detailed in S1–S3 Tables). The rate of subjective memory complaints increased with age, from 26.4% among 60–69 year-olds to 30.7% among 70–79 year-olds (χ2 = 33.95, df = 1, P < .001), and to 37.5% among 80–89 year-olds (χ2 = 67.58, df = 1, P < .001 vs. 70–79 year-olds). Conversely, the rates of functional independence decreased with age, from 97.7% among 60–69 year-olds to 94.5% among 70–79 year-olds (χ2 = 112.63, df = 1, P < .001), and to 83.8% among 80–89 year-olds (χ2 = 480.77, df = 1, P < .001 vs. 70–79 year-olds). There was no significant difference in the rate of objective cognitive impairment between 60–69 year-olds (20.6%) and 70–79 year-olds (19.5%; χ2 = 1.84, df = 1, P = .175), though the rate was higher for 80–89 year-olds (24.5%) than for 70–79 year-olds (χ2 = 30.06, df = 1, P < .001).
Discussion
We analysed pooled data from 11 international cohort studies and found that applying uniform criteria to harmonized data greatly reduced the variation in MCI prevalence internationally. This was the case with each of the three definitions of cognitive impairment that we used to make separate classifications of MCI: performance in the bottom 6.681%, CDR of 0.5, and MMSE score of 24–27. The overall estimates found with these methods were between 6% and 12%, at the lower end of the 3% to 42% range reported by the international studies included in a recent review [14]. Our estimates for the studies contributing to the present investigation are also mostly lower than they themselves have previously published (Fig 1), which is due to the differential criteria used. Differences in the criteria for objective cognitive impairment may be particularly relevant [20], even in some cases where the same −1.5 SD threshold recommended by published criteria [11, 54] is used (and as per our definition of impairment being performance in the bottom 6.681%). For example, the criterion for impairment in the Sydney MAS was performance on any one of 12 individual neuropsychological tests being 1.5 SDs below published normative values [51]. In contrast, the COSMIC criterion for impairment was one of only four cognitive domain scores <−1.5 SD. The COSMIC approach of applying performance thresholds to domain scores, rather than to individual tests, was taken to prevent different prevalence estimates of MCI resulting merely from differences in the number of tests administered. The use of the −1.5 SD threshold in COSMIC also made a difference; e.g., EAS had previously used a 20th percentile (approximately −0.84 SD) threshold [16]. For purposes of harmonization, we used only the most generalized self-report item from each study to ascertain the presence of a cognitive complaint. However, some of the contributing studies administered multiple cognitive complaint questions and/or scales to their participants, and sometimes also sought informant reports. With multiple opportunities, a participant may be more likely to endorse a complaint and thus more likely to be classified as having MCI (if meeting the other criteria). This could help account for why the prevalences of MCI we determined are lower than those previously reported by some studies. It must also be stated that the exclusion of dementia for this analysis altered the denominator in some of the studies, thereby influencing the prevalence estimates, albeit to a small extent only. Note that not all studies contained participants with dementia in their original samples, with some excluding individuals with dementia at the time of recruitment.
There being higher prevalence of MCI when less stringent criteria are applied reinforces the need for a harmonized approach. Compared to the −1.5 SD threshold for cognitive impairment we used, the DSM-5 definition of mild neurocognitive disorder recommends a less stringent criterion of −1.0 to −2.0 SD, without specifying how many tests should comprise a domain. Of course, the use of a threshold assumes that normative data are available for each test. We derived norms from the non-demented population of the same study. This approach offers the advantage of removing potential sociocultural and ethnic biases in any external source of normative data uniformly applied across all studies, and a similar approach was used by the 10/66 group [15]. A disadvantage is that it will mask the true extent of real differences in the populations themselves. In our study, use of this approach produced nearly identical percentages of impairment within each cognitive domain investigated. However, there were overall differences in impairment between studies because of differences in the number of individuals with impairment in multiple domains (see S3 Table). Even so, differences in MCI criteria other than objective cognitive impairment, including subjective memory complaints and functional independence, should be considered as major influences on the differences in MCI prevalence estimates we observed when using this particular approach.
Differences in MCI prevalence between studies may also stem from differences in methodology other than MCI criteria, including differences in recruitment procedures. It has been shown that including institutionalized individuals and obtaining proxy-based data for others either unable or unwilling to participate directly can elevate estimates of moderate and severe dementia prevalence [55]. A similar effect could be expected for MCI, and thus differences in response rates and the inclusion of institutionalized individuals in 3 of the 11 samples are likely to have contributed to some of the pre-existing and remaining (post-harmonization) variance in MCI prevalence across the studies we investigated.
In our study, the prevalence was about twice as high if MMSE was used to define objective impairment. The MMSE has many limitations when used for this purpose: it has age and education biases [56]; it shows cultural and linguistic artefacts [57]; it is strongly influenced by verbal memory function while not covering all domains of cognition adequately; and, though adopted as a definition for MCI by others [41, 42], the range of 24–27 for MCI has not been validated. Prevalence estimates using a CDR score of 0.5 as the basis for cognitive impairment were in between the estimates based on MMSE scores and those based on harmonized cognitive domain scores. A CDR score of 0.5 is a commonly-used criteria for MCI (e.g., [45, 46]). However, the use of CDR for the diagnosis of MCI has not been established; it is informant-dependent and requires clinical judgment that is difficult to standardize, and its correspondence with the generally accepted criteria for MCI is low in our study.
We did not find any significant sex differences in MCI prevalence. This is consistent with some previous literature [7, 15], but a possibly higher prevalence in men has also been reported [18]. We did find that the prevalence of MCI increased with age, though the pattern across age groups differed between men and women. There were also differences in how the prevalence of MCI increased with age across the three definitions of cognitive impairment we used. Prevalences determined on the basis of MMSE scores exhibited the largest increase with age, whereas those determined on the basis of performance in the bottom 6.681% showed the smallest (see Fig 2). The smaller changes observed with the latter definition are not surprising, given that age effects were likely underestimated by the use of age-adjusted neuropsychological test scores. Supplementary analyses on the harmonized variables used in classifying MCI suggest that an increase across the age groups in subjective memory complaints helped drive the increase in MCI with age. Conversely, rates of functional independence decreased with age. The increase in prevalence with age we found for MCI based on MMSE scores comes closest (of the different definitions used) to matching the exponential rise with age found for the global prevalence of dementia [58]. That study also found the global prevalence of dementia to be greater among women than among men, which differs from our findings for MCI. This suggests that MCI should not be conceptualized solely as a pre-dementia syndrome, but as a distinct syndrome with some overlap with pre-dementia. This, and MCI being associated with subtle impairments in high level or complex functional tasks [11, 13] that pose a burden on the individual and society, makes the prevalence of MCI of great interest in its own right.
We observed higher rates of MCI for White European populations than for Chinese when these were based on MMSE scores. Direct comparisons of dementia rates between Chinese and Whites appear to be scarce, and even more so for MCI. Previous work suggests the possibility of lower rates of dementia in China and Singapore compared to rates for the USA and Europe [59]. While loosely consistent with this, our findings of higher rates of MCI among Whites should be viewed very tentatively for a number of reasons. These include limitations in using the MMSE to classify MCI (as described above), there being no difference in rates between Chinese and Whites with the other definitions for MCI, and neither of the Chinese samples we investigated coming from mainland China.
The prevalence of MCI was lower in those with higher education, despite the neuropsychological test results having been corrected for education. Compared to not having completed high school, an apparent protective effect was found for all levels of education from having completed high school and above. However, though this effect was significant for having tertiary education (odds ratio = 0.73), it was not as strong as for either having completed high school (odds ratio = 0.58) or technical college/diploma (odds ratio = 0.55). The likely protective effect of education is consistent with the literature of a lower prevalence of dementia [60] and cognitive decline [61] in those with higher education.
It is noteworthy that our analysis showed higher prevalence estimates of naMCI to aMCI by a ratio of nearly 2:1, which is consistent with some studies [62, 63] but contrary to another [7]. The literature, however, has not examined naMCI with the same rigor as aMCI, and the common use of the 1999 Mayo Clinic criteria for MCI [54] conflates aMCI with MCI. It is arguable that our finding is artefactual since there are three non-memory domains, and it is thus statistically more likely for an individual to have impairment in a non-memory domain than in the sole memory domain. However, it may also be the case that a higher prevalence of naMCI stems from this being a more heterogeneous and unstable condition than aMCI, as evidenced by less progression to dementia and higher rates of reversion to normal cognition upon follow-up [64–66]. This issue deserves further study as it has potentially important clinical implications.
Strengths of our study include the large number of independent cohorts examined from diverse geographical, ethnic and sociocultural groups, and rigorous standardization of data. However, there are also some weaknesses. While the samples were epidemiologically derived, they were from specific regions and cannot be said to be necessarily representative of the countries or entire populations they come from. While all studies are longitudinal, this analysis is cross-sectional. Different instruments were used in the different studies, and ideally the harmonization process should begin at the time of study inception and not retrospectively. Cultural effects are also not to be ignored. For example, differences in rates of functional independence between studies could be influenced by cultural differences in reporting disability [67]. This in turn could contribute to differences in the estimated prevalences of MCI between studies (though the study with the lowest rate of dependence, ESPRIT, also had a lower prevalence of MCI than the study with the highest rate of dependence, WHICAP). Two studies had Chinese populations, but both were in high income countries, and while the American studies had some participants from black and Hispanic communities, these data are not presented separately. We have also restricted the analyses to prevalence figures and not examined determinants, which is worthy of future work.
Supporting Information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
The members of the contributing COSMIC studies are: CFAS: CB (study leader), FEM, BCMS; EAS: RBL, MJK (study leaders); ESPRIT: KR, MLA (study leaders), IC; HK-MAPS: LCWL (study leader), CHYW, AWTF; Invece.Ab: AG (study leader), RV, AD; MoVIES: MG (study leader), HHD, TH; PATH: KJA (study leader), NC, PB; SLAS I & II: TPN (study leader), QG; Sydney MAS: PSS, HB (study leaders), DML, NAK, JDC, AT, GA, SR; WHICAP: NS (study leader), JM, YS; ZARADEMP: AL (study leader), RLA, JS.
The authors of particular studies acknowledge: EAS: the contributions of Molly Zimmerman and Carol Derby; HK-MAPS: the contributions of Grace T.Y. Leung, Wai Chi Chan, Department of Health of Hong Kong SAR, the participants and the social centres for their assistance in the assessment, and thank Novartis and Astra Zeneca for their sponsorship of souvenirs for the participants in the baseline study; (Invece.Ab): the further study members Letizia Polito, Simona Abbondanza, Eleonora Valle, Mauro Colombo, Silvia Francesca Vitali, Silvia Fossi, Daniele Zaccaria and the contributions of Gianluigi Forloni, ”Mario Negri” Institute for Pharmacological Research, Milan, Italy and Simona Villani, University of Pavia, Pavia, Italy, and are also grateful to the relative’s association, “Federazione Alzheimer Italia”, Milan, Italy, for supporting the study. MoVIES: the contributions of 1681 study participants from the Monongahela Valley and of multiple MoVIES project personnel over the years. PATH: the further study members Helen Christensen, Andrew MacKinnon, Simon Easteal, Project Managers Trish Jacomb, Karen Maxwell, participants and the NHMRC. SLAS I and II: and gratefully thank the help and support of the following voluntary welfare organizations: Geylang East Home for the Aged, Presbysterian Community Services, Thye Hua Kwan Moral Society (Moral Neighbourhood Links), Yuhua Neighbourhood Link, Henderson Senior Citizens’ Home, NTUC Eldercare Co-op Ltd, Thong Kheng Seniors Activity Centre (Queenstown Centre), Redhill Moral Seniors Activity Centre, SARAH Seniors Activity Centre, and Training, Research Academy at Jurong Point (TaRA@JP). Sydney MAS: the contributions of members of the MAS Team: Allison Bowman, Kim Burns, Anthony Broe, Joula Dekker, Louise Dooley, Michele de Permentier, Sarah Fairjones, Janelle Fletcher, Therese French, Cathy Foster, Emma Nugent-Cleary-Fox, Chien Gooi, Evelyn Harvey, Rebecca Helyer, Sharpley Hsieh, Laura Hughes, Sarah Jacek, Mary Johnston, Donna McCade, Samantha Meeth, Eveline Milne, Angharad Moir, Ros O’Grady, Kia Pfaeffli, Carine Pose, Laura Reuser, Amanda Rose, Peter Schofield, Zeeshan Shahnawaz, Amanda Sharpley, Claire Thompson, Wiebke Queisser, and Sam Wong. WHICAP: the contributions of Richard Mayeux, Principal Investigator of the WHICAP study, co-investigators Adam Brickman and Jose Luchsinger, and study team members Danurys Sanchez, Ming X. Tang and Howard Andrews. ZARADEMP: the further study members Guillermo Marcos, Concepción De-la-Cámara, Pedro Saz, Tirso Ventura, Miguel Angel Quintanilla, and Elena Lobo, and the contributions of the ZARADEMP Workgroup who participated in the study.
Data Availability
Data were provided by the contributing studies to COSMIC on the understanding and proviso that the relevant study leaders be contacted for any further use of their data. Author affiliations with the contributing studies are listed in the Acknowledgments, and contact details can be found on the COSMIC website (http://cheba.unsw.edu.au/group/cosmic).
Funding Statement
National Health and Medical Research Council of Australia Program Grant (ID 568969; PSS). For the contributing studies: Major awards from the UK Medical Research Council and the Department of Health (CB, FEM, BCMS); National Institute on Health/National Institute on Aging grants (5P01 AG003949, 1R03 AG045474; RBL, MJK); Novartis (KR, MLA, IC); Mr. Lai Seung Hung & Mrs. Lai Chan Pui Ngong Dementia in Hong Kong Research Fund, and an educational fund from Eisai (LCWL, CHYW, AWTF); Fondazione Golgi Cenci and Federazione Alzheimer Italia (AG, RV, AD); National Institute on Aging, National Institutes of Health, United States Department of Health and Human Services (Grant # R01AG07562; MG, HD, TH); National Health and Medical Research Council of Australia (Grants 973302, 179805, 157125 and 1002160; KJA, NC, PB); Research grants (No. 03/121/17/214 and No. 08/1/21/19/567) from the Biomedical Research Council, Agency for Science, Technology and Research (A*STAR) in Singapore (TPN, QG); National Health & Medical Research Council of Australia Program Grant (ID 350833; PSS, DML, NAK, JDC, AT, GA, SR, HB); National Institute of Health/National Institute on Aging (Grants # R01 AG037212, P01 AG07232; NS, JM, YS); Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Spanish Ministry of Health, Madrid, Spain (Grants 94/1562, 97/1321E, 98/0103, 01/0255, 03/0815, 06/0617, and G03/128) and Pfizer Foundation, Madrid (AL, RLA, JS). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Petersen RC, Caracciolo B, Brayne C, Gauthier S, Jelic V, Fratiglioni L. Mild cognitive impairment: a concept in evolution. J Intern Med. 2014;275(3):214–28. 10.1111/joim.12190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–72. [DOI] [PubMed] [Google Scholar]
- 3. Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136–9. [DOI] [PubMed] [Google Scholar]
- 4. Farias ST, Mungas D, Reed BR, Harvey D, DeCarli C. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Arch Neurol. 2009;66(9):1151–7. 10.1001/archneurol.2009.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Flicker C, Ferris SH, Reisberg B. Mild cognitive impairment in the elderly: predictors of dementia. Neurology. 1991;41(7):1006–9. [DOI] [PubMed] [Google Scholar]
- 6. Ganguli M, Snitz BE, Saxton JA, Chang CC, Lee CW, Vander Bilt J, et al. Outcomes of mild cognitive impairment by definition: a population study. Arch Neurol. 2011;68(6):761–7. 10.1001/archneurol.2011.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Petersen RC, Roberts RO, Knopman DS, Boeve BF, Geda YE, Ivnik RJ, et al. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66(12):1447–55. 10.1001/archneurol.2009.266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Aretouli E, Okonkwo OC, Samek J, Brandt J. The fate of the 0.5s: predictors of 2-year outcome in mild cognitive impairment. J Int Neuropsychol Soc. 2011;17(2):277–88. 10.1017/S1355617710001621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sachdev PS, Lipnicki DM, Crawford J, Reppermund S, Kochan NA, Trollor JN, et al. Factors predicting reversion from mild cognitive impairment to normal cognitive functioning: a population-based study. PLoS One. 2013;8(3):e59649 10.1371/journal.pone.0059649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256(3):183–94. [DOI] [PubMed] [Google Scholar]
- 11. Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7(3):270–9. 10.1016/j.jalz.2011.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund LO, et al. Mild cognitive impairment—beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med. 2004;256(3):240–6. [DOI] [PubMed] [Google Scholar]
- 13. Reppermund S, Brodaty H, Crawford JD, Kochan NA, Draper B, Slavin MJ, et al. Impairment in instrumental activities of daily living with high cognitive demand is an early marker of mild cognitive impairment: the Sydney Memory and Ageing Study. Psychol Med. 2013;43(11):2437–45. 10.1017/S003329171200308X [DOI] [PubMed] [Google Scholar]
- 14. Ward A, Arrighi HM, Michels S, Cedarbaum JM. Mild cognitive impairment: disparity of incidence and prevalence estimates. Alzheimers Dement. 2012;8(1):14–21. 10.1016/j.jalz.2011.01.002 [DOI] [PubMed] [Google Scholar]
- 15. Sosa AL, Albanese E, Stephan BC, Dewey M, Acosta D, Ferri CP, et al. Prevalence, distribution, and impact of mild cognitive impairment in Latin America, China, and India: a 10/66 population-based study. PLoS Med. 2012;9(2):e1001170 10.1371/journal.pmed.1001170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Katz MJ, Lipton RB, Hall CB, Zimmerman ME, Sanders AE, Verghese J, et al. Age-specific and sex-specific prevalence and incidence of mild cognitive impairment, dementia, and Alzheimer dementia in blacks and whites: a report from the Einstein Aging Study. Alzheimer Dis Assoc Disord. 2012;26(4):335–43. 10.1097/WAD.0b013e31823dbcfc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. O'Bryant SE, Johnson L, Reisch J, Edwards M, Hall J, Barber R, et al. Risk factors for mild cognitive impairment among Mexican Americans. Alzheimers Dement. 2013;9(6):622–31 e1 10.1016/j.jalz.2012.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Petersen RC, Roberts RO, Knopman DS, Geda YE, Cha RH, Pankratz VS, et al. Prevalence of mild cognitive impairment is higher in men. The Mayo Clinic Study of Aging. Neurology. 2010;75(10):889–97. 10.1212/WNL.0b013e3181f11d85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ganguli M, Dodge HH, Shen C, DeKosky ST. Mild cognitive impairment, amnestic type: an epidemiologic study. Neurology. 2004;63(1):115–21. [DOI] [PubMed] [Google Scholar]
- 20. Kochan NA, Slavin MJ, Brodaty H, Crawford JD, Trollor JN, Draper B, et al. Effect of different impairment criteria on prevalence of "objective" mild cognitive impairment in a community sample. Am J Geriatr Psychiatry. 2010;18(8):711–22. [DOI] [PubMed] [Google Scholar]
- 21. Bondi MW, Smith GE. Mild cognitive impairment: a concept and diagnostic entity in need of input from neuropsychology. J Int Neuropsychol Soc. 2014;20(2):129–34. 10.1017/S1355617714000010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sachdev PS, Lipnicki DM, Kochan NA, Crawford JD, Rockwood K, Xiao S, et al. COSMIC (Cohort Studies of Memory in an International Consortium): an international consortium to identify risk and protective factors and biomarkers of cognitive ageing and dementia in diverse ethnic and sociocultural groups. BMC Neurol. 2013;13:165 10.1186/1471-2377-13-165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Brayne C, McCracken C, Matthews FE. Cohort profile: the Medical Research Council Cognitive Function and Ageing Study (CFAS). Int J Epidemiol. 2006;35(5):1140–5. [DOI] [PubMed] [Google Scholar]
- 24. Ritchie K, Carriere I, Ritchie CW, Berr C, Artero S, Ancelin ML. Designing prevention programmes to reduce incidence of dementia: prospective cohort study of modifiable risk factors. BMJ. 2010;341:c3885 10.1136/bmj.c3885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wong CH, Leung GT, Fung AW, Chan WC, Lam LC. Cognitive predictors for five-year conversion to dementia in community-dwelling Chinese older adults. Int Psychogeriatr. 2013;25(7):1125–34. 10.1017/S1041610213000161 [DOI] [PubMed] [Google Scholar]
- 26. Guaita A, Colombo M, Vaccaro R, Fossi S, Vitali SF, Forloni G, et al. Brain aging and dementia during the transition from late adulthood to old age: design and methodology of the "Invece.Ab" population-based study. BMC Geriatr. 2013;13:98 10.1186/1471-2318-13-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ganguli M, Dodge HH, Chen P, Belle S, DeKosky ST. Ten-year incidence of dementia in a rural elderly US community population: the MoVIES Project. Neurology. 2000;54(5):1109–16. [DOI] [PubMed] [Google Scholar]
- 28. Anstey KJ, Christensen H, Butterworth P, Easteal S, Mackinnon A, Jacomb T, et al. Cohort profile: the PATH through life project. Int J Epidemiol. 2012;41(4):951–60. 10.1093/ije/dyr025 [DOI] [PubMed] [Google Scholar]
- 29. Feng L, Chong MS, Lim WS, Lee TS, Collinson SL, Yap P, et al. Metabolic syndrome and amnestic mild cognitive impairment: singapore longitudinal ageing study-2 findings. J Alzheimers Dis. 2013;34(3):649–57. 10.3233/JAD-121885 [DOI] [PubMed] [Google Scholar]
- 30. Feng L, Gwee X, Kua EH, Ng TP. Cognitive function and tea consumption in community dwelling older Chinese in Singapore. J Nutr Health Aging. 2010;14(6):433–8. [DOI] [PubMed] [Google Scholar]
- 31. Sachdev PS, Brodaty H, Reppermund S, Kochan NA, Trollor JN, Draper B, et al. The Sydney Memory and Ageing Study (MAS): methodology and baseline medical and neuropsychiatric characteristics of an elderly epidemiological non-demented cohort of Australians aged 70–90 years. Int Psychogeriatr. 2010;22(8):1248–64. 10.1017/S1041610210001067 [DOI] [PubMed] [Google Scholar]
- 32. Tang MX, Cross P, Andrews H, Jacobs DM, Small S, Bell K, et al. Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neurology. 2001;56(1):49–56. [DOI] [PubMed] [Google Scholar]
- 33. Lobo A, Saz P, Marcos G, Día J, De-la-Cámara C, Ventura T, et al. The ZARADEMP Project on the incidence, prevalence and risk factors of dementia (and depression) in the elderly community: II. Methods and first results. Eur J Psychiatry. 2005;19:40–54. [Google Scholar]
- 34. Morris JC. Clinical dementia rating: a reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. Int Psychogeriatr. 1997;9 (Suppl 1):173–6. [DOI] [PubMed] [Google Scholar]
- 35. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–86. [PubMed] [Google Scholar]
- 36. Thal LJ, Grundman M, Golden R. Alzheimer's disease: a correlational analysis of the Blessed Information-Memory-Concentration Test and the Mini-Mental State Exam. Neurology. 1986;36(2):262–4. [DOI] [PubMed] [Google Scholar]
- 37. Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4 ed New York, NY: Oxford University Press; 2004. [Google Scholar]
- 38. Strauss E, Sherman EMS, Spreen O. A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary. 3rd ed New York, NY: Oxford University Press; 2006. [Google Scholar]
- 39. Weintraub S, Salmon D, Mercaldo N, Ferris S, Graff-Radford NR, Chui H, et al. The Alzheimer's Disease Centers' Uniform Data Set (UDS): the neuropsychologic test battery. Alzheimer Dis Assoc Disord. 2009;23(2):91–101. 10.1097/WAD.0b013e318191c7dd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hayden KM, Makeeva OA, Newby LK, Plassman BL, Markova VV, Dunham A, et al. A comparison of neuropsychological performance between US and Russia: Preparing for a global clinical trial. Alzheimers Dement. 2014;10(6):760–8 e1 10.1016/j.jalz.2014.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Gussekloo J, Westendorp RG, Remarque EJ, Lagaay AM, Heeren TJ, Knook DL. Impact of mild cognitive impairment on survival in very elderly people: cohort study. BMJ. 1997;315(7115):1053–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Vellas B, Andrieu S, Sampaio C, Wilcock G. Disease-modifying trials in Alzheimer's disease: a European task force consensus. Lancet Neurol. 2007;6(1):56–62. [DOI] [PubMed] [Google Scholar]
- 43. Neale R, Brayne C, Johnson AL. Cognition and survival: an exploration in a large multicentre study of the population aged 65 years and over. Int J Epidemiol. 2001;30(6):1383–8. [DOI] [PubMed] [Google Scholar]
- 44. Wang W, Shinto L, Connor WE, Quinn JF. Nutritional biomarkers in Alzheimer's disease: the association between carotenoids, n-3 fatty acids, and dementia severity. J Alzheimers Dis. 2008;13(1):31–8. [DOI] [PubMed] [Google Scholar]
- 45. Miller SL, Fenstermacher E, Bates J, Blacker D, Sperling RA, Dickerson BC. Hippocampal activation in adults with mild cognitive impairment predicts subsequent cognitive decline. J Neurol Neurosurg Psychiatry. 2008;79(6):630–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Moustafa AA, Hewedi DH, Eissa AM, Myers CE, Sadek HA. The relationship between associative learning, transfer generalization, and homocysteine levels in mild cognitive impairment. PLoS One. 2012;7(9):e46496 10.1371/journal.pone.0046496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17(8):857–72. [DOI] [PubMed] [Google Scholar]
- 48. Stephan BC, Matthews FE, McKeith IG, Bond J, Brayne C. Early cognitive change in the general population: how do different definitions work? J Am Geriatr Soc. 2007;55(10):1534–40. [DOI] [PubMed] [Google Scholar]
- 49. Guaita A, Abbondanza S, Colombo M, Davin A, Forloni G, Polito L, et al. Cognitive impairment, dementia and "good perfomers": prevalence in the population study "InveCe.Ab" [abstract]. J Nutr Health Aging. 2012;16:827–8. [Google Scholar]
- 50. Anstey KJ, Cherbuin N, Eramudugolla R, Sargent-Cox K, Easteal S, Kumar R, et al. Characterizing mild cognitive disorders in the young-old over 8 years: prevalence, estimated incidence, stability of diagnosis, and impact on IADLs. Alzheimers Dement. 2013;9(6):640–8. 10.1016/j.jalz.2012.11.013 [DOI] [PubMed] [Google Scholar]
- 51. Brodaty H, Heffernan M, Kochan NA, Draper B, Trollor JN, Reppermund S, et al. Mild cognitive impairment in a community sample: the Sydney Memory and Ageing Study. Alzheimers Dement. 2013;9(3):310–7 e1 10.1016/j.jalz.2011.11.010 [DOI] [PubMed] [Google Scholar]
- 52. Manly JJ, Bell-McGinty S, Tang MX, Schupf N, Stern Y, Mayeux R. Implementing diagnostic criteria and estimating frequency of mild cognitive impairment in an urban community. Arch Neurol. 2005;62(11):1739–46. [DOI] [PubMed] [Google Scholar]
- 53. Lopez-Anton R, Santabarbara J, De-la-Camara C, Gracia-Garcia P, Lobo E, Marcos G, et al. Mild cognitive impairment diagnosed with the new DSM-5 criteria: prevalence and associations with non-cognitive psychopathology. Acta Psychiatr Scand. 2015;131(1):29–39. 10.1111/acps.12297 [DOI] [PubMed] [Google Scholar]
- 54. Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Archives of Neurology. 1999;56(3):303–8. [DOI] [PubMed] [Google Scholar]
- 55. Riedel-Heller SG, Schork A, Matschinger H, Angermeyer MC. Recruitment procedures and their impact on the prevalence of dementia. Results from the Leipzig Longitudinal Study of the Aged (LEILA75+). Neuroepidemiology. 2000;19(3):130–40. [DOI] [PubMed] [Google Scholar]
- 56. Anderson TM, Sachdev PS, Brodaty H, Trollor JN, Andrews G. Effects of sociodemographic and health variables on Mini-Mental State Exam scores in older Australians. Am J Geriatr Psychiatry. 2007;15(6):467–76. [DOI] [PubMed] [Google Scholar]
- 57. Escobar JI, Burnam A, Karno M, Forsythe A, Landsverk J, Golding JM. Use of the Mini-Mental State Examination (MMSE) in a community population of mixed ethnicity. Cultural and linguistic artifacts. J Nerv Ment Dis. 1986;174(10):607–14. [DOI] [PubMed] [Google Scholar]
- 58. Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9(1):63–75 e2 10.1016/j.jalz.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 59. Graham C, Howard R, Ha Y. Dementia and ethnicity. Int Psychogeriatr. 1998;10(2):183–91. [DOI] [PubMed] [Google Scholar]
- 60. Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol. 2011;10(9):819–28. 10.1016/S1474-4422(11)70072-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Plassman BL, Williams JW Jr., Burke JR, Holsinger T, Benjamin S. Systematic review: factors associated with risk for and possible prevention of cognitive decline in later life. Ann Intern Med. 2010;153(3):182–93. 10.7326/0003-4819-153-3-201008030-00258 [DOI] [PubMed] [Google Scholar]
- 62. Luck T, Luppa M, Briel S, Matschinger H, Konig HH, Bleich S, et al. Mild cognitive impairment: incidence and risk factors: results of the leipzig longitudinal study of the aged. J Am Geriatr Soc. 2010;58(10):1903–10. 10.1111/j.1532-5415.2010.03066.x [DOI] [PubMed] [Google Scholar]
- 63. Luck T, Riedel-Heller SG, Luppa M, Wiese B, Wollny A, Wagner M, et al. Risk factors for incident mild cognitive impairment—results from the German Study on Ageing, Cognition and Dementia in Primary Care Patients (AgeCoDe). Acta Psychiatr Scand. 2010;121(4):260–72. 10.1111/j.1600-0447.2009.01481.x [DOI] [PubMed] [Google Scholar]
- 64. Fischer P, Jungwirth S, Zehetmayer S, Weissgram S, Hoenigschnabl S, Gelpi E, et al. Conversion from subtypes of mild cognitive impairment to Alzheimer dementia. Neurology. 2007;68(4):288–91. [DOI] [PubMed] [Google Scholar]
- 65. Roberts RO, Knopman DS, Mielke MM, Cha RH, Pankratz VS, Christianson TJ, et al. Higher risk of progression to dementia in mild cognitive impairment cases who revert to normal. Neurology. 2014;82(4):317–25. 10.1212/WNL.0000000000000055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Teng E, Tingus KD, Lu PH, Cummings JL. Persistence of neuropsychological testing deficits in mild cognitive impairment. Dement Geriatr Cogn Disord. 2009;28(2):168–78. 10.1159/000235732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Nikula S, Jylha M, Bardage C, Deeg DJ, Gindin J, Minicuci N, et al. Are IADLs comparable across countries? Sociodemographic associates of harmonized IADL measures. Aging Clin Exp Res. 2003;15(6):451–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
Data were provided by the contributing studies to COSMIC on the understanding and proviso that the relevant study leaders be contacted for any further use of their data. Author affiliations with the contributing studies are listed in the Acknowledgments, and contact details can be found on the COSMIC website (http://cheba.unsw.edu.au/group/cosmic).