Abstract
Streptococcus pneumoniae (the pneumococcus) continues to account for significant morbidity and mortality worldwide, causing life-threatening diseases such as pneumonia, bacteremia and meningitis, as well as less serious infections such as sinusitis, conjunctivitis and otitis media. Current polysaccharide vaccines are strictly serotype-specific and also drive the emergence of non-vaccine serotype strains. In this study, we used microarray analysis to compare gene expression patterns of either serotype 4 or serotype 6A pneumococci in the nasopharynx and blood of mice, as a model to identify genes involved in invasion of blood in the context of occult bacteremia in humans. In this manner, we identified 26 genes that were significantly up-regulated in the nasopharynx and 36 genes that were significantly up-regulated in the blood that were common to both strains. Gene Ontology classification revealed that transporter and DNA binding (transcription factor) activities constitute the significantly different molecular functional categories for genes up-regulated in the nasopharynx and blood. Targeted mutagenesis of selected genes from both niches and subsequent virulence and pathogenesis studies identified the manganese-dependent superoxide dismutase (SodA) as most likely to be essential for colonization, and the cell wall-associated serine protease (PrtA) as important for invasion of blood. This work extends our previous analyses and suggests that both PrtA and SodA warrant examination in future studies aimed at prevention and/or control of pneumococcal disease.
Introduction
Streptococcus pneumoniae (the pneumococcus) is a formidable human pathogen, responsible for significant morbidity and mortality worldwide. It causes a broad spectrum of diseases ranging from less serious infections such as sinusitis, conjunctivitis and otitis media, to potentially fatal diseases such as pneumonia, bacteraemia and meningitis. The burden of pneumococcal disease is greatest in developing countries, where an estimated 1.1 million children under 5 years of age die each year from pneumonia (approximately 20% of all deaths in this age group), of which S. pneumoniae is the single commonest cause [1]. The continuing problem of pneumococcal disease is partly attributable to the rate at which this organism is acquiring resistance to multiple antimicrobials and the rapid global spread of highly resistant clones [2]. The problem is being exacerbated by the major shortcomings associated with the current capsular polysaccharide-based vaccines, including cost, strictly serotype-specific protection, incomplete serotype coverage, and replacement carriage and disease caused by non-vaccine serotypes [3].
Concerted global efforts are focused on accelerating the development of alternative pneumococcal vaccine strategies that address the shortcomings of existing approaches, without compromising efficacy. One such approach involves a detailed assessment of pneumococcal proteins that contribute to pathogenesis and are common to all serotypes, their development as vaccine antigens, and an understanding of the mechanism whereby protection might be elicited. The virulence proteins which have received the greatest attention and shown consistent promise as vaccine candidates to date include the thiol-activated toxin pneumolysin (Ply), two choline-binding surface proteins called pneumococcal surface protein A (PspA) and choline-binding protein A (CbpA) (also referred to as PspC or SpsA), iron uptake protein PiuA and various combinations thereof [4–11].
Additional candidate proteins have been identified and appraised for inclusion in multi-component pneumococcal protein vaccine formulations. These include autolysin (LytA) [12], heat-shock protein ClpP [13], neuraminidase A (NanA) [14, 15], pili (RrgA, RrgB, RrgC) [16], the polyhistidine triad (Pht) proteins (particularly PhtD) [6, 17–19], PotD [20], StkP and PcsB [21]. Experimental multivalent protein vaccines are currently being optimized to obtain the best formulation that could confer sufficiently synergistic protection against a wider variety of S. pneumoniae strains to warrant clinical development as an alternative to existing conjugate vaccines. As part of these activities, we carried out systematic microarray comparisons of gene expression kinetics of two pneumococcal strains (WCH16 [serotype 6A] and WCH43 [serotype 4]) in the nasopharynx, lungs, blood and brain of mice. The analyses yielded a number of niche-specific, up-regulated genes that contribute to pathogenesis, some of which were shown to encode good vaccine candidates [22, 23]. However, direct comparisons of gene expression profiles of these pneumococci between the nasopharynx and blood is yet to be reported, although in early childhood, this direct transition to blood is a complication of pneumococcal carriage [24]. We hypothesized that pneumococcal genes that are consistently up-regulated in the blood relative to nasopharynx are likely to be important for survival and/or virulence, while those that are consistently up-regulated in the nasopharynx relative blood are likely to be genes that are important for colonization. In order to test this hypothesis, we carried out comparison of pneumococcal gene expression patterns between the nasopharynx and blood using existing transcriptomic data derived from the two S. pneumoniae strains after intranasal challenge of mice.
Materials and Methods
Ethics Statement
Outbred 5- to 6-week-old sex-matched CD1 (Swiss) mice, obtained from the Laboratory Animal Services breeding facility of the University of Adelaide, were used in all experiments. The Animal Ethics Committee of The University of Adelaide approved all animal experiments (approval numbers S-2010-001 and S-2013-053). The study was conducted in compliance with the Australian Code of Practice for the Care and Use of Animals for Scientific Purposes (7th Edition 2004) and the South Australian Animal Welfare Act 1985.
Bacterial strains and growth conditions
The pneumococcal strains used in this study are serotype 4 (WCH43), serotype 6A (WCH16), and their otherwise isogenic mutant derivatives (Table 1). Serotype-specific capsule production was confirmed by Quellung reaction, as described previously [25]. Opaque-phase variants of the three strains, selected on Todd-Hewitt broth supplemented with 1% yeast extract (THY)-catalase plates [26], were used in all animal experiments. Before infection, the bacteria were grown statically at 37°C in serum broth (10% heat-inactivated horse serum in nutrient broth) to A 600 of 0.16 (equivalent to approx. 5 × 107 CFU/ml).
Table 1. S. pneumoniae strains and primers used in this study.
| Strain/Primer | Description (Sequence type) | Source/Reference |
|---|---|---|
| WCH16 | Capsular serotype 6A clinical isolate (4966) | Women’s and Children’s Hospital, North Adelaide, Australia |
| WCH43 | Capsular serotype 4 clinical isolate (205) | Women’s and Children’s Hospital, North Adelaide, Australia |
| WCH16::ΔprtA | prtA deletion mutant of WCH16 [EryR] | Present study |
| WCH16::ΔsodA | sodA deletion mutant of WCH16 [EryR] | Present study |
| WCH16::ΔvanZ | vanZ deletion mutant of WCH16 [SpecR] | Present study |
| WCH43::ΔprtA | prtA deletion mutant of WCH43 [EryR] | Present study |
| WCH43::ΔsodA | sodA deletion mutant of WCH43 [EryR] | Present study |
| WCH43::ΔulaA | ulaA deletion mutant of WCH43 [SpecR] | Present study |
| WCH43::ΔvanZ | vanZ deletion mutant of WCH43 [SpecR] | Present study |
| prtA Ery X | 5’-TTGTTCATGTAATCACTCCTTCTATTTATATAACTTCCAATAGATA-3’ | |
| prtA Ery Y | 5’-CGGGAGGAAATAATTCTATGAGTATAGAAAAAAATGGTTTATGTACTGA-3’ | |
| prtA Flank F | 5’-GAATGCATCTGATTTTTATCAGAC-3’ | |
| prtA Flank R | 5’-TCTAAAACCTCTTTGTTTACGAGAG-3’ | |
| prtA UpSeq | 5’-GAGCTTGGTTCCAAGTGGTTGATT-3’ | |
| sodA Ery X | 5’-TTGTTCATGTAATCACTCCTTCTTTCTTTCTATATGAAAATGATAACGC-3’ | |
| sodA Ery Y | 5’-CGGGAGGAAATAATTCTATGAGGAGGGAAGAATTGTTCTTCTCTTTTTAG-3’ | |
| sodA Flank F | 5’-CTTTGCGGATGAGAAAATCGTGAT-3’ | |
| sodA Flank R | 5’-GACAGATAAACCATAGTGTTGACGC-3’ | |
| sodA UpSeq | 5’-GCCAATGTTCACGCCTTTTATCAAC-3’ | |
| ulaA Spec X | 5’-TATGTATTCATATATATCCTCCTCTTGAATTGTTTTTGTAAGTTTATTATATA-3’ | |
| ulaA Spec Y | 5’-AAATAACAGATTGAAGAAGGTATAATATCTAGAAAAGGAGAAATAAAATGGTT-3’ | |
| ulaA Flank F | 5’-GCTATTAAAAAAATAGAGGAAGAAGGT-3’ | |
| ulaA Flank R | 5’-GCTGGATCCACAGCCTCTGTAATTC-3’ | |
| ulaA UpSeq | 5’-TCTTTGCAGTTTATGCGCCAGGTG-3’ | |
| vanZ Spec X | 5’-TATGTATTCATATATATCCTCCTCGTTTGAAGCCGTCTTCAACAAACA-3’ | |
| vanZ Spec Y | 5’-AAATAACAGATTGAAGAAGGTATAACTAATGATTAAAAAGGAGAATATAATG-3’ | |
| vanZ Flank F | 5’-CTTAAGGAAGTTCTACTTGAGCCG-3’ | |
| vanZ Flank R | 5’-GAAAACGCCGTGCATCTTCTCAGC-3’ | |
| vanZ UpSeq | 5’-CAAGACTGGGGTTAAAGAACCCGT-3’ |
Intranasal challenge of mice and extraction of total pneumococcal RNA
The protocols used for mouse challenge and analysis of in vivo gene expression by WCH16 and WCH43 have been described in detail previously [22, 23]. Briefly, groups of female mice were challenged intranasally (i.n.) with either WCH16 or WCH43 under anaesthesia. For the current study, RNA was extracted from pneumococci harvested from the nasopharynx and blood of at least 12 mice at each of 48, 72 and 96 h post-challenge using acid-phenol–chloroform–isoamyl alcohol (125:24:1; pH 4.5; Ambion) and purified using RNeasy minikit (Qiagen). The experiment was performed three times for each strain.
Transcriptomic analyses
Microarray experiments were performed on whole genome S. pneumoniae PCR arrays obtained from the Bacterial Microarray Group at St George's Hospital Medical School, London (http://bugs.sghms.ac.uk/). The array was designed using TIGR4 base strain annotation [27] and extra target genes from strain R6 [28]. The array design is available in BμG@Sbase (Accession No. A-BUGS-14; http://bugs.sgul.ac.uk/A-BUGS-14) and also GEO (Platform GPL4001). Pair-wise comparisons were made between the nasopharynx and blood RNA samples from the 48, 72 and 96 h time points. RNA samples were reverse-transcribed using Superscript III (Invitrogen), labeled with either Alexa Fluor 546 or Alexa Fluor 647 dye using the 3DNA Array 900 MPX labeling kit (Genisphere) and then hybridized to the surface of the microarray, essentially as described [29, 30]. Slides were scanned at 10 μm resolution using a Genepix 4000B Scanner (Molecular Devices, USA) and spots were analyzed using the Spot plugin (CSIRO, Australia) within the R statistical software package (http://www.R-project.org). The Limma plugin for R [31] was used for data processing and statistical analysis and ratio values were normalized using the print-tip Loess normalization routine [32]. The replicate arrays were normalized to each other to give similar ranges of mRNA expression values. These statistics were used to rank the mRNAs from those most likely to be differentially expressed to the least likely using false-discovery rate values of p< 0.05. A two-sample Bayesian t-test was also used to analyze the transcriptomic data [33] using FlexArray software (McGill University, Canada), and values with a p = 0.05 were considered to be statistically significant. In this manner, microarray analysis examining RNA from infected nasopharynx vs blood was performed on at least 9 independent hybridizations for each strain, including at least one dye reversal per comparison.
Gene Ontology (GO) classification and GO-based network construction
To gain a detailed view and a better understanding of the functions of the differentially regulated pneumococcal genes in the nasopharynx and blood, we carried out gene ontology (GO) classification and network analysis of the genes using our recently developed comparative GO web application [34]. Particular attention was paid to “molecular function” and “biological process” GO categories. Data from GO protein distributions were analyzed by two-sample Kolmogorov–Smirnov (K–S) and Goodness-of-Fit (Chi-square) tests [35]. We also utilized the information from the GO analysis for selection of genes subjected to mutation.
Construction of mutants and assessment of bacterial growth in vitro
Defined, non-polar mutants of selected genes of interest were constructed in strains WCH16 and WCH43. Selection criteria included known or putative contribution to pneumococcal metabolism, pathogenesis and virulence. Mutants were constructed by overlap extension PCR as described previously [36] and validated by PCR and sequencing to be in-frame deletion mutation replacements. All PCR procedures were performed with the Phusion High Fidelity Kit (FINNZYMES). The primer pairs used for construction and validation of the mutants are listed in Table 1. In order to evaluate the growth rate of the mutants in comparison to the wild type, bacterial strains were grown in serum broth (SB) and A 600 monitored overnight on a Spectramax M2 spectrophotometer (Millennium Science).
Virulence assessment of mutants
To assess the virulence potential of mutants, groups of 12 male mice were challenged i.n. with approx 1 × 107 CFU of either mutant or wild type bacteria in 50 μl SB, under deep anesthesia. The survival of mice (time to moribund) was monitored closely (four times daily for the first 5 days (and more frequently if they show signs of distress as outlined below), twice daily for the next 5 days, and then daily until 14 days after challenge. During the monitoring period, the condition of each mouse was measured based on a predetermined Clinical Record Score and written on a Clinical Record Sheet approved by the Animal Ethics Committee of The University of Adelaide. Mice are humanely euthanized either by CO2 asphyxiation or by cervical dislocation if they become moribund or show any evidence of distress. The following criteria were considered sufficient evidence of distress to warrant such intervention in order to minimize pain or suffering to the animals: loss of balance, extreme hyperactivity or other evidence of meningitis or CNS involvement; severe weight loss (>20% body weight); ear temperature falling below 24°C; paralysis or extreme reluctance or inability to move freely, and/or refusal or inability to eat or drink. Differences in survival times for mice between wild-type and mutants were analyzed by the Kaplan-Meier survival (log-rank [Mantel-Cox] and Gehan-Breslow-Wilcoxon) tests using GraphPad Prism v6 software.
Pathogenesis experiments
For pathogenesis experiments, S. pneumoniae derivatives with mutations in genes of interest (ΔprtA, ΔsodA and ΔvanZ) and the isogenic wild-type strain (WCH16 or WCH43) were grown separately in SB to A 600 = 0.16 (approx. 5 × 107 CFU/ml). For this analysis, groups of 6 mice were anesthetized by intraperitoneal injection of pentobarbital sodium (Nembutal; Ilium) at a dose of 66 mg per g of body weight and separately challenged i.n. with 50 μl suspension containing approx. 3 × 106 CFU of either wild-type or the isogenic mutant. At 48 h post-challenge, mice from each separate infection experiment were sacrificed and bacteria were enumerated from the nasopharynx, lungs and blood, as described previously [22, 23]. The experiment was repeated once.
Results
In this work, we carried out a direct comparison of pneumococcal gene expression between the nasopharynx and blood of mice in order to identify differentially expressed genes between the two niches. The analyses were performed using existing transcriptomic data obtained from two S. pneumoniae strains, WCH16 and WCH43, after intranasal challenge of mice.
Identification of differentially expressed genes between the nasopharynx and blood
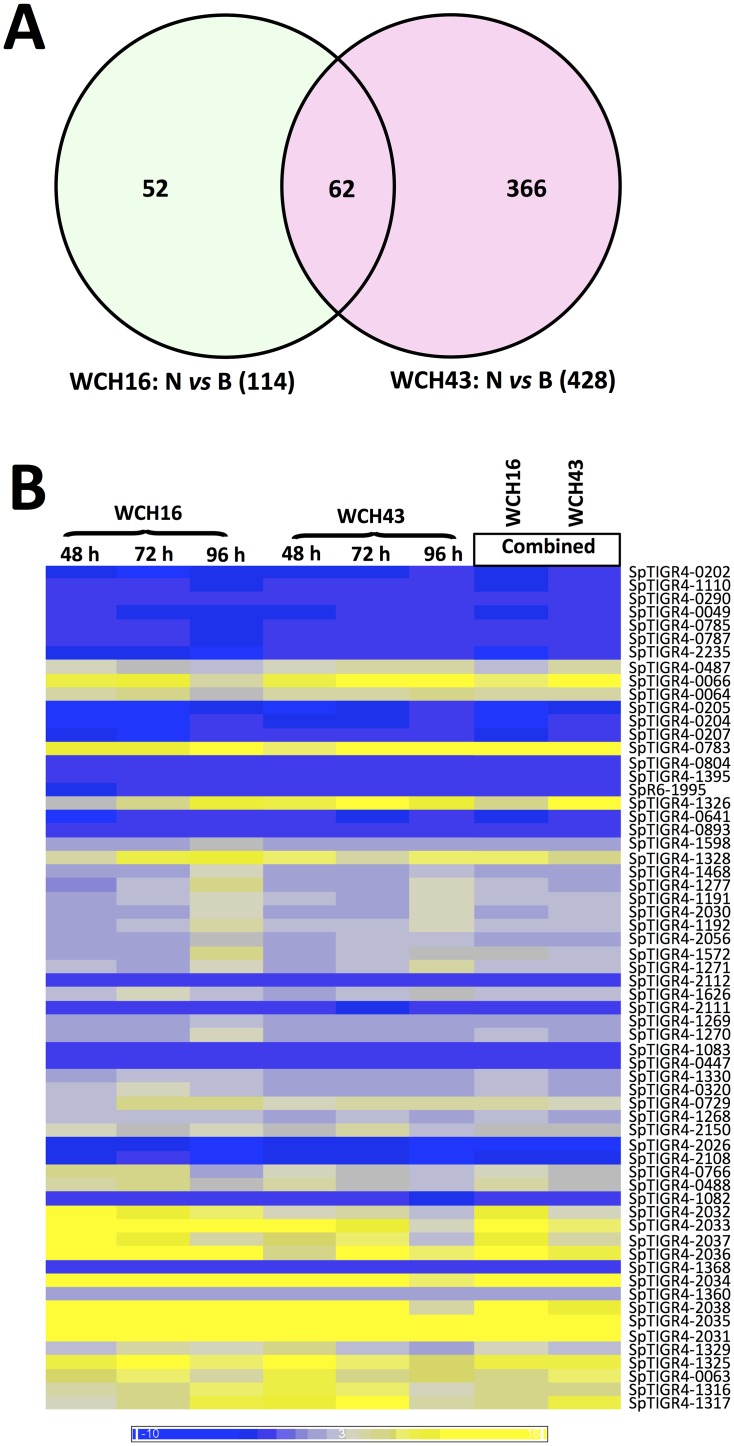
We carried out a two-color microarray comparison of mRNA extracted from pneumococci harvested from the nasopharnyx and blood of mice at 48, 72 and 96 h post-infection in separate challenge experiments with either WCH16 or WCH43. The comparisons yielded 114 differentially regulated genes in the blood relative to the nasopharynx for WCH16, and 428 genes differentially regulated in the blood for WCH43, of which 62 differentially expressed genes were found to be common to both strains (Fig 1A and 1B). Details of combined expression values for all the 62 genes are in S1 Table. Fully annotated microarray data have been deposited (GEO accession number GSE73217).
Fig 1. Regulation of pneumococcal gene expression between nasopharynx and blood of mice infected i.n. with WCH16 and WCH43.
(A). Venn diagram of differentially expressed genes from microarray comparisons of Nasopharynx (N) versus Blood (B) in WCH16 and WCH43. (B). Heat map showing regulated gene expression; yellow to blue scales represent fold difference in mRNA level; yellow, up-regulation in nasopharynx relative to blood; blue, downregulation in nasopharynx relative to blood.
Functional classification of differentially expressed genes
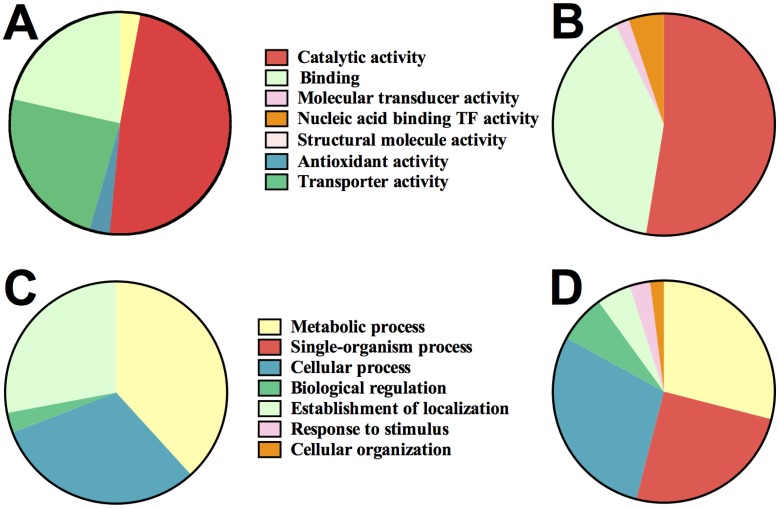
We utilized our recently developed comparative GO web application [34] to assess any differences in the functional categories of genes up-regulated either in the nasopharynx or blood, with particular attention to molecular function and biological process. The analyses showed that under “molecular function”, the GO protein distributions between the nasopharynx and blood were significantly different (p = 0.0008; two-sample K-S test). GO groups involved in transporter activity were significantly up-regulated in the nasopharynx relative to blood [p = 0.01; Chi square test], while those involved in transcription factor (DNA binding) activity were substantially up-regulated in the blood (Fig 2A and 2B). Similarly, under “biological process”, the GO protein distributions between the two niches were significantly different [p = 0.0043; two-sample K-S test] (Fig 2C and 2D), although this did not reach statistical significance for any of the GO groups identified between the two niches by Chi square test.
Fig 2. GO classification of pneumococcal genes differentially up-regulated in the nasopharynx and blood of mice.
Molecular functional categories of genes (A), up-regulated in the nasopharynx, and (B), up-regulated in the blood. (C and D), Biological process categories of up-regulated genes in the nasopharynx (C), and up-regulated genes in the blood (D).
Contribution of up-regulated pneumococcal genes to colonization and virulence
Earlier studies had shown that the pneumococcus undergoes spontaneous phase variation between a transparent and an opaque colony phenotype in vitro, with the transparent phenotype commonly associated with nasopharyngeal colonization and the opaque variant being favored in the blood [26, 37]. These findings led to the suggestion that phase variation might provide important clues to the interaction of the pneumococcus with its host, the opaque phenotype being significantly more virulent than the transparent phenotype [26, 38]. Interestingly, subsequent work in our laboratory indicated that niche-specific differences in expression of selected pneumococcal virulence genes were not attributable to phase variation. In order to eliminate the contribution of phase variation to selection of genes for further analysis, we initially compared gene expression of transparent pneumococci with those harvested from the nasopharynx, and also compared gene expression of opaque pneumococci with those harvested from the blood. We reasoned that such analyses would identify genes that are most likely to be essential for either colonization, or important for blood invasion or systemic disease. We also examined our existing in vivo transcriptomic comparisons of nasopharynx vs lungs, as well as data from lungs vs blood comparisons to guide our gene selection. In this manner, only pneumococcal genes that were either up-regulated in the nasopharynx or blood were selected for further analyses, independent of colony phenotype.
We then set an arbitrary threshold of >2-fold regulation to select differentially regulated genes in the two niches that are considered to be physiologically relevant. Consequently, 2 of the up-regulated genes in the nasopharynx (SP_0766 [sodA] and SP_2038 [ulaA]) and 2 genes up-regulated in the blood (SP_0049 [vanZ] and SP_0641 [prtA]) were selected for further analysis and validated by RT-PCR for both strains (Table 2). S. pneumoniae WCH43 derivatives with marked mutations in the 4 selected genes were constructed by targeted mutagenesis using overlap PCR. The in vitro growth rate of WCH16 and all its isogenic mutants was similar over a 3-hour period as well as overnight as judged by A 600 measurements in serum broth on a Spectramax M2 spectrophotometer (Millennium Science). For WCH43, growth of the sodA mutant was slightly delayed (approx. 20 minutes) over the 3-hour growth period, as well as during overnight growth. Nevertheless, this delay in growth of the sodA mutant of WCH43 would not account for its attenuation in mice, as similar result were obtained for the sodA mutant of WCH16, as described below.
Table 2. Differential expression profiles of selected S. pneumoniae WCH16 and WCH43 genes between Nasopharynx and Blood by microarray analysis.
| Gene ID a | Gene annotation | Fold change (Nasopharynx/Blood) | |
|---|---|---|---|
| WCH16 | WCH43 | ||
| SP_0049 | VanZ protein, putative | -2.61 (-59.03) b | -2.02 (-13.78) |
| SP_0641 | Serine protease (PrtA) | -2.45 (-34.80) | -2.25 (-6.82) |
| SP_0766 | Superoxide dismutase, manganese-dependent (SodA) | 4.16 (7.15) | 3.32 (3.39) |
| SP_2038 | PTS system ascorbate-specific transporter subunit IIC (UlaA) | 15.48 (22.94) | 9.66 (278.20) |
a Gene IDs were obtained from the genome of S. pneumoniae TIGR4 (serotype 4) as deposited in the Kyoto Encyclopedia of Genes and Genomes (KEGG) database.
b Data in parentheses represent corresponding real time RT-PCR expression values from comparisons of total mRNA from at least 2 independent experiments.
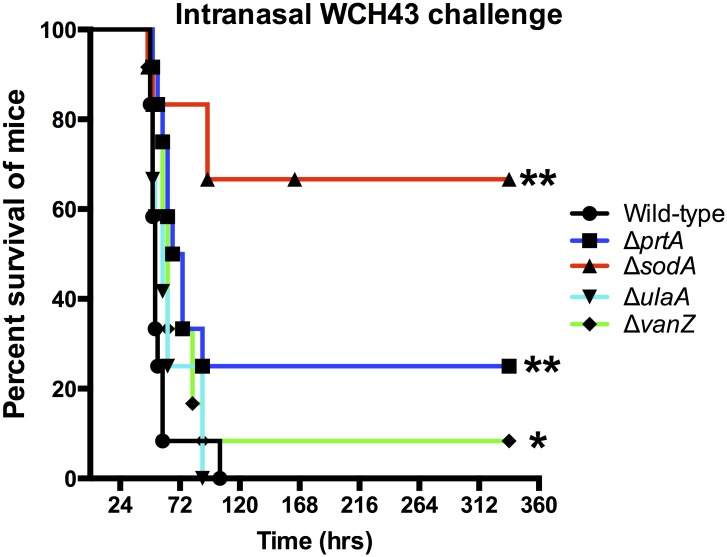
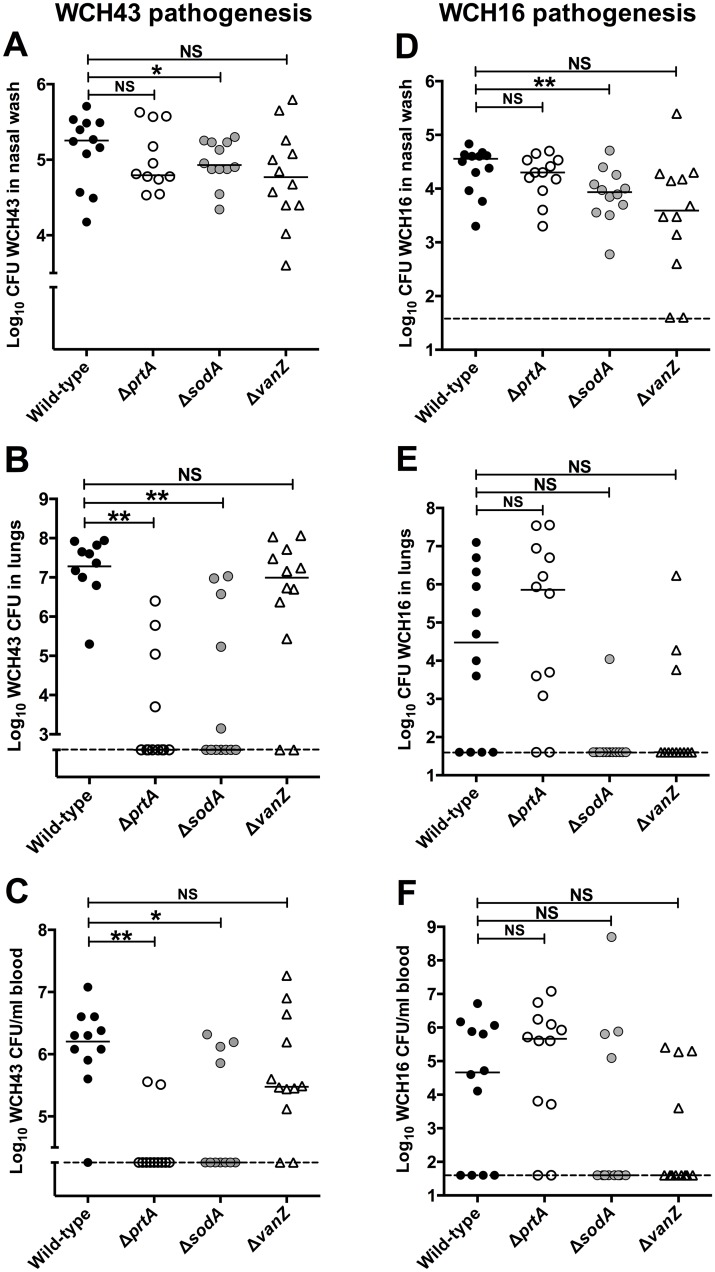
After intranasal challenge of mice, the ΔprtA, ΔsodA mutants and, to a lesser extent, the ΔvanZ mutant of WCH43 were significantly attenuated for virulence, while the ΔulaA mutant was essentially as virulent as the wild type (Fig 3). To assess the involvement of prtA, sodA and vanZ in colonization or blood invasion, we challenged groups of mice i.n. with approx. 3 × 106 CFU of either mutant or the isogenic wild-type WCH16 or WCH43 strain and harvested bacteria from the nasopharynx, lungs and blood at 48 h post-infection. For WCH43, we found that only the ΔsodA mutant was significantly attenuated for colonization of the nasopharynx (Fig 4A), while the numbers of ΔprtA and ΔsodA mutants were significantly lower in lungs (Fig 4B) and blood (Fig 4C) compared to wild type. However, while the numbers of the ΔvanZ mutant bacteria were generally lower in blood than those for the wild type, this did not reach statistical significance. To verify these results, we repeated the pathogenesis experiment using WCH16 and its isogenic ΔprtA, ΔsodA and ΔvanZ mutants. As observed for WCH43, the ΔsodA mutant was also significantly attenuated for colonization of the nasopharynx (Fig 4D), However, the differences in pathogenesis of the mutants in WCH16 in lungs (Fig 4E) and blood (Fig 4F) did not reach statistical significance, consistent with our previous observations that WCH16 displays minimal lung and blood involvement during pathogenesis [39, 40].
Fig 3. Survival times for mice after i.n. challenge with WCH43 and isogenic mutant derivatives.
Groups of 12 CD1 male mice were challenged i.n. with approx. 1 × 107 CFU of the indicated strains. Survival curves were compared using log-rank [Mantel-Cox] and Gehan-Breslow-Wilcoxon) tests. (* P<0.05; ** P<0.01).
Fig 4. Pathogenesis of WCH43 (A-C) and WCH16 (D-F) and their isogenic mutant derivatives in male CD1 mice.
Bacteria were enumerated from the nasopharynx (A, D); lungs (B, E) and blood (C, F) of each mouse at 48 h post-infection (n = 12 per group per time-point). Horizontal line represents geometric mean; horizontal broken line denote limit of detection (40 CFU). *, P < 0.05; ** P<0.01; unpaired t-test, one-tailed.
Discussion
In spite of the availability of antimicrobial therapy and conjugate vaccines, S. pneumoniae continues to be responsible for massive global morbidity and mortality. The problems associated with pneumococcal disease are largely due to our incomplete understanding of the molecular mechanisms underlying pneumococcal pathogenesis. Therefore, successful control of pneumococcal disease and identification of novel vaccine candidates will require a detailed understanding of the molecular mechanisms and virulence determinants underpinning the development of invasive pneumococcal disease (IPD). Such investigations will include a thorough examination of factors up-regulated during transition from nasopharyngeal colonization to invasive or meningeal infection, in conjunction with developing an understanding of the regulatory mechanisms underpinning such translocation.
As an extension of our efforts toward identifying the critical determinants of pathogenesis, we have used microarray analysis to do a direct comparison of pneumococcal gene expression between the nasopharynx and blood of mice. This assessment was undertaken in order to identify the genes specifically up-regulated during blood invasion from the nasopharynx (“occult bacteremia”), which is often a complication of pneumococcal carriage in young children [24, 41]. This is critical in the context of optimization of a multi-component protein vaccine that targets all forms of pneumococcal disease, considering the hypothesis that many pneumococcal virulence factors have dual roles in the maintenance of carriage and invasive disease [38, 42, 43].
Our analysis identified a number of common factors significantly up-regulated in the nasopharynx relative to blood in the two pneumococcal strains; not surprisingly, the vast majority of the encoded proteins function in carbohydrate metabolism and/or transporter activity. Mutation of one of the two genes up-regulated in the nasopharynx, sodA, resulted in significant attenuation of virulence in a mouse intranasal challenge model, in agreement with previous reports [42, 44]. In a pathogenesis experiment, there was significant reduction in numbers of sodA mutant bacteria recovered from the nasopharynx and a concomitant significant reduction in the lungs and blood at 48 hr post-challenge. These results are consistent with a significant role for SodA in oxidative stress management [44, 45], suggesting it might be a good a drug target against carriage. However, deletion of ulaA (with a putative function of the encoded product in transporter activity) did not have any effect on virulence, suggesting functional redundancy.
We also analyzed the genes that were significantly up-regulated in the blood relative to nasopharynx in the two pneumococcal strains. Most of the genes encode enzymes involved in metabolism of cofactors, vitamins and amino acids, as well as those required for transcriptional regulation of metabolites. This would be consistent with the need to up-regulate such factors for sensing and adaptation to challenging environments such as the blood. For some of these factors, their role in pneumococcal virulence is well documented. For instance, CbpA (SpR_1995/SP_2190) has been shown to be involved in multiple stages of pneumococcal pathogenesis [43, 46–48]. Another protein, MalX (SP_2108), was shown to be important for colonization [49] and lung infection [42, 44]. Like CbpA, the finding in this study that malX is significantly up-regulated in the blood relative to the nasopharynx suggests that it might also be involved in multiple stages of pathogenesis, which would make it an ideal protein vaccine candidate.
We then mutated 2 of the genes, prtA and vanZ, encoding a cell wall-localized subtilisin-like serine protease (PrtA) and a putative vancomycin resistant protein (VanZ), respectively. The prtA mutant was significantly attenuated in a mouse intranasal challenge model in the WCH43 background; the vanZ mutant also exhibited a small, but statistically significant attenuation. The attenuation of the prtA mutant is in agreement with a previous report [50], although in that study, the challenge was via an intraperitoneal route, using a different pneumococcal strain, D39 [50]. Interestingly, in our study, pathogenesis studies show significantly low numbers of WCH43 prtA mutant bacteria in the bloodstream of intranasally-challenged mice relative to wild-type bacteria, which would be consistent with its attenuated virulence, but in contrast to the earlier study which showed more prtA mutant bacteria in the blood of intraperitoneally challenged mice [50]. Another recent study showed modest effects of a D39ΔprtA mutation in lungs and blood of intranasally-infected mice [51]. A possible explanation for the apparent contradiction in these results could be that expression of PrtA is more important for pathogenesis and virulence of WCH43, while this effect is masked by other virulence factors produced by D39 (which displays high grade bacteremia), suggesting strain-specific differences. This is further highlighted by our pathogenesis results with WCH16 prtA mutant. Moreover, the different routes of infection and challenge doses used in these studies could also account for the discordant results. The discrepancy in attenuation of virulence of a specific factor in different pneumococcal backgrounds is not unprecedented, as was reported for cbpA - [pspC -] [25, 43, 47, 52, 53] and psaR [54] mutants. With respect to VanZ, its specific role in pneumococcal pathogenesis is yet to be described, although it was found to be essential for lung infection [42] and its homolog has been shown to confer resistance to teicoplanin in Enterococcus faecium [55].
It is as yet unclear how PrtA contributes to the virulence of S. pneumoniae. It was shown previously that PrtA acts by cleaving apolactoferrin (the iron-free form of human lactoferrin) to produce a lactoferricin-like peptide, which is highly bactericidal for pneumococci [56]. This would suggest that expressing PrtA might be counter-productive, because anti-PrtA antibodies could inhibit killing of the pneumococcus. Nevertheless, strongly reactive anti-PrtA antibody was prominent in convalescent-phase human sera [50, 57, 58], and a prtA mutant was attenuated for virulence as demonstrated in the present study. Therefore, more work, both in vitro and in vivo, is needed to clarify the role of PrtA in the biology of S. pneumoniae, and to determine whether it is worthy of further consideration as a vaccine candidate.
Other workers have compared transcriptomes of pneumococci harvested from various in vitro and in vivo sources by microarray analysis or RNA-Seq. For example, one previous study [59] used in vitro alternatives for specific in vivo niches (e.g. co-culture with Detroit 562 cells to mimic nasopharyngeal colonization; co-culture with type II pneumocytes to mimic lung infection). The workers further compared whole transcriptomes of a particular pneumococcal strain (TIGR4) harvested in vitro (to mimic colonization) with whole transcriptomes of a different pneumococcal strain (D39) harvested from mouse blood (to mimic invasive disease). Recently, another group of workers [60] characterized pneumococcal RNA harvested from a human respiratory epithelial cell line (to mimic lung infection), using S. pneumoniae EF3030, which causes focal pneumonia in their infection experiments. Furthermore, Pettigrew et al. compared transcriptional profiles of planktonic and biofilm-grown EF3030 with influenza A virus-dispersed bacteria. Genes that have been well characterized to play a prominent role in pneumococcal pathogenesis and/or virulence (such as ply, pspA, cbpA, malX) were commonly identified in those previous studies and in our study. Nevertheless, we are of the view that our mouse intranasal infection model closely mimics natural progression of invasive pneumococcal disease in humans; the use of multiple strains of different pathogenicity characteristics also increases the likelihood of identifying common, novel genes that might be critical to pneumococcal pathogenesis.
Supporting Information
(DOCX)
Acknowledgments
JCP is a NHMRC Senior Principal Research Fellow.
Data Availability
Fully annotated microarray data have been deposited in GEO (accession number GSE73217 [http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE73217]).
Funding Statement
This work was supported by Meningitis Research Foundation (GB; www.meningitis.org) Research Grant 0802.0 to ADO, JCP and LKM, as well as by National Health and Medical Research Council of Australia (NHMRC; http://www.nhmrc.gov.au) Program Grant 565526 to JCP, a Senior Principal Research Fellow, and Project Grant 627142 to JCP and ADO. The authors acknowledge BμG@S (the Bacterial Microarray Group at St George’s, University of London; www.bugs.sgul.ac.uk) for supply of the microarray slides and advice and The Wellcome Trust for funding the multi-collaborative microbial pathogen microarray facility under its Functional Genomics Resources Initiative. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization Media Centre; Pneumonia: Fact sheet No 331. 2013.
- 2. World Health Organization; Antimicrobial resistance: global report on surveillance. 2014. [Google Scholar]
- 3. Brueggemann AB, Pai R, Crook DW, Beall B. Vaccine escape recombinants emerge after pneumococcal vaccination in the United States. PLoS Pathog. 2007. November;3(11):e168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Briles DE, Hollingshead SK, Paton JC, Ades EW, Novak L, van Ginkel FW, et al. Immunizations with pneumococcal surface protein A and pneumolysin are protective against pneumonia in a murine model of pulmonary infection with Streptococcus pneumoniae . J Infect Dis. 2003. August 1;188(3):339–48. [DOI] [PubMed] [Google Scholar]
- 5. Ogunniyi AD, Folland RL, Briles DE, Hollingshead SK, Paton JC. Immunization of mice with combinations of pneumococcal virulence proteins elicits enhanced protection against challenge with Streptococcus pneumoniae . Infect Immun. 2000. May;68(5):3028–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ogunniyi AD, Grabowicz M, Briles DE, Cook J, Paton JC. Development of a vaccine against invasive pneumococcal disease based on combinations of virulence proteins of Streptococcus pneumoniae . Infect Immun. 2007. January;75(1):350–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brown JS, Ogunniyi AD, Woodrow MC, Holden DW, Paton JC. Immunization with components of two iron uptake ABC transporters protects mice against systemic Streptococcus pneumoniae infection. Infect Immun. 2001. November;69(11):6702–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hammerschmidt S, Talay SR, Brandtzaeg P, Chhatwal GS. SpsA, a novel pneumococcal surface protein with specific binding to secretory immunoglobulin A and secretory component. Molecular Microbiology. 1997. September;25(6):1113–24. [DOI] [PubMed] [Google Scholar]
- 9. Paton JC, Lock RA, Hansman DJ. Effect of immunization with pneumolysin on survival time of mice challenged with Streptococcus pneumoniae . Infect Immun. 1983. May;40(2):548–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rosenow C, Ryan P, Weiser JN, Johnson S, Fontan P, Ortqvist A, et al. Contribution of novel choline-binding proteins to adherence, colonization and immunogenicity of Streptococcus pneumoniae . Mol Microbiol. 1997. September;25(5):819–29. [DOI] [PubMed] [Google Scholar]
- 11. Paton JC. New pneumococcal vaccines: basic science developments, p. 382–402. In: Tuomanen EI, Mitchell TJ, Morrison DA, Spratt BG (ed), The Pneumococcus. 2004;ASM Press, Washington DC. [Google Scholar]
- 12. Lock RA, Hansman D, Paton JC. Comparative efficacy of autolysin and pneumolysin as immunogens protecting mice against infection by Streptococcus pneumoniae . Microb Pathog. 1992. February;12(2):137–43. [DOI] [PubMed] [Google Scholar]
- 13. Kwon HY, Ogunniyi AD, Choi MH, Pyo SN, Rhee DK, Paton JC. The ClpP protease of Streptococcus pneumoniae modulates virulence gene expression and protects against fatal pneumococcal challenge. Infection and Immunity. 2004. October;72(10):5646–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lock RA, Paton JC, Hansman D. Comparative efficacy of pneumococcal neuraminidase and pneumolysin as immunogens protective against Streptococcus pneumoniae . Microb Pathog. 1988. December;5(6):461–7. [DOI] [PubMed] [Google Scholar]
- 15. Tong HH, Li D, Chen S, Long JP, DeMaria TF. Immunization with recombinant Streptococcus pneumoniae neuraminidase NanA protects chinchillas against nasopharyngeal colonization. Infect Immun. 2005. November;73(11):7775–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moschioni M, De Angelis G, Harfouche C, Bizzarri E, Filippini S, Mori E, et al. Immunization with the RrgB321 fusion protein protects mice against both high and low pilus-expressing Streptococcus pneumoniae populations. Vaccine. 2012. February 8;30(7):1349–56. 10.1016/j.vaccine.2011.12.080 [DOI] [PubMed] [Google Scholar]
- 17. Adamou JE, Heinrichs JH, Erwin AL, Walsh W, Gayle T, Dormitzer M, et al. Identification and characterization of a novel family of pneumococcal proteins that are protective against sepsis. Infect Immun. 2001. February;69(2):949–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hamel J, Charland N, Pineau I, Ouellet C, Rioux S, Martin D, et al. Prevention of pneumococcal disease in mice immunized with conserved surface-accessible proteins. Infect Immun. 2004. May;72(5):2659–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Plumptre CD, Ogunniyi AD, Paton JC. Vaccination against Streptococcus pneumoniae using truncated derivatives of polyhistidine triad protein D. PLoS One. 2013. October 31;8(10):e78916 10.1371/journal.pone.0078916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shah P, Swiatlo E. Immunization with polyamine transport protein PotD protects mice against systemic infection with Streptococcus pneumoniae . Infect Immun. 2006. October;74(10):5888–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Giefing C, Meinke AL, Hanner M, Henics T, Bui MD, Gelbmann D, et al. Discovery of a novel class of highly conserved vaccine antigens using genomic scale antigenic fingerprinting of pneumococcus with human antibodies. J Exp Med. 2008. January 21;205(1):117–31. 10.1084/jem.20071168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mahdi LK, Wang H, Van der Hoek MB, Paton JC, Ogunniyi AD. Identification of a novel pneumococcal vaccine antigen preferentially expressed during meningitis in mice. J Clin Invest. 2012. June 1;122(6):2208–20. 10.1172/JCI45850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ogunniyi AD, Mahdi LK, Trappetti C, Verhoeven N, Mermans D, Van der Hoek MB, et al. Identification of genes that contribute to the pathogenesis of invasive pneumococcal disease by in vivo transcriptomic analysis. Infect Immun. 2012. September;80(9):3268–78. 10.1128/IAI.00295-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Weiser JN. The pneumococcus: why a commensal misbehaves. J Mol Med (Berl). 2010. February;88(2):97–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Berry AM, Paton JC. Additive attenuation of virulence of Streptococcus pneumoniae by mutation of the genes encoding pneumolysin and other putative pneumococcal virulence proteins. Infect Immun. 2000. January;68(1):133–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Weiser JN, Austrian R, Sreenivasan PK, Masure HR. Phase variation in pneumococcal opacity: relationship between colonial morphology and nasopharyngeal colonization. Infect Immun. 1994. June;62(6):2582–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tettelin H, Nelson KE, Paulsen IT, Eisen JA, Read TD, Peterson S, et al. Complete genome sequence of a virulent isolate of Streptococcus pneumoniae . Science. 2001. July 20;293(5529):498–506. [DOI] [PubMed] [Google Scholar]
- 28. Hoskins J, Alborn WE Jr., Arnold J, Blaszczak LC, Burgett S, DeHoff BS, et al. Genome of the bacterium Streptococcus pneumoniae strain R6. J Bacteriol. 2001. October;183(19):5709–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. McCluskey J, Hinds J, Husain S, Witney A, Mitchell TJ. A two-component system that controls the expression of pneumococcal surface antigen A (PsaA) and regulates virulence and resistance to oxidative stress in Streptococcus pneumoniae . Mol Microbiol. 2004. March;51(6):1661–75. [DOI] [PubMed] [Google Scholar]
- 30. Ogunniyi AD, Mahdi LK, Jennings MP, McEwan AG, McDevitt CA, Van der Hoek MB, et al. Central role of manganese in regulation of stress responses, physiology, and metabolism in Streptococcus pneumoniae . J Bacteriol. 2010. September;192(17):4489–97. 10.1128/JB.00064-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Smyth GK. Limma: linear models for microarray data In: Gentleman R, Carey V, Dudoit S, Irizarry R, Huber W, editors. Bioinformatics and Computational Biology Solutions using R and Bioconductor. New York: Springer; 2005. p. 397–420. [Google Scholar]
- 32. Smyth GK, Speed T. Normalization of cDNA microarray data. Methods. 2003. December;31(4):265–73. [DOI] [PubMed] [Google Scholar]
- 33. Fox RJ, Dimmic MW. A two-sample Bayesian t-test for microarray data. Bmc Bioinformatics. 2006. March 10;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fruzangohar M, Ebrahimie E, Ogunniyi AD, Mahdi LK, Paton JC, Adelson DL. Comparative GO: a web application for comparative gene ontology and gene ontology-based gene selection in bacteria. PLoS One. 2013;8(3):e58759 10.1371/journal.pone.0058759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stephens MA. Edf Statistics for Goodness of Fit and Some Comparisons. J Am Stat Assoc. 1974;69(347):730–7. [Google Scholar]
- 36. Horton RM, Ho SN, Pullen JK, Hunt HD, Cai Z, Pease LR. Gene splicing by overlap extension. Methods Enzymol. 1993;217:270–9. [DOI] [PubMed] [Google Scholar]
- 37. Kim JO, Weiser JN. Association of intrastrain phase variation in quantity of capsular polysaccharide and teichoic acid with the virulence of Streptococcus pneumoniae . J Infect Dis. 1998. February;177(2):368–77. [DOI] [PubMed] [Google Scholar]
- 38. Briles DE, Novak L, Hotomi M, van Ginkel FW, King J. Nasal colonization with Streptococcus pneumoniae includes subpopulations of surface and invasive pneumococci. Infect Immun. 2005. October;73(10):6945–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. LeMessurier KS, Ogunniyi AD, Paton JC. Differential expression of key pneumococcal virulence genes in vivo . Microbiology-SGM. 2006. February;152:305–11. [DOI] [PubMed] [Google Scholar]
- 40. Mahdi LK, Ogunniyi AD, LeMessurier KS, Paton JC. Pneumococcal virulence gene expression and host cytokine profiles during pathogenesis of invasive disease. Infect Immun. 2008. February;76(2):646–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kuppermann N. Occult bacteremia in young febrile children. Pediatr Clin North Am. 1999. December;46(6):1073–109. [DOI] [PubMed] [Google Scholar]
- 42. Hava DL, Camilli A. Large-scale identification of serotype 4 Streptococcus pneumoniae virulence factors. Mol Microbiol. 2002. September;45(5):1389–406. [PMC free article] [PubMed] [Google Scholar]
- 43. Orihuela CJ, Gao G, Francis KP, Yu J, Tuomanen EI. Tissue-specific contributions of pneumococcal virulence factors to pathogenesis. J Infect Dis. 2004. November 1;190(9):1661–9. [DOI] [PubMed] [Google Scholar]
- 44. Yesilkaya H, Kadioglu A, Gingles N, Alexander JE, Mitchell TJ, Andrew PW. Role of manganese-containing superoxide dismutase in oxidative stress and virulence of Streptococcus pneumoniae . Infect Immun. 2000. May;68(5):2819–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Eijkelkamp BA, Morey JR, Ween MP, Ong CL, McEwan AG, Paton JC, et al. Extracellular zinc competitively inhibits manganese uptake and compromises oxidative stress management in Streptococcus pneumoniae . PLoS One. 2014;9(2):e89427 10.1371/journal.pone.0089427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Brooks-Walter A, Briles DE, Hollingshead SK. The pspC gene of Streptococcus pneumoniae encodes a polymorphic protein, PspC, which elicits cross-reactive antibodies to PspA and provides immunity to pneumococcal bacteremia. Infect Immun. 1999. December;67(12):6533–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ogunniyi AD, LeMessurier KS, Graham RMA, Watt JM, Briles DE, Stroeher UH, et al. Contributions of pneumolysin, pneumococcal surface protein A (PspA), and PspC to pathogenicity of Streptococcus pneumoniae D39 in a mouse model. Infect Immun. 2007. April;75(4):1843–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Orihuela CJ, Mahdavi J, Thornton J, Mann B, Wooldridge KG, Abouseada N, et al. Laminin receptor initiates bacterial contact with the blood brain barrier in experimental meningitis models. J Clin Invest. 2009. June;119(6):1638–46. 10.1172/JCI36759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Moffitt KL, Gierahn TM, Lu YJ, Gouveia P, Alderson M, Flechtner JB, et al. T(H)17-based vaccine design for prevention of Streptococcus pneumoniae colonization. Cell Host Microbe. 2011. February 17;9(2):158–65. 10.1016/j.chom.2011.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bethe G, Nau R, Wellmer A, Hakenbeck R, Reinert RR, Heinz HP, et al. The cell wall-associated serine protease PrtA: a highly conserved virulence factor of Streptococcus pneumoniae . FEMS Microbiol Lett. 2001. November 27;205(1):99–104. [DOI] [PubMed] [Google Scholar]
- 51. de Stoppelaar SF, Bootsma HJ, Zomer A, Roelofs JJ, Hermans PW, van 't Veer C, et al. Streptococcus pneumoniae serine protease HtrA, but not SFP or PrtA, is a major virulence factor in pneumonia. PLoS One. 2013;8(11):e80062 10.1371/journal.pone.0080062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Balachandran P, Brooks-Walter A, Virolainen-Julkunen A, Hollingshead SK, Briles DE. Role of pneumococcal surface protein C in nasopharyngeal carriage and pneumonia and its ability to elicit protection against carriage of Streptococcus pneumoniae . Infect Immun. 2002. May;70(5):2526–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Iannelli F, Chiavolini D, Ricci S, Oggioni MR, Pozzi G. Pneumococcal surface protein C contributes to sepsis caused by Streptococcus pneumoniae in mice. Infection and Immunity. 2004. May;72(5):3077–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hendriksen WT, Bootsma HJ, van Diepen A, Estevao S, Kuipers OP, de Groot R, et al. Strain-specific impact of PsaR of Streptococcus pneumoniae on global gene expression and virulence. Microbiology. 2009. May;155(Pt 5):1569–79. 10.1099/mic.0.025072-0 [DOI] [PubMed] [Google Scholar]
- 55. Arthur M, Depardieu F, Molinas C, Reynolds P, Courvalin P. The vanZ gene of Tn1546 from Enterococcus faecium BM4147 confers resistance to teicoplanin. Gene. 1995. February 27;154(1):87–92. [DOI] [PubMed] [Google Scholar]
- 56. Mirza S, Wilson L, Benjamin WH Jr., Novak J, Barnes S, Hollingshead SK, et al. Serine protease PrtA from Streptococcus pneumoniae plays a role in the killing of S. pneumoniae by apolactoferrin. Infect Immun. 2011. June;79(6):2440–50. 10.1128/IAI.00489-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Zysk G, Bethe G, Nau R, Koch D, Grafin Von Bassewitz VC, Heinz HP, et al. Immune response to capsular polysaccharide and surface proteins of Streptococcus pneumoniae in patients with invasive pneumococcal disease. J Infect Dis. 2003. January 15;187(2):330–3. [DOI] [PubMed] [Google Scholar]
- 58. Zysk G, Bongaerts RJ, ten Thoren E, Bethe G, Hakenbeck R, Heinz HP. Detection of 23 immunogenic pneumococcal proteins using convalescent-phase serum. Infect Immun. 2000. June;68(6):3740–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Orihuela CJ, Radin JN, Sublett JE, Gao G, Kaushal D, Tuomanen EI. Microarray analysis of pneumococcal gene expression during invasive disease. Infect. Immun. 2004. October;72(10):5582–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Pettigrew MM, Marks LR, Kong Y, Gent JF, Roche-Hakansson H, Hakansson AP. Dynamic changes in the Streptococcus pneumoniae transcriptome during transition from biofilm formation to invasive disease upon influenza A virus infection. Infect Immun. 2014. November;82(11):4607–19. 10.1128/IAI.02225-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
Fully annotated microarray data have been deposited in GEO (accession number GSE73217 [http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE73217]).