Abstract
Adverse childhood experiences (ACEs) represent substantial threats to public health and affect about 58% of youth in the US. In addition to their acute effects such as injury and physical trauma, ACEs are associated with an increased risk of several negative health outcomes throughout the life course. Emerging evidence suggests sleep disorders may be one such outcome, but existing studies have not been systematically reviewed and summarized. We conducted a systematic review to summarize the evidence concerning the relationship between ACEs and sleep disorders and disturbances, with a focus on adult women. Original publications were identified through searches of the electronic databases MEDLINE, Embase, and Web of Science using key words “childhood,” “adversity,” “abuse,” and “sleep” as well as searches of the reference lists of eligible studies. Studies evaluating ACEs that occurred before 18 years of age and sleep outcomes that were assessed at 18 years or older were adjudicated and included. A total of 30 publications were identified. Of the 30 studies, 28 were retrospective analyses and there was vast heterogeneity in types of ACEs and sleep outcomes measured. The majority of retrospective studies (N=25 of 28) documented statistically significant associations between sleep disorders including sleep apnea, narcolepsy, nightmare distress, sleep paralysis, and psychiatric sleep disorders with a history of childhood adversity. In many studies, the strengths of associations increased with the number and severity of adverse experiences. These associations were corroborated by the two prospective studies published to date. Notably, investigators have documented statistically significant associations between family conflict at 7-15 years of age and insomnia at 18 years of age (OR = 1.4; 95% CI = 1.2-1.7) and between childhood sexual abuse and sleep disturbances 10 years later in adult women (β = 0.24, p < 0.05). There is a growing scientific body of knowledge suggesting an association between ACEs and multiple sleep disorders in adulthood. Available evidence indicates the need to develop treatment strategies such as trauma-informed care for survivors of abuse who are suffering from sleep disorders and disturbances. Further, longitudinal studies among diverse populations are needed to improve overall understanding of this association and to investigate potential gender and racial/ethnic disparities in the strength of the association.
Keywords: adverse childhood experience, abuse, sleep
1. Introduction
Adverse childhood experiences (ACEs), typically defined as stressful or traumatic life events that occur during the first 18 years of life, such as emotional, physical, or sexual abuse, emotional or physical neglect, or other forms of family dysfunction, are pervasive and significant public health problems [1-3]. A 2008 nationally representative telephone survey estimated that about 61% of children and youth in the US experience at least one ACE per year [4]. This figure slightly decreased to 57.7% in 2011 [5]. The 2011 national survey reported that 13.7% of children had experienced maltreatment, 8.0% had experienced emotional abuse, and 3.7% had experienced physical abuse in the year prior to survey [5]. With regards to sexual abuse, 5.6% of children had been sexually victimized in the last year while 2.2% had been sexually assaulted. These estimates vary greatly by sex; among 14- to 17-year-old girls, 22.8% had experienced sexual victimization in the last year and 10.7% were sexually assaulted [5]. Additionally, the likelihood of lifetime sexual assaults was significantly higher for girls than for boys (17.4% vs. 4.2%) [5]. Because ACEs affect the majority of American children, it is gravely important to understand the burdens associated with these early-life events.
In addition to their acute effects such as injury and physical trauma, ACEs are associated with an increased risk of several negative health outcomes across the life course, such as mental illness, substance abuse, heart disease, and premature mortality [1-3, 6-13]. Among the few studies that have been conducted among women, investigators have identified suicide attempts and revictimization as additional outcomes of ACEs that have been exclusively identified among women [12, 13]. Early detection of a history of ACEs is critical in developing trauma-informed care for subsequent health consequences and in preventing further adverse health outcomes [14]. As a result, there is a pressing need to identify the long-term effects of ACEs.
Current evidence suggests that adult sleep disorders may be one such effect of ACEs. Sleep disorders are highly prevalent health concerns, estimated to affect 50 to 70 million Americans, and have cumulative effects over time [15]. Sleep disorders not only contribute to lost work-related productivity, they also lead to severe health outcomes such as obesity, hypertension, diabetes, occupational injuries, depression and premature mortality [16-20]. Identifying sleep disorders as a consequence of ACEs will inform the development of more effective therapy for survivors of abuse who are suffering from sleep disorders. Additionally, an accumulating body of epidemiologic evidence has identified sleep as a common mediator of many of the associations between ACEs and the aforementioned health outcomes. Thus, identifying and treating sleep disorders in patients exposed to an ACE could prevent additional downstream health and social consequences [7, 21-23]. Understanding the association between ACEs and adult sleep disorders in women is of particular interest because women are disproportionately affected by certain types of ACEs (e.g. sexual abuse) and sleep problems (e.g. difficulty maintaining sleep and excessive daytime sleepiness), and because women are at risk for unique health outcomes (e.g. revictimization and suicide) as a result of physical and emotional abuse [5, 12, 13, 24]. The following is a review of the literature regarding the association between ACEs and sleep disorders in adulthood. Because of the high burden of victimization and the potential for revictimization among girls and women, we place particular emphasis on summarizing the influences of childhood adversity and sleep disorders among women. Information gleaned from this review will contribute to a research and public health agenda that addresses the needs of survivors of ACEs.
2. Methods
The literature search for this systematic review included original studies of human subjects with no limitation on year of publication. The search was open to observational studies, including case series with 10 or more subjects, cross-sectional, prospective cohort, retrospective cohort, and case-control studies, as well as randomized trials. The exposure of interest, ACEs, was limited to adversity- or abuse-related events that occurred before 18 years of age. ACEs could have been assessed using self-report, family member reporting, or information extracted from police records. The outcome of interest was any measure of sleep disorders and/or quality (e.g. sleep deprivation, nightmare distress, or insomnia) assessed at 18 years or older. This outcome could have been assessed subjectively, objectively, or via clinical diagnosis.
Studies were identified through searches of the electronic databases MEDLINE, Embase, and Web of Science. The last search was conducted on 23 July 2014. In MEDLINE, we used the following search terms: “childhood”[All Fields] AND (“advers*”[All Fields] OR “abuse”[All Fields]) AND (“sleep”[MeSH Terms] OR “sleep”[All Fields]). In Embase, we used the following search terms: ‘childhood’ AND ‘adverse’ OR ‘adversity’ OR ‘abuse’) AND ‘sleep’ AND ‘article’/it. Finally, in Web of Science, we used the following search terms: childhood AND (advers* OR abuse) AND sleep. Two reviewers (SK and BG) conducted an abstract screen for all three databases separately. The reviewers then conducted a full-text screen after excluding ineligible abstracts and removing duplicate articles. An article was excluded if it was not an example of primary data collection or analysis (reviews, meeting abstracts, editorials, etc.), if it was a case series with fewer than 10 subjects, if the exposure included violence, trauma, or abuse experienced at 18 years of age or older, if the sleep-related outcome was assessed during childhood, or if the subjects were non-human. A search of the reference lists of eligible articles was then conducted to identify any missed articles. We considered conducting meta-analyses of the included articles, however the heterogeneity in exposure and outcome measures did not allow for any meaningful pooled analyses.
3. Results
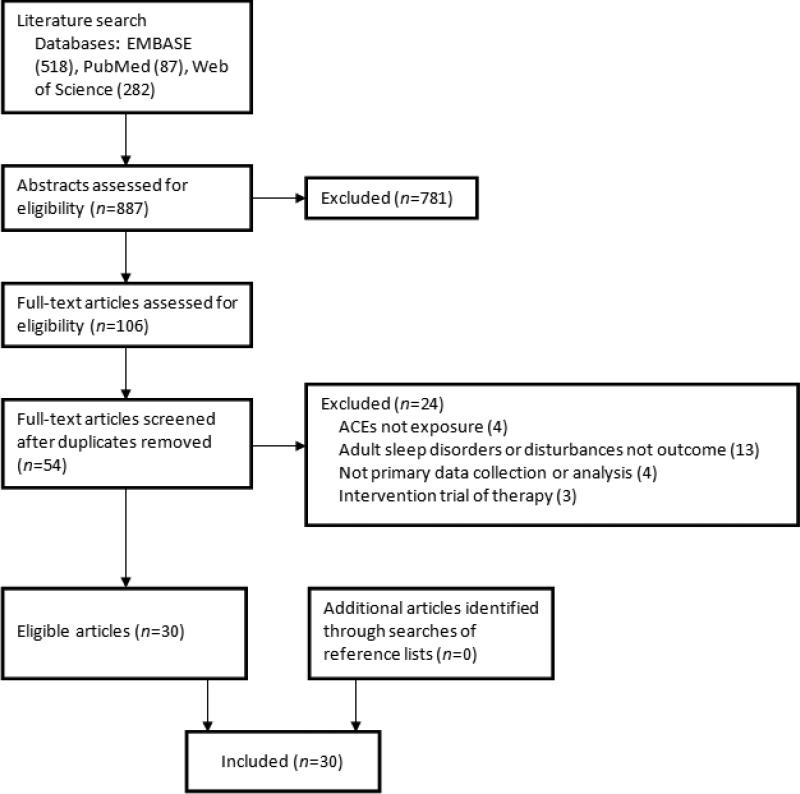
A total of 887 articles were identified through the electronic database search (87 from MEDLINE, 518 from Embase, and 282 from Web of Science). After the initial screening, based on titles and careful review of the abstracts, a total of 781 articles were excluded. After removing duplicates, 54 unique articles remained and underwent a full-text screen by the two reviewers. Overall, 24 articles were excluded during the full-text screen based on the aforementioned exclusion criteria. Figure 1 illustrates the search and screening process. The 30 articles that met the inclusion criteria are listed in Table 1 along with their study characteristics and a brief summary of major research findings. Overall, 14 of the 30 studies were conducted in the US, and 8 were conducted among women only. Childhood sexual abuse was the most common type of ACE investigated and self-reported sleep disturbances were the most common sleep-related outcomes studied. All relevant studies identified were published in the English language. The following is a summary of the literature concerning the relationship between ACEs and adult sleep disorders.
Figure 1.
Flowchart of study selection for systematic review
Table 1.
Characteristics of included articles
| Author, year | Study design | Population | Age | Exposure(s) | Sleep-related Outcome(s) | Covariates | Main findings |
|---|---|---|---|---|---|---|---|
| Abrams, 2008 | Cross-sectional, retrospective | 263 Canadian university students | Mean: 22.24 (men); 22.25 (women) | Childhood sexual abuse (confirmed, unconfirmed, none) | Sleep paralysis | None | Exposed group scored higher than control group on intruder index (MD=3.57, p<0.01) and incubus index (MD=3.56, p<0.01) |
| Agargun, 2002 | Cross-sectional, retrospective | 382 Turkish university students | Mean: 20.9 (men); 20.06 (women) | Childhood sexual abuse, physical abuse, parental loss, parental separation (binary) | VBS | None | % of those with VBS v. no VBS with history of sexual abuse (10.6 v. 5.5), physical abuse (26.5 v. 12.1), parental loss (6.4 v. 9.3), and parental separation (11.7 v. 7.9) |
| Agargun, 2003 | Cross-sectional, retrospective | 292 Turkish university students | Mean: 20.4 | Childhood physical abuse, sexual abuse, maternal loss, maternal separation (binary) | Nightmare frequency, difficulty falling sleep, fear of sleeping, trouble sleeping, daytime sleepiness | None | Rate of childhood traumatic events among subjects who reported nightmares often = 55%, among those who reported nightmares sometimes = 27%, and those who reported no nightmares = 24% |
| Bader, 2007 | Retrospective | 39 Swiss adults with insomnia | Mean: 43.0 | German version of CTQ (continuous) | Actigraphy: sleep onset latency, sleep efficiency, no. of body movements, moving time | Depression, arousability predisposition, stress level of the last week, daily hassles of the last month, critical life events of the last 6 mo, sex, age | ACEs explained 38.7% of variance in sleep onset latency, 36.6% of variance in sleep efficiency, 40.3% of variance in no. of body movements, and 35.7% of variance in moving time |
| Bader, 2007 | Retrospective | 59 Swiss adults with insomnia | Mean: 43.6 | German version of CTQ (continuous) | PSG, actigraphy, PSQI | Age | Insomniacs with moderate-severe ACEs v. low or no ACEs had greater no. of awakenings (4.7 v. 3.6), greater no. of movement arousals (5.8 v. 4.4), lower sleep efficiency (76.5 v. 87.2), greater no. of body movements (38.8 v. 12.8), and greater proportion of sleep time spent moving (23.3 v. 12.7). No significant differences in PSQI score (9.9 v. 9.3) |
| Bader, 2013 | Retrospective | 45 Swiss adults with insomnia | Mean: 45.1 | German version of CTQ (continuous) | PSG | Age, number of critical life events in past 6 mo | Insomniacs with history of ACEs had greater β 1 (p=0.033) and β 2 (p=0.037) activity during non-REM sleep and greater δ (p=8.98), σ (p=0.038), β 1 (p=0.037), and β 2 (p=0.038) activity during REM sleep than controls |
| Barker-Collo, 1999 | Cross-sectional, retrospective | 138 Canadian women with history of sexual abuse | Mean: 31.4 | Race (Native Canadian v. White Canadian) | Sleep Disturbance subscale of TSC-40 | None | Significant differences between Native Canadians v. Whites in insomnia (2.42 v. 1.99, p=0.045), early morning wakings (2.17 v. 1.46, p=0.003), and mid-night wakings (2.40 v. 1.83, p=0.007) |
| Brower, 2012 | Cross-sectional, retrospective | 285 Polish adults with alcohol dependence | Mean: 43.2 | Childhood physical and sexual abuse (binary) | Insomnia | Neuroticism, impulsiveness, Michigan Alcoholism Screening Test score, drinking days, mental health score, physical health score | Childhood abuse predicted insomnia severity (β=0.143, p=0.013) |
| Chambers, 1998 | Cross-sectional, retrospective | 97 Canadian university students | Mean: 21.6 | Physical, sexual, or psychological/emotional abuse, emotional or physical neglect, medical or other trauma (binary) | Sleep and dream disturbance | None | Abuse/trauma group scored more negatively than controls in all measures; significant associations were nightmare frequency (p<0.05), sleep apnea (p<0.01), narcolepsy (p<0.01), nightmare distress (p<0.01), nightmare impact (p<0.01), and psychiatric sleep disorder (p<0.01) |
| Chapman, 2011 | Retrospective cohort | 17337 adults in US | Range: 19- Mean: 34 | Emotional, physical, or sexual abuse, household substance abuse, household mental illness, witnessed domestic violence, incarcerated household member, parental separation or divorce (binary) | Self-reported sleep disturbances | Sex, age, race, education | aORs of reporting trouble falling/staying asleep ranged from 1.1-1.7 and of feeling tired after sleep ranged from 1.2-1.6. Odds increased with increasing no. of ACEs (ptrend < 0.0001 for both outcomes) |
| Chapman, 2013 | Cross-sectional, retrospective | 25810 adults in US | 18 and older | Physical, sexual, or verbal abuse, household mental illness, incarcerated household members, household substance abuse, parental separation/divorce, witnessing domestic violence (binary) | Frequent insufficient sleep | Gender, age, race/ethnicity, education, body mass index | aORs of frequent insufficient sleep ranged from 1.1-1.4. Odds increased with increasing no. of ACEs (aORs ranged from 1.3-2.5 for 1 ACE to 5 or more ACEs v. none) |
| Duval, 2013 | Cross-sectional, retrospective | 352 Canadian female university students | Mean: 21.4 | French version of CTQ (continuous) | Disturbed dreaming | None | Medium and high abuse/neglect were significant predictors of disturbed dreaming (β=0.125 and 0.197). Low abuse/neglect did not reach statistical significance (β=0.086) |
| Elliott, 1992 | Cross-sectional, retrospective | 2963 women in US | Mean: 41.7 | Childhood sexual abuse (binary) | Sleep Disturbance subscale of TSC-40 | None | Mean score for those with sexual abuse v. no sexual abuse = 5.84 v. 5.03 out of 18 (t=6.24, p<0.0001) |
| Gal, 2011 | Cross-sectional, retrospective | 4859 Israeli adults | Median: 47 | Childhood physical and childhood and adolescent sexual abuse (binary) | Self-reported sleep disturbances | Gender, mood and anxiety disorders, age, education, immigration, marital status, religious observance during childhood, report on additional childhood stressful events, number of fateful events during 24 mo preceding survey | Associations between sleep disturbances and childhood sexual abuse (OR=1.7), adolescent sexual abuse (OR=1.6), childhood physical abuse (OR=2.5), any childhood abuse (OR=2.0), and any adolescent abuse (OR=1.5) |
| Greenfield, 2011 | Cross-sectional, retrospective | 835 adults in US | Mean: 58.27 | Frequent or occasional childhood physical, sexual, or emotional abuse (categorical) | PSQI score | Age, gender, marital status, residing with child under age of 6, educational attainment, annual adjusted income, employment status, living with both biological parents until age 16, parents’ educational attainment, twin status | Associations between PSQI score > 5 and frequent physical and emotional with sexual abuse (OR=3.7), frequent physical and emotional without sexual abuse (OR=3.3), and occasional physical and emotional with sexual abuse (OR=1.7) compared with no abuse history |
| Gregory, 2006 | Longitudinal (over 18 years) | 1037 children in New Zealand | Mean: 18 | Family conflict in childhood (continuous) | Insomnia at 18 years of age | Sex, socioeconomic status, sleep problems at 9 years, health problems at 18 years | Family conflict at 7 to 15 years associated with insomnia at 18 years (aOR = 1.4) |
| Hairston, 2011 | Retrospective | 184 first-time mothers in US | Mean: 27.5 | Short form of CTQ (continuous) | Subjective sleep difficulty | PTSD, postpartum depression, socioeconomic status | Main effect of group for sleep difficulty between mothers with childhood abuse and PTSD, mothers with childhood abuse and no PTSD, and controls (F1,187=16.2, p<0.001) |
| Haj-Yahia, 2008 | Cross-sectional, retrospective | 476 Sri Lankan medical students | Mean: 22.2 | Witnessing interparental violence, experiencing parental violence (continuous) | Subjective sleep disturbances | Age, gender, father's age, father's level of education, mother's age, mother's level of education, number of siblings, socioeconomic status, family functioning and environment | Witnessing parental violence associated with sleep disturbances (β=0.32, p<0.001) as was experiencing abuse by a parent (β=0.37, p<0.001) |
| Heath, 1996 | Cross-sectional, retrospective | 492 adults in US with history of sexual abuse | Mean: 43 (men); 38 (women) | Severity of childhood sexual abuse (categorical) | Sleep Disturbance subscale of TSC-33 | None | Sexual abuse severity explained 6% of the variation in sleep disturbance in men and 10% of the variance in women |
| Heitkemper, 2011 | Retrospective | 40 women in US with IBS | Mean: 31.3 | CTQ (binary) | PSQI and PSG | Age | PSQI score was greater among women with abuse/neglect history than controls (7.2 v. 5.0). No significant differences in PSG data, except % time in REM was greater in abuse/neglect group (23.2 v. 20.4) |
| Hulme, 2000 | Cross-sectional retrospective | 395 women in US | Mean: 34.5 | Childhood sexual abuse (binary) | Reporting “can't sleep at night” | None | Chi-square = 25.4, p<0.001 |
| Insana, 2012 | Retrospective | 63 military veterans in US | Mean: 39.25 | Number of traumatic events (as measured by THQ) before age 18 (continuous) | PSQI, REM %, no. of REM periods, REM fragmentation, REM latency, delta EEG in REM, beta EEG in REM | Age, combat exposure, later-life trauma | No significant associations, except with increased REM fragmentation (df=57, r=0.36, p=0.005) |
| Kelly, 2010 | Cross-sectional, retrospective | 33 Latina immigrant women in US | Mean: 39.7 | Childhood sexual assault (binary) | Self-reported sleeping difficulty | None | Childhood sexual assault and sleep difficulty were strongly correlated (r=0.349) |
| Koskenvuo, 2010 | Cross-sectional, retrospective | 25898 Finnish adults | Range: 20-54 | Divorce or separation of the parents, long-term financial difficulties in the family, serious conflicts in the family, frequent fear of a family member, severe illness of a family member, alcohol problem of a family member (categorical by number of adversities) | Self-reported sleep quality | Age, gender; work status; psychotropic drugs; health behavior; recent life events; child-parent relationships | Significant graded association between childhood adversities and sleep quality: OR for 1-2 adversities v. 0 = 1.9 and OR for 3-6 adversities v. 0 = 3.6 |
| McNally, 2005 | Cross-sectional, retrospective | 84 adults in US | Mean: 41.9 | Childhood sexual abuse (repressed, recovered, continuous, none) | Sleep paralysis | None | Women with repressed, recovered, or continuous memories of childhood sexual abuse reported sleep paralysis more frequently than women with no abuse history (44%, 43%, 47%, and 13%, respectively) |
| Noll, 2006 | Longitudinal (over 10 years) | 147 women in US | Median: 18.23 | Childhood sexual abuse (binary) | Self-reported sleep disturbances | Age | Childhood sexual abuse was significantly associated with sleep disturbances (β = 0.24, p < 0.05) |
| Poon, 2011 | Retrospective | 877 adults in US aged 60+ | Mean: 69.25 | Parental physical abuse, emotional abuse, and neglect (binary) | Self-reported sleep complaints | Age, sex, race, education, marital status, self-rated health, parental death before age 17, parental divorce before age 17 | Emotional abuse was significantly associated with sleep complaints (β=0.11), but physical abuse and neglect were not (β=−0.04 and 0.07, respectively) |
| Ramsawh, 2011 | Retrospective | 327 university students in US | Mean: 18.9 | CTQ (continuous) | PSQI | None | CTQ total score was significantly associated with a PSQI score ≥ 5 (38.2 v. 32.9) |
| Schafer, 2013 | Retrospective | 48 Swiss psychiatric outpatients | Mean: 31.4 | Childhood stress load in five domains: health, family, friendships/relationships, education, and others (continuous) | Subjective: sleep quality, restorative value of sleep, psychosomatic symptoms during sleep; Actigraphic: total sleep time, sleep onset latency, sleep efficiency, no. of body movements | Age | Childhood stress load significant associated with actigraphic measures of total sleep time (β=−0.32), prolonged sleep latency (β=0.32), decreased sleep efficiency (β=−0.32), and increased no. of body movements (β=0.27). Stress load not significantly associated with subjective measures |
| Zhabenko, 2012 | Cross-sectional, retrospective | 304 Polish adults with alcohol dependence | Mean: 43.5 | Childhood sexual or physical abuse (binary) | Insomnia | None | Childhood sexual or physical abuse was significantly associated with insomnia (OR=2.4) |
VBS = violent behavior during sleep; CTQ = Childhood Trauma Questionnaire; ACEs = adverse childhood experiences; PSG = polysomnography; PSQI = Pittsburgh Sleep Quality Index; REM = rapid eye movement; TSC = Trauma Symptom Checklist; aOR = adjusted odds ratio; OR = odds ratio; PTSD = post-traumatic stress disorder; THQ = Trauma History Questionnaire; EEG = electroencephalography.
3.1 Early Research on ACEs and Adult Sleep
Three studies provided initial evidence of an association between ACEs and subjective sleep in adulthood [25-27]. In their study of 97 Canadian university students, Chambers et al. [25] found that participants who had a history of ACEs had higher mean scores than participants without ACEs in all subjective sleep disorder measures. Statistically significant differences were found for nightmare frequency (0.7 vs. 0.3), sleep apnea (17.8 vs. 14.5), narcolepsy (25.8 vs. 21.1), nightmare distress (31.9 vs. 26.0), nightmare impact (25.2 vs. 18.5), and psychiatric sleep disorders (22.7 vs. 17.2). Chambers et al. [25] also identified resilience as a potential mediator of the relationship between abuse/trauma and sleep outcomes. Agargun et al. [26], in their study of 382 Turkish undergraduate students, identified a statistically significant association between ACEs and violent behavior during sleep (VBS), a disorder involving self-mutilation, sexual assault, or murder attempt during sleep. The authors reported that a greater proportion of participants with VBS reported a history of sexual abuse (10.6% vs. 5.5%), physical abuse (26.5% vs. 12.1%), parental loss (6.4% vs. 9.3%), and parental separation (11.7% vs. 7.9%) compared with controls. In a 2003 study of 292 undergraduate students, Agargun et al. [27] found that the frequency of childhood traumatic events was higher among subjects who reported having nightmares often (55%) compared with subjects who reported having nightmares sometimes (27%) and subjects who reported no nightmares (24%). In addition to nightmare frequency, physical abuse and sexual abuse were statistically significantly associated with difficulty falling asleep, fear of sleeping, and trouble sleeping compared with no abuse [27]. Collectively, these early studies support cross-sectional associations of history of ACEs and a number of subjective sleep disorders and disturbances.
3.2 Recent Evidence on ACEs and Adult Sleep Quality
In recent years, there has been an accumulating body of epidemiologic evidence documenting an association between ACEs and subjective sleep quality in adulthood, despite differences in study design, study populations, and instruments used to classify sleep disturbance [21, 28-33]. Two studies used the Pittsburgh Sleep Quality Index (PSQI) to assess overall sleep quality [31, 33]. Greenfield et al. [31] identified an association between three categories of ACEs and poor sleep quality (defined as a global PSQI score > 5 out of 21). Compared with no abuse history, poorer sleep quality was observed among those reporting frequent physical and emotional with sexual abuse (OR = 3.7; 95% CI = 1.8-7.6), frequent physical and emotional without sexual abuse (OR = 3.3; 95% CI = 1.8-5.9), and occasional physical and emotional with sexual abuse (OR = 1.7; 95% CI = 1.1-2.7). Ramsawh et al. [33] utilized the PSQI to measure subjective sleep quality in relation to participants’ scores on the Childhood Trauma Questionnaire (CTQ) and found mean CTQ scores to be positively associated with PSQI scores (β = 0.26, p < 0.001). Taken together, available evidence suggests that a history of ACEs is associated with poor sleep quality as measured by the PSQI.
Other studies have assessed the relationship between ACEs and adult sleep disturbances [21, 28-30, 32]. For example, Gal et al. [29] found statistically significant associations between the following exposures and self-reported sleep disturbances: sexual abuse in childhood (OR = 1.7; 95% CI = 1.1-2.7), physical abuse in childhood (OR = 2.5; 95% CI = 1.5-4.1), and general abuse in childhood (OR = 2.0; 95% CI = 1.5-2.8). Haj-Yahia et al. [28] reported a similar association between physical abuse and subjective sleep disturbances. Chapman et al. [30] identified statistically significant associations for trouble falling/staying asleep and feeling tired after a good night's sleep with eight categories of ACEs: emotional abuse, witnessing domestic violence, household substance abuse, household mental illness, parental separation/divorce, and household member imprisonment. The strongest associations were observed between physical abuse and emotional abuse and trouble falling/staying asleep, adjusted for demographic characteristics (adjusted odds ratio (aOR) for both = 1.7; 95% CI = 1.5-1.9) [30]. In 2013, Chapman et al. [21] found these eight types of ACEs to be associated with frequent insufficient sleep, even after adjusting for mental distress. For example, the authors reported a strong association between physical abuse and frequent insufficient sleep (aOR = 1.4; 95% CI = 1.2-1.7) [21]. A study among adults aged 60 years and older found that parental emotional abuse was statistically significantly associated with sleep complaints (β = 0.11, p < 0.05), however the associations between sleep complaints and physical abuse (β = −0.04, p > 0.05) and emotional neglect (β = 0.07, p > 0.05) were not statistically significant [32]. In addition to the cross-sectional associations identified, Gregory et al. [34] identified a longitudinal association between family conflict at 7-15 years of age and insomnia at 18 years of age after controlling for sex, socioeconomic status, sleep problems at 9 years, and self-reported health at 18 years (aOR = 1.4; 95% CI = 1.2-1.7).
Furthermore, investigators have found statistically significant, graded relationships between the number of ACEs and sleep disorders [21, 30, 35]. These relationships are particularly important because ACEs are highly interrelated [3, 21, 36]. Koskenvuo et al. [35] found statistically significant associations between number of childhood adversities and subjective sleep quality. After controlling for age, gender, and recent stressful life events, the aOR of self-reported poor sleep quality comparing 1-2 adversities with 0 adversities was 1.9 (95% CI = 1.6-2.3) and comparing 3-6 childhood adversities with 0 adversities was 3.5 (95% CI = 2.7-4.4). In Chapman et al. [30]'s analysis of sleep disturbances, the odds of having trouble falling/staying asleep and of feeling tired after sleeping increased with increasing number of ACEs (Ptrend < 0.0001 for both). Relative to those with no ACEs, the odds of having trouble falling/staying asleep ranged from 1.2-fold greater (95% CI = 1.1-1.3) to 2.1-fold greater (95% CI = 1.8-2.4) as number of ACEs increased. These figures for feeling tired after sleeping were 1.2 (95% CI = 1.1-1.3) and 2.0 (95% CI = 1.7-2.3) [30]. In 2013, Chapman et al. [21] also found a statistically-significant, graded relationship between number of ACEs and the prevalence of frequent insufficient sleep after adjusting for mental distress (aOR for 1 ACE vs. 0 = 1.2, 95% CI = 1.0-1.4; aOR for 5 or more ACEs vs. 0 = 1.8, 95% CI = 1.5-2.2). In summary, current evidence suggests that the more ACEs that a child experiences, the greater his/her risk for sleep disorders is in adulthood.
We found two studies that assessed sleep outcomes in men and women using objective methods [37, 38]. In their study of 63 military veterans, Insana et al. [37] reported that early life trauma, assessed using the Trauma History Questionnaire (THQ), was not statistically significantly correlated with rapid eye movement (REM) latency, % REM, number of REM periods, or REM microarousals measured via polysomnography (PSG). Similar null findings were noted when sleep quality was assessed using the PSQI. The only sleep outcome found to be correlated with veterans’ history of child trauma was REM fragmentation (r = 0.36, p = 0.005). Schafer et al. [38] compared stress load in early life with both subjective and 7-day actigraphic measures of sleep. The authors found that childhood stress load was a correlate of objectively measured total sleep time (β = −0.32, p ≤ 0.05), sleep latency (β = 0.32, p ≤ 0.05), sleep efficiency (β = −0.32, p ≤ 0.05), and number of body movements (β = 0.27, p < 0.10) [38]. Similarly, childhood stress load was not statistically significantly associated with any subjective measures of sleep. Although the lack of a statistically significant association between childhood stress and trauma and subjective measures of sleep was not concordant with prior studies of subjective sleep, the exposures evaluated in these two studies are much broader than ACEs, including other exposures to stress such as bullying, educational demands, or disablements [37, 38]. This heterogeneity in definition of ACEs or the small samples of participants studied (N=63 and N=48, respectively) might have contributed to the null findings observed in these two studies.
Some investigators have examined the extent to which ACEs affect a specific sleep disorder—sleep paralysis [39, 40]. Sleep paralysis occurs when the motor paralysis characteristic of REM sleep continues after awakening and is often accompanied by tactile and visual hallucinations [39, 40]. McNally et al. [39] found that reports of sleep paralysis were more common among participants with a history of childhood sexual abuse, either repressed (44%), recovered (43%), or continuous (47%), compared to those with no history of childhood sexual abuse (13%). Further, Abrams et al. [40] found that participants reporting a history of childhood sexual abuse reported more frequent and more distressing episodes of sleep paralysis than those who reported no abuse. Specifically, a larger proportion of those reporting a history of sexual abuse reported having incubus (17%) and intruder (19%) episodes of sleep paralysis frequently/always relative to vestibular motor episodes (5%), which are categorized as being much less distressing, and relative to the group with no sexual abuse history (incubus: 6%, intruder: 6%, vestibular motor: 5%) [40].
3.3 Special Populations
In this section, we provide a brief summary of studies that have assessed associations of ACEs with sleep outcomes in specified subpopulations.
3.3.1 Studies among Women
Limited research among the general population suggests gender differences in the relationship between ACEs and sleep, but the data are generally inconclusive [33, 35, 41-43]. Four studies [23, 44-46] have evaluated the association between childhood sexual abuse and subjective sleep disturbances in women, one of which had a longitudinal design [23]. The investigators found that abuse status was a statistically significant predictor of sleep disturbances (β = 0.24, p < 0.05) 10 years after disclosure of abuse [23]. The remaining three studies on this topic found statistically significant cross-sectional associations between childhood sexual abuse and subjective sleep disturbances in women [44-46]. Overall, there is evidence of a strong association between subjective sleep disturbances in adulthood and childhood sexual abuse among women; however more evidence is needed on other forms of ACEs.
We found three additional studies conducted among women in which the CTQ was used to assess childhood trauma experiences [47-49]. One of these studies, conducted among 40 women with irritable bowel syndrome (IBS), utilized both subjective and objective measures of sleep [48]. Women with IBS and a history of abuse and/or neglect had a statistically significantly higher mean PSQI score (7.2) when compared with women with IBS and no history of ACEs (5.0) and women without IBS or a history of ACEs (4.0). Of note, of all the objectively measured sleep outcomes assessed, only one – time to REM sleep – was statistically significant when the investigators compared women with a history of childhood trauma and those without such a history [48]. The two studies that used subjective sleep measures found a statistically significant association between childhood abuse/neglect and disturbed dreaming [49] as well as a main effect of group for sleep difficulty between mothers with childhood abuse and PTSD, mothers with childhood abuse without PTSD, and controls (F1,187=16.2, p < 0.001) [47]. This suggests an association between childhood abuse and sleep difficulty among postpartum women, but the independent contribution of childhood abuse (with or without PTSD) was not assessed. On balance, there is a dearth of research concerning the influence of childhood adversity and sleep outcomes (measured subjectively or objectively), among adult women.
A 1999 retrospective study of 138 Canadian women is the only study, to our knowledge, that examined racial/ethnic differences in the association between ACEs and sleep disturbances using a sample of Native Canadian and White Canadian women [50]. The investigators sought to describe differences in the long-term correlates of childhood abuse between these two groups due to the high prevalence of childhood sexual abuse among Native Canadians and because previous research had been limited to primarily White individuals [50]. All of the women included in the study had a history of childhood sexual abuse. The Native Canadian participants’ scores on the sleep disturbance subscale of the TSC-40 were compared to those of the White Canadian participants. The Native Canadian women scored statistically significantly higher on multiple measures of sleep disturbances compared with the White Canadian women: insomnia (2.4 vs. 2.0, p = 0.45), early morning wakings (2.2 vs. 1.5, p = 0.003), and mid-night wakings (2.4 vs. 1.8, p = 0.007) [50]. This presents initial evidence of a potential racial/ethnic disparity in the association between ACEs and sleep disturbances however further investigation is necessary to understand this potential disparity.
3.3.2 Insomnia Patients
Studies of ACEs among insomniacs demonstrate that patients with a history of ACEs have different sleep characteristics than those without a history of ACEs. Bader et al. [41] found that insomniacs who reported moderate to severe ACEs vs. low or no ACEs had a statistically significantly greater proportion of awakenings during sleep time (3.4% vs. 2.3%, p = 0.034), greater proportion of movement arousals during sleep time (5.8% vs. 4.4%, p = 0.012), lower sleep efficiency (76.5% vs. 87.2%, p = 0.023), and greater proportion of sleep time spent moving (23.3% vs. 12.7%, p = 0.008) all of which were measured objectively. Furthermore, Bader et al. [42] found that a history of abuse and neglect explained a moderate amount of the variance in actigraphically assessed sleep onset latency (39%), sleep efficiency (37%), number of bodily movements (40%) and moving time (36%) in their study population.
3.3.3 Alcohol-Dependent Patients
Zhabenko et al. [51] assessed the relationship between ACEs and insomnia and found that the odds of insomnia among participants with a childhood history of sexual or physical abuse was 2.4-fold greater (95% CI = 1.2-4.6) than the odds among participants without a history of abuse. Brower et al. [52] assessed the same relationship using linear regression and the results were in general agreement with those of Zhabenko et al.
4. Discussion
4.1 Significance of the Association between ACEs and Adult Sleep
This systematic review found that ACEs are associated with multiple sleep disorders and disturbances in adulthood. Having a better understanding of the relationship between ACEs and sleep in adulthood is of great clinical significance for multiple reasons. First, disturbed sleep in adulthood may serve as an indicator for the assessment of abuse or trauma history and may also be a consequence of more serious underlying health problems. There is a pressing need for identification of symptoms that would suggest a history of abuse, specifically among women, so that proper treatment and care can be provided [53]. Diagnostic routines for sleep disorders typically fail to include an assessment of trauma history unless the patient is suspected of having depression or PTSD. However, mounting evidence suggests that ACEs and sleep disorders are associated regardless of mental health status [21, 23, 42, 52, 53].
A second implication of an established association between ACEs and sleep disorders is the improvement of treatment for sleep disorders among survivors of childhood abuse. A randomized trial of interpersonal psychotherapy was conducted among women with major depression and a history of childhood sexual abuse [54]. The authors found that interpersonal psychotherapy resulted in significant improvements in depression severity (measured using multiple depression scales), but did not result in any significant improvements in insomnia severity. Thus, it appears as though survivors of ACEs with insomnia may require more complex therapy than those without insomnia [54]. Additionally, there is evidence that patients with sleep disorders and a history of ACEs require different treatment than those without a history of ACEs. For example, authors have suggested that treatment for sleep problems in women with a history of sexual abuse is unique and should involve psychosocial intervention [23]. The same may be true for all adults with a history of any ACEs. Finally, it may be necessary to develop treatment for sleep paralysis, which typically goes untreated. Abrams et al. [40] argue that an educational program for patients suffering from sleep paralysis as a result of childhood sexual abuse is warranted. Development of additional treatment options may be necessary.
Another implication of this association is recognizing that sleep may be an important mediator of the relationships between ACEs and other serious health outcomes. For instance, a review of the literature concerning sleep as a mediator of the association between violence-induced trauma and poorer health found sleep to be a significant mediator for multiple outcomes, including immune dysfunction and depression, thus it is likely that this holds for associations between ACEs and poorer health [55]. Lee et al. [22] found that a history of childhood abuse is statistically significantly associated with metabolic syndrome symptoms and diagnosis in adults: poor sleep quality explained 24% of the association between abuse and risk of metabolic syndrome diagnosis in women and 20% in men. Additionally, multiple studies have identified associations between sleep disturbances and later abuse in adulthood [23, 56]. Noll et al. [23] found the occurrence of sleep disturbances to be statistically significantly associated with revictimization among female survivors of sexual abuse (β = 0.25, p < 0.01). It is critical to identify adult sleep disorders as mechanisms through which ACEs result in other negative health outcomes in order to prevent such downstream consequences. Identifying and treating sleep disorders in patients with a history of ACEs may prevent these additional health outcomes.
4.2 Significance in Women
Enhanced understanding of the association between ACEs and adult sleep disorders in women is particularly important because there is currently contradictory evidence regarding gender differences in the strength of this association. We are using the term gender to describe these supposed disparities due to our speculation that the disparities are socially driven [57]. However, because previous studies on this topic have used sex and gender interchangeably, we cannot be certain that differences in this association are exclusively attributable to either sex or gender. Available evidence suggests that women have an increased likelihood of developing negative outcomes after an ACE [33, 57, 58]. As a result, the burden of ACE-related morbidity may be expected to be higher in women. To our knowledge, only five studies have evaluated gender differences in the association of interest [33, 35, 41-43]. Two of these four studies reported no statistically significant gender differences [41, 42]. However, the other three studies found significant gender differences. Heath et al. [43] reported that childhood sexual abuse severity explained a greater percentage of the variation in sleep disturbances among women than men (10% vs. 6%) and Koskenvuo et al. [35] found a stronger association between ACEs and subjective sleep quality among women than men when controlling for work status and health behaviors. On the contrary, Ramsawh et al. [33] found a stronger association between ACEs and subjective sleep quality among men (β for ACE and gender interaction term = 0.52, p = 0.023). The research surrounding gender differences in the association between ACEs and sleep is largely inconclusive, demonstrating a need for more data.
Another reason for the importance of understanding this association among women is that women are at risk for unique sequelae involving both ACEs and sleep disorders. For example, research indicates that infants of women with a history of ACEs are at an increased risk of developing sleep disorders through a process known as intergenerational transmission of trauma [47]. Another aspect of the ACE-sleep association that is unique to women is the role of vasomotor symptoms of menopause. Thurston et al. [59] studied the association between childhood abuse or neglect and vasomotor symptoms, which often affect sleep quality. The authors found that women with any child abuse or neglect had 1.7 (95% CI = 1.2-2.4) times the odds of reporting hot flashes and 1.8 (95% CI = 1.3-2.4) times the odds of reporting night sweats compared with women without a history of child abuse or neglect. Furthermore, these associations were statistically significantly stronger in African American women than in White women, further indicating the importance of studying racial/ethnic disparities in the association between ACEs and sleep [59].
4.3 Potential Mechanisms
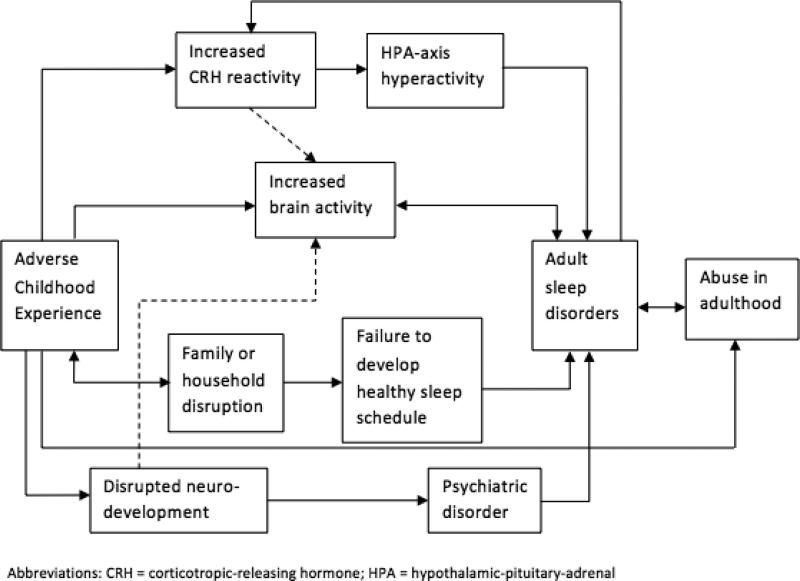
Several investigators suggest that exposure to stress or trauma in childhood causes general circadian dysregulation and thereby disrupts sleep regulation [23, 31, 60]. However, the mechanism through which ACEs alter circadian regulation is unclear. There is substantial evidence to suggest that corticotropin-releasing hormone (CRH) plays a key role. Elevated CRH, and subsequently hypothalamic-pituitary-adrenal (HPA) axis hyperactivity, is associated with diminished sleep [61, 62]. It is possible that childhood adversity increases CRH reactivity, which subsequently affects sleep quality, but the research concerning the association between ACEs and cortisol is inconclusive. Multiple investigators have shown that a history of childhood abuse or maltreatment is associated with increased cortisol reactivity, supporting the proposed hypothesis [63-67], while others have shown ACEs to be associated with diminished cortisol reactivity [68-70]. Thus, it is unclear whether or not elevated CRH explains the association between ACEs and poorer sleep.
Another proposed mechanism of this association is increased neuron activity in the brain as measured by electroencephalography (EEG), particularly in patients with insomnia. Investigators have shown that insomniacs have increased β EEG activity [41, 71, 72]. A recent study conducted among patients with insomnia reported that participants with a history of moderate to severe childhood maltreatment exhibited increased β EEG activity compared to those with no history of maltreatment [73]. This study provides initial evidence that increased brain activity may explain the association between ACEs and adult insomnia. Additionally, it is possible that this mechanism is linked with the proposed mechanism involving elevated CRH. Elevated CRH increases brain activity during sleep; however, the evidence surrounding which EEG frequency band it affects is ambiguous [61]. More research is needed to understand the relationship between CRH and β EEG activity to better inform a potential mechanism between ACEs and sleep.
An additional mechanism to explain the association between ACEs and adult sleep is a strictly social mechanism. Investigators have posited that children exposed to ACEs grow up with increased family chaos and household disruption and thus never learn proper sleeping habits [31, 41]. As adults, these individuals may still lack the ability to maintain a healthy sleep schedule. It has been further suggested that individuals exposed to ACEs in childhood have an increased likelihood of experiencing multiple subsequent stressors across the life course, including revictimization, which may continue to negatively impact their sleep quality [31, 56]. Such social mechanisms may explain the persistence of sleep pathology into adulthood following an ACE. When speculating about social mechanisms, it is also important to consider the potential mediating role of resilience in the relationship between childhood abuse and adult sleep outcomes. Prior evidence has suggested that resilience can protect individuals from the negative effects of abuse or trauma [25]. Chambers et al. [25] found that individuals exposed to ACEs who had resilient characteristics (measured using the Internal-External Locus of Control Scale, a Resilient Characteristics Questionnaire, and the Ways of Coping questionnaire) still suffered from sleep disturbance, but were better able to cope with these sleep problems. In fact, some social scientists consider good sleep quality to be an indicator of resilience [74]. So, while resilience may not impact the development of sleep disorders as a result of childhood abuse, it may play a role in recovery and coping.
Finally, another plausible mechanism that may explain the relationship between ACEs and adult sleep outcomes in some individuals involves the development of a mood disorder due to traumatic stress experienced during childhood or adolescence. Childhood and adolescence are periods of rapid brain development. Neuroimaging research has provided evidence that traumatic experiences during this developmental stage interfere with normal brain development and impair individuals’ ability to develop the life skills necessary for becoming independent adults [75]. This impairment is often associated with psychiatric disorders, such as PTSD and major depressive disorder, of which sleep disturbance is a common symptom [75]. It is important to note that each individual proposed mechanism does not fully explain observed associations of ACEs with sleep disturbances; it is more likely that these mechanisms interact with one another involving both biological and social pathways. Figure 2 presents a conceptual model integrating these diverse and plausible mechanisms that may underlie consistently observed associations of childhood adversity with sleep disorders and disturbances.
Figure 2.
Potential mechanisms
4.4 Limitations of Studies
The studies included in this systematic review have some limitations that merit consideration. Of the 30 included studies, 28 were retrospective by design; only two studies used a prospective longitudinal study design [23, 34]. Hence, the majority of the studies are subject to possible recall bias. Because the vast majority of studies relied on subjective reports of sleep disorders and disturbances, the likelihood of misclassification cannot be excluded. The lack of prospective data makes it difficult to clearly elucidate the temporal relationship between adverse experiences and the occurrence of sleep disorders. The generalizability of available findings is limited, in part, because the vast majority of published studies to date have minimal to no representation of ethnic and racial minority groups. For example, we noted that 78% of the studies in which race was reported focused primarily on Whites. Lastly, causal inferences for many of the studies reviewed are limited, in part, because few investigators used multivariable analytical techniques to adjust for possible confounding factors.
5. Summary and Future Directions
ACEs are highly prevalent among children growing up in the US and can result in severe long-term health and social consequences [1-3, 5-13]. Multiple retrospective studies have identified associations between ACEs and sleep disorders and disturbances measured subjectively [21, 25-33, 35]. Two studies found a statistically significant association between childhood sexual abuse and sleep paralysis [39, 40]. Limited available evidence documents association between ACEs and sleep in women, a population with high burden of ACE exposure and who are uniquely vulnerable to sleep disorders across the life course [5, 24]. Those studies focused on women have suggested associations between different types of ACEs and subjective measures of sleep [23, 44-46, 49]. Investigators have also identified associations between ACEs and sleep disorders among other particularly vulnerable populations including insomnia patients and individuals dependent on alcohol [41, 42, 51, 52].
On the basis of the available literature, we have identified a need to develop trauma-informed care for survivors of abuse who are suffering from sleep disorders or disturbance. Our position is supported by empirical evidence from a clinical intervention study. Krakow et al. [76] conducted a randomized controlled trial of imagery rehearsal therapy among 168 sexual abuse survivors to determine its effectiveness in treating chronic nightmares. At 3-month follow-up, participants who received imagery rehearsal therapy had significantly greater improvements than control participants in the following measures: nights per week with nightmares (Cohen d = 1.2 vs. 0.1), nightmares per week (Cohen d = 1.0 vs. −0.1), PSQI scores (Cohen d = 0.8 vs. 0.3), and PTSD symptoms (Cohen d = 1.1 vs. 0.3) [76]. Krakow et al. [77] also evaluated the efficacy of imagery rehearsal therapy in a sample of incarcerated adolescent girls who had experienced childhood sexual abuse and found generally similar results. These results suggest that imagery rehearsal therapy may be an effective method to treat patients suffering from nightmares and sleep disorders who have a history of ACEs. Further research is needed on the effectiveness of imagery rehearsal therapy among different populations and at different times throughout the life course.
In addition to the development of trauma-informed care, there are several important gaps in the research that should be addressed in future research initiatives. First, there is a need for a carefully designed longitudinal analysis of the relationship between ACEs, resilient characteristics, and adult sleep to avoid recall bias and to better disentangle psychiatric from sleep disorders. Second, because the research surrounding gender differences in the association between ACEs and sleep disorders currently conflicts, more research is needed to further understand disparities due to gender. Finally, to date, only one study has evaluated racial/ethnic disparities in the association between ACEs and adult sleep disorders and provides evidence that such disparities exist [50]. Future research should investigate this hypothesis because of differences in the burden of childhood abuse among different racial/ethnic groups [50]. Evidence emerging from clinical epidemiologic studies adopting more rigorous study designs and analytical approaches will allow for improved understandings of the relationship between ACEs and sleep disorders in adulthood; and will facilitate the identification of treatment approaches to mitigate the burden of sleep disorders among survivors of childhood adversity.
Highlights.
Multiple studies have identified associations between ACEs and sleep disorders.
Few studies have assessed ACEs and sleep disorders in women.
Women with a history of ACEs appear to have high burden of sleep disorders.
Longitudinal studies of mediators of ACEs-sleep disorders associations are needed.
Acknowledgements
This research was supported by grants from the National Institutes of Health (the Eunice Kennedy Shriver Institute of Child Health and Human Development (NICHD): R01-HD-059835; and the National Center for Research Resources (NCRR)/ National Center for Advancing Translational Sciences (NCATS): 8UL1TR000170-07).
Abbreviations
- ACEs
adverse childhood experiences
- aOR
adjusted odds ratio
- CI
confidence interval
- CRH
corticotropin-releasing hormone
- CTQ
Childhood Trauma Questionnaire
- EEG
electroencephalography
- HPA
hypothalamic-pituitary-adrenal
- IBS
irritable bowel syndrome
- OR
odds ratio
- PSG
polysomnography
- PSQI
Pittsburgh Sleep Quality Index
- PTSD
post-traumatic stress disorder
- REM
rapid eye movement
- THQ
Trauma History Questionnaire
- TSC
Trauma Symptom Checklist
- VBS
violent behavior during sleep
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256:174–86. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. 2009;37:389–96. doi: 10.1016/j.amepre.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 3.Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82:217–25. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 4.Finkelhor D, Turner H, Ormrod R, Hamby SL. Violence, abuse, and crime exposure in a national sample of children and youth. Pediatrics. 2009;124:1411–23. doi: 10.1542/peds.2009-0467. [DOI] [PubMed] [Google Scholar]
- 5.Finkelhor D, Turner HA, Shattuck A, Hamby SL. Violence, crime, and abuse exposure in a national sample of children and youth: an update. JAMA Pediatr. 2013;167:614–21. doi: 10.1001/jamapediatrics.2013.42. [DOI] [PubMed] [Google Scholar]
- 6.Anda RF, Brown DW, Felitti VJ, Bremner JD, Dube SR, Giles WH. Adverse childhood experiences and prescribed psychotropic medications in adults. Am J Prev Med. 2007;32:389–94. doi: 10.1016/j.amepre.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation. 2004;110:1761–6. doi: 10.1161/01.CIR.0000143074.54995.7F. [DOI] [PubMed] [Google Scholar]
- 8.Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addict Behav. 2002;27:713–25. doi: 10.1016/s0306-4603(01)00204-0. [DOI] [PubMed] [Google Scholar]
- 9.Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111:564–72. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- 10.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 11.Goodwin RD, Stein MB. Association between childhood trauma and physical disorders among adults in the United States. Psychol Med. 2004;34:509–20. doi: 10.1017/s003329170300134x. [DOI] [PubMed] [Google Scholar]
- 12.McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, et al. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA. 1997;277:1362–8. [PubMed] [Google Scholar]
- 13.Spertus IL, Yehuda R, Wong CM, Halligan S, Seremetis SV. Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice. Child Abuse Negl. 2003;27:1247–58. doi: 10.1016/j.chiabu.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Center for Substance Abuse T. Trauma-Informed Care in Behavioral Health Services. Substance Abuse and Mental Health Services Administration (US); Rockville (MD): 2014. SAMHSA/CSAT Treatment Improvement Protocols. [PubMed] [Google Scholar]
- 15.Colten HR, Altevogt BM. Sleep disorders and sleep deprivation: an unmet public health problem. Institute of Medicine: National Academies Press; Washington, DC: 2006. Institute of Medicine Committee on Sleep Medicine and Research. [PubMed] [Google Scholar]
- 16.Davies SK, Ang JE, Revell VL, Holmes B, Mann A, Robertson FP, et al. Effect of sleep deprivation on the human metabolome. Proc Natl Acad Sci U S A. 2014;111:10761–6. doi: 10.1073/pnas.1402663111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uehli K, Miedinger D, Bingisser R, Durr S, Holsboer-Trachsler E, Maier S, et al. Sleep quality and the risk of work injury: a Swiss case-control study. J Sleep Res. 2014 doi: 10.1111/jsr.12146. doi: 10.1111/jsr.12146. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Combs K, Smith PJ, Sherwood A, Hoffman B, Carney RM, Freedland K, et al. Impact of sleep complaints and depression outcomes among participants in the standard medical intervention and long-term exercise study of exercise and pharmacotherapy for depression. J Nerv Ment Dis. 2014;202:167–71. doi: 10.1097/NMD.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 19.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–9. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 21.Chapman DP, Liu Y, Presley-Cantrell LR, Edwards VJ, Wheaton AG, Perry GS, et al. Adverse childhood experiences and frequent insufficient sleep in 5 U.S. States, 2009: a retrospective cohort study. BMC Public Health. 2013;13:3. doi: 10.1186/1471-2458-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee C, Tsenkova V, Carr D. Childhood trauma and metabolic syndrome in men and women. Soc Sci Med. 2014;105:122–30. doi: 10.1016/j.socscimed.2014.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noll JG, Trickett PK, Susman EJ, Putnam FW. Sleep disturbances and childhood sexual abuse. J Pediatr Psychol. 2006;31:469–80. doi: 10.1093/jpepsy/jsj040. [DOI] [PubMed] [Google Scholar]
- 24.Lindberg E, Janson C, Gislason T, Bjornsson E, Hetta J, Boman G. Sleep disturbances in a young adult population: can gender differences be explained by differences in psychological status? Sleep. 1997;20:381–7. doi: 10.1093/sleep/20.6.381. [DOI] [PubMed] [Google Scholar]
- 25.Chambers E, Belicki K. Using sleep dysfunction to explore the nature of resilience in adult survivors of childhood abuse or trauma. Child Abuse Negl. 1998;22:753–8. doi: 10.1016/s0145-2134(98)00059-3. [DOI] [PubMed] [Google Scholar]
- 26.Agargun MY, Kara H, Ozer OA, Kiran U, Selvi Y, Kiran S. Sleep-related violence, dissociative experiences, and childhood traumatic events. Sleep Hypn. 2002;4:52–7. [Google Scholar]
- 27.Agargun MY, Kara H, Ozer OA, Selvi Y, Kiran U, Kiran S. Nightmares and dissociative experiences: The key role of childhood traumatic events. Psychiatry Clin Neurosci. 2003;57:139–45. doi: 10.1046/j.1440-1819.2003.01093.x. [DOI] [PubMed] [Google Scholar]
- 28.Haj-Yahia MM, de Zoysa P. Rates and psychological effects of exposure to family violence among Sri Lankan university students. Child Abuse Negl. 2008;32:994–1002. doi: 10.1016/j.chiabu.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Gal G, Levav I, Gross R. Psychopathology among adults abused during childhood or adolescence: results from the Israel-based World Mental Health Survey. J Nerv Ment Dis. 2011;199:222–9. doi: 10.1097/NMD.0b013e31820c7543. [DOI] [PubMed] [Google Scholar]
- 30.Chapman DP, Wheaton AG, Anda RF, Croft JB, Edwards VJ, Liu Y, et al. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. 2011;12:773–9. doi: 10.1016/j.sleep.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 31.Greenfield EA, Lee C, Friedman EL, Springer KW. Childhood abuse as a risk factor for sleep problems in adulthood: evidence from a U.S. national study. Ann Behav Med. 2011;42:245–56. doi: 10.1007/s12160-011-9285-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Poon CY, Knight BG. Impact of childhood parental abuse and neglect on sleep problems in old age. J Gerontol B Psychol Sci Soc Sci. 2011;66:307–10. doi: 10.1093/geronb/gbr003. [DOI] [PubMed] [Google Scholar]
- 33.Ramsawh HJ, Ancoli-Israel S, Sullivan SG, Hitchcock CA, Stein MB. Neuroticism mediates the relationship between childhood adversity and adult sleep quality. Behav Sleep Med. 2011;9:130–43. doi: 10.1080/15402002.2011.583895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gregory AM, Caspi A, Moffitt TE, Poulton R. Family conflict in childhood: a predictor of later insomnia. Sleep. 2006;29:1063–7. doi: 10.1093/sleep/29.8.1063. [DOI] [PubMed] [Google Scholar]
- 35.Koskenvuo K, Hublin C, Partinen M, Paunio T, Koskenvuo M. Childhood adversities and quality of sleep in adulthood: A population-based study of 26,000 Finns. Sleep Med. 2010;11:17–22. doi: 10.1016/j.sleep.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 36.Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, et al. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse Negl. 2004;28:771–84. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 37.Insana SP, Kolko DJ, Germain A. Early-life trauma is associated with rapid eye movement sleep fragmentation among military veterans. Biol Psychol. 2012;89:570–9. doi: 10.1016/j.biopsycho.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schafer V, Bader K. Relationship between early-life stress load and sleep in psychiatric outpatients: a sleep diary and actigraphy study. Stress Health. 2013;29:177–89. doi: 10.1002/smi.2438. [DOI] [PubMed] [Google Scholar]
- 39.McNally RJ, Clancy SA. Sleep paralysis in adults reporting repressed, recovered, or continuous memories of childhood sexual abuse. J Anxiety Disord. 2005;19:595–602. doi: 10.1016/j.janxdis.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 40.Abrams MP, Mulligan AD, Carleton RN, Asmundson GJ. Prevalence and correlates of sleep paralysis in adults reporting childhood sexual abuse. J Anxiety Disord. 2008;22:1535–41. doi: 10.1016/j.janxdis.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 41.Bader K, Schafer V, Schenkel M, Nissen L, Schwander J. Adverse childhood experiences associated with sleep in primary insomnia. J Sleep Res. 2007;16:285–96. doi: 10.1111/j.1365-2869.2007.00608.x. [DOI] [PubMed] [Google Scholar]
- 42.Bader K, Schafer V, Schenkel M, Nissen L, Kuhl HC, Schwander J. Increased nocturnal activity associated with adverse childhood experiences in patients with primary insomnia. J Nerv Ment Dis. 2007;195:588–95. doi: 10.1097/NMD.0b013e318093ed00. [DOI] [PubMed] [Google Scholar]
- 43.Heath V, Bean R, Feinauer L. Severity of childhood sexual abuse: Symptom differences between men and women. Am J Fam Ther. 1996;24:305–14. [Google Scholar]
- 44.Elliott DM, Briere J. Sexual abuse trauma among professional women: Validating the trauma symptom checklist-40 (TSC-40). Child Abuse Negl. 1992;16:391–8. doi: 10.1016/0145-2134(92)90048-v. [DOI] [PubMed] [Google Scholar]
- 45.Hulme PA. Symptomatology and health care utilization of women primary care patients who experienced childhood sexual abuse. Child Abuse Negl. 2000;24:1471–84. doi: 10.1016/s0145-2134(00)00200-3. [DOI] [PubMed] [Google Scholar]
- 46.Kelly U. Intimate partner violence, physical health, posttraumatic stress disorder, depression, and quality of life in latinas. West J Emerg Med. 2010;11:247–51. [PMC free article] [PubMed] [Google Scholar]
- 47.Hairston IS, Waxler E, Seng JS, Fezzey AG, Rosenblum KL, Muzik M. The role of infant sleep in intergenerational transmission of trauma. Sleep. 2011;34:1373–83. doi: 10.5665/SLEEP.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Heitkemper MM, Cain KC, Burr RL, Jun SE, Jarrett ME. Is childhood abuse or neglect associated with symptom reports and physiological measures in women with irritable bowel syndrome? Biol Res Nurs. 2011;13:399–408. doi: 10.1177/1099800410393274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Duval M, McDuff P, Zadra A. Nightmare frequency, nightmare distress, and psychopathology in female victims of childhood maltreatment. J Nerv Ment Dis. 2013;201:767–72. doi: 10.1097/NMD.0b013e3182a214a1. [DOI] [PubMed] [Google Scholar]
- 50.Barker-Collo SL. Reported symptomatology of native Canadian and Caucasian females sexually abused in childhood -A comparison. J Interpers Violence. 1999;14:747–60. [Google Scholar]
- 51.Zhabenko N, Wojnar M, Brower KJ. Prevalence and correlates of insomnia in a Polish sample of alcohol-dependent patients. Alcohol Clin Exp Res. 2012;36:1600–7. doi: 10.1111/j.1530-0277.2012.01771.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brower KJ, Wojnar M, Sliwerska E, Armitage R, Burmeister M. PER3 polymorphism and insomnia severity in alcohol dependence. Sleep. 2012;35:571–7. doi: 10.5665/sleep.1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cuddy MA, Belicki K. Nightmare frequency and related sleep disturbance as indicators of a history of sexual abuse. Dreaming. 1992;2:15–22. [Google Scholar]
- 54.Pigeon WR, May PE, Perlis ML, Ward EA, Lu N, Talbot NL. The effect of interpersonal psychotherapy for depression on insomnia symptoms in a cohort of women with sexual abuse histories. J Trauma Stress. 2009;22:634–8. doi: 10.1002/jts.20456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spilsbury JC. Sleep as a mediator in the pathway from violence-induced traumatic stress to poorer health and functioning: a review of the literature and proposed conceptual model. Behav Sleep Med. 2009;7:223–44. doi: 10.1080/15402000903190207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chu JA. The revictimization of adult women with histories of childhood abuse. J Psychother Pract Res. 1992;1:259–69. [PMC free article] [PubMed] [Google Scholar]
- 57.Fisher H, Morgan C, Dazzan P, Craig TK, Morgan K, Hutchinson G, et al. Gender differences in the association between childhood abuse and psychosis. Br J Psychiatry. 2009;194:319–25. doi: 10.1192/bjp.bp.107.047985. [DOI] [PubMed] [Google Scholar]
- 58.Haatainen KM, Tanskanen A, Kylma J, Honkalampi K, Koivumaa-Honkanen H, Hintikka J, et al. Gender differences in the association of adult hopelessness with adverse childhood experiences. Soc Psychiatry Psychiatr Epidemiol. 2003;38:12–7. doi: 10.1007/s00127-003-0598-3. [DOI] [PubMed] [Google Scholar]
- 59.Thurston RC, Bromberger J, Chang Y, Goldbacher E, Brown C, Cyranowski JM, et al. Childhood abuse or neglect is associated with increased vasomotor symptom reporting among midlife women. Menopause. 2008;15:16–22. [PMC free article] [PubMed] [Google Scholar]
- 60.Glod CA. Circadian dysregulation in abused individuals: a proposed theoretical model for practice and research. Arch Psychiatr Nurs. 1992;6:347–55. doi: 10.1016/0883-9417(92)90087-y. [DOI] [PubMed] [Google Scholar]
- 61.Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab. 2005;90:3106–14. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- 62.Vgontzas AN, Bixler EO, Lin HM, Prolo P, Mastorakos G, Vela-Bueno A, et al. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: clinical implications. J Clin Endocrinol Metab. 2001;86:3787–94. doi: 10.1210/jcem.86.8.7778. [DOI] [PubMed] [Google Scholar]
- 63.Arborelius L, Owens MJ, Plotsky PM, Nemeroff CB. The role of corticotropin-releasing factor in depression and anxiety disorders. J Endocrinol. 1999;160:1–12. doi: 10.1677/joe.0.1600001. [DOI] [PubMed] [Google Scholar]
- 64.Elzinga BM, Spinhoven P, Berretty E, de Jong P, Roelofs K. The role of childhood abuse in HPA-axis reactivity in Social Anxiety Disorder: a pilot study. Biol Psychol. 2010;83:1–6. doi: 10.1016/j.biopsycho.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 65.Nicolson NA, Davis MC, Kruszewski D, Zautra AJ. Childhood maltreatment and diurnal cortisol patterns in women with chronic pain. Psychosom Med. 2010;72:471–80. doi: 10.1097/PSY.0b013e3181d9a104. [DOI] [PubMed] [Google Scholar]
- 66.Videlock EJ, Adeyemo M, Licudine A, Hirano M, Ohning G, Mayer M, et al. Childhood trauma is associated with hypothalamic-pituitary-adrenal axis responsiveness in irritable bowel syndrome. Gastroenterology. 2009;137:1954–62. doi: 10.1053/j.gastro.2009.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, et al. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA. 2000;284:592–7. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- 68.Carpenter LL, Tyrka AR, Ross NS, Khoury L, Anderson GM, Price LH. Effect of childhood emotional abuse and age on cortisol responsivity in adulthood. Biol Psychiatry. 2009;66:69–75. doi: 10.1016/j.biopsych.2009.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.MacMillan HL, Georgiades K, Duku EK, Shea A, Steiner M, Niec A, et al. Cortisol response to stress in female youths exposed to childhood maltreatment: results of the youth mood project. Biol Psychiatry. 2009;66:62–8. doi: 10.1016/j.biopsych.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bicanic IAE, Postma RM, Sinnema G, De Roos C, Olff M, Van Wesel F, et al. Salivary cortisol and dehydroepiandrosterone sulfate in adolescent rape victims with post traumatic stress disorder. Psychoneuroendocrinology. 2013;38:408–15. doi: 10.1016/j.psyneuen.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 71.Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14:19–31. doi: 10.1016/j.smrv.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 72.Perlis ML, Giles DE, Mendelson WB, Bootzin RR, Wyatt JK. Psychophysiological insomnia: the behavioural model and a neurocognitive perspective. J Sleep Res. 1997;6:179–88. doi: 10.1046/j.1365-2869.1997.00045.x. [DOI] [PubMed] [Google Scholar]
- 73.Bader K, Schafer V, Nissen L, Schenkel M. Heightened beta EEG activity during nonrapid eye movement sleep in primary insomnia patients with reports of childhood maltreatment. J Clin Neurophysiol. 2013;30:188–98. doi: 10.1097/WNP.0b013e3182767c4a. [DOI] [PubMed] [Google Scholar]
- 74.Logan-Greene P, Green S, Nurius PS, Longhi D. Distinct contributions of adverse childhood experiences and resilience resources: a cohort analysis of adult physical and mental health. Soc Work Health Care. 2014;53(8):776–97. doi: 10.1080/00981389.2014.944251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sher L. The concept of post-traumatic mood disorder and its implications for adolescent suicidal behavior. Minerva Pediatr. 2008;60:1393–9. [PubMed] [Google Scholar]
- 76.Krakow B, Hollifield M, Johnston L, Koss M, Schrader R, Warner TD, et al. Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder: a randomized controlled trial. JAMA. 2001;286:537–45. doi: 10.1001/jama.286.5.537. [DOI] [PubMed] [Google Scholar]
- 77.Krakow B, Sandoval D, Schrader R, Keuhne B, McBride L, Yau CL, et al. Treatment of chronic nightmares in adjudicated adolescent girls in a residential facility. J Adolesc Health. 2001;29:94–100. doi: 10.1016/s1054-139x(00)00195-6. [DOI] [PubMed] [Google Scholar]