Abstract
Background
Patient navigation may reduce cancer disparities associated with socioeconomic status (SES) and household factors. We examined whether these factors were associated with delays in diagnostic resolution among patients with cancer screening abnormalities and whether patient navigation ameliorated these delays.
Methods
We analyzed data from five of ten centers from the NCI Patient Navigation Research Program that collected SES and household data on employment, income, education, housing, marital status, and household composition. The primary outcome was time to diagnostic resolution following a cancer screening abnormality. We fit separate adjusted Cox proportional hazard models for each SES and household factor and included an interaction between that factor and intervention status.
Results
Among 3777 participants (n=1968 control, n=1809 navigation intervention), 91% were women, with a mean age of 44 years, and 43% were Hispanic, 28% White, and 27% African American. Within the control arm, the unemployed experienced longer time to resolution than the full-time employed (HR=0.85, p=0.02). Renters (HR=0.81, p=0.02) and those with other (i.e., unstable) housing (HR=0.60, p<0.001) had delays compared to homeowners. Never married (HR=0.70, p<0.001) and previously married participants (HR=0.85, p=0.03) had longer time to care than married participants. There were no differences in time to diagnostic resolution by any of these variables within the navigation intervention arm.
Conclusions
Delays in diagnostic resolution exist by employment, housing type, and marital status. Patient navigation eliminated these disparities in our study sample. Our findings demonstrate the value of providing patient navigation to patients at high risk for delays in cancer care.
Keywords: Patient navigation, healthcare disparities, early detection of cancer, breast neoplasms, prostatic neoplasms, colonic neoplasms, uterine cervical neoplasms
Disparities exist in cancer survival by socioeconomic status (SES) and household factors. Race/ethnicity, income, education, employment status, and marital status are all associated with later stage at cancer diagnosis1-4 and cancer survival rates.1,3-6 While some aspects of these disparities may reflect biological differences, a significant contributor to cancer health disparities are barriers to timely access to care.
Patient navigation programs are increasingly being utilized to address disparities in health care generally and in care across the cancer continuum specifically.7,8 In particular, patient navigation programs have helped to improve screening rates9,10 and time to diagnostic resolution after abnormal screening in several different patient populations.11-14 Successful patient navigation includes both instrumental interventions to identify and meet patients’ needs (e.g., insurance, transportation, information) and relationship interventions to enhance the patient-navigator and patient-clinician interactions.7
Since lower SES is specifically associated with poorer outcomes, we hypothesized that patient navigation would be specifically beneficial to this low SES group. We performed a secondary analysis of data collected by the multicenter Patient Navigation Research Program (PNRP) to determine whether SES and household factors were associated with delays in time to diagnostic resolution among patients with an abnormal cancer screening test who did not receive patient navigation. Our second objective was to determine whether patient navigation could eliminate these disparities in outcomes associated with SES and household factors.
Methods
Data for this analysis come from five of ten PNRP centers that collected supplemental data on SES and household factors.15 The PNRP study, conducted from 2007 to 2011, examined whether patient navigation reduced the time to diagnostic resolution following an abnormal screening test for breast, cervical, colorectal, and prostate cancer. Navigators used the Care Management Model16 to identify barriers to recommended care, develop strategies to address these barriers, and track participants through the steps in their medical evaluation, with the focus on timely completion of the diagnostic evaluation. Navigators maintained contact (e.g., telephone, mail, in-person meetings) with participants, their families, and their health care providers, along with social service agencies, where appropriate. Examples of navigation services included arranging financial support, arranging transportation and childcare, coordinating care among providers, arranging interpreter services, ensuring that medical records were available, linking to community resources and providing other services to overcome access barriers.15
Study participants with the following abnormal cancer screening tests were included: abnormal clinical breast exam or abnormal imaging (BIRADS 0, 4, or 5), high and low grade cervical intraepithelial neoplasia, abnormal stool hemoccult testing, and abnormal prostate specific antigen (PSA) or PSA velocity.15 Because of community based-participatory research methods, centers did not use the same method of subject allocation into the control and intervention arms, with some using individual randomization, some using group randomization and some using non-randomized allocation methods.13,15 Institutional Review Boards at each center approved the study.
Demographic data were obtained from either participant self-report or clinical registration data. Race and ethnicity were collapsed into a single categorical variable: non-Hispanic White, non-Hispanic Black/African-American, Hispanic, and Other. Health insurance coverage at the time of study entry was hierarchically categorized into private, public, and no insurance coverage. Study centers also collected supplemental data from participants on the following SES and household factors: employment (full time, part time, unemployed); household income (<$10,000, $10,000 to $19,999, $20,000 to $49,999, $50,000+); educational attainment (<high school, high school diploma, some college, college graduate); housing (own, rent, “other,” which included those without stable or permanent housing); marital status (currently married, previously married, never married); household size; and number of dependents. An additional variable for non-dependent household size was created by subtracting the number of dependents from the household size. All available data were used for analyses of these SES and household variables.
Statistical Analysis
Baseline demographic, clinical, SES, and household characteristics were described using means (standard deviations, SD), or frequencies (percentages). These characteristics were compared across study arm using two-sample t-tests or chi-squared tests.
The outcome of interest was time to diagnostic resolution of the screening abnormality, defined as the time from the date of the initial screening abnormality to the date when the final definitive diagnostic test or evaluation was completed. Participants were censored at 365 days if they did not reach diagnostic resolution. We calculated the median time (25th-75th percentile) to diagnostic resolution for each SES and household factor by navigation arm and compared the levels within each arm using the log-rank test. We present Kaplan-Meier curves for two sample SES and household variables (marital status and household status) by navigation arm. A horizontal line is included when 50% reach diagnostic resolution and two vertical lines are included for 90 and 365 days.
Multivariable Cox proportional hazards models were fit using data from both the control and intervention arm for each SES and household variable, adjusting for sex, age, cancer type, race/ethnicity, and health insurance, stratifying by center of care. Interaction terms between patient navigation arm and the SES or household variable were included in these models to assess for effect modification of patient navigation. We calculated adjusted hazard ratios (HRs) for each SES and household factor by patient navigation arm using the estimates for the interaction terms. The proportional hazards assumption was assessed by testing for interactions between the covariates and log time and visually inspecting the plots of log(−log(survival)) versus log of survival time. To assess the impact of violations in the proportional hazards assumption, we subsetted the data into the patient navigation arm and control arm. We calculated adjusted HRs for each SES and household factor in these subsetted datasets. Statistical tests were two sided with an alpha of 0.05 and analyses were conducted using Stata Version 10.0 (2007).
Results
Among the analytic sample of 3777, the average age was 44 years (SD=14) and 91% of participants were women (Table 1). Hispanic was the most common race/ethnicity (43%), followed by non-Hispanic White (28%), non-Hispanic Black/African American (27%), and other (2%). Nearly equal proportions of participants were uninsured (40%) and publicly insured (37%) while only 23% were privately insured. More than half (60%) of participants had breast cancer screening abnormalities, followed by cervical (24%), colorectal (13%), and prostate (3%). Forty-eight percent were in the patient navigation arm and 52% were in the control arm. There were statistically significant differences in sex, age, race/ethnicity, health insurance, cancer type, and study center across the intervention and control arms, reflecting the differences in intervention allocation.
Table 1.
Demographic, socioeconomic, and household characteristics by patient navigation arm: National Patient Navigation Research Program
| Overall (N=3777) | Control Arm (N=1968) |
Navigation Arm (N=1809) |
|
|---|---|---|---|
| Demographic and Socioeconomic Characteristics | |||
| Female sex, n (%)* | 3421 (91%) | 1982 (91%) | 1881 (93%) |
| Mean age—yr, mean (SD) | 44.0 (14.3) | 44.9 (14.7) | 43.0 (13.8) |
| Race/ethnicity, n (%)*** | |||
| Non-Hispanic White | 1048 (28%) | 537 (28%) | 511 (28%) |
| Non-Hispanic Black/African American |
1004 (27%) | 569 (30%) | 435 (24%) |
| Hispanic | 1580 (43%) | 751 (39%) | 829 (46%) |
| Other | 85 (2%) | 52 (3%) | 33 (2%) |
| Health insurance, n (%)*** | |||
| Uninsured | 1501 (40%) | 694 (36%) | 807 (45%) |
| Public | 1386 (37%) | 795 (41%) | 591 (33%) |
| Private | 847 (23%) | 459 (24%) | 388 (22%) |
| Cancer type, n (%)* | |||
| Breast | 2260 (60%) | 1136 (58%) | 1124 (62%) |
| Cervical | 891 (24%) | 488 (25%) | 403 (22%) |
| Colorectal | 497 (13%) | 278 (14%) | 219 (12%) |
| Prostate | 129 (3%) | 66 (3%) | 63 (3%) |
| Sites, n (%)*** | |||
| A | 245 (6%) | 100 (5%) | 145 (8%) |
| B | 864 (23%) | 510 (26%) | 354 (20%) |
| D | 798 (21%) | 412 (21%) | 386 (21%) |
| E | 610 (16%) | 271 (14%) | 339 (19%) |
| G | 1260 (33%) | 675 (34%) | 585 (32%) |
| Socioeconomic and Household Characteristics | |||
| Employment, n (%)*** | |||
| Unemployed | 1785 (57%) | 959 (61%) | 826 (53%) |
| Part-time | 420 (13%) | 172 (11%) | 248 (16%) |
| Full-time | 914 (29%) | 439 (28%) | 475 (31%) |
| Household income, n (%) | |||
| < $10K | 1124 (40%) | 496 (41%) | 628 (39%) |
| $10K - < $20K | 733 (26%) | 315 (26%) | 418 (26%) |
| $20K - < $50K | 594 (21%) | 244 (20%) | 350 (22%) |
| $50K + | 343 (12%) | 147 (12%) | 196 (12%) |
| Education, n (%)*** | |||
| < High school | 910 (34%) | 327 (29%) | 583 (37%) |
| High school diploma | 689 (26%) | 279 (25%) | 410 (26%) |
| Some college | 624 (23%) | 291 (26%) | 333 (21%) |
| College graduate | 468 (17%) | 218 (20%) | 250 (16%) |
| Housing, n (%) | |||
| Own | 651 (32%) | 277 (32%) | 374 (31%) |
| Rent | 1099 (53%) | 460 (53%) | 639 (53%) |
| Other | 312 (15%) | 124 (14%) | 188 (16%) |
| Marital Status, n (%)*** | |||
| Currently married | 1340 (37%) | 636 (34%) | 704 (41%) |
| Previously married | 776 (22%) | 418 (22%) | 358 (21%) |
| Never married | 1481 (41%) | 808 (43%) | 673 (39%) |
| Household size, n (%) | |||
| One | 450 (22%) | 193 (22%) | 257 (21%) |
| Two | 593 (29%) | 247 (29%) | 346 (29%) |
| Three or more | 1027 (50%) | 423 (49%) | 604 (50%) |
| Dependents, n (%) | |||
| None | 592 (46%) | 222 (49%) | 370 (45%) |
| One | 278 (22%) | 103 (23%) | 175 (21%) |
| Two or more | 408 (32%) | 131 (29%) | 131 (29%) |
| Non-dependent household size, n (%) |
|||
| One | 526 (42%) | 184 (41%) | 342 (42%) |
| Two | 438 (35%) | 153 (34%) | 285 (35%) |
| Three or more | 294 (23%) | 109 (24%) | 185 (23%) |
Comparing control to navigation arm:
for P < 0.05
for P < 0.01
for P < 0.001
Values demonstrate a low SES sample with more than half of participants being unemployed (57%), 40% having an income less than $10,000, and 34% having less than a high school diploma (Table 1). More than half of participants reported renting as their housing arrangement (53%), 32% reported owning their home, and the remaining 15% reported other, including unstable housing. Slightly over 60% were not currently married, 50% had a household size of three or more, 32% had two or more dependents, and 23% had three or more non-dependent household members. Regarding differences across arms, the control group had more participants who were unemployed (p<0.001), had higher educational attainment (p<0.001), and were never married (p<0.001) than the navigation arm.
Time to Diagnostic Resolution by Study Arm
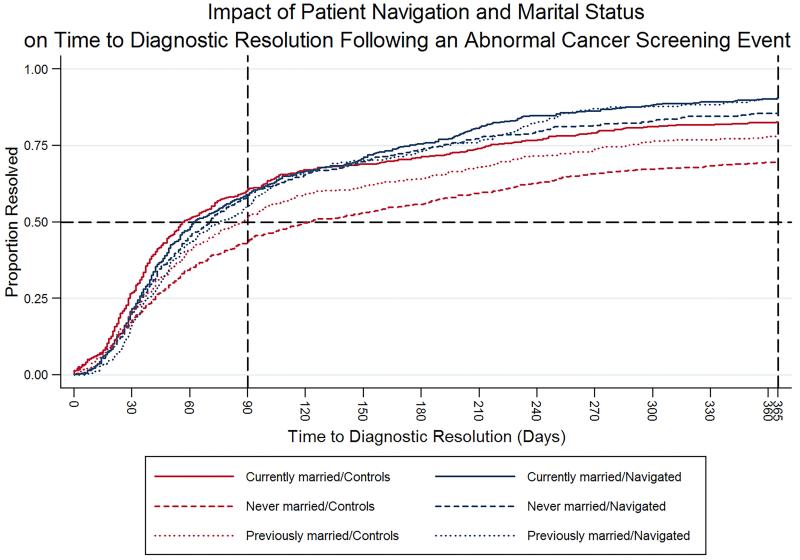
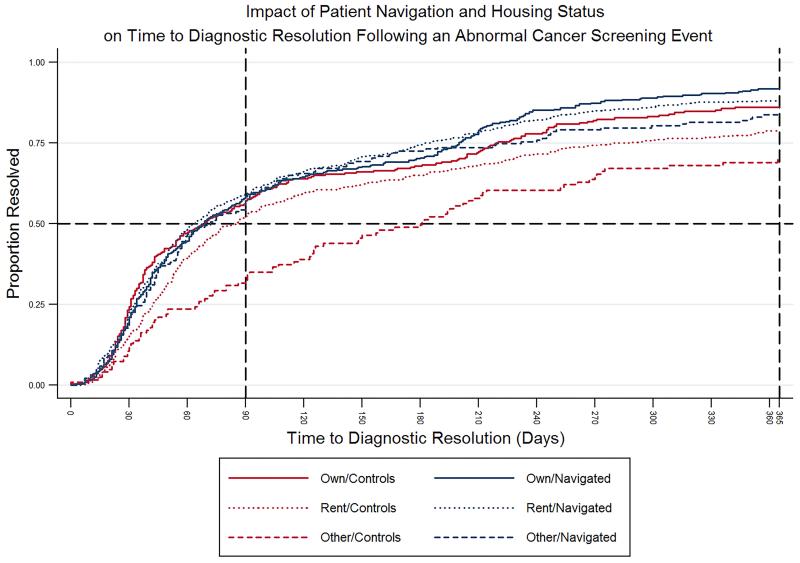
By 365 days, 3057 (80.9%) of participants had reached diagnostic resolution. Overall, the median number of days to diagnostic resolution in the control arm was greater than the navigation arm (86 vs. 69 days; p<0.001). Table 2 provides the unadjusted median time to diagnostic resolution for each SES and household factor by study arm. Within the control arm there were significant differences in delays in time to resolution by underemployment (p=0.01), low income (p=0.04), educational attainment (p=0.05), non-homeownership (p<0.001), and non-married status (p<0.001). There were significant differences in median time to resolution by income (p=0.02) in the navigation arm. Figures 1 and 2 show Kaplan Meier plots for marital status and household status, respectively, by navigation arm.
Table 2.
Median time to diagnostic resolution by patient navigation arm: National Patient Navigation Research Program
| Median Days to Resolution in Control Arm (25th-75th percentile) |
Log-rank test p- value |
Median Days to Resolution in Navigation Arm (25th-75th percentile) |
Log-rank test p- value |
|
|---|---|---|---|---|
| Employment | 0.01 | 0.06 | ||
| Full-time | 69 (33, 249) | 70 (37, 192) | ||
| Part-time | 77 (32, 227) | 63 (35, 149) | ||
| Unemployed | 97 (36, --) | 73 (36, 203) | ||
| Household Income | 0.04 | 0.02 | ||
| < $10,000 | 89 (38, 306) | 75 (37, 204) | ||
| $10,000 – $19,999 | 70 (32, 270) | 64 (34, 165) | ||
| $20,000 - $49,999 | 75 (32, 226) | 60 (34, 158) | ||
| $50,000 + | 57 (33, 220) | 70 (34, 202) | ||
| Education | 0.05 | 0.12 | ||
| < High school | 85 (32, 327) | 63 (33, 163) | ||
| High school diploma | 72 (35, 267) | 69 (36, 189) | ||
| Some college | 100 (40, 332) | 77 ( 37, 202) | ||
| College graduate | 70 (32, 231) | 62 (34, 196) | ||
| Housing | <0.001 | 0.27 | ||
| Own | 69 (31, 220) | 69 (34, 200) | ||
| Rent | 85 (42, 288) | 64 (32, 183) | ||
| Other | 181 (65, --) | 72 (37, 232) | ||
| Marital Status | <0.001 | 0.12 | ||
| Currently married | 57 (28, 216) | 62 (34, 174) | ||
| Previously married | 87 (35, 287) | 76 (38, 192) | ||
| Never married | 122 (42, --) | 70 (35, 191) | ||
| Household Size | 0.31 | 0.12 | ||
| One | 100 (44, 316) | 81 (41, 222) | ||
| Two | 77 (35, 276) | 70 (34, 191) | ||
| 3 or more | 87 (37, 238) | 59 (30, 178) | ||
| Dependents | 0.27 | 0.51 | ||
| None | 75 (36, 223) | 59 (30, 189) | ||
| One | 76 (39, 258) | 59 (33, 208) | ||
| 2 or more | 90 (47, 243) | 52 (28, 161) | ||
| Non-dependent household size |
0.18 | 0.83 | ||
| One | 87 (40, 232) | 54 (30, 186) | ||
| Two | 62 (35, 216) | 62 (32, 194) | ||
| 3 or more | 106 (54, 243) | 55 (29, 146) |
Figure 1.
Kaplan-Meier curves for impact of patient navigation and marital status on time to diagnostic resolution following an abnormal cancer screening event.
Figure 2.
Kaplan-Meier curves for impact of patient navigation and housing status on time to diagnostic resolution following an abnormal cancer screening event.
Adjusted Analyses and Impact of Patient Navigation
Assessment of the proportional hazards assumption showed that none of the interactions between SES or household factors and log time were significant. Although the interactions between patient navigation and log time were significant in all models, inspection of the log(−log(survival)) plots did not indicate severe proportional hazards violations.
In the multivariable-adjusted models, several SES and household factors were significantly associated with time to diagnostic resolution in the control arm (Table 3). The unemployed experienced longer time to resolution than those employed full-time (HR=0.85; 95% CI: 0.74, 0.98). Renters (HR=0.81; 95% CI: 0.68, 0.96) and those with other housing, including unstable housing, (HR=0.60; 95% CI: 0.46, 0.78) had delays in care compared to homeowners. Never married (HR=0.70; 95% CI: 0.61, 0.80) and previously married participants (HR=0.85; 95% CI: 0.74, 0.98) had longer time to care than currently married participants. There were no statistically significant differences in time to resolution by income, education, household size, and non-dependent household size in the control arm.
Table 3.
Adjusted hazard ratios for time to diagnostic resolution by patient navigation arm: National Patient Navigation Research Program
| Adjusted HR for Control Arm (95% C.I.) |
P value |
Adjusted HR for Navigation Arm (95% C.I.) |
P value |
Global p value for interaction term |
|
|---|---|---|---|---|---|
| Employment (N=3052) | 0.17 | ||||
| Full time | Ref. | Ref. | |||
| Part time | 1.00 (0.82, 1.23) | 0.99 | 1.14 (0.97, 1.35) | 0.12 | |
| Unemployed | 0.85 (0.74, 0.98) | 0.02 | 0.97 (0.85, 1.10) | 0.65 | |
| Household Income (N=2736) |
0.06 | ||||
| < $10,000 | 0.81 (0.64, 1.02) | 0.08 | 1.02 (0.82, 1.26) | 0.89 | |
| $10,000 – $19,999 | 0.90 (0.71, 1.16) | 0.43 | 1.12 (0.89, 1.40) | 0.34 | |
| $20,000 - $49,999 | 0.87 (0.68, 1.10) | 0.25 | 1.15 (0.94, 1.42) | 0.17 | |
| $50,000 + | Ref. | Ref. | |||
| Education (N=2648) | 0.20 | ||||
| < High school | 0.82 (0.67, 1.02) | 0.07 | 0.97 (0.81, 1.17) | 0.77 | |
| High school diploma | 0.91 (0.74, 1.12) | 0.39 | 1.02 (0.84, 1.23) | 0.86 | |
| Some college | 0.83 (0.68, 1.01) | 0.06 | 0.97 (0.80, 1.16) | 0.73 | |
| College graduate | Ref. | Ref. | |||
| Housing (N=2040) | |||||
| Own | Ref. | Ref. | 0.001 | ||
| Rent | 0.81 (0.68, 0.96) | 0.02 | 1.07 (0.92, 1.24) | 0.41 | |
| Other | 0.60 (0.46, 0.78) | <0.001 | 0.95 (0.77, 1.18) | 0.64 | |
| Marital Status (N=3515) | |||||
| Currently married | Ref. | Ref. | 0.001 | ||
| Previously married | 0.85 (0.74, 0.98) | 0.03 | 1.03 (0.89, 1.18) | 0.71 | |
| Never married | 0.70 (0.61, 0.80) | <0.001 | 1.00 (0.88, 1.13) | 0.98 | |
| Household Size (N=2048) | |||||
| One | Ref. | Ref. | 0.98 | ||
| Two | 1.08 (0.87, 1.34) | 0.51 | 1.01 (0.85, 1.21) | 0.88 | |
| 3 or more | 0.91 (0.75, 1.12) | 0.38 | 0.97 (0.83, 1.15) | 0.76 | |
| Dependents (N=1256) | |||||
| None | Ref. | Ref. | 0.19 | ||
| One | 0.91 (0.70, 1.19) | 0.50 | 1.01 (0.83, 1.24) | 0.90 | |
| 2 or more | 0.80 (0.62, 1.03) | 0.08 | 1.01 (0.85, 1.21) | 0.91 | |
| Non-dependent household size (N=1236) |
|||||
| One | Ref. | Ref. | 0.93 | ||
| Two | 1.10 (0.87, 1.40) | 0.4 | 0.93 (0.79, 1.11) | 0.44 | |
| 3 or more | 0.80 (0.61, 1.05) | 0.10 | 0.96 (0.79, 1.18) | 0.70 |
Each SES and household model was adjusted for sex, age, cancer type, race/ethnicity, insurance, and includes an interaction between the SES and household variable and patient navigation arm.
The disparities in time to diagnostic resolution observed in the control arm were not observed in the patient navigation arm. We no longer saw statistically significant delays in diagnostic resolution compared to the reference group for unemployed participants (HR=0.97; 95% CI: 0.85, 1.10; p=0.65), renters (HR=1.07; 95% CI: 0.92, 1.24; p=0.41) or those with other housing arrangements (HR=0.95; 95% CI: 0.77, 1.18; p=0.64), and previously married (HR=1.03; 95% CI: 0.89, 1.18; p=0.71) or never married participants (HR=1.00; 95% CI: 0.88, 1.13; p=0.98).
The interaction terms between each of SES and household factors and the study arm (Table 3) show that the effect of marital status and housing status is significantly different by study arm. It confirms that for the control group the delays in resolution are significantly greater for those who are not homeowners or are currently unmarried, while these factors are no longer associated with delays in care for the patient navigation group.
Assessment of the proportional hazards assumption showed that none of the interactions between SES or household factors and log time were significant. Although the interactions between patient navigation and log time were significant in all models, inspection of the log(−log(survival)) plots did not indicate severe proportional hazards violations. The subsetted analyses by patient arm did not provide any HR outside the confidence interval of the models with both control and navigated subjects combined in the single model. Results in the subsetted model were still significant for housing status and marital status, but not unemployment. Since the single model directly addresses the research question, we present this as the final model for our results. We present analyses subsetted by patient navigation arm in Supplementary Table A.
Discussion
In our sample of low income, predominantly minority participants who had an abnormal cancer screening test, delays in timely diagnostic care were associated with SES and household factors and patient navigation eliminated these disparities. Among those without support of a patient navigator, there were delays in diagnostic resolution by unemployment, non-homeownership, and unmarried status. Patient navigation was shown to be effective for the provision of timely care in these disadvantaged groups.
Previous research has shown that disparities in cancer survival exist by SES and household factors, such as employment, education, income, and marital status,1,2 and that these disparities may be partially explained by differences in detection or treatment rates.17-21 Despite interventions to eliminate health disparities in cancer over the past 20 years, these disparities continue to persist.4,22 Our findings within the control arm further support the continued existence of these disparities in cancer care, specifically in timely care after abnormal cancer screening.
Patient navigation programs have become effective tools for addressing cancer disparities by improving screening rates and time to diagnostic resolution. However, most research on patient navigation has focused on the overall averaged effects across patient-level SES and household factors9-13 without examining whether patient navigation is an effect modifier that can mitigate disparities for specific patient groups. In this analysis, we determined that delays in care were mitigated among those participants receiving patient navigation that were identified as being unemployed, non-homeowners, or unmarried.
Kaplan-Meier plots show the clinical impact of patient navigation on time to diagnostic resolution. For example, by 90 days ~60% of the never married group in the navigation arm reached diagnostic resolution, while ~40% of the never married group in the control arm reached resolution. We also observed that 50% of the never married group in the navigation arm reached resolution at 70 days while it took 120 days for the never married group in the control arm to reach 50% resolution. Longer time to diagnostic resolution translates to delays in treatment, which can result in worse prognosis. In fact, previous research has shown that delays >90 days were associated with poorer outcomes, including survival,23 indicating that our observed differences may demonstrate in a clinically meaningful improvement of outcomes.
Patient navigation addresses emotional, informational, and instrumental barriers.24,25 A review of cancer patient navigation identified four major areas in which patient navigators intervene building on the construct of social support: 1) overcoming health system barriers, including coordination, scheduling, and help with paperwork (i.e., instrumental support); 2) providing health education, including written information, discussion, and answering questions (i.e., informational support); 3) addressing patient barriers, such as lack of transportation, financial and insurance barriers, lack of childcare, low literacy, and language translation (i.e., instrumental support); and 4) providing psychosocial support (i.e., emotional support).8 The SES and household disparities that were alleviated by patient navigation in our study aligned with these areas in which patient navigators focus. For example, addressing patient-level barriers may help explain the elimination of the effects of financial strain or lack of insurance related to unemployment. Additionally, those without employment or stable housing may benefit from health information or assistance in overcoming health system barriers. Although the current analysis does not assess the specific barriers each patient experienced, separate analyses of data from the Patient Navigation Research Program Study identified the following areas of patient-reported barriers: comorbidity, financial, attitudinal, transportation, interpersonal, and system.26 To address these barriers, frequent navigator activities included making arrangements, scheduling appointments, referrals, and education.26 Another analysis found that social service barriers (e.g., insurance, financial problems, housing, employment issues, childcare issues, adult care) were associated with longer time to diagnostic resolution.27
With the America College of Surgeons requiring patient navigation based on community needs assessment for cancer center accreditation as of 2015,28 PN programs are increasingly being implemented in cancer care systems.7-14 The lack of guidance on how best to implement these patient navigation programs adds an additional challenge. Furthermore, among systems with PN programs, most rely on either institutional resources or grant support for funding. Our findings add to the evidence base for effective patient navigation and suggest that navigation interventions could target limited resources to patients at risk for experiencing the greatest delays in care using information already collected as part of routine care, or collectible at intake to care. For example, a patient might have higher educational attainment but unstable housing and therefore might benefit from patient navigation.
One limitation of our study included the differing intervention allocation strategies used at each center, including individual and group randomization as well as non-randomized group allocation, which resulted in imbalances between the intervention and control arms. However, our adjustment for demographic and clinical factors should reduce this potential confounding bias. There were some violations of the proportional hazards assumption by navigation arm. To understand the impact of these violations, we calculated adjusted HRs in datasets subsetted by patient navigation arm (see Supplement). Results were still significant for housing status and marital status, but not unemployment. This change in results could be due to decreased power or because we appropriately addressed the PH assumption. Strengths of the study include the large and diverse population of vulnerable participants, those for whom navigation interventions are intended. The use of multicenter study design reduces the impact of a single navigator or system and infers generalizability of our results across different centers and populations.
Disparities in diagnostic resolution continue to exist by SES and household factors, such as employment, housing, and marital status. Patient navigation eliminated these disparities in our population. These findings point to the promise of patient navigation as a targeted intervention for patients at highest risk for delays in cancer care. As the Institute of Medicine moves to capture social determinants of health in electronic health records,29 identifying these at-risk patients will become a more straightforward part of practice and should result in more timely care and improved outcomes.
Supplementary Material
Acknowledgments
Funding: This study was supported by NIH Grants U01 CA116892, U01 CA117281, U01CA116903, U01CA116937, U01CA116924, U01CA116885, U01CA116875, U01CA116925, American Cancer Society, including #SIRSG-05-253-01 and #CRP-12-219-01-CPPB, and the Avon Foundation.
Footnotes
Disclosures: The authors have nothing to disclose.
Trial Registrations: clinicaltrials.gov Identifiers: NCT00613275, NCT00496678, NCT00375024, NCT01569672
Additional Contribution: The authors acknowledge the contributions of the following members of the Patient Navigation Research Program:
Patient Navigation Research Program Investigators:
Clinical Centers
Boston Medical Center and Boston University: Karen M Freund (principal investigator (PI)) and Tracy A Battaglia (co-PI).
Denver Health and Hospital Authority: Peter Raich (PI) and Elizabeth Whitley (co-PI).
George Washington University Cancer Institute: Steven R Patierno (PI), Lisa M Alexander, Paul H Levine, Heather A Young, Heather J Hoffman, and Nancy L LaVerda.
H. Lee Moffitt Cancer Center and Research Institute: Richard G Roetzheim (PI), Cathy Meade, and Kristen J Wells.
Northwest Portland Area Indian Health Board: Victoria Warren-Mears (PI).
Northwestern University Robert H. Lurie Comprehensive Cancer Center: Steven Rosen (PI) and Melissa Simon.
Ohio State University: Electra Paskett (PI). Douglas Post, Mira Katz
University of Illinois at Chicago and Access Community Health Center: Elizabeth Calhoun (PI) and Julie Darnell.
University of Rochester: Kevin Fiscella (PI) and Samantha Hendren.
University of Texas Health Science Center at San Antonio Cancer Therapy and Research Center: Donald Dudley (PI), Kevin Hall, Anand Karnard, and Amelie Ramirez.
Program Office
National Cancer Institute, Center to Reduce Cancer Health Disparities: Martha Hare, Mollie Howerton, Ken Chu, Emmanuel Taylor, and Mary Ann Van Dyun
Evaluation Contractor
NOVA Research Company: Paul Young and Frederick Snyder
Contributor Information
Angie Mae Rodday, Institute for Clinical Research and Health Policy Studies, Tufts Medical Center and Tufts University School of Medicine, Boston, MA.
Susan K. Parsons, Institute for Clinical Research and Health Policy Studies, Tufts Medical Center and Tufts University School of Medicine, Boston, MA.
Frederick Snyder, NOVA Research Company, Silver Spring, MD.
Melissa A. Simon, Departments of Obstetrics and Gynecology and Preventive Medicine, Northwestern University Feinberg School of Medicine and Robert H. Lurie Comprehensive Cancer Center, Chicago, IL.
Adana A.M. Llanos, Rutgers Biomedical and Health Sciences School of Public Health and Rutgers Cancer Institute of New Jersey, New Brunswick, NJ.
Victoria Warren-Mears, Northwest Tribal Epidemiology Center, Northwest Portland Area Indian Health Board, Portland, OR.
Donald Dudley, Department of Obstetrics and Gynecology, University of Texas Health Science Center at San Antonio, San Antonio, TX.
Ji-Hyun Lee, Department of Internal Medicine, University of New Mexico and UNM Cancer Center, Albuquerque, NM.
Steve R. Patierno, George Washington University Cancer Institute, Washington, DC, and Duke Cancer Institute, Durham, NC.
Talar W. Markossian, Public Health Services, Loyola University Chicago, Chicago, IL.
Mechelle Sanders, Department of Family Medicine, Department of Public Health Sciences, University of Rochester, Rochester, NY.
Elizabeth Whitley, Colorado Department of Public Health and Environment, Denver, CO.
Karen M. Freund, Institute for Clinical Research and Health Policy Studies, Tufts Medical Center and Tufts University School of Medicine, Boston, MA.
Reference List
- 1.Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54:78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 2.Clegg LX, Reichman ME, Miller BA, et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20:417–435. doi: 10.1007/s10552-008-9256-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thuret R, Sun M, Budaus L, et al. A population-based analysis of the effect of marital status on overall and cancer-specific mortality in patients with squamous cell carcinoma of the penis. Cancer Causes Control. 2013;24:71–79. doi: 10.1007/s10552-012-0091-y. [DOI] [PubMed] [Google Scholar]
- 4.Simard EP, Fedewa S, Ma J, Siegel R, Jemal A. Widening socioeconomic disparities in cervical cancer mortality among women in 26 states, 1993-2007. Cancer. 2012;118:5110–5116. doi: 10.1002/cncr.27606. [DOI] [PubMed] [Google Scholar]
- 5.Tannenbaum SL, Koru-Sengul T, Miao F, Byrne MM. Disparities in survival after female breast cancer diagnosis: a population-based study. Cancer Causes Control. 2013;24:1705–1715. doi: 10.1007/s10552-013-0246-5. [DOI] [PubMed] [Google Scholar]
- 6.Whitman S, Orsi J, Hurlbert M. The racial disparity in breast cancer mortality in the 25 largest cities in the United States. Cancer Epidemiol. 2012;36:e147–e151. doi: 10.1016/j.canep.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 7.Jean-Pierre P, Hendren S, Fiscella K, et al. Understanding the processes of patient navigation to reduce disparities in cancer care: perspectives of trained navigators from the field. J Cancer Educ. 2011;26:111–120. doi: 10.1007/s13187-010-0122-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wells KJ, Battaglia TA, Dudley DJ, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113:1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Honeycutt S, Green R, Ballard D, et al. Evaluation of a patient navigation program to promote colorectal cancer screening in rural Georgia, USA. Cancer. 2013;119:3059–3066. doi: 10.1002/cncr.28033. [DOI] [PubMed] [Google Scholar]
- 10.Phillips CE, Rothstein JD, Beaver K, Sherman BJ, Freund KM, Battaglia TA. Patient navigation to increase mammography screening among inner city women. J Gen Intern Med. 2011;26:123–129. doi: 10.1007/s11606-010-1527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee JH, Fulp W, Wells KJ, Meade CD, Calcano E, Roetzheim R. Patient navigation and time to diagnostic resolution: results for a cluster randomized trial evaluating the efficacy of patient navigation among patients with breast cancer screening abnormalities, Tampa, FL. PLoS One. 2013;8:e74542. doi: 10.1371/journal.pone.0074542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Battaglia TA, Bak SM, Heeren T, et al. Boston Patient Navigation Research Program: the impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiol Biomarkers Prev. 2012;21:1645–1654. doi: 10.1158/1055-9965.EPI-12-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freund KM, Battaglia TA, Calhoun E, et al. Impact of patient navigation on timely cancer care: the Patient Navigation Research Program. J Natl Cancer Inst. 2014;106:dju115. doi: 10.1093/jnci/dju115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffman HJ, LaVerda NL, Young HA, et al. Patient navigation significantly reduces delays in breast cancer diagnosis in the District of Columbia. Cancer Epidemiol Biomarkers Prev. 2012;21:1655–1663. doi: 10.1158/1055-9965.EPI-12-0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Freund KM, Battaglia TA, Calhoun E, et al. National Cancer Institute Patient Navigation Research Program: methods, protocol, and measures. Cancer. 2008;113:3391–3399. doi: 10.1002/cncr.23960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Longest BB, Young GJ. Coordination and Communication. Health care management: Organizational design and behavior. Delmar Publishers; Albany, NY: 2000. pp. 237–75. [Google Scholar]
- 17.Tejeda S, Darnell JS, Cho YI, Stolley MR, Markossian TW, Calhoun EA. Patient barriers to follow-up care for breast and cervical cancer abnormalities. J Womens Health (Larchmt) 2013;22:507–517. doi: 10.1089/jwh.2012.3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith EC, Ziogas A, Anton-Culver H. Association between insurance and socioeconomic status and risk of advanced stage Hodgkin lymphoma in adolescents and young adults. Cancer. 2012;118:6179–6187. doi: 10.1002/cncr.27684. [DOI] [PubMed] [Google Scholar]
- 19.Rundle A, Neckerman KM, Sheehan D, et al. A prospective study of socioeconomic status, prostate cancer screening and incidence among men at high risk for prostate cancer. Cancer Causes Control. 2013;24:297–303. doi: 10.1007/s10552-012-0108-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Quaglia A, Lillini R, Mamo C, Ivaldi E, Vercelli M. Socio-economic inequalities: a review of methodological issues and the relationships with cancer survival. Crit Rev Oncol Hematol. 2013;85:266–277. doi: 10.1016/j.critrevonc.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 21.Hoffman HJ, LaVerda NL, Levine PH, Young HA, Alexander LM, Patierno SR. Having health insurance does not eliminate race/ethnicity-associated delays in breast cancer diagnosis in the District of Columbia. Cancer. 2011;117:3824–3832. doi: 10.1002/cncr.25970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh GK, Miller BA, Hankey BF, Edwards BK. Persistent area socioeconomic disparities in US incidence of cervical cancer, mortality, stage, and survival, 1975-2000. Cancer. 2004;101:1051–1057. doi: 10.1002/cncr.20467. [DOI] [PubMed] [Google Scholar]
- 23.Richards MA, Westcombe AM, Love SB, Littlejohns P, Ramirez AJ. Influence of delay on survival in patients with breast cancer: a systematic review. Lancet. 1999;353:1119–1126. doi: 10.1016/s0140-6736(99)02143-1. [DOI] [PubMed] [Google Scholar]
- 24.House JS, Kahn RL. Measures and concepts of social support. Social Support and Health Academic Press, Inc.; 1985. pp. 83–108. [Google Scholar]
- 25.Helgeson VS, Cohen S. Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Health Psychol. 1996;15:135–148. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- 26.Katz ML, Young GS, Reiter PL, et al. Barriers reported among patients with breast and cervical abnormalities in the patient navigation research program: impact on timely care. Womens Health Issues. 2014;24:e155–e162. doi: 10.1016/j.whi.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Primeau SW, Freund KM, Ramachandran A, et al. Social service barriers delay care among women with abnormal cancer screening. J Gen Intern Med. 2014;29:169–175. doi: 10.1007/s11606-013-2615-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American College of Surgeons Commission on Cancer [Accessed on 6/20/14];Cancer Program Standards 2012: Ensuring Patient-Centered Care. Retrieved from http://www.facs.org/cancer/coc/programstandards2012.pdf.
- 29.Institute of Medicine . Capturing Social and Behavioral Domains in Electronic Health Records: Phase 1. The National Academies Press; Washington, DC: 2014. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.