Publisher's Note: There is an Inside Blood Commentary on this article in this issue.
Key Points
A salvage therapy for adults with refractory hemophagocytic lymphohistiocytosis.
Liposomal doxorubicin treatment combined with etoposide and methylprednisolone showed an encouraging overall response and was well-tolerated.
Abstract
Hemophagocytic lymphohistiocytosis (HLH) is a refractory immune disorder with a significant risk of death. Although standard therapy has dramatically improved survival in HLH patients, approximately 30%, especially adults, show no response to current treatment strategies. This prospective study aimed to investigate the efficacy of liposomal doxorubicin treatment combined with etoposide and methylprednisolone (doxorubicin-etoposide-methylprednisolone; DEP) as a salvage therapy for adult refractory HLH. Adult patients who did not achieve at least partial response 2 weeks after initial standard HLH therapy were enrolled in this study between June 2013 and June 2014. Response to salvage therapy was assessed at 2 and 4 weeks after initiation of DEP therapy and patients were followed until death or until November 2014. Sixty-three refractory HLH patients were enrolled, including 29 cases of lymphoma-associated HLH, 22 cases of Epstein-Barr virus–associated HLH, and 4 cases of familial HLH. There were 8 cases with unknown underlying diseases. Seventeen cases (27.0%) achieved complete response and 31 cases (49.2%) achieved partial response. The overall response was 76.2% (48/63). Patients who showed no response to DEP died within 4 weeks after salvage therapy. Twenty-nine of the 48 patients who achieved partial or complete response survived to subsequent chemotherapy, allogenic hematopoietic stem cell transplantation, or splenectomy. Our study suggests that DEP regimen is an effective salvage regimen for adult refractory HLH, which can prolong patient survival as we continue to understand the responsible mechanisms and bridge the gap between HLH and its underlying diseases. This study was registered in the Chinese Clinical Trials Registry Platform (http://www.chictr.org.cn/) as ChiCTR-IPC-14005514.
Introduction
Hemophagocytic lymphohistiocytosis (HLH) is an immune disorder characterized by uncontrolled T lymphocyte and macrophage activation and an excessive production of inflammatory cytokines. Active HLH develops rapidly, with a high mortality rate if reasonable and effective interventions are not undertaken. In the 1980s, the median survival rate of HLH was only 1 to 2 months, and the 1-year overall survival rate was only 5%.1 Currently, HLH-94 or HLH-04 regimens are the standard HLH treatment strategies and have increased the disease response rate from less than 10% in the past few years to about 70%. In this regimen, etoposide and dexamethasone, with or without cyclosporine A, are used to treat active HLH. However, HLH-94 study results suggest that about 30% of patients are unresponsive to standard therapy, and most deaths occur within the first few weeks of treatment.2 Additionally, transplant-related mortality may likely increase if HLH is poorly controlled before allogenic hematopoietic stem cell transplantation.3 So far, there have been few studies that focus on adult HLH. A recent review estimated that the mortality rate of adult HLH was approximately 41%.4 Although HLH-94 is applicable to the treatment of adult HLH, its response rate during the active phase is significantly lower than in pediatric patients; this disparity might be due to the more complex etiology and varied inducing factors of adult HLH.5
Large-sample prospective studies that may guide physicians regarding choice of therapy for refractory HLH patients who show no response to current treatment have been lacking. Application of salvage therapies that can effectively treat HLH refractory patients is of utmost importance and worthy of further research. Here, we conducted a multicenter, prospective, single-arm clinical study that aimed to investigate the efficacy of liposomal doxorubicin together with etoposide and high-dose methylprednisolone (DEP regimen) as a salvage therapy for adult refractory HLH.
Materials and methods
Subject eligibility criteria
The study was registered in Chinese Clinical Trials Registry Platform (ChiCTR-IPC-14005514) and approved by the Ethics Committee at Beijing Friendship Hospital. Patients who enrolled in this study fulfilled the following criteria: (1) met HLH-2004 diagnostic criteria6; (2) were older than 18 years of age; (3) were treated with HLH-94 no less than 2 weeks before enrollment and did not achieve at least partial response; and (4) did not have active gastrointestinal bleeding and had a left ventricular ejection fraction of ≥50% at the time of enrollment. Patients who met these criteria and agreed to accept DEP salvage therapy were enrolled between June 2013 and June 2014. Informed consent was obtained from all participants.
There are no accepted diagnostic criteria for refractory HLH. It is recognized that absence of response at 2 to 3 weeks is often a sign of refractory HLH.7 Our clinical experience also supports 2 weeks as the key response time point. Therefore, in this study, we defined refractory HLH as patients who did not achieve at least partial response 2 weeks after initial standard HLH therapy.
Assessment of therapy
The assessment of treatment was previously described in a research study for pediatric HLH.8 We modified the treatment based on our experience with adult HLH patients. A complete response was defined as normalization of all of the quantifiable symptoms and laboratory markers of HLH, including levels of sCD25, ferritin, and triglyceride; hemoglobin; neutrophil counts; platelet counts; and alanine aminotransferase (ALT). A partial response was defined as at least a 25% improvement in 2 or more quantifiable symptoms and laboratory markers by 2 weeks following DEP regimen as follows: sCD25 response was >1.5-fold decreased; ferritin and triglyceride decreased at least 25%; for patients with an initial neutrophil count of <0.5 × 109/L, a response was defined as an increase by at least 100% to >0.5 × 109/L; for patients with a neutrophil count of 0.5 to 2.0 × 109/L, an increase by at least 100% to >2.0 × 109/L was considered a response; and for patients with ALT >400 U/L, response was defined as an ALT decrease of at least 50%. Additionally, subjects’ body temperature had to revert to normal ranges in either complete response or partial response. Other observational indicators in the study included liver and spleen size, bilirubin, and albumin.
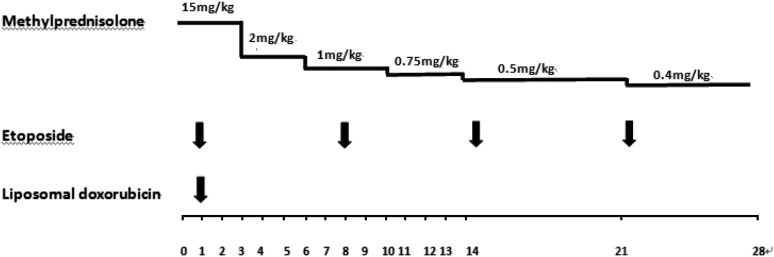
DEP regimen
The specific drugs and doses in the DEP regimen included the following: liposomal doxorubicin (doxorubicin hydrochloride liposome injection) 25 mg/m2 day 1; etoposide 100 mg/m2 was administered once on the first day of every week; methylprednisolone 15 mg/kg days 1 to 3, 2 mg/kg days 4 to 6, 1 mg/kg days 7 to 10, 0.75 mg/kg days 11 to 14, 0.5 mg/kg days 15 to 21, and 0.4 mg/kg days 22 to 28 (Figure 1). The efficacy was evaluated 2 and 4 weeks after initiating DEP salvage therapy. Treatment was followed by 0.3 mg/kg of methylprednisolone from the fifth week and was reduced by 0.1 mg/kg every week. Etoposide 100 mg/m2 was still administered once a week. Patients would receive further treatment of the underlying disease of HLH as soon as it had been clarified and the HLH was controlled. DEP regimen could be repeated after 3 weeks of salvage therapy in some partial response patients who had not received further treatment of their underlying disease. Liposomal doxorubicin 25 mg/m2 could only be repeated at the fourth week. The dosage of methylprednisolone and etoposide in the repeat treatments were the same as the following treatment. If patients presented recurrent signs of HLH, they could also be treated with the entire DEP regimen again.
Figure 1.
Dosage of DEP regimen. The horizontal axis of this figure is a timeline, split into days.
Side effects and complications
We closely monitored subjects for any signs of toxicity and complications that occurred during the treatment, including myelosuppression, infection, bleeding, heart function, and adverse drug reactions.
Survival and follow-up
As the HLH patients were being treated, their primary underlying diseases were explored by many methods, including genetic testing, pathogen screening, biopsy pathological examination, and immunological inspection. The primary diseases were treated by antitumor chemotherapy, antipathogen treatment, or allogeneic hematopoietic stem cell transplantation, as appropriate.
The survival time was calculated from the time patients received DEP salvage therapy until death or November 2014.
Statistical analysis
SPSS 19.0 statistical software was adopted, all normally distributed data were represented by means ± standard deviations, and comparison of multiple samples between groups was performed by independent sample t-test. All data that were not distributed normally were represented by median and range, and comparison of multiple samples between groups was performed by Wilcoxon rank sum test. Survival was analyzed by Kaplan-Meier survival curve. In all analyses, P < .05 indicated statistical significance.
Results
Study characteristics
The data in this study were collected from 6 medical institutions in China: Beijing Friendship Hospital, Affiliated Hospital Academy of Military Medical Sciences, Peking University First Hospital, Beijing Chao-yang Hospital, Peking University Third Hospital, and Navy General Hospital. Sixty-three eligible patients with refractory HLH were enrolled, including 42 males and 21 females. The median age was 34 (18 to 78) years old.
The primary disease could not be determined in 8 of the 63 HLH patients; in the other 55 patients, the primary disease was clarified within 8 weeks of HLH diagnosis. Primary diseases included: 4 cases of primary HLH, including 2 cases with familial HLH-2 (FHL-2), 1 with FHL-3, and 1 with X-linked lymphoproliferative syndrome type 1 HLH; 22 cases of Epstein-Barr virus (EBV)–associated HLH; 29 cases of lymphoma-associated HLH, including 2 cases of angioimmunoblastic T-cell lymphoma, 2 cases of non-Hodgkin diffuse large B-cell lymphoma, 1 case of non-Hodgkin mantle cell lymphoma, 5 cases of peripheral T-cell lymphoma, and 19 cases of non-Hodgkin natural killer/T-cell lymphoma. All the lymphoma-associated HLH patients were in stage III-IV (Ann Arbor) and the International Prognostic Index levels were 2 to 4. In addition, 16 cases of lymphoma-associated HLH were EBV-DNA positive (55.2%). The main clinical features of enrolled patients are summarized in Table 1.
Table 1.
The main clinical features of enrolled patients
| All (n = 63) | EBV-HLH (n = 22) | LAHS (n = 29) | FHL (n = 4) | Unclear (n = 8) | |
|---|---|---|---|---|---|
| General | |||||
| Gender (male/female), n | 42/21 | 16/6 | 19/10 | 3/1 | 4/4 |
| Median age (range), y | 34 (18-78) | 30.5 (18-57) | 40 (18-78) | 32 (18-60) | 27.5 (20-36) |
| Clinical features | |||||
| Fever, n | 63 | 22 | 29 | 4 | 8 |
| Neutropenia, n | 59 | 19 | 28 | 4 | 8 |
| Anemia, n | 49 | 14 | 26 | 2 | 7 |
| Thrombocytopenia, n | 52 | 20 | 26 | 2 | 4 |
| Splenomegaly, n | 50 | 17 | 23 | 4 | 6 |
| Hepatomegaly, n | 25 | 7 | 14 | 2 | 2 |
| Hypertriglyceridemia, n | 27 | 9 | 16 | 1 | 1 |
| Hypofibrinogen, n | 33 | 8 | 17 | 2 | 6 |
| Ferritin↑, n | 63 | 22 | 29 | 4 | 8 |
| Bilirubin↑, n | 44 | 17 | 18 | 4 | 5 |
| Alanine aminotransferase↑, n | 48 | 18 | 22 | 6 | 2 |
| Albumin↓, n | 35 | 11 | 19 | 1 | 4 |
| Soluble CD25↑, n | 63 | 22 | 29 | 4 | 8 |
| Previous treatment of HLH | |||||
| Regimen | HLH-94 ± rituximab | HLH-94 ± rituximab | HLH-94 | HLH-94 | HLH-94 |
| Weeks from initial therapy to DEP, median (range) | 3 (2-28) | 3 (2-23) | 2 (2-5) | 11.5 (3-28) | 3.5 (2-24) |
LAHS, lymphoma-associated HLH.
Before DEP salvage therapy, these patients had been treated by etoposide and glucocorticoid induction therapy for more than 2 weeks according to the HLH-94 regimen; partial response was not achieved as assessed by efficacy evaluation. The median time from patients received initial therapy to DEP regimen was 3 weeks (range, 2-28 weeks). Six subjects showed a response to initial therapy but relapsed and failed to respond to HLH-94 the second time. Three cases of EBV-HLH had been treated with a rituximab-based regimen but failed to respond.
Response of DEP regimen
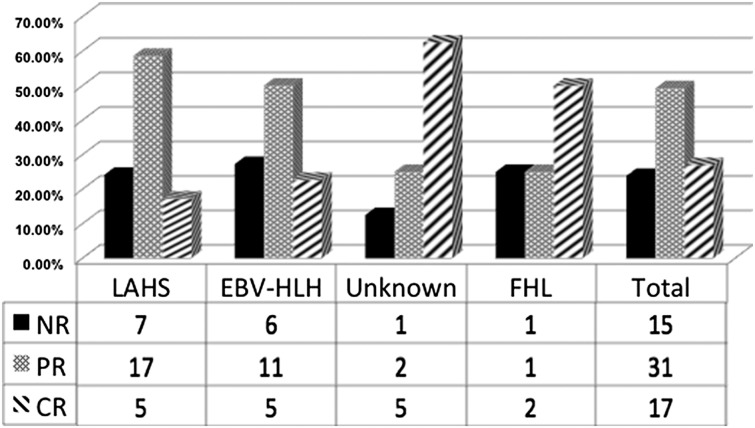
The overall response rate of the 63 patients with refractory HLH to DEP salvage regimen was 76.2% (48/63 patients), with 27.0% (17/63 patients) in complete response and 49.2% (31/63 patients) in partial response. There were 2 cases of complete response and 1 case of partial response in primary HLH patients, with an overall response rate of 75%, and 5 cases of complete response and 17 cases of partial response in patients with lymphoma-associated HLH, with an overall response rate of 75.7%. Additionally, there were 5 cases of complete response and 11 cases of partial response in patients with EBV-associated HLH, with an overall response rate of 72.7%, and 5 cases of complete response and 2 cases of partial response in patients with unexplained HLH, with an overall response rate of 87.5%. Fifteen patients were nonresponsive to the treatment (Figure 2). In addition, 7 of the partial response patients were subjected to a second liposomal doxorubicin 25 mg/m2 treatment at the fourth week before they received further treatment of their underlying disease.
Figure 2.
Response rates of refractory HLH to DEP salvage treatment. CR, complete response; NR, no response; PR, partial response; unknown, unclear underlying disease.
Changes in evaluation indicators before and after DEP salvage therapy
Partial response or better was achieved in 48 patients with refractory HLH receiving DEP salvage therapy. We analyzed 10 laboratory parameters at HLH diagnosis, before DEP salvage treatment, and 2 and 4 weeks after DEP salvage treatment. These indicators included white blood cell (WBC), hemoglobin (Hgb), platelet (PLT), ferritin, ALT, total bilirubin, triglycerides (TGs), albumin, fibrinogen (Fbg), and soluble CD25 (sCD25). The following 3 results were obtained. First, serum ferritin and sCD25 levels before DEP salvage therapy were significantly higher than those at HLH diagnosis (P < .05), suggesting that elevated serum ferritin and sCD25 levels were important indicators of disease progression. Second, there was statistically significant improvement in WBC, PLT, Fe, ALT, TG, Fbg, and sCD25 2 weeks after DEP salvage therapy compared with data before treatment. Third, 4 weeks after DEP salvage therapy, WBC, PLT, Fe, ALT, TG, Fbg, and sCD25 had continuously improved, and Hgb showed statistically significant improvement (the changes in the major indicators of HLH patients at HLH diagnosis, before and after DEP salvage treatment, are shown in Table 2).
Table 2.
Changes in evaluation indicators before and after salvage therapy
| At HLH diagnosis | Before DEP regimen | 2 weeks after DEP regimen | 4 weeks after DEP regimen | |
|---|---|---|---|---|
| WBC (×109/L) | 1.88 ± 0.89 | 1.60 ± 0.86 | 3.05 ± 1.91 | 4.26 ± 1.49 |
| P value | .119 | 9.711 × 10−6 | 9.339 × 10-17 | |
| Hgb (g/L) | 84.54 ± 18.13 | 79.98 ± 15.87 | 81.63 ± 17.97 | 90.40 ± 17.59 |
| P value | .193 | 0.635 | 0.003 | |
| PLT (×109/L) | 52.88 ± 28.72 | 61.33 ± 55.90 | 88.25 ± 67.11 | 115.79 ± 67.34 |
| P value | .354 | .035 | 4.003 × 10-5 | |
| Ferritin (μg/L) | 3386.0 (622-55 402.0) | 6786.5 (555.0-44 180.0) | 2339.0 (67.4-21 489.0) | 1119.5 (79.2-9372.0) |
| P value | 0.048 | 5.389 × 10-5 | 6.183 × 10-9 | |
| ALT (U/L) | 104.92 ± 80.02 | 95.96 ± 70.58 | 69.60 ± 42.30 | 37.83 ± 24.12 |
| P value | .562 | .029 | 1.311 × 10-6 | |
| TBIL (μmol/L) | 23.48 (8.5-293.0) | 25.45 (5-308.0) | 20.28 (4.6-181.2) | 19.89 (5.54-137.0) |
| P value | .671 | .324 | .151 | |
| TG (mmol/L) | 2.64 ± 1.22 | 2.76 ± 1.34 | 2.25 ± 0.79 | 2.28 ± 0.97 |
| P value | .636 | .027 | .048 | |
| ALB (g/L) | 31.47 ± 6.20 | 30.62 ± 6.96 | 31.73 ± 5.32 | 32.81 ± 5.08 |
| P value | .528 | .386 | .083 | |
| Fbg (g/L) | 1.54 (0.47-5.70) | 1.51 (0.60-5.04) | 1.65 (0.71-6.09) | 1.70 (0.93-3.38) |
| P value | .265 | .070 | .003 | |
| sCD25 (pg/mL) | 22435.0 (8695.0-44 000.0) | 39285.0 (10 485.0-44 000.0) | 16 100.9 (4598.0-29 167.0) | 6878 (2117.0-15 152.0) |
| P value | .004 | 2.794 × 10-11 | 2.030 × 10-16 |
ALB, albumin; TBIL, total bilirubin.
Of the patients who responded to DEP regimen, the peak value of body temperature declined rapidly after the start of treatment. The overall time of recovery to normal body temperature was from 24 hours to 5 days. Splenomegaly was observed in 50 patients, and hepatomegaly was observed in 25 patients with ultrasound examination. At the fourth week after DEP regimen, the liver size recovered to normal size in all responding patients, whereas splenomegaly was still observed in 15 partial response patients. However, the length of the spleen, which was initially larger than normal at the start of treatment, had decreased more than 50%.
Side effects and complications
Bone marrow suppression and cytopenia.
All patients had cytopenia in 1 or more blood cell lines before DEP salvage treatment, among which 61 patients had cytopenia in 2 or more blood cell lines. All patients were examined with bone marrow biopsy at HLH diagnosis and showed active bone marrow hyperplasia. Bone marrow biopsy was repeated in 39 patients at 3 to 4 weeks after DEP regimen and still showed active bone marrow hyperplasia. Among the 48 patients responsive to DEP regimen after salvage therapy, leukocytes in 4 patients, platelets in 3 patients, and hemoglobin in 8 patients were lower at 2 weeks after salvage treatment than at the start of their DEP regimen. However, the indicators were decreased by less than 50% of the baseline level and were significantly improved after 4 weeks. The peripheral blood cells were also significantly improved, instead of being significantly decreased, in the other patients responding to DEP regimen after salvage treatment. The 3 lines of peripheral blood cells were transiently improved in 6 of the 15 patients not responding to the DEP regimen. The marrow toxicity of the DEP regimen was difficult to evaluate because cytopenia was the main clinical feature of HLH, but, overall, there was no evidence of bone marrow toxicity directly associated with the drug in this study.
Infection.
Twenty-nine of the 63 enrolled patients had radiological signs of pulmonary infection before DEP salvage therapy. Ten patients had bacterial infections confirmed by sputum examination, including Pseudomonas aeruginosa, Enterobacter cloacae, Acinetobacter baumannii, and Staphylococcus aureus. Four patients had candidiasis, and 2 patients had aspergillosis. These patients received appropriate antibiotic treatment and DEP salvage therapy; the infections improved in varying degrees. Infection aggravation or new infections directly induced by DEP regimen were not observed.
Bleeding.
Before salvage treatment, prothrombin time was prolonged for more than 3 seconds in 18 patients; activated partial thromboplastin time was prolonged for more than 10 seconds in 37 patients; and Fbg level was lower than 1.0 g/L in 19 patients and the platelet level was lower than 40 × 109/L in 25 patients. These patients were appropriately treated by supportive therapies, including platelet or clotting factor infusion. However, there were still 2 cases of grade 5 lower gastrointestinal bleeding after salvage therapy. Before salvage therapy, 1 of the 2 patients had significant prothrombin time and activated partial thromboplastin time prolongation and significantly reduced Fbg and PLT; another patient had thrombocytopenia without obvious abnormality in the coagulation indicators. The remaining patients did not have grade ≥2 bleeding.
Cardiac function.
Six of the enrolled patients had a history of hypertension and 2 had a history of coronary atherosclerosis. However, the left ventricular ejection fraction was greater than 50% in all patients before treatment. The patients with cardiovascular disease continued to take effective cardiovascular drugs during treatment, and there were no adverse reactions, including acute coronary syndrome, significant increase of blood pressure, malignant arrhythmias, or acute heart failure, reported in any patient during the study observation period.
Other drug-related adverse reactions.
Three patients had type 2 diabetes before treatment. They were treated by insulin to control blood sugar and were closely monitored. There were no adverse reactions, such as persistent hyperglycemia and diabetic ketoacidosis. Hand-foot syndrome associated with liposomal doxorubicin was not observed in any patient.
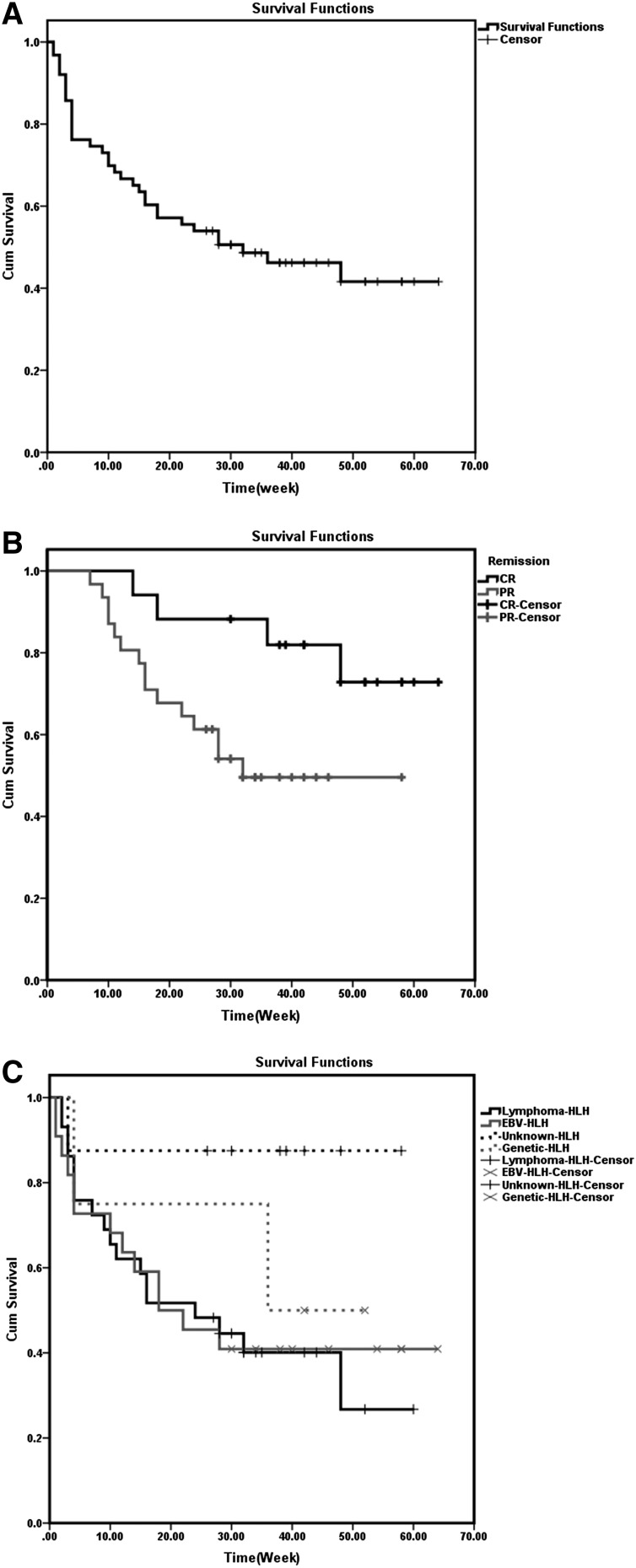
Survival analysis
The overall mortality rate in the 63 patients with refractory HLH was 54.0% (34/63 patients), with a median survival of 28 weeks (1 to 64 weeks) (Figure 3A). Fifteen patients who were nonresponsive to DEP salvage therapy died within 4 weeks after the start of salvage therapy. In 29 of the 48 patients who achieved partial response and complete response, the primary disease treatments, including antitumor chemotherapy (5 cases), antiviral therapy (4 cases), allogeneic hematopoietic stem cell transplantation (13 cases), and splenectomy (7 cases), were intensified after HLH alleviation, and disease conditions were persistently relieved.
Figure 3.
Kaplan-Meier analysis of survival of patients receiving DEP salvage therapy. (A) Overall survival. (B) Comparison of the survival of patients with CR and PR. (C) Comparison of the survival of patients with different primary diseases.
Death occurred in 19 patients who achieved partial or complete response. Eleven patients failed to accept systematic primary disease treatment after response, which resulted in HLH recurrence and death, including 7 cases of EBV-associated HLH, 3 cases of lymphoma-associated HLH, and 1 case of primary HLH. After reusing DEP salvage therapy, 3 relapsing patients had improvement in more than 1 of the evaluation indicators; however, they died of repeated HLH resulting from uncontrollable primary disease. Eight patients died of primary disease (lymphoma-associated HLH) progression, and there was no evidence of active HLH at death.
The response evaluation of the DEP regimen and the comparison of the survival difference between different primary disease groups suggested that the overall survival was significantly prolonged in patients who reached complete response after DEP salvage therapy compared with patients who reached partial response (P = .027; Figure 3B), and there was no significant difference in the overall survival of the HLH patients with different primary diseases (P = .181; Figure 3C). However, the survival of HLH patients with unknown underlying disease was better than lymphoma-associated HLH or EBV-HLH.
Discussion
Hemophagocytic lymphohistiocytosis is a life-threatening disorder characterized by high inflammatory cytokines production induced by excessive immune activation. Patients who are nonresponsive to standard treatment often die of uncontrollable disease activities. Therefore, exploring an effective salvage regimen is essential to reduce HLH mortality. At present, there is no unanimously recommended salvage HLH treatment regimen, and there are few case reports or clinical reports with small sample sizes concerning salvage therapy after first-line treatment failure. It has been reported that infliximab, daclizumab, anakinra, vincristine, tocilizumab, and other drugs have been used in HLH salvage therapy.9-13 One single-center clinical study with 38 subjects showed that initial treatment combined with antithymocyte globulins increased the complete response rate to 73%; however, the early recurrence rate was also high, and there was no superiority in long-term prognosis.14 A retrospective study suggested that alemtuzumab therapy of refractory HLH resulted in improvement and survival to allogeneic HCT in most patients. That study showed that 64% of refractory HLH patients achieved partial response, but no complete response was observed because many patients received additional courses of alemtuzumab or moved quickly to HCT.8 However, there are no available data to show the applicability of alemtuzumab in adult HLH patients. Although adult HLH has been recognized in recent decades and presented similar clinical features as in children, adult HLH has some different traits from pediatric HLH, such as underlying cause, diagnostic process, and treatment response. In pediatric patients, genetic defects or immunodeficiencies are the major causes of HLH. Alemtuzumab resulted in improvement and survival to allogeneic HCT in most patients because of its rapid and efficient depletion of CD52-expressing cells. Yet, it is unclear whether the significant immune clearance is suitable because the underlying causes of HLH in adults are varied. In our study, DEP regimen showed an encouraging overall response (76.2%) and tolerance in adult refractory HLH patients.
According to the pathophysiologic mechanisms of HLH, an ideal salvage regimen should have strong multi-immunosuppression. Based on our experience in the diagnosis and treatment of HLH, we modified the HLH-94 standard treatment regimen by using etoposide and corticosteroids as the core treatment, increasing the dosage of corticosteroids for pulse therapy during initial induction period, and using liposomal doxorubicin as an important induction therapy. First, glucocorticoids have strong inhibitory effects in the process of activation, differentiation, chemotaxis, and immune effect’s production. In refractory HLH, uncontrolled immune activation induces sustained secretion of inflammatory cytokines, and high-dose steroid pulse therapy might more efficiently inhibit the effects of inflammatory cytokines and quickly control the disease in patients unresponsive to conventional-dose hormone therapy. Second, doxorubicin, a broad-spectrum chemotherapeutic drug, has a wide range of biochemical effects on the body and has strong cell toxicity. The present study suggests that cytotoxic chemotherapy is a feasible approach for HLH treatment, especially EBV-associated HLH and lymphoma-associated HLH. However, conventional chemotherapies have poor effects.15,16 Some research showed that rituximab-containing regimens appeared well-tolerated and improved clinical status in 43% of patients17; however, we did not find significant improvement compared with a nonrituximab regimen in our small series of EBV-HLH (unpublished observations). We identified the lineage of EBV-infected cells from EBV-HLH patients by immunohistochemistry double staining and identified most of them as CD3+/EBER+. This suggests that EBV predominantly infects T cells in Chinese populations, which could explain the nonsuperiority of rituximab in Chinese adult EBV-HLH. However, liposomes can promote drug accumulation in capillary permeability-increased sites and enrichment in the lymphatic system, prevent the drug from being engulfed by macrophages and monocytes, and prolong the drug half-life to ultimately increase the therapeutic effect.18,19 Therefore, based on the core treatment with etoposide, which inhibits monocytes and tissue cell activation, improved glucocorticoid application method combined with liposomal doxorubicin could inhibit inflammatory cytokine secretion and the corresponding invasive damages more efficiently. In addition, HLH patients are often accompanied by severe complications; therefore, the low cardiotoxicity risk of liposomal doxorubicin, low liver toxicity and water-sodium retention risk of methylprednisolone, and other advantages can reduce the risk of treatment-related injuries to a certain extent. In the present clinical study, serious DEP-related bone marrow toxicity and cardiotoxicity were not observed. The occurrence of serious infections was not increased from the administration of effective anti-infective therapy. Although the serious gastrointestinal bleeding might be due to thrombocytopenia or coagulation abnormalities before treatment, these observations suggested that the regimen might have the potential to increase the risk of bleeding, especially in patients with significant coagulation disorders.
There is no unanimously recommended guideline for refractory HLH. The appropriate time point to initiate salvage treatment in patients nonresponsive to a standard HLH regimen should be investigated in further clinical studies. Mainstream international academic views report that the deterioration of liver function and hemogram—as well as gradual increases in serum ferritin, sCD25, and sCD163—are signs of HLH activity. If a patient does not show at least partial response within 2 to 3 weeks after the start of treatment, salvage therapy should be considered.7,20 Our clinical research data also showed that most deaths in the active stage of HLH occurred within 4 weeks of treatment initiation.21 In the present study, 7 indicators, including WBC, PLT, Fe, ALT, TG, Fbg, and sCD25, were significantly improved at 2 weeks; Hgb was also significantly improved at 4 weeks in responding patients. These results suggested that if effective treatment regimens are administered in patients, improvement of some indicators can be observed within 2 weeks of treatment initiation. Therefore, patients’ condition assessments at 2 weeks after HLH treatment initiation might be a key time point for evaluating the efficacy of primary regimen and determining whether the treatment regimen should be altered. Initiating salvage therapy as early as possible in patients with poor response to initial treatment might decrease early mortality. However, there are no data concerning whether patients who are nonresponsive to 2 weeks of standard HLH regimen are still nonresponsive if they continue to receive original regimen; therefore, randomized and controlled clinical studies with large sample sizes are needed to show whether these patients can truly benefit from DEP salvage therapy.
HLH treatment strategy includes 2 main aspects; namely, the short-term regimen that primarily controls the excessive inflammation status and the long-term strategy that mainly cures the underlying primary disease or immune deficiencies.22 Allogenic hematopoietic stem cell transplantation after response induction is a key method for improving survival for primary HLH with genetic defects. However, the primary disease in patients with acquired HLH significantly affects their survival. Among the different causes of adult HLH, malignancies, particularly T- or natural killer–/T-cell lymphoma, have the worst prognosis, whereas the prognosis of autoimmune disease–associated HLH is better.5 In infection-induced HLH, refractory EBV infection is most difficult to treat.23 This highlights why the refractory HLH subjects enrolled in this study consisted mainly of patients with lymphomas and EBV-associated HLH. In this study, although refractory HLH patients still exhibited good responses to DEP regimen after initial treatment failure, nearly half of the patients died. The patients who were nonresponsive to DEP salvage therapy died within 4 weeks after the start of salvage therapy. In addition, 19 of 48 patients who achieved partial response or complete response died from a lack of systematic treatments for the primary diseases after HLH was controlled, or the primary diseases progressed again, with or without HLH relapse. This observation suggested that selecting an effective induction regimen to actively control the excessive inflammation in the early stages of HLH progression provides time and opportunity to clarify the cause of disease and reduce mortality, whereas primary disease control is essential for the treatment in the late stages.
All current studies on the treatment of adults are noncontrolled and retrospective small-sample studies,16,24-26 and this study provides encouraging results for the salvage therapy of refractory HLH. Our study might bridge the transition from induction therapy to etiology therapy. A multicenter, prospective, randomized, and controlled study about DEP salvage treatment of adult HLH is ongoing. In that study, patients who do not achieve partial response after 2 weeks of HLH-94 regimen treatment are enrolled and randomized into 2 groups. One group receives DEP salvage therapy, whereas the other group continues to receive the HLH-94 regimen treatment. The objective of that study is to further demonstrate the efficacy and safety of the DEP regimen.
Acknowledgments
The authors thank the members of the Chinese Hemophagocytic Lymphohistiocytosis Group.
This work was supported by the Beijing Science and Technology Plan (grant Z151100004015172), the National Natural Science Fund, China (grant 81401627), and the Medical Development Research Foundation of the Capital, China (grant 2014-4-2025).
Footnotes
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: Z.W. designed and performed research; Y.W. performed statistical analysis and wrote the manuscript; W.H. collected data and performed statistical analysis; and L.H., X.C., L.L., J.W., J.S., and N.W. performed research.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Zhao Wang, Professor of Hematology, Department of Hematology, Beijing Friendship Hospital, Capital Medical University, 95 Yong’an Rd, Xicheng District, Beijing, 100050; e-mail: zhaowww263@outlook.com.
References
- 1.Janka GE. Familial hemophagocytic lymphohistiocytosis. Eur J Pediatr. 1983;140(3):221–230. doi: 10.1007/BF00443367. [DOI] [PubMed] [Google Scholar]
- 2.Henter JI, Samuelsson-Horne A, Aricò M, et al. Histocyte Society. Treatment of hemophagocytic lymphohistiocytosis with HLH-94 immunochemotherapy and bone marrow transplantation. Blood. 2002;100(7):2367–2373. doi: 10.1182/blood-2002-01-0172. [DOI] [PubMed] [Google Scholar]
- 3.Baker KS, Filipovich AH, Gross TG, et al. Unrelated donor hematopoietic cell transplantation for hemophagocytic lymphohistiocytosis. Bone Marrow Transplant. 2008;42(3):175–180. doi: 10.1038/bmt.2008.133. [DOI] [PubMed] [Google Scholar]
- 4.Ramos-Casals M, Brito-Zerón P, López-Guillermo A, Khamashta MA, Bosch X. Adult haemophagocytic syndrome. Lancet. 2014;383(9927):1503–1516. doi: 10.1016/S0140-6736(13)61048-X. [DOI] [PubMed] [Google Scholar]
- 5.Huang W, Wang Y, Wang J, et al. [Clinical characteristics of 192 adult hemophagocytic lymphohistiocytosis]. Zhonghua Xue Ye Xue Za Zhi. 2014;35(9):796–801. doi: 10.3760/cma.j.issn.0253-2727.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Henter JI, Horne A, Aricó M, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48(2):124–131. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 7.Jordan MB, Allen CE, Weitzman S, Filipovich AH, McClain KL. How I treat hemophagocytic lymphohistiocytosis. Blood. 2011;118(15):4041–4052. doi: 10.1182/blood-2011-03-278127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marsh RA, Allen CE, McClain KL, et al. Salvage therapy of refractory hemophagocytic lymphohistiocytosis with alemtuzumab. Pediatr Blood Cancer. 2013;60(1):101–109. doi: 10.1002/pbc.24188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bruck N, Suttorp M, Kabus M, Heubner G, Gahr M, Pessler F. Rapid and sustained remission of systemic juvenile idiopathic arthritis-associated macrophage activation syndrome through treatment with anakinra and corticosteroids. J Clin Rheumatol. 2011;17(1):23–27. doi: 10.1097/RHU.0b013e318205092d. [DOI] [PubMed] [Google Scholar]
- 10.Henzan T, Nagafuji K, Tsukamoto H, et al. Success with infliximab in treating refractory hemophagocytic lymphohistiocytosis. Am J Hematol. 2006;81(1):59–61. doi: 10.1002/ajh.20462. [DOI] [PubMed] [Google Scholar]
- 11.Imashuku S, Hibi S, Ohara T, et al. Histiocyte Society. Effective control of Epstein-Barr virus-related hemophagocytic lymphohistiocytosis with immunochemotherapy. Histiocyte Society. Blood. 1999;93(6):1869–1874. [PubMed] [Google Scholar]
- 12.Olin RL, Nichols KE, Naghashpour M, et al. Successful use of the anti-CD25 antibody daclizumab in an adult patient with hemophagocytic lymphohistiocytosis. Am J Hematol. 2008;83(9):747–749. doi: 10.1002/ajh.21236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teachey DT, Rheingold SR, Maude SL, et al. Cytokine release syndrome after blinatumomab treatment related to abnormal macrophage activation and ameliorated with cytokine-directed therapy. Blood. 2013;121(26):5154–5157. doi: 10.1182/blood-2013-02-485623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahlaoui N, Ouachée-Chardin M, de Saint Basile G, et al. Immunotherapy of familial hemophagocytic lymphohistiocytosis with antithymocyte globulins: a single-center retrospective report of 38 patients. Pediatrics. 2007;120(3):e622–e628. doi: 10.1542/peds.2006-3164. [DOI] [PubMed] [Google Scholar]
- 15.Imashuku S. Clinical features and treatment strategies of Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis. Crit Rev Oncol Hematol. 2002;44(3):259–272. doi: 10.1016/s1040-8428(02)00117-8. [DOI] [PubMed] [Google Scholar]
- 16.Shin HJ, Chung JS, Lee JJ, et al. Treatment outcomes with CHOP chemotherapy in adult patients with hemophagocytic lymphohistiocytosis. J Korean Med Sci. 2008;23(3):439–444. doi: 10.3346/jkms.2008.23.3.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chellapandian D, Das R, Zelley K, et al. EBV-HLH Rituximab Study Group. Treatment of Epstein Barr virus-induced haemophagocytic lymphohistiocytosis with rituximab-containing chemo-immunotherapeutic regimens. Br J Haematol. 2013;162(3):376–382. doi: 10.1111/bjh.12386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huwyler J, Drewe J, Krähenbuhl S. Tumor targeting using liposomal antineoplastic drugs. Int J Nanomedicine. 2008;3(1):21–29. [PMC free article] [PubMed] [Google Scholar]
- 19.Schiffelers RM, Storm G, Bakker-Woudenberg IA. Host factors influencing the preferential localization of sterically stabilized liposomes in Klebsiella pneumoniae-infected rat lung tissue. Pharm Res. 2001;18(6):780–787. doi: 10.1023/a:1011080211226. [DOI] [PubMed] [Google Scholar]
- 20.Lin TF, Ferlic-Stark LL, Allen CE, Kozinetz CA, McClain KL. Rate of decline of ferritin in patients with hemophagocytic lymphohistiocytosis as a prognostic variable for mortality. Pediatr Blood Cancer. 2011;56(1):154–155. doi: 10.1002/pbc.22774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang Y, Wang Z, Wu L, et al. [A multicenter retrospective analysis of diagnosis and treatment on 72 hemophagocytic syndrome cases.] Zhonghua Xue Ye Xue Za Zhi. 2009;30(12):793–798. [PubMed] [Google Scholar]
- 22.Janka GE, Lehmberg K. Hemophagocytic lymphohistiocytosis: pathogenesis and treatment. Hematology (Am Soc Hematol Educ Program) 2013;2013:605–611. doi: 10.1182/asheducation-2013.1.605. [DOI] [PubMed] [Google Scholar]
- 23.Rosado FG, Kim AS. Hemophagocytic lymphohistiocytosis: an update on diagnosis and pathogenesis. Am J Clin Pathol. 2013;139(6):713–727. doi: 10.1309/AJCP4ZDKJ4ICOUAT. [DOI] [PubMed] [Google Scholar]
- 24.Ahn JS, Rew SY, Shin MG, et al. Clinical significance of clonality and Epstein-Barr virus infection in adult patients with hemophagocytic lymphohistiocytosis. Am J Hematol. 2010;85(9):719–722. doi: 10.1002/ajh.21795. [DOI] [PubMed] [Google Scholar]
- 25.Tateishi Y, Oda S, Sadahiro T, et al. Continuous hemodiafiltration in the treatment of reactive hemophagocytic syndrome refractory to medical therapy. Transfus Apheresis Sci. 2009;40(1):33–40. doi: 10.1016/j.transci.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 26.Imashuku S, Kuriyama K, Sakai R, et al. Treatment of Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis (EBV-HLH) in young adults: a report from the HLH study center. Med Pediatr Oncol. 2003;41(2):103–109. doi: 10.1002/mpo.10314. [DOI] [PubMed] [Google Scholar]