Abstract
Introduction
There is a lack of agreed and established guidelines for the treatment of acute exacerbations of idiopathic pulmonary fibrosis (AE-IPF). This reflects, in part, the limited evidence-base underpinning the management of AE-IPF. In the absence of high-quality evidence, the aim of this research was to develop a clinician-led consensus statement for the definition, diagnosis and treatment of AE-IPF.
Methods
A literature review was conducted to obtain published material on the definition and treatment of AE-IPF. The results of this review were circulated to an online panel of clinicians for review. Statements were then shared with ten expert respiratory clinicians who regularly treat patients with IPF. A Delphi technique was then used to develop a consensus statement for the definition, diagnosis and treatment of AE-IPF. During the first round of review, clinicians rated the clarity of each statement, the extent to which the statement should be included and provided comments. In two subsequent rounds of review, clinicians were provided with the group median inclusion rating for each statement, and any revised wording of statements to aid clarity. Clinicians were asked to repeat the clarity and inclusion ratings for the revised statements.
Results
The literature review, online panel discussion, and face-to-face meeting generated 65 statements covering the definition, diagnosis, and management of AE-IPF. Following three rounds of blind review, 90% of clinicians agreed 39 final statements. These final statements included a definition of AE-IPF, approach to diagnosis, and treatment options, specifically: supportive measures, use of anti-microbials, immunosuppressants, anti-coagulants, anti-fibrotic therapy, escalation, transplant management, and long-term management including discharge planning.
Conclusion
This clinician-led consensus statement establishes the ‘best practice’ for the management and treatment of AE-IPF based on current knowledge, evidence, and available treatments.
Funding
Boehringer Ingelheim Ltd., Bracknell, West Berkshire, UK.
Electronic supplementary material
The online version of this article (doi:10.1007/s12325-015-0249-6) contains supplementary material, which is available to authorized users.
Keywords: Acute exacerbations, Acute lung injury, Best practice, Consensus statement, Definition, Diagnosis, Idiopathic pulmonary fibrosis, Interstitial lung disease, Qualitative research, Treatment
Introduction
The most common form of idiopathic interstitial pneumonia (IIP) is idiopathic pulmonary fibrosis (IPF) [1, 2], accounting for almost 25% of all interstitial lung diseases (ILD) [3, 4]. IPF is a chronic, progressive, and irreversible life-limiting condition. Prognosis is poor, with many patients surviving less than 3–5 years following diagnosis [5–7]. IPF is typically characterized clinically by progressive dyspnea with worsening respiratory status [1, 2], resulting in progressive functional limitation and poor health-related quality of life (HRQoL) [8]. IPF is most common in middle-aged and older adults [2, 9], with five times more men than women being diagnosed with the condition [10, 11]. Environmental factors, such as cigarette smoking and occupational exposures, are often cited as triggers for the development of IPF, with recent research indicating that a family history of fibrosis may be the strongest risk factor [12]. However, the exact etiology of the condition is currently unknown [13]. Within the United Kingdom (UK), the incidence of IPF was estimated to be 6.8 per 100,000 in 2000–2003 [14]. Global estimates suggest an incidence of 14–43 per 100,000 [15], resulting in approximately 5 million sufferers worldwide [16], a burden which, it is suggested, will continue to increase [17].
IPF progression is associated with unpredictable acute deteriorations in respiratory function which are not associated with any identifiable cause such as infection, pulmonary embolism, or heart failure [18]. These episodes are termed acute exacerbations of IPF (AE-IPF) [19, 20] and frequently result in premature death. Mortality rate in the year following an AE-IPF is reported to be as high as 80% [13]. The American Thoracic Society (ATS) and European Respiratory Society (ERS) working groups have provided diagnostic criteria and guidelines for identifying possible AE-IPF. Despite the terminology and criteria proposed [2], guidance on the real-world diagnosis and treatment of AE-IPF is largely absent from IPF guidelines. For example, AE-IPF was absent from the 2000 ATS/ERS international consensus statement [2]. AE-IPF was mentioned, but not defined nor discussed, in the 2002 ATS/ERS international multidisciplinary consensus statement [21], and only briefly discussed within the 2011 ATS/ERS/Japanese Respiratory Society/Latin American Thoracic Association statement [22].
There are a number of important barriers impeding the management and treatment of patients with AE-IPF. Despite the 2007 guidelines outlined by Collard et al. [23], there remains a lack of consensus in defining AE-IPF, especially relating to excluding, or understanding, the role of infection in the pathogenesis of the condition. In the absence of an agreed definition, there is a lack of clear guidelines for diagnosing and treating AE-IPF [24].
Consensus methods such as the Delphi technique are widely used and accepted for medical and health service research [25–30]. For example, the Delphi technique has recently been used in the development of international clinical practice statements for the treatment of neuropsychiatric conditions associated with epilepsy [31] and cystic fibrosis pulmonary guidelines [32]. This specific technique is often used in circumstances when there are gaps or contradictions in knowledge [25].
The primary objective of this study was to use the Delphi technique to develop a consensus statement for the definition, diagnosis, and treatment of AE-IPF to guide clinicians in efficient diagnosis and treatment.
Methods
A structured literature review was conducted using Medline, PsycINFO, and EMBASE with a supplemental search of grey literature, to generate published materials that could contribute an initial list of statements to enter the Delphi process. The review focused on three specific areas: current opinion on the definition and diagnosis of AE-IPF; consensus or agreement on the treatment of patients with AE-IPF; and current treatment options for patients with AE-IPF. The search specifically targeted English language articles published between 2003 and October 2013 using search terms that were reviewed and agreed with clinicians participating in the Delphi process (Table 1).
Table 1.
Literature review search strategy
| Search terms |
|---|
| Idiopathic pulmonary fibrosis OR IPF OR pulmonary fibrosis OR interstitial lung disease(s) OR idiopathic interstitial pneumonia OR IIP OR cryptogenic fibrosing alveolitis OR usual Interstitial pneumonia OR UIP |
| AND acute OR exacerbation(s) |
| AND guideline(s) OR consensus OR statement(s) OR recommendation(s) OR best practice |
| AND treatment(s) |
Following completion of the literature review, a panel of ten experts was invited to participate in an online forum. These experts were all practicing clinicians with experience in treating patients with IPF. The purpose of the online forum was to explore the results from the literature review and discuss additional themes that might be appropriate for inclusion in a consensus statement. Discussion topics included: definitions of AE-IPF proposed in the literature review, diagnostic criteria relevant for AE-IPF, and considerations influencing treatment decisions. Seven of the ten participated in the forum, during which initial statements were formulated and reviewed by the panel chairperson to confirm clinical accuracy before the first round of the Delphi technique.
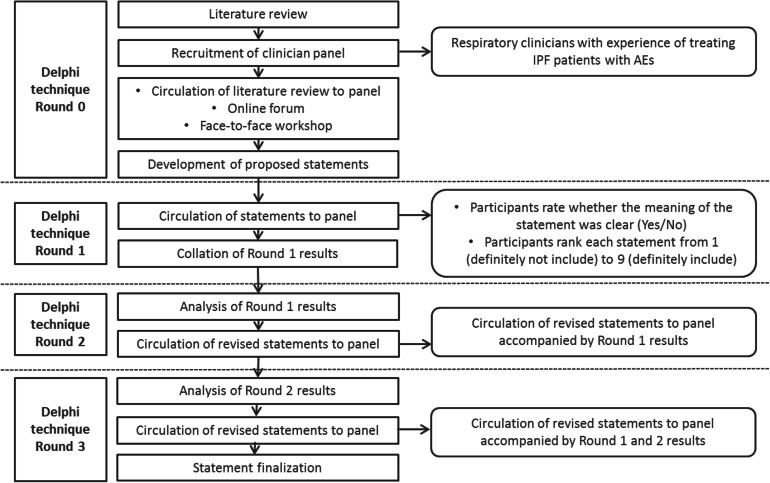
The Delphi technique was executed largely in accordance with the methods described by Jones and Hunter [25]. Delphi Panel participants (ten specialist respiratory clinicians with experience in treating patients with IPF) were identified by the panel chairperson, based on common adopted criteria [33] and independently recruited to participate. An iterative approach was employed where sequential surveys were presented to the panel of experts to gain consensus [34]. Participants reviewed and commented on the statements in isolation and all responses were anonymized, ensuring each participant provided their own opinion without influence [25]. For each statement, all ten participants were asked to judge whether the statement was clear (‘yes’ or ‘no’), whether they believed that the statement should be included (1 = ‘definitely not include’ to 9 = ‘definitely include’), and finally to provide any comments, in the form of free text, that might help clarify the meaning of the statement (Fig. 1).
Fig. 1.
Overview of consensus statement development and the Delphi technique. AEs acute exacerbations, IPF idiopathic pulmonary fibrosis
Using the criteria in Table 2, all statements were analyzed to determine whether the statement should be considered for inclusion, with or without modification [35]. All ten clinicians participated in round one and two, and nine clinicians participated in round three. Following the first round of the Delphi technique, participants were presented with the panel results. Where statements remained unmodified, participants were shown their individual ratings and the group ratings. This included the percentage of the group that agreed the statement was clear, median rating for inclusion, percentage of the group who rated the statement as ‘definitely include’, and combined comments. Where a statement was modified, participants were shown the same information and asked to re-rate the revised statements. Deleted statements were not presented to the panel in subsequent rounds.
Table 2.
Delphi technique statement inclusion key
| Statement result | Threshold applied |
|---|---|
| Definitely include |
1. ≥80% of panel rate statement as = 9 OR 2. Median rating of ≥8 |
| Maybe include |
1. ≥70% of panel rate statement as = 9 OR 2. Median rating of ≥7 |
| Definitely exclude |
1. <70% of panel rate statement as = 9 AND 100% panel understand statement OR 2. Median ≤6 AND 100% panel understand statement (suggesting that low scores are not due to lack of understanding of item) |
| Review |
1. Major revisions suggested OR 2. <70% of panel rate statement as = 9 AND <100% panel understand statement (suggesting that low scores are not due to lack of understanding of item) |
Non-responders were sent weekly follow-up email reminders to complete the online survey. Data collection for all three rounds took place over 5 months; however, data collection per round lasted no longer than 4 weeks. Consistent thresholds were maintained throughout each round [35].
A diagrammatic representation of the entire research process is presented in Fig. 1. All research was designed to comply with the British Healthcare Business Intelligence Association (BHBIA) Legal and Ethical Framework.
Results
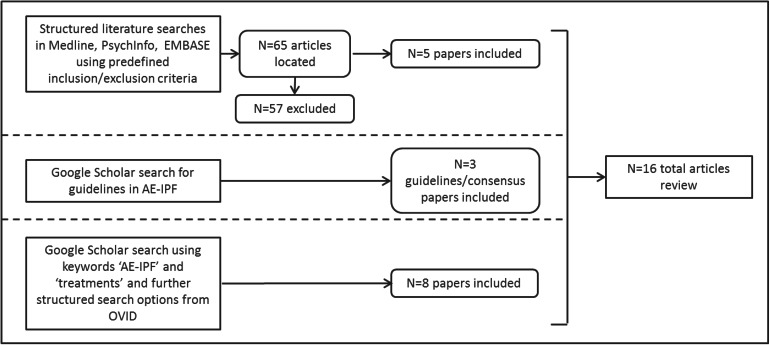
The literature search strategy (Fig. 2) identified 16 articles for inclusion in the literature review [1, 15, 21–23, 36–46] including, 8 original articles, 5 review articles on IPF management, outcomes, diagnosis or prognosis, and 3 guidelines/consensus statement articles.
Fig. 2.
Literature search strategy. AE-IPF acute exacerbations of idiopathic pulmonary fibrosis
Findings from the literature review indicated contradictory opinions regarding AE-IPF definition and diagnosis, with some suggesting the Collard [41] definition excluded many patients who would be treated for an acute exacerbation in routine clinical practice. There was also little consensus or agreement on AE-IPF treatment, with studies suggesting a number of pharmacological treatments such as corticosteroids [15, 23, 38, 40, 41, 43, 46], immunosuppressants [38, 40, 41, 45], combinations of immunosuppressants and anti-fibrotic drugs [39, 40], antibiotics [38], tyrosine kinase receptor inhibitor [44], anti-coagulation therapy [23, 40], and non-pharmacological treatments such as polymyxin B-immobilized fiber column treatment [36, 37, 40], mechanical ventilation [38, 40, 46], and lung transplantation [40].
Seven participants took part in the online forum with five of these also participating in a face-to-face meeting to discuss clinically meaningful ways to define AE-IPF and its treatment. Following the online forum and face-to-face meeting, 65 statements were developed. These addressed AE-IPF definition, AE-IPF acute treatment including supportive measures, anti-microbials, immunosuppressants, anti-coagulants, anti-fibrotic therapy, escalation, transplant management, and long-term management including discharge planning and preventative therapies.
Ten senior respiratory consultants participated in the initial and second rounds of the Delphi survey. Nine participated in the third and final rounds. All participants were experienced in treating patients with AE-IPF (Table 3).
Table 3.
Delphi technique panel member demographic characteristics
| Demographic characteristics | Round 1 (N = 10) | Round 2 (N = 10) | Round 3 (N = 9) |
|---|---|---|---|
| Gender, n (%) | |||
| Male | 5 (50%) | 5 (50%) | 4 (44%) |
| Female | 5 (50%) | 5 (50%) | 5 (56%) |
| Age (years), mean (SD) | 44.9 (5.1) | 44.9 (5.1) | 44.6 (5.4) |
| Time as a respiratory specialist (years), mean (SD) | 12.6 (3.8) | 12.6 (3.8) | 12.8 (4.0) |
| Patients with IPF treated in the last 12 months | |||
| Mean (SD) | 156 (112.7) | 151 (118.3) | 157 (124.9) |
| Min–Max | (25–300) | (25–350) | (25–350) |
IPF idiopathic pulmonary fibrosis, SD standard deviation
Following round 1 review of the 65 statements, 10 were deleted, 29 revised, and 26 remained unmodified (Table 4). AE-IPF definition statements were revised such that infection was excluded ‘as far as possible’ rather than ‘per routine clinical practice’. As such, an anti-infective treatment path statement was also revised to include a footnote that negative diagnosis is never completely certain. Additionally, references to specific doses of treatments were removed. All deleted statements in round one were excluded due to low ratings.
Table 4.
Results of Delphi review of statements
| Statement result | Round 1 | Round 2 | Round 3 |
|---|---|---|---|
| Number of statements, N | 65 | 55 | 44 |
| Definitely include, n | 36 | 35 | 36 |
| Median rating of statements | 8.76 | 8.82 | 8.89 |
| Percentage of panel rating statements ≥9 | 62% | 73% | 83% |
| Percentage of panel understanding statement | 94% | 98% | 99% |
| Maybe include, n | 7 | 9 | 3 |
| Median rating of statements | 7.29 | 7.22 | 7.00 |
| Percentage of panel rating statements ≥9 | 37% | 20% | 15% |
| Percentage of panel understanding statement | 86% | 96% | 100% |
| Definitely exclude, n | 4 | 5 | 3 |
| Median rating of statements | 5.38 | 5.90 | 6.00 |
| Percentage of panel rating statements ≥9 | 25% | 14% | 7% |
| Percentage of panel understanding statement | 100% | 100% | 100% |
| Review, n | 18 | 6 | 2 |
| Median rating of statements | 5.33 | 6.00 | 6.00 |
| Percentage of panel rating statements ≥9 | 24% | 10% | 22 |
| Percentage of panel understanding statement | 83% | 83% | 84 |
| Final number of statements, N | 55 | 44 | 39 |
Fifty-five remaining statements were reviewed in round 2, 11 of which were deleted, 32 unmodified, and 12 revised based on participants’ comments. Following round two, statements were revised to either enhance clarity or exclude reference to specific potentially preventive therapies, such as co-trimoxazole, nintedanib, and anti-fibrotic therapy. Additionally, examples of supportive measures were removed from statements as they were not considered exhaustive. Two treatment statements were removed relating to oxygen supportive measures as it was agreed there is current lack of evidence to guide oxygen therapy. Of the remaining 44 statements in round 3, 1 was revised and 5 deleted resulting in 39 final statements (Table 4). Statements were deleted from oxygen supportive measures, treatment paths, anti-reflux therapy, and anti-infective topics due to their low ratings. The final consensus statement is presented in Table 5. The single statement revision in round three was a grammatical change to enhance clarity. Statements were deleted at each round either due to low ratings or conceptual overlapping with other statements.
Table 5.
Final AE-IPF consensus statement
| AE-IPF definition |
|
Development or worsening of breathlessness within the preceding 30 days that is otherwise unexplained New diffuse chest infiltrates on chest X-ray and/r HRCT that are otherwise unexplained Exclusion of infection, in as far as possible, according to routine clinical practice and standard local practice, through microbiological studies and viral studies Exclusion of alternative causes as per routine clinical practice including left heart failure, PE, and identifiable causes of acute lung injury |
| AE-IPF treatment path |
| Supportive measures should be provided to increase patient comfort |
|
AE-IPF treatment path Acute treatment Supportive measure: Oxygen |
|
Oxygen should be supplied to correct hypoxia and improve dyspnea It is advised to titrate SpO2 to >88% High-flow oxygen delivery mechanism, e.g., Optiflow™ (Fisher & Paykel Healthcare), may be required A test dose of a benzodiazepine (generally lorazepam) may be prescribed followed by monitoring of SaO2 to avoid respiratory depression If a benzodiazepine is beneficial, dose should be titrated accordingly to manage symptoms Opiates may be prescribed in combination with a benzodiazepine, or alone if a benzodiazepine test dose is not tolerated |
| Supportive measure: psychological and spiritual support |
| Psychological and/or spiritual support should be offered to all patients as appropriate |
| Anti-infectives a |
|
A broad spectrum respiratory antibiotic should be prescribed as determined by clinical judgment in conjunction with local guidelines If a patient has recently been admitted as an inpatient they should additionally be covered for hospital acquired infection Anti-virals should not be prescribed routinely but only in cases of strong clinical suspicion and in accordance with local guidelines |
| Immunosuppressants |
| Corticosteroids should be considered in all patients unless specifically contra-indicated |
| Long-term corticosteroid dosing should be determined based on the individual patient |
| Cyclophosphamide/azathioprine/MMF should not be prescribed |
| The use of biologics, e.g., rituximab, is not recommended |
| Anti-coagulants |
| LMW heparin and/or anticoagulants should be initiated prophylactically to prevent DVT according to standard hospital policy, unless patients are already receiving anticoagulation therapy |
| Anti-fibrotic therapy |
|
If patients are already receiving anti-fibrotic therapy then this should be continued Patients should not be initiated on anti-fibrotic therapy in the setting of an acute exacerbation |
| Escalation |
|
Intubation and mechanical ventilation are not part of standard care Where possible the decision not to intubate or initiate mechanical ventilation should be discussed with patients at an early stage after IPF diagnosis CPAP can provide a helpful supportive measure End of life care should be discussed and agreed with patients and their families |
| Transplant |
|
If patients are already on the transplant waiting list then the transplant unit should be informed If patients recover from AE-IPF review suitability for transplant referral, ideally at an early follow-up appointment in the clinic |
| Long-term management |
|
Appropriate long-term management is essential following AE-IPF by a clinician with specialist expertise in IPF management As part of long-term management a review should assess the need for transplant referral As part of long-term management a review should assess the need for anti-fibrotic treatment As part of long-term management a review should assess the suitability for inclusion in clinical trials As part of long-term management a review by a respiratory physiotherapist should assess the need for pulmonary rehabilitation Appropriate supportive and palliative care mechanisms should be put in place |
| Discharge planning |
|
Discharge planning should ensure adequate home oxygen is in place prior to discharge if required Discharge planning should ensure an early post-discharge review at an ILD clinic is in place (within 4–6 weeks) An appropriate discharge letter should be provided |
| Preventative therapies |
| There is no clear evidence to provide recommendations for preventative therapies at present |
| Additional information |
| Note that this is an opinion-led standard of care and that there is an absence of an evidence base |
AE-IPF acute exacerbations of idiopathic pulmonary fibrosis, CPAP continuous positive airway pressure, DVT deep venous thrombosis, HRCT high-resolution computed tomography, ILD interstitial lung disease, LMW low molecular weight, MMF mycophenolate mofetil, PE pulmonary embolism, SpO 2 peripheral oxygen saturation
aNegative diagnosis is never completely certain
Discussion
The aim of this study was to develop a consensus statement for AE-IPF definition, diagnosis, and treatment to guide clinicians in efficient diagnosis and treatment. The literature review, online discussion, and Delphi technique generated 65 initial statements. Following 3 rounds of review, 39 statements were included in the final consensus statements.
The aim of a consensus statement is to reach an acceptable level of agreement between panel members on a particular issue to achieve convergence of opinion. This specific methodology, as opposed to alternative consensus approaches such as nominal group technique [47] or social judgment analysis [48], was considered a more appropriate approach because of lack of clinical guidelines currently in the literature. As a consensus method, the Delphi technique has advantages in that it can accommodate knowledge gathering from a number of clinical experts in various geographical locations, reducing potential participant burden by omitting travel. The Delphi technique has been applied to achieve a variety of objectives: determining a range of possible program alternatives, exploring underlying assumptions leading to different judgments within a respondent panel, correlating informed judgments on a topic spanning a wide range of disciplines, educating the respondent panel to diverse and interrelated topics, and, importantly, generating consensus [33]. This method is useful in the absence of extensive research-based evidence, when the development of guidelines must be based on the experience and opinions of clinicians [49]. Additionally, the Delphi technique offers the advantage of numerically combining participant responses, resulting in a more reliable statement than estimates from a single person [49]. Moreover, this approach allows the iterative exchange of information between individuals under controlled conditions, limiting the potentially detrimental effects of interaction [49].
Following each round of review, changes and deletions were made to statements that highlight some of the challenging decisions in this area. Revisions were made to AE-IPF definition statements to clarify that exclusion of infection should be ‘as far as possible’ rather than ‘as per routine clinical practice’. This change was made to reflect the challenges inherent in disproving any contribution of infection in the etiology of at least some cases of AE-IPF and the difficulties frequently encountered in clinical practice of performing intrusive investigations such as bronchoscopy on often critically unwell patients.
Reference to specific doses of drugs was removed from statements, as there is no empirical evidence to support a specific dosing regimen, for example, for corticosteroids, in AE-IPF. Additionally, statements were revised to exclude reference to specific preventative therapies as, at the time of conducting this research, there was no clear evidence to support any such recommendations. Despite the lack of evidence, preventative therapies that were routinely advised by the panel are influenza and pneumococcal vaccination, and prompt treatment of lower respiratory tract infections.
The role of oxygen therapy in AE-IPF generated considerable discussion. Clinicians believed that the British Thoracic Society (BTS) oxygen guidelines [50] are unhelpful in individuals with IPF because they are based heavily on evidence derived from studies of patients with chronic obstructive pulmonary disease (COPD); a disease which is characterized by an altogether different pathophysiology. The BTS guidelines advise titrating oxygen therapy by measuring arterial blood gases. The panel considered that it is inappropriate to perform repeated arterial sampling on ill patients suffering from an AE-IPF because unlike COPD these patients typically develop hypoxic rather than hypercapnic respiratory failure, so that oxygen saturations provide sufficient information.
Most statements relating to psychological support, escalation, anti-fibrotic therapy, transplant, long-term management, and discharge planning were retained with only minor wording modifications to enhance clarity of statements. Three statements were included relating to benzodiazepines and opiates; minor word modifications were made to these statements following round two to refer to benzodiazepine rather than lorazepam, and all clinicians agreed on the importance of benzodiazepine and opiates as anxiolytic supportive measures. Statements recommended that benzodiazepine may be prescribed alongside monitoring of oxygen saturation to avoid respiratory depression, and benzodiazepines and opiates may be used in combination, or alone, if well tolerated. However, it should be noted that decisions to remove and modify statements per round were based on clinical expert opinion rather than being evidence based.
Despite the degree of input and consensus among clinical experts to generate these statements, this study is not without limitations. The literature review aimed to stimulate discussion for the online forum and was based on a small number of papers focusing on AE-IPF diagnosis and management. Given that the literature review was limited in scope and not a systematic review, the scope was not exhaustive. However, a specialist clinician reviewed the literature review report, strengthening confidence in the literature review evidence. The online forum and Delphi technique included a small number of specialist clinicians from the UK, so results may not be generalizable to other countries. However, as the number of specialist clinicians treating AE-IPF is small, the study sample is considered reasonable. Nevertheless, the use of specialist clinicians only in the UK limits the generalizability of the study findings. Furthermore, there are limitations to the Delphi technique, with some authors suggesting it does not meet the rigorous standards of other scientific methods [51, 52]. However, given that there is limited AE-IPF guidance, the anonymous, iterative process of controlled feedback and clinical input achieved by this technique was best suited to the development of a consensus statement for AE-IPF. Furthermore, this technique has been successfully implemented to generate consensus statements in other therapeutic areas [26].
Conclusions
The final 39 consensus statements included topics on definition of AE-IPF, approach to diagnosis, and treatment options, specifically: supportive measures, use of anti-microbials, immunosuppressants, anti-coagulants, anti-fibrotic therapy, escalation, transplant management, and long-term management including discharge planning. The clinician-led consensus statement resulting from this Delphi technique outlines appropriate guidance for AE-IPF definition, diagnosis, and treatment, and is intended to direct decision making in the clinical management of patients with AE-IPF.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
Sponsorship for this study was funded by Boehringer Ingelheim Ltd., Bracknell, West Berkshire, UK. The article processing charges and the open access fee for this publication were funded by Boehringer Ingelheim Ltd. Conduct of the literature review and online forum, analysis of Delphi panel results, and preparation of the manuscript was provided by Adelphi Values. Elaine Brohan, Beverley Taylor, Bryan Bennett, and Nicola Williamson are employees of Adelphi Values and conducted this research on behalf of Boehringer Ingelheim Ltd and received a fee for this work. Alice Turnbull was an employee of Adelphi Values when this research was conducted. The Delphi panel was administered online by Adelphi Research UK. Dr. Toby Maher, Professor Moira Whyte, Dr. Rachel Hoyles, and Dr. Helen Parfrey participated in the online forum, face-to-face workshop, and Delphi panel. Dr. Gisli Jenkins participated in the online forum and Delphi Panel. Dr. Surinder Birring participated in the online forum and face-to-face workshop. Dr. George Chalmers, Dr. Michael Gibbons, Dr. Nazia Chaudhuri, Dr. Simon Hart, and Dr. Joanna Porter participated in the Delphi Panel. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. Adelphi Values had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Disclosures
TMM has received industry-academic research funding from GlaxoSmithKline R&D, UCB, and Novartis, and has received consultancy or speakers fees from Astra Zeneca, Bayer, Biogen Idec, Boehringer Ingelheim, Cipla, Dosa, GlaxoSmithKline R&D, Lanthio, InterMune, ProMetic, Roche, Sanofi-Aventis, Takeda, and UCB. MKBW received support from Boehringer Ingelheim for attendance at meetings. RKH has received consultancy fees from Intermune, Roche, and Boehringer Ingelheim. HP has received industry academic research funding from InterMune and consultancy fees from InterMune and Boehringer Ingelheim. YO is an employee of Boehringer Ingelheim Ltd. NM is an employee of Boehringer Ingelheim Ltd. Bryan M. Bennett is an employee of Adelphi Values. Nicola Williamson is an employee of Adelphi Values. Alice Turnbull was an employee of Adelphi Values when this research was conducted.
Compliance with ethics guidelines
All procedures followed were in accordance with the ethical standards of the British Healthcare Business Intelligence Association (BHBIA) Legal and Ethical Framework and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all clinicians for being included in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
References
- 1.American Thoracic Society Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. American Thoracic Society (ATS), and the European Respiratory Society (ERS) Am J Respir Crit Care Med. 2000;161((2 Pt 1)):646–664. doi: 10.1164/ajrccm.161.2.ats3-00. [DOI] [PubMed] [Google Scholar]
- 2.American Thoracic S. European Respiratory S American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002;165(2):277–304. doi: 10.1164/ajrccm.165.2.ats01. [DOI] [PubMed] [Google Scholar]
- 3.Noble PW. Idiopathic pulmonary fibrosis: natural history and prognosis. Clin Chest Med. 2006;27(1):11–16. doi: 10.1016/j.ccm.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal R, Jindal SK. Acute exacerbation of idiopathic pulmonary fibrosis: a systematic review. Eur J Intern Med. 2008;19(4):227–235. doi: 10.1016/j.ejim.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 5.Bjoraker JA, Ryu JH, Edwin MK, et al. Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998;157(1):199–203. doi: 10.1164/ajrccm.157.1.9704130. [DOI] [PubMed] [Google Scholar]
- 6.Flaherty KR, Travis WD, Colby TV, et al. Histopathologic variability in usual and nonspecific interstitial pneumonias. Am J Respir Crit Care Med. 2001;164(9):1722–1727. doi: 10.1164/ajrccm.164.9.2103074. [DOI] [PubMed] [Google Scholar]
- 7.Nicholson AG, Colby TV, du Bois RM, Hansell DM, Wells AU. The prognostic significance of the histologic pattern of interstitial pneumonia in patients presenting with the clinical entity of cryptogenic fibrosing alveolitis. Am J Respir Crit Care Med. 2000;162(6):2213–2217. doi: 10.1164/ajrccm.162.6.2003049. [DOI] [PubMed] [Google Scholar]
- 8.Fell CD. Idiopathic pulmonary fibrosis: phenotypes and comorbidities. Clin Chest Med. 2012;33(1):51–57. doi: 10.1016/j.ccm.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 9.Ryu JH, Colby TV, Hartman TE, editors. Idiopathic pulmonary fibrosis: current concepts. Mayo Clinic Proceedings. Elsevier; 1998. [DOI] [PubMed]
- 10.Selman M, King TE, Pardo A. Idiopathic pulmonary fibrosis: prevailing and evolving hypotheses about its pathogenesis and implications for therapy. Ann Intern Med. 2001;134(2):136–151. doi: 10.7326/0003-4819-134-2-200101160-00015. [DOI] [PubMed] [Google Scholar]
- 11.Du Bois R. Strategies for treating idiopathic pulmonary fibrosis. Nat Rev Drug Discov. 2010;9(2):129–140. doi: 10.1038/nrd2958. [DOI] [PubMed] [Google Scholar]
- 12.García-Sancho C, Buendía-Roldán I, Fernández-Plata M, et al. Familial pulmonary fibrosis is the strongest risk factor for idiopathic pulmonary fibrosis. Respir Med. 2011;105(12):1902. doi: 10.1016/j.rmed.2011.08.022. [DOI] [PubMed] [Google Scholar]
- 13.Ryu JH, Moua T, Daniels CE, et al., editors. Idiopathic pulmonary fibrosis: evolving concepts. Mayo Clinic Proceedings. Elsevier; 2014. [DOI] [PubMed]
- 14.Gribbin J, Hubbard RB, Le Jeune I, Smith CJ, West J, Tata LJ. Incidence and mortality of idiopathic pulmonary fibrosis and sarcoidosis in the UK. Thorax. 2006;61(11):980–985. doi: 10.1136/thx.2006.062836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meltzer EB, Noble PW. Idiopathic pulmonary fibrosis. Orphanet J Rare Dis. 2008;3(8):5. doi: 10.1186/1750-1172-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raghu G, Weycker D, Edelsberg J, Bradford WZ, Oster G. Incidence and prevalence of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2006;174(7):810–816. doi: 10.1164/rccm.200602-163OC. [DOI] [PubMed] [Google Scholar]
- 18.Kim DS. Acute exacerbation of idiopathic pulmonary fibrosis. Clin Chest Med. 2012;33(1):59–68. doi: 10.1016/j.ccm.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Kondoh Y, Taniguchi H, Kawabata Y, Yokoi T, Suzuki K, Takagi K. Acute exacerbation in idiopathic pulmonary fibrosis. Analysis of clinical and pathologic findings in three cases. Chest. 1993;103(6):1808–1812. doi: 10.1378/chest.103.6.1808. [DOI] [PubMed] [Google Scholar]
- 20.Kondo A, Saiki S. Acute exacerbation in idiopathic interstitial pneumonia (IIP) In: Harasawa M, Fukuchi Y, Morinari H, editors. Interstitial pneumonia of unknown etiology. Tokyo: University of Tokyo Press; 1989. [Google Scholar]
- 21.Demedts M, Costabel U. ATS/ERS international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Eur Respir J. 2002;19(5):794–796. doi: 10.1183/09031936.02.00492002. [DOI] [PubMed] [Google Scholar]
- 22.Raghu G, Chang J. Idiopathic pulmonary fibrosis: current trends in management. Clin Chest Med. 2004;25(4):621–636. doi: 10.1016/j.ccm.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 23.Collard HR, Loyd JE, King TE, Jr, Lancaster LH. Current diagnosis and management of idiopathic pulmonary fibrosis: a survey of academic physicians. Respir Med. 2007;101(9):2011–2016. doi: 10.1016/j.rmed.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Collard H, Yow E, Richeldi L, Anstrom K, Glazer C, investigators ftI Suspected acute exacerbation of idiopathic pulmonary fibrosis as an outcome measure in clinical trials. Respir Res. 2013;14(1):73. doi: 10.1186/1465-9921-14-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones J, Hunter D. Qualitative research: consensus methods for medical and health services research. BMJ (Clin Res Ed) 1995;311(7001):376–380. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Avouac J, Fransen J, Walker U, et al. Preliminary criteria for the very early diagnosis of systemic sclerosis: results of a Delphi Consensus Study from EULAR Scleroderma Trials and Research Group. Ann Rheum Dis. 2011;70(3):476–481. doi: 10.1136/ard.2010.136929. [DOI] [PubMed] [Google Scholar]
- 27.Powell BJ, McMillen JC, Proctor EK, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev. 2012;69(2):123–157. doi: 10.1177/1077558711430690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ilic D, Nordin RB, Glasziou P, Tilson JK, Villanueva E. Development and validation of the ACE tool: assessing medical trainees’ competency in evidence based medicine. BMC Med Educ. 2014;14(1):114. doi: 10.1186/1472-6920-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosier PF, De Ridder D, Meijlink J, Webb R, Whitmore K, Drake MJ. Developing evidence-based standards for diagnosis and management of lower urinary tract or pelvic floor dysfunction. Neurourol Urodyn. 2012;31(5):621–624. doi: 10.1002/nau.21253. [DOI] [PubMed] [Google Scholar]
- 30.Dimitrow MS, Airaksinen MS, Kivelä SL, Lyles A, Leikola SN. Comparison of prescribing criteria to evaluate the appropriateness of drug treatment in individuals aged 65 and older: a systematic review. J Am Geriatr Soc. 2011;59(8):1521–1530. doi: 10.1111/j.1532-5415.2011.03497.x. [DOI] [PubMed] [Google Scholar]
- 31.Kerr MP, Mensah S, Besag F, et al. International consensus clinical practice statements for the treatment of neuropsychiatric conditions associated with epilepsy. Epilepsia. 2011;52(11):2133–2138. doi: 10.1111/j.1528-1167.2011.03276.x. [DOI] [PubMed] [Google Scholar]
- 32.Flume PA, Mogayzel PJ, Jr, Robinson KA, Rosenblatt RL, Quittell L, Marshall BC. Cystic fibrosis pulmonary guidelines: pulmonary complications: hemoptysis and pneumothorax. Am J Respir Crit Care Med. 2010;182(3):298–306. doi: 10.1164/rccm.201002-0157OC. [DOI] [PubMed] [Google Scholar]
- 33.Hsu C-C, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12(10):1–8. [Google Scholar]
- 34.Linstone HA, Turoff M. The Delphi method: techniques and applications. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- 35.Clement S, Jarrett M, Henderson C, Thornicroft G. Messages to use in population-level campaigns to reduce mental health-related stigma: consensus development study. Epidemiol Psichiatr Soc. 2010;19(1):72–79. doi: 10.1017/S1121189X00001627. [DOI] [PubMed] [Google Scholar]
- 36.Abe S, Seo Y, Hayashi H, et al. Neutrophil adsorption by polymyxin B-immobilized fiber column for acute exacerbation in patients with interstitial pneumonia: a pilot study. Blood Purif. 2010;29(4):321–326. doi: 10.1159/000287232. [DOI] [PubMed] [Google Scholar]
- 37.Abe S, Azuma A, Mukae H, et al. Polymyxin B-immobilized fiber column (PMX) treatment for idiopathic pulmonary fibrosis with acute exacerbation: a multicenter retrospective analysis. Intern Med. 2012;51(12):1487–1491. doi: 10.2169/internalmedicine.51.6965. [DOI] [PubMed] [Google Scholar]
- 38.Al-Hameed FM, Sharma S. Outcome of patients admitted to the intensive care unit for acute exacerbation of idiopathic pulmonary fibrosis. Can Respir J J Can Thorac Soc. 2004;11(2):117–122. doi: 10.1155/2004/379723. [DOI] [PubMed] [Google Scholar]
- 39.Azuma A, Nukiwa T, Tsuboi E, et al. Double-blind, placebo-controlled trial of pirfenidone in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2005;171(9):1040–1047. doi: 10.1164/rccm.200404-571OC. [DOI] [PubMed] [Google Scholar]
- 40.Cerri S, Spagnolo P, Luppi F, Richeldi L. Management of idiopathic pulmonary fibrosis. Clin Chest Med. 2012;33(1):85–94. doi: 10.1016/j.ccm.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 41.Collard HR, Moore BB, Flaherty KR, et al. Acute exacerbations of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2007;176(7):636–643. doi: 10.1164/rccm.200703-463PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Horita N, Akahane M, Okada Y, et al. Tacrolimus and steroid treatment for acute exacerbation of idiopathic pulmonary fibrosis. Inter Med (Tokyo, Japan) 2010;50(3):189–195. doi: 10.2169/internalmedicine.50.4327. [DOI] [PubMed] [Google Scholar]
- 43.Lynch JP, Saggar R, Weigt SS, Zisman DA, White ES, editors. Usual interstitial pneumonia. Seminars in respiratory and critical care medicine; 2006: Copyright© 2006 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY 10001, USA.
- 44.Richeldi L, Costabel U, Selman M, et al. Efficacy of a tyrosine kinase inhibitor in idiopathic pulmonary fibrosis. N Engl J Med. 2011;365(12):1079–1087. doi: 10.1056/NEJMoa1103690. [DOI] [PubMed] [Google Scholar]
- 45.Sakamoto S, Homma S, Miyamoto A, Kurosaki A, Fujii T, Yoshimura K. Cyclosporin A in the treatment of acute exacerbation of idiopathic pulmonary fibrosis. Intern Med (Tokyo, Japan) 2009;49(2):109–115. doi: 10.2169/internalmedicine.49.2359. [DOI] [PubMed] [Google Scholar]
- 46.Song JW, Hong SB, Lim CM, Koh Y, Kim DS. Acute exacerbation of idiopathic pulmonary fibrosis: incidence, risk factors and outcome. Eur Respir J. 2011;37:356–363. doi: 10.1183/09031936.00159709. [DOI] [PubMed] [Google Scholar]
- 47.Delbecq AL, Van De Ven AH. A group process model for problem identification and program planning. J Appl Behav Sci. 1971;7(4):466–492. doi: 10.1177/002188637100700404. [DOI] [Google Scholar]
- 48.Murphy M, Black N, Lamping D, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess (Winch, Engl). 1998;2(3):i. [PubMed]
- 49.Murphy M, Black N, Lamping D, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess (Winch, Engl) 1997;2(3):i–iv. [PubMed] [Google Scholar]
- 50.Society BT BTS guidelines for home oxygen use in adults. J Br Thorac Soc. 2015;70(1):i1–i43. [Google Scholar]
- 51.Sackman H. Delphi critque. Lexington: Lexington Books; 1975. [Google Scholar]
- 52.Goodman CM. The Delphi technique: a critique. J Adv Nurs. 1987;12(6):729–734. doi: 10.1111/j.1365-2648.1987.tb01376.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.