Abstract
Introduction
Cardiovascular diseases (CVDs) represent a major Public Health burden. High serum cholesterol levels have been linked to major CV risk. The objectives of this study were to review the epidemiology of hypercholesterolemia in high risk CV patients from Spain, by assessing its prevalence, the proportion of diagnosed patients undergoing pharmacological treatment and the degree of attained lipid control.
Methods
A systematic literature review was carried out using Medline and two Spanish databases. Manuscripts containing information on hypercholesterolemia in several high CV risk groups [diabetes mellitus (DM), Systematic COronary Risk Evaluation (SCORE) risk >5, or documented CVD], published between January 2010 and October 2014, were included.
Results
Of the 1947 published references initially retrieved, a full-text review was done on 264 manuscripts and 120 were finally included. Prevalence of hypercholesterolemia ranged from 50 to 84% in diabetics, 30–60% in patients with DM or elevated SCORE risk, 64–74% with coronary heart disease, 40–70% in stroke patients, and 60–80% in those with peripheral artery disease. Despite the finding that most of them were on pharmacological treatment, acceptable control of serum lipids was very variable, ranging from 15% to 65%. Among those with heterozygous familial hypercholesterolemia, 95–100% received treatment but less than 50% achieved their therapeutic goals.
Conclusions
An elevated prevalence of hypercholesterolemia can be found in targeted groups at high CV risk. Although most patients are receiving pharmacological treatment, rates of lipid control continue to be low, both in primary and secondary prevention.
Electronic supplementary material
The online version of this article (doi:10.1007/s12325-015-0252-y) contains supplementary material, which is available to authorized users.
Keywords: Cardiovascular disease, Control, Drug, Dyslipidemia, Hypercholesterolemia, Prevalence
Introduction
The overall prevalence of hypercholesterolemia in the Spanish adult population has been estimated between 34% and 50% in recent studies [1–3]. The importance of this high prevalence is due to the association of high levels of serum cholesterol with cardiovascular disease (CVD), which has been well established [4, 5]. For instance, the occurrence of CV events in patients with familial hypercholesterolemia has been highlighted, with a prevalence of premature CVD (before 55 years of age in men and before 65 years of age in women) of 10%, in contrast to less than 3% in relatives without familial hypercholesterolemia [6].
The therapeutic arsenal available for hypercholesterolemia includes the standard treatment based on lifestyle and dietary modification strategies, and lipid-lowering medications, mainly statins [7]. Other existing treatments for controlling low-density lipoprotein cholesterol (LDLc) levels are ezetimibe (added to statins in primary hypercholesterolemia and homozygous familial hypercholesterolemia or as a monotherapy in cases of statin intolerance or if they are contraindicated), fibrates and bile-acid sequestrants. In addition, newly developed lipid-lowering drugs (monoclonal antibodies proprotein convertase subtilisin/kexin type 9 inhibitor) have been recently approved by the Food and Drug Administration and European Medicines Agency. Lipid-lowering treatments (LLT) are efficacious in reducing LDLc levels and reducing the burden of major CV events as well as CV mortality, even among populations without known CVD [8, 9]. Consequently, recent European Clinical Practice Guidelines have established LDLc targets accordingly to individual’s CV risk [7]: LDLc levels <100 mg/dl for patients without CVD, but with diabetes mellitus (DM) or with high CV risk based on a Systematic COronary Risk Evaluation (SCORE) risk assessment >5 (Primary prevention hereinafter), and <70 mg/dl for patients with overt CVD, i.e., those who have suffered a previous CV event (Secondary prevention). However, according to the results published in a multinational study conducted between 2006 and 2007, despite the use of LLT, a significant proportion of patients did not attain target levels of LDLc [10], which means they still have a significant CV residual risk. Understanding the contemporary magnitude of this condition is of importance to plan additional interventions to reach LDLc targets and to reduce the burden of the related CV events and deaths. Thus, the objectives of the present research were to review the published evidence addressing the prevalence of hypercholesterolemia, the usual clinical management of lipid profile, and the attained control of LDLc levels in patients with high CV risk from Spain.
Methods
A systematic review of the literature was conducted in accordance with the accepted standards [11] and with a research question defined with reference to Patients, Interventions, Comparisons, Outcomes, and Study design (PICOS) (please see Table S1 in the supplementary material for details). The search was run on the second week of October 2014 (from 6th to 10th) in Medline and two Spanish electronic databases: Biblioteca Virtual de la Salud (BVS) and Medes. The search strategies included both controlled and free terms in both English and Spanish languages. The search strategies executed in each electronic public-access libraries are presented in Table S2 in the supplementary material.
The information gathered was manually cross-checked using the relevant references given in the publications included. To select the studies, titles and abstracts were first examined. After this, full text of selected manuscripts was reviewed. The selection criteria for publications were as follows:
Inclusion Criteria
Studies carried out in Spain and focused on lipid levels of patients belonging to one of the following groups: (a) heterozygous familial hypercholesterolemia (HeFH); (b) overt CVD including acute coronary syndrome (ACS), chronic coronary heart disease (CHD), ischemic stroke (IS) and peripheral arterial disease (PAD); (c) DM; or (d) high CV risk. ACS was defined as acute myocardial infarction or unstable angina in the last 12 months. Chronic CHD refers to patients with ACS occurred longer than 12 months, or with stable angina or revascularization. Regarding CV risk, a SCORE risk assessment >5 (tables for countries with low CV risk) or equivalent was considered. Furthermore, according to the objectives described before, the studies had to include information on one of the following results: (a) prevalence of hypercholesterolemia; (b) rates of pharmacological treatment or (c) control of LDLc levels.
Exclusion Criteria
Manuscripts were discarded if any of the following conditions applied: (a) carried out outside Spain; (b) studies that did not include original patient data (i.e., reviews, editorials or letters); (c) studies that did not include human data; (d) studies with pediatric populations or (e) case reports.
Compliance with Ethics Guidelines
This article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by any of the authors.
Results
A total of 1362 publications were retrieved from PubMed, 537 from the BVS and 560 from Medes (512 were duplicates so an initial pool of 1947 original manuscripts were identified for title and abstract review). Following the selection process, the full text of 264 manuscripts was reviewed, of which a total of 120 original papers were finally considered (Fig. 1).
Fig. 1.
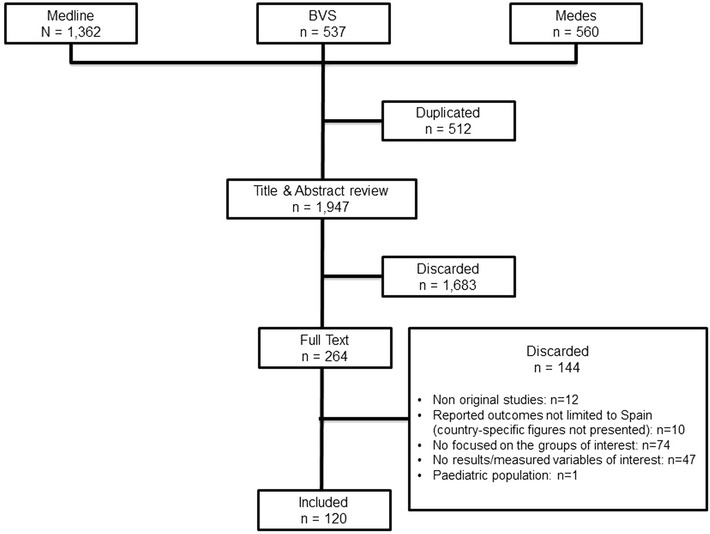
Flow diagram showing the selection process of the included articles. BVS Biblioteca Virtual de la Salud
HeFH
In the study using data from the electronic database of the Spanish Familial Hypercholesterolemia Longitudinal Cohort Study (SAFEHEART) [12], 84% of the HeFH patients were receiving LLT at the time of inclusion (97% index cases and 78% HeFH relatives). 95% of treated patients received statins, 58% as monotherapy and 31% in combination, mostly with ezetimibe. Meanwhile, in another observational study [13] which included 241 patients with HeFH and 286 with combined familial hypercholesterolemia, 100% received LLT during a monitoring period of 1 year. Patients took an average of 1.5 lipid-lowering drugs (94% statins and 33% ezetimibe).
Despite the high proportion of patients undergoing a LLT in both studies [12, 13], between 72% and 96%, approximately, did not reach a target LDLc below 100 mg/dl and only 45% reduced LDLc levels by >50% (Table 1).
Table 1.
Lipid-lowering treatments and LDL cholesterol targets in Heterozygous familial hypercholesterolemia
| Study | Study size | Treatment | Control |
|---|---|---|---|
| [12]a | N = 1852 (1262 FH and 590 relatives non FH) |
LLT: 83.7% (97% FH and 78% relatives FH) Statins monotherapy: 58.3% Statin + ezetimibe: 31.3% |
LDLc <100 mg/dl: 33 (3.4%) of FH on LLT |
| [13]b | N = 527 (241 HeFH and 286 combined FH) |
LLT: 100% 1 year after study entry Statins: 94.3% Ezetimibe: 33.4% |
LDLc <100 mg/dl: 28.5% |
| [14] | 37 HeFH and 37 controls |
Statins: 100% HeFH and 100% no-HeFH Ezetimibe: 23 (62.2%) HeFH; 4 (10.8%) no-HeFH |
LDLc <100 mg/dl: 11% of HeFH |
LLT lipid-lowering treatment, FH familiar hypercholesterolemia, LDLc low-density lipoprotein cholesterol, HeFH heterozygous familial hypercholesterolemia
aOnly 13% received maximum daily statin doses, defined as simvastatin 80 mg, pravastatin 40 mg, lovastatin 80 mg, fluvastatin 80 mg, atorvastatin 80 mg, rosuvastatin 20–40 mg or maximum statin dose plus ezetimibe 10 mg/day
bThe strength of the lipid-lowering treatment in HeFH patients was considered low (lovastatin 10–40 mg, fluvastatin 80 mg, pravastatin 20–40 mg, simvastatin 10–20 mg, atorvastatin 10 mg) in 6.9% of cases, moderate (lovastatin 80 mg, simvastatin 40 mg, atorvastatin 20–40 mg, rosuvastatin 5–10 mg, simvastatin + ezetimibe 20 + 10 mg) in 40% and high (atorvastatin 80 mg, rosuvastatin 20 mg, simvastatin + ezetimibe 40 + 10 mg) in 53%
Hypercholesterolemia in Secondary Prevention
ACS
In studies carried out among patients with ACS the prevalence of hypercholesterolemia was highly variable ranging from 45% to 80% [15–31]. The proportion of ACS patients undergoing LLT ranged between 33% and 90%, but control levels were poor with only 14% of patients with LDLc levels <70 mg/dl and 56% meeting the target of LDLc <100 mg/dl [26] (Table 2; Fig. 2).
Table 2.
Lipid-lowering treatments and LDL cholesterol targets in secondary prevention
| Study | Study size | Treatment | Control |
|---|---|---|---|
| Acute coronary syndrome (ACS) | |||
| [26] | N = 4334 |
Statins: 90.8% Statins + ezetimibe: 24.7% |
LDLc <70 mg/dl: 14.3% LDLc <100 mg/dl: 55.7% |
| [28] | N = 1381 |
LDLc <70 mg/dl: 11% first ACS; 14.1% recurrent ACS LDLc 70–99 mg/dl: 24.1% first ACS; 23.2% recurrent ACS |
|
| Coronary heart disease (CHD) | |||
| [32] | N = 7600 | Statins: 80.6% | LDLc <100 mg/dl: 26.1% |
| [33] | N = 1452 (5256 visits) | Statins: 92.1% |
LDLc <70 mg/dl: 292 (5.7%) LDLc 70–100 mg/dl (non DM): 916 (18%) LDLc 70–100 mg/dl (DM): 640 (12.6%) LDLc >100 mg/dl: 3244 (63.7%) |
| [34] | N = 1108 | Statins: 967 (87.3%); non DM: 678 (85.8%); DM 289 (90.9%) | LDLc <100 mg/dl: 454 (41%); non DM: 301 (38.1%); DM: 153 (48.1%) |
| [35] | N = 7823 | Statins: 80.4% | LDLc >100 mg/dl: 73.8% |
| [36] | N = 1038 |
Statins: 82.9%; 82.8% >65 years; 83.1% ≤65 years Ezetimibe 17.4%; 16.2% >65 years; 18.7% ≤65 years |
LDLc <100: 42.4% >65years; 46.5% ≤65 years |
| [37] | N = 2292 |
Statins: 94.1% Statins monotherapy: 74% Ezetimibe: 18.3% |
LDLc >100 mg/dl: 44.9% |
| [38] | N = 2024 | LDLc <100 mg/dl- BMI 20-24.9: 35.2%; BMI 25–29.9: 30.5%; BMI ≥30: 27.9%. | |
| Ischemic stroke | |||
| [39] | N = 473 |
LLT: 319 (67.4%) Statins: 311 (65.8%) |
LDLc <100 mg/dl: 33% |
| [40] | N = 955 |
LLT: 75.5% Statins: 695 (72.8%) Ezetimibe: 76 (8%) |
LDLc <100 mg/dl: 28.9% of treated patients |
| [41] | N = 407 |
LLT: 193 (47.4%): Statins: 180 (44.2%) |
LDLc <100 mg/dl: 101 (24.8%); LDLc >100 mg/dl: 139 (34.2%); unknown: 167 (41.0%) |
| Peripheral arterial disease (PAD) | |||
| [42] | N = 4087 |
LLT: 79.1% Statins: 76.2% |
LDLc <100 mg/dl: 30.4% |
| [43] | N = 105 | LLT: 45.7% | |
LLT lipid-lowering treatment, FH familiar hypercholesterolemia, DM diabetes mellitus, LDLc low-density lipoprotein cholesterol, ACS acute coronary syndrome, CHD coronary heart disease, BMI body mass index
Fig. 2.
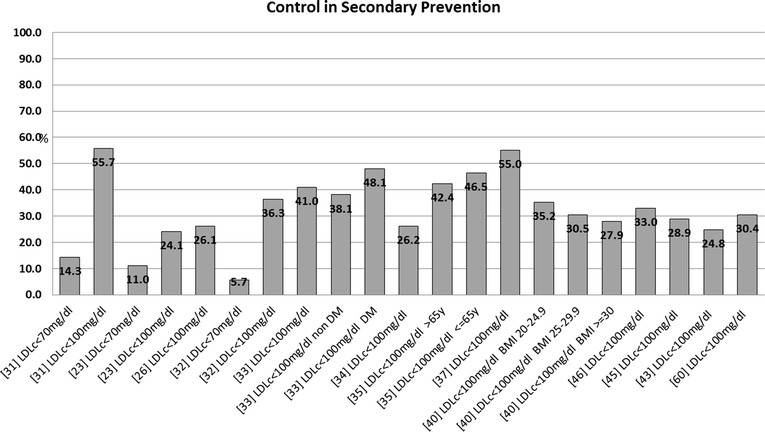
Control in secondary prevention. LDLc low-density lipoprotein cholesterol, DM diabetes mellitus, BMI body mass index
CHD
The prevalence of hypercholesterolemia in patients with chronic CHD was more uniform than that found in patients with ACS, according to the information collected, ranging from 64% to 74% [32–38, 44–46]. More than 80% of patients were receiving LLT, statins accounting for 95% of them [37]. Again, despite the high proportion of treatment, only between 26% and 55% of patients had LDLc levels <100 mg/dl (Table 2).
IS
The prevalence of hypercholesterolemia in patients with IS ranged from 40% to 70% [39–41, 47–60]. The proportion of treated patients was lower than that found in ACS or CHD patients. Upon discharge from hospital following an IS episode, between 38% and 76% of patients were receiving LLT [39, 40, 49]. In addition, one observational study with 203 patients admitted for medium- to long-term stays in one hospital between 2009 and 2010 found that only 20% of the total number of post-event patients received the dosage recommended by current guidelines [54].
With regards to attained cholesterol levels, 3 studies were found [39–41], reporting figures on LDLc control of <100 mg/dl between 25% and 33%. In two additional studies [54, 61] in which targets were set at Total Cholesterol (TC) < 175 mg/dl, control rates were between 43% and 77% (Table 2; Fig. 2).
PAD
A very limited number of studies were identified for this particular subgroup [42, 62–64]. In these studies, the clinical diagnosis of PAD was based on an ankle-brachial index <0.9. A prevalence of hypercholesterolemia between 60% and 80% was reported. With regard to treatment applied and results achieved, between 46% and 79% of patients received LLT. However, only 30% of them achieved a target LDLc <100 mg/dl (Table 2; Fig. 2).
Hypercholesterolemia in Primary Prevention
DM
In accordance with a previous diagnosis or the use of LLT, data indicated that between 50% and 84% of DM patients would present with hypercholesterolemia [44, 57, 65–68].
Regarding the rates of LLT usage (Table 3; Fig. 3), between 45% and 90% of DM patients were using a LLT [26, 69, 70]. With respect to the lipid control achieved in this population, rates ranged from 40% to 50% in DM patients with no CVD history (LDLc goal <100 mg/dl), to only 15% in DM patients with a history of CVD (LDLc goal <70 mg/dl).
Table 3.
Lipid-lowering treatments and LDL cholesterol targets in primary prevention: diabetes mellitus
| Study | Study size | Treatment | Control |
|---|---|---|---|
| [33] | N = 1452 (612 DM) patients; 5256 visits | Statins: 92.1% |
LDLc <70 mg/dl: 292 (5.7%) LDLc 70–100 mg/dl non DM: 916 (18%) LDLc 70–100 mg/dl DM: 640 (12.6%) LDLc >100 mg/dl: 3244 (63.7%) |
| [71] | N = 3703 (1445 DM) | Statins: 100% (during at least 3 months) |
LDLc >100 mg/dl: 59.2% of DM patients LDLc >100 mg/dl: 44.5% of non DM patients |
| [72] | N = 1828 (320 DM). 2 visits |
At baseline, 55.4% received ≥1 drug: Statins: 830 (45.4%) Ezetimibe: 126 (6.9%) Statin + ezetimibe: 8 (0.4%) At follow up: Statins: 1232 (67.4%) Ezetimibe: 332 (18.2%) Statin + ezetimibe: 61 (3.3%) |
LDLc <100 mg/dl in DM or CVD and LDLc <115 in high risk patients: Baseline: All 30.5%; CVD 40.4%; DM 35.8% Follow up: All 44.7%; CVD 65.3%; DM 50.4% LDLc <70: CVD 17.9%; DM 16.5% |
| [26] | N = 4402 (1748 DM) |
Statins: 76.7%: Statins + ezetimibe: 18.8% |
LDLc >100 mg/dl: 56.9% LDLc >70 mg/dl: 84.7% |
| [73] | N = 3710 (39% DM) |
Statins: 100% Ezetimibe: 17.4% |
LDLc >100 mg/dl in high risk or >120 mg/dl in low risk: 63.1% CVD (n = 846); LDLc >100 mg/dl: 64.7% |
| [3] |
N = 11,544 Rate of awareness: 53.6% (53.5% males; 53.7% women) |
LLT treatment: 44.1% of patients aware of elevated LDLc 23.7% of all patients with elevated LDLc |
LDLc <115 mg/dl (<100 mg/dl DM and CVD): 40.2% of treated patients (9.5% of total sample with elevated LDLc) LDLc <115 mg/dl (<70 DM and CVD): 31.3% (7.3%) % of DM or CVD patients with LDLc <100 mg/dl: 40.5% or 43.6%, respect % of DM or CVD patients with LDLc <70 mg/dl: 7.0% or 5.2% respectively |
| [67] | N = 2412 |
Before clinical session: Statins: 59.5% Ezetimibe: 0.9% At clinical session: Statins: 65.5% Ezetimibe: 4.2% |
Before clinical session: LDLc <100 mg/dl: 22.7% At clinical session: LDLc <100 mg/dl: 28.6% |
| [68] | N = 1177 | Statins 48% | LDLc <100 mg/dl: 25.6% |
| [74] | N = 4776 (12.5% DM patients) |
In n = 409 DM patients LDL ≤100 mg/dl: 45.3% LDL ≤70 mg/dl: 11.8% |
|
| [66] | N = 771 DM |
Statin: 722 (93.6%) Ezetimibe: 151 (19.6%) |
LDLc >70 mg/dl: 501 (73.4%) LDLc >100 mg/dl: 243 (31.5%) |
| [75] | N = 2704 (1067 DM) | LLT: 1634 (60.4%) |
LDLc <100 mg/dl in DM or CVD; <130 mg/dl others: 930 (34.4%) LDLc <100 mg/dl: 34.7% DM; 34.2% CVD |
| [76] |
N = 1748 DM and CHD N = 2654 DM without CHD |
LLT: 76.7% Statin and ezetimibe: 18.8% |
LDLc >100 mg/dl: 56.9% LDLc >70 mg/dl: 84.7% |
| [69] | N = 320 DM | Statins: 60% | LDLc ≤100 mg/dl: males 41.7%; females 39.1% |
LLT lipid-lowering treatment, FH familiar hypercholesterolemia, DM diabetes mellitus, CVD cardiovascular disease, LDLc low-density lipoprotein cholesterol, CHD coronary heart disease
Fig. 3.
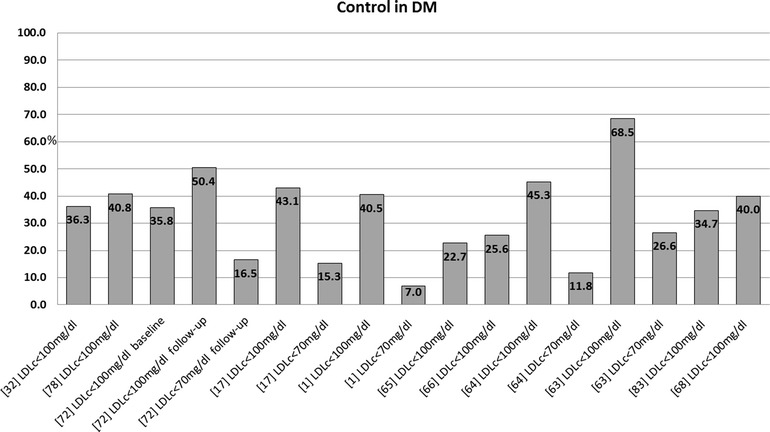
Control in primary prevention: diabetes mellitus. LDLc low-density lipoprotein cholesterol, DM diabetes mellitus
Patients with High CV Risk
Within this group of special interest in the prevention of CVD, between 30% and 60% had a specific diagnosis of hypercholesterolemia, based on a TC >200 mg/dl or previous treatment [1, 3, 76–78].
LLT was used in 50% to 60% of these patients [1], while control rates ranged from 35% to 65%, considering a LDLc target of <100 mg/dl [1, 72, 73]. Table 4 and Fig. 4 summarize these data.
Table 4.
Lipid-lowering treatments and LDL cholesterol targets in primary prevention: high cardiovascular risk patients
| High or very high cardiovascular risk | |||
|---|---|---|---|
| Study | Study size | Treatment | Control |
| [73] | N = 3710 (39% DM) |
Statins: 100% Ezetimibe: 17.4% |
High risk patients (CVD, DM or SCORE >5%; n = 2574), LDLc >100 mg/dl: 60.7% SCORE >5% without CVD nor DM (n = 407), LDLc >100 mg/dl: 83.2% |
| [72] | N = 1828 2 visits |
At baseline, 1013 (55.4%) received at least 1 drug: Statins: 830 (45.4%) Ezetimibe: 126 (6.9%) Statin + ezetimibe: 8 (0.4%) At follow up: Statins: 1232 (67.4%) Ezetimibe: 332 (18.2%) Statin + ezetimibe: 61 (3.3%) |
LDLc levels <100 mg/dl in DM or CVD and LDLc <115 in high risk patients: Baseline: All 30.5%; CVD 40.4%; DM 35.8% Follow up: All 44.7%; CVD 65.3%; DM 50.4% LDLc <70 mg/dl: CVD 17.9%; DM 16.5% |
| [79] |
RCT. 2 arms: Experimental-EG (n = 33) Supportive system to decision making Control-CG (n = 44) |
Use of High intensity statins: EG: 74.6%/CG: 25.4% Statins + ezetimibe or niacin/laropiprant: GI: 32.4%/GC: 2.3% |
After 12 weeks: LDLc <70: 55% GI; 12.5% GC LDLc <100: 75% GI; 45.8% GC |
| [80] | N = 37 |
Statins: 100% Ezetimibe: 10.8% |
LDLc <130 md/dl: 43% |
| [81] | N = 222. | LLT: 85% |
LDLc <100 mg/dl: 51.3% of high risk patients LDLc <70 mg/dl: 7.5% of high risk patients |
| [77] | N = 3716 (15.5% calibrated-SCORE >5) | Statins: 25.3% |
Patients with SCORE between 5 and 10: LDLc <100 mg/dl: 10.61% SCORE >10 LDLc <70 mg/dl: 1.79% |
| [1] | N = 27,903 (n = 9335 with dyslipidemia) High–very high risk: 11.3% males and 2.3% female | LLT REGICOR >10: 50% males, 59% females |
LDLc <100 mg/dl in DM or high–very high risk: <3% LDLc <100 mg/dl in DM or <130 mg/dl in moderate to very high risk or <160 mg/dl in low risk): 46% males, 52% females |
| [75] | N = 2704 | LLT: 1634 (60.4%) |
LDLc <100 mg/dl in DM or CVD; <130 mg/dl others: 930 (34.4%) LDLc <100 mg/dl: 34.7% DM; 34.2% CVD |
| [82] | N = 217 |
Ezetimibe (monotherapy): 42.4% Ezetimibe + statins: 43.3% |
LDLc <100 mg/dl or 70 mg/dl: 43.8% of high or very high risk patients |
| [3] |
N = 11,544 Rate of awareness: 53.6% (53.5% males; 53.7% women) |
LLT treatment: 44.1% of patients aware of elevated LDLc 23.7% of all patients with elevated LDLc |
LDLc <115 mg/dl (<100 DM and CVD): 40.2% of treated patients (9.5% of total sample with elevated LDLc) LDLc <115 mg/dl (<70 DM and CVD): 31.3% (7.3%) % of DM or CVD patients with LDLc < 100 mg/dl: 40.5% or 43.6%, respect. % of DM or CVD patients with LDLc <70 mg/dl: 7.0% or 5.2% respectively |
LLT lipid-lowering treatment, FH familiar hypercholesterolemia, DM diabetes mellitus, CVD cardiovascular disease, LDLc low-density lipoprotein cholesterol, EG experimental group, CG control group
Fig. 4.
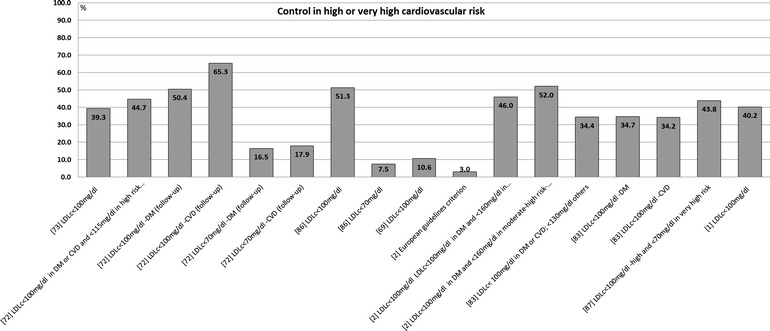
Control in primary prevention: high or very high risk patients. LDLc low-density lipoprotein cholesterol, DM diabetes mellitus, CVD cardiovascular disease
Discussion
It has been shown that hypercholesterolemia is significantly present among patients with an increased vascular risk and those who have already suffered a CV event: 50–84% of patients with DM [44, 57, 67, 68, 74], 30–50% of high risk patient [1, 3, 76–78], and between 35% and above 80% in those with overt CVD, depending on the type of event [15–41, 44–60]. The association of this condition with the risk of CV events [9, 83] makes it all the more necessary to endorse the interventions aimed at managing the modifiable risk factors (diet and exercise), to prescribe a LLT accordingly to individual’s CV risk [7], and also to plan an adequate monitoring of the pharmacological therapies implemented to maximize their benefit. There are many examples of this relationship in our country: hypercholesterolemia doubled the risk of an ischemic disease [84, 85], and would be the cause of 22% of all coronary events. The risk increased significantly among patients who did not have their lipid values controlled, while among those diagnosed with controlled hypercholesterolemia and, who are undergoing a lipid-lowering treatment, the increased risk of ischemic heart disease was not statistically significant [84].
Due, in large part, to the information above, the use of lipid-lowering drugs in Spain has increased from 18.9 defined daily doses (DDD) per 1000 inhabitants per day (DDD/1000 inhabitants/day) in the year 2000 to 102.6 DDD/1000 inhabitants/day in the year 2012, an increase of 442% [86]. Statins are the most commonly used drugs (91.7 DDD/1000 inhabitants/day in 2012) representing 89.3% of all LLT, but also fibrates, bile-acid sequestrants, ezetimibe, and omega 3 fatty acids contributed during 2012 to LLT use [86]. The increase in the use of LLT can be justified by their ability to reduce the risk of CV events, and the associated burden of disease.
Although treatments available have led to an improvement in the clinical situation and prognosis of these cases, it is clear that there is a lot of effort still to be made until LDLc targets defined by current European guidelines [7] can be reached by most of patients. In all of the groups analyzed, an important number could still be found with total cholesterol and LDLc levels above the acceptable threshold. For example, among diabetics, only between 15% (in case of those with previous CVD) and 40–50% (in those without CVD) attained recommended levels of lipids in the blood [26, 69–71], and the situation is not better in secondary prevention or among patients with HeFH. This picture, which is similar to other western countries [87–89], highlights the need to continue maximizing the control of lipids in the blood and to minimize therapeutic inertia. Regarding this, in one recent study with CHD patients, therapeutic inertia was estimated to be as high as 73% [33].
It should be noted, as the main limitation of the present work, how difficult it is to make a more exact approximation of the estimations presented in this manuscript. This is due in great part to the sheer heterogeneity of the criteria used in the various studies in defining hypercholesterolemia, CV risk, ACS or CHD. In addition, one other relevant aspect to consider is the nature of the studies included. They are mainly cross-sectional investigations and with a wide range of different sampling procedures and sample sizes. Even more, many studies are based on the analysis of individuals coming from the same national databases or registries. Considering these important constraints, a more analytic approach as meta-analysis might be applied at least with those studies following comparable clinical criteria to have a more accurate estimation of disease prevalence and control in each of the groups of interest, and to highlight the significance of the heterogeneity found between studies. Despite this, an important strength of the present manuscript is that all the relevant studies carried out in Spain and published in peer review journals have been systematically identify and reviewed to facilitate a global but comprehensive report of this condition in our country.
Conclusions
There is an elevated prevalence of hypercholesterolemia in Spain among those selected groups with a high CV risk. Although LLT is present in an elevated proportion, controls rates of lipid levels need to be improved both in primary and secondary prevention.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
Sponsorship, article processing charges, and the open access charge for this study were funded by Sanofi Iberia. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Disclosures
Marta Rubio works at the Health Economics and Outcomes Research department of Sanofi Iberia. Rudi Subirà works at the Health Economics and Outcomes Research department of Sanofi Iberia. Alex de la Sierra has served as a scientific advisor to Sanofi and declares honoraria for participation in advisory board/scientific meetings funded by Abbott, Daiichi-Sankyo, Lacer, Menarini, Merck, Sharp and Dohme, Pfizer, and Sanofi. Xavier Pintó has served as a scientific advisor to Sanofi. Carlos Guijarro has served as a scientific advisor to Sanofi and declares honoraria as a speaker or consultant from Sanofi, MSD, Astra Zeneca. José López Miranda has served as a scientific advisor to Sanofi and declares fees for participation in advisory board/scientific meetings from Sanofi. Daniel Callejo has served as a scientific advisor to Sanofi. Jesús Cuervo has served as a scientific advisor to Sanofi.
Compliance with ethics guidelines
This article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
References
- 1.Baena-Díez JM, Félix FJ, Grau M, Cabrera De León A, Sanz H, Leal M, et al. Tratamiento y control de los factores de riesgo según el riesgo coronario en la población española del estudio DARIOS. Rev Esp Cardiol. 2011;64:766–73. 10.1016/j.recesp.2011.04.019 [DOI] [PubMed] [Google Scholar]
- 2.Grau M, Elosua R, Cabrera De León A, Guembe MJ, Baena-Díez JM, Vega Alonso T, et al. Factores de riesgo cardiovascular en España en la primera década del siglo XXI: análisis agrupado con datos individuales de 11 estudios de base poblacional, estudio DARIOS. Rev Esp Cardiol. 2011;64:295–304. 10.1016/j.recesp.2010.11.005 [DOI] [PubMed] [Google Scholar]
- 3.Guallar-Castillón P, Gil-Montero M, León-Muñoz LM, Graciani A, Bayán-Bravo A, Taboada JM, et al. Magnitud y manejo de la hipercolesterolemia en la población adulta de España, 2008–2010: el estudio ENRICA. Rev Esp Cardiol. 2012;65:551–8. 10.1016/j.recesp.2012.02.005 [DOI] [PubMed] [Google Scholar]
- 4.Alzamora MT, Fores R, Baena-Diez JM, Pera G, Toran P, Sorribes M, et al. The peripheral arterial disease study (PERART/ARTPER): prevalence and risk factors in the general population. BMC Public Health. 2010;10:38. 10.1186/1471-2458-10-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramos R, Balló E, Marrugat J, Elosua R, Sala J, Grau M, et al. Validez del Sistema de Información para el Desarrollo de la Investigación en Atención Primaria (SIDIAP) en el estudio de enfermedades vasculares: estudio EMMA. Validity for use in research on vascular diseases of the SIDIAP (Information System for the Development of Research in Primary Care): the EMMA study. Rev Esp Cardiol. 2012;65(1):29–37. 10.1016/j.recesp.2011.07.017 [DOI] [PubMed] [Google Scholar]
- 6.Alonso R, Andres E, Mata N, Fuentes-Jimenez F, Badimon L, Lopez-Miranda J, et al. Lipoprotein(a) levels in familial hypercholesterolemia: an important predictor of cardiovascular disease independent of the type of LDL receptor mutation. J Am Coll Cardiol. 2014;63(19):1982–9. 10.1016/j.jacc.2014.01.063 [DOI] [PubMed] [Google Scholar]
- 7.Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012;33(13):1635–701. 10.1093/eurheartj/ehs092 [DOI] [PubMed] [Google Scholar]
- 8.Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–81. 10.1016/S0140-6736(10)61350-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581–90. 10.1016/S0140-6736(12)60367-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waters DD, Brotons C, Chiang CW, Ferrieres J, Foody J, Jukema JW, et al. Lipid treatment assessment project 2: a multinational survey to evaluate the proportion of patients achieving low-density lipoprotein cholesterol goals. Circulation. 2009;120(1):28–34. 10.1161/CIRCULATIONAHA.108.838466 [DOI] [PubMed] [Google Scholar]
- 11.Perestelo-Pérez L. Standards on how to develop and report systematic reviews in Psychology and Health. Int J Clin Health Psychol. 2013;13:49–57. 10.1016/S1697-2600(13)70007-3 [DOI] [Google Scholar]
- 12.Mata N, Alonso R, Badimon L, Padro T, Fuentes F, Muniz O, et al. Clinical characteristics and evaluation of LDL-cholesterol treatment of the Spanish Familial Hypercholesterolemia Longitudinal Cohort Study (SAFEHEART). Lipids Health Dis. 2011;10:94. 10.1186/1476-511X-10-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lahoz C, Mostaza JM, Pinto X, de la Cruz JJ, Banegas JR, Pedro-Botet J. LDL-cholesterol control in patients with genetic dyslipidemia followed up by Lipid and Vascular Risk Units of the Spanish Society of Arteriosclerosis. Clin Investig Arterioscler. 2015;27(1):1–8. 10.1016/j.arteri.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 14.Suades R, Padro T, Alonso R, Lopez-Miranda J, Mata P, Badimon L. Circulating CD45+/CD3+ lymphocyte-derived microparticles map lipid-rich atherosclerotic plaques in familial hypercholesterolaemia patients. Thromb Haemost. 2014;111(1):111–21. 10.1160/TH13-07-0612 [DOI] [PubMed] [Google Scholar]
- 15.Aros F, Heras M, Vila J, Sanz H, Ferreira-Gonzalez I, Permanyer-Miralda G, et al. Reduction in 28 days and 6 months of acute myocardial infarction mortality from 1995 to 2005. Data from PRIAMHO I, II and MASCARA Registries. Rev Esp Cardiol (Engl Ed). 2011;64(11):972–80. 10.1016/j.recesp.2011.05.011 [DOI] [PubMed] [Google Scholar]
- 16.Cordero A, Moreno-Arribas J, Bertomeu-González V, Agudo P, Miralles B, Masiá M, et al. Las concentraciones bajas de colesterol unido a las lipoproteínas de alta densidad se asocian de manera independiente a enfermedad coronaria aguda en pacientes que ingresan por dolor torácico. Rev Esp Cardiol. 2012;65:319–25. 10.1016/j.recesp.2011.07.022 [DOI] [PubMed] [Google Scholar]
- 17.Cordero A, Lopez-Palop R, Bertomeu-González V, Carrillo P, Moreno-Arribas J, Bertomeu-Martínez V. Perfil clínico y pronóstico de los pacientes con síndrome coronario agudo y colesterol unido a lipoproteínas de baja densidad <70 mg/dl. Rev Esp Cardiol. 2013;66:588–9. 10.1016/j.recesp.2013.01.012 [DOI] [PubMed] [Google Scholar]
- 18.Cordero A, Lopez-Palop R, Carrillo P, Miralles B, Masiá M, Bertomeu-Martínez V. Valor pronóstico de la escala INTERHEART-colesterol para pacientes que ingresan por dolor torácico. Rev Esp Cardiol. 2014;67:578–80. 10.1016/j.recesp.2014.02.013 [DOI] [PubMed] [Google Scholar]
- 19.Cubedo J, Padro T, Alonso R, Cinca J, Mata P, Badimon L. Differential proteomic distribution of TTR (pre-albumin) forms in serum and HDL of patients with high cardiovascular risk. Atherosclerosis. 2012;222(1):263–9. 10.1016/j.atherosclerosis.2012.02.024 [DOI] [PubMed] [Google Scholar]
- 20.Garcia-Moll X, Fácila L, Conthe P, Zapata A, Artigas R, Bertomeu V, et al. ¿Cómo se usan los bloqueadores beta en España? Análisis de las limitaciones para su uso en medicina interna y cardiología: estudio CARACTER-BETA. Rev Esp Cardiol. 2011;64:883–90. 10.1016/j.recesp.2011.05.023 [DOI] [PubMed] [Google Scholar]
- 21.Jover A, Corbella E, Muñoz A, Millán J, Pintó X, Mangas A, et al. Prevalencia del síndrome metabólico y de sus componentes en pacientes con síndrome coronario agudo. Rev Esp Cardiol. 2011;64:579–86. 10.1016/j.recesp.2011.03.010 [DOI] [PubMed] [Google Scholar]
- 22.Machon M, Basterretxea M, Martinez-Camblor P, Aldasoro E, Vicente JM, Larranaga N. Sex differences in relative survival and prognostic factors in patients with a first acute myocardial infarction in guipuzcoa, Spain. Rev Esp Cardiol (Engl Ed). 2010;63(6):649–59. 10.1016/S0300-8932(10)70157-3 [DOI] [PubMed] [Google Scholar]
- 23.Martinez-Quintana E, Rodriguez-Gonzalez F, Nieto-Lago V, Novoa FJ, Lopez-Rios L, Riano-Ruiz M. Serum glucose and lipid levels in adult congenital heart disease patients. Metabolism. 2010;59(11):1642–8. 10.1016/j.metabol.2010.03.014 [DOI] [PubMed] [Google Scholar]
- 24.Millán J, Pedro-Botet J, Muñoz A, Corbella E, Mangas A, Zúñiga M, et al. Perfil lipídico residual en la cardiopatía isquémica recurrente. Med Clin (Barc). 2012;138:238–41. 10.1016/j.medcli.2011.01.010 [DOI] [PubMed] [Google Scholar]
- 25.Olivencia PL, Bueno CA, Soto Blanco JM, Yuste Ossorio ME, Barranco RF. Acute coronary syndrome in women. Gender differences. Med Clin (Barc). 2011;137(14):623–30. 10.1016/j.medcli.2011.03.039 [DOI] [PubMed] [Google Scholar]
- 26.Pérez De Isla L, Saltijeral Cerezo A, Vitale G, González Timón B, Torres Do Rego A, Álvarez-Sala Walther LA. Prevalencia de colesterol LDL inadecuado en pacientes con enfermedad coronaria y/o diabetes mellitus tipo 2 (Prevalence of inappropriate LDL cholesterol levels in patients with coronary disease and/or type 2 diabetes). Rev Clin Esp. 2012;212(10):475–81. 10.1016/j.rce.2012.07.003 [DOI] [PubMed] [Google Scholar]
- 27.Pineda J, Marin F, Marco P, Roldan V, Valencia J, Ruiz-Nodar JM, et al. The prognostic value of biomarkers after a premature myocardial infarction. Int J Cardiol. 2010;143(3):249–54. 10.1016/j.ijcard.2009.02.019 [DOI] [PubMed] [Google Scholar]
- 28.Rodríguez-Roca GC, Rodríguez-Padial L, Alonso-Moreno FJ, Romero-Gutiérrez A, Akerström F, Segura-Fragoso A, et al. Perfil lipídico en pacientes ingresados por síndrome coronario agudo en España: datos del área sanitaria de Toledo entre los años 2005 y 2008. Semergen. 2013;39:298–303. 10.1016/j.semerg.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 29.Ruiz-Bailén M, Romero-Bermejo FJ, Expósito-Ruiz M, Zamora-Zamora F, Martínez-Ramírez MJ, Castillo-Rivera AM, et al. Tratamiento precoz con estatinas en el infarto agudo de miocardio. Med Intensiv. 2014;38:11–20. 10.1016/j.medin.2012.12.009 [DOI] [PubMed] [Google Scholar]
- 30.Sanfelix-Gimeno G, Peiro S, Ferreros I, Perez-Vicente R, Librero J, Catala-Lopez F, et al. Adherence to evidence-based therapies after acute coronary syndrome: a retrospective population-based cohort study linking hospital, outpatient, and pharmacy health information systems in Valencia, Spain. J Manag Care Pharm. 2013;19(3):247–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sicras-Mainar A, Fernández De Bobadilla J, Navarro-Artieda R, Martín I, Varela-Moreno C. Morbimortalidad y consumo de recursos asociados tras síndrome coronario agudo en una población española. Rev Clin Esp. 2011;211:560–71. 10.1016/j.rce.2011.07.007 [DOI] [PubMed] [Google Scholar]
- 32.Lahoz C, Mostaza J, Mantilla M, Taboada M, Tranche S, López-Rodríguez I, et al. Prevalencia de síndrome metabólico en pacientes con enfermedad coronaria estable: objetivos terapéuticos y utilización de fármacos cardiovasculares. Rev Clin Esp. 2011;211:1–8. 10.1016/j.rce.2010.05.018 [DOI] [PubMed] [Google Scholar]
- 33.Lázaro P, Murga N, Aguilar D, Hernández-Presa MA. Inercia terapéutica en el manejo extrahospitalario de la dislipemia en pacientes con cardiopatía isquémica. Estudio Inercia. Rev Esp Cardiol. 2010;63:1428–37. 10.1016/S0300-8932(10)70269-4 [DOI] [PubMed] [Google Scholar]
- 34.Otero-Raviña F, Mazon-Ramos P, Grigorian-Shamagian L, Nores-Lorenzo A, Zugaza-Gurruchaga L, Seoane-Blanco R, et al. Effect of diabetes on the clinical characteristics and prognosis of patients with chronic ischemic heart disease. The CIBAR study. Rev Esp Cardiol. 2010;63(11):1371–6. 10.1016/S0300-8932(10)70307-9 [DOI] [PubMed] [Google Scholar]
- 35.Lahoz C, Mostaza JM, Tranche S, Martin-Jadraque R, Mantilla MT, Lopez-Rodriguez I, et al. Atherogenic dyslipidemia in patients with established coronary artery disease. Nutr Metab Cardiovasc Dis. 2012;22(2):103–8. 10.1016/j.numecd.2010.04.010 [DOI] [PubMed] [Google Scholar]
- 36.Barrios V, Escobar C, Murga N, Quijano JJ. Clinical profile and management of patients with chronic ischemic heart disease according to age in the population daily attended by cardiologists in Spain: the ELDERCIC study. Eur J Intern Med. 2010;21(3):180–4. 10.1016/j.ejim.2010.01.003 [DOI] [PubMed] [Google Scholar]
- 37.González-Juanatey JR, Cordero A, Vitale GC, González-Timón B, Mazón P, Bertomeu V. Magnitud y características del riesgo residual lipídico en pacientes con antecedentes de revascularización coronaria: estudio ICP-Bypass. Rev Esp Cardiol. 2011;64:862–8. 10.1016/j.recesp.2011.05.022 [DOI] [PubMed] [Google Scholar]
- 38.Barrios V, Escobar C, Calderon A. Clinical profile and management of patients with hypertension and chronic ischemic heart disease according to BMI. Obesity (Silver Spring). 2010;18(10):2017–22. 10.1038/oby.2010.12 [DOI] [PubMed] [Google Scholar]
- 39.Vidal-Pérez R, Otero-Raviña F, Domínguez-López J, Fabeiro-Romero D, Gómez-Vázquez JL, de Blas-Abad P, et al. Características clínicas y pronóstico de pacientes con enfermedad cerebrovascular crónica (estudio ICBAR). Rev Neurol. 2011;53:449–56. [PubMed] [Google Scholar]
- 40.Abellán Alemán J, Ruilope Urioste LM, Leal Hernández M, Armario García P, Tiberio López G, Martell Claros N. Control de los factores de riesgo cardiovascular en pacientes con ictus atendidos en Atención Primaria en España. Estudio ICTUSCARE. Med Clin (Barc). 2011;136:329–35. 10.1016/j.medcli.2010.04.035 [DOI] [PubMed] [Google Scholar]
- 41.Rubio Gil E, Martínez Pastor A, López-Picazo Ferrer J, Leal Hernández M, Morales Ortiz A, Martinez Navarro A, et al. Calidad del registro en OMI-AP de los pacientes con ictus seguidos en atención primaria quality of records in OMI-AP of the patients with stroke followed in primary care. Rev Calid Asist. 2010;25(6):341–7. 10.1016/j.cali.2010.06.004 [DOI] [PubMed] [Google Scholar]
- 42.Mostaza JM, Puras E, Blasco M, Lahoz C, Samaniego ML. Utilización de tratamientos cardiovasculares preventivos y consecución de objetivos terapéuticos en pacientes con enfermedad arterial periférica. Rev Esp Cardiol. 2012;65:713–8. 10.1016/j.recesp.2012.02.020 [DOI] [PubMed] [Google Scholar]
- 43.Félix-Redondo FJ, Fernández-Berges D, Grau M, Baena-Diez JM, Mostaza JM, Vila J. Prevalence and clinical characteristics of peripheral arterial disease in the study population Hermex. Rev Esp Cardiol (Engl Ed). 2012;65(8):726–33. 10.1016/j.recesp.2012.03.008 [DOI] [PubMed] [Google Scholar]
- 44.Dalli E, Colomer E, Tormos MC, Cosin-Sales J, Milara J, Esteban E, et al. Crataegus laevigata decreases neutrophil elastase and has hypolipidemic effect: a randomized, double-blind, placebo-controlled trial. Phytomedicine. 2011;18(8–9):769–75. 10.1016/j.phymed.2010.11.011 [DOI] [PubMed] [Google Scholar]
- 45.Piulats-Egea N, Albaigès-Ràfols MC, Solé-Sancho J, Benito-Badorrey MB, Casas-Rodríguez J, Sendra-Pons M. Cardiopatía isquémica en población inmigrante. Hipertens Riesgo Vasc. 2014;31:40–4. 10.1016/j.hipert.2013.11.001 [DOI] [Google Scholar]
- 46.Ruescas-Escolano E, Orozco-Beltran D, Gaubert-Tortosa M, Navarro-Palazón A, Cordero-Fort A, Navarro-Pérez J, et al. El estudio PROPRESE: resultados de un nuevo modelo organizativo en atención primaria para pacientes con cardiopatía isquémica crónica basado en una intervención multifactorial. Aten Primaria. 2014;46:10–5. 10.1016/S0212-6567(14)70060-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arrospide A, Mar J, Vivancos-Mora J, Rejas-Gutierrez J, Caro J. Cost-effectiveness analysis of using high doses of atorvastatin for the secondary stroke prevention in Spain. Rev Neurol. 2010;51(1):1–11. 10.1016/j.neuroimage.2010.02.036 [DOI] [PubMed] [Google Scholar]
- 48.Brea D, Roquer J, Serena J, Segura T, Castillo J. Oxidative stress markers are associated to vascular recurrence in non-cardioembolic stroke patients non-treated with statins. BMC Neurol. 2012;12:65. 10.1186/1471-2377-12-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clua-Espuny JL, Piñol-Moreso JL, Gil-Guillén VF, Orozco-Beltrán D, Panisello-Tafalla A, Lucas-Noll J, et al. Resultados de prevención cardiovascular primaria y secundaria en pacientes con ictus: riesgo de recurrencia y supervivencia asociada (estudio Ebrictus). Rev Neurol. 2012;54:81–92. [PubMed] [Google Scholar]
- 50.Jiménez-Caballero PE, López-Espuela F, Portilla-Cuenca JC, Jiménez-Gracia MA, Casado-Naranjo I. Detección de factores de riesgo vascular y fibrilación auricular no conocida en pacientes ingresados en la unidad de ictus. Rev Neurol. 2013;56:464–70. [PubMed] [Google Scholar]
- 51.López-Farre AJ, Zamorano-León JJ, Segura A, Mateos-Caceres PJ, Modrego J, Rodriguez-Sierra P, et al. Plasma desmoplakin I biomarker of vascular recurrence after ischemic stroke. J Neurochem. 2012;121(2):314–25. 10.1111/j.1471-4159.2012.07683.x [DOI] [PubMed] [Google Scholar]
- 52.Martinez-Sanchez P, Fuentes B, Fernandez-Dominguez J, Ortega-Casarrubios ML, Aguilar-Amar MJ, Abenza-Abildua MJ, et al. Young women have poorer outcomes than men after stroke. Cerebrovasc Dis. 2011;31(5):455–63. 10.1159/000323851 [DOI] [PubMed] [Google Scholar]
- 53.Merida-Rodrigo L, Poveda-Gomez F, Camafort-Babkowski M, Rivas-Ruiz F, Martin-Escalante MD, Quiros-Lopez R, et al. Long-term survival of ischemic stroke. Rev Clin Esp. 2012;212(5):223–8. 10.1016/j.rce.2011.12.019 [DOI] [PubMed] [Google Scholar]
- 54.Pardo-Cabello AJ, Bermudo-Conde S, Manzano-Gamero V, Gómez-Jiménez FJ, Torres-Puchol JdlH. Implementación de las guías de práctica clínica sobre ictus isquémico agudo en atención especializada. Implementation of clinical practice guidelines for acute ischaemic stroke in specialist. Neurologia. 2013;28(3):137–44. 10.1016/j.nrl.2012.04.008 [DOI] [PubMed] [Google Scholar]
- 55.Purroy F, Montserrat J, Begue R, Gil MI, Quilez A, Sanahuja J, et al. Higher carotid intima media thickness predicts extracranial vascular events and not stroke recurrence among transient ischemic attack patients. Int J Stroke. 2012;7(2):125–32. 10.1111/j.1747-4949.2011.00764.x [DOI] [PubMed] [Google Scholar]
- 56.Rodriguez-Sanz A, Fuentes B, Martinez-Sanchez P, Prefasi D, Martinez-Martinez M, Correas E, et al. High-density lipoprotein: a novel marker for risk of in-hospital infection in acute ischemic stroke patients? Cerebrovasc Dis. 2013;35(3):291–7. 10.1159/000347077 [DOI] [PubMed] [Google Scholar]
- 57.Roquer J, Rodriguez-Campello A, Cuadrado-Godia E, Giralt-Steinhauer E, Jimenez-Conde J, Degano IR, et al. Ischemic stroke in prediabetic patients. J Neurol. 2014;261:1866–70. 10.1007/s00415-014-7431-7 [DOI] [PubMed] [Google Scholar]
- 58.Rubio Gil E, Martínez Pastor A, López-Picazo Ferrer J, Leal Hernández M, Martínez Navarro A, Abellán Alemán J. Estudio de los registros de seguimiento y control de los factores de riesgo en pacientes con ictus seguidos en atención primaria por historia clínica informatizada (OMI-AP). Estudio ictus-OMI. Aten Primaria. 2011;43:209–10. 10.1016/j.aprim.2010.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ruiz-Ares G, Fuentes B, Martinez-Sanchez P, Martinez-Martinez M, Diez-Tejedor E. Utility of the assessment of echogenicity in the identification of symptomatic carotid artery atheroma plaques in ischemic stroke patients. Cerebrovasc Dis. 2011;32(6):535–41. 10.1159/000330654 [DOI] [PubMed] [Google Scholar]
- 60.Serrano-Villar S, Fresco G, Ruiz-Artacho P, Bravo A, Valencia C, Fuentes-Ferrer M, et al. Stroke in the very old: myths and realities. Med Clin (Barc). 2013;140(2):53–8. 10.1016/j.medcli.2012.05.036 [DOI] [PubMed] [Google Scholar]
- 61.Polo-Romero F, Santisteban-López Y, Ramírez-Relinque L, Rodríguez-Martín B. Estrategias para mejorar el control lipídico: aumentar dosis de estatinas o asociar ezetimiba? Rev Clin Esp. 2010;210:425–6. 10.1016/j.rce.2010.01.015 [DOI] [PubMed] [Google Scholar]
- 62.Estirado E, Lahoz C, Laguna F, Garcia-Iglesias F, Gonzalez-Alegre MT, Mostaza JM. Metabolic syndrome in patients with peripheral arterial disease. Rev Clin Esp. 2014;214:437–44. 10.1016/j.rce.2014.05.005 [DOI] [PubMed] [Google Scholar]
- 63.Ferreras-Amez JM, Sanjuán-Domingo R, Visiedo-Sánchez S, Sarrat-Torres MA, Vicente-Molinero A, Abadía-Gallego V, et al. Análisis del control de factores de riesgo cardiovascular en pacientes con enfermedad arterial periférica. Semergen. 2013;39:63–9. 10.1016/j.semerg.2012.06.010 [DOI] [PubMed] [Google Scholar]
- 64.Félix-Redondo FJ, Fernández-Bergés D, Palomo-Cobos L, Buitrago-Ramírez F, Pérez-Castán JF, Lozano-Mera L. Prevalencia de consumo de alcohol y factores de riesgo cardiovascular en un área sanitaria de Extremadura. Estudio Hermex. Aten Primaria. 2012;44:201–8. 10.1016/j.aprim.2011.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martínez-Hervás J, Priego A, Lorente R, Molina M, Navarro-Hidalgo MI, Real JT, et al. Arteriosclerosis carotídea subclínica en pacientes con hiperlipidemia familiar combinada. Evolución tras dos años de tratamiento con dosis altas de atorvastatina. Med Clin (Barc). 2012;138:1–6. 10.1016/j.medcli.2010.12.009 [DOI] [PubMed] [Google Scholar]
- 66.Mazon-Ramos P, Cordero A, Gonzalez-Juanatey JR, Bertomeu MV, Delgado E, Vitale G, et al. Control of cardiovascular risk factors in revascularized patients with diabetes: a subanalysis of the ICP-Bypass Study. Rev Esp Cardiol (Engl Ed). 2015;68:115–20. 10.1016/j.recesp.2014.03.021 [DOI] [PubMed] [Google Scholar]
- 67.Pérez A, González-Blanco C, Hernández-Presa MÁ, Chaves J. Estrategia de tratamiento de la dislipemia y consecución de objetivos en la población española con diabetes tipo 2 sin enfermedad cardiovascular. Endocrinol Nutr. 2011;58:283–90. 10.1016/j.endonu.2011.03.005 [DOI] [PubMed] [Google Scholar]
- 68.Roca-Rodríguez MM, Carral-San Laureano F, Baena-Nieto G, Aguilar-Diosdado M. Evaluación del grado de consecución de objetivos de control metabólico en pacientes con diabetes mellitus tipo 2. Endocrinol Nutr. 2010;57:434–439. [DOI] [PubMed]
- 69.López-Simarro F, Brotons C, Moral I, Cols-Sagarra C, Selva A, Aguado-Jodar A, et al. Inercia y cumplimiento terapéutico en pacientes con diabetes mellitus tipo 2 en atención primaria. Med Clin (Barc). 2012;138:377–84. 10.1016/j.medcli.2011.07.023 [DOI] [PubMed] [Google Scholar]
- 70.Pérez De Isla L, Saltijeral Cerezo A, Vitale G, González-Timón B, Torres Do Rego A, Álvarez-Sala Walther LA. Cifras de colesterol adecuadas en pacientes coronarios y diabéticos. Análisis según especialidades médicas y comunidades autónomas. Rev Esp Cardiol. 2013;66:748–9. 10.1016/j.recesp.2013.04.012 [DOI] [PubMed] [Google Scholar]
- 71.Millan J, Alegría E, Guijarro C, Lozano JV, Vitale GC, González-Timón B, et al. Dislipemia en población diabética tratada con estatinas. Resultados del estudio DYSIS en España. Med Clin (Barc). 2013;141:430–6. 10.1016/j.medcli.2012.09.030 [DOI] [PubMed] [Google Scholar]
- 72.Pedro-Botet J, Mostaza JM, Pinto X, Banegas JR. Consecución del objetivo terapéutico del colesterol de las lipoproteínas de baja densidad en las unidades de lípidos y riesgo vascular de la Sociedad Española de Arteriosclerosis. Clin Investig Arterioscler. 2013;25:155–63. 10.1016/j.arteri.2013.07.006 [DOI] [PubMed] [Google Scholar]
- 73.González-Juanatey JR, Millán J, Alegría E, Guijarro C, Lozano JV, Vitale GC. Prevalencia y características de la dislipemia en pacientes en prevención primaria y secundaria tratados con estatinas en España. Estudio DYSIS-España. Rev Esp Cardiol. 2011;64:286–94. 10.1016/j.recesp.2010.10.030 [DOI] [PubMed] [Google Scholar]
- 74.Martinez-Hervas S, Carmena R, Ascaso J, Real J, Masana L, Catala M, et al. Prevalence of plasma lipid abnormalities and its association with glucose metabolism in Spain: the di@bet.es study. Clin Investig Arterioscler. 2014;26(3):107–14. 10.1016/j.arteri.2013.12.001 [DOI] [PubMed] [Google Scholar]
- 75.De la Peña A, Roca-Cusachs À, Suarez C, Bonet S. Riesgo vascular en las consultas de Medicina Interna. Estudio MICARE. Med Clin (Barc). 2013;140:246–54. 10.1016/j.medcli.2012.05.043 [DOI] [PubMed] [Google Scholar]
- 76.Divisón-Garrote JA, Massó-Orozco J, Carrión-Valero L, López-Abril J, Carbayo-Herencia JA, Artigao-Rodenas LM, et al. Evolución de la prevalencia de factores de riesgo y del riesgo cardiovascular global en población mayor de 18 años de la provincia de Albacete (1992–94 a 2004–06). Rev Esp Salud Publica. 2011;85:277–86. 10.1590/S1135-57272011000300006 [DOI] [PubMed] [Google Scholar]
- 77.Brotons C, Moral I, Soriano N, Cuixart L, Osorio D, Bottaro D, et al. Impacto de la utilización de las diferentes tablas SCORE en el cálculo del riesgo cardiovascular. Rev Esp Cardiol. 2014;67:94–100. 10.1016/j.recesp.2013.06.021 [DOI] [PubMed] [Google Scholar]
- 78.Félix-Redondo FJ, Fernández-Bergés D, Fernando-Pérez J, Zaro MJ, García A, Lozano L, et al. Prevalencia, detección, tratamiento y grado de control de los factores de riesgo cardiovascular en la población de Extremadura (España). Estudio HERMEX. Aten Primaria. 2011;43:426–34. 10.1016/j.aprim.2010.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zamora A, de Fernandez BF, Carrion C, Vazquez G, Paluzie G, Elosua R, et al. Pilot study to validate a computer-based clinical decision support system for dyslipidemia treatment (HTE-DLP). Atherosclerosis. 2013;231(2):401–4. 10.1016/j.atherosclerosis.2013.09.029 [DOI] [PubMed] [Google Scholar]
- 80.Suades R, Padro T, Alonso R, Mata P, Badimon L. Lipid-lowering therapy with statins reduces microparticle shedding from endothelium, platelets and inflammatory cells. Thromb Haemost. 2013;110(2):366–77. 10.1160/TH13-03-0238 [DOI] [PubMed] [Google Scholar]
- 81.Antón-García F, Correcher-Salvador E, Rodríguez-Lagos FA, González-Caminero S. Evaluación durante 6 años de la dislipidemia en un centro de salud. Importancia de las acciones de mejora. Semergen. 2014;40:241–6. 10.1016/j.semerg.2013.09.013 [DOI] [PubMed] [Google Scholar]
- 82.Díaz-Díaz J, Suárez-Tembra M, Díaz-Peromingo J, Pena-Seijo M, Martínez-Ramonde T, Pose-Reino A. Eficacia y seguridad de ezetimiba en unidades de riesgo vascular. Rev Clin Esp. 2011;211:283–90. 10.1016/j.rce.2011.01.010 [DOI] [PubMed] [Google Scholar]
- 83.Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey SG, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;1:CD004816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Huerta JM, Tormo MJ, Gavrila D, Navarro C. Cardiovascular risk estimated after 13 years of follow-up in a low-incidence Mediterranean region with high-prevalence of cardiovascular risk factors. BMC Public Health. 2010;10:640. 10.1186/1471-2458-10-640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Marin A, Medrano MJ, Gonzalez J, Pintado H, Compaired V, Barcena M, et al. Risk of ischaemic heart disease and acute myocardial infarction in a Spanish population: observational prospective study in a primary-care setting. BMC Public Health. 2006;6:38. 10.1186/1471-2458-6-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ministerio de Sanidad Servicios Sociales e Igualdad, Agencia Española de Medicamentos y Productos Sanitarios. Utilización de medicamentos hipolipemiantes en España durante el periodo 2000–2012. Madrid: MSSSI; 2014. Informe de utilización de medicamentos: U/HLP/V1/17012014.
- 87.Mindell J, Aresu M, Zaninotto P, Falaschetti E, Poulter N. Improving lipid profiles and increasing use of lipid-lowering therapy in England: results from a national cross-sectional survey—2006. Clin Endocrinol (Oxf). 2011;75(5):621–7. 10.1111/j.1365-2265.2011.04094.x [DOI] [PubMed] [Google Scholar]
- 88.Omboni S, Carabelli G, Ghirardi E, Carugo S. Awareness, treatment, and control of major cardiovascular risk factors in a small-scale Italian community: results of a screening campaign. Vasc Health Risk Manag. 2013;9:177–85. 10.2147/VHRM.S40925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Verhave JC, Troyanov S, Mongeau F, Fradette L, Bouchard J, Awadalla P, et al. Prevalence, awareness, and management of CKD and cardiovascular risk factors in publicly funded health care. Clin J Am Soc Nephrol. 2014;9(4):713–9. 10.2215/CJN.06550613 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


