Myeloproliferative neoplasms (MPNs) are myeloid malignancies characterized by stem cell-derived clonal myeloproliferation. There are seven designated conditions under the category of MPNs including chronic myelogenous leukemia (CML) and polycythemia vera (PV).1 CML is characterized by the presence of the Philadelphia chromosome (Ph), a translocation involving chromosomes 9 and 22 that results in the formation of the BCR-ABL fusion gene. PV is a Ph-negative MPN characterized by erythrocytosis and the presence of an activating JAK2 mutation in >95% of cases. PV and CML are considered to be mutually exclusive; however, rare cases of concurrent Ph-positive CML and a JAK2 V617F-positive PV have been described in the literature.2, 3, 4, 5, 6, 7, 8, 9 Previous reports have suggested that the two disorders may arise independently,2, 3, 4 or from within the same clone,5, 6, 7, 8, 9 but definitive clonal analysis has never been documented. We report a case of a patient with JAK2 V617F-positive PV who subsequently developed chronic phase Ph-positive CML. The patient was successfully treated with the combination of dasatinib and ruxolitinib. Cytogenetic and molecular responses suggested that the two disorders arose independently, which was corroborated by genotyping analyses of single-cell-derived colonies.
A 55-year-old woman was first diagnosed with PV in 2001 when she presented with a hemoglobin (Hgb) of 20.0 g/dl. Over the ensuing 10 years, the patient was treated with aspirin and intermittent hydroxyurea and anagrelide, with poor compliance. In May 2011 (10 years after initial PV diagnosis), she presented with worsening fatigue, weight loss and splenomegaly. Laboratory studies revealed an elevated white blood cell count (WBC) of 45 × 109/l and a Hgb of 9.5 g/dl. Examination of the peripheral smear demonstrated leukoerythroblastic changes with few circulating blasts. A bone marrow biopsy showed hypercellularity with granulocytic and megakaryocytic hyperplasia, no excess blasts, and moderate fibrosis on reticulin staining. A diagnosis of post-PV myelofibrosis was initially suspected; however, cytogenetics showed t(9;22) in 20 out of 20 metaphase cells and fluorescence in situ hybridization for BCR-ABL was positive (92.5%). Quantitative PCR for JAK2 V617F revealed an allele burden of 6%. Therefore, it appeared that the patient had developed CML with relative clonal dominance over PV.
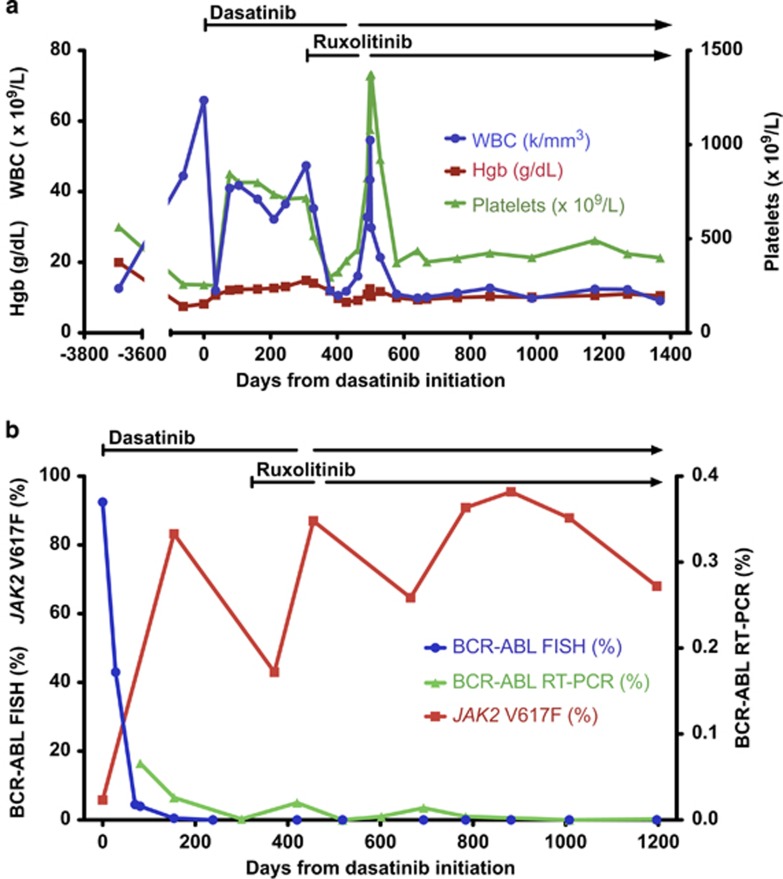
Treatment with dasatinib 100 mg daily was initiated in July 2011, resulting in dramatic improvement in the patient's leukocytosis and anemia within 1 month (Figure 1a). Shortly thereafter, however, her WBC and platelet count began to rise. Three months after starting dasatinib, the patient's complete blood count (CBC) showed a WBC of 42 × 109/l, Hgb 12.3 g/dl and platelet count of 799 × 109/l. BCR-ABL by fluorescence in situ hybridization had decreased to 4.0% however, the JAK2 V617F allele burden had increased to 83% (Figure 1b). Therefore, recrudescence of leukocytosis and thrombocytosis in this patient appeared to be due to re-emergence of the JAK2-mutant clone in the setting of suppression of the BCR-ABL-positive CML clone by dasatinib.
Figure 1.
Hematologic, cytogenetic and molecular data. (a) CBC parameters over time are shown in relationship to treatment with dasatinib and ruxolitinib. (b) Cytogenetic and molecular analyses of BCR-ABL and JAK2 V617F over time are shown in relationship to treatment with dasatinib and ruxolitinib.
The patient was treated with hydroxyurea without significant improvement in leukocytosis or thrombocytosis, and there was also no response when hydroxyurea was changed to anagrelide. A repeat bone marrow biopsy performed in May 2012 (300 days after initiation of dasatinib) revealed a hypercellular marrow, no increased blasts and severe fibrosis on reticulin staining. Cytogenetic analysis demonstrated a complete cytogenetic response with BCR-ABL by qRT-PCR detected at 0.001% (normalized to β-2 microglobulin). Despite minimal residual clonal burden from CML, the patient continued to report fatigue and poor appetite, progressive weight loss of 15 pounds and persistent splenomegaly.
Owing to the progressive increase in counts, ongoing constitutional symptoms and poor tolerance of hydroxyurea, treatment with ruxolitinib 10 mg twice daily was commenced (in addition to continuation of dasatinib) in June 2012. Within 6 weeks, there was significant improvement in the patient's blood counts (WBC 11.9 × 109/l, Hgb 11.9 g/dl, platelets 297 × 109/l), as well as improvement in constitutional symptoms and splenomegaly. The patient tolerated treatment with the combination of ruxolitinib and dasatinib well, but was noted to have worsening anemia in September 2012, approximately 4 months after starting treatment with both therapies. She was advised to hold ruxolitinib but accidentally held dasatinib for 1 month. Subsequently, dasatinib was resumed and ruxolitinib was held in October 2012 for a month, following which the patient's Hgb improved, and she was restarted on ruxolitinib at a decreased dose of 5 mg twice daily. Two months later, the dose of ruxolitinib was increased to 10 mg alternating with 5 mg twice daily.
Three years after starting treatment with dasatinib and ruxolitinib, the patient's symptoms and CBC remain stable and she has continued on combination therapy with dasatinib and ruxolitinib. The patient has maintained a complete cytogenetic response with low level BCR-ABL detectable by qRT-PCR, while the JAK2 V617F allele burden has fluctuated between 43 and 96%.
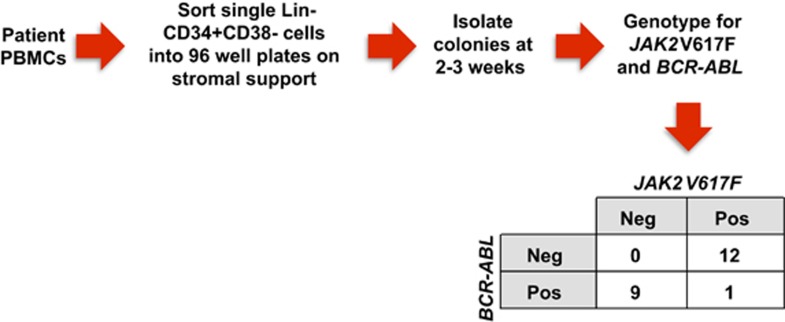
Serial quantitative measurements of BCR-ABL and JAK2 V617F following treatment with dasatinib demonstrated a marked decrease in BCR-ABL levels with a concomitant increase in the JAK2 V617F allele burden, suggesting that the two disorders arose from independent clones. To further address this issue, single cell-derived progenitor colonies were isolated and genotyped for BCR-ABL and JAK2 V617F (Figure 2). The majority of the colonies demonstrated only the presence of JAK2 V617F or BCR-ABL, but not both, confirming that the two disorders arose within distinct clones.
Figure 2.
Genotyping of individual progenitor colonies. Informed consent was obtained from the patient, and samples were collected under a protocol approved by the Washington University Human Studies Committee (#01-1014). Colonies were isolated from the peripheral blood at time of CML diagnosis and were genotyped for BCR-ABL and JAK2 V617F. The number of colonies with each genotype is shown.
Several other case reports observed a similar increase in the JAK2 V617F allele burden following successful treatment with an ABL tyrosine kinase inhibitor (TKI),5, 6, 7, 8 including a recently published report of two patients with PV/CML who were treated with the combination of imatinib and ruxolitinib.9 Similar to our case, treatment with imatinib did not lead to improvement in constitutional symptoms or splenomegaly in either patient, although they both achieved complete cytogenetic and major molecular responses of their CML. The addition of ruxolitinib to imatinib in both cases produced an improvement in constitutional symptoms and splenomegaly; however, both patients required dose reductions of ruxolitinib and imatinib owing to hematologic toxicity.
To our knowledge, this is the first case report of a patient with concurrent PV and CML treated with a JAK inhibitor and a second generation ABL TKI that definitively demonstrates that the two neoplasms arose from separate clones. None of the prior case reports included correlative clonal analysis of patients treated with this combination of therapy. Genotyping of individual progenitor colonies suggests that the two disorders arose from independent clones, which is consistent with the findings from serial quantitative measurements of BCR-ABL and JAK2 V617F during treatment; however, it is still possible that these two clones originated from a shared ancestral clone.
The combination of ruxolitinib and dasatinib was safe and effective in the treatment of concomitant PV and CML in this patient. The optimal schedule of treatment (for example, simultaneous, sequential or syncopated TKI regimens) for treatment of patients with concomitant PV/CML is still unclear, but can potentially be guided by molecular monitoring and biologic correlative analyses. Ultimately, the best treatment approach will be determined by the kinetic dynamics of each clone and the tolerability of combining TKIs.
Acknowledgments
This work was supported by NIH grants K08HL106576 (Oh), K12HL087107 (Oh) and T32HL007088 (Engle, Fisher). Technical support was provided by the Alvin J. Siteman Cancer Center Tissue Procurement and Flow Cytometry Cores, which are supported by NCI Cancer Center Support Grant P30CA91842. We thank D. Moore for assistance with tissue banking, and L. He, G. Rippberger and M. Fulbright for assistance with JAK2 and BCR-ABL genotyping experiments.
The authors declare no conflict of interest.
References
- 1Tefferi A, Vardiman JW. Classification and diagnosis of myeloproliferative neoplasms: the 2008 World Health Organization criteria and point-of-care diagnostic algorithms. Leukemia 2008; 22: 14–22. [DOI] [PubMed] [Google Scholar]
- 2Wang X, Tripodi J, Kremyanskaya M, Blouin A, Roda P, Hoffman R et al. BCR-ABL1 is a secondary event after JAK2V617F in patients with polycythemia vera who develop chronic myeloid leukemia. Blood 2013; 121: 1238–1239. [DOI] [PubMed] [Google Scholar]
- 3Bocchia M, Vannucchi AM, Gozzetti A, Guglielmelli P, Poli G, Crupi R et al. Insights into JAK2-V617F mutation in CML. Lancet Oncol 2007; 8: 864–866. [DOI] [PubMed] [Google Scholar]
- 4Campiotti L, Appio L, Solbiati F, Ageno W, Venco A. JAK2-V617F mutation and Philadelphia positive chronic myeloid leukemia. Leuk Res 2009; 33: e212–e213. [DOI] [PubMed] [Google Scholar]
- 5Hussein K, Bock O, Theophile K, Seegers A, Arps H, Basten O et al. Chronic myeloproliferative diseases with concurrent BCR-ABL junction and JAK2V617F mutation. Leukemia 2008; 22: 1059–1062. [DOI] [PubMed] [Google Scholar]
- 6Cambier N, Renneville A, Cazaentre T, Soenen V, Cossement C, Giraudier S et al. JAK2V617F-positive polycythemia vera and Philadelphia chromosome-positive chronic myeloid leukemia: one patient with two distinct myeloproliferative disorders. Leukemia 2008; 22: 1454–1455. [DOI] [PubMed] [Google Scholar]
- 7Bee PC, Gan GG, Nadarajan VS, Latiff NA, Menaka N. A man with concomitant polycythaemia vera and chronic myeloid leukemia: the dynamics of the two disorders. Int J Hematol 2010; 91: 136–139. [DOI] [PubMed] [Google Scholar]
- 8Pingali SR, Mathiason MA, Lovrich SD, Go RS. Emergence of chronic myelogenous leukemia from a background of myeloproliferative disorder: JAK2V617F as a potential risk factor for BCR-ABL translocation. Clin Lymphoma Myeloma 2009; 9: E25–E29. [DOI] [PubMed] [Google Scholar]
- 9Iurlo A, Gianelli U, Rapezzi D, Cattaneo D, Fermo E, Binda F et al. Imatinib and ruxolitinib association: first experience in two patients. Haematologica 2014; 99: e76–e77. [DOI] [PMC free article] [PubMed] [Google Scholar]