Abstract
This article examines the current knowledge of the effects of both exogenous and endogenous glucocorticoids on bone and muscle. It demonstrates the similarity of effects of supraphysiologic loads of glucocorticoids regardless of whether they enter the body in the form of medication or are manufactured by the body in response to stimuli such as inflammation. The effects of endogenous glucocorticoids and the systemic inflammatory response resulting from pediatric burn injury are compared and the difficulty in sorting out which of the two factors is responsible for the ultimate effects on bone and muscle is pointed out. The focus then switches to the body’s response to the influence of both glucocorticoids and inflammatory cytokines and evidence supporting a common pathway of response to oxidative damage caused by both is discussed. Current recommended medical management of glucocorticoid-induced bone and muscle loss is discussed and the failure to reconcile current management with known mechanisms is highlighted.
Keywords: glucocorticoids, bone, muscle, oxidative stress, forkhead box O
Introduction
Much has been learned since 1932 when Harvey Cushing described the set of symptoms that denoted hypersecretion of ACTH most often due to a pituitary adenoma. A set of symptoms prominently featured include truncal obesity, a rounded face, increased fat around the neck, and peripheral muscle wasting, weakened bones, leading to vertebral compression fractures, striae on the abdomen and buttocks, hirsutism, fatigue, muscle weakness, fatigue, fluid retention, hypertension, and hyperglycemia (1)
The original publication by Cushing (2), as it turns out, was the first description of the effects of endogenous glucocorticoids on bone and muscle, a description that became identified with the effects of exogenous glucocorticoids, or steroid medication for a variety of chronic inflammatory and neoplastic diseases. Thus for the longest time the deleterious effects of glucocorticoids on bone and muscle were identified exclusively with steroid-based medications
This review will touch on the clinical side-effects of glucocorticoid medications and then will proceed to the more complex subject of the effects of endogenous glucocorticoids on bone and muscle and the interactions of glucocorticoids with the systemic inflammatory response. Following this the discussion will move on to focus on the identification of a common mechanism of glucocorticoid effect on both bone and muscle and will conclude by examining unanswered questions regarding the interactions of bone and muscle under the influence of glucocorticoids. A discussion of current management of these glucocorticoid side effects will provide a perspective as to how far we have yet to go in order to match mechanism with clinical management. It is hoped that this review will shed light on both the depth and the complexity of glucocorticoid effects on bone and muscle.
The Epidemiology and Clinical Effects of Steroid Medications on Bone and Muscle
The clinical side-effects of steroid medications on bone and muscle have been the subject of numerous reviews and textbook descriptions. Glucocorticoid-based medications have potent anti-inflammatory effects and are widely used to treat chronic inflammatory conditions such as inflammatory bowel disease, systemic lupus, rheumatoid arthritis, neuromuscular diseases such as Duchenne muscular dystrophy, reactive airway diseases such as asthma, and immunosuppression in organ transplantation, among other situations. As concisely stated in a review by Ziegler and Kasperk (3), glucocorticoids can cause both muscle wasting and decreased bone formation. There is a question as to whether they truly cause calcium malabsorption with resultant secondary hyperparathyroidism and resorptive bone loss, but this has recently been reported in mice with the mechanism attributed to glucocorticoid-associated decreased expression of intestinal calcium channel TRPV6 (4). It is unclear, however, as to the significance of this mechanism in humans. Nonetheless, the effects of exogenous glucocorticoids on bone formation and peripheral muscle wasting are well described. The likelihood of muscle wasting and steroid-induced osteoporosis increases if the duration of treatment exceeds 3 months or consists of 3–4 courses of treatment per year with an oral dose of at least 5 mg prednisone per day(5). To minimize the chances of systemic steroid side effects the dose of oral steroids should be less than 7.5 mg daily, should last less than 3 months, and should be given less than 3–4 times per year (6).
Glucocorticoid-induced osteoporosis is a condition that causes fractures in 30–50% of adults on long-term treatment and approximately 1.5% of post-menopausal women in the United Kingdom receive long-term treatment with glucocorticoids (7). In 2000 approximately 1% of the population of the United Kingdom was treated with steroids at any one time with 22% of the total treated for more than six months (7). From data obtained in Iceland approximately 26% of the population treated with long-term glucocorticoids developed osteoporosis (7). While fracture rates increase with age, long-term steroid intake of prednisolone 5mg/day or greater increases the fracture rate by an additional 20%, a figure that increases to an additional 60% if the amount of prednisolone taken reaches 20 mg/day (7).
The Effects of Endogenous Glucocorticoids on Bone and Muscle
While steroid side effects can be produced by supraphysiologic doses of steroid medications, it is well-known from Cushing’s initial description that endogenous glucocorticoids are capable of producing identical effects, whether it be from a pituitary tumor, as first described (2), or from another condition. It is important for the physician to be aware of which conditions have been documented to produce excessive endogenous glucocorticoids. Representative conditions can be found in Table 1.
Table 1.
Pathologic Conditions Stimulating Endogenous Glucocorticoid Production
The mechanism of action by which angiotensin II infusion stimulates endogenous glucocorticoid production is not identified to date but urinary production of glucocorticoids is elevated in mice and rats (11)
A good illustration of the pathophysiologic elevation of endogenous glucocorticoids is the scenario that occurs following a severe burn injury. Burns can be considered to be an appropriate case study to examine mechanisms of glucocorticoid effects on bone and muscle because in clinical situations, with the exception of glucocorticoid-producing tumors, elevation of glucocorticoids does not occur in isolation. Although it can be argued that burn injury causes tissue damage and necrosis, which may result in activation of pathways other than what is observed with exogenous glucocorticoid injury, the injury itself results in at least two major adaptive responses that occur immediately following a burn injury. The first is the systemic inflammatory response, during which a variety of pro-inflammatory cytokines are released, notably interleukin (IL)-1β and IL-6, the former being three-fold elevated and the latter one hundred-fold elevated (9). At approximately the same time, urinary free cortisol excretion is 3–8-fold elevated (9). It is not certain whether the trauma of the burn injury activates both responses independently of each other or whether the release of proinflammatory cytokines precedes the rise in endogenous glucocorticoid production (6). The timing of this sequence has not yet been studied. Nonetheless both responses are vigorous and both occur acutely following burns and to argue that necrosis may trigger different mechanisms is speculative.
The initial effect on bone, as illustrated in a sheep model of burn injury (12), is an acute increase in urinary excretion of the C-telopeptide of type I collagen, or CTx, a biomarker of bone resorption, on day one post-burn. By day 5 post-burn there is histologic evidence of increased bone resorption, as shown by the presence of scalloping on scanning electron microscopy (12). The significance of this finding is that in those first five days at least, despite the elevation of urinary free cortisol excretion, there is no significant steroid-mediated apoptosis of osteoblasts or osteocytes. The reason for the persistence of resorption despite the presence of large quantities of glucocorticoids that can cause osteoblast and osteocyte apoptosis is not understood.
The dictum that glucocorticoids can stimulate bone cells to transiently increase production of the ligand of the receptor activator of NFκB (RANK ligand ) is not uniformly agreed upon. Work by Weinstein et al (13) indicates that glucocorticoid exposure prolongs the life of mature resorptive osteoclasts, therefore, possibly prolonging resorptive activity. However, extensive work by by Kim et al (14) demonstrate in vitro and in vivo in mice that knockout of the glucocorticoid receptor in the osteoclast lineage cells protects the animal from bone resorption while wild type mice exposed to glucocorticoids actually experience an inhibition of bone resorption as a result of cytoskeletal disorganization within the osteoclast.
Also of interest is that by 2 weeks post-burn, at least in children, a hypodynamic-adynamic bone turnover is observed (9).This hypodynamic state occurs in spite of the persistence of very high blood levels of pro-inflammatory cytokines (9). At this point in time, two weeks post-burn, not only have osteoblasts disappeared from the bone surface of the iliac crest but osteoblast differentiation is also impaired (15). At this time point resorption is also low as noted by lower-than-normal urinary concentration of deoxypyridinoline (Dpd), a biomarker of type I collagen breakdown fragments (9). Thus, in the setting of acute burn injury bone resorption takes place immediately but it takes approximately two weeks for the injury to affect bone cell production. It would therefore appear as if inflammation-mediated bone resorption occurs early post-burn and it takes approximately two weeks for the effects of glucocorticoid excess to manifest themselves.
Why events occur in this particular order is not clear. If the pro-inflammatory cytokine response stimulates acute bone resorption and yet those cytokine levels persist at 2 weeks post-burn, why does the resorption slow down or stop? There are at least two possibilities that could explain this scenario. The first is that the osteoclast proliferation resulting from the high production of inflammatory cytokines may result in the release of osteoclastic clastokines, substances such as sphingosine-1-phosphate that can stimulate osteoblastogenesis. It is possible that by 2 weeks post-burn clastokine production slows down or stops. The second possibility is the gradual loss of osteocytes. As they become fewer in number the amount of ligand of the receptor activator of nuclear transcription factor NFκB (RANKL) they produce is insufficient to sustain bone resorption at the level at which it was initially driven by the stimulus from pro-inflammatory cytokines.
Immobilization, which occurs very early on following the burn injury, appears to be mediate an increase in sympathetic tone. Osteoblasts contain beta adrenergic receptors and it is possible that early immobilization may contribute to the increase in bone resorption that is observed as long as the osteoblasts remain viable. Mechanisms of muscle wasting related to immobilization are not entirely clear.
Another reported effect of glucocorticoids is to decrease intestinal calcium absorption, which results in secondary hyperparathyroidism (3). At the very least this is not always the case. In our sheep model of burns, there is a 50% up-regulation of the parathyroid calcium-sensing receptor at 48h post-burn (16). In pediatrics this results in hypocalcemic hypoparathyroidism with hypercalciuria (17). In this case burn patients receive large quantities of calcium intravenously to try to compensate for the hypocalcemia (17); thus malabsorption of calcium is not an issue.
With regard to muscle, catabolism begins early. Within the first few days of burn injury muscle protein breakdown exceeds muscle protein synthesis as demonstrated by stable isotope infusion studies of labeled phenylalanine (18). It is not known exactly how early the muscle breakdown begins because of the critical state of the patient until he or she is stabilized. However, muscle breakdown and resorptive bone loss are occurring simultaneously. The inflammatory response itself is capable of causing muscle breakdown so it is not certain precisely which process, inflammation or endogenous glucocorticoid production, is the primary cause of initial muscle breakdown. However, it is clear that as bone becomes hypodynamic to adynamic, muscle breakdown continues (19). Thus, precisely when glucocorticoids begin to effect muscle breakdown is not clear at present.
Large numbers of studies have been carried out on the catabolic effect of burn injury on muscle. Most of these have been done using stable isotope measurements of muscle protein synthesis, breakdown, and net balance. These techniques are described below in order to give the reader a basis for evaluating the published studies on which this review is based.
The technique for carrying out the stable isotope infusion studies involves a lengthy protocol (18–20) consisting of a timed intravenous infusion of labeled phenylalanine followed by an infusion of unlabeled amino acids. Phenylalanine is neither synthesized nor oxidized in muscle and its rate of disappearance from arterial blood is an index of muscle protein synthesis and the rate of appearance in venous blood is an index of muscle protein breakdown. The unlabeled amino acids given during the last three hours of the infusion provide additional substrate for the synthesis of muscle protein. The subject has catheters placed in an artery and a vein. Baseline blood samples and muscle biopsies are obtained, and leg blood flow is measured using an indocyanine green dilution technique (20). From timed sample collections and leg blood flow determinations the fractional synthesis rate, breakdown rate, and net balance of phenylalanine can be calculated.
At this point there are no good biomarkers that can help to distinguish effects caused by inflammation and those caused by glucocorticoids. This difficulty actually suggests that the effects of inflammation and glucocorticoids may evoke a common response from the body and that similarly the effects of glucocorticoids on both muscle and bone may result in a common response. This will be examined in the next section.
Is There A Common Mechanism By Which Glucocorticoids Affect Both Bone and Muscle?
In this section the question of what glucocorticoids do to both bone and muscle will be altered to address the subject of the body’s response to glucocorticoid exposure as manifested in both bone and muscle.
Addressing the response of bone to glucocorticoids, it has recently been reported that glucocorticoids induce oxidative stress in bone (21,22) and in tendon (23) and that the body’s response to the oxidative stress (21–24) is what may produce the effects on bone that are attributed to steroid toxicity. It is not immediately apparent as to why or how glucocorticoids in excess stimulate production of reactive oxygen species by the body. However, the association of glucocorticoids with reactive oxygen species has been reported in several tissues including the nervous system and studies carried out in neural tissue can perhaps shed some additional light on what is taking place in both bone and muscle.
Thus Du and colleagues (25) showed that the incubation of cortical neurons with corticosterone increased mitochondrial oxidation in a dose and time-dependent manner. Most cellular electrons that leak from the electron transport chain react with oxygen in the mitochondria, producing a superoxide. These superoxides are then converted to hydrogen peroxide in the mitochondria by the action of superoxide dismutase. You et al (26), in studying rat hippocampal slice cultures, showed that incubation with dexamethasone increased the hippocampal oxidative state by 200% in a dose-dependent fashion; this condition was inhibited by pre-treatment with the steroid receptor antagonist RU 486 or the reactive oxygen species scavenger N-acetyl L cysteine. Furthermore, in vivo studies by Sato et al (27) in the rat demonstrated that 2 weeks of exogenous administration of corticosterone increased hippocampal oxidative markers such as lipid peroxidation while the anti-oxidant enzymes, such as superoxide dismutase, catalase, and glutathione peroxidase activities decreased. Concomitantly, this study also documented reduced glucocorticoid receptor expression, a feature of elevated hippocampal glucocorticoid levels (27). Similar findings have been reported in rats by Zafir and Banu (28).
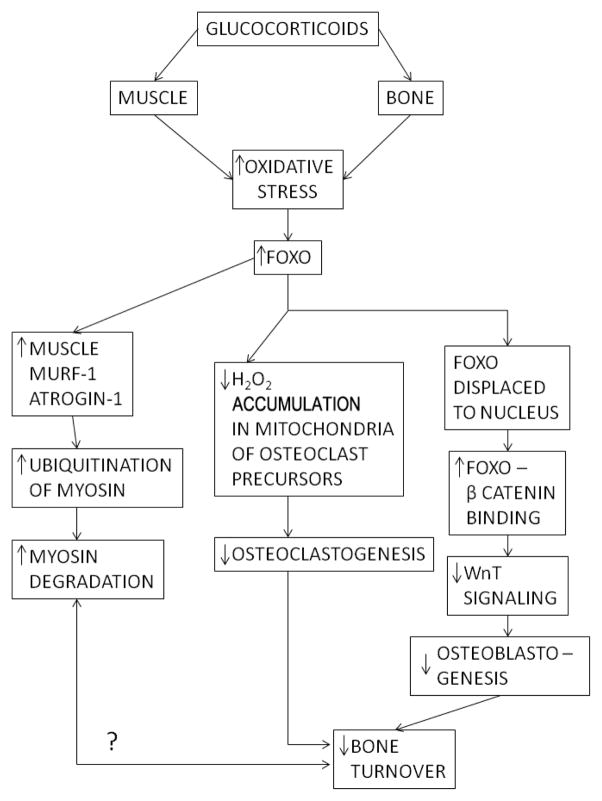
In bone, studies in mice have shown that oxidative stress activates the nuclear transcription factors in the forkhead box O family, more commonly known as FOXO (22). FOXO transcription factors are capable of entering the cell nucleus under conditions of oxidative stress, binding to β-catenin, and diverting it from binding with T cell factors that allow development of osterix positive marrow stem cells into osteoblasts (22). In this way FOXO transcription factors can suppress the Wnt-β catenin signaling pathway in the development of osteoblasts. In osteoclasts, reactive oxygen species generate osteoclastogenesis (24). FOXO proteins can attenuate hydrogen peroxide accumulation in the mitochondria of osteoclast precursor cells, thereby inhibiting their differentiation into osteoclasts (24). The consequence of this function is reduced osteoclast numbers and reduced bone resorption. Therefore, FOXO transcription factors can reproduce the hypodynamic-adynamic bone seen in conditions of glucocorticoid excess.
With regard to muscle, FOXOs, in particular FOXO1 and FOXO3, have also been implicated in muscle wasting. Two muscle-specific ubiquitin ligases, muscle ring finger protein-1 (MuRF-1) and atrogin-1 muscle atrophy F box, ubiquitinate various sarcomeric proteins, such as myosin heavy chain, which are then targeted for degradation. Thus, Castillero et al (29) reported that peroxisome proliferator-activator (PPAR) β/δ up-regulates muscle FOXO1 expression with downstream up-regulation of ubiquitin ligases atrogin 1 and MuRF 1, which initiate muscle wasting and that the muscle wasting can be blocked by inhibition of PPAR β/δ. Moreover, a functional glucocorticoid response element has been identified in the mouse FOXO1 promoter (30), and the administration of an anti-oxidant, resveratrol, prevents dexamethasone stimulation of muscle atrophy-related ubiquitin ligases, the downstream signals from FOXO transcription factors, in vitro (31). The timing of the muscle atrophy induced by steroids is relatively rapid. In the case of the rat it can occur within 24h (32). Moreover, it is possible that sepsis-induced FOX01 is also mediated by glucocorticoids (33).
Thus, glucocorticoids likely cause oxidative damage to both bone and muscle and it is the body’s adaptive response to this damage, i.e., stimulation of FOXO transcription factors to protect the tissues from further oxidative damage, that itself appears to produce both the hypodynamic-adynamic bone as described in the paragraph above as well as the peripheral muscle wasting. Moreover, inflammatory cytokines (21) and sepsis (33) have also been shown to work through stimulating FOXO1 production. Might this be a final common pathway that is shared by glucocorticoids, inflammatory cytokines, and perhaps other deleterious factors?
While the above mechanism has been worked out in animals, the extent to which it is functional in humans has not yet been determined. Moreover, the situation in muscle is more complex than that which has been so far been described for bone. Thus, for example, fast-twitch muscles contain a greater glucocorticoid receptor density than slow-twitch muscles (34). This finding suggests that slow-twitch fibers may be spared in glucocorticoid toxicity. Furthermore, in addition to regulating protein breakdown through the ubiquitin ligases, both MuRF-1 and atrogin-1 may also contribute to a decrease in protein synthesis in response to glucocorticoid administration (35).
To complicate matters further, glucocorticoids may stimulate inflammatory pathways as a means of contributing to muscle atrophy. Thus glucocorticoids can stimulate the protein TRAF6, which couples inflammatory signals from membrane-bound cytokine receptors to transcription factors such as NFκB, which help induce the inflammatory response (36). This report thus provides evidence that both the inflammatory and stress responses may work in the same pathway.
Also, myostatin, the protein produced in skeletal muscle that downregulates myogenic differentiation, is upregulated by glucocorticoids. Glucocorticoid response elements are present in in the human myostatin promoter (37). Further, glucocorticoids serve as insulin antagonists and prevent the insulin-activated pathway that stimulates phosphatidyl inositol kinase, resulting in the up-regulation of FOXO transcription factors (38).Micro RNAs may also contribute to the glucocorticoid-induced muscle atrophy as several of them are up-regulated during the process of glucocorticoid therapy (39).Finally, synthetic glucocorticoids appear to be potent inhibitors of the muscle satellite, or stem cell, population (40). Thus, while muscle and bone may have some atrophy-resorption pathways in common the situation remains extremely complex.
Muscle-Bone-Neural Interactions
If we accept the evidence above that glucocorticoids induce a common response in both bone and muscle, that is, up-regulation of the body’s anti-oxidant system via FOXO signaling, how would muscle and bone influence each other’s actions when oxidative damage is causing muscle atrophy and hypodynamic bone? Reduction in skeletal loading as would occur with muscle atrophy would presumably result in further decreased bone formation and potentially increased resorption, and similarly, if bone communicates with muscle (19) what might occur if muscle wasting were to be stimulated by FOXO? This issue is not addressed but serves to illustrate the complexity of the interactions of muscle and bone under circumstances of stress. Moreover, when increased oxidation of neural tissue is added to these organ interactions the complexity of these interactions becomes greater still.
Management
Given the recent developments in understanding of the effects of glucocorticoids on muscle and bone, there are no specific therapies developed to date that address these mechanisms. Clearly the targeted use of anti-oxidants needs to be studied, as well as the properties of drugs currently used to treat bone loss, in order to determine whether any of these treatments have anti-oxidant properties. Further updates will be awaited in this area. However, given that no mechanism-based therapy has been developed to manage glucocorticoid-induced bone and muscle loss, recommendations still exist for the management of this condition, at least in adults. The United States Food and Drug Administration endorses the use of some bisphosphonates such as alendronate, risedronate and zolendronate to treat glucocorticoid-induced osteoporosis. The rationale for the use of bisphosphonates is to utilize the anti-resorptive properties of bisphosphonates to prevent resorptive bone loss in conditions associated with long-term steroid treatment, although whether the glucocorticoids themselves exacerbate resorptive bone loss or whether the resorption is due to inflammatory cytokines has long been a subject of much debate. Currently there is no answer to this question. Are anti-resorptives effective? A recent study by Overman et al (41) demonstrated that in a group of nearly 8000 post-menopausal women taking long-term glucocorticoid medication initiation of osteoporosis treatment within the first 90 days of steroid use, either with an anti-resorptive or with parathyroid hormone, resulted in a 48% reduction in fracture incidence during the first year of steroid use and a 32% reduction in fracture incidence over the first three years of glucocorticoid therapy. This would definitely indicate a certain measure of efficacy but with use of parathyroid hormone does not speak specifically to a single mechanism of action in reducing fracture risk. The recent 2010 guidelines proposed by the American College of Rheumatology (42) recommend that patients at low to moderate fracture risk according to computer-based FRAX (http://www.sheffield.ac.uk/FRAX) calculations of <10% as low and 10–20% as moderate probability of a major fracture should be treated if they are receiving chronic steroid therapy of at least 7.5 mg per day. In contrast, those at high risk for major fracture with a FRAX calculation > 20%, or a bone mineral density T score of −2.5 or below should be treated if they receive any dose of glucocorticoid for greater than one month’s time or if they receive greater than 5mg/day of prednisolone equivalent for less than one month The American College of Rheumatology also recommends treatment of pre-menopausal women of non-childbearing potential who receive steroid therapy for at 1–3 months.
This method of management contrasts with that of pediatric patients exposed to chronic glucocorticoid therapy for in the management of chronic rheumatoid arthritis. According to a recent survey taken of 86 practicing pediatric rheumatologists in North America, Soybilgic et al (43) reported that 79% of the practitioners did not obtain a baseline bone density examination prior to initiation of glucocorticoid therapy, only 42% followed bone density annually, and 35–50% of practitioners prescribe bisphosphonates sometimes, frequently, or always. Therefore, there is great variability in the evaluation of pediatric patients receiving long-term glucocorticoid therapy, as well as in their management, although approximately 80% of the practitioners polled stated they prescribe calcium and vitamin D supplements, despite the lack of evidence supporting the use of these supplements in the prevention of osteoporosis or osteoporotic fractures.
Recommendations are far more tentative with regard to prevention of the muscle wasting occurring with glucocorticoid treatment. There are no guidelines issued by any professional society regarding recommended measures for treatment or prevention of steroid-induced muscle loss. The most current recommendations mix resistance training exercise with a high protein diet in helping to control muscle wasting (44,45).
Summary and Conclusions
Glucocorticoids have been demonstrated to produce oxidative stress in multiple tissue, including bone, nervous tissue, and possibly muscle. The common response to this form of stress, the up-regulation of “anti-oxidant” transcription factors in the forkhead box O family, may be at least partially responsible for the conditions of hypodynamic/adynamic bone and muscle atrophy. The fact that inflammatory reactions can also access the FOXO anti-oxidant pathways complicate the ability to pinpoint which body responses stem from inflammation and which from stress exposure. Other unanswered questions include how, if at all, the FOXO up-regulation is responsible for the biphasic response of bone to inflammation and stress with initial high bone turnover followed by hypodynamic bone. In addition, the relationship between muscle and bone is unclear under conditions of oxidative stress that affect both tissues. At present, no management regimen addresses the pathophysiologic mechanisms elucidated here, although the United States Food and Drug Administration has recommendations in place at least for adults with regard to management and prevention of glucocorticoid-induced bone loss. In fact, while the search is being made for a common mechanism of bone and muscle loss as a result of glucocorticoid exposure, bone and muscle loss are considered two distinct clinical entities both in the literature and by the Food and Drug Administration.
Figure 1.
Depicted is a schematic diagram of the proposed final common pathway of oxidative damage to both bone and muscle. Abbreviations include MuRF-1 = muscle ring-finger protein-1 and atrogin-1= atrogin-1 muscle atrophy F box. The final bidirectional arrow between muscle and bone with the question mark illustrates the point that there is no known interaction between muscle and bone with oxidative stress but neither is an interaction ruled out.
Acknowledgments
Some of the data cited from the author’s own work was supported by a grant from the National Institutes of Health P50 GM 60338 (4) and by multiple grants from Shriners Hospitals for Children.
Footnotes
The author discloses that he had served on the Bone Toxicity Advisory Board of Novartis Pharmaceuticals in August 2012.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Bibliography
- 1.National Endocrine and Metabolic Diseases Information Service. Cushing’s disease. National Institute of Diabetes, Digestive and Kidney Diseases, National Institutes of Health, Department of Health and Human Services; 2008. pp. 1–10. NIH Publication 08-300. [Google Scholar]
- 2.Cushing H. The basophil adenomas of the pituitary body and their clinical manifestations (pituitary basophilism) Bull Johns Hopkins Hosp. 1932;50:137–195. [Google Scholar]
- 3.Ziegler R, Kasperk C. Glucocorticoid-induced osteoporosis: prevention and treatment. Steroids. 1998;63:344–348. doi: 10.1016/s0039-128x(98)00022-1. [DOI] [PubMed] [Google Scholar]
- 4.Huybers S, Naber TH, Bindels RJ, Hoenderop JG. Prednisolone-induced Ca2+ malabsorption is caused by diminished expression of the epithelial Ca2+ channelTRPV6. Am J Physiol Gastrointest Liver Physiol. 2007;292:G92. doi: 10.1152/ajpgi.00317.2006. [DOI] [PubMed] [Google Scholar]
- 5.Zikan V, Tyblova M, Raska I, Jr, Havrdova E, Luchavova M, Michalska D, Kubena AA. Bone mineral density and body composition in men with multiple sclerosis chronically treated with low dose steroids. Physiol. 2012;61:405–417. doi: 10.33549/physiolres.932299. [DOI] [PubMed] [Google Scholar]
- 6.Von Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C. Use of oral corticosteroids and risk of fractures. J Bone Miner Res. 2000;15:993–1000. doi: 10.1359/jbmr.2000.15.6.993. [DOI] [PubMed] [Google Scholar]
- 7.Rizzoli R, Adachi JD, Cooper C, Dere W, Devogelaer JP, Diez Perez A, Kanis JA, Laslop A, Mitlak B, Papapoulos S, Ralston S, Reiter S, Werhya G, Reginster JY. Management of glucocorticoid-induced osteoporosis. Calcif Tissue Int. 2012;91:225–243. doi: 10.1007/s00223-012-9630-5. [DOI] [PubMed] [Google Scholar]
- 8.Ruzek MC, Pearce BD, Miller AH, Biron CA. Endogenous glucocorticoids protect against cytokine-mediated lethality during viral infection. J Immunol. 1999;162:3527–3533. [PubMed] [Google Scholar]
- 9.Klein GL, Herndon DN, Goodman WG, Langman CB, Phillips WA, Dickson IR, Eastell R, Naylor KE, Maloney NA, Desai M, Benjamin D, Alfrey AC. Histomorphometric and biochemical characterization of bone following acute severe burns in children. Bone. 1995;17:455–460. doi: 10.1016/8756-3282(95)00279-1. [DOI] [PubMed] [Google Scholar]
- 10.Hu Z, Huiling W, Lee IH, Du J, Mitch WE. Endogenous glucocorticoids and impaired insulin signaling are both required to stimulate muscle wasting under pathophysiologic conditions in mice. J Clin Invest. 2009;119:3059–3069. doi: 10.1172/JCI38770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song Y-H, Li Y, Du J, Mitch WE, Rosenthal N, Delafontaine P. Muscle-specific expression of IGF-1 blocks angiotensin II-induced skeletal muscle wasting. J Clin Invest. 2005;115:451–458. doi: 10.1172/JCI22324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klein GL, Xie Y, Qin YX, Lin L, Hu M, Enkhbaatar P, Bonewald LF. Preliminary evidence of early bone resorption in a sheep model of acute burn injury: an observational study. J Bone Miner Metab. 2014;32:136–141. doi: 10.1007/s00774-013-0483-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC. Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. J Clin Invest. 1998;102:274–282. doi: 10.1172/JCI2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim HJ, Zhao H, Kitaura H, Bhattacharyya S, Brewer JA, Muglia LJ, Ross FP, Teitelbaum SL. Glucocorticoids and the osteoclast. Ann NY Acad Sci. 2007;1116:335–339. doi: 10.1196/annals.1402.057. [DOI] [PubMed] [Google Scholar]
- 15.Klein GL, Bi LX, Sherrard DJ, Beavan SR, Ireland D, Compston JE, Williams WG, Herndon DN. Evidence supporting a role of glucocorticoids in short-term bone loss in burned children. Osteoporos Int. 2004;15:468–474. doi: 10.1007/s00198-003-1572-3. [DOI] [PubMed] [Google Scholar]
- 16.Murphey ED, Chattopadhyay N, Bai M, Kifor O, Harper D, Traber DL, Hawkins HK, Brown EM, Klein GL. Up-regulation of the parathyroid calcium-sensing receptor after burn injury in sheep: a potential contributory factor to post-burn hypocalcemia. Crit Care Med. 2000;28:3885–3890. doi: 10.1097/00003246-200012000-00024. [DOI] [PubMed] [Google Scholar]
- 17.Klein GL, Nicolai M, Langman CB, Cuneo BF, Sailer DE, Herndon DN. Dysregulation of calcium homeostasis after severe burn injury in children: possible role of magnesium depletion. J Pediatr. 1997;131:246–251. doi: 10.1016/s0022-3476(97)70161-6. [DOI] [PubMed] [Google Scholar]
- 18.Hart DW, Wolf SE, Mlcak R, Chinkes DL, Ramzi PI, Obeng MK, Ferrando AA, Wolfe RR, Herndon DN. Persistence of muscle catabolism after severe burn. Surgery. 2000;128:312–319. doi: 10.1067/msy.2000.108059. [DOI] [PubMed] [Google Scholar]
- 19.Borsheim E, Herndon DN, Hawkins HK, Suman OE, Cotter M, Klein GL. Pamidronate attenuates muscle loss following pediatric burn injury. J Bone Miner Res. 2014;29:1369–1372. doi: 10.1002/jbmr.2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolfe RR, Chinkes DL. Isotope tracers in metabolic research. New York: John Wiley and Sons; 2004. pp. 51–76. [Google Scholar]
- 21.Almeida M, Han L, Ambrogini E, Weinstein RS, Manolagas SC. Glucocorticoids and tumor necrosis factor α increase oxidative stress and suppress Wnt protein signaling in osteoblasts. J Biol Chem. 2011;286:44326–44335. doi: 10.1074/jbc.M111.283481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iyer S, Ambrogini E, Bartell SM, Han L, Roberson PK, deCabo R, Jilka RL, Weinstein RS, O’Brien CA, Manolagas SC, Almeida M. FOXOs attenuate bone formation by preventing Wnt signaling. J Clin Invest. 2013;123:3409–3419. doi: 10.1172/JCI68049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poulsen RC, Carr AJ, Hulley PA. Protection against glucocorticoid damage in human tenocytes by modulation of ERK, Akt, and forkhead signaling. Endocrinol. 2011;152:503–14. doi: 10.1210/en.2010-1087. [DOI] [PubMed] [Google Scholar]
- 24.Bartell SM, Kim HN, Ambrogini E, Han L, Iyer S, Serra Ucer S, Rabinovitch P, Jilka RL, Weinstein RS, Zhao H, O’Brien CA, Manolagas SC, Almeida M. FOXO proteins restrain osteoclastogenesis and bone resorption by attenuating H2O2 accumulation. Nat Commun. 2014;5:3773. doi: 10.1038/ncomms4773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Du J, Wang Y, Hunter R, Wei Y, Blumenthal R, Falke C, Khairova R, Zhou R, Yuan P, Machado-Vieira R, McEwen BS, Manji HK. Dynamic regulation of mitochonidrial function by glucocorticoids. Proc Natl Acad Sci USA. 106:3543–3548. doi: 10.1073/pnas.0812671106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.You JM, Yun SJ, Nam KN, Kang C, Won R, Lee EH. Mechanism of oxidative stress in rat hippocampal slice cultures. Can J Physiol Pharmacol. 2009;87:440–447. doi: 10.1139/y09-027. [DOI] [PubMed] [Google Scholar]
- 27.Sato H, Takahashi T, Sumitani K, Takatsu H, Urano S. Glucocorticoid generates ROS to induce oxidative injury in the hippocampus, leading to impairment of cognitive function in rats. J Clin Biochem Nutr. 2010;47:224–232. doi: 10.3164/jcbn.10-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zafir A, Banu N. Modulation of in vivo oxidative status by exogenous corticosterone and restraint stress in rats. Stress. 2009;12:167–177. doi: 10.1080/10253890802234168. [DOI] [PubMed] [Google Scholar]
- 29.Castillero E, Alamdari N, Aversa Z, Gurav A, Hasselgren PO. PPAR β/δ regulates glucocorticoid and sepsis-induced FOXO1 activation and muscle wasting. PLoS One. 2013;8:e59726. doi: 10.1371/journal.pone.0059726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qin W, Pan J, Qin Y, Lee DN, Bauman WA, Cardozo C. Identification of glucocorticoid response element in the mouse FOXO1 promoter. Biochem Biophys Res Comm. 2014;450:979–983. doi: 10.1016/j.bbrc.2014.06.080. [DOI] [PubMed] [Google Scholar]
- 31.Alamdari N, Aversa Z, Castillero E, Gurav A, Petkova V, Tizio S, Hasselgren PO. Reservatrol prevents dexamethasone-induced expression of muscle atrophy-related ubiquitin ligases atrogin-1 and MuRF-1 in cultured myotubes through a SIRT 1-dependent mechanism. Biochem Biophys Res Commun. 2012;417:528–533. doi: 10.1016/j.bbrc.2011.11.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu Y, Hou J, Collier L, Pan J, Hou L, Qin W, Bauman WA, Cardozo CP. The administration of high-dose methylprednisolone for 24h induced muscle size and increased atrophy-related gene expression in spinal cord-injured rats. Spinal Cord. 2011;49:867–873. doi: 10.1038/sc.2011.28. [DOI] [PubMed] [Google Scholar]
- 33.Smith IJ, Alamdari N, O’Neal P, Gonnella P, Aversa Z, Hasselgren PO. Sepsis increases the expression and activity of forkhead box O in skeletal muscle by a glucocorticoid-dependent mechanism. Int J Biochem Cell Biol. 2010;42:701–711. doi: 10.1016/j.biocel.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shimizu N, Yoshikawa N, Ito N, Maruyama T, Suzuki Y, Takeda S, Nakae J, Taqata Y, Nishitani S, Takahana A, Sano M, Fukuda K, Suematsu M, Morimoto C, Tanaka H. Crosstalk between glucocorticoid receptor and nutritional sensor in mTor skeletal muscle. Cell Metab. 2011;13:170–182. doi: 10.1016/j.cmet.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 35.Csibi A, Leibovitch MP, Kornille K, Tintignac LA, Leibovitch SA. MAF/bx/Atrogin-1 controls the activity of the initiation factor ElF-3F in skeletal muscle atrophy by targeting multiple C-terminal lysines. J Biol Chem. 2009;284:4413–4421. doi: 10.1074/jbc.M807641200. [DOI] [PubMed] [Google Scholar]
- 36.Braun TP, Grossberg AJ, Krasnow SM, Levasseur PR, Szulmowski M, Zhu XX, Maxson JE, Knoll JG, Barnes AP, Marks DL. Cancer- and endotoxin-induced cachexia require intact glucocorticoid signaling in skeletal muscle. FASEB J. 2013;27:3572–3582. doi: 10.1096/fj.13-230375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ma K, Mallidis C, Artaza J, Taylor W, Gonzalez-Cadavid N, Bhasin S. Characterization of the 5′ region of the human myostatin gene: regulation by dexamethasone in vivo. Am J Physiol Endocrinol Metab. 2001;281:E1128–E1136. doi: 10.1152/ajpendo.2001.281.6.E1128. [DOI] [PubMed] [Google Scholar]
- 38.Sandri M, Sandri C, Gilbert A, Skurk C, Calabria E, Picard A, Walsh K, Schiaffino S, Lecker SH, Goldberg AL. Foxo transcription factors induce the atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy. Cell. 2004;117:399–412. doi: 10.1016/s0092-8674(04)00400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shen H, Lu T, Fu L, Zhao S, Fan B, Cao J, Li X. Identification of micro RNAs involved in dexamethasone-induced muscle atrophy. Mol Cell Biochem. 2013;381:105–113. doi: 10.1007/s11010-013-1692-9. [DOI] [PubMed] [Google Scholar]
- 40.Dong Y, Pan JS, Zhang L. Myostatin suppression of Akirin-1 mediates glucocorticoid-induced satellite cell dysfunction. PLoS ONE. 2013;8:e58554. doi: 10.1371/journal.pone.0058554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Overman RA, Gourlay ML, Deal CL, Farley JF, Brookhart MA, Layton JB. Fracture rate associated with quality metric-based anti-osteoporosis treatment in glucocorticoid-induced osteoporosis. Osteoporos Int. 2015 doi: 10.1007/s00198-014-3022-9. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grossman JM, Gordon R, Ranganath VK, Deal C, Caplan L, Chen W, Curtis JR, Furst DE, McMahon M, Patkar NM, Volkmann E, Saag KG. American College of Rheumatology 2010 Recommendations for the Prevention and Treatment of Glucocorticoid-induced Osteoporosis. Arthrits Care Res. 2010;62:1515–1526. doi: 10.1002/acr.20295. [DOI] [PubMed] [Google Scholar]
- 43.Soybilgic A, Tesher M, Wagner-Weiner L, Onel KB. A survey of steroid-related osteoporosis diagnosis, prevention, and treatment practices of pediatric rheumatologists in North America. Pediatr Rheumatol Online J. 2014 Jul 9;12:24. doi: 10.1186/1546-0096-12-24. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Daly RM, O’Connell SL, Mundell NL, Grimes CA, Dunstan DW, Nowson CA. Protein-enriched diet, with the use of lean red meat, combined with progressive resistance training, enhances lean tissue mass and muscle strength and reduces circulating IL-6 concentrations in elderly women: a cluster randomized controlled trial. Am J Clin Nutr. 2014;99:899–910. doi: 10.3945/ajcn.113.064154. [DOI] [PubMed] [Google Scholar]
- 45.Daly RM, Duckham RL, Gianoudis J. Evidence for an interaction between exercise and nutrition for improving bone and muscle health. Curr Osteoporos Rep. 2014;12:219–226. doi: 10.1007/s11914-014-0207-2. [DOI] [PubMed] [Google Scholar]