Abstract
Nipah virus (NiV) is a zoonotic emerging pathogen that can cause severe and often fatal respiratory disease in humans. The pathogenesis of NiV infection of the human respiratory tract remains unknown. Reactive oxygen species (ROS) produced by airway epithelial cells in response to viral infections contribute to lung injury by inducing inflammation and oxidative stress; however, the role of ROS in NiV-induced respiratory disease is unknown. To investigate whether NiV induces oxidative stress in human respiratory epithelial cells, we used oxidative stress markers and monitored antioxidant gene expression. We also used ROS scavengers to assess their role in immune response modulation. Oxidative stress was confirmed in infected cells and correlated with the reduction in antioxidant enzyme gene expression. Infected cells treated by ROS scavengers resulted in a significant decrease of the (F2)-8-isoprostane marker, inflammatory responses and virus replication. In conclusion, ROS are induced during NiV infection in human respiratory epithelium and contribute to the inflammatory response. Understanding how oxidative stress contributes to NiV pathogenesis is crucial for therapeutic development.
Introduction
Nipah virus (NiV) is an emerging zoonotic pathogen that belongs to the genus Henipavirus, family Paramyxoviridae (Eaton et al., 2005). NiV causes severe and often fatal respiratory disease and/or encephalitis in humans. NiV was first identified during an outbreak of severe encephalitis in Malaysia and Singapore in 1998–1999 (Chua et al., 2000; Goh et al., 2000), which involved more than 276 individuals, with a case fatality rate of 38 % (Chong et al., 2002). Although the fruit bat (Pteropus spp.) is the natural vector (Enserink, 2000), pigs were identified as the intermediate amplifying host during this particular outbreak (Ali et al., 2001; Premalatha et al., 2000). Since then, outbreaks of NiV infection have occurred regularly in south-east Asia (Harit et al., 2006; Hossain et al., 2008; Rockx et al., 2012), with the most recent cases identified in Bangladesh in February 2015 (Anonymous, 2015). The case fatality rate varies from 43 to 100 % in sporadic cases in Bangladesh/India (Anonymous, 2014; Marsh & Wang, 2012; Rockx et al., 2012), and transmission in these outbreaks is associated with consumption of raw date palm sap believed to be contaminated with NiV excreted by bats (Rahman et al., 2012). In addition, human-to-human transmission has been reported during more recent outbreaks (Gurley et al., 2007; Harit et al., 2006). Respiratory symptoms were reported more frequently during the outbreaks in Bangladesh/India (70 % of cases) compared with the outbreak in Malaysia ( < 30 %) (Lo & Rota, 2008) and included cough, difficulty breathing (Lo & Rota, 2008), severe pneumonia (Goh et al., 2000; Paton et al., 1999) and an acute respiratory distress-like syndrome (Hossain et al., 2008), suggesting differences in pathogenesis between the two genetically distinct Nipah virus strains (Harcourt et al., 2005). Data on histopathological lesions in the respiratory tract caused by the NiV-Bangladesh (NiV-B) strain are not available, whilst those caused by the NiV Malaysia strain are localized mainly in the small airways and include necrotizing alveolitis with haemorrhage, pulmonary oedema and aspiration pneumonia (Wong et al., 2002). However, the pathogenesis of NiV-induced airway disease in humans is still unknown, and no treatment is available to ameliorate this clinical outcome.
We reported previously that primary human respiratory epithelial cells from the small airways (SAECs) are highly permissive to NiV-B infection, resulting in a strong inflammatory and innate immune response (Escaffre et al., 2013). Further analysis of our data indicated that the nuclear factor (erythroid-derived 2)-like 2 (Nrf2)-mediated oxidative stress response pathway is one of the canonical pathways that was most significantly affected during infection of SAECs (Escaffre et al., 2013). Upon exposure of cells to oxidative stress, Nrf2 translocates to the nucleus and binds to the antioxidant response elements within the promoter of detoxifying/metabolizing enzymes and antioxidant enzymes, and activates their transcription. These enzymes are numerous and include glutathione S-transferase, NAD(P)H quinone oxidoreductase, haem oxygenase and superoxide dismutase (SOD) (Allen & Tresini, 2000; Gabbita et al., 2000).
Oxidative stress has multiple origins and is the result of an accumulative effect in cells of reactive oxygen species (ROS), which are highly unstable molecules generated as byproducts of the metabolism of oxygen. The production of ROS comes from either mitochondrial function or external stressors that, when not managed by the endogenous antioxidant defences, can lead to the oxidation of cellular components like lipids, proteins and DNA (Allen & Tresini, 2000; Gabbita et al., 2000). ROS are significant cell regulators, and oxidative stress contributes to the pathogenesis of acute and chronic lung inflammatory diseases such as asthma, acute respiratory distress and chronic obstructive pulmonary disease (MacNee, 2001; Morcillo et al., 1999). Interestingly, influenza and respiratory syncytial virus (RSV; another member of the family Paramyxovirus) have also been shown to induce ROS in multiple cell types (Akaike et al., 1996; Hosakote et al., 2009; Yamada et al., 2012). Specifically, ROS produced in RSV-infected primary human respiratory epithelial cells can modulate the immune response (Garofalo et al., 2013; Hosakote et al., 2009, 2012), and ROS in RSV-infected mice are associated with lung inflammation and overall clinical outcome (Castro et al., 2006; Hosakote et al., 2011).
We hypothesized that the deregulation of antioxidant enzyme (AOE) expression in NiV-infected respiratory epithelial cells leads to increased ROS production and oxidative stress, which results in the release of cytokines/chemokines and subsequent inflammatory cell recruitment. In order to gain further insight into the early steps of infection, here we investigated the role of oxidative stress in NiV-infected SAECs. Our results showed that NiV induces oxidative stress and modulation of AOE gene expression in SAECs, which correlate with ROS accumulation. In addition, ROS production in infected SAECs was reduced using specific ROS scavengers in a dose-dependent manner that also impacted on cytokine secretion.
Results
NiV-B induces oxidative stress in human respiratory epithelial cells
To investigate whether oxidative stress is induced during NiV-B infection in respiratory epithelial cells, two oxidative stress markers, (F2)-8-isoprostane concentration and the ratio of total glutathione to oxidized glutathione (GSH/GSSG), were monitored in mock- and NiV-B-infected SAECs. NiV-B infection of SAECs resulted in a significant increase of (F2)-8-isoprostane levels at 24 and 48 h post-infection (p.i.) compared with control cells (Fig. 1a). In addition, there was a significant decrease in the GSH/GSSG ratio in NiV-B-infected SAECs compared with control SAECs at 6 and 24 h p.i. (Fig. 1b). No glutathione could be assessed in infected cells at 48 h p.i. Altogether, an increase of (F2)-8-isoprostane concentration and a concomitant decrease in GSH/GSSG ratio during infection confirmed that NiV-B infection induces oxidative stress in SAECs.
Fig. 1. NiV-B induces oxidative stress in SAEC and modifies antioxidant gene expression. (a, b) (F2)-8-isoprostane quantification in SAEC culture supernatants (a) and GSH/GSSG ratio assessment in SAECs (b) were performed as described in Methods. *P < 0.05, **P < 0.01, Student's t-test. (c) qPCR analysis of SOD2, SOD3, catalase, GST-α4 and transcription factor Nrf2 gene expression in NiV-B-infected SAECs compared with non-infected SAECs. The horizontal dashed line represents the threshold at which there was no gene expression change. Anything above or below this threshold indicates upregulation or downregulation, respectively, of a particular gene in infected cells compared with control cells. All results are expressed as the mean ± sd of three biological samples. **P < 0.01, Student's t-test.
NiV-B modulates AOE gene expression in SAECs
To determine whether oxidative stress in NiV-B-infected SAECs resulted from changes in AOE expression, we quantified the expression of AOE genes throughout the infection. Selection of AOEs was based on results from a previous microarray study (Escaffre et al., 2013) showing that the Nrf2-mediated oxidative stress response ranked third among all canonical pathways affected by NiV-B infection in SAECs (Escaffre et al., 2013). Based on this result, the gene expression of the transcription factor Nrf2 and SOD1, SOD2, SOD3, catalase and glutathione S-transferase (GST)-α4 were assessed in NiV-B-infected SAECs.
The gene expression of transcription factor Nrf2 remained unchanged in NiV-B-infected SAECs at 6 and 48 p.i. but was downregulated at 24 h p.i. (Fig. 1c), in agreement with the microarray study. Whilst SOD1 (data not shown) and SOD2 gene expression levels did not follow a clear trend throughout the infection, only SOD2 was downregulated at 48 h p.i. (Fig. 1c). SOD3, GST-α4 and catalase gene expression levels were also significantly downregulated at 24 and 48 h p.i. compared with the control (Fig. 1c). These data showed that Nrf2, SOD2–3, GST-α4 and catalase gene expression are downregulated late in NiV-B-infected SAECs, which probably results in high levels of cellular free radical species such as superoxide anions and hydroxyl radicals, and no or limited hydrogen peroxide cellular detoxification, resulting in oxidative stress.
NiV-B-induced oxidative stress in SAECs is reduced by treatment with ROS scavengers
In order to determine whether oxidative stress in NiV-B-infected SAECs can be prevented, SAECs were treated with compounds known to have direct or indirect antioxidant effect. Two ROS scavengers, pyrrolidine dithiocarbamate (PDTC) and butylated hydroxyanisole (BHA), were tested as well as the ROS xanthine oxidase enzyme inhibitor febuxostat (Feb). Feb was significantly less efficient in reducing oxidative stress compared with the other two compounds (Fig. 2a). Indeed, SAEC treatment with PDTC and BHA, but not with Feb, drastically lowered the difference in (F2)-8-isoprostane levels at 48 h p.i. between uninfected and infected cells. Interestingly, none of the drug compounds tested reduced syncytium formation or delayed the cytopathic effects (data not shown). The reduction in (F2)-8-isoprostane levels in NiV-B infection by treatment with PDTC and BHA was dose dependent (Fig. 2b, c). Overall, BHA treatment resulted in a more potent reduction in oxidative stress compared with PDCT. These data showed that PDTC and BHA treatment of SAECs can prevent oxidative stress during NiV-B infection.
Fig. 2. Oxidative stress in NiV-B-infected SAECs can be lowered using ROS scavengers. (a) Levels of lipid peroxidation product (F2)-8-isoprostane quantified at the 48 h time point in supernatants of SAECs undergoing different drug treatments. The assay was performed with biological triplicates using 7.5 μM PDTC, 100 μM BHA or 2.5 μM Feb. ***P < 0.001 (Student's t-test). (b, c) Levels of lipid peroxidation product (F2)-8-isoprostane quantified at the 48 h time point in supernatants of SAECs undergoing twofold dilution treatments with PDTC (b) and BHA (c). **P < 0.01 or ***P < 0.001 corresponds to a significant difference of (F2)-8-isoprostane level between infected cells non-pre-treated or pre-treated with various PDTC (b) or BHA (c) concentrations (ANOVA and Bonferroni's multiple comparison test).
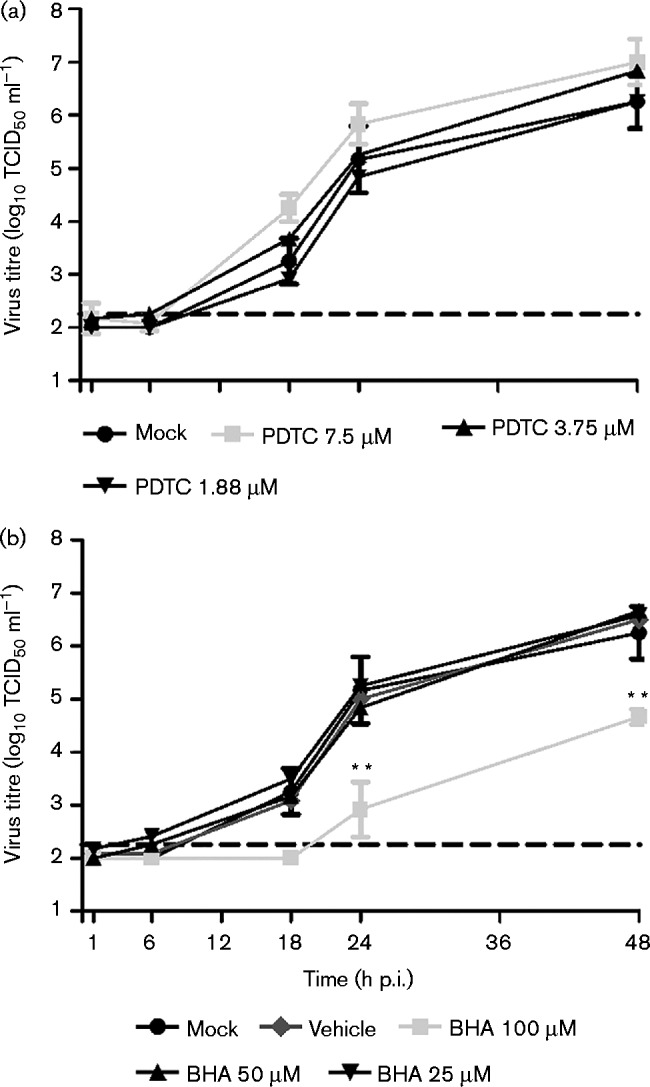
BHA reduces NiV-B replication in SAECs
As the level of oxidative stress induced during NiV-B infection of SAECs was significantly modulated by PDTC and BHA, we investigated whether these compounds also had antiviral properties (Fig. 3). Regardless of the concentration used, the treatment of SAECs with PDTC did not significantly affect the virus titre at any time point when compared with the virus titre in non-treated SAECs (Fig. 3a). Pre-treatment of SAECs with 100 μM BHA significantly reduced the virus titre by 2 log10 at 24 h p.i. and by 1 log10 at 48 h p.i. compared with the virus titres in non-pre-treated SAECs (Fig. 3b). However, this reduction in virus titre was not observed at lower concentrations of BHA. These data showed that BHA not only has an antioxidant effect but also can reduce virus replication.
Fig. 3. Effect of antioxidant pre-treatment of SAECs on NiV-B replication. Kinetics of virus replication in SAECs treated with PDTC (a) or BHA (b) starting 1 h prior to infection. Results are expressed as the mean ± sd of three biological repetitions. The horizontal dashed line corresponds to the detection limit. **P < 0.01 corresponds to a significant difference in virus replication level between non-pre-treated and pre-treated infected cells, with the highest PDTC or BHA concentration (ANOVA and Bonferroni's multiple comparison test).
PDTC and BHA affect cytokine production in NiV-B-infected SAECs
In order to determine the effect of ROS modulation on the host response, a subset of cytokines/chemokines was quantified. Selection of the cytokines was based on results from previous studies (Escaffre et al., 2013). Among a panel of 15 human cytokines/chemokines, the expression levels of four cytokines [granulocyte colony-stimulating factor (G-CSF), granulocyte–macrophage colony-stimulating factor (GM-CSF), IL-6 and CXCL10] were reduced by the two lower concentrations of PDTC in infected SAECs at 48 h p.i. (Fig. 4). Specifically, G-CSF, GM-CSF, IL-6 and CXCL10 concentrations were all significantly lower in PDTC-treated compared with non-treated infected SAECs. The concentration of IL-6 was also significantly decreased in 7.5 μM PDTC-treated compared with non-treated infected SAECs, whereas the GM-CSF level was significantly increased under the same experimental conditions. However, its level relative to uninfected controls was lower in treated versus untreated cells.
Fig. 4. Quantification of cytokines/chemokines secreted by PDTC-treated SAECs. Results shown the amount of G-CSF (a), GM-CSF (b), IL-6 (c) and CXCL10 (d) secreted by PDTC-treated SAECs at 48 h p.i. Results are expressed as the mean ± sd of three biological repetitions. *P < 0.05, **P < 0.01 and ***P < 0.001 (ANOVA and Bonferroni's multiple comparison test).
Only GM-CSF and IL-6 cytokine secretion levels were reduced by BHA treatment (Fig. 5a, b). In particular, the levels of GM-CSF and IL-6 were significantly lowered in 100 μM BHA-treated compared with non-treated infected SAECs. These data showed that PDTC and BHA are able to reduce the secretion of several inflammatory cytokines including G-CSF, GM-CSF, IL-6 and CXCL-10 in NiV-B-infected SAECs.
Fig. 5. Quantification of cytokines/chemokines secreted by BHA-treated SAECs. Results shown the amount of G-CSF (a) and IL-6 (b) secreted by BHA-treated SAECs at 48 h p.i. Results are expressed as the mean ± sd of three biological repetitions. *P < 0.01 and ***P < 0.001 (ANOVA and Bonferroni's multiple comparison test).

Discussion
NiV is a deadly emerging zoonotic virus that can cause severe and acute respiratory disease and/or encephalitis in humans. To date, studies have mostly focused on the neurological aspects of the disease, whilst infection of the human respiratory tract remains poorly investigated. We recently showed that NiV efficiently infects and replicates in human respiratory epithelial cells, resulting in a strong inflammatory response (Escaffre et al., 2013; Valbuena et al., 2014). Here, we specifically report Nrf2-mediated oxidative stress response canonical pathway deregulation and oxidative stress in NiV-B-infected SAECs, and we investigated whether an antioxidant treatment could both reduce oxidative stress and modulate the innate immune response that contributes to NiV pathogenesis in the human respiratory tract. In the current study, NiV-B was used, as it has been associated with increased respiratory disease and is the only NiV strain known to currently circulate and cause outbreaks in Bangladesh/India (Anonymous, 2014; Lo & Rota, 2008).
ROS that encompass oxidants and free radical species are generated by molecular oxygen reduction, deregulated mitochondria and cell membrane-associated specific enzymes, and by other mechanisms. The ROS level regulates the Nrf2-mediated oxidative stress response pathway. The transcription factor Nrf2, when not sequestered by its inhibitor Kelch-like ECH-associated protein 1 (KEAP1) in the cytoplasm, translocates to the nucleus and activates AOE genes by binding to their antioxidant response elements (Allen & Tresini, 2000; Gabbita et al., 2000). The antioxidants can then detoxify the cell from ROS and prevent new ROS formation.
Both (F2)-8-isoprostane levels and total versus oxidized glutathione ratios have been used previously as markers of oxidative stress (Hosakote et al., 2009). Using these markers, we also demonstrated here that oxidative stress occurs in NiV-B-infected SAECs. Similar to what was observed during RSV-induced oxidative stress in SAECs (Hosakote et al., 2009), NiV-B triggered a downregulation of the Nrf2 gene and affected AOE gene expression involved in ROS neutralization and detoxification. The increase in oxidized glutathione in NiV-B-infected SAECs starting at 6 h p.i. suggested an early increase in free radical species, similar to RSV-induced oxidative stress in SAECs (Hosakote et al., 2009). The level of gene expression of GST-α4, which participates in ROS detoxification, decreased over time in NiV-B-infected SAECs; this has also been described for another member of GST with a similar function in RSV-infected A549 cells (Hosakote et al., 2009). Finally, ROS levels at a late stage of infection in NiV-B-infected SAECs were then probably even more increased due to lower gene expression of SOD2/SOD3 and catalase, which are responsible for free radical species dismutation and oxidant catalysis, respectively. Again, these phenomena were also observed in RSV- and influenza virus-induced oxidative stress in respiratory epithelial cells (Hosakote et al., 2009; Pyo et al., 2014). Surprisingly, SOD2 gene expression was downregulated at a late stage of NiV-B infection in SAECs whilst it was strongly upregulated by RSV (Hosakote et al., 2009). SOD2 upregulation in RSV-infected SAECs was attributed to RSV-induced activation of the NF-κB transcription factor (Garofalo et al., 1996), which can bind to the SOD2 gene promoter (Kinnula & Crapo, 2003). This was also reported in influenza virus-infected A549 cells (Knobil et al., 1998) and suggests that regulation of the SOD2 gene in respiratory epithelial cells is modulated differently between NiV-B and RSV or influenza virus. Altogether, these results suggest that, similar to RSV, oxidative stress in NiV-B-infected SAECs is at least in part due to deregulation of the Nrf2-mediated oxidative stress response pathway. However, the exact mechanism by which NiV-B and RSV directly interact with this pathway remains unknown.
Antioxidants have been used previously in different models of respiratory infections to control ROS levels (Castro et al., 2006; Knobil et al., 1998; Uchide et al., 2002). The mechanisms by which PDTC and BHA modulate ROS levels are different from one another; PDTC has a similar effect to the cellular antioxidant glutathione (Uchide & Toyoda, 2011), whilst BHA prevents lipid oxidation (Aksu & Kaya, 2005; Casola et al., 2001; Kashanian & Ezzati Nazhad Dolatabadi, 2009) and indirectly induces activation of Nrf2 (Kong et al., 2001; Yuan et al., 2006). Here, our data showed that PDTC and BHA were able to control oxidative stress in NiV-B-infected SAECs in a dose-dependent manner.
In addition, PDTC blocks influenza virus proliferation by recruiting intracellular copper and zinc ions (Kim et al., 1999), which inhibit the viral polymerase activity (Oxford & Perrin, 1974). Here, PDTC did not affect NiV-B replication in SAECs but it is unknown whether NiV-B viral polymerase is sensitive to these ions or if the lack of effect on replication is due to the PDTC concentration used in this study. Conversely, BHA reduced NiV-B replication in SAECs when used at high concentration. Consistent with our data, BHA protects Vero cells from vesicular stomatitis virus-induced oxidative stress and lowered virus replication (Riva et al., 2006), but the mechanism by which BHA interferes with replication of viruses remains unknown.
PDTC and BHA treatment of NiV-B-infected SAECs significantly decreased the secretion level of cytokines such as G-CSF, GM-CSF, IL-6 and CXCL10. The mechanism of action for PDTC is unknown but, when used at a high concentration, appears to increase the baseline cytokine production possibly masking the effect. Consistent with our data, IL-6 gene expression is prevented by PDTC treatment of influenza virus-infected A549 cells (Uchide & Toyoda, 2011) and the level of IL-6 and GM-CSF is also significantly lowered by BHA treatment of RSV-infected mice, as is the migration of neutrophils into the lung (Castro et al., 2006). Interestingly, CXCL10 and IL-6 gene upregulation correlates with pulmonary inflammatory cell infiltrates in NiV-infected hamsters (Rockx et al., 2011). NiV-infected human lung grafts exhibiting syncytia formation in the epithelium also have increased secretion levels of G-CSF, GM-CSF, IL-6 and CXCL10 among other cytokines (Valbuena et al., 2014). Therefore, these data suggest that PDTC and BHA attenuate part of the inflammatory response in NiV-B-infected SAECs and that both PDTC and BHA could reduce NiV-B-induced acute lung injury.
In conclusion, our data indicate that NiV-B infection of SAECs deregulates the Nrf2-mediated oxidative stress response pathway, which lowers AOE production, contributing to increased intracellular ROS levels and oxidative stress. Antioxidants such as PDTC and BHA decreased oxidative stress and displayed an antiviral effect for the latter. This study also demonstrated that NiV-B-induced oxidative stress contributes to an inflammatory response in SAECs and suggests that oxidative stress may play an important role in NiV-B pathogenesis by causing inflammation-mediated oxidative stress injury in the human respiratory tract. Understanding how alterations in the cytoprotective defences against oxidative stress, in the context of NiV-B infection, can contribute to respiratory disease is critical to help us identify molecular targets for future therapeutic development.
Methods
Virus and cells
NiV-B was kindly provided by the Special Pathogens Branch (Centers for Disease Control and Prevention, GA, USA). NiV-B was isolated from a throat swab of a patient exhibiting a respiratory involvement during the 2004 outbreak in Rajbari district, Bangladesh. The virus was propagated in Vero cells (CCL-81; American Type Culture Collection) as described previously (Escaffre et al., 2013).
SAECs from the distal airspace were obtained with the Clonetics Normal Human Small Airway Epithelial cell system (CC-2547; Clonetics). Monolayers of non-differentiated SAECs were cultured in a 150 cm3 flask for 8 days (37 °C, 5 % CO2) with Small Airway Epithelial Cell Basal Medium supplemented with growth factors (SAGM BulletKit; Clonetics). SAECs were seeded in 12-well plates at 0.4 × 106 cells per well (each condition was performed in triplicate) the day prior to infection. Six hours prior to infection, the medium was removed and replaced with basal medium, not supplemented with growth factors, as described previously (Hosakote et al., 2009). All SAEC infections were performed at an m.o.i. of 1 for 1 h at 37 °C. Cells were then rinsed three times with 1 × PBS and appropriate medium was added (basal medium without growth factors).
Viruses were titrated on Vero cells in 96-well plates using 10-fold virus dilutions in triplicate as described previously (Escaffre et al., 2013). Virus titre was expressed as TCID50 ml− 1 using the method of Reed & Muench (1938). All infectious work was performed in a class II biological safety cabinet in a Biosafety Level 4 Laboratory at the Galveston National Laboratory, University of Texas Medical Branch.
Measurement of lipid peroxidation products
Measurement of the lipid peroxidation marker (F2)-8-isoprostane in cell culture supernatants (experiment performed with biological triplicates) was performed using a competitive enzyme immunoassay (Cayman Chemical), as described previously (Hosakote et al., 2009).
Determination of glutathione
Total or oxidized glutathione concentrations in the cell lysates (experiment performed with biological triplicates) were measured using a glutathione colorimetric assay (Cayman Chemical), as described previously (Hosakote et al., 2009). Briefly, total cell lysates were deproteinated by adding an equal volume of metaphosphoric acid reagent (0.1 g ml− 1 in HPLC-grade water). After incubation at room temperature for 5 min and centrifugation at 2000 g for 2 min, the supernatant was collected, and after addition of 4 M triethanolamine (TEAM) reagent, it was used for total glutathione (GSH) measurement. For oxidized glutathione (GSSG) measurement, 2-vinylpyridine (1 M) was added to the sample solution with TEAM reagent, incubated at room temperature for 1 h and then assayed for GSSG, according to the manufacturer's instructions.
qPCR
Total cellular RNA from SAECs was extracted (experiment performed with biological triplicates) using TRIzol reagent (Invitrogen), following the manufacturer's recommendations. Quantitative reverse transcription (RT)-PCR assays were performed using TaqMan gene expression assays (Life Technologies), which provide a 20 × mix of a single TaqMan MGB probe and two unlabelled oligonucleotide primers to specifically assess SOD1, SOD2, SOD3, catalase, GST-α4 or Nrf2 gene expression. In addition, the 18S rRNA gene (VIC dye-labelled probe) TaqMan assay reagent was used as an endogenous control (Life Technologies). Single-plex one-step RT-PCRs were performed using the Quantifast Probe RT-PCR kit (Qiagen). The cycling parameters for one-step RT-PCR were the following: reverse transcription 50 °C for 10 min, followed by 45 cycles of activation 95 °C for 5 min, denaturation 95 °C for 10 s and annealing/extension 60 °C for 30 s on a Bio-Rad CFX96. Duplicate threshold cycle (CT) values were analysed using the comparative CT (ΔΔCT) method. The amount of target gene expression level (2− ΔΔCT) was calculated by normalizing to the endogenous reference (18S rRNA gene) sample.
Compound preparation and viability test
The two ROS scavengers PDTC and BHA (Sigma-Aldrich) were resuspended in sterile PBS and absolute ethanol, respectively, and aliquoted prior to storage at − 80 °C. Feb (Cayman Chemicals), a ROS xanthine oxidase enzyme inhibitor, was resuspended in absolute ethanol, aliquoted and stored at − 80 °C. PDTC was further diluted to 7.5, 3.75 and 1.88 μM in SAEC basal medium prior to use. Similarly, BHA was diluted to 100, 50 and 25 μM. Feb was diluted to 2.5, 1.25 and 0.63 μM. The concentration at which each compound was not cytotoxic for SAECs was evaluated by first seeding 2 × 106 SAECs per 96-well plate, treating each row of cells of the plates with twofold serial dilutions of either PDTC, BHA, Feb or SAEC basal medium for 48 h (experiment performed in quadruplicate) and then using a cell growth determination MTT-based kit (Sigma-Aldrich) following the manufacturer's instructions. From these results, PDTC, BHA and Feb were used at a maximum concentration of 7.5, 100 and 2.5 μM, respectively.
Antioxidant treatment
SAEC culture and seeding in 12-well plates was performed as described above. Starting 1 h prior to infection, the basal medium was replaced by basal medium supplemented with different concentrations of either PDTC or BHA. All SAEC infections were performed as described above. Cells were then rinsed three times with 1 × PBS, and fresh basal medium supplemented with different concentrations of either PDTC or BHA was added (performed in triplicate).
Milliplex analysis
Cytokine/chemokine concentrations in the supernatant of henipavirus-infected SAECs were determined using a Milliplex Human Cytokine 15 Plex Immunoassay custom kit (Millipore). Prior to analysis, samples (experiment performed with biological triplicates) were inactivated on dry ice by gamma irradiation (5 Mrad). The assay was performed according to the manufacturer's instructions. The human cytokine standards were prepared using the SAEC basal medium. The concentrations of 15 cytokines [G-CSF, GM-CSF, IFN-α2, IFN-γ, IL-1α, IL-1β, IL-6, IL-8, IL-1RA, CXCL10, eotaxin, monocyte chemotactic protein-1, TNF-α, fractalkine (CX3CL1) and vascular endothelial growth factor A] were quantified.
Statistical analyses
Comparisons of virus replication levels and cytokine/chemokine secretion levels were subjected to a repeated measure one-way ANOVA test. When the ANOVAs revealed a significant main effect, a post-hoc test such as Bonferroni's multiple comparison test was used to determine whether treatment means were significantly different from one another. Comparison of GSH/GSSG ratios and (F2)-8-isoprostane levels was performed using a two-tailed Student's t-test. All data are presented in the figures as means ± sd (*P < 0.05, **P < 0.01, ***P < 0.001).
Acknowledgements
This work was supported by the University of Texas Medical Branch startup funds (to B. R.), National Institutes of Health (1R21AI111042-01 to B. R. and P01AI07924602 to A. C.), and a UTMB Center for Tropical Diseases Postdoctoral Fellowship (to O. E.). The authors would like to thank Drs Alexander Freiberg and Gustavo Valbuena for helpful discussions.
References
- Akaike T., Noguchi Y., Ijiri S., Setoguchi K., Suga M., Zheng Y.M., Dietzschold B., Maeda H. (1996). Pathogenesis of influenza virus-induced pneumonia: involvement of both nitric oxide and oxygen radicals Proc Natl Acad Sci U S A 93 2448–2453 10.1073/pnas.93.6.2448 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aksu M.I., Kaya M. (2005). The effect of α-tocopherol and butylated hydroxyanisole on the colour properties and lipid oxidation of kavurma, a cooked meat product Meat Sci 71 277–283 10.1016/j.meatsci.2005.03.023 . [DOI] [PubMed] [Google Scholar]
- Ali R., Mounts A.W., Parashar U.D., Sahani M., Lye M.S., Isa M.M., Balathevan K., Arif M.T., Ksiazek T.G. (2001). Nipah virus among military personnel involved in pig culling during an outbreak of encephalitis in Malaysia, 1998-1999 Emerg Infect Dis 7 759–761 10.3201/eid0704.017433 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen R.G., Tresini M. (2000). Oxidative stress and gene regulation Free Radic Biol Med 28 463–499 10.1016/S0891-5849(99)00242-7 . [DOI] [PubMed] [Google Scholar]
- Anonymous (2014). ProMED-mail 2014. January 12, 2014, archive no. 20140118.2181682. Nipah encephalitis, human – Bangladesh (02) Dhaka Tribune .
- Anonymous (2015). ProMED-mail 2015. February 02, 2015, archive no. 20150204.3143251. Nipah encephalitis, human – Bangladesh Daily Star .
- Casola A., Burger N., Liu T., Jamaluddin M., Brasier A.R., Garofalo R.P. (2001). Oxidant tone regulates RANTES gene expression in airway epithelial cells infected with respiratory syncytial virus. Role in viral-induced interferon regulatory factor activation J Biol Chem 276 19715–19722 10.1074/jbc.M101526200 . [DOI] [PubMed] [Google Scholar]
- Castro S.M., Guerrero-Plata A., Suarez-Real G., Adegboyega P.A., Colasurdo G.N., Khan A.M., Garofalo R.P., Casola A. (2006). Antioxidant treatment ameliorates respiratory syncytial virus-induced disease and lung inflammation Am J Respir Crit Care Med 174 1361–1369 10.1164/rccm.200603-319OC . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong H.T., Kunjapan S.R., Thayaparan T., Tong J.M.G., Petharunam V., Jusoh M.R., Tan C.T. (2002). Nipah encephalitis outbreak in Malaysia, clinical features in patients from Seremban Can J Neurol Sci 29 83–87 10.1017/S0317167100001785 . [DOI] [PubMed] [Google Scholar]
- Chua K.B., Bellini W.J., Rota P.A., Harcourt B.H., Tamin A., Lam S.K., Ksiazek T.G., Rollin P.E., Zaki S.R., other authors (2000). Nipah virus: a recently emergent deadly paramyxovirus Science 288 1432–1435 10.1126/science.288.5470.1432 . [DOI] [PubMed] [Google Scholar]
- Eaton B.T., Broder C.C., Wang L.F. (2005). Hendra and Nipah viruses: pathogenesis and therapeutics Curr Mol Med 5 805–816 10.2174/156652405774962308 . [DOI] [PubMed] [Google Scholar]
- Enserink M. (2000). Emerging diseases. Malaysian researchers trace Nipah virus outbreak to bats Science 289 518–519 10.1126/science.289.5479.518 . [DOI] [PubMed] [Google Scholar]
- Escaffre O., Borisevich V., Carmical J.R., Prusak D., Prescott J., Feldmann H., Rockx B. (2013). Henipavirus pathogenesis in human respiratory epithelial cells J Virol 87 3284–3294 10.1128/JVI.02576-12 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbita S.P., Robinson K.A., Stewart C.A., Floyd R.A., Hensley K. (2000). Redox regulatory mechanisms of cellular signal transduction Arch Biochem Biophys 376 1–13 10.1006/abbi.1999.1685 . [DOI] [PubMed] [Google Scholar]
- Garofalo R., Sabry M., Jamaluddin M., Yu R.K., Casola A., Ogra P.L., Brasier A.R. (1996). Transcriptional activation of the interleukin-8 gene by respiratory syncytial virus infection in alveolar epithelial cells: nuclear translocation of the RelA transcription factor as a mechanism producing airway mucosal inflammation J Virol 70 8773–8781 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R.P., Kolli D., Casola A. (2013). Respiratory syncytial virus infection: mechanisms of redox control and novel therapeutic opportunities Antioxid Redox Signal 18 186–217 10.1089/ars.2011.4307 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh K.J., Tan C.T., Chew N.K., Tan P.S., Kamarulzaman A., Sarji S.A., Wong K.T., Abdullah B.J., Chua K.B., Lam S.K. (2000). Clinical features of Nipah virus encephalitis among pig farmers in Malaysia N Engl J Med 342 1229–1235 10.1056/NEJM200004273421701 . [DOI] [PubMed] [Google Scholar]
- Gurley E.S., Montgomery J.M., Hossain M.J., Bell M., Azad A.K., Islam M.R., Molla M.A., Carroll D.S., Ksiazek T.G., other authors (2007). Person-to-person transmission of Nipah virus in a Bangladeshi community Emerg Infect Dis 13 1031–1037 10.3201/eid1307.061128 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harcourt B.H., Lowe L., Tamin A., Liu X., Bankamp B., Bowden N., Rollin P.E., Comer J.A., Ksiazek T.G., other authors (2005). Genetic characterization of Nipah virus, Bangladesh, 2004 Emerg Infect Dis 11 1594–1597 10.3201/eid1110.050513 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harit A.K., Ichhpujani R.L., Gupta S., Gill K.S., Lal S., Ganguly N.K., Agarwal S.P. (2006). Nipah/Hendra virus outbreak in Siliguri, West Bengal, India in 2001 Indian J Med Res 123 553–560 . [PubMed] [Google Scholar]
- Hosakote Y.M., Liu T., Castro S.M., Garofalo R.P., Casola A. (2009). Respiratory syncytial virus induces oxidative stress by modulating antioxidant enzymes Am J Respir Cell Mol Biol 41 348–357 10.1165/rcmb.2008-0330OC . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosakote Y.M., Jantzi P.D., Esham D.L., Spratt H., Kurosky A., Casola A., Garofalo R.P. (2011). Viral-mediated inhibition of antioxidant enzymes contributes to the pathogenesis of severe respiratory syncytial virus bronchiolitis Am J Respir Crit Care Med 183 1550–1560 10.1164/rccm.201010-1755OC . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosakote Y.M., Komaravelli N., Mautemps N., Liu T., Garofalo R.P., Casola A. (2012). Antioxidant mimetics modulate oxidative stress and cellular signaling in airway epithelial cells infected with respiratory syncytial virus Am J Physiol Lung Cell Mol Physiol 303 L991–L1000 10.1152/ajplung.00192.2012 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain M.J., Gurley E.S., Montgomery J.M., Bell M., Carroll D.S., Hsu V.P., Formenty P., Croisier A., Bertherat E., other authors (2008). Clinical presentation of Nipah virus infection in Bangladesh Clin Infect Dis 46 977–984 10.1086/529147 . [DOI] [PubMed] [Google Scholar]
- Kashanian S., Ezzati Nazhad Dolatabadi J. (2009). In vitro study of calf thymus DNA interaction with butylated hydroxyanisole DNA Cell Biol 28 535–540 10.1089/dna.2009.0906 . [DOI] [PubMed] [Google Scholar]
- Kim C.H., Kim J.H., Hsu C.Y., Ahn Y.S. (1999). Zinc is required in pyrrolidine dithiocarbamate inhibition of NF-κB activation FEBS Lett 449 28–32 10.1016/S0014-5793(99)00390-7 . [DOI] [PubMed] [Google Scholar]
- Kinnula V.L., Crapo J.D. (2003). Superoxide dismutases in the lung and human lung diseases Am J Respir Crit Care Med 167 1600–1619 10.1164/rccm.200212-1479SO . [DOI] [PubMed] [Google Scholar]
- Knobil K., Choi A.M., Weigand G.W., Jacoby D.B. (1998). Role of oxidants in influenza virus-induced gene expression Am J Physiol 274 L134–L142 . [DOI] [PubMed] [Google Scholar]
- Kong A.N., Owuor E., Yu R., Hebbar V., Chen C., Hu R., Mandlekar S. (2001). Induction of xenobiotic enzymes by the MAP kinase pathway and the antioxidant or electrophile response element (ARE/EpRE) Drug Metab Rev 33 255–271 10.1081/DMR-120000652 . [DOI] [PubMed] [Google Scholar]
- Lo M.K., Rota P.A. (2008). The emergence of Nipah virus, a highly pathogenic paramyxovirus J Clin Virol 43 396–400 10.1016/j.jcv.2008.08.007 . [DOI] [PubMed] [Google Scholar]
- MacNee W. (2001). Oxidative stress and lung inflammation in airways disease Eur J Pharmacol 429 195–207 10.1016/S0014-2999(01)01320-6 . [DOI] [PubMed] [Google Scholar]
- Marsh G.A., Wang L.F. (2012). Hendra and Nipah viruses: why are they so deadly? Curr Opin Virol 2 242–247 10.1016/j.coviro.2012.03.006 . [DOI] [PubMed] [Google Scholar]
- Morcillo E.J., Estrela J., Cortijo J. (1999). Oxidative stress and pulmonary inflammation: pharmacological intervention with antioxidants Pharmacol Res 40 393–404 10.1006/phrs.1999.0549 . [DOI] [PubMed] [Google Scholar]
- Oxford J.S., Perrin D.D. (1974). Inhibition of the particle-associated RNA-dependent RNA polymerase activity of influenza viruses by chelating agents J Gen Virol 23 59–71 10.1099/0022-1317-23-1-59 . [DOI] [PubMed] [Google Scholar]
- Paton N.I., Leo Y.S., Zaki S.R., Auchus A.P., Lee K.E., Ling A.E., Chew S.K., Ang B., Rollin P.E., other authors (1999). Outbreak of Nipah-virus infection among abattoir workers in Singapore Lancet 354 1253–1256 10.1016/S0140-6736(99)04379-2 . [DOI] [PubMed] [Google Scholar]
- Premalatha G.D., Lye M.S., Ariokasamy J., Parashar U.D., Rahmat R., Lee B.Y., Ksiazek T.G. (2000). Assessment of Nipah virus transmission among pork sellers in Seremban, Malaysia Southeast Asian J Trop Med Public Health 31 307–309. [PubMed] [Google Scholar]
- Pyo C.W., Shin N., Jung K.I., Choi J.H., Choi S.Y. (2014). Alteration of copper-zinc superoxide dismutase 1 expression by influenza A virus is correlated with virus replication Biochem Biophys Res Commun 450 711–716 10.1016/j.bbrc.2014.06.037 . [DOI] [PubMed] [Google Scholar]
- Rahman M.A., Hossain M.J., Sultana S., Homaira N., Khan S.U., Rahman M., Gurley E.S., Rollin P.E., Lo M.K., other authors (2012). Date palm sap linked to Nipah virus outbreak in Bangladesh, 2008 Vector Borne Zoonotic Dis 12 65–72 10.1089/vbz.2011.0656 . [DOI] [PubMed] [Google Scholar]
- Reed L.J., Muench H. (1938). A simple method of estimating fifty per cent endpoints Am J Hyg 27 493–497. [Google Scholar]
- Riva D.A., Ríos de Molina M.C., Rocchetta I., Gerhardt E., Coulombié F.C., Mersich S.E. (2006). Oxidative stress in Vero cells infected with vesicular stomatitis virus Intervirology 49 294–298 10.1159/000094245 . [DOI] [PubMed] [Google Scholar]
- Rockx B., Brining D., Kramer J., Callison J., Ebihara H., Mansfield K., Feldmann H. (2011). Clinical outcome of henipavirus infection in hamsters is determined by the route and dose of infection J Virol 85 7658–7671 10.1128/JVI.00473-11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockx B., Winegar R., Freiberg A.N. (2012). Recent progress in henipavirus research: molecular biology, genetic diversity, animal models Antiviral Res 95 135–149 10.1016/j.antiviral.2012.05.008 . [DOI] [PubMed] [Google Scholar]
- Uchide N., Toyoda H. (2011). Antioxidant therapy as a potential approach to severe influenza-associated complications Molecules 16 2032–2052 10.3390/molecules16032032 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchide N., Ohyama K., Bessho T., Yuan B., Yamakawa T. (2002). Effect of antioxidants on apoptosis induced by influenza virus infection: inhibition of viral gene replication and transcription with pyrrolidine dithiocarbamate Antiviral Res 56 207–217 10.1016/S0166-3542(02)00109-2 . [DOI] [PubMed] [Google Scholar]
- Valbuena G., Halliday H., Borisevich V., Goez Y., Rockx B. (2014). A human lung xenograft mouse model of Nipah virus infection PLoS Pathog 10 e1004063 10.1371/journal.ppat.1004063 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong K.T., Shieh W.J., Kumar S., Norain K., Abdullah W., Guarner J., Goldsmith C.S., Chua K.B., Lam S.K., other authors (2002). Nipah virus infection: pathology and pathogenesis of an emerging paramyxoviral zoonosis Am J Pathol 161 2153–2167 10.1016/S0002-9440(10)64493-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada Y., Limmon G.V., Zheng D., Li N., Li L., Yin L., Chow V.T., Chen J., Engelward B.P. (2012). Major shifts in the spatio-temporal distribution of lung antioxidant enzymes during influenza pneumonia PLoS One 7 e31494 10.1371/journal.pone.0031494 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan X., Xu C., Pan Z., Keum Y.S., Kim J.H., Shen G., Yu S., Oo K.T., Ma J., Kong A.N. (2006). Butylated hydroxyanisole regulates ARE-mediated gene expression via Nrf2 coupled with ERK and JNK signaling pathway in HepG2 cells Mol Carcinog 45 841–850 10.1002/mc.20234 . [DOI] [PubMed] [Google Scholar]





