Abstract
Influenza A virus is a major pathogen of birds, swine and humans. Strains can jump between species in a process often requiring mutations and reassortment, resulting in outbreaks and, potentially, pandemics. H9N2 avian influenza is predominant in poultry across Asia and occasionally infects humans and swine. Pandemic H1N1 (H1N1pdm) is endemic in humans and swine and has a history of reassortment in pigs. Previous studies have shown the compatibility of H9N2 and H1N1pdm for reassortment in ferrets, a model for human infection and transmission. Here, the effects of ferret adaptation of H9 surface gene segments on the infectivity and transmission in at-risk natural hosts, specifically swine and quail, were analysed. Reassortant H9N1 and H9N2 viruses, carrying seven or six gene segments from H1N1pdm, showed infectivity and transmissibility in swine, unlike the wholly avian H9N2 virus with ferret-adapted surface genes. In quail, only the reassortant H9N2 with the six internal gene segments from the H1N1pdm strain was able to infect and transmit, although less efficiently than the wholly avian H9N2 virus with ferret-adapted surface genes. These results highlight that ferret-adapted mutations on the haemagglutinin of H9 subtype virus do not restrict the ability of the virus to infect swine and quail, and that the ability to transmit in these species depends on the context of the whole virus. As such, this study emphasizes the threat that H9N2 reassortant viruses pose to humans and agricultural species and the importance of the genetic constellation of the virus to its ability to replicate and transmit in natural hosts of influenza.
Introduction
Influenza A viruses (IAVs) are classified into subtypes based on the antigenic differences of the surface glycoproteins haemagglutinin (HA) and neuraminidase (NA) into 18 HA and 11 NA subtypes, with aquatic birds considered the natural hosts of all subtypes of except H17N10 and H18N11 viruses (Fouchier et al., 2005; Gamblin & Skehel, 2010; Tong et al., 2012, 2013; Webster et al., 1992). IAVs of the H9N2 subtype are low-pathogenic viruses, and two geographically distinct lineages have been described – the North American and Eurasian lineages. Members of the Eurasian lineage jumped into poultry in Asia in the late 1980s causing outbreaks. These outbreaks have occurred in land-based poultry in many countries including China, Iran, Pakistan, Lebanon, Israel and Egypt (Barbour et al., 2006; Davidson et al., 2014; Naeem et al., 1999; Nili & Asasi, 2003), and H9N2 viruses are currently endemic in poultry populations across much of Asia and the Middle East, mainly in chickens, quail and turkeys (Alexander, 2000; Guo et al., 2000; Naeem et al., 1999; Sun et al., 2010).
The H9N2 IAV host range is not restricted to birds. Human and swine infections with H9N2 have been reported. Human infections with H9N2 viruses are relatively few and have been associated with direct contact with infected birds (Uyeki et al., 2002). The first human isolates of H9N2 were recovered in 1999 in Hong Kong from two patients reporting mild respiratory symptoms (Peiris et al., 1999). Studies showed that these isolates were of the Eurasian G1-like sublineage (Lin et al., 2000). Subsequent isolates from sporadic human cases have been from the G1- and Y280-like lineages (Butt et al., 2005, 2010; Cheng et al., 2011). In 1998, the first swine H9N2 of the Y280-like sublineage was isolated in Hong Kong. Unlike human infections, swine infections appear to be more common and are associated with all sublineages (Cong et al., 2007; Rui-Hua et al., 2011; Xu et al., 2008). Incidental and experimental infection of canines and felines with H9N2 have also been reported (Zhang et al., 2013)
H9N2 viruses are of particular interest as they have been identified along with H7 and H5 as having pandemic potential (WHO, 2011). H9N2 viruses have also been identified as the donor, as well as recipient, of the internal genes to the highly pathogenic IAV H5N1 and the newly emerged H7N9 and H10N8 viruses that have infected humans in Asia (Chen et al., 2014; Liu et al., 2013; Wu et al., 2013). Homosubtypic and heterosubtypic H9N2 reassortants have been isolated from both birds and swine in nature (Abolnik et al., 2007; Cong et al., 2007; Wang et al., 2012; Wu et al., 2015; Yu et al., 2008, 2011). Under experimental conditions, H9N2 viruses also demonstrate compatibility for reassortment, especially with regard to human seasonal H3N2 and H1N1pdm viruses, with many reassortants showing increased infectivity, transmissibility and pathogenicity in mice and ferrets (Kimble et al., 2011, 2014; Qiao et al., 2012; Sorrell et al., 2009; Sun et al., 2011; Wan et al., 2008)
We previously reported that a reassortant virus having surface genes from an avian H9N2 virus (A/guinea fowl/Hong Kong/WF10/1999) and internal genes from a human H3N2 virus (A/Memphis/14/1998) – herein referred to as 2WF10 : 6M98 – were transmitted only to direct-contact (DC) ferrets (Wan et al., 2008). We further showed that following mammalian adaptation of the 2WF10 : 6M98 virus in ferrets, a ferret-adapted virus emerged, 2P10 : 6M98, in which only three amino acid changes in the surface genes (T189A in HA1, G192R in HA2 and I28V in the NA) were sufficient for airborne transmission to indirect-contact ferrets (Sorrell et al., 2009). Transferring the HA gene segment of the 2P10 : 6M98 virus (with or without the NA gene segment) into the H1N1pdm backbone (1P10 : 7pdm or 2P10 : 6pdm) also allowed efficient airborne transmission in ferrets (Kimble et al., 2011, 2014).
Whilst our previous results show that two mutations (T189A in HA1 and G192R in HA2) in the HA were essential for airborne transmission of H9 : H1N1pdm reassortants in ferrets, it is unknown whether these mutations would restrict the host range of the reassortant viruses. In this regard, it is important to note that the ferret is widely used as an animal model to study airborne transmission of influenza viruses; adaptive changes that lead to such a phenotype have been identified in the H9, H7 and H5 subtypes (Herfst et al., 2012; Imai et al., 2013; Kimble et al., 2011; Ku et al., 2014; Li et al., 2014; Sorrell et al., 2009; Sutton et al., 2014; Wan et al., 2008). However, further studies are lacking to demonstrate whether the ferret-adaptive mutations increase or restrict the host range of the virus. In this particular case, we aimed to investigate whether H9 HA ferret-adaptive mutations would affect the replication and transmission phenotype of these reassortants in pigs and quail. We chose the pig, an important agricultural species and intermediate host of influenza virus, and the quail, a land-based poultry species that has been shown to allow the replication of multiple influenza viruses (Makarova et al., 2003). Our results showed that the replication and transmission of H9 : H1N1pdm reassortant viruses differed in the swine and quail hosts, and that molecular changes that confer efficient transmission can be virus and host specific.
Results
Effects of ferret-adapted mutations on infectivity, transmissibility and pathogenicity of H9 subtype viruses in swine
To test the effect of mammalian-adapted (ferret-adapted) mutations of the H9 HA (Kimble et al., 2011; Sorrell et al., 2009) for replication and transmission in pigs and quail, five viruses were prepared (Table 1). Viruses containing the ferret-adapted H9 HA gene segment from the A/ferret/Maryland/P10_UMD/2008 (H9N2) virus (2P10 : 6WF10, 2P10 : 6pdm and 1P10 : 7pdm) were rescued in the context of the avian-origin A/guinea fowl/Hong Kong/WF10/1999 (H9N2) (WF10, G1 lineage) or the pandemic-origin A/Netherlands/602/2009 (H1N1) (H1N1pdm). Controls included reverse genetics versions of the wt WF10 and H1N1pdm viruses. Pigs were screened for prior influenza exposure and were negative by an ELISA prior to the study. IAV was not detected in nasal secretions of any pig at 0 days post-inoculation (p.i.). Negative-control pigs remained negative for virus isolation throughout the course of the experiment. Pigs, regardless of group, showed no clinical signs of disease over the course of the study.
Table 1. Genetic content and mutations in viruses used for each experimental group in pigs and quail.
| Virus group | HA subtype | NA subtype | Internal gene | Mutations (gene) |
|---|---|---|---|---|
| 2P10 : 6WF10 | H9 (ferret adapted) | N2 (ferret adapted) | Avian H9N2 | T189A (HA1), G192R (HA2) I28V (NA) |
| 2P10 : 6pdm | H9 (ferret adapted) | N2 (ferret adapted) | Pandemic H1N1 | T189A (HA1), G192R (HA2) I28V (NA) |
| 1P10 : 7pdm | H9 (ferret adapted) | N1(human adapted) | Pandemic H1N1 | T189A (HA1), G192R (HA2) |
| WF10 | H9 (avian) | N2 (avian) | Avian H9N2 | na |
| H1N1pdm | H1 (human adapted) | N1 (human adapted) | Pandemic H1N1 | na |
na, Not applicable.
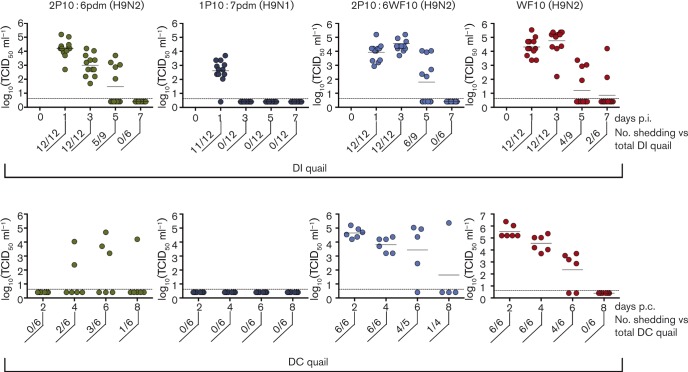
None of the 15 pigs directly inoculated (DI) with the 2P10 : 6WF10 (H9N2 virus with ferret-adaptive mutations in the background of a wt avian H9N2 virus) showed viral shedding at any sampling time points, nor did the DC pigs (data not shown). In contrast and as expected, all nasal swabs from the wt H1N1pdm DI group were positive from 2 to 5 days p.i. and had lower levels of viral shedding on day 6 (3/5 positive), and the pigs stopped shedding virus by 8 days p.i. (Fig. 1, and data not shown). All six H1N1pdm DC pigs were positive for virus by 2 days post-contact (p.c.) and continued shedding for up to 6 days p.c. before beginning to clear the virus, with low levels of virus shedding by 8 days p.c. (3/6 positive) and 10 days p.c. (1/6 positive). The 2P10 : 6pdm (H9N2 virus with ferret-adaptive mutations in the background of six internal gene segments from H1N1pdm) DI pigs shed virus from 2 to 6 days p.i., although the virus titre was, on average, ∼1.5 log10 lower than the group infected with the H1N1pdm virus. DC pigs in the 2P10 : 6pdm group became infected later when compared with the H1N1pdm group. Additionally, there was an apparent second round of transmission within the infected DC pigs, as two previously negative DC pigs began shedding at 10 days p.c., well after the DI pigs had cleared the virus. Overall, four of the six DC pigs became infected with 2P10 : 6pdm virus. Finally, all 1P10 : 7pdm (H9N1 virus with ferret-adaptive mutations in the background of seven gene segments from H1N1pdm) DI pigs shed virus from 2 to 6 days p.i. but were negative by 8 days p.i. (Fig. 1, and data not shown). The 1P10 : 7pdm virus was transmitted efficiently, as five of the six DC pigs began shedding by 4 days p.c. with clearance by 8–10 days p.c. There was also an apparent secondary transmission event in this group, as the one previously negative DC pig began shedding virus at 10 days p.c., making all six of the contact pigs positive for infection. Of note, nasal swabs collected from five DI pigs in the 1P10 : 7pdm virus group that were euthanized on day 3 p.i. were clearly positive for virus isolation but the titres were just above the limit of detection (indicated with an asterisk in Fig. 1). This observation was inconsistent with virus titres in nasal swabs collected from these and other DI pigs in this group at 2 and 4 days p.i., but was consistent with lower virus titres in the bronchoalveolar fluid (BALF) at 3 days p.i. in the same subset of five pigs (Fig. 2c). The significance of such findings remains to be discerned, but it does not change the observation that the 1P10 : 7pdm virus replicated in the respiratory tract of DI pigs.
Fig. 1. Reassortant H9 viruses are transmitted in swine. Pigs (n = 15 per group) were inoculated (DI) with the viruses indicated and nasal swabs were collected at various days p.i. The number of DI pigs positive for viral shedding in each group versus the total number of pigs is listed under each time point. At 3 and 5 days p.i., five DI pigs per group were sacrificed for virus titration in bronchoalveolar fluid. DC pigs (n = 6 per group) were introduced in the same pen housing the DI pigs at 1 day p.i. Nasal swabs were collected from DC pigs and titrated as indicated above. The number of DC pigs positive for viral shedding in each group versus the total number of pigs is listed under each time point. Note the DC graphs were measured in days post-contact (days p.c.) not days p.i. The dashed line indicates the limit of detection and the asterisk denotes virus titers in samples just above limit of detection.
Fig. 2. H9 reassortants result in intermediate pathology and replication in swine lungs. (a, b) Five DI pigs per group were euthanized on day 3 (a) and day 5 p.i. (b). Lungs were scored for visible lesions and the total percentage of the lung surface affected was calculated as described previously (Halbur et al., 1995). Results are shown as means ± sd. (c) BALF samples were collected at the time of necropsy and titrated for virus as TCID50 in Madin–Darby canine kidney cells. Each square represents BALF titres per pig at different time points. A two-way ANOVA was used to determine significant differences with virus and time as factors. The dotted braces indicate statistically significant differences between groups (*P < 0.05; **P < 0.01). The dashed line indicates the limit of detection.
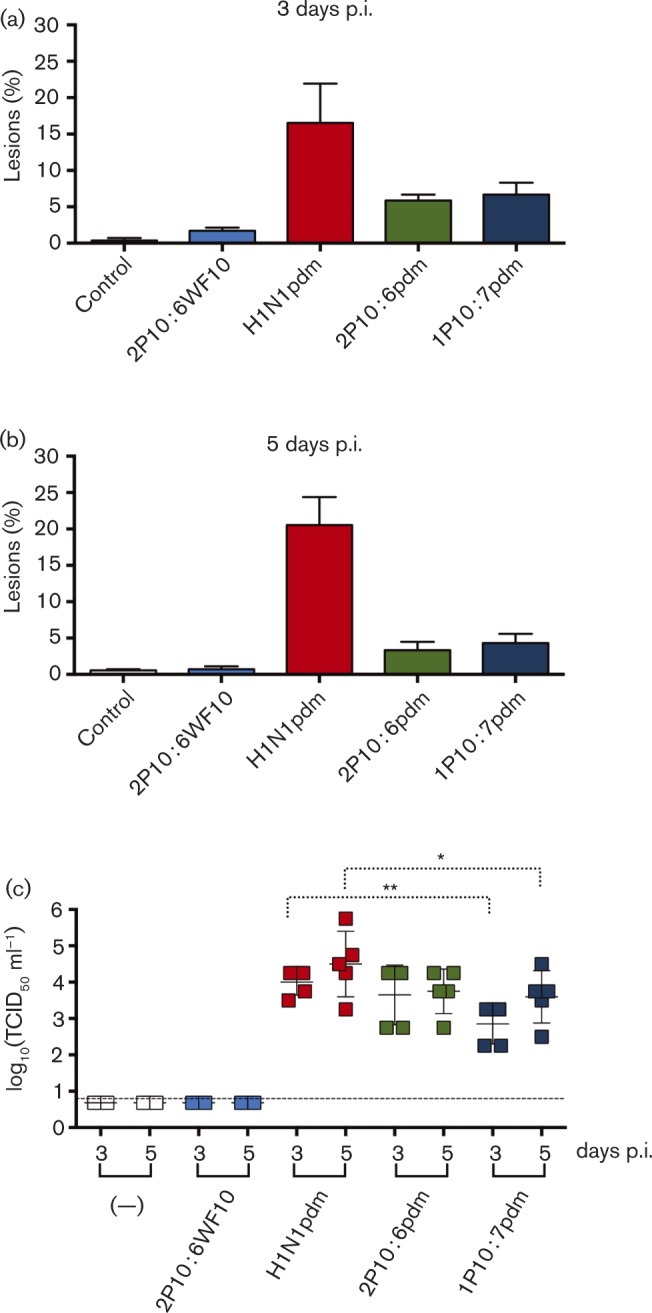
Pathological analysis revealed that pigs inoculated with the 2P10 : 6WF10 virus had very few visible lung lesions at 3 days p.i. and were not different from the negative-control group at 5 days p.i. The H1N1pdm-infected pigs showed the most significant macroscopic lung lesions (Fig. 2a, b), with the mean percentage of lung affected (mean of five pigs per group) being 16.5 and 20.5 % at 3 and 5 days p.i., respectively. Pigs inoculated with the 2P10 : 6pdm and 1P10 : 7pdm viruses showed an intermediate level of gross pathology. The 2P10 : 6pdm group had means of 5.6 and 3.3 % at 3 and 5 days p.i., respectively. The 1P10 : 7pdm group had lesions covering 6.7 and 4.3 % of visible lung surface at 3 and 5 days p.i., respectively (Fig. 2a, b).
The 2P10 : 6WF10 group had no detectable virus in the BALF at either 3 or 5 days p.i., consistent with the nearly complete lack of pathology and lack of virus shedding at these time points (Fig. 2c). The H1N1pdm group had the highest mean titre of all five groups at both 3 and 5 days p.i. The 1P10 : 7pdm group had the lowest mean titre for both days; however, by 5 days p.i. the titre was nearly equivalent to the 2P10 : 6pdm virus group. Consistent with virus shedding in nasal swabs, BALF virus titres from the H1N1pdm-infected pigs were significantly higher than for the 1P10 : 7pdm group at both 3 and 5 days p.i.
Effect of ferret-adapted mutations on infectivity, transmissibility and pathogenicity of H9 subtype viruses in quail
Virus replication in quail respiratory samples was evident in the 2P10 : 6pdm group (Fig. 3), in which DI quail shed virus in the trachea from 1 to 5 days p.i. and became negative by 7 days p.i. In contrast, DI quail in the 1P10 : 7pdm group were positive only at 1 day p.i., quickly clearing the virus and remaining negative for the remainder of the experiment. DI quail in the 2P10 : 6WF10 group were positive for virus from 1 to 5 days p.i. with the highest virus titres at 3 days p.i. This was similar to the wt WF10-infected quail, although in this latter group, virus could be detected at 7 days p.i. None of the DI quail showed clinical signs of disease, consistent with previous observations (Perez et al., 2003a). No virus was isolated from cloacal swabs in any of the groups except occasional shedding in the 2P10 : 6WF10 and wt WF10 groups. None of the PBS control quail shed virus (not shown).
Fig. 3. H9 reassortant viruses replicate and transmit in quail. Quail (n = 12 per group) were inoculated (DI) with the viruses indicated and tracheal and cloacal swabs collected at various days p.i. The number of DI quail positive for viral shedding in each group versus the total number of quail is listed under each time point. DC quail (n = 6 per group) were introduced in the same pen housing the DI pigs at 1 day p.i. The number of DC quail positive for viral shedding in each group versus the total number of quail is listed under each time point. Note the DC graphs were measured in days p.c., not days p.i. The dotted lines indicate the limit of detection.
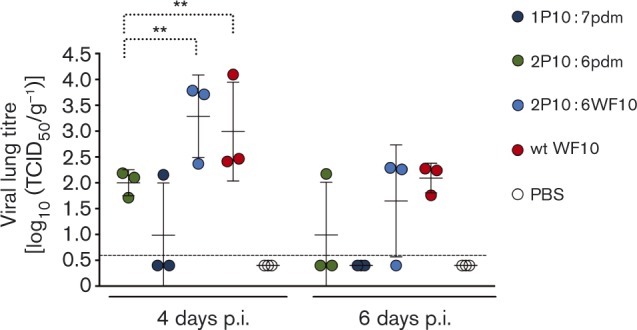
In the DC groups, two of the six DC quail in the 2P10 : 6pdm group were positive for virus by 4 days p.i. and another began shedding on day 5, with these quail shedding for only 2–3 days. DC transmission did not occur in the 1P10 : 7pdm group, as none of the DC quail became positive during the course of the experiment, consistent with the limited shedding in the corresponding DI group. All DC quail in the 2P10 : 6WF10 and wt WF10 groups became positive by 2 days p.c., began to clear virus by 6 days p.c. and had stopped shedding by day 8, except for one DC quail in the 2P10 : 6WF10 group (Fig. 3). Two quail in the 2P10 : 6WF10 DC group were found dead on days 6 and 7 p.c.; however, the cause of death was ruled as idiopathic in nature. Virus titres in the lungs of inoculated quail collected at 4 and 6 days p.i. corresponded well with virus titres in tracheal swabs (Figs 3 and 4). Virus titres in the lungs of quail infected with viruses carrying the WF10 internal gene segments (2P10 : 6WF10 and wt WF10) were ∼1.5 log10 higher compared with those having the pdm backbone (2P10 : 6pdm and 1P10 : 7pdm; Fig. 4).
Fig. 4. Reassortant viruses replicate in quail lungs. On days 4 and 6 p.i., three DI quail per group were euthanized and lung samples were collected for virus titration. Each circle represents the lung titre per quail at different time points. A two-way ANOVA was used to determine significant differences with virus and time as factors. The dotted braces indicates statistically significant differences between groups (**P < 0.01). The dotted line indicates the limit of detection.
Seroconversion in swine and quail is consistent with H9 influenza virus infection
To measure seroconversion to the challenge virus, all surviving pigs were bled at 14 and 20 days p.i. and tested by ELISA for the nucleoprotein (NP) (Table 2). No PBS control pigs showed evidence of seroconversion (data not shown). From the 2P10 : 6WF10 group, only three of the remaining five DI pigs had seroconverted by 20 days p.i. and none of the DC pigs seroconverted, consistent with poor virus replication in this group. It should be noted that one DI pig in the 2P10 : 6pdm group and one DI pig in the H1N1pdm group were euthanized prior to serum collection due to unforeseen circumstances unrelated to the experiment. The DI H1N1pdm group showed seroconversion in three of the four remaining DI pigs at 14 days p.i. and in all four pigs at 20 days p.i. All six DC pigs in the H1N1pdm group seroconverted by 14 days p.i. The DI pigs in the 2P10 : 6pdm group had two out of four seropositive at 14 days p.i. and all four at 20 days p.i.. The two DC pigs that were positive by virus isolation by 6 days p.c. seroconverted by 20 days p.i. and were the only DC pigs to do so. The five remaining DI pigs in the 1P10 : 7pdm virus group were seropositive by 20 days p.i., and four of the six DC pigs in this group seroconverted at 14 days p.i. but only three were positive by 20 days p.i.
Table 2. Seroconversion in pigs and quail after exposure to different viruses.
| Virus group | Pigs: NP ELISA-positive serum* | Quail: HI titres 21 days p.i.† | ||||
|---|---|---|---|---|---|---|
| DI 14 days p.i. | DC 14 days p.i. | DI 20 days p.i. | DC 20 days p.i. | DI | DC | |
| 2P10 : 6pdm | 2/4 | 0/6 | 4/4 | 2/6 | 6/6 (226)‡ | 4/6 |
| 1P10 : 7pdm | 2/5 | 4/6 | 5/5 | 3/6 | 5/6 (57) | 0/6 |
| 2P10 : 6WF10 | 2/5 | 0/6 | 3/5 | 0/6 | 6/6 (1140) | 3/3 (320) |
| H1N1pdm | 3/4 | 6/6 | 4/4 | 6/6 | na | na |
| WF10 | na | na | na | na | 6/6 (507) | 5/5 (735) |
NA, Not applicable.
Number of seropositive pigs out of total number of inoculated (DI) or contact (DC) pigs at 14 and 20 days p.i., using a commercially available kit.
Number of seropositive quail out of total number of DI or DC birds at 21 days p.i.
Numbers in parentheses are geometric mean titres of seropositive samples ± 40.
Quail (six DI and six DC quail per group) serum samples were tested for seroconversion by haemagglutination inhibition (HI) assay (Table 2). None of the negative-control quail seroconverted. Of the six DI quail in the 1P10 : 7pdm group, only one did not seroconvert; however, HI titres were low ( ≤ 80), which is consistent with virus replication below the limit of detection. Also consistent with this observation was the lack of seroconversion in the DC quail in this group, indicating a lack of transmission. All DI quail in the other virus groups had significant HI titres (2P10 : 6pdm ≥ 80; 2P10 : 6WF10 and wt WF10 ≥ 320) against the respective homologous viruses, consistent with active virus replication. Likewise all DC quail in the 2P10 : 6WF10 and wt WF10 groups had HI titres of ≥ 320 consistent with efficient virus transmission. The DC quail in the 2P10 : 6pdm group showed low levels of seroconversion (HI titre ≤ 80) in four of the six quail. In this group, one bird that never shed detectable virus had low HI levels.
Discussion
H9N2 viruses in South-east Asia continue to play a pivotal role in the emergence and maintenance of other avian influenza viruses that affect poultry and are a threat to human health. H9N2 viruses have been the donors of broad-host-range genes through reassortment leading to the emergence of zoonotic viruses like the H5N1, H7N9 and H10N8 strains in China and, more recently, the introduction of Eurasian-lineage H5N8 into the USA and Canada, and subsequent reassortments generating H5N2 and H5N1 mixed-lineage viruses (Eurasian–American) (Chen et al., 2014; Guan et al., 1999; Lee et al., 2015; Liu et al., 2013; Pasick et al., 2015; Wu et al., 2013; Yu et al., 2011). Many of the recent H9N2 isolates from poultry in Asia and the Middle East possess hallmarks of human adaptation and have demonstrated the capacity to occasionally infect humans and swine. The typical mild nature of human H9N2 infections reported to date (Chen et al., 2011; Kimble et al., 2011) suggests that many occurrences may go unreported. Indeed, human serological studies suggest that human exposure is high in poultry workers and in individuals in contact with poultry where H9N2 viruses are present. Studies in Cambodia, Egypt, India, Nigeria and Vietnam have revealed significant exposure of humans to H9N2 viruses (Blair et al., 2013; Huang et al., 2013; Liu et al., 2009; Okoye et al., 2013; Pawar et al., 2012; Uyeki et al., 2012; Zhou et al., 2014).
In this study, we tested the replication and transmission of reassortant H9 : pdm viruses having ferret-adaptive mutations in pigs and quail. We reported previously that three amino acid changes in the surface genes of an avian H9N2 virus conferred efficient airborne transmission of a reassortant H9N2 : H3N2 virus in the ferret model (Sorrell et al., 2009). We further showed that, on the H1N1pdm backbone, the two changes in the HA alone were sufficient for airborne transmission in ferrets without further adaptation (Kimble et al., 2011). In this study, we sought to determine whether the ferret-adaptive mutations would restrict the host range of these viruses in other natural hosts of influenza.
Swine carry both avian (α-2,3 sialic acid)- and human (α-2,6 sialic acid)-like influenza receptors in their respiratory tract (Ito et al., 1998; Kimble et al., 2010; Wan & Perez, 2006). This allows for infection with both avian and human viruses and creates an ideal environment where two different viruses may reassort and lead to novel genotypes. Similar to our results in ferrets, both the 1P10 : 7pdm and 2P10 : 6pdm viruses replicated and were transmitted to contact pigs, with the number of transmission events (number of DC pigs that became virus positive) higher in the 1P10 : 7pdm (H9N1) group compared with the 2P10 : 6pdm (H9N2) group. In a similar study, Qiao et al. (2012) tested alternative H9N1 and H9N2 viruses having H1N1pdm internal gene segment in pigs and chickens and found that the H9N1 reassortant virus with a wholly avian-origin HA gene was also more efficient in replication and transmission in swine compared with a reassortant H9N2, but not in chickens. It is important to emphasize that the studies in that report were consistent with the notion that the H9 HA and N1 NA combination favours the transmission of these viruses in ferrets and pigs but not in chickens or quail. This leaves the possibility of a swine H9N2 : H1N1pdm reassortant adapting to the pig respiratory tract with the potential to transmit to humans. In a report by He et al. (2014) where H9N2 : H1N1pdm reassortants were tested in the guinea pig model, the results were somewhat different, with the (H9N2)2 : 6pdm reassortants transmitting more efficiently than the (H9N1)1 : 7pdm, although the (H9N1)1 : 7pdm viruses displayed enhanced pathogenicity. The animal origin of the H9N2 viruses (avian and swine) as well as different lineages (G1 and Y280) may account for these differences. A recent report from Li et al. (2014) showed that some naturally occurring H9N2 isolates have the capacity for respiratory droplet transmission in ferrets without adaptation. At least one of these isolates was transmitted with apparently higher efficiency, although the mean peak titres were lower than those observed for the H9N2 and H9N1 avian/human reassortants presented previously. The HA of the natural isolates from the study by Li et al. (2014) have in common with our ferret-adapted P10 H9 the I155T mutation, which favours binding to α-2,6 sialic acid, which may favour replication in mammals. However, P10 HA also differed from the viruses described by Li et al. (2014) at 21 other amino acid positions (compared with sites with consensus amino acids). It remains to be determined whether wholly avian H9N2 viruses from the Li et al. (2014) study are compatible for replication and transmission in pigs. It also remains to be determined whether the viruses that showed improved replication and transmission in ferrets in the Li et al. (2014) report will have a similar phenotype in pigs. Further detailed sequence analyses of viruses should shed light on the adaptive changes that take place during initial rounds of replication in different hosts.
A recent report concluded that the H1N1pdm matrix (M) and NA genes cooperate to allow improved replication and transmission of a triple reassortant swine virus in pigs (Ma et al., 2012). Another study showed that the inclusion of the H1N1pdm M and NA genes in the background of a laboratory-adapted A/Puerto Rico/8/1934 (PR8) virus increased the replication and transmission of the resultant reassortant virus compared with the wt PR8 virus in a guinea pig model (Campbell et al., 2014). Our present results in the pig as well as our previous finding in the ferret support this notion, as the efficiency of transmission was increased with the 1P10 : 7pdm virus in both ferrets and pigs.
Quail are another important agricultural species that are susceptible to infection with many influenza subtypes (Makarova et al., 2003; Thontiravong et al., 2012b) and could act as mixing vessels for reassortment (Perez et al., 2003a, b; Thontiravong et al., 2012a). In the quail study, our results showed that reassortant viruses with both ferret-adapted H9 surface genes (HA and NA) on a wt H9 or H1N1pdm backbone (2P10 : 6WF10 and 2P10 : 6pdm, respectively) replicated and were transmitted in quail. The role of the internal gene constellation appeared to be an important factor in the replication and transmission phenotype observed in quail. The 2P10 : 6pdm virus having ferret-adapted surface genes on an H1N1pdm backbone replicated in the quail and was transmitted to 50 % of the infected birds. Replacing the H1N1pdm internal genes with the avian WF10 backbone increased the transmission efficiency of the 2P10 : 6WF10 virus to 100 %, similar to that of wt WF10. This observation reflects the adaptation of the avian- and mammalian-origin backbones for their respective hosts. The importance of the origin of internal genes in the transmission event was also observed in the pigs. In the 2P10 : 6WF10 virus, despite having surface genes that allowed transmission in pigs, the presence of an avian-origin internal gene constellation obliterated replication and transmission in pigs. In the quail study, we also found that the molecular changes due to mammalian adaptation did not affect the ability of the virus to replicate when both ferret-adapted surface genes were present. It has been reported that a functional balance between HA and NA activity is important for virus replication and transmission (Sun et al., 2013; Yen et al., 2011). An imbalance caused by an avian-origin HA and a mammalian-origin NA may account for the lack of proper replication and transmission observed in quail with the 1P10 : 7pdm virus. This poor replication phenotype of an H9N1 reassortant has been reported previously in chickens (Qiao et al., 2012). Amino acids at positions 106 and 248 of the N1 NA of H1N1pdm viruses have been reported to play a role in the low-pH stability of H1N1pdm viruses (Takahashi et al., 2013). This low-pH stability has been shown to be important for N2 NA replication in ducks (Takahashi et al., 2003). A valine-to-isoleucine substitution at position 106 and asparagine-to-aspartic acid at position 248 increased the replication of A/California/04/9009 virus by 10-fold in Madin–Darby canine kidney (MDCK) cells. The N1 NA used in this study had V106 and N248, which may have contributed to the poor replication observed in quail. Further tests to confirm the effects of these mutations are needed but are beyond the scope of the present report.
This study highlighted the potential role that pigs and quail may play as amplifiers of reassortant influenza viruses. It also underscores the potential threat that H9N2 viruses could pose to humans as a future pandemic subtype. Swine can be host to both H9N2 and H1N1pdm viruses, and both viruses have a history of reassortment in swine (Howard et al., 2011; Vijaykrishna et al., 2010; Yu et al., 2011). Pigs could also serve as a suitable environment for adaptation to the mammalian host of any potential reassortant virus. Similarly, quail can be infected with H9 viruses, and H1N1pdm virus has been shown to reassort experimentally in quail following co-infection with other avian influenza viruses (Thontiravong et al., 2012a). The results in this report showed that quail are susceptible to and can transmit reassortant H9N2:H1N1pdm viruses and that transmission of these viruses depends on the compatibility of the surface and internal gene segments. These findings emphasize the need for continued surveillance of influenza in swine and quail and the need for additional research on how H9N2 influenza virus behaves in both species and how hosts can affect reassortment.
Methods
Viruses
Viruses were generated by reverse genetics using previously described plasmids (Kimble et al., 2011; Sorrell et al., 2009). Plasmids containing the genes for A/Netherlands/602/2009 (H1N1) (H1N1pdm), A/guinea fowl/Hong Kong/WF10/1999 (H9N2) (WF10) and the ferret-adapted surface genes from the A/ferret/Maryland/P10_UMD/2008 (H9N2) (P10) virus were used. Five viruses were prepared (Table 1): the wt H1N1pdm and WF10 viruses, the P10 HA and NA on the WF10 backbone (2P10 : 6WF10), the P10 HA with the seven other genes from H1N1pdm (1P10 : 7pdm), and the P10 HA and NA with the six remaining genes from H1N1pdm (2P10 : 6pdm).
Animal studies
Swine studies were performed in large-animal Biosafetly Level 3 for agricultural hazards (BSL3-Ag) facilities of the National Animal Disease Center (NADC), Ames, IA, USA, following protocols approved by the NADC and the University of Maryland Institutional Animal Care and Use Committees (IACUC). The study was done on 3-week-old crossbred pigs obtained from a high-health herd free of swine IAV and porcine reproductive and respiratory syndrome virus. NP-blocking ELISA (IDEXX Laboratories) was used to confirm the absence of antibodies to IAV. Prior to the start of the study, pigs were treated with ceftiofur crystalline-free acid (Pfizer Animal Health) and enrofloxacin (Bayer Animal Health) to reduce bacterial contaminants. The pigs were divided into five groups (n = 15 per group) and inoculated with 2 ml intratracheally and 1 ml intranasally (105 TCID50 ml− 1) of 2P10 : 6pdm, 1P10 : 7pdm, H1N1pdm or 2P10 : 6WF10 virus, or mock inoculated with PBS. Inoculation was performed under anaesthesia, using an intramuscular injection of a cocktail of ketamine [8 mg (kg body weight)− 1], xylazine (4 mg kg− 1) and tiletamine-zolazepam [Telazol; 6 mg (kg body weight)− 1] (Fort Dodge Animal Health). At 2 days p.i., six naive pigs for each virus group were introduced to the 15 inoculated pigs as direct contacts, except in the PBS control group. Nasal swabs (Fisherbrand Dacron swabs; Fisher Scientific) were collected in 2 ml minimal essential medium on 2, 4, 6, 8, 10 and 12 days p.i. On days 3 and 5 p.i., five pigs from each group were swabbed, bled and humanely euthanized with a lethal dose of pentobarbital (Fatal Plus; Vortech Pharmaceuticals). The lungs were scored for macroscopic lesions, followed by collection of BALF for virus titration. Nasal swabs were filtered and subjected to virus isolation by inoculating 200 μl aliquots and 200 μl serum-free Opti-MEM (Gibco, Life Technologies) supplemented with 1 μg tosylsulfonyl phenylalanyl chloromethyl ketone (TPCK)-trypsin ml− 1 and antibiotics onto confluent PBS-washed MDCK cells in 24-well plates. Virus isolation-positive nasal swab and BALF samples were then titrated in MDCK cells as described previously (Kitikoon et al., 2006), and TCID50 titres were calculated according to the method of Reed & Muench (1938).
Quail studies were conducted in a BSL3+ facility at the Department of Veterinary Medicine, University of Maryland, under protocols approved by the IACUC. Four-week-old Japanese quail obtained from B&D Game Farm (Harrah, OK, USA) were kept under observation for 1 week prior to the start of the experiment. NP-blocking ELISA (Synbiotics Co.) was used to confirm the absence of antibodies to influenza virus prior to infection. Quail were randomly divided into four groups (n = 12 per group) and housed in HEPA-filtered isolators. Each quail was infected with 1 ml containing 106 TCID50 ml− 1 of the respective virus through the nares, trachea and cloaca (0.25 ml administered via the trachea and nares and 0.5 ml via the cloaca). A negative-control group of six quail received 1 ml PBS through the same routes. Naive quail (n = 6 per group) were introduced as DC quail at 1 day p.i. Tracheal and cloacal swabs were collected from all quail daily up to 14 days p.i. Swabs were suspended in 1 ml 3.7 % brain–heart infusion medium (Becton Dickinson) containing 10 000 U penicillin, 10 mg streptomycin and 25 μl amphotericin B, and stored at − 80 °C until used in virus titrations. At 4 and 6 days p.i., three DI quail per group were euthanized (two quail in the control group) and lung tissue was collected for viral load titration. The left lung lobe was homogenized in 0.5 ml PBS using 3 mm tungsten carbide beads (Qiagen) in a Tissuelyser LT (Qiagen) at 50 cycles min− 1 for 10 min. Samples were then clarified by centrifugation at 1000 g for 10 min and stored at − 80 °C until used. Swabs and lung homogenate samples were titrated in MDCK cells, as described above.
Serological analysis
Pig serum samples collected at 14 and 20 days p.i. were tested for anti-NP antibodies by ELISA as described above. Quail serum samples collected at 21 days p.i. were tested by HI assay. HI assays were performed following treatment of the samples with receptor-destroying enzyme (Denka Seiken) and heat inactivation at 56 °C for 30 min to remove non-specific HA inhibitors and natural serum agglutinins. HI assays were performed with 8 haemagglutination units of each virus antigen and 0.5 % chicken red blood cells according to standard techniques (WHO, 2002). Negative and positive controls were included in the assay. Seroconversion was considered positive when HI titres to homologous virus were ≥ 40.
Statistical analysis
Statistical analyses were performed using GraphPad Prism software version 4.00 (GraphPad Software). Comparison between two treatment means was done using Student's t-test, whilst multiple mean comparisons was done using two-way ANOVA followed by Bonferroni's multiple comparison test. P < 0.05 was considered significant.
Acknowledgements
We thank Diego Lopez and Haichen Song for technical assistance. This research was funded by NIAID-NIH contracts (HHSN266200700010C and HHSN272201400008C) and USDA-ARS. The studies presented above were performed prior to the USG moratorium on gain-of-function studies implemented on 17 October 2014.
References
- Abolnik C., Bisschop S., Gerdes T., Olivier A., Horner R. (2007). Outbreaks of avian influenza H6N2 viruses in chickens arose by a reassortment of H6N8 and H9N2 ostrich viruses Virus Genes 34 37–45 10.1007/s11262-006-0007-6 . [DOI] [PubMed] [Google Scholar]
- Alexander D.J. (2000). A review of avian influenza in different bird species Vet Microbiol 74 3–13 10.1016/S0378-1135(00)00160-7 . [DOI] [PubMed] [Google Scholar]
- Barbour E.K., Sagherian V.K., Sagherian N.K., Dankar S.K., Jaber L.S., Usayran N.N., Farran M.T. (2006). Avian influenza outbreak in poultry in the Lebanon and transmission to neighbouring farmers and swine Vet Ital 42 77–85 . [PubMed] [Google Scholar]
- Blair P.J., Putnam S.D., Krueger W.S., Chum C., Wierzba T.F., Heil G.L., Yasuda C.Y., Williams M., Kasper M.R., other authors (2013). Evidence for avian H9N2 influenza virus infections among rural villagers in Cambodia J Infect Public Health 6 69–79 10.1016/j.jiph.2012.11.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butt K.M., Smith G.J.D., Chen H., Zhang L.J., Leung Y.H.C., Xu K.M., Lim W., Webster R.G., Yuen K.Y., other authors (2005). Human infection with an avian H9N2 influenza A virus in Hong Kong in 2003 J Clin Microbiol 43 5760–5767 10.1128/JCM.43.11.5760-5767.2005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butt A.M., Siddique S., Idrees M., Tong Y. (2010). Avian influenza A (H9N2): computational molecular analysis and phylogenetic characterization of viral surface proteins isolated between 1997 and 2009 from the human population Virol J 7 319 10.1186/1743-422X-7-319 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell P.J., Danzy S., Kyriakis C.S., Deymier M.J., Lowen A.C., Steel J. (2014). The M segment of the 2009 pandemic influenza virus confers increased neuraminidase activity, filamentous morphology, and efficient contact transmissibility to A/Puerto Rico/8/1934-based reassortant viruses J Virol 88 3802–3814 10.1128/JVI.03607-13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Zheng Q., Yang K., Zeng F., Lau S.Y., Wu W.L., Huang S., Zhang J., Chen H., Xia N. (2011). Serological survey of antibodies to influenza A viruses in a group of people without a history of influenza vaccination Clin Microbiol Infect 17 1347–1349 10.1111/j.1469-0691.2011.03538.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Yuan H., Gao R., Zhang J., Wang D., Xiong Y., Fan G., Yang F., Li X., other authors (2014). Clinical and epidemiological characteristics of a fatal case of avian influenza A H10N8 virus infection: a descriptive study Lancet 383 714–721 10.1016/S0140-6736(14)60111-2 . [DOI] [PubMed] [Google Scholar]
- Cheng V.C., Chan J.F., Wen X., Wu W.L., Que T.L., Chen H., Chan K.H., Yuen K.Y. (2011). Infection of immunocompromised patients by avian H9N2 influenza A virus J Infect 62 394–399 10.1016/j.jinf.2011.02.007 . [DOI] [PubMed] [Google Scholar]
- Cong Y.L., Pu J., Liu Q.F., Wang S., Zhang G.Z., Zhang X.L., Fan W.X., Brown E.G., Liu J.H. (2007). Antigenic and genetic characterization of H9N2 swine influenza viruses in China J Gen Virol 88 2035–2041 10.1099/vir.0.82783-0 . [DOI] [PubMed] [Google Scholar]
- Davidson I., Fusaro A., Heidari A., Monne I., Cattoli G. (2014). Molecular evolution of H9N2 avian influenza viruses in Israel Virus Genes 48 457–463 10.1007/s11262-014-1037-0 . [DOI] [PubMed] [Google Scholar]
- Fouchier R.A., Munster V., Wallensten A., Bestebroer T.M., Herfst S., Smith D., Rimmelzwaan G.F., Olsen B., Osterhaus A.D. (2005). Characterization of a novel influenza A virus hemagglutinin subtype (H16) obtained from black-headed gulls J Virol 79 2814–2822 10.1128/JVI.79.5.2814-2822.2005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamblin S.J., Skehel J.J. (2010). Influenza hemagglutinin and neuraminidase membrane glycoproteins J Biol Chem 285 28403–28409 10.1074/jbc.R110.129809 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan Y., Shortridge K.F., Krauss S., Webster R.G. (1999). Molecular characterization of H9N2 influenza viruses: were they the donors of the “internal” genes of H5N1 viruses in Hong Kong? Proc Natl Acad Sci U S A 96 9363–9367 10.1073/pnas.96.16.9363 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y.J., Krauss S., Senne D.A., Mo I.P., Lo K.S., Xiong X.P., Norwood M., Shortridge K.F., Webster R.G., Guan Y. (2000). Characterization of the pathogenicity of members of the newly established H9N2 influenza virus lineages in Asia Virology 267 279–288 10.1006/viro.1999.0115 . [DOI] [PubMed] [Google Scholar]
- Halbur P.G., Paul P.S., Frey M.L., Landgraf J., Eernisse K., Meng X.J., Lum M.A., Andrews J.J., Rathje J.A. (1995). Comparison of the pathogenicity of two US porcine reproductive and respiratory syndrome virus isolates with that of the Lelystad virus Vet Pathol 32 648–660 10.1177/030098589503200606 . [DOI] [PubMed] [Google Scholar]
- He L., Wu Q., Jiang K., Duan Z., Liu J., Xu H., Cui Z., Gu M., Wang X., other authors (2014). Differences in transmissibility and pathogenicity of reassortants between H9N2 and 2009 pandemic H1N1 influenza A viruses from humans and swine Arch Virol 159 1743–1754 10.1007/s00705-014-2009-3 . [DOI] [PubMed] [Google Scholar]
- Herfst S., Schrauwen E.J., Linster M., Chutinimitkul S., de Wit E., Munster V.J., Sorrell E.M., Bestebroer T.M., Burke D.F., other authors (2012). Airborne transmission of influenza A/H5N1 virus between ferrets Science 336 1534–1541 10.1126/science.1213362 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard W.A., Essen S.C., Strugnell B.W., Russell C., Barass L., Reid S.M., Brown I.H. (2011). Reassortant pandemic (H1N1) 2009 virus in pigs, United Kingdom Emerg Infect Dis 17 1049–1052 10.3201/eid/1706.101886 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang R., Wang A.R., Liu Z.H., Liang W., Li X.X., Tang Y.J., Miao Z.M., Chai T.J. (2013). Seroprevalence of avian influenza H9N2 among poultry workers in Shandong Province, China Eur J Clin Microbiol Infect Dis 32 1347–1351 10.1007/s10096-013-1888-7 . [DOI] [PubMed] [Google Scholar]
- Imai M., Herfst S., Sorrell E.M., Schrauwen E.J., Linster M., De Graaf M., Fouchier R.A., Kawaoka Y. (2013). Transmission of influenza A/H5N1 viruses in mammals Virus Res 178 15–20 10.1016/j.virusres.2013.07.017 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito T., Couceiro J.N., Kelm S., Baum L.G., Krauss S., Castrucci M.R., Donatelli I., Kida H., Paulson J.C., other authors (1998). Molecular basis for the generation in pigs of influenza A viruses with pandemic potential J Virol 72 7367–7373 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimble B., Nieto G.R., Perez D.R. (2010). Characterization of influenza virus sialic acid receptors in minor poultry species Virol J 7 365 10.1186/1743-422X-7-365 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimble J.B., Sorrell E., Shao H., Martin P.L., Perez D.R. (2011). Compatibility of H9N2 avian influenza surface genes and 2009 pandemic H1N1 internal genes for transmission in the ferret model Proc Natl Acad Sci U S A 108 12084–12088 10.1073/pnas.1108058108 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimble J.B., Angel M., Wan H., Sutton T.C., Finch C., Perez D.R. (2014). Alternative reassortment events leading to transmissible H9N1 influenza viruses in the ferret model J Virol 88 66–71 10.1128/JVI.02677-13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitikoon P., Nilubol D., Erickson B.J., Janke B.H., Hoover T.C., Sornsen S.A., Thacker E.L. (2006). The immune response and maternal antibody interference to a heterologous H1N1 swine influenza virus infection following vaccination Vet Immunol Immunopathol 112 117–128 10.1016/j.vetimm.2006.02.008 . [DOI] [PubMed] [Google Scholar]
- Ku K.B., Park E.H., Yum J., Kim H.M., Kang Y.M., Kim J.C., Kim J.A., Kim H.S., Seo S.H. (2014). Transmissibility of novel H7N9 and H9N2 avian influenza viruses between chickens and ferrets Virology 450–451 316–323 10.1016/j.virol.2013.12.022 . [DOI] [PubMed] [Google Scholar]
- Lee D.H., Torchetti M.K., Winker K., Ip H.S., Song C.S., Swayne D.E. (2015). Intercontinental spread of Asian-origin H5N8 to North America through Beringia by migratory birds J Virol 89 6521–6524 10.1128/JVI.00728-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Shi J., Guo J., Deng G., Zhang Q., Wang J., He X., Wang K., Chen J., other authors (2014). Genetics, receptor binding property, and transmissibility in mammals of naturally isolated H9N2 avian influenza viruses PLoS Pathog 10 e1004508 10.1371/journal.ppat.1004508 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y.P., Shaw M., Gregory V., Cameron K., Lim W., Klimov A., Subbarao K., Guan Y., Krauss S., other authors (2000). Avian-to-human transmission of H9N2 subtype influenza A viruses: relationship between H9N2 and H5N1 human isolates Proc Natl Acad Sci U S A 97 9654–9658 10.1073/pnas.160270697 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Lu E.J., Wang Y.L., Di B., Li T.G., Zhou Y., Yang L.L., Xu X.Y., Fu C.X., Wang M. (2009). [Avian influenza virus infection in people occupied in poultry fields in Guangzhou city] Zhonghua Liu Xing Bing Xue Za Zhi 30 1111–1113 (in Chinese). [PubMed] [Google Scholar]
- Liu D., Shi W., Shi Y., Wang D., Xiao H., Li W., Bi Y., Wu Y., Li X., other authors (2013). Origin and diversity of novel avian influenza A H7N9 viruses causing human infection: phylogenetic, structural, and coalescent analyses Lancet 381 1926–1932 10.1016/S0140-6736(13)60938-1 . [DOI] [PubMed] [Google Scholar]
- Ma W., Liu Q., Bawa B., Qiao C., Qi W., Shen H., Chen Y., Ma J., Li X., other authors (2012). The neuraminidase and matrix genes of the 2009 pandemic influenza H1N1 virus cooperate functionally to facilitate efficient replication and transmissibility in pigs J Gen Virol 93 1261–1268 10.1099/vir.0.040535-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makarova N.V., Ozaki H., Kida H., Webster R.G., Perez D.R. (2003). Replication and transmission of influenza viruses in Japanese quail Virology 310 8–15 10.1016/S0042-6822(03)00094-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naeem K., Ullah A., Manvell R.J., Alexander D.J. (1999). Avian influenza A subtype H9N2 in poultry in Pakistan Vet Rec 145 560 10.1136/vr.145.19.560 . [DOI] [PubMed] [Google Scholar]
- Nili H., Asasi K. (2003). Avian influenza (H9N2) outbreak in Iran Avian Dis 47 828–831 10.1637/0005-2086-47.s3.828 . [DOI] [PubMed] [Google Scholar]
- Okoye J., Eze D., Krueger W.S., Heil G.L., Friary J.A., Gray G.C. (2013). Serologic evidence of avian influenza virus infections among Nigerian agricultural workers J Med Virol 85 670–676 10.1002/jmv.23520 . [DOI] [PubMed] [Google Scholar]
- Pasick J., Berhane Y., Joseph T., Bowes V., Hisanaga T., Handel K., Alexandersen S. (2015). Reassortant highly pathogenic influenza A H5N2 virus containing gene segments related to Eurasian H5N8 in British Columbia Canada, 2014. Sci Rep 5 9484 10.1038/srep09484 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawar S.D., Tandale B.V., Raut C.G., Parkhi S.S., Barde T.D., Gurav Y.K., Kode S.S., Mishra A.C. (2012). Avian influenza H9N2 seroprevalence among poultry workers in Pune, India, 2010 PLoS One 7 e36374 10.1371/journal.pone.0036374 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris M., Yuen K.Y., Leung C.W., Chan K.H., Ip P.L., Lai R.W., Orr W.K., Shortridge K.F. (1999). Human infection with influenza H9N2 Lancet 354 916–917 10.1016/S0140-6736(99)03311-5 . [DOI] [PubMed] [Google Scholar]
- Perez D.R., Lim W., Seiler J.P., Yi G., Peiris M., Shortridge K.F., Webster R.G. (2003a). Role of quail in the interspecies transmission of H9 influenza A viruses: molecular changes on HA that correspond to adaptation from ducks to chickens J Virol 77 3148–3156 10.1128/JVI.77.5.3148-3156.2003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez D.R., Webby R.J., Hoffmann E., Webster R.G. (2003b). Land-based birds as potential disseminators of avian mammalian reassortant influenza A viruses Avian Dis 47 1114–1117 10.1637/0005-2086-47.s3.1114 . [DOI] [PubMed] [Google Scholar]
- Qiao C., Liu Q., Bawa B., Shen H., Qi W., Chen Y., Mok C.K., García-Sastre A., Richt J.A., Ma W. (2012). Pathogenicity and transmissibility of reassortant H9 influenza viruses with genes from pandemic H1N1 virus J Gen Virol 93 2337–2345 10.1099/vir.0.044040-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed L.J., Muench H. (1938). A simple method for estimating fifty per cent endpoints Am J Hyg 27 493–497. [Google Scholar]
- Rui-Hua Z., Hong-Yu C., Ming-Ju X., Kai L., Hua-Lan C., Cun-Lian W., Dong W., Cun-Xin L., Tong X. (2011). Molecular characterization and pathogenicity of swine influenza H9N2 subtype virus A/swine/HeBei/012/2008/(H9N2) Acta Virol 55 219–226 10.4149/av_2011_03_219 . [DOI] [PubMed] [Google Scholar]
- Sorrell E.M., Wan H., Araya Y., Song H., Perez D.R. (2009). Minimal molecular constraints for respiratory droplet transmission of an avian–human H9N2 influenza A virus Proc Natl Acad Sci U S A 106 7565–7570 10.1073/pnas.0900877106 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Pu J., Jiang Z., Guan T., Xia Y., Xu Q., Liu L., Ma B., Tian F., other authors (2010). Genotypic evolution and antigenic drift of H9N2 influenza viruses in China from 1994 to 2008 Vet Microbiol 146 215–225 10.1016/j.vetmic.2010.05.010 . [DOI] [PubMed] [Google Scholar]
- Sun Y., Qin K., Wang J., Pu J., Tang Q., Hu Y., Bi Y., Zhao X., Yang H., other authors (2011). High genetic compatibility and increased pathogenicity of reassortants derived from avian H9N2 and pandemic H1N1/2009 influenza viruses Proc Natl Acad Sci U S A 108 4164–4169 10.1073/pnas.1019109108 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Tan Y., Wei K., Sun H., Shi Y., Pu J., Yang H., Gao G.F., Yin Y., other authors (2013). Amino acid 316 of hemagglutinin and the neuraminidase stalk length influence virulence of H9N2 influenza virus in chickens and mice J Virol 87 2963–2968 10.1128/JVI.02688-12 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton T.C., Finch C., Shao H., Angel M., Chen H., Capua I., Cattoli G., Monne I., Perez D.R. (2014). Airborne transmission of highly pathogenic H7N1 influenza virus in ferrets J Virol 88 6623–6635 10.1128/JVI.02765-13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi T., Suzuki T., Hidari K.I.P.J., Miyamoto D., Suzuki Y. (2003). A molecular mechanism for the low-pH stability of sialidase activity of influenza A virus N2 neuraminidases FEBS Lett 543 71–75 10.1016/S0014-5793(03)00403-4 . [DOI] [PubMed] [Google Scholar]
- Takahashi T., Song J., Suzuki T., Kawaoka Y. (2013). Mutations in NA that induced low pH-stability and enhanced the replication of pandemic (H1N1) 2009 influenza A virus at an early stage of the pandemic PLoS One 8 e64439 10.1371/journal.pone.0064439 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thontiravong A., Kitikoon P., Wannaratana S., Tantilertcharoen R., Tuanudom R., Pakpinyo S., Sasipreeyajan J., Oraveerakul K., Amonsin A. (2012a). Quail as a potential mixing vessel for the generation of new reassortant influenza A viruses Vet Microbiol 160 305–313 10.1016/j.vetmic.2012.05.043 . [DOI] [PubMed] [Google Scholar]
- Thontiravong A., Wannaratana S., Tantilertcharoen R., Prakairungnamthip D., Tuanudom R., Sasipreeyajan J., Pakpinyo S., Amonsin A., Kitikoon P., Oraveerakul K. (2012b). Comparative study of pandemic (H1N1) 2009, swine H1N1, and avian H3N2 influenza viral infections in quails J Vet Sci 13 395–403 10.4142/jvs.2012.13.4.395 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong S., Li Y., Rivailler P., Conrardy C., Castillo D.A., Chen L.M., Recuenco S., Ellison J.A., Davis C.T., other authors (2012). A distinct lineage of influenza A virus from bats Proc Natl Acad Sci U S A 109 4269–4274 10.1073/pnas.1116200109 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong S., Zhu X., Li Y., Shi M., Zhang J., Bourgeois M., Yang H., Chen X., Recuenco S., other authors (2013). New world bats harbor diverse influenza A viruses PLoS Pathog 9 e1003657 10.1371/journal.ppat.1003657 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uyeki T.M., Chong Y.H., Katz J.M., Lim W., Ho Y.Y., Wang S.S., Tsang T.H., Au W.W., Chan S.C., other authors (2002). Lack of evidence for human-to-human transmission of avian influenza A (H9N2) viruses in Hong Kong, China 1999 Emerg Infect Dis 8 154–159 10.3201/eid0802.010148 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uyeki T.M., Nguyen D.C., Rowe T., Lu X., Hu-Primmer J., Huynh L.P., Hang N.L., Katz J.M. (2012). Seroprevalence of antibodies to avian influenza A (H5) and A (H9) viruses among market poultry workers, Hanoi, Vietnam, 2001 PLoS One 7 e43948 10.1371/journal.pone.0043948 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijaykrishna D., Poon L.L., Zhu H.C., Ma S.K., Li O.T., Cheung C.L., Smith G.J., Peiris J.S., Guan Y. (2010). Reassortment of pandemic H1N1/2009 influenza A virus in swine Science 328 1529 10.1126/science.1189132 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan H., Perez D.R. (2006). Quail carry sialic acid receptors compatible with binding of avian and human influenza viruses Virology 346 278–286 10.1016/j.virol.2005.10.035 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan H., Sorrell E.M., Song H., Hossain M.J., Ramirez-Nieto G., Monne I., Stevens J., Cattoli G., Capua I., other authors (2008). Replication and transmission of H9N2 influenza viruses in ferrets: evaluation of pandemic potential PLoS One 3 e2923 10.1371/journal.pone.0002923 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B., Chen Q., Chen Z. (2012). Complete genome sequence of an H9N2 avian influenza virus isolated from egret in Lake Dongting wetland J Virol 86 11939 10.1128/JVI.02042-12 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster R.G., Bean W.J., Gorman O.T., Chambers T.M., Kawaoka Y. (1992). Evolution and ecology of influenza A viruses Microbiol Rev 56 152–179 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2002). Identification of influenza isolates by haemagglutination. In WHO Manual on Animal Influenza Diagnosis and Surveillance, pp. 28–36 Geneva: World Health Organization. [Google Scholar]
- Wu S., Wu F., He J. (2013). Emerging risk of H7N9 influenza in China Lancet 381 1539–1540 10.1016/S0140-6736(13)60767-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu D., Zou S., Bai T., Li J., Zhao X., Yang L., Liu H., Li X., Yang X., other authors (2015). Poultry farms as a source of avian influenza A (H7N9) virus reassortment and human infection Sci Rep 5 7630 10.1038/srep07630 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X.J., Xu G.Y., Zhou H.B., Yu Z.J., Zhang A.D., Song Y.F., Jin M.L., Chen H.C. (2008). Evolutionary characterization of influenza virus A/duck/Hubei/W1/2004 (H9N2) isolated from central China Virus Genes 36 79–83 10.1007/s11262-007-0123-y . [DOI] [PubMed] [Google Scholar]
- Yen H.L., Liang C.H., Wu C.Y., Forrest H.L., Ferguson A., Choy K.T., Jones J., Wong D.D.Y., Cheung P.P.H., other authors (2011). Hemagglutinin–neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets Proc Natl Acad Sci U S A 108 14264–14269 10.1073/pnas.1111000108 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H., Hua R.H., Wei T.C., Zhou Y.J., Tian Z.J., Li G.X., Liu T.Q., Tong G.Z. (2008). Isolation and genetic characterization of avian origin H9N2 influenza viruses from pigs in China Vet Microbiol 131 82–92 10.1016/j.vetmic.2008.02.024 . [DOI] [PubMed] [Google Scholar]
- Yu H., Zhou Y.J., Li G.X., Ma J.H., Yan L.P., Wang B., Yang F.R., Huang M., Tong G.Z. (2011). Genetic diversity of H9N2 influenza viruses from pigs in China: a potential threat to human health? Vet Microbiol 149 254–261 10.1016/j.vetmic.2010.11.008 . [DOI] [PubMed] [Google Scholar]
- Zhang K., Zhang Z., Yu Z., Li L., Cheng K., Wang T., Huang G., Yang S., Zhao Y., other authors (2013). Domestic cats and dogs are susceptible to H9N2 avian influenza virus Virus Res 175 52–57 10.1016/j.virusres.2013.04.004 . [DOI] [PubMed] [Google Scholar]
- Zhou P., Zhu W., Gu H., Fu X., Wang L., Zheng Y., He S., Ke C., Wang H., other authors (2014). Avian influenza H9N2 seroprevalence among swine farm residents in China J Med Virol 86 597–600 10.1002/jmv.23869 . [DOI] [PubMed] [Google Scholar]