Abstract
Objectives.
Evidence suggests social relationships may be important facilitators for recovery from functional impairment, but the extant literature is limited in its measurement of social relationships including an over emphasis on filial social support and a paucity of nationally representative data.
Methods.
Using data from Waves 4–9 (1998–2008) of the Health and Retirement Study (HRS), this research examines the association between social relationships and recovery from severe mobility limitation (i.e., difficulty walking one block or across the room) among older Americans. Using a more nuanced measure of recovery that includes complete and partial recovery, a series of discrete-time event history models with multiple competing recovery outcomes were estimated using multinomial logistic regression.
Results.
Providing instrumental support to peers increased the odds of complete and partial recovery from severe mobility limitation, net of numerous social, and health factors. Having relatives living nearby decreased the odds of complete recovery, while being engaged in one’s neighborhood increased the odds of partial recovery. The influence of partner status on partial and complete recovery varied by gender, whereby partnered men were more likely to experience recovery relative to partnered women. The effect of neighborhood engagement on partial recovery also varied by gender. Disengaged women were the least likely to experience partial recovery compared with any other group.
Discussion.
The rehabilitative potential of social relationships has important policy implications. Interventions aimed at encouraging older adults with mobility limitation to be engaged in their neighborhoods and/or provide instrumental support to peers may improve functional health outcomes.
Key Words: Functional health—Gender—Mobility, Recovery, Social relationships, Social support
The link between social relationships and health has been well documented. Larger social networks (i.e., greater numbers of ties or denser networks) and perceived social support have been found to be negatively associated with mortality (Eng, Rimm, Fitzmaurice, & Kawachi, 2002; House, Landis, & Umberson, 1988), psychiatric morbidity (Bowling, Farquhar, & Browne, 1991), and functional impairment (Mendes de Leon et al., 1999) in later life. The purpose of this article is to extend this line of research by testing the rehabilitative potential of social relationships for functional health recovery among older adults. Specifically, we test whether social relationships serve as facilitators of recovery from severe mobility limitation (i.e., difficulty walking one block or across the room). The loss of mobility is an important predictor of disability onset, institutionalization, and premature mortality (Melzer, Lan, & Guralnik, 2003). Prior research has emphasized the benefits of social relationships for preventing functional health declines (e.g., disability onset), yet research exploring the link between social relationships and recovery from functional impairment has typically been more limited. Previous research on disease management and postsurgical recovery in relation to social relationships suggests the rehabilitative potential of social relationships. For example, a large body of empirical evidence links positive social relationships to better functional health outcomes among stroke patients (see Glass & Maddox, 1992; Tsouna-Hadjis, Vemmos, Zakopoulos, & Stamatelopoulos, 2000). While these and other similar studies provide evidence for the significance of social relationships for recovery, most rely on clinical data and are often limited in scope and may represent homogenous populations. Moreover, measured sources of support are almost exclusively spousal, adult child, and/or healthcare professional, neglecting the importance of peer relationships for health. Clinical studies also frequently overlook the gendered nature of older adults’ social relationships, a limitation addressed by this analysis.
This research aims to broaden the current social relationship and recovery literature by examining multiple sources of social support among a national sample of older Americans and testing whether gender moderates the effect of social relationships on recovery from severe mobility limitation. The aspects of social relationships that are protective for maintaining mobility in later life may continue to play a role in recovery from mobility limitation. Indeed, social relationships may become more salient for those who have experienced a serious health decline or loss of independence.
Social Relationships and Health
The term “social relationships” often refers to multiple distinct features of social connection offered by relationships, including social integration, quality of relationships, and network structures (Umberson & Montez, 2010). Cohen, Underwood, and Gottlieb (2000) conceptualize social relationships as influencing health via two main processes: social support and social participation. Social support refers to the specific supportive actions performed by network members, such as the provision of emotional or financial support (Gruenewald & Seeman, 2010). Cohen et al. (2000) highlight the importance of exchange (e.g., instrumental, informational, or emotional) when defining social support. Social participation shapes health status through participation in social groups by influencing “cognitions, emotions, behaviors, and biological responses” (Cohen et al., 2000: 4) and is differentiated from social support by its emphasis on social connections rather than exchange of resources.
Within the processes of social support and social participation, there are numerous underlying mechanisms linking social relationships to better health, broadly classified as psychosocial and behavioral mechanisms. Within the psychosocial framework, social relationships are typically viewed as a stress buffer. Social relationships may mitigate stressful events through social exchange (e.g., sharing resources), social comparison, or personal control. While psychosocial mechanisms may refer to aspects of mental health such as emotional responses or the role of symbolic meanings and norms, behavioral explanations emphasize the influence of social relationships on the participation in health behaviors such diet and physical activity as well as healthcare utilization (Umberson & Montez, 2010). Social support and social participation often occur simultaneously; therefore, it is difficult to isolate the specific explanatory factors for each process. However, it is clear that social relationships have the capacity to influence psychosocial and behavioral reactions via social support and participation, which, in turn, influences health.
Social Relationships, Gender, and Physical Health among Older Adults
Most research examining social relationships in later life underscores the role of family. Previous empirical research has noted the predominance of family within the social networks of older adults (Antonucci, 1990). In particular, prior research suggests that spouses and adult children are key members of the elderly’s social network (Zhang & Hayward, 2001). Although family members are essential members of older adults’ social networks, friends and neighbors are also valuable sources of social support. Previous research demonstrates a preference among the elderly to receive social support from friends or neighbors rather than family (Adams & Blieszner, 1989; Adams & Blieszner, 1995; Griffith, 1985). Additionally, a study exploring social participation and mortality among older adults observed an increase in rates of survival among respondents who spent time with friends; this association was not found for other types of social contact including time spent with spouse or family after adjusting for numerous demographic and health covariates (Maier & Klumb, 2005). Maier & Klumb, (2005) research suggests that time spent with friends was more important for survival than other types of social contact. According to Gallant, Spitze, and Prohaska (2007), among older adults managing a chronic illness, social support from friends has fewer negative influences than family members. Likewise, compared with family members, friends of older adults with chronic illness are more important for the provision of emotional and informational support (Gallant et al., 2007) and participating in health-promoting management behavior (Gallant, 2003; Schiøtz et al., 2012). While family members may provide various kinds of social support, previous research suggests that family members are the primary suppliers of instrumental support, whereas friendships appear to benefit health mainly through emotional and information support.
There are important gender differences in composition and effect of older adults’ social networks. Older women generally have larger social networks, while older men tend to have smaller networks with their wives (partners) occupying a central role (Antonucci, 1990; Antonucci & Akiyama, 1987; Umberson, 1992). To illustrate, wives are much less likely (with a 75% reduction in the odds) to select their husband as a primary caregiver while undergoing cancer treatments (Allen, Goldscheider, & Ciambrone, 1999). In general, the presence of family members and positive social support in an older individual’s social network confers physical health advantages for both men and women (Seeman, Singer, Ryff, Dienberg Love, & Levy-Storms, 2002; Warner & Kelley-Moore, 2012), yet men and women may experience differing levels of health benefits from filial support. Not only are men more likely to be partnered in later life (England & McClintock, 2010), but these partnerships appear to be more advantageous for men’s health partly due to wives’ emotional responsiveness and enactment of greater social control of men’s health behaviors (Spitze & Ward, 2000; Umberson, 1992). Furthermore, regarding functional health specifically, older men may derive greater benefit from more social ties (above and beyond spousal support) than older women (Unger, McAvay, Bruce, Berkman, & Seeman, 1999). Thus, while older women tend to have larger and more diverse social networks (Fischer & Beresford, 2014), current research suggests that men acquire more health benefits from social relationships, particularly from their partners.
Linking Social Relationships to Recovery from Mobility Limitation
Compared with other functional health outcomes, social relationships may be equally or even more important for recovery from mobility limitation, defined as the (in)ability to move about independently in one’s environment, and a critical link in the pathway to onset of disability in tasks essential to independent living (Fried, Bandeen-Roche, Chaves, & Johnson, 2000). For example, emotional social support may become more relevant as a stress buffer during a health shock resulting in a loss of mobility. Social participation may also become more relevant due to the benefits to mobility afforded by the increased physical activity associated with engagement.
In order to capture multiple aspects of social relationships, we identified variables that approximate familial social network, instrumental social support, neighborhood engagement and embeddedness, and community engagement. The familial social network describes the availability of family members including whether an individual is partnered, has adult living children, living siblings, or relatives living nearby. Family members are a critical source of instrumental support, so the composition of one’s familial social network may be significant for older adults’ ability to recover from mobility limitation. While receiving instrumental support has potential health benefits, it may also lead to poorer functional health because those who receive assistance may become overly dependent on caregivers and lose the ability to independently carry out daily activities (Mendes de Leon, Gold, Glass, Kaplan, & George, 2001).
The familial social network measures test whether the presence of family members shape recovery outcomes; however, we also use two specific measures of instrumental support (i.e., receiving financial support from family and giving unpaid help) to explore whether giving or receiving impacts recovery outcomes. Financial instrumental support may be associated with recovery from mobility limitations since those receiving instrumental support may have more resources to modify their environment or manage their underlying condition. Alternatively, receiving financial support may cause distress due to negative emotions associated with receiving support versus giving support (see Liang, Krause, & Bennett, 2001). Providing instrumental support may also influence recovery because it is associated with positive emotions and increased confidence (e.g., self-efficacy) (Brown, Nesse, Vinokur, & Smith, 2003).
Neighborhood engagement and embeddedness refers to whether a person visits (engagement) or feels close to (embeddedness) their neighbors. Neighborhood engagement is indicative of an individual being active and involved within their neighborhood, while neighborhood embeddedness is indicative of social connectedness. Finally, community engagement (i.e., volunteering) may also signify involvement. Frequent contact with neighbors is associated with a greater sense of community and individual well-being (Farrell, Aubry, & Coulombe, 2004), which positively influences health. Despite having a mobility limitation individuals who are involved in their neighborhoods and communities may experience better functional health outcomes because their involvement encourages physical activity outside of the home. Simonsick, Guralnik, Volpato, Balfour, and Fried (2005) emphasize the importance of just getting “out the door” for older women’s functional health status; the authors observed protective effects from regular walking among functionally impaired older women. Among older adults who are socially engaged, not only they are encouraged to leave their homes thus contributing to positive mobility, they may also benefit from the resources associated with being embedded in their neighborhoods and communities such as emotional, informational, and instrumental social support. To illustrate, Pilkington, Windsor, and Crisp (2012) found that higher reports of positive subjective well-being among older individuals who volunteer, is related to more extensive social networks.
Taken together, the extant literature reveals the potential for social relationships to positively influence functional health outcomes including recovery. However, not all facets of social relationships may be positive such as receiving instrumental support. Additionally, the social networks of older adults are often gendered and the health benefits from positive social relationships appears to vary by gender with men experiencing greater health advantages from being partnered (and generally having more social ties (see Unger et al., 1999)). Much of the previous research exploring recovery from functional impairment does not address the importance of friends and neighbors and neglects gender differences in social relationships. This research attempts to address these gaps by examining recovery from severe mobility limitation using data from a nationally representative sample of older Americans. We utilize multiple measures of social relationships from a variety of sources and investigate whether social relationships and recovery is moderated by gender.
Methods
Data
Data for this research come from the Health and Retirement Study (HRS) (1998–2008), an ongoing, nationally representative, panel study of an American cohort born in 1931–1941. The HRS is sponsored by the National Institute of Aging (grant number NIA U01AG009740) and is conducted by the Institute for Social Research at the University of Michigan (HRS, 2011). At baseline (1992), face-to-face interviews were conducted for HRS respondents and their spouses regardless of the spouses’ age. Follow-up interviews have been conducted via telephone every 2 years since baseline. In 1998, the HRS merged with another on-going survey, the Asset and Health Dynamics among the Oldest Old (AHEAD), which consisted of respondents born in 1923 or before. Additionally, two more cohorts were added in 1998, the War Baby (WB) cohort (born 1942–1947) and the Children of the Great Depression (CODA) (born 1924–1930). The sample size, in 1998, including all four cohorts (and respondent spouses) was 21,384 (HRS, 2011). The HRS employs a multi-stage, clustered probability frame and oversamples Blacks/African Americans (1.86:1), Hispanics/Latino (1.72:1), and Florida residents (2:1) (HRS, 2011). The 1998 response rate was 88.3%, and the response rate for subsequent waves ranged from 87.6% to 88.9% for all cohorts (HRS, 2011).
Analyses are based on the RAND HRS Data file (version L), a user-friendly, longitudinal data set created from original HRS data by the National Institute on Aging and the Social Security Administration (RAND, 2011). The RAND data file maximizes cross-wave concordance of variables to facilitate longitudinal analyses, including the careful imputation of missing data (RAND, 2011). The sample (N = 20,244) for this study includes all respondents and spouses who were over the age of 50 years in 1998 with valid data for the mobility and social relationship measures (approximately 6% of the sample was omitted due to missing data on these indicators). We follow these respondents to 2008 using event history analysis to examine the factors influencing recovery from mobility limitations across each 2-year interval.
Measures
Dependent variables
Severe mobility limitation
Recovery from severe mobility limitation was measured using self-reports of walking difficulty. There are three measures of difficulty walking available in the HRS which reflect varying distances and levels of strain: (a) difficulty walking several blocks; (b) difficulty walking one block; (c) difficulty walking across the room. These measures can be conceptualized as hierarchal indicators of mobility limitation, where difficulty walking shorter distances is indicative of greater walking impairment. Respondents were considered to have severe mobility limitation if they reported difficulty walking across the room or one block. We conceptualized recovery from severe mobility limitation as either complete recovery (i.e., reporting no difficulty with any walking distance the subsequent wave) or partial recovery (i.e., reporting only difficulty walking several blocks the subsequent wave).
Risk group
The risk group for these analyses was respondents with severe mobility limitation. Because of the dynamic nature of mobility limitation onset and recovery, the risk group was refreshed at the beginning of each interval (i.e., 2-year period). In 1998, the at-risk sample included 2,722 respondents. The subsequent at-risk samples from 2000 to 2008 ranged from 2,321 to 2,515 respondents.
Outcome variables
The analytic strategy for this research utilized event history analysis with multiple competing events. The outcome variables of interest were: (a) complete recovery from severe mobility limitation and (b) partial recovery from severe mobility limitation. In addition to the two recovery outcome variables, mortality and attrition (i.e., lost to follow-up) were included as competing outcomes. The findings for these outcomes are not presented, but are available from the authors upon request. Persistent severe mobility limitation was the reference outcome variable; all outcome variables were compared with persistent severe mobility limitation.
Independent variables
Social relationships
Social relationships were the independent variables of interest. We attempted to include as many domains of social relationships as possible using the measures available in the HRS from 1998 to 2008. All measures of social relationships were treated as time-varying. As a group, the social relationship measures represent familial social network, engagement and embeddedness, and instrumental support. Familial social network was comprised of four measures: (a) partnered status, (b) number of living children, (c) number of living siblings, and (d) relatives residing nearby. A dichotomous measure of married/partnered status was created, where partnered = 1. The number of living children and living siblings were treated as continuous measures. Respondents who reported having relatives living in the neighborhood were considered to have relatives residing nearby (=1).
Neighborhood engagement and embeddedness as well as community engagement were included in the analyses. Neighborhood engagement was constructed from one question: “How often do you get together with any of your neighbors just to chat or for a social visit?” Likewise, neighborhood embeddedness was constructed from one question: “Do you have any good friends living in your neighborhood?” Because of concordance issues, the neighborhood engagement measure was collapsed into a dichotomous variable, where any visitation with neighbors = 1 (engaged). Similarly, the neighborhood embeddedness was coded dichotomously, where having good friends in the neighborhood = 1 (embedded). Whether a respondent volunteered was employed as a community engagement measure, and a dichotomous variable (yes = 1) was created from: “Have you spent any time in the past 12 months doing volunteer work for religious, educational, health-related or other charitable organizations?”
Two measures of instrumental support were created from two questions, which reflect given and received instrumental support. A dichotomous measure of given social support (yes = 1) was created from the item: “Have you spent any time in the past 12 months helping friends, neighbors, or relatives who did not live with you and did not pay you for the help?” Similarly, a dichotomous measure of received social support (yes = 1) was created from: “Did you [or your husband/wife/partner] receive financial help totaling $500 or more in the last 2 years from friends or relatives?” Unfortunately, the given and received measures do not assess the same form of instrumental support. There was not a comparable measure of financial support across all waves to use for given instrumental support and vice versa for the helping measure.
Sociodemographic characteristics
Sociodemographic characteristics and health risk factors were included in the analyses as control variables. Time-fixed measures included gender, race/ethnicity, educational attainment, and age groups at baseline (i.e., relative age within sample), while income and proxy status were treated as time-varying. A dichotomous dummy variable was created for gender, where female = 1. Three dummy variables capture race/ethnicity comparing White (reference), with Black/African American, Latino/Hispanic, and Other Race. A three category measure of education was created based on credential achievement: less than high school (i.e., respondents without a high school diploma or equivalent), high school (i.e., respondents with a high school diploma or equivalent) (reference), and more than high school (i.e., respondents with an Associate degree or higher). Age (in years) was assessed at baseline (1998), and then a categorical measure was created, where 51–59 years (reference), 60–69 years, 70–79 years, and 80+ years were the age categories. Household income was measured using quartiles with the bottom quartile (i.e., the modal category) used as the reference. Quartiles were created for each wave using the full sample (respondents 51 years or older in 1998). Additionally, a dichotomous indicator of whether proxy interviews were used was created, where yes = 1.
Health risk factors
All health risk factors were treated as time-varying and included measures of health behaviors, healthcare access, and healthcare utilization. Two health behaviors were included in the analysis: smoking status and body mass index (BMI). Smoking status was measured as a three-category variable with never smoked, former smoker, and current smoker as the categories. A categorical measure of BMI was constructed from self-reported weight and height measures (height in meters/weight in kilograms squared); the categories were based established guidelines (CDC, 2011) and included underweight (BMI below 18.5), healthy weight (normal) (BMI = 18.5–24.9), overweight (BMI = 25–29.9), and obese (BMI above 30).
A trichotomous measure for health insurance was created, where respondents with either individual or spousal private insurance, government insurance, or no insurance coverage were the categories. Health insurance coverage was measured as a time-varying variable. Healthcare utilization included doctor visits, hospitalizations, outpatient surgery, regularly taking medication, and nursing home stays. All healthcare utilization measures were asked about the past 2 years. A dichotomous measure was created for each healthcare utilization indicator, where utilization in the past 2 years = 1.
Morbidity status
Two measures were employed to assess morbidity status including the number of chronic conditions and self-rated health. A count of chronic conditions (i.e., arthritis, cancer, diabetes, heart problems, high blood pressure, lung disease, stroke, and psychiatric problems) was used. The chronic conditions were based on physician-diagnosed self-reports. Self-rated health was measured continuously on a five-point Likert scale with 1 = poor health and 5 = excellent health.
Analytic Strategy
To assess the effect of social relationships on recovery outcomes, we employed discrete-time event history analysis with multiple competing events, which was estimated using multinomial logistic regression. This approach is also called the multinomial logit model of competing events/risks. Our models do not assume a particular shape of the hazard function but do assume that the effects of the covariates on the hazard function are the same across all time points. Our modeling strategy is a type of survival analysis characterized by its handling of time as a discrete variable (e.g., with indicators of time intervals included in the model) rather than as a continuous variable with a specified time hazard function (e.g., Weibull).
With six waves of data collected biennially, we have up to five 2-year intervals for each respondent. The risk group at the beginning of each interval included respondents with severe mobility limitation, and possible outcomes at 2-year follow-up included: severe mobility limitation (persistent) (reference), complete recovery, partial recovery, death, and attrition. Although death and attrition are explicitly modeled as a competing event, they are not the focus of this analysis; therefore, the results are not presented. Because respondents could contribute multiple observations over the observation period (i.e., repeated events), which increases the sample size and potentially deflates standard errors, we employed robust standard errors to adjust for clustering within persons (see Allison, 2010 for an overview). Log odds and odds ratio estimates were ascertained for each independent variable. The analyses were left unweighted because many of the attributes (e.g., gender, race/ethnicity, and marital status) for which the weights are calculated are included in the analysis and prior research has suggested that unweighted HRS data is less biased (Botoseneanu & Liang, 2011; Winship & Radbill, 1994). However, our analyses using weighted data (not shown) yielded a similar pattern of results.
Because this research was interested in the specific association between social relationships and recovery from severe mobility limitation numerous controls were employed. Controlling for sociodemographic characteristics, health risk factors, and morbidity status gives increased confidence that any positive effect of social relationships is attributable to the mechanisms associated with social relationships and health and not selection based on socioeconomic status (SES) and health. Additionally, because prior literature has suggested that men and women have differing social relationships in older ages, we tested gender and social relationship interactions for each social relationship measure (only significant interactions at an alpha level of less than 0.05 are presented).
Results
Descriptive Statistics
Table 1 displays the descriptive statistics the initial risk group (i.e., sample respondents with severe mobility limitation in 1998) by gender. Nearly two-thirds of the total sample was women. Among the social relationship variables, relative to men, fewer women were partnered and engaged at baseline. Additionally, women received more instrumental support in the form of financial assistance and gave less instrumental support in the form of unpaid help. In prior research, older women are often described as being more engaged and having more social ties; however, in our initial risk group of older adults with severe mobility limitation, it is men who appear to have more engagement within the neighborhood. Furthermore, women in the initial risk group were older and poorer than men. In general, comparing the total sample with the original sample of all respondents over the age of 50 in 1998 (not shown), the initial risk group was comprised of respondents with fewer social relationships, lower SES, more healthcare utilization, and poorer morbidity status.
Table 1.
Comparison of Descriptive Statistics by Gender for Initial Risk Groupa in 1998
| Distributional informationb | Total sample (N = 2,722) | Women (N = 1,787) | Men (N = 935) |
|---|---|---|---|
| Social relationships | |||
| Familial social network | |||
| Partnered (yes = 1) | 48.2% | 38.0% | 67.6% |
| Number of living children | 3.2 (2.5) | 3.1 (2.5) | 3.3 (2.4) |
| Number of living siblings | 2.3 (2.4) | 2.3 (2.4) | 2.2 (2.4) |
| Relatives residing nearby | 34.1% | 34.7% | 32.9% |
| Neighborhood engagement and embeddedness | |||
| Engaged (yes = 1) | 70.2% | 68.4% | 73.6% |
| Embedded (yes = 1) | 63.6% | 62.5% | 65.8% |
| Community engagement (yes = 1) | 12.8% | 13.2% | 12.2% |
| Instrumental support | |||
| Received (financial) | 2.0% | 2.4% | 1.2% |
| Given (unpaid help) | 30.0% | 28.0% | 33.9% |
| Sociodemographic characteristics | |||
| Gender (female = 1) | 65.7% | — | — |
| Race/ethnicity | |||
| White | 72.1% | 71.1% | 74.0% |
| Black | 18.4% | 19.4% | 16.5% |
| Latino/Hispanic | 7.6% | 7.8% | 7.3% |
| Other Race | 1.9% | 1.7% | 2.2% |
| Baseline age groups | |||
| 51–59 years (ref.) | 16.3% | 16.8% | 15.4% |
| 60–69 years | 24.7% | 23.1% | 27.6% |
| 70–79 years | 27.7% | 26.2% | 30.6% |
| 80+ years | 31.3% | 33.9% | 26.4% |
| Education | |||
| Less than high school | 47.8% | 48.0% | 47.5% |
| High school degree/GED | 42.6% | 42.8% | 42.1% |
| More than high school | 9.6% | 9.2% | 10.4% |
| Income quartiles | |||
| Bottom quartile | 48.8% | 55.6% | 35.9% |
| Bottom-middle quartile | 26.5% | 24.0% | 31.3% |
| Upper-middle quartile | 15.6% | 13.2% | 20.2% |
| Upper quartile | 9.1% | 7.3% | 12.5% |
| Proxy interview (yes = 1) | 22.5% | 19.5% | 28.2% |
| Health risk factors | |||
| Health behaviors | |||
| Smoking status | |||
| Never smoked | 39.2% | 49.5% | 19.6% |
| Former smoker | 43.3% | 34.9% | 59.3% |
| Current smoker | 17.5% | 15.6% | 21.1% |
| Body mass index (BMI) | |||
| Underweight | 9.0% | 10.4% | 6.3% |
| Healthy weight | 32.6% | 31.7% | 34.4% |
| Overweight | 30.1% | 26.3% | 37.2% |
| Obese | 28.3% | 31.6% | 22.0% |
| Healthcare access | |||
| Private health insurance | 9.0% | 9.3% | 8.4% |
| Government insurance | 85.1% | 84.7% | 86.0% |
| No health insurance | 5.9% | 6.0% | 5.6% |
| Healthcare utilization | |||
| Doctor’s visit (past 2 years) | 97.0% | 97.7% | 95.6% |
| Hospitalization (past 2 years) | 52.6% | 50.6% | 56.5% |
| Outpatient surgery (past 2 years) | 21.0% | 20.8% | 21.2% |
| Regularly taking R x (past 2 years) | 91.8% | 93.1% | 89.3% |
| Nursing home stay (past 2 years) | 14.5% | 15.6% | 12.3% |
| Morbidity status | |||
| Number of chronic conditions | 2.8 (1.5) | 2.8 (1.4) | 2.8 (1.5) |
| Self-rated health (5 = excellent) | 1.9 (1.0) | 1.9 (1.0) | 1.8 (0.9) |
aInitial risk group = respondents with severe mobility limitation in 1998.
bPercentages shown for categorical variables; mean and (standard deviation) shown for continuous variables.
Bolded items indicate significant (p < .05) distributional differences between women and men.
Discrete-time Event History with Multiple Competing Events Main Effects Models
Table 2 presents findings obtained from multinomial logistic regression analysis for complete recovery and partial recovery versus persistent severe mobility limitation by social relationships, sociodemographic characteristics, health risk factors, and morbidity status. Log odds estimates and odds ratios are presented. The analytic sample consisted of 11,322 person-intervals. To assess goodness-of-fit, a likelihood-ratio statistic was generated comparing the unadjusted model (i.e., social relationships only) to the intercept only model (ΔG 2 = 1,244.287.169, df = 52, two-tailed p < .001) as well as the comparing the fully adjusted model to the unadjusted model (ΔG 2 = 1,099.169, df = 108, two-tailed p < .001). The likelihood-ratio statistics provide strong evidence of overall goodness of fit for both the unadjusted and fully adjusted models. Five observational intervals were generated from six waves of data. Approximately 7% of at-risk respondents experienced transitions from severe to no mobility limitation, our measure of complete recovery, while about 12% of at-risk respondents experienced transitions from severe to mild limitation, which we define as partial recovery. Additionally, 20% of at-risk respondents died and approximately 9% attrited during the observational period.
Table 2.
Log Odds Parameter and Odds Ratio Estimates (95% Confidence Intervals) of Severe Mobility Limitation Recovery, by Social Relationships, Sociodemographic Characteristics, Health Risk Factors, Morbidity Status, and Time (N = 11,322 person-intervals)
| Complete recovery versus persistent severe mobility limitation | Partial recovery versus persistent severe mobility limitation | |||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||
| Log odds | Odds ratios | log odds | Odds ratios | Log odds | Odds ratios | Log odds | Odds ratios | |
| Social relationships | ||||||||
| Familial social network | ||||||||
| Partnered (yes = 1) | 0.468*** | 1.60 (1.35–1.89) | 0.041 | 1.04 (0.84–1.30) | 0.209** | 1.23 (1.08–1.40) | −0.071 | 0.93 (0.79–1.10) |
| Number of living children | 0.021 | 1.02 (0.99–1.06) | 0.028 | 1.03 (0.99–1.07) | 0.021 | 1.02 (1.00–1.05) | 0.021 | 1.02 (0.99–1.05) |
| Number of living siblings | 0.055*** | 1.06 (1.02–1.09) | 0.027 | 1.03 (0.99–1.07) | 0.027* | 1.03 (1.00–1.06) | 0.008 | 1.01 (0.98–1.04) |
| Relatives residing nearby | −0.316*** | 0.73 (0.61–0.87) | −0.219* | 0.80 (0.67–0.96) | −0.031 | 0.97 (0.85–1.10) | 0.014 | 1.01 (0.89–1.16) |
| Neighborhood engagement and embeddedness | ||||||||
| Engaged (yes = 1) | 0.123 | 1.13 (0.93–1.37) | 0.106 | 1.11 (0.91–1.36) | 0.193* | 1.21 (1.04–1.41) | 0.181* | 1.20 (1.03–1.40) |
| Embedded (yes = 1) | −0.095 | 0.91 (0.76–1.10) | −0.104 | 0.90 (0.74–1.10) | 0.120 | 1.13 (0.98–1.31) | 0.094 | 1.10 (0.95–1.28) |
| Community engagement (yes = 1) | 0.313** | 1.37 (1.11–1.68) | 0.068 | 1.06 (0.85–1.32) | 0.204* | 1.23 (1.11–1.68) | 0.095 | 1.10 (0.92–1.31) |
| Instrumental support | ||||||||
| Received (financial) | −0.001 | 0.99 (0.59–1.66) | 0.009 | 1.01 (0.58–1.74) | −0.417 | 0.66 (0.41–1.05) | −0.397 | 0.67 (0.42–1.08) |
| Given (unpaid help) | 0.639*** | 1.89 (1.60–2.25) | 0.368*** | 1.45 (1.20–1.73) | 0.468*** | 1.60 (1.39–1.83) | 0.295*** | 1.34 (1.16–1.55) |
| Sociodemographic characteristics | ||||||||
| Gendera (female = 1) | −0.262** | 0.77 (0.63–0.94) | −0.183* | 0.83 (0.72–0.97) | ||||
| Race/ethnicitya | ||||||||
| White (ref.) | ||||||||
| Black | 0.283* | 1.33 (1.05–1.69) | 0.026 | 1.03 (0.85–1.24) | ||||
| Latino/Hispanic | 0.611*** | 1.84 (1.34–2.53) | 0.451*** | 1.57 (1.24–1.99) | ||||
| Other race | 0.218 | 1.24 (0.68–2.28) | 0.319 | 1.38 (0.87–2.18) | ||||
| Baseline age groupsa | ||||||||
| 51–59 years (ref.) | ||||||||
| 60–69 years | 0.005 | 1.01 (0.79–1.29) | 0.098 | 1.10 (0.91–1.34) | ||||
| 70–79 years | −0.286 | 0.75 (0.56–1.00) | −0.035 | 0.97 (0.77–1.21) | ||||
| 80+ years | −0.911*** | 0.40 (0.27–0.59) | −0.396** | 0.67 (0.51–0.89) | ||||
| Educationa | ||||||||
| Less than high school | 0.037 | 1.04 (0.85–1.27) | −0.078 | 0.93 (0.79–1.08) | ||||
| High school degree/GED (ref.) | ||||||||
| More than high school | −0.064 | 0.94 (0.72–1.23) | −0.160 | 0.85 (0.69–1.06) | ||||
| Income quartiles | ||||||||
| Bottom quartile (ref.) | ||||||||
| Bottom-middle quartile | 0.137 | 1.15 0.91–1.45) | 0.192* | 1.21 (1.02–1.44) | ||||
| Upper-middle quartile | 0.098 | 1.10 (0.84–1.44) | 0.083 | 1.09 (0.89–1.34) | ||||
| Upper quartile | 0.473** | 1.61 (1.17–2.20) | 0.248 | 1.28 (0.99–1.66) | ||||
| Proxy interview (yes = 1) | −0.370* | 0.69 (0.51–0.93) | −0.413*** | 0.66 (0.53–0.82) | ||||
| Health risk factors | ||||||||
| Health behaviors | ||||||||
| Smoking status | ||||||||
| Never smoked (ref.) | ||||||||
| Former smoker | −0.176 | 0.84 (0.69–1.02) | −0.113 | 0.89 (0.77–1.04) | ||||
| Current smoker | −0.597*** | 0.55 (0.42–0.73) | −0.203 | 0.82 (0.66–1.01) | ||||
| Body mass index (BMI): | ||||||||
| Underweight | −0.774** | 0.46 (0.27–0.79) | −0.519** | 0.60 (0.42–0.85) | ||||
| Healthy weight (ref.) | ||||||||
| Overweight | −0.181 | 0.83 (0.67–1.04) | −0.092 | 0.91 (0.77–1.08) | ||||
| Obese | −0.591*** | 0.55 (0.44–0.70) | −0.283** | 0.75 (0.63–0.90) | ||||
| Healthcare access | ||||||||
| Private health insurance (ref.) | ||||||||
| Government insurance | −0.826*** | 0.44 (0.33–0.58) | −0.555*** | 0.57 (0.45–0.73) | ||||
| No health insurance | −0.124 | 0.88 (0.60–1.30) | −0.045 | 0.96 (0.68–1.35) | ||||
| Healthcare utilization | ||||||||
| Doctor’s visit (past 2 years) | −0.342 | 0.71 (0.46–1.10) | 0.182 | 1.20 (0.80–1.80) | ||||
| Hospitalization (past 2 years) | −0.047 | 0.95 (0.80–1.13) | −0.023 | 0.98 (0.86–1.11) | ||||
| Outpatient surgery (past 2 years) | 0.231* | 1.26 (1.05–1.52) | −0.011 | 1.01 (0.87–1.17) | ||||
| Regularly taking Rx (past 2 years) | −0.112 | 0.89 (0.65–1.24) | −0.060 | 0.94 (0.71–1.26) | ||||
| Nursing home stay (past 2 years) | −0.694*** | 0.50 (0.33–0.75) | −0.740*** | 0.48 (0.36–0.63) | ||||
| Morbidity status | ||||||||
| Number of chronic conditions | −0.256*** | 0.77 (0.72–0.83) | −0.084** | 0.92 (0.87–0.97) | ||||
| Self-rated health (5 = excellent) | 0.408*** | 1.50 (1.38–1.64) | 0.191*** | 1.21 (1.13–1.30) | ||||
| Observation intervals | ||||||||
| Interval 1 (ref.) | ||||||||
| Interval 2 | −0.066 | −0.121 | −0.063 | −0.077 | ||||
| Interval 3 | −0.235* | −0.219 | 0.064 | 0.091 | ||||
| Interval 4 | −0.304* | −0.273* | −0.068 | −0.055 | ||||
| Interval 5 | −0.165 | −0.105 | −0.082 | −0.067 | ||||
| Intercept | −2.515*** | −0.560 | −2.014*** | −1.133*** | ||||
| −2LogLikelihood | 27,956.569 | 26,857.400 | 27,956.569 | 26,857.400 | ||||
| Degrees of freedom | 52 | 160 | 52 | 160 | ||||
aTime-fixed measures.
*p ≤ .05. **p ≤ .01. ***p ≤ .001.
Complete Recovery Versus Persistent Severe Mobility Limitation
In Model 1, social relationships were included in the analysis without controls; therefore, Model 1 represents the unadjusted risk of recovery by social relationships. Several measures of social relationships were significantly associated with complete recovery (see Table 2, left panel). In the unadjusted model, partnered respondents (odds ratio (OR) =1.60) were more likely to experience complete recovery than single respondents. Having more living siblings (OR = 1.06) was associated with greater unadjusted odds of complete recovery. Respondents living near relatives (OR = 0.73) had lower unadjusted odds of complete recovery. Community engagement (OR = 1.37) and giving instrumental support (OR = 1.89) were both associated with greater unadjusted odds of complete recovery.
After fully adjusting for sociodemographic characteristic, health risk factors, and morbidity status (Model 2), partnered status, number of siblings, and community engagement were no longer associated with complete recovery. However, having relatives residing nearby (OR = 0.80) remained significantly associated with lower odds of complete recovery. Similarly, giving instrumental social support (OR = 1.45) continued to be linked to greater odds of complete recovery. Among sociodemographic characteristics, gender, race/ethnicity, age, and income were associated with complete recovery. Women (OR = 0.77) had lower odds of complete recovery, relative to men. Compared with Whites, Black (OR = 1.33), and Latino/Hispanic (OR = 1.84) respondents were more likely to experience complete recovery. Older ages were negatively associated with complete recovery with the oldest age group (i.e., 80+ years at baseline) having a 60% reduction in the odds of recovery compared with the youngest age group. Higher household incomes were associated with greater odds of recovery. More specifically, being in the upper income quartile (OR = 1.61), compared with the bottom quartile, was associated with increased odds of complete recovery. Additionally, respondents with proxy interviews (OR = 0.69) had lower odds of complete recovery.
Many health risk factors were significantly associated with complete recovery. Current smokers (OR = 0.55) as well as underweight (OR = 0.46) and obese (OR = 0.55) respondents were less likely to experience complete recovery from severe mobility limitation. Government health insurance (OR = 0.44), relative to private health insurance, was also linked to lower odds of recovery. Nursing home stays (0.50) was associated with diminished odds of complete recovery, whereas outpatient surgery (OR = 1.26) was associated with increased odds. Additionally, more chronic conditions (OR = 0.77) were associated with lower odds of recovery, while better ratings of self-rated health (OR = 1.50) were associated with greater odds.
Partial Recovery versus Persistent Severe Mobility Limitation
In the right panel of Table 2, the unadjusted model (Model 1) indicated that several social relationships measures were significantly associated with partial recovery including partner status, the number of living siblings, neighborhood engagement, community engagement, and giving instrumental support. Being partnered (OR = 1.23) and having more siblings (OR = 1.03) were associated with greater odds of partial recovery. Being engaged, whether in the neighborhood (OR = 1.21) or community (OR = 1.23), was positively associated with partial recovery from severe mobility limitations. Giving instrumental support (OR = 1.60) was also linked to improved odds of partial recovery.
In the fully adjusted model (Model 2), neighborhood engagement (OR = 1.20) and giving instrumental support (OR = 1.34) remained significant predictors of partial recovery. Among the sociodemographic characteristics, gender, race/ethnicity, age, and household income were linked to partial recovery. Women (OR = 0.83) were less likely to experience partial recovery relative to men. Latino/Hispanic (OR = 1.57) respondents were more likely to recover compared with White respondents. Compared with the youngest age group, the oldest age (i.e., 80+ years at baseline) (OR = 0.67) group had lower odds of partial recovery. Being in the bottom-middle income quartile (OR = 1.21) relative to the bottom quartile was also linked to greater odds of partial recovery. Respondents with proxy interviews (OR = 0.66) had reduced odds of partial recovery. Among health risk factors, underweight (OR = 0.60) and obese (OR = 0.75) respondents were less likely experience partial recovery. Having government insurance (OR = 0.57), compared with private insurance, was linked to lower odds of recovery. Nursing home stays (OR = 0.48) were also negatively associated with partial recovery. Both morbidity measures were significantly associated with partial recovery. Having more chronic conditions (OR = 0.92) was negatively associated with partial recovery, whereas better self-rated health (OR = 1.21) was positively associated with partial recovery.
Gender Interaction Effects
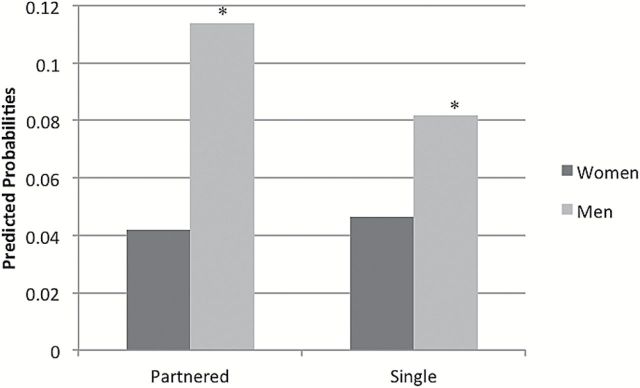
Figures 1–3 present the predicted probabilities for the significant (p < .05) gender and social relationship interactions for complete and partial recovery. Predicted probabilities were generated based on the interaction effects models. The interaction effects models are available online (see Supplementary Table 1). Figure 1 illustrates the predicted probabilities of complete recovery by gender and partner status. Compared with partnered women, partnered men were more likely to experience complete recovery. Partnered men had nearly three times greater predicted probability of complete recovery relative to partnered women. Additionally, single men were more likely to experience complete recovery relative to single women.
Figure 1.
Predicted probabilities of complete recovery by gender and partner status.
Figure 3.
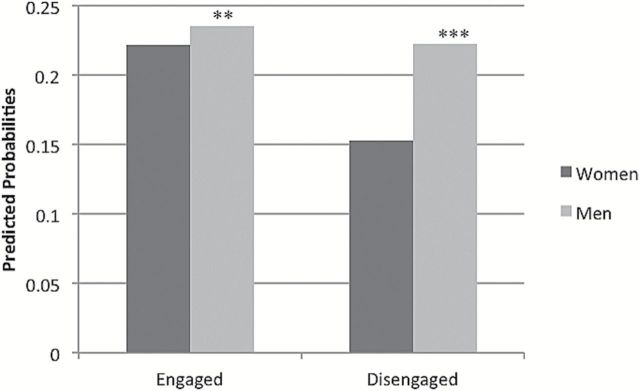
Predicted probabilities of partial recovery by gender and neighborhood engagement status.
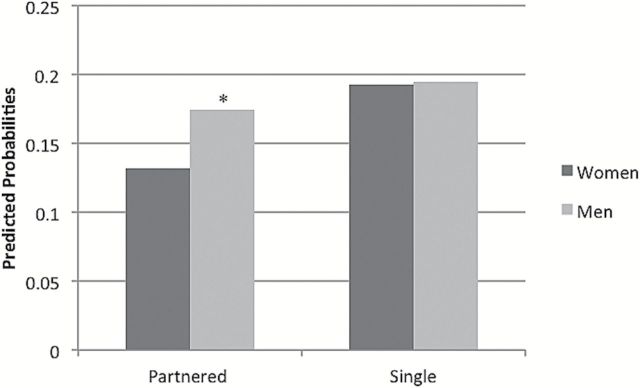
Similar to complete recovery, the interaction between gender and partner status was significant. Figure 2 illustrates the predicted probabilities for partial recovery by gender and partner status. Again, partnered men were more likely to experience partial recovery relative to partnered women. Finally, an interaction between gender and neighborhood engagement was modeled. The interaction was significant, and the predicted probabilities (Figure 3) demonstrate gender differences by neighborhood engagement for partial recovery. Engaged men were more likely to experience partial recovery compared with engaged women. Additionally, disengaged men were more likely to experience partial recovery compared with disengaged women. Notably, disengaged women were the least likely to experience partial recovery compared with any group.
Figure 2.
Predicted probabilities of partial recovery by gender and partner status.
Discussion
Results from the foregoing analysis suggest that social relationships serve as facilitators of recovery from severe mobility limitation, and that the influence of social relationships varies by outcome and recovery type. For complete recovery, giving instrumental support was one of the most robust social relationship predictors. Net of sociodemographic characteristics, health risk factors, and morbidity status, respondents who gave instrumental support had about a 45% increase in the odds of complete recovery in the next 2-year period. Another robust predictor of complete recovery was whether relatives resided nearby. Respondents living in the same neighborhood as relatives had about a 20% decrease in the odds of complete recovery, controlling for all other risk factors. There were also two robust predictors of partial recovery: neighborhood engagement and giving instrumental support. Both social relationship measures were positively associated with partial recovery. Engaged respondents, relative to disengaged respondents, had approximately a 20% increase in the odds of partial recovery, whereas respondents who had given instrumental support had approximately a 34% increase in the odds of partial recovery.
We also explored whether there were any gendered interactions among social relationships and recovery. For both complete and partial recovery, partner status was moderated by gender. In both cases, partnered men were more likely to recover than partnered women. For partial recovery, neighborhood engagement was also moderated by gender, where engaged men were more likely to experience recovery than engaged women. Furthermore, it appeared that disengaged women were the least likely to experience partial recovery.
Giving instrumental support to friends, neighbors, or relatives appears to be valuable for recovery outcomes. Despite having severe mobility limitation, those respondents who helped their friends and family were more likely to experience complete or partial recovery. Prior research suggests that providing social support is more beneficial to health among older adults than receiving social support (Abolfathi Momtaz, Ibrahim, & Hamid, 2014; Brown et al., 2003). Providing support is linked to positive feelings, greater sense of control (self-efficacy), and self-esteem, which positively influences health (Brown et al., 2003; Grant & Dutton, 2012; Warner, Schüz, Wurm, Ziegelmann, & Tesch-Römer, 2010). For example, providing social support lowers levels depressive symptomology among older adults (Krause, Herzog, & Baker, 1992). Additionally, the residual effects of increased feelings of self-efficacy associated with providing instrumental support may spillover to other beneficial health behaviors, which could improve recovery outcomes.
Another positive predictor of recovery was neighborhood engagement. Respondents who reported visiting friends and neighbors were more likely to experience partial recovery. Visiting with neighbors suggests that individuals are leaving their home despite their mobility limitations. Being engaged and active within one’s neighborhood may be an important pathway for partial recovery. Not only do these individuals benefit from the emotional and informational support of companionship, they may also be benefitting from “just getting out the door,” where even small amounts of walking helps maintain mobility (Simonsick et al., 2005). Older adults who are disengaged and more socially isolated are less likely to leave the home, which negatively impacts functional health (Simonsick, Kasper, & Phillips, 1998).
The only social relationship measure to be negatively associated with recovery was having relatives living nearby. While this data cannot explicitly speak to the mechanisms linking family proximity to worse recovery outcomes, it is possible to gain insight from prior research. This association may stem from neighboring relatives providing instrumental support and reducing chances to complete tasks that encourage greater mobility and functional health. Mendes de Leon et al. (2001) observed increased disability risk among individuals who received instrumental support, and attributed this finding to the process of deconditioning, whereby individuals who received assistance with daily activities gradually lose the physical capacity to complete these tasks alone. In addition, Mendes de Leon et al. (2001) suggested that receiving instrumental support could weaken a person’s self-efficacy and generate a sense of dependency upon others. While neighboring relatives may provide important social support opportunities for aging family members with functional impairment, it is possible that an overdependence on assistance from nearby family members could arise and have negative consequences for functional health and recovery. An alternative explanation may be that individuals who have families who reside in close proximity have worse health trajectories (prognoses); however, given the numerous health and morbidity controls, we contend that deconditioning may be a more fitting interpretation of these results. Nevertheless, it is possible that both explanations contribute to this finding.
These findings also highlight important gender differences among social relationships in relation to mobility limitation recovery. In general, partnered men were more likely to experience recovery than partnered women. Previous research has noted that marriage/partnership may be more advantageous for men’s health than women’s health (see Kiecolt-Glaser & Newton, 2001). Furthermore, prior research has suggested that older men and women’s sources of support are different with men relying more heavily on their spouse and women relying on multiple sources including friends (Antonucci, 1990; Antonucci & Akiyama, 1987; Umberson, 1992). This research suggests that the health benefits that partnership confers to men may extend to recovery outcomes. Additionally, the positive effect of neighborhood engagement on partial recovery was moderated by gender. In general, it appeared that disengaged women were the most disadvantaged group regarding partial recovery. Disengagement and greater social isolation may be particularly deleterious for older women’s functional health. Because older women tend to have more diverse social networks including a greater reliance on friends, relative to men, a lack of neighborhood engagement among women may have larger implications for recovery from mobility limitation. Previous research suggests that social support from friends is one of the best predictors of physical activity among older women (Harvey &Alexander, 2012); therefore, the absence of neighborhood engagement among older women may be indicative of fewer opportunities for health promoting get-togethers that include exchanges of emotional and information support as well as lower participation in physical activities.
Strengths and Limitations
This study benefitted from the use of repeated measures of function and social relationships collected prospectively over a 10-year period. An additional strength of this research was using measures that represented social relationships from multiple sources such as friends and neighbors. In order to address potential endogeneity in the temporal sequence between social relationships and recovery, we modeled the social relationship measures in all those “at-risk” for recovery at the beginning of each time interval and recovery by the end of each 2-year period. This modeling strategy is advantageous because social relationships were assessed during the period of mobility impairment and then recovery outcomes were assessed 2 years later, which minimizes concerns about reverse causality. Individuals who experience functional health declines often encounter a negative impact on their social relationships; however, our modeling strategy measures current social relationships after functional impairment onset has occurred. A potential limitation with this strategy is that it was possible for respondents to have recovered multiple times, thus contributing to the study multiple observations of recovery; however, only a small proportion (<3%) of respondents who recovered experience multiple recovery episodes. Supplementary analyses were completed omitting respondents with multiple recovery episodes and the substantive findings remained unchanged.
Additionally, our mobility limitation and recovery measures were based on self-reports, which may be subject to reporting error. While performance-based measures of recovery would have been preferred, there is a wealth of research using the HRS self-reported functional health measures, which documents the reliability of these measures. Another limitation stems from restricted social relationship measures. The HRS is superior for longitudinal investigation of health outcomes among older adults; however, we were limited by the social relationship questions available across multiple waves. Finally, it is possible that respondents who maintain certain social relationships despite severe mobility limitation may be unique (e.g., positive affect, extroversion, or high levels of mastery) or have unique social networks (e.g., stable, dense, or resource rich); however, numerous controls were included in the analysis and according to descriptive statistics the majority of the at-risk sample was engaged and embedded. Although this research has key limitations, it still provides evidence that social relationships hold the potential to facilitate recovery from functional impairment.
Conclusion
This research may speak to interventions aimed at promoting mobility and functional health within individuals’ communities. Helping friends and neighbors was a robust predictor of complete and partial recovery. Interventions aimed at encouraging community members with functional impairment to provide instrumental support to peers may improve functional health outcomes. Increased opportunities for proving instrumental support through the use of community services and programs may bolster the health of the provider, recipient, and community at large. To illustrate, peer or mutual support programs have had success for various disease/condition management interventions (Heisler, 2010; Pistrang, Barker, & Humphreys, 2008). Promoting neighborhood engagement despite severe mobility limitation may be another fruitful avenue for targeted interventions. More research is needed to explain variations in the effect of neighborhood engagement on partial recovery by gender; however, this research suggests that disengaged women may be a particularly vulnerable group for worse functional health outcomes. Disengaged women may benefit from directed interventions aimed at functional health promotion.
When considering social relationships and health, the type of social relationship measures and the type of health outcome (e.g., onset vs. recovery) may have differing underlying mechanisms. This research reiterates the complexity surrounding social relationships and health. It is not simply that all social relationships benefit health—most may be positive, but some may be negative and, as this research demonstrates, some social relationship measures may be more important for recovery. We encourage future researchers to examine different and more nuanced measures of social relationships in relation to both functional health declines and recovery. In particular, we recommend future research investigating perceived social support and other measures of social relationships in relation to recovery with the aim to undercover the specific mechanisms linking social relationships to mobility limitation recovery. We also urge researchers and clinicians to develop interventions aimed at facilitating recovery from functional health declines through social relationships.
Supplementary Material
Supplementary material can be found at: http://psychsocgerontology.oxfordjournals.org/
Funding
This research was partially supported by an NIA training grant (T32 AG000221) and NICHD Center Grant (R24 HD041028) from the University of Michigan.
Supplementary Material
Acknowledgments
K. Latham gratefully acknowledges use of the services and facilities of the Population Studies Center, while at the University of Michigan’s Institute for Social Research.
References
- Adams R. G., Blieszner R. (1989). Older adult friendship: Structure and process (Vol. 103). Newbury Park, CA: Sage Publications. [Google Scholar]
- Adams R. G., Blieszner R. (1995). Aging well with friends and family. American Behavioural Scientist, 39, 209–224. [Google Scholar]
- Abolfathi Momtaz, Y., Ibrahim, R., & Hamid, T. A. (2014). The impact of giving support to others on older adults’ perceived health status. Psychogeriatrics, 14, 31–37. [DOI] [PubMed] [Google Scholar]
- Allen S. M., Goldscheider F., Ciambrone D. A. (1999). Gender roles, marital intimacy, and nomination of spouse as primary caregiver. The Gerontologist, 39, 150–158. [DOI] [PubMed] [Google Scholar]
- Allison P. D. (2010). Survival analysis. In G. Hancock, R. O. Mueller. (Eds.), The reviewer’s guide to quantitative methods in the social sciences, (pp. 413–425). New York, NY: Routledge. [Google Scholar]
- Antonucci T. C. (1990). Social supports and social relationships. Handbook of aging and the social sciences, 3, 205–226. [Google Scholar]
- Antonucci T. C., Akiyama H. (1987). An examination of sex differences in social support among older men and women. Sex Roles, 17, 737–749. [Google Scholar]
- Botoseneanu A., Liang J. (2011). Social stratification of body weight trajectory in middle-age and older americans: results from a 14-year longitudinal study. Journal of Aging and Health, 23, 454–480. :10.1177/0898264310385930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A., Farquhar M., Browne P. (1991). Life satisfaction and associations with social network and support variables in three samples of elderly people. International Journal of Geriatric Psychiatry, 6, 549–566. :10.1002/gps.930060803 [Google Scholar]
- Brown S. L., Nesse R. M., Vinokur A. D., Smith D. M. (2003). Providing social support may be more beneficial than receiving it: results from a prospective study of mortality. Psychological Science, 14, 320–327. :10.1111/1467-9280.14461 [DOI] [PubMed] [Google Scholar]
- Cohen S., Underwood L., Gottlieb B. H. (2000). Social support measurement and intervention: A guide for health and social scientists. New York, NY: Oxford University Press. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2011). About BMI for Adults Atlanta, GA: Centers for Disease Control and Prevention; Retrieved http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. [Google Scholar]
- Eng P. M., Rimm E. B., Fitzmaurice G., Kawachi I. (2002). Social ties and change in social ties in relation to subsequent total and cause-specific mortality and coronary heart disease incidence in men. American Journal of Epidemiology, 155, 700–709. :10.1093/aje/155.8.700 [DOI] [PubMed] [Google Scholar]
- England P., McClintock E. A. (2009). The gendered double standard of aging in US marriage markets. Population and Development Review, 35, 797–816. :10.1111/j.1728-4457.2009.00309.x [Google Scholar]
- Farrell S. J., Aubry T., Coulombe D. (2004). Neighborhoods and neighbors: Do they contribute to personal well‐being? Journal of Community Psychology, 32, 9–25. :10.1002/jcop.10082 [Google Scholar]
- Fischer C. S., Beresford L. (2014). Changes in support networks in late middle age: The extension of gender and educational differences. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. :10.1093/geronb/gbu057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried L. P., Bandeen-Roche K., Chaves P. H., Johnson B. A. (2000). Preclinical mobility disability predicts incident mobility disability in older women. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 55, M43–M52. :10.1093/gerona/55.1.M43 [DOI] [PubMed] [Google Scholar]
- Gallant M. P. (2003). The influence of social support on chronic illness self-management: a review and directions for research. Health Education & Behavior: the official publication of the Society for Public Health Education, 30, 170–195. :10.1177/1090198102251030 [DOI] [PubMed] [Google Scholar]
- Gallant M. P., Spitze G. D., Prohaska T. R. (2007). Help or hindrance? How family and friends influence chronic illness self-management among older adults. Research on Aging, 29, 375–409. :10.1177/0164027507303169 [Google Scholar]
- Glass T. A., Maddox G. L. (1992). The quality and quantity of social support: stroke recovery as psycho-social transition. Social Science & Medicine (1982), 34, 1249–1261. :10.1016/0277-9536(92)90317-J [DOI] [PubMed] [Google Scholar]
- Grant A., Dutton J. (2012). Beneficiary or benefactor: are people more prosocial when they reflect on receiving or giving? Psychological Science, 23, 1033–1039. :10.1177/0956797612439424 [DOI] [PubMed] [Google Scholar]
- Griffith J. (1985). Social support providers: Who are they? Where are they met? and the relationship of network characteristics to psychological distress. Basic and Applied Social Psychology, 6, 41–60. :10.1207/s15324834basp0601_4 [Google Scholar]
- Gruenewald T., Seeman T. 2010. Social support and physical health: links and mechanisms. In A. Steptoe, K. E. Freedland. (Eds.), Handbook of behavioral medicine: Medicine and applications (pp. 225–261). New York, NY: Springer. [Google Scholar]
- Harvey I. S., Alexander K. (2012). Perceived social support and preventive health behavioral outcomes among older women. Journal of Cross-Cultural Gerontology, 27, 275–290. :10.1007/s10823-012-9172-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Retirement Study (HRS). (2011). Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, MI. [Google Scholar]
- Heisler M. (2010). Different models to mobilize peer support to improve diabetes self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Family Practice, 27, i23–i32. :10.1093/fampra/cmp003 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- House J. S., Landis K. R., Umberson D. (1988). Social relationships and health. Science (New York, NY), 241, 540. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser J. K., Newton T. L. (2001). Marriage and health: his and hers. Psychological Bulletin, 127, 472–503. :10.1037/0033-2909.127.4.472 [DOI] [PubMed] [Google Scholar]
- Krause N., Herzog A. R., Baker E. (1992). Providing support to others and well-being in later life. Journal of Gerontology, 47, P300–P311. [DOI] [PubMed] [Google Scholar]
- Liang J., Krause N. M., Bennett J. M. (2001). Social exchange and well-being: is giving better than receiving? Psychology and aging, 16, 511–523. :10.1037/0882-7974.16.3.511 [DOI] [PubMed] [Google Scholar]
- Maier H., Klumb P. L. (2005). Social participation and survival at older ages: is the effect driven by activity content or context? European Journal of Ageing, 2, 31–39. :10.1007/s10433-005-0018-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melzer D., Lan T. Y., Guralnik J. M. (2003). The predictive validity for mortality of the index of mobility-related limitation–results from the EPESE study. Age and Ageing, 32, 619–625. :10.1093/ageing/afg107 [DOI] [PubMed] [Google Scholar]
- Mendes de Leon C. F., Gold D. T., Glass T. A., Kaplan L., George L. K. (2001). Disability as a function of social networks and support in elderly African Americans and Whites The Duke EPESE 1986–1992. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56, S179–S190. :10.1093/geronb/56.3.S179 [DOI] [PubMed] [Google Scholar]
- Mendes de Leon C.F., Glass T. A., Beckett L. A., Seeman T. E., Evans D. A., Berkman L. F. (1999). Social networks and disability transitions across eight intervals of yearly data in the New Haven EPESE. The Journals of Gerontology, Social Sciences, 54, S162–S172. 10.1093/geronb/54B.3.S162 [DOI] [PubMed] [Google Scholar]
- Pistrang N., Barker C., Humphreys K. (2008). Mutual help groups for mental health problems: a review of effectiveness studies. American Journal of Community Psychology, 42, 110–121. :10.1007/s10464-008-9181-0 [DOI] [PubMed] [Google Scholar]
- Pilkington P. D., Windsor T. D., Crisp D. A. (2012). Volunteering and subjective well-being in midlife and older adults: the role of supportive social networks. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 249–260. 10.1093/geronb/gbr154 [DOI] [PubMed] [Google Scholar]
- RAND HRS Data, Version K. 2011. Produced by the RAND Center for the Study of Aging, with funding from the National Institute on Aging and the Social Security Administration. Santa Monica, CA. [Google Scholar]
- Seeman T. E., Singer B. H., Ryff C. D., Dienberg Love G., Levy-Storms L. (2002). Social relationships, gender, and allostatic load across two age cohorts. Psychosomatic Medicine, 64, 395–406. [DOI] [PubMed] [Google Scholar]
- Schiøtz, M. L., Bøgelund, M., Almdal, T., Jensen, B. B., & Willaing, I. (2012). Social support and self-management behaviour among patients with Type 2 diabetes. Diabetic Medicine, 29(5), 654–661. 10.1111/j.1464-5491.2011.03485.x [DOI] [PubMed] [Google Scholar]
- Simonsick E. M., Kasper J. D., Phillips C. L. (1998). Physical disability and social interaction: factors associated with low social contact and home confinement in disabled older women (The Women’s Health and Aging Study). The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 53, S209–S217. :10.1093/geronb/53B.4.S209 [DOI] [PubMed] [Google Scholar]
- Simonsick E. M., Guralnik J. M., Volpato S., Balfour J., Fried L. P. (2005). Just get out the door! Importance of walking outside the home for maintaining mobility: findings from the women’s health and aging study. Journal of the American Geriatrics Society, 53, 198–203. :10.1111/j.1532-5415.2005.53103.x [DOI] [PubMed] [Google Scholar]
- Spitze G., Ward R. (2000). Gender, marriage, and expectations for personal care. Research on Aging, 22, 451–469. :10.1177/0164027500225001 [Google Scholar]
- Tsouna-Hadjis E., Vemmos K. N., Zakopoulos N., Stamatelopoulos S. (2000). First-stroke recovery process: the role of family social support. Archives of Physical Medicine and Rehabilitation, 81, 881–887. :10.1053/apmr.2000.4435 [DOI] [PubMed] [Google Scholar]
- Umberson D. (1992). Gender, marital status and the social control of health behavior. Social Science & Medicine (1982), 34, 907–917. :10.1016/0277-9536(92)90259-S [DOI] [PubMed] [Google Scholar]
- Umberson D., Montez J. K. (2010). Social relationships and health: a flashpoint for health policy. Journal of Health and Social Behavior, 51, S54. :10.1177/0022146510383501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger J. B., McAvay G., Bruce M. L., Berkman L., Seeman T. (1999). Variation in the impact of social network characteristics on physical functioning in elderly persons: MacArthur Studies of Successful Aging. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 54, S245–S251. :10.1093/geronb/54B.5.S245 [DOI] [PubMed] [Google Scholar]
- Warner D. F., Kelley-Moore J. (2012). The social context of disablement among older adults: does marital quality matter for loneliness? Journal of health and social behavior, 53, 50–66. :10.1177/0022146512439540 [DOI] [PubMed] [Google Scholar]
- Warner L. M., Schüz B., Wurm S., Ziegelmann J. P., Tesch-Römer C. (2010). Giving and taking–differential effects of providing, receiving and anticipating emotional support on quality of life in adults with multiple illnesses. Journal of Health Psychology, 15, 660–670. :10.1177/1359105310368186 [DOI] [PubMed] [Google Scholar]
- Winship C., Radbill L. (1994). Sampling weights and regression analysis. Sociological Methods & Research, 23, 230–257. :10.1177/0049124194023002004 [Google Scholar]
- Zhang Z., Hayward M. D. (2001). Childlessness and the psychological well-being of older persons. Journal of Gerontology, Social Sciences, 56B, S331–S320. doi:10.1093/geronb/56.5.S311 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.