Abstract
Piriformis muscle syndrome (PMS) is a controversial neuromuscular disorder that is presumed to involve compression neuropathy of the sciatic nerve at the level of the piriformis muscle. Botulinum toxin A (BTX-A) injection into the piriformis muscle is widely used as a treatment aimed at relieving sciatic nerve compression.
In 2 patients with PMS, magnetic resonance neurography (MRN) was taken before and after BTX-A injection. The first MRN was performed as a diagnostic tool, and the second to identify the effect of the treatment. Signal change of the sciatic nerve under the hypertrophied piriformis muscle was confirmed by MRN. In follow-up MRN performed after BTX-A injection into the piriformis muscle, changes of the sciatic nerve and piriformis muscle were noticed as well as improvement of clinical symptoms.
MRN is a useful tool to add certainty of diagnosis and verify the effect of treatment in PMS.
INTRODUCTION
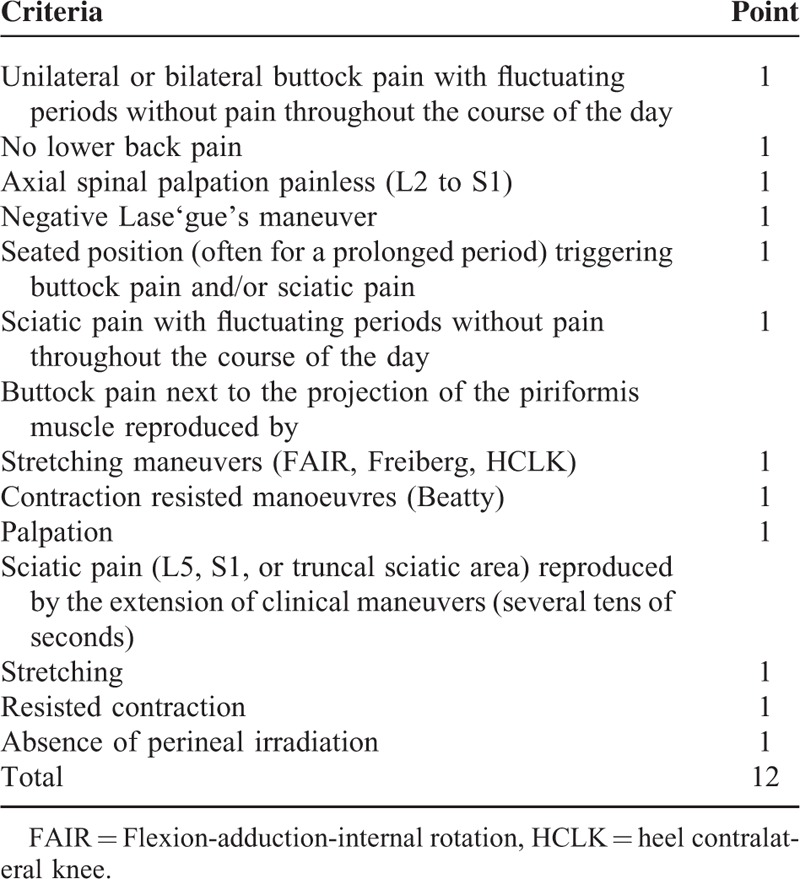
Piriformis muscle syndrome (PMS) can be diagnosed from the patient's history, physical examination, and exclusion of other possible causes,1 but it has been difficult to obtain objective evidence for the syndrome.2 Michel et al proposed a clinical scoring system consisting of clinical symptoms, signs, and several provocation maneuver tests for the diagnosis of PMS (Table 1).3 They suggest using a score of 8 or greater on the scale from 0 to 12 to confirm the diagnosis of PMS. The sensitivity and specificity of the score were 96.4% and 100%, respectively, whereas the positive predictive value was 100% and the negative predictive value 86.9%.
TABLE 1.
Proposal for a Clinical Scoring System for the Diagnosis of Piriformis Muscle Syndrome
Electrophysiological tests and imaging studies add certainty to the diagnosis of PMS.4 The recently introduced neuroradiological technique, magnetic resonance neurography (MRN), is useful for the diagnosis of peripheral neuropathy by directly showing the nerve anatomy.5 MRI performed with higher structural resolution and improved nerve lesion contrast to assess intrinsic nerve disorders was termed MRN by Filler et al in the early 1990s.3,4 Heavily T2-weighted sequences with fat saturation were found to be most advantageous and an increase in the intraneural T2-weighted signal was identified to be a highly sensitive.5,6 MRN has been used to evaluate unexplained chronic sciatica and has led to identification of various changes relating to the piriformis muscle and sciatic nerve.2
For the treatment of PMS, piriformis muscle injection is usually offered as part of multimodal therapy, and ultrasound-guided injection improves the accuracy of injection.4 The response to injections of lidocaine and steroid can be immediate but may be of short duration.6,7 Several randomized, controlled trials demonstrated better efficacy with botulinum toxin type A (BTX-A) over both placebo and corticosteroid plus lidocaine.6–9 BTX-A seems to be a logical treatment choice, because it reverses the presumed underlying pathophysiology of PMS by leading to muscle weakness, atrophy, and relief of sciatic nerve compression.8 Here we describe 2 cases of sciatic nerve signal change under the hypertrophied piriformis muscle confirmed by MRN and the change in imaging findings after BTX-A injection to the piriformis muscle.
CASE REPORTS
CASE 1
A 58-year-old man with no particular medical history except hypertension visited the hospital with a complaint of severe left buttock pain and tingling sensations in the left lower extremity. The symptoms had developed about 2 months prior and had worsened progressively. A week before visiting the hospital, he had undergone a left fourth lumbar partial hemilaminectomy based on a diagnostic impression of lumbar radiculopathy in other clinic, but the pain and numbness were not improved. The symptoms worsened, and when the patient visited the hospital, he could not sit at all due to buttock pain and could only walk 4 to 5 m with minimal assistance of another person. The pain was aggravated by sitting and standing, with a visual analogue scale (VAS) score of 8. During the physical examination, there was no weakness of the bilateral lower extremities, but the straight leg-raising test (SLRT) showed 40 degrees of limitation on the left side. Patrick sign and Lasègue sign were negative.
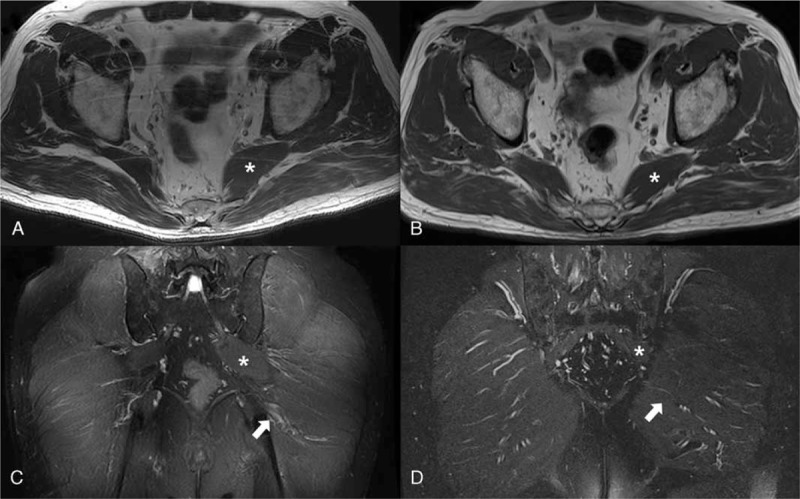
The clinical scoring system for the diagnosis of PMS yielded a score of 10.3 Severe local tenderness was detected at the left piriformis muscle area, and hypesthesia was reported on the posterolateral aspect of the left thigh. There was no history of blunt trauma, but through detailed history-taking we learned that the patient usually put his wallet in the left rear pocket of his pants. The left tibial H-reflex showed a 1.86 ms prolongation on flexion, adduction, and internal rotation (FAIR) test (Table 2). A pelvic MRN was performed at ∼ 2 months after the symptom onset. Hypertrophy of the left piriformis muscle compared with the right side and swelling of the left sciatic nerve with bright signal intensity were observed (Fig. 1). With MRN findings, PMS was diagnosed more conclusively. Hypertrophied piriformis muscle was targeted for treatment. BTX-A (Botox®) 100 unit was injected into the left piriformis muscle under ultrasound guidance. The lowest dose with proven therapeutic effect in previous studies was selected to minimize the possible complication.8 A 4-ml injection containing 100 unit of BTX-A in preserve-free normal saline was administrated via the peppering technique. The patient was tolerable through the procedure, and there was no adverse or unanticipated event. Ethical approval was not necessary since the procedure was performed for therapeutic purpose and the clinical effect of procedure has already been proven. Three days later, the patient could sit down, and the SLRT was improved to 70 degrees. Seven days after the injection, the patient could sit for >30 min and walk independently 300 to 400 m without pain; additionally, the SLRT was improved to 80 degrees. Pain was decreased to VAS 3, and the prolongation of the H-reflex in the FAIR position was improved to 1.05 ms in the follow-up study performed 1 month after the injection (Table 2). Follow-up pelvic MRN taken 1 month after the BTX-A injection, when compared with the diagnostic MRN, indicated equivocal decrease of left piriformis muscle volume and significant decrease of left sciatic nerve swelling (Figs. 1 and 2). At the 6th month follow-up after the treatment, the VAS score was 4. The pain gradually exacerbated and by the 9th month after the treatment, the VAS score was 5 but the patient did not need repeat injection since the improved functional status was maintained.
TABLE 2.
Change in H-reflex Values Before and After Treatment
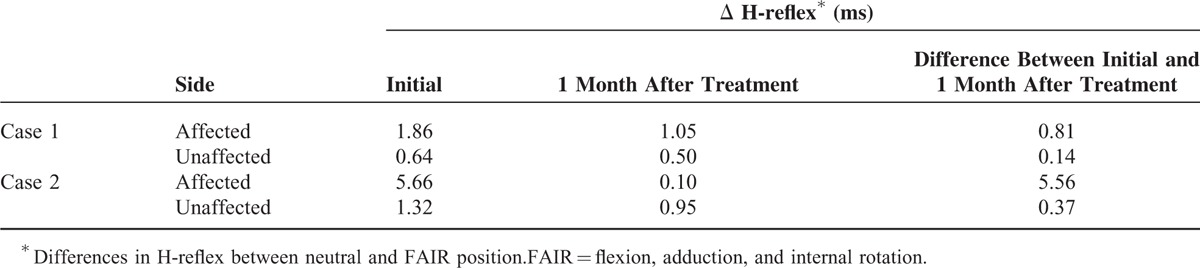
FIGURE 1.
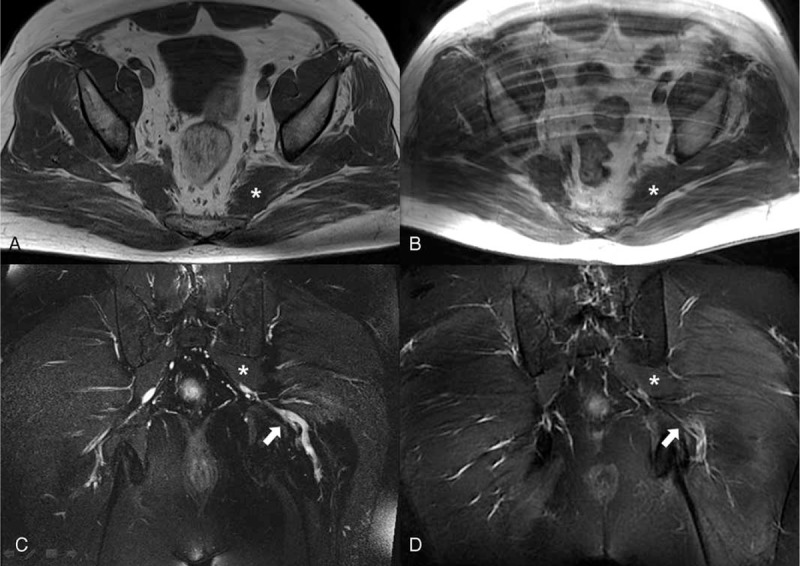
Pelvic magnetic resonance neurography of Case 1. Axial T2-weighted cross-section taken before the treatment (A) and 1 month after the treatment (B). Coronal T2-neurography cross-section taken before the treatment (C) and 1 month after the treatment (D). Hypertrophy of the left piriformis muscle (asterisk) is seen (A, C). One month after the injection, equivocal decrease of left piriformis muscle (asterisk) volume is observed (B, D). Swelling of the left sciatic nerve (white arrow) at and around the left piriformis muscle is observed (C). Significant decrease of left sciatic nerve (white arrow) swelling was noted after the injection (D).
FIGURE 2.
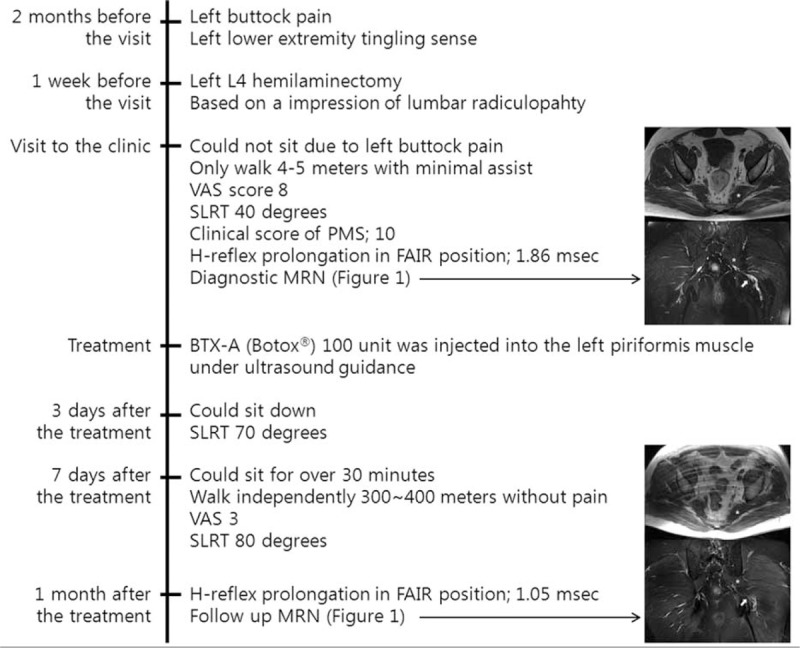
Timeline of Case 1.
CASE 2
A 64-year-old man with no notable medical history visited the hospital with a complaint of gait disturbance for the past 6 months. Before the onset of gait disturbance, he had been healthy enough for mountaineering, with no apparent triggering event including trauma. As time went on his symptoms worsened, and he was wheelchair-bound when he visited department of physical medicine and rehabilitation. On the initial physical examination, both upper and lower extremities showed Medical Research Council (MRC) grade V muscle strength, and there were no abnormal findings on sensory examination. However, when trying to walk, he could not bear his weight on the left side and demonstrated lumbar hyperextension in the swing phase. The clinical scoring system for the diagnosis of PMS indicated a score of 12.3 On electrodiagnostic study, the left tibial H-reflex showed 5.66 ms prolongation by the FAIR test compared with the neutral position (Table 2). A pelvic MRN was performed with impression of the PMS. Hypertrophy of the left piriformis muscle with slight swelling of the lumbosacral plexus anterior to the muscle was observed, suggesting the possibility of PMS (Fig. 3). BTX-A (Botox®) 100 unit was injected into the left piriformis muscle under ultrasound guidance. The lowest dose with proven therapeutic effect in previous studies was selected to minimize the possible complication.8 A 4-ml injection containing 100 unit of BTX-A in preserve-free normal saline was administrated via the peppering technique. Ethical approval was not necessary since the procedure was performed for therapeutic purpose and the clinical effect of procedure has already been proven. The patient was tolerable through the procedure, and there was no adverse or unanticipated event. Three days after the injection, the patient could bear his weight on the left side, and the lumbar hyperextension seen in the swing phase and gait endurance were improved. A week after the injection, he could walk indoors > 300 m without a walking aid such as a wheelchair or cane. Two months after the injection, he could walk outside independently > 500 m. The prolongation of the H-reflex in the FAIR position was improved to 0.10 ms in the follow-up study performed 1 month after the injection (Table 2). Compared with the diagnostic MRN, a marked decreased of the left piriformis muscle volume and significant decrease of left sciatic nerve swelling were noted in the follow-up pelvic MRN taken 2 months after BTX-A injection (Figs. 3 and 4). Four months after the injection, pain completely resolved and the patient had no limitation on walking or other activities of daily living. The improved state was maintained until the 6th month after injection and did not need more follow-up.
FIGURE 3.
Pelvic magnetic resonance neurography of Case 2. Axial T2-weighted cross-section taken before the treatment (A) and 2 months after the treatment (B). Coronal T2-neurography cross-section taken before the treatment (C) and 2 months after the treatment (D). Hypertrophy of the left piriformis muscle (asterisk) is apparent (A, C), and a marked decreased of the left piriformis muscle (asterisk) volume is noted 2 months after the injection (B, D). Slight swelling of the sciatic nerve (white arrow) is observed (C). After the injection, significant decrease of left sciatic nerve (white arrow) swelling was noted (D).
FIGURE 4.
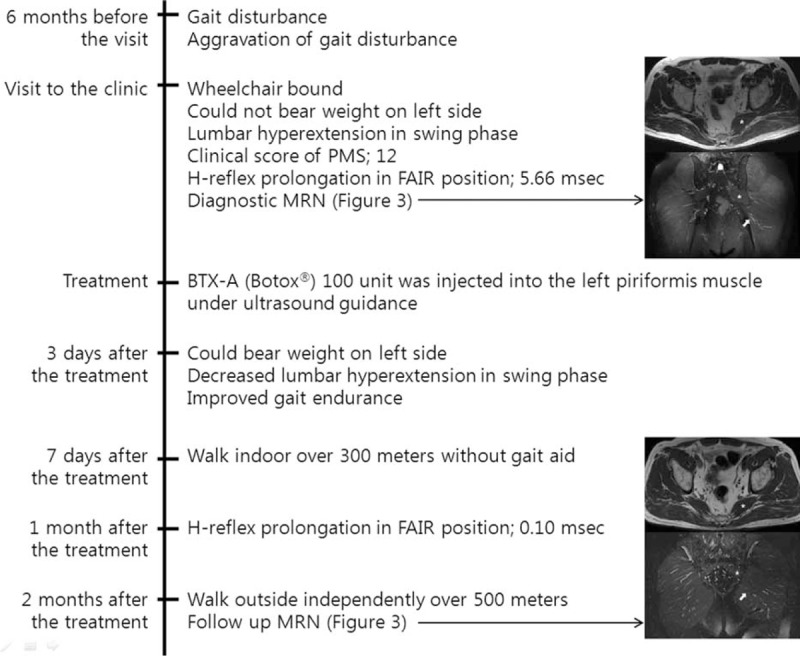
Timeline of Case 2.
DISCUSSION
PMS is an underdiagnosed cause of buttock and leg pain that can be difficult to treat. There is no gold standard in diagnosing PMS. Physical examination may reveal signs of sciatic nerve compression.10 The diagnostic value of electrophysiological tests can be improved by stressing the muscle in flexion, adduction, and internal rotation (the FAIR test). A prolongation of 1.86 ms in the FAIR test is an electrophysiological criterion for diagnosing PMS.11 Imaging modalities such as plain radiography, computed tomography, and ultrasound add certainty in diagnosis. MRI is increasingly being selected over other imaging modalities. MRI of the nerves, also known as MRN, is increasingly being used as a noninvasive means of diagnosing peripheral nerve disease. MRN directly shows the nerve anatomy and is accomplished by using a combination of pulse sequences allowing detection of changes in both nerve signal and architecture.5 MRN findings allow differentiation of neuropathic conditions related to entrapment, trauma, iatrogenic injury, extrinsic mass effect, and tumors/tumor-like lesions of the nerves.2 Chhabra and colleagues reported the optimal cutoff value of nerve/vessel signal intensity ratio for predicting sciatic neuropathy was 0.89, with sensitivity of 94.1% and specificity of 90.2% (area under the ROC curve, 0.963;95%confidence interval, 0.886–0.994).7 On MRN images, a normal nerve has intermediate signal intensity similar to muscle on T1-weighted images and intermediate to minimally increased signal intensity on T2-weighted images, depending on the amount of endoneurial fluid and background fat suppression. When the nerve sustains an injury, normal endoneurial fluid protected by an intact perineurial blood-nerve barrier becomes altered, and the nerve signal demonstrates higher intensity on T2-weighted images due to proximal accumulation of the endoneurial fluid, vascular congestion, and distal Wallerian degeneration.8,9
There are few studies using MRN in PMS. Lewis et al used MRN to image the lumbosacral plexus and sciatic nerve and demonstrated high signal intensity of the sciatic nerve mostly at the sciatic notch or at the level of the piriformis muscle.2 These authors utilized MRN to diagnose PMS and determine the method of treatment, but they did not confirm changes to the sciatic nerve after treatment.
PMS usually responds to conservative treatments, but when patients fail to respond to simple conservative therapy, interventional modalities are considered. Injections of local anesthetics, steroid, or botulinum toxin into the piriformis muscle are generally performed.4 Botulinum toxin injection is more effective in treating PMS than either triamcinolone acetonide and lidocaine injections or placebo injections.6
With ultrasound guidance, the accuracy of injections increases. It was validated in a cadaver study, suggesting an accuracy of 95%.10 Blunk verified the accuracy of needle placement under ultrasound guidance via MRI in human subjects.11 Based on these reports, we injected botulinum toxin into the piriformis muscle under ultrasound guidance.
The clinical effects of ultrasound-guided botulinum toxin injection are already widely known12–14 but changes to the anatomical structures after the injection have been confirmed in few studies. Al-Al-Shaikh et al used MRI to evaluate changes in piriformis muscle morphology after treatment with botulinum toxin injections and the treated piriformis muscle demonstrated a reduction in thickness and volume and an increase in fatty infiltration compared to the normal contralateral muscle.15 Although the results indicated the effect of botulinum toxin, they compared changes to the treated muscle with the contralateral side, not the identical muscle before treatment. Fanucci performed MRI before and 3 months after botulinum toxin injection in PMS patients and the denervation process of the piriformis muscle or only atrophy of the treated muscle was detected.16
Previous studies of MRN and BTX-A injection in PMS demonstrated changes in the piriformis muscle but did not describe changes in the sciatic nerve itself. In this study, although it is a limited case series, we describe the changes to the nerve morphology before and after the BTX-A injection treatment in addition to other anatomical structures. In these patients, MRN revealed increased signal of the sciatic nerve under the hypertrophied piriformis muscle, supporting the suspicion of PMS arising from physical examination. We then confirmed that the swelling of the sciatic nerve and volume of the piriformis muscle were decreased on follow-up MRN after the BTX-A injection.
Ultrasound-guided BTX-A to the piriformis muscle achieved definite clinical improvement and normalization of electrophysiological test results. Additionally, it was found via MRN that BTX-A injection can cause resolution of signal change and swelling of sciatic nerve secondary to atrophy of the piriformis muscle. MRN can be an effective tool for diagnosis as well as to confirm the response to treatment in PMS.
Footnotes
Abbreviations: BTX-A = botulinum toxin type A, FAIR = flexionadduction and internal rotation, MRI = magnetic resonance imaging, MRN = magnetic resonance neurography, PS = piriformis syndrome, VAS = visual analogue scale.
Disclosure: Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
REFERENCES
- 1.Lang AM. Botulinum toxin type B in piriformis syndrome. Am J Phys Med Rehabil 2004; 83:198–202. [DOI] [PubMed] [Google Scholar]
- 2.Lewis AM, Layzer R, Engstrom JW, et al. Magnetic resonance neurography in extraspinal sciatica. Arch Neurol 2006; 63:1469–1472. [DOI] [PubMed] [Google Scholar]
- 3.Filler AG, Howe FA, Hayes CE, et al. Magnetic resonance neurography. Lancet 1993; 13: 341:659–661. [DOI] [PubMed] [Google Scholar]
- 4.Howe FA, Filler AG, Bell BA, et al. Magnetic resonance neurography. Magn Reson Med 1992; 28:328–338. [DOI] [PubMed] [Google Scholar]
- 5.Stoll G, Bendszus M, Perez J, et al. Magnetic resonance imaging of the peripheral nervous system. J Neurol 2009; 256:1043–1051. [DOI] [PubMed] [Google Scholar]
- 6.Koltzenburg M, Bendszus M. Imaging of peripheral nerve lesions. Curr Opin Neurol 2004; 17:621–626. [DOI] [PubMed] [Google Scholar]
- 7.Chhabra A, Chalian M, Soldatos T, et al. 3-T high-resolution MR neurography of sciatic neuropathy. Am J Roentgenol 2012; 198:W357–364. [DOI] [PubMed] [Google Scholar]
- 8.Husarik DB, Saupe N, Pfirrmann CW, et al. Elbow nerves: MR findings in 60 asymptomatic subjects—normal anatomy, variants, and pitfalls. Radiology 2009; 252:148–156. [DOI] [PubMed] [Google Scholar]
- 9.Petchprapa CN, Rosenberg ZS, Sconfienza LM, et al. MR imaging of entrapment neuropathies of the lower extremity. Part 1: The pelvis and hip. Radiographics 2010; 30:983–1000. [DOI] [PubMed] [Google Scholar]
- 10.Finnoff JT, Hurdle MF, Smith J. Accuracy of ultrasound-guided versus fluoroscopically guided contrast-controlled piriformis injections: a cadaveric study. J Ultrasound Med 2008; 27:1157–1163. [DOI] [PubMed] [Google Scholar]
- 11.Blunk JA. MRI verification of ultrasound-guided infiltrations of local anesthetics into the piriformis muscle. Pain Med 2013. [DOI] [PubMed] [Google Scholar]
- 12.Fishman LM, Anderson C, Rosner B. BOTOX and physical therapy in the treatment of piriformis syndrome. Am J Phys Med Rehabil 2002; 81:936–942. [DOI] [PubMed] [Google Scholar]
- 13.Fishman LM, Konnoth C, Rozner B. Botulinum neurotoxin type B and physical therapy in the treatment of piriformis syndrome: a dose-finding study. Am J Phys Med Rehabil 2004; 83:42–50.quiz 51-43. [DOI] [PubMed] [Google Scholar]
- 14.Yoon SJ, Ho J, Kang HY, et al. Low-dose botulinum toxin type A for the treatment of refractory piriformis syndrome. Pharmacotherapy 2007; 27:657–665. [DOI] [PubMed] [Google Scholar]
- 15.Al-Al-Shaikh M, Michel F, Parratte B, et al. An MRI evaluation of changes in piriformis muscle morphology induced by botulinum toxin injections in the treatment of piriformis syndrome. Diagn Intervent Imaging 2014. [DOI] [PubMed] [Google Scholar]
- 16.Fanucci E. CT-guided injection of botulinic toxin for percutaneous therapy of piriformis muscle syndrome with preliminary MRI results about denervative process. Eur Radiol 2001; 11:2543–2548. [DOI] [PubMed] [Google Scholar]


