Abstract
Inpatient hospice care can reduce futile treatment and medical costs. However, the cost trimming effect of home-based hospice care in hospital has yet not been explored. This study evaluates the impact of home-based hospice care on end-of-life expenditure in hospitals with different spending intensity.
This is a population-based retrospective study in Taiwan. Cancer decedents were identified in the National Health Insurance Research Database (NHIRD) from 2009 to 2011. They are categorized by hospital spending intensity. A hierarchical linear regression model with a random-intercept model was used to analyze the relationship between end-of-life expenditure (dependent variable) with and without home-based hospice, and both patient-level and hospital-level characteristics.
A total of 78,613 cancer decedents were identified in the NHIRD from 2009 to 2011. Of these decedents, 17,638, 43,286, and 17,689 were categorized by hospital spending intensity as high, moderate, and low, respectively. Decedents with home-based hospice care were associated with US$2452 less in expenditure per patient compared with those without home-based hospice care. The majority of savings occurred in the last 3 months of life. These savings with home-based hospice care were consistent in hospitals with different levels of spending intensity.
Home-based hospice reduced one-fifth expenditure at the end of life of cancer decedents treated in hospitals with different spending intensity.
INTRODUCTION
End-of-life (EOL) care is an issue in terminal decedents with cancer. In the United States, more than 1 quarter of Medicare spending was consumed by EOL care of decedents in their last year of life.1 Futile treatment has been discussed extensively. And in Canada, decedents with <6 months of life comprised 1.1% of the population but consumed more than one-fifth of healthcare spending.2 Hospice care is a management to reduce the expenditure and increase quality of life at the EOL.
Hospice care can benefit terminally ill patients by increasing family satisfaction,3 and reduce futile treatment and medical costs.4,5 On the other hand, hospice disenrollment is a marker for higher healthcare use and expenditure for care.6 Many studies have investigated the relationship between inpatients hospice care and EOL treatment and costs.7,8 Contrasted with inpatient hospice care, the cost trimming effect of home-based hospice care in hospitals with different spending intensity has yet not been explored. Although it has been mentioned early in 1992.9 As the telemedicine systems develop, home-based hospice is becoming more feasible and convenient.10,11 Rural area previous in lack of hospice may benefit from home-based hospice care.12
The aim of this study was to increase our understanding about the expenditure-reducing effect of home-based hospice care in hospitals with different levels of spending intensity. We investigated whether home-based hospice care can reduce EOL costs in all kinds of hospitals.
METHODS
Ethics Statement
This study was approved by the Institutional Review Board of Buddhist Dalin Tzu Chi General Hospital, Chiayi, Taiwan. The institutional review board stated that written consents from patients were not required for this study because the identification numbers and personal information about participants were not included in the secondary files.
Database
The data for this study were collected from the Taiwan National Health Insurance Research Database (NHIRD) from the years 2009 through 2011. This dataset has been organized and managed by the Taiwan National Health Research Institutes but collected by the Taiwan National Health Insurance Program since 1995. The program covers approximately 99% of the residents in Taiwan and has contracts with 97% of medical providers nationwide. To verify the accuracy of diagnosis, the Taiwan Bureau of National Health Insurance randomly interviews patients and reviews the charts of 1 per 100 ambulatory and 1 per 20 inpatient claims.13 Taiwan's NHI has the unique characteristics of universal insurance coverage and a single-payer system with the government as sole insurer.
Setting
This is a retrospective, population-based study. This study enrolled decedents with cancer diagnoses during the study period (2009–2011). We calculated the expenditure for each decedent for 6 months before death. To determine the factors associated with EOL expenditure, decedents and hospital-level characteristics were identified and analyzed with hierarchical linear regression using a random-intercept model to solve the cluster effect of hospitals. We specifically looked at the impact of home-based hospice care trends in EOL expenditure for 6 months before death. We also looked at home-based hospice care as a modifying factor in hospital spending intensity (HSI).
Participants
A total of 78,613 cancer decedents were identified in the NHIRD from 2009 to 2011. Cancer diagnoses were identified by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 140.x to 239.x, and the diagnoses were verified by comparing them with the Catastrophic Illness dataset. Decedents were identified by a record of death during the study period (2009–2011).
Home-Based Hospice Care
Home-based hospice care was identified by outpatient claims with case type code 65.
Hospital Spending Intensity Index
The HSI index was calculated from the expenditure of a different cohort in their last 6 months of life in the same hospital to reduce the potential “reverse causality effect.” Similar work can be found in previous study by Chang et al14 and Stukel et al.15 Because Stukel et al15 found that EOL expenditure and acute-care expenditure were highly correlated (r = 0.81), EOL expenditure can represent the intensity of hospital care provided to patients, such as the usage of intensive care units, physician visits, specialist consultations, and diagnostic tests. It was categorized into approximate terciles of high, medium, and low hospital spending index.
Measurements
The key independent variable was the total amount of the healthcare expenditure for the last 6 months of life for the cancer decedents. The analysis was further stratified by the HSI. Disease severity was estimated by using the Deyo adaptation of the Charlson Comorbidity Index Score (CCIS), which was derived from inpatient diagnoses in the last 6 months of life.16,17 Socioeconomic status (SES) was classified into 3 groups by individual income as our previous study.18 Diagnosis and metastatic status were combined to identify 7 subgroups (I–VII) of cancers that were homogeneous in terms of survival and disease course.19 Metastatic status was identified by using ICD-9 codes 196.xx to 199.xx. Subgroups included 4 cancer types: germ cell tumors and prostate cancer; lung, liver, and pancreatic cancer; hematologic malignancies; and all other cancers. Other patient characteristics included age, gender, and region of patients’ residence and primary physician's specialty. Hospital characteristics included district caseload, urbanization, and geographic region. The methods of recording and definitions of these variables were described in our previous studies.20,21
Statistical Methods
The SPSS version 15 (SPSS, Inc., Chicago, IL) was used to analyze the data. We used χ2 test for categorical variables and 1-way ANOVA test for continuous variables in Table 1. We performed multilevel analysis (hierarchical linear regression) using hospital as a random-intercept model to compare the EOL medical expenditure in their last 6 months of life between cancer decedents with and without home-based hospice care in Table 2. We also used multilevel analysis using a random-intercept model to compare the EOL medical expenditure in their last 6 months of life between cancer decedents with and without home-based hospice care by different hospital spending intensities in Table 3. The model was chosen because of the potential clustering effect exerted by a hospital. Hospital-level policies, procedures, or physician compensation mechanisms may produce differential EOL expenditure patterns in each hospital. A value of P < 0.05 was used to determine statistical significance.
TABLE 1.
Baseline Characteristics of Cancer Decedents From 2009 to 2011 (n = 78,613)
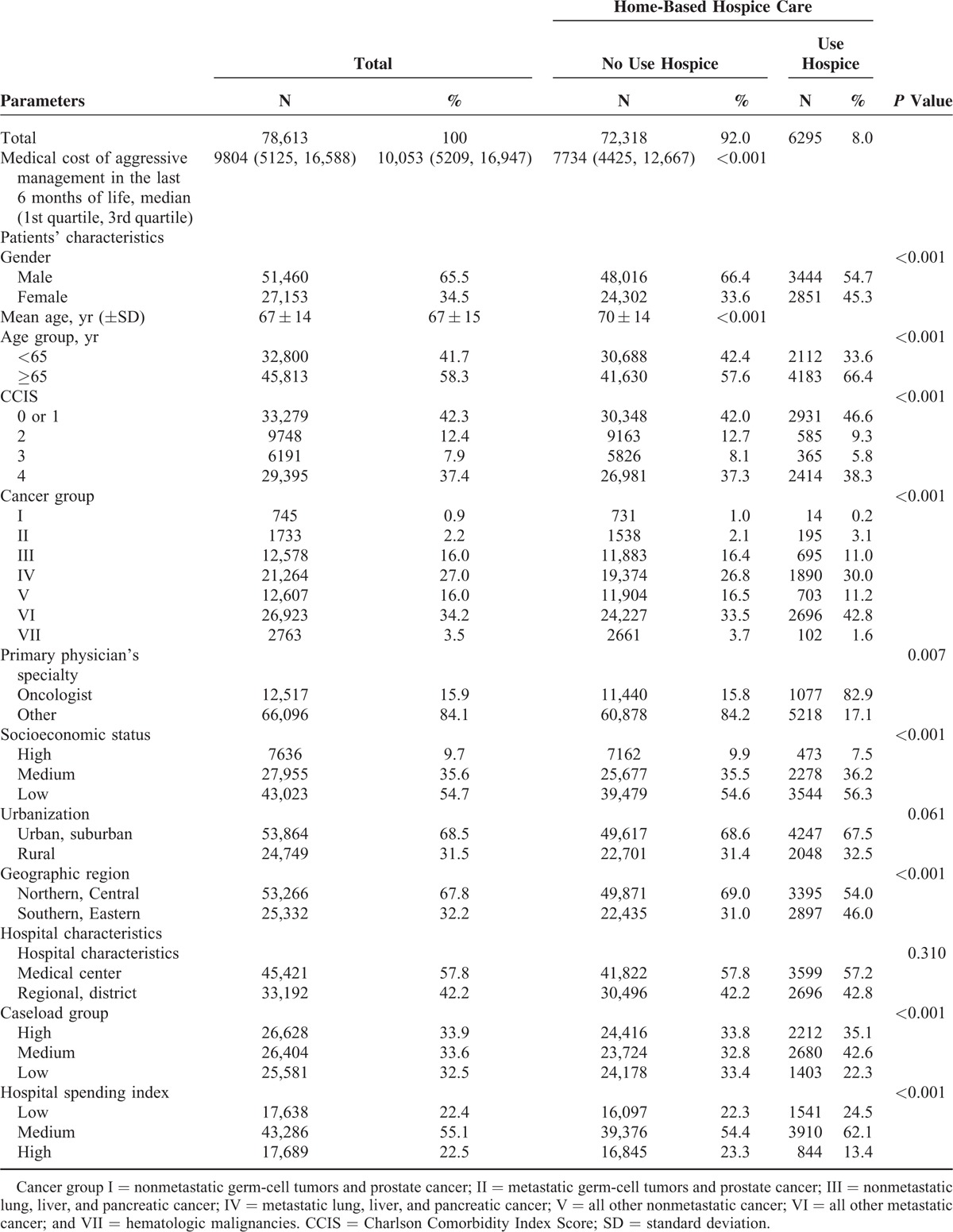
TABLE 2.
Medical Cost for Taiwanese Cancer Decedents From 2009 to 2011 by Multivariate Analysis Using a Random-Intercept Model (n = 78,613)
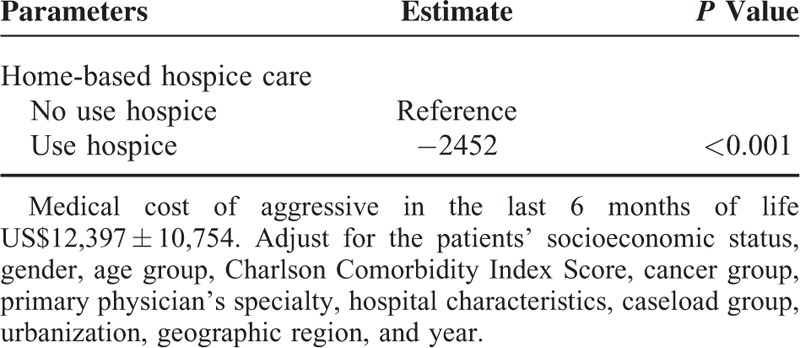
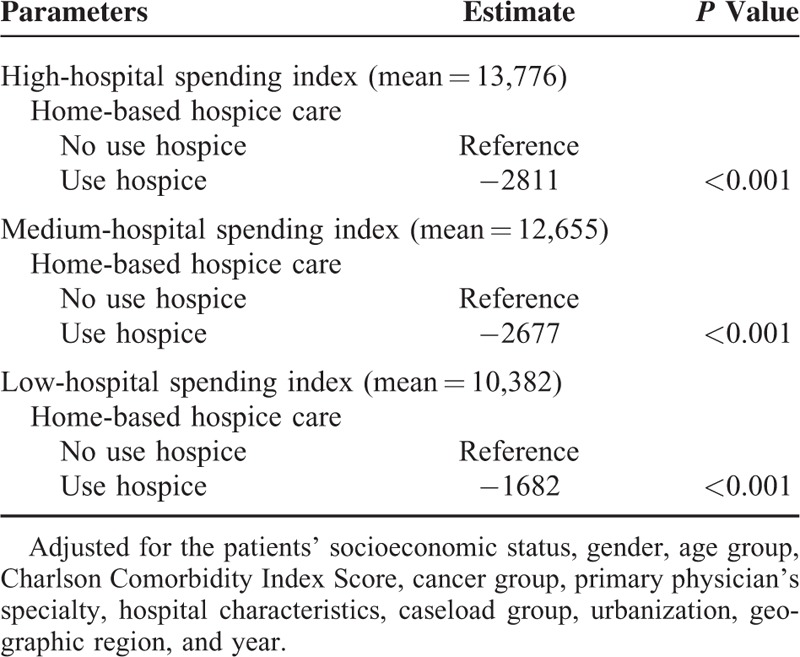
TABLE 3.
Medical Cost for Taiwanese Cancer Decedents From 2009 to 2011 by Multivariate Analysis Using a Random-Intercept Model According to Hospital Spending Intensity
RESULTS
A total of 78,613 decedents with cancer diagnoses were identified in the NHIRD database from 2009 to 2011. According to the HSI levels of the hospitals, we identified 17,638, 43,286, and 17,689 decedents admitted to hospitals with high, moderate, and low HSI, respectively. Eight percent of decedents had used home-based hospice care in their last 6 months of life. The median medical cost of aggressive management in the last 6 months of life was US$10,053 per decedents without home-based hospice use and US$7734 per decedents with home-based hospice. The baseline characteristics of these decedents are shown in Table 1.
The EOL cost for cancer decedents increased each month as they approached death except for the last 1 in Figure 1. Cancer decedents with home-based hospice care were associated with much less EOL cost than those without home-based hospice care. A similar pattern was found in hospitals with different levels of spending intensity in Figure 2, especially over the last 3 months, during which home-based hospice care was mostly responsible for reducing the cost.
FIGURE 1.
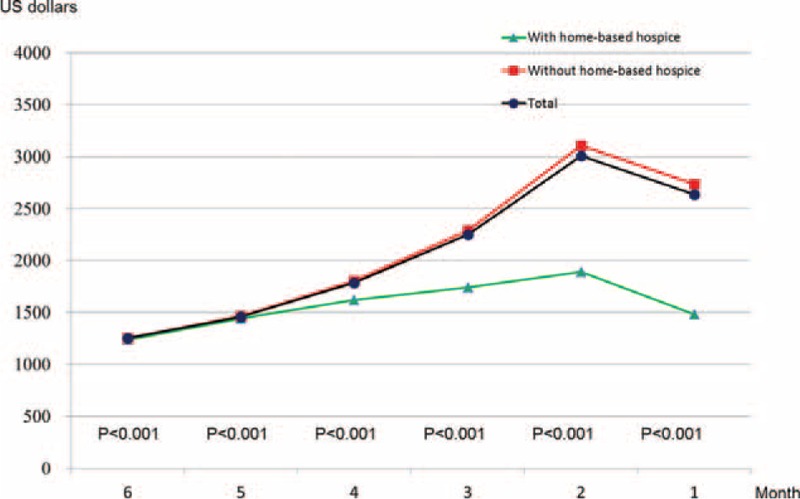
Trends of end of life expenditure in the last 6 months among cancer decedents with and without home-based hospice care in Taiwan.
FIGURE 2.
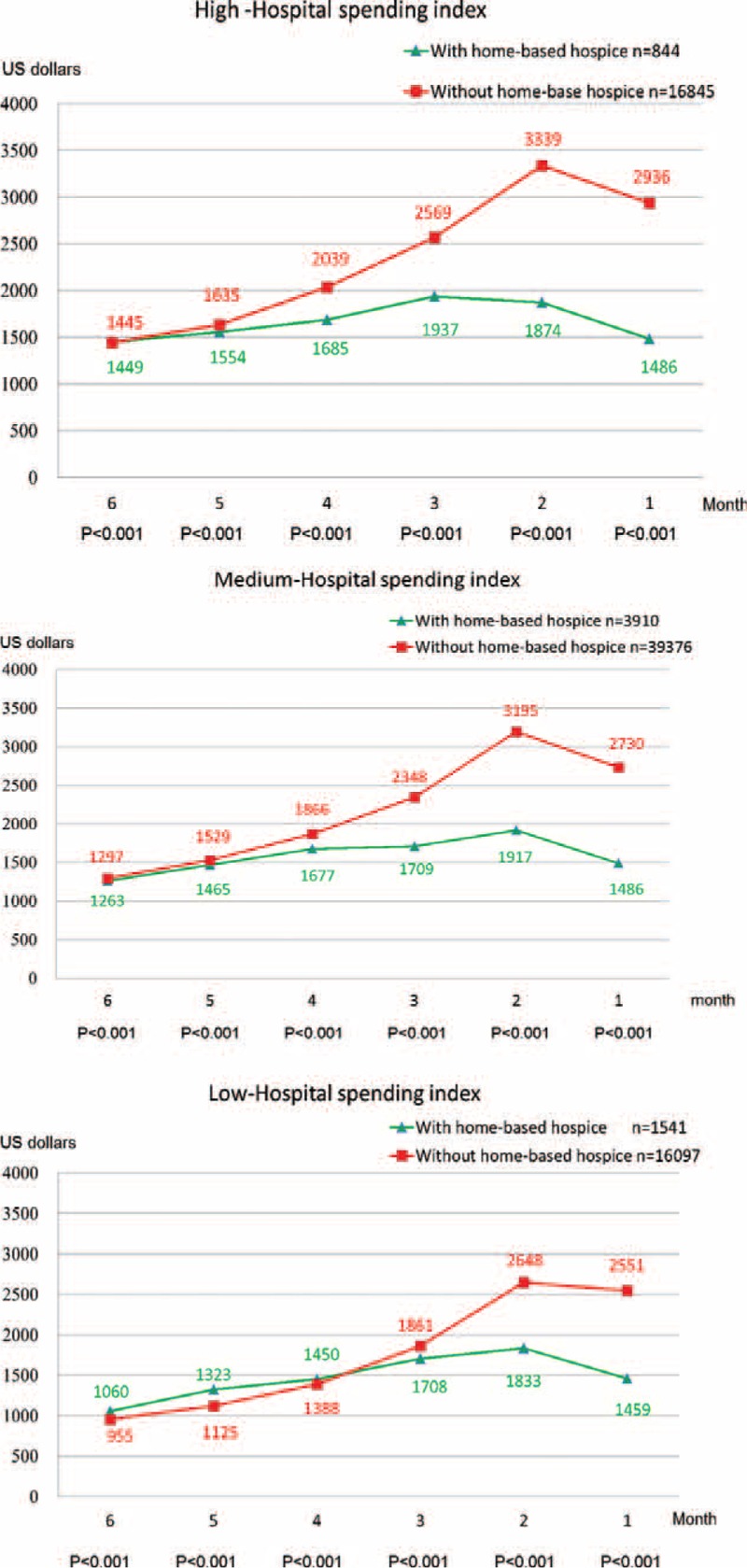
Trends of end of life expenditure for cancer decedents with or without home-based hospice care in hospitals with high, medium, and low hospital spending index.
The median EOL expenditure per decedent in the last 6 months of life was US$9804. Home-based hospital care was associated with US$2452 less in cost (−19.8%) in Table 2. Other variables were not shown here. That is, low SES, low HSI, CCIS 1 or 0, and living in a rural area were also associated with less cost. Male gender, age >65, and care by an oncologist were associated with higher cost. The year 2011 cost less than 2009. Different cancer groups were associated with various EOL costs. Of these, hematologic malignancy cost extraordinarily more. We have further analyzed that in another article.22
In multivariate analysis using a random-intercept model according to different hospital spending intensities, home-based hospice reduced US$2811 (20.4%), US$2677 (21.2%), and US$1682 (16.2%) in cost per decedents among cancer decedents treated by high, medium, and low hospital intensity, respectively, in Table 3.
DISCUSSION
This study found that home-based hospice care was associated with less EOL expenditure in hospitals with different levels of spending intensity. The expenditure at EOL increased as decedents approached death. The gap between EOL expenditure curves of decedents with and without hospice care increased as they approached death as well, especially in the last 3 months. These results have implications for public health policy makers who could offer hospice incentives to healthcare providers because home-based hospice care may help to reduce the expenditure at the EOL among cancer decedents in hospitals with different spending intensities or practice styles. If the incentive covered the profit of health service providers, then they might promote hospice care, and the overall financial burden would thus be reduced.
The strength of this study was that it consisted of huge patient numbers to lessen the effects of minor confounding factors. And we used multilevel analysis to reduce the clustering effect exerted by the practice pattern of a hospital. The Taiwan Health Insurance Program has covered approximately 99% of the population since 1995, and a growing body of articles has confirmed the validity of the dataset. We observed a robust influence of home-based hospice care on the expenditure on EOL care in cancer decedent in hospitals, and calculated the amount that could be saved by home-based hospice care. We found no other study which discussed the effect of home-based hospice care on EOL care in hospitals with different practice styles.
It has been shown that hospice care may reduce medical costs for cancer decedents.23,24 In Canada, Dumont et al25 showed that the overall costs of EOL care gradually increased from the fifth to the last month of the patient's life, and informal care costs were particularly high over the last 3 months of life. In Israel, Bentur et al found that 1 quarter of their terminal cancer patients received home-based hospice care. Their average cost was $13,648 compared with $18,503 for patients without home-hospice care.26 Postier et al27 found that noncancer patients with at least 6 months of home-based pediatric palliative care exposure showed a significant decrease in total hospital charges of nearly $275,000 from pre to postprogram admission. Our study showed similar cost trimming effect.
HSI is calculated according to EOL expenditure. Higher spending intensity level was associated with lower mortality in common inpatients conditions.15,28 Though some studies showed that different HSI levels were not necessarily related to better survival or quality of care.29,30 HSI levels can still reflect different practice styles.
One limitation of this study was that the cancer diagnosis and co-morbid conditions were acquired from the National Health Insurance claims using ICD-9 codes. These ICD-9 codes could differ from actual condition of the decedents. To decrease the mistakes of coding, the National Health Insurance Bureau in Taiwan randomly reviewed charts and contact with patients to improve the accuracy of diagnosis. Furthermore, some disease diagnoses have been validated in the NHIRD.31 The data from NHIRD also lack cancer stage, quality of life, laboratory data, and pathology report. However, given the robustness of the evidence and the statistical analysis in this study, these limitations were less likely to compromise the validity of our results.
This study revealed that home-based hospice care was associated with lower EOL expenditure in hospitals with different spending intensity levels. Compared to other countries, the penetration rate of home-based hospice care in Taiwan presents a great opportunity for improvement. Policy makers should consider incentives for home-based hospice care in order to improve its utilization.
Footnotes
Abbreviations: CCIS = Charlson Comorbidity Index Score, EOL = end of life, HSI = hospital spending intensity, ICD-9-CM = International Classification of Disease, 9th Revision, Clinical Modification, NHIRD = National Health Insurance Research Database, SD = standard deviation, SES = socioeconomic status.
Contribution: Conception and design: L-FC and C-YH; administrative support: C-MC and C-YH; collection and assembly of data: all authors; data analysis and interpretation: C-MC; manuscript writing: L-FC and C-YH; and final approval of manuscript: all authors.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding was received for this study.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Riley GF, Lubitz JD. Long-term trends in Medicare payments in the last year of life. Health Serv Res 2010; 45:565–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fassbender K, Fainsinger RL, Carson M, et al. Cost trajectories at the end of life: the Canadian experience. J Pain Symptom Manage 2009; 38:75–80. [DOI] [PubMed] [Google Scholar]
- 3.Lin W-Y, Chiu T-Y, Hsu H-S, et al. Medical expenditure and family satisfaction between hospice and general care in terminal cancer patients in Taiwan. J Formosan Med Assoc 2009; 108:794–802. [DOI] [PubMed] [Google Scholar]
- 4.Abernethy AP, Kassner CT, Whitten E, et al. Death service ratio: a measure of hospice utilization and cost impact. J Pain Symptom Manage 2011; 41:e5–e6. [DOI] [PubMed] [Google Scholar]
- 5.Gozalo PL, Miller SC, Intrator O, et al. Hospice effect on government expenditures among nursing home residents. Health Serv Res 2008; 43:134–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlson MDA, Herrin J, Du Q, et al. Impact of hospice disenrollment on health care use and Medicare expenditures for patients with cancer. J Clin Oncol 2010; 28:4371–4375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Langton JM, Blanch B, Drew AK, et al. Retrospective studies of end-of-life resource utilization and costs in cancer care using health administrative data: a systematic review. Palliat Med 2014; 28:1167–1196. [DOI] [PubMed] [Google Scholar]
- 8.Binney ZO, Quest TE, Feingold PL, et al. Feasibility and economic impact of dedicated hospice inpatient units for terminally ill ICU patients. Crit Care Med 2014; 42:1074–1080.doi:10.1097/CCM.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 9.Lubin S. Palliative care—could your patient have been managed at home? J Palliat Care 1992; 8:18–22. [PubMed] [Google Scholar]
- 10.Doolittle GC, Yaezel A, Otto F, et al. Hospice care using home-based telemedicine systems. J Telemed Telecare 1998; 4 Suppl 1:58–59. [DOI] [PubMed] [Google Scholar]
- 11.Hong HS, Kim IK, Lee SH, et al. Adoption of a PDA-based home hospice care system for cancer patients. Comput Inf Nurs 2009; 27:365–371.doi:10.1097/NCN.0b013e3181bcab43. [DOI] [PubMed] [Google Scholar]
- 12.Virnig BA, Ma H, Hartman LK, et al. Access to home-based hospice care for rural populations: identification of areas lacking service. J Palliat Med 2006; 9:1292–1299. [DOI] [PubMed] [Google Scholar]
- 13.Tseng C-H. Mortality and causes of death in a national sample of diabetic patients in Taiwan. Diabetes Care 2004; 27:1605–1609. [DOI] [PubMed] [Google Scholar]
- 14.Chang T-S, Huang K-Y, Chang C-M, et al. The association of hospital spending intensity and cancer outcomes: a population-based study in an Asian country. Oncologist 2014; 19:990–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stukel TA, Fisher ES, Alter DA, et al. Association of hospital spending intensity with mortality and readmission rates in Ontario hospitals. JAMA 2012; 307:1037–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992; 45:613–619. [DOI] [PubMed] [Google Scholar]
- 17.Ho TH, Barbera L, Saskin R, et al. Trends in the aggressiveness of end-of-life cancer care in the universal health care system of Ontario. Canada J Clin Oncol 2011; 29:1587–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang C-Y, Hung Y-T, Chang C-M, et al. The association between individual income and aggressive end-of-life treatment in older cancer decedents in Taiwan. PLoS ONE 2015; 10:e0116913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tang ST, Wu S-C, Hung Y-N, et al. Determinants of aggressive end-of-life care for Taiwanese cancer decedents, 2001 to 2006. J Clin Oncol 2009; 27:4613–4618. [DOI] [PubMed] [Google Scholar]
- 20.Ho T-Y, Huang K-Y, Huang T-T, et al. The impact of influenza vaccinations on the adverse effects and hospitalization rate in the elderly: a national based study in an Asian country. PLoS ONE 2012; 7:e50337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee C-C, Su Y-C, Ho H-C, et al. Risk of stroke in patients hospitalized for isolated vertigo: a four-year follow-up study. Stroke 2011; 42:48–52. [DOI] [PubMed] [Google Scholar]
- 22.Hung Y-T, Huang C-Y, Chang C-M, et al. The association of hematological malignancy and end-of-life expenditure in cancer decedents: a population-based study in an Asian country. Medicine 2015; 94:e1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Campbell DE, Lynn J, Louis TA, et al. Medicare program expenditures associated with hospice use. Ann Intern Med 2004; 140:269–277. [DOI] [PubMed] [Google Scholar]
- 24.Emanuel EJ, Ash A, Yu W, et al. Managed care, hospice use, site of death, and medical expenditures in the last year of life. Arch Intern Med 2002; 162:1722–1728. [DOI] [PubMed] [Google Scholar]
- 25.Dumont S, Jacobs P, Turcotte V, et al. The trajectory of palliative care costs over the last 5 months of life: a Canadian longitudinal study. Palliat Med 2010; 24:630–640. [DOI] [PubMed] [Google Scholar]
- 26.Bentur N, Resnizky S, Balicer R, et al. Utilization and cost of services in the last 6 months of life of patients with cancer—with and without home hospice care. Am J Hosp Palliat Med 2014; 31:723–725. [DOI] [PubMed] [Google Scholar]
- 27.Postier A, Chrastek J, Nugent S, et al. Exposure to home-based pediatric palliative and hospice care and its impact on hospital and emergency care charges at a single institution. J Palliat Med 2014; 17:183–188. [DOI] [PubMed] [Google Scholar]
- 28.Romley JA, Jena AB, Goldman DP. Hospital spending and inpatient mortality: evidence from California: an observational study. Ann Intern Med 2011; 154:160–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med 2003; 138:273–287. [DOI] [PubMed] [Google Scholar]
- 30.Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med 2003; 138:288–298. [DOI] [PubMed] [Google Scholar]
- 31.Cheng C-L, Kao Y-HY, Lin S-J, et al. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf 2011; 20:236–242. [DOI] [PubMed] [Google Scholar]


