Abstract
T-cell depletion of an HLA-haploidentical graft is often used to prevent graft-vs.-host disease (GvHD), but the procedure may lead to increased graft failure, relapse, and infections due to delayed immune recovery. We hypothesized that selective depletion of the CD45RA+ subset can effectively reduce GvHD through removal of naïve T cells, while providing improved donor immune reconstitution through adoptive transfer of CD45RA– memory T cells. Herein, we present results from the first 17 patients with poor-prognosis hematologic malignancy who received haploidentical donor transplantation with CD45RA-depleted progenitor cell grafts following a novel reduced intensity conditioning regimen without total body irradiation or serotherapy. Extensive depletion of CD45RA+ T cells and B cells, with preservation of abundant memory T cells, was consistently achieved in all 17 products. Neutrophil engraftment (median day +10) and full donor chimerism (median day +11) was rapidly achieved post-transplantation. Early T-cell reconstitution directly correlated with the CD45RA-depleted graft content. T-cell function recovered rapidly with broad TCR Vβ spectra. There was no infection-related mortality in this heavily pretreated population, and no patient developed acute GvHD despite infusion of a median of >100 million per kilogram haploidentical T cells.
Introduction
Hematopoietic cell transplantation (HCT) is effective therapy for many patients with high-risk hematologic malignancies.1 Unfortunately, even with enormous volunteer donor registries, a substantial number of patients remain without an available HLA-matched related or unrelated donor.2 These patients then must undergo HCT using an alternative HLA-mismatched source such as unrelated umbilical cord blood or related haploidentical donor.3-5 Haploidentical donors are viable alternatives, as family members are highly motivated and readily available for a majority of patients.6 Initial success with haploidentical donors was achieved using grafts that were extensively T-cell depleted ex vivo.7-12 However, these transplants were met with relatively high rates of graft failure, relapses, or infections due to delayed hematopoietic and immune reconstitution.13, 14 More recently developed haploidentical donor HCT approaches have diminished some of these early challenges. T-cell replete haploidentical donor transplant has been increasingly utilized and demonstrate outcomes comparable to those of sibling donor transplantations.15-20 Other recent T-cell depleted haploidentical donor transplantation regimens employ selective T-cell depletion techniques9 or selected T-cell add back procedures14 to alleviate the risks of rejection, acute GvHD, infection, and relapse.
When T cells are depleted either ex vivo or in vivo, the patient must wait for the slow process of de novo T-cell production and education.21 Therefore, a selective T-cell depletion method that depletes naïve T cells to prevent GvHD but preserves memory cells would provide immediate functional T cells with anti-infection, anti-leukemia22, and anti-rejection effects weeks to months before de novo T-cell development.23, 24 One such technique is selective depletion of the CD45RA+ subset.25, 26 CD45, also called leukocyte common antigen, is expressed on all white cell lineages. Naïve T cells express CD45RA, until exposure to its cognate antigen, when there is a switch to the CD45RO isoform.27
Herein, we describe the results of CD45RA+ cell depletion of haploidentical donor grafts and early immune reconstitution in patients with poor-prognosis hematologic malignancies. We found reliable engraftment with promising early memory T-cell reconstitution and a low rate of acute GvHD.
Methods
Patient Selection
Patients with a poor-prognosis hematologic malignancy for which HCT is indicated, or with chemotherapy-refractory leukemia, who lack an available suitable HLA-matched related or unrelated donor, and have a KIR receptor-ligand mismatched haploidentical donor, are offered enrollment on this research protocol. Additional eligibility criteria include left ventricular ejection fraction >40%, creatinine clearance ≥50 ml/min/1.73m2, forced vital capacity ≥50% of predicted, performance score ≥50, total bilirubin ≤3 times the upper limit of normal (ULN), and alanine aminotransferase ≤5 ULN. The protocol was approved by the St. Jude Children’s Research Hospital Institutional Review Board. The protocol is open under FDA approved IDE for the use of the CliniMACS device. Written informed consent was obtained from the patient, parent or guardian, and assent from the patient, as appropriate. This trial is registered at ClinicalTrials.gov, Identifier:NCT01807611. The first 17 consecutive treated patients are presented in this study.
Treatment
Recipients received a preparative regimen that consisted of 8 Gy total lymphoid irradiation (TLI) over 4 equal fractions, 150mg/m2 fludarabine divided daily over 5 days, a single dose of cyclophosphamide at 60mg/kg, thiotepa 10mg/kg divided twice daily for one day, and melphalan 140mg/m2 divided daily over two days. On Day 0, the patients received their first hematopoietic progenitor cell graft (HPC), which was CD34+ enriched. The following day, they received a second HPC that was CD45RA-depleted. On Day +6, they received an NK cell infusion from the HPC donor. G-CSF was started Day +7. Sirolimus (n=9) or mycophenolate mofetil (MMF) (n=8) was started one week following NK cell graft infusion, with plans to stop before Day +60 if absence of circulating naïve T cells was confirmed.
Graft Preparation
HPCs were obtained via G-CSF mobilization of the haploidentical donor, and collection by leukapheresis on day 5 and 6 of G-CSF. The first HPC product collected on day 5 was T-cell-depleted using the CliniMACS device and CD34 Microbead (Miltenyi Biotec, Auburn, CA, USA). Minimum cell dose required for the CD34+ enriched progenitor cell graft was 2 × 106 CD34+ cells/kg. Maximum CD3+ dose allowed for the CD34+ enriched HPC was 0.1 × 106 CD3+ cells/kg.
The HPC product collected on day 6 was processed for CD45RA+ cell depletion using the CliniMACS device and its “Depletion 3.1” software. There was no target CD34+ dose or CD3+ dose on the CD45RA+ depleted product; however release criteria of the product includes a ≥2 log10 depletion of CD45RA+ cells. Two of the 17 patients did not meet the minimum CD45RA depletion after a single depletion step. Per standard operating procedure, a second run under the same conditions was performed and the requisite level of depletion was achieved in both products.
The NK cell product was collected by leukapheresis 5 days after the second HPC collection. It was a nonmobilized product, and was processed on the CliniMACS device as previously described.28, 29 All three cell products were infused fresh.
Post-transplant evaluations
Outcomes are censored as of October 29, 2014. Complete blood counts were performed daily until neutrophil engraftment. Chimerism studies were performed weekly on peripheral blood by variable number tandem repeat analysis until Day +100 and then monthly. Patients were monitored at least weekly for the first 100 days for CMV, EBV, and adenoviral viremia by PCR. Patients who received treatment for viral infection or reactivation were captured. Flow cytometry quantification of lymphocyte subsets, and lymphocyte response to mitogens were performed at Day +30, +60, +100, and +180, and TREC and Vβ spectratyping were performed at Day +100 in all patients who were alive without relapse.
Flow cytometry
Flow cytometry analysis was performed to quantify lymphocyte subsets on BD LSR II flow cytometer with BD FACS DIVA software (BD Biosciences, Heidelberg, Germany). The following antibodies were used for phenotypic analysis: CD45-FITC, CD19/20-PE, CD14-Cy-7, CD25-FITC, CD127-PE, CD45RA-APC, CD3-APC Cy-7, CD8-FITC, CD4-PE, CD4-APC Cy7, CD8-APC Cy7, CD62L-FITC, CCR7-PE, CD27-FITC, CD62L-PE, (Beckton Dickinson, Franklin Lakes, NJ, USA), CD3-ECD, CD56-APC, CD45RO-ECD (Beckman Coulter, Miami, FL, USA).30
TCR β chain CDR3 spectratyping
TCR Vβ CDR3 size spectratyping was performed by RT-PCR with 25 forward TCR Vβ subfamily–specific primers and a FAM-labeled reverse Cβ primer as described previously.31, 32 Denatured PCR products were electrophoresed and analyzed using 3130xl Genetic Analyzer (Applied Biosystems, Foster City, CA). Spectratype complexity score is calculated as the summation of number of subfamilies (i.e. 25) per score with a maximum possible score of 200 (8 peaks for each family and 25 families; 8 × 25 = 200).
Quantification of Single-Joint TREC
Quantification of sj-TREC was performed by real-time PCR using 7900HT Fast Real-time PCR system. sj TREC and Cα pDNA were made as previously described.33 TREC copies per milliliter blood were reported.
Lymphocyte proliferation assay and alloreactivity
Antigen-specific and mitogen-activated lymphocyte proliferation assay was performed using the DELFIA Cell Proliferation Kit (PerkinElmer Life Sciences, Turku, Finland). The following antigens and mitogen were used: CMV purified lysate, and HSV purified lysate 0.1 μg /ml (Advanced Biotechnologies Inc., Columbia, MD, USA); Tetanus Toxoid 1 μg/ml (Sanofi Pasteur Inc., Swiftwater, PA,USA); and PHA 1 μg/ml (Sigma, St. Louis, MO, USA). 100 μl of antigen/mitogen and 1×105 cells were dispensed to each well in the 96 well plate. The antigen/mitogen stimulated cells were incubated at 37°C in 5% CO2 for 96 hours. On day 5, the stimulated cells were labeled by Brdu solution followed by developing the Eu-fluorescence as the manufacturer’s instruction and measured the Eu-fluorescence counts using Victor2 1420 multilabel counter (PerkinElmer Life Sciences, Turku, Finland). Eu-Fluorescence Counts were reported.
CD45RA+ or CD45RA- fractions from healthy donors were stimulated in mixed leukocyte reaction (MLR) at 1:1 ratio with irradiated (30Gy) allogeneic PBMCs derived from other healthy donors for 96 hours. DELFIA Cell Proliferation Kit (PerkinElmer Life Sciences, Turku, Finland) was used to measure T-cell-mediated alloreactivity as the manufacture’s instruction. Eu-Fluorescence Counts were reported.
Statistical analysis
Summary statistics including median and range for continuous variables and frequency for categorical variables were provided. The cumulative incidences of cell recovery, acute GVHD, full donor chimerism, relapse, transplant related mortality (TRM) were estimated using the Kalbfleisch and Prentice method, adjusting for competing risk factors. The cumulative incidence (CI) of an event was defined as the time from transplantation until event, censoring those without events at last follow-up. In the estimation of CI of cell recovery, acute GVHD, full donor chimerism and relapse, TRM was considered a competing event. In the estimation of CI of TRM, relapse was considered a competing event.
Results
Patients
Seventeen consecutive patients have received transplantation and are at least 100 days post-transplantation at the time (October 29, 2014) the data was frozen for analyses. Sixteen patients had acute leukemia, of which 10 had detectable disease (2 in morphologic remission with molecularly detectable disease, 8 with active disease - median 19%) at the time of HCT. One patient had therapy-related myelodysplastic syndrome with some response (blasts <5%) to hypomethylation chemotherapy.(Table 1) All received three parental haploidentical donor-cell products. The first product was given as a primary source of hematopoietic progenitor cells. It was CD34+ enriched, and provided a median CD34+ and CD3+ dose of 11.2 (range 2.0 to 38.4) and 0.012 (range 0.002 to 0.088) ×106/kg, respectively.
Table 1.
Patient Summary (n=17)
| Age | ||
|---|---|---|
| Median (range); years | 7.7 | (0.6-20.3) |
| Weight | ||
| Median (range); kg | 24.5 | (6.4-158) |
| Sex | ||
| Male | 11 | (65%) |
| Female | 6 | (35%) |
| Race | ||
| Caucasian | 7 | (41%) |
| Non-Caucasian | 10 | (59%) |
| Hispanic | 6 | |
| African American | 3 | |
| Mix (Asian/Hispanic) | 1 | |
| Disease | ||
| Acute Lymphoblastic Leukemia | 6 | (35%) |
| B cell | 4 | |
| T cell (early T-cell precursor) | 2 | |
| Acute Myeloid Leukemia | 9 | (53%) |
| de novo | 7 | |
| Therapy-related | 1 | |
| Myeloid sarcoma | 1 | |
| Mixed Lineage Leukemia | 1 | (6%) |
| Myelodysplastic Syndrome | 1 | (6%) |
| Therapy-related | 1 | |
| Disease Stage | ||
| CR1 | 5 | (29%) |
| Detectable disease | 1 | |
| Subsequent CR | 3 | (18%) |
| Detectable disease | 1 | |
| Active Relapse | 3 | (18%) |
| Induction Failure | 4 | (24%) |
| Refractory Anemia | 1 | (6%) |
| Untreated | 1 | (6%) |
| HLA match status | ||
| 4 of 8 | 13 | (76%) |
| 5 of 8 | 3 | (18%) |
| 6 of 8 | 1 | (6%) |
| CMV status (Donor/Patient) | ||
| Negative/Negative | 1 | (6%) |
| Positive/Positive | 8 | (47%) |
| Positive/Negative | 4 | (24%) |
| Negative/Positive | 4 | (24%) |
CD45RA+ cell depletion
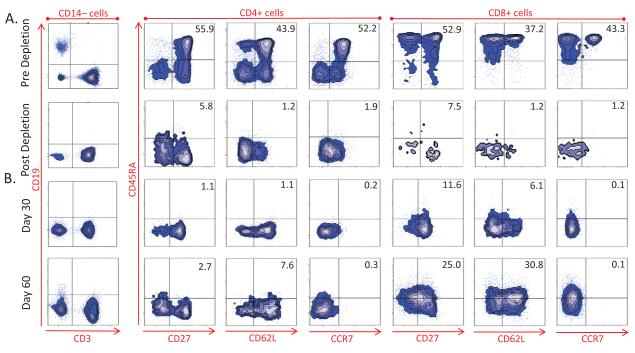
The second product was provided to adoptively transfer a large number of donor memory T cells and additional progenitor cells. The median pre- and post-processing values for the CD45RA-depleted progenitor cell grafts are detailed in Table 2. After processing, the CD34+ cell dose was a median of 6.4 (range 1.7 to 31.6) ×106/kg, and the median recovery of CD34+ cells post-processing was 59.6%. Thus, the combined CD34+ cell dose of the two progenitor cell grafts was a median of 17.8 (range 3.6 to 67.5) ×106/kg. After CD45RA+ cell depletion, the CD3+ cell dose was a median of 121.8 (range 23.6 to 528.4) ×106/kg. The CD3+CD45RA+ cell dose was a median of <0.001 (range <0.001 to 0.128) ×106/kg. The median log10 depletion of CD45RA+ cells was 3.6 (range 2.3 to 3.95), and the median log10 depletion of CD3+CD45RA+ cells was >5.23 (range 2.35 to >6.10). The CD19+ cell dose was a median of 0.15 (range 0.02 to 2.7) ×106/kg. Figure 1A shows representative flow cytometry from pre- and post-processing – demonstrating profound depletion of CD45RA+ T cells and B cells. Post-processing samples from the CD45RA+ fraction and CD45RA-depleted fraction were assessed immunologically for the first two donor grafts. In comparison to CD45RA+ cells, in both cases the CD45RA– sample demonstrated superior proliferative responses to antigens (CMV, EBV, HSV, tetanus), similar response to mitogen (PHA), and reduced proliferation in a MLR assay against third-party cells.(Supplemental Figure 2)
Table 2.
Cell counts before and after CD45RA+ cell depletion and NK-cell enrichment respectively. (n=17) (Median Values)
| Pre-Processing | Post-Processing | Recovery | Log Depletion | |
|---|---|---|---|---|
| CD45RA-Depleted Product | ||||
| TNC (×108/kg) | 19.43 | 5.42 | ||
| CD34+ (×106/kg) | 11.72 | 6.38 | 59.6% | |
| CD3+ (×106/kg) | 468.85 | 121.78 | 0.58 | |
| CD45RA+ (×106/kg) | 626.04 | 0.26 | 3.57 | |
| CD3+ CD45RA+ (×106/kg) | 205.57 | <0.001 | >5.23 | |
| CD19+ (×106/kg) | 101.60 | 0.15 | 2.63 | |
| CD3−CD56+ (×106/kg) | 69.05 | 3.53 | 6.31% | |
| NK-cell Enriched Product | ||||
| TNC (×108/kg) | 3.72 | 0.14 | ||
| CD3−CD56+ (×106/kg) | 32.27 | 13.11 | 40.6% | |
| CD3+ (×106/kg) | 235.74 | 0.01 | 4.10 | |
| CD3+CD56−(×106/kg) | 202.03 | <0.01 | >4.16 | |
| CD19+ (×106/kg) | 49.04 | 0.04 | 3.09 | |
Figure 1.
Flow cytometry evaluation of CD45RA-depleted product and lymphocyte reconstitution on Day 30 and Day 60
Representative evaluation of samples from patient 6 (the patient with median tempo of immune cell reconstitution). Gates were set for CD14–, CD4+, or CD8+ cells as indicated at the top of the panels. See supplemental figure 1 for post-transplant flow cytometry gating strategies from a representative umbilical cord blood recipient.
NK-cell Enrichment
The third and final donor cell product was given to provide additional donor NK cells in the early post-transplant period. The median pre- and post-processing values for the NK-cell enriched grafts are detailed in Table 2. These products were highly purified for NK cells, with a median CD3-CD56+ cell purity of 96.4%. The median NK-cell dose was 13.11 (range 1.65 to 56.10) ×106/kg. After processing, the CD3+CD56– T-cell dose was a median of <0.01 (range <0.01 to 0.01) ×106/kg. The median log10 depletion of CD3+CD56– cells was >4.16. The CD19+ cell dose was a median of 0.04 (range <0.01 to 1.07) ×106/kg.
Outcomes
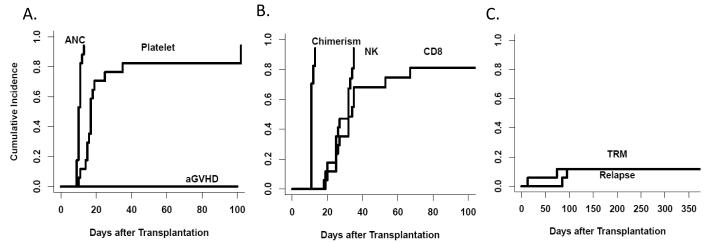
All patients achieved neutrophil engraftment at a median of 10 (range 9 to 13) days post-transplant.(Figure 2) The median time to platelet engraftment was 17 (range 10-102) days post-transplant. The median time to 100% donor chimerism was Day +11. One patient (UPN 14) experienced a post-engraftment fall in donor chimerism in conjunction with the development of anti-D antibodies (Donor O+, Recipient O-). He was successfully returned to 100% donor with G-CSF-mobilized DLI.
Figure 2.
Engraftment, immune recovery, and outcomes
(A)Time to neutrophil engraftment (ANC >500/μL), platelet engraftment (>20 × 109/L), and onset of acute GvHD. (B)Time to full donor chimerism, normalization of NK cell or CD8+ T cell counts. (C) Time to relapse or transplant-related mortality (TRM).
To date, three patients have received anti-viral treatment for CMV reactivation. None have progressed to CMV disease, and all cleared CMV viremia without donor lymphocyte infusion (DLI). One patient received anti-viral treatment for adenoviral viremia. That patient developed hemorrhagic cystits with urine positive for adenovirus, which resolved without DLI. No patient has developed post-transplant lymphoproliferative disease nor have any received treatment for EBV reactivation. One patient experienced HSV reactivation, with oral HSV occurring prior to engraftment and resolving within two weeks. Other significant viral infections which occurred include four cases of community acquired rotavirus and one case of community acquired influenza A. No patient has died with a viral infection.
Thirteen patients (76.5%) remain alive at a median of 223 (range 174 to 469) days post-transplant. One patient died suddenly with arrhythmia on Day +13, and another of culture negative acute respiratory distress syndrome on Day +74. Two patients have relapsed, and both subsequently died with progressive disease.(Table 3)
Table 3.
Detailed Patient Summary
| UPN | Disease | Stage | Pre-HCT disease burden¥ |
Combined cell dose(×106/kg)* |
Day to ANC >500 |
Day to plt >20k |
PB Chimerism %donor d+30 |
Lymphocytes (d+30)‡ | Outcome | (day) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CD34+ | CD3+ | CD19+ | B | T4 | T8 | NK | |||||||||
| 1 | AML | PIF | 3% (a) | 7.62 | 45.9 | 0.07 | 13 | NA | 100 | <10 | 60 | 300 | 150 | Relapse | 95 |
| 2 | B ALL | Relapse 1 | 73% | 17.11 | 215.5 | 0.48 | 12 | NE | NE | NE | NE | NE | NE | TRM | 13 |
| 3 | t-AML | CR1 | 0.01% | 6.66 | 55.9 | 0.24 | 11 | 16 | 100 | <10 | 100 | 310 | 90 | Alive CR | 469 |
| 4 | B ALL | CR2 | <0.01% | 10.56 | 26.6 | 0.69 | 10 | 17 | 99-100 | <10 | 190 | 590 | 130 | Alive CR | 442 |
| 5 | AML, M7 | PIF | 2.3% (c) | 28.97 | 121.8 | 0.09 | 10 | 17 | 100 | <10 | 80 | 200 | 120 | Relapse | 85 |
| 6 | ETP ALL | CR1 | <0.01% | 14.17 | 99.2 | 0.33 | 11 | 14 | 100 | <10 | 190 | 280 | 350 | Alive CR | 433 |
| 7 | Infant ALL | PIF | 0.04% (a) | 51.64 | 528.5 | 3.15 | 9 | 102 | 100 | <10 | 100 | 300 | 190 | Alive CR | 419 |
| 8 | AML, M5 | Relapse 1 | 3.9% (a) | 10.86 | 57.1 | 0.13 | 10 | 18 | 100 | <10 | 320 | 320 | 260 | Alive CR | 363 |
| 9 | AML, M0 | PIF | 71% | 18.77 | 133.6 | 0.63 | 11 | 15 | 100 | <10 | 180 | 790 | 120 | TRM | 74 |
| 10 | t-MDS | RA | 2% | 35.10 | 99.21 | 0.82 | 10 | 15 | 100 | <10 | 130 | 140 | 230 | Alive CR | 272 |
| 11 | AML, MLL+ | CR1 | <10−4 (p) | 23.81 | 269.21 | 0.81 | 9 | 17 | 100 | <10 | 140 | 800 | 110 | Alive CR | 223 |
| 12 | ETP ALL | CR1 | <0.01% | 13.82 | 31.52 | 0.34 | 10 | 19 | 100 | <10 | 310 | 30 | 160 | Alive CR | 216 |
| 13 | AML, FLT3+ | Relapse 2 | 34% | 17.8 | 200.44 | 0.54 | 12 | 25 | 100 | <10 | 180 | 420 | 190 | Alive CR | 209 |
| 14 | MS, 7− | untreated | 75% (f) | 67.55 | 199.48 | 1.82 | 11 | 10 | 56 | 10 | 10 | 80 | 0 | Alive CR | 204 |
| 15 | AML | CR2 | unavailable | 25.96 | 122.08 | 0.87 | 10 | 17 | 100 | <10 | 590 | 130 | 180 | Alive CR | 188 |
| 16 | Mix lineage | CR1 | <10−4 (p) | 23.43 | 234.05 | 0.60 | 9 | 11 | 100 | <10 | 490 | 800 | 110 | Alive CR | 181 |
| 17 | B ALL | CR3 | 0.06% | 3.63 | 23.58 | 0.10 | 11 | 35 | 100 | <10 | 90 | 100 | 310 | Alive CR | 174 |
Values per flow cytometry minimal residual disease (MRD) testing unless otherwise noted: (p)=quantitative PCR, (f)=FISH, (a)=aplastic marrow, (c)=clusters of disease apparent
Total cell dose for progenitor cell grafts (CD34+ selected and CD45RA-depleted), NK infusion not included
Values listed are cells/μL; normal values based on 57 healthy children 1 − 18y: B(Bcells)=100-1620, T4(CD4+Tcells)=550-2150, T8(CD8+Tcells)=200-1400, NK(NK cells)=100-750; or based on 38 healthy adults 18 − 58y: B(Bcells)=100-770, T4(CD4+Tcells)=450-2500, T8(CD8+Tcells)=210-1300, NK(NK cells)=50-450
UPN=unique patient number, AML=acute myeloid leukemia, ALL=acute lymphoblastic leukemia, t-AML=therapy-related AML, ETP=early T-cell precursor, MS=myeloid sarcoma, PIF=primary induction failure, CR=complete remission, kg=kilogram, ANC=absolute neutrophil count, NA=not achieved, NE=not evaluable because patient expired day +13
No patient has developed acute GvHD. Six patients have presented with clinical features of chronic oral GvHD, and 3 of the 6 also had skin findings. Five patients experienced resolution with topical therapy alone. One patient had progression despite topical therapy, responded rapidly to tacrolimus and oral corticosteroid, and is now quiescent on weaning low dose prednisone. No patient has developed severe34 chronic GvHD.
*A comprehensive review of enrolled subjects by internal and extramural experts concluded that three of the 17 patients had clinical findings consistent with acute GvHD⩾grade III. The authors agree with this independent consensus and thus, the incidence of grade III/IV acute GvHD should be reported as 17.6%, rather than zero.
Quantitative Lymphocyte Reconstitution
Quantitative values for NK cells and CD8+ T cells rapidly reached normal values in the peripheral blood.(Figure 2) At Day +30, 11 of the 16 surviving patients had normal number of CD8+ T cells and 15 had a normal number of NK cells.(Table 3) CD4+ T cells reconstituted to a median of 160 cells/μL at Day +30. As expected, B cells were virtually absent in the peripheral blood due to effective B cell depletion.
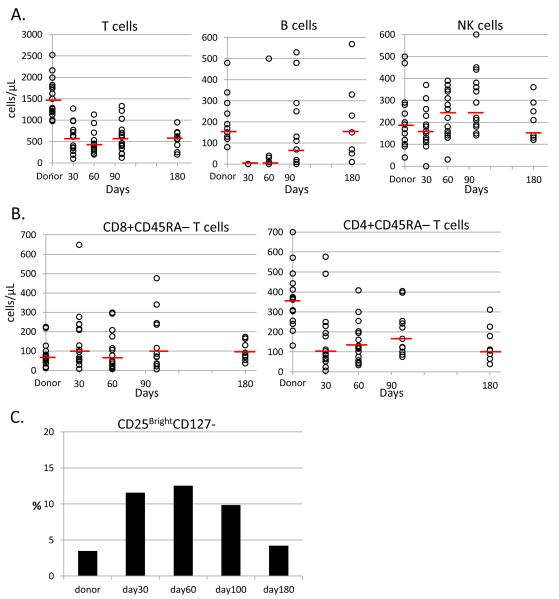
Figure 3 further details lymphocyte subset recovery. By Day +30, a majority of patients demonstrated a substantial number of both CD8+CD45RA– and CD4+CD45RA– memory T cells.(Figure3B) There was no sign of exhaustion, as the number of memory cells in both CD4+ and CD8+ subsets remained stable during the six-month observation period. The proportion of regulatory T cells (CD25brightCD127–) in the CD4+ T-cell fraction was high in the early post-transplant period, before returning to donor level.(Figure 3C) In the first 100 days after transplantation, we confirmed that there was a paucity of all naïve T-cell subsets (CD27+CD45RA+; CD62L+CD45RA+; and particularly the most naïve population CCR7+CD45RA+).(Figure 3D-F) Thus, the distribution of T-cell subsets recapitulated the CD45RA-depleted graft composition(Figure 1A). These data suggest that the T cells present in the early post-transplant period were adoptively transferred rather than stem-cell derived.(Figure1B)
Figure 3.
Quantitative subset analysis
Values are from all patients who were alive without relapse at each time point. Data from donors are prior to G-CSF mobilization. (A) Absolute number of T, B, and NK-lymphocytes, red line denotes median value. (B) Absolute number of CD8+CD45RA– and CD4+CD45RA– memory T cells, red line denotes median value. (C) Median percentage of CD25brightCD127− regulatory T cells in the CD3+CD4+ fraction. (D-F) Average proportion of the following subsets: effector memory T cells (CD45RA−CD27−, CD45RA− CCR7−, or CD45RA−CD62L−); central memory T cells (CD45RA−CD27+, CD45RA−CCR7+, or CD45RA−CD62L+); terminal effector memory RA+ cells (CD45RA+CD27−, CD45RA+CCR7−, or CD45RA+CD62L−); and naïve T cells (CD45RA+CD27+, CD45RA+CCR7+, or CD45RA+CD62L+)
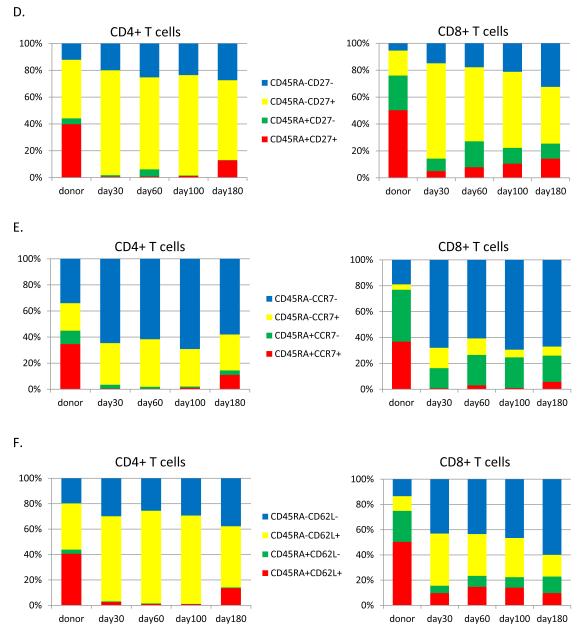
Early Lymphocyte Function and T-cell receptor (TCR) repertoire
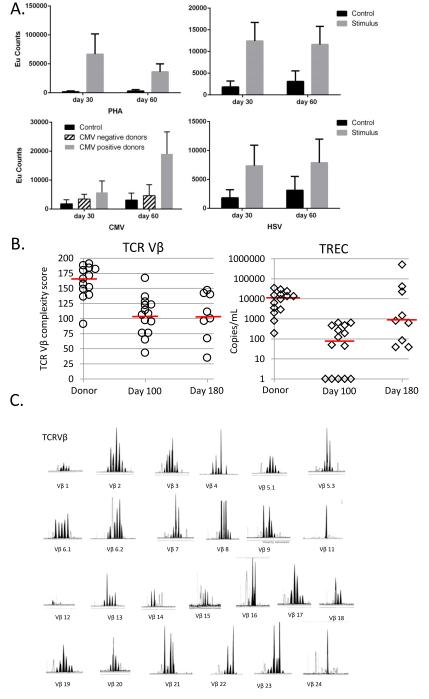
The proliferative response to PHA, tetanus toxoid, CMV, and HSV lysates was robust as early as Day +30.(Figure 4A) TREC and Vβ spectratyping were available in all 100-day survivors.(Figure 4B) All demonstrated low TREC copy numbers, whereas the patients consistently demonstrated a good Vβ spectratyping complexity score at the same time point. These data indicate that broad TCR repertoire could be achieved with adoptively transferred memory cells before naïve thymic output. Figure 4C shows the Vβ spectratyping from the patient with the median Vβ spectratyping complexity score (106) at day +100.
Figure 4.
Functional and TCR studies
(A)Median lymphocyte proliferation as measured by Brdu incorporation at day +30 and +60 post-transplant. Patients with CMV seropositive and seronegative donors are presented separately. (B)TCR Vβ spectratyping score and TREC per mL of blood (log-scale) from all donors and patients who were alive without relapse at each time point, red line denotes median value. (C) Representative Vβ spectratyping from the patient with a median Vβ spectratyping score
Discussion
Adoptive transfer of CD45RA-depleted T cells and enriched NK cells in conjunction with CD34+ selected haploidentical HPCs, infused after a novel reduced intensity conditioning regimen without antibody or total body irradiation (TBI), is feasible and well tolerated in our patients with very high-risk leukemia. The first 17 consecutive patients on this study represent a very poor prognosis population of heavily pre-treated patients. All patients achieved rapid donor neutrophil engraftment, and no patient has developed acute GvHD. Tolerability is acceptable, with only two patients experiencing TRM. Importantly, no TRM was associated with infection, which is atypical in HLA-mismatched HCT. Two patients have experience relapse of their disease, and the remaining 13 patients remain alive at a median of Day +223, all in molecular remission. Continued accrual and follow-up is needed to assess long term clinical outcomes.
Profound depletion of CD45RA+ T cells was reliably obtained in all products, with a median CD3+CD45RA+ cell dose of <103/kg. Thus, despite the infusion of a median of >100 million haploidentical T cells/kg, no patient developed acute GvHD. In addition, the majority of the pre-processing CD34+ cell population was preserved after CD45RA+ cell depletion, allowing a large progenitor cell dose to be given to all patients concurrent with the memory cell transfer. The B cell content was also substantially depleted in all grafts, abrogating the need for additional ex vivo or in vivo B cell depletion for the prevention of EBV-LPD. The processing of NK cell products was similarly successful in all cases, with minimal T and B-cell content. Collectively, infusions of the three haploidentical products were well tolerated and patients have so far experienced low rates of rejection, infection, acute GvHD, and relapse - the most common serious side effects seen early after allogeneic transplantation.
Assessment of immune reconstitution in the early post-transplant period after adoptive transfer of donor NK cells and CD45RA-depleted cells demonstrated robust reconstitution of innate and memory immunity. There is a rapid reconstitution of NK cells and CD8+ T cells to quantitatively normal values, and a substantial number of CD4+ T cells are already present by Day +30. It is clear that early post-transplant T-lymphocyte subset distribution recapitulates the CD45RA-depleted graft composition, confirming successful adoptive transfer of balanced memory T-cell populations. Both effector memory T cells and central memory T cells are present and sustainable in numbers for up to 6 months after transplantation in both the CD4+ and CD8+ T-cell populations, providing critical protection against infections before stem cell-derived thymic output. A high proportion of regulatory T cells were present early, and naïve T cells were virtually absent. This allowed successful discontinuation of GvHD prophylaxis by Day +60 without acute GvHD. Some patients have developed mild chronic GvHD, and it has predominately been responsive without the need for systemic therapy.
In addition to the rapid quantitative reconstitution of NK cells and memory T cells, early functional recovery was confirmed as well. Proliferative responses to mitogen and antigens are uniformly recovered between Day +30 and +60. There has been no development of significant CMV and EBV disease. Additionally, only one infection each from adenovirus and HSV has occurred. Although follow-up remains short, the control of HSV, CMV, EBV, and adenoviral reactivation appears much better than expected compared to our prior experience.35
By Day +100 after transplantation, patients uniformly demonstrated low level TREC production, but all (including those with no evidence of thymic output) demonstrated substantial V Beta spectratyping diversity. These TCR data, in combination with the predominant CD45RO+ phenotypes, support the hypothesis that the T-cell immunity in the first months after HCT was provided by successful adoptive transfer from the CD45RA-depleted grafts.
The use of HLA-mismatched donor, such as haploidentical donors, is frequently associated with an increased risk of graft failure. Some investigators use TBI to provide high level of immuno- and myeloablation.3, 10 However, TBI is associated with many short term and long term toxicities.36-38 Lymphodepleting antibodies are also often utilized to facilitate donor engraftment and reduce GvHD.18, 39 However, these agents have a long half-life and typically lengthen the time to donor lymphocyte reconstitution.40, 41 TLI has been utilized in reduced intensity regimens, and it has been associated with good engraftment, low GvHD, and low toxicity.42-44 In this study, the novel TLI-based reduced intensity preparative regimen has allowed patients to avoid TBI and anti-T cell antibody therapy, yet rapidly achieved neutrophil engraftment with full donor chimerism in all patients.
Although this regimen shows promise, there is substantial cost and complexity inherent in the utilization of three manipulated donor products. A cost and bed-utility analysis is underway to assess whether the short hospital stay and low cost in GvHD and infection control outweigh the cost of donor cell processing and allow more transplantations per transplant bed. If the high rate of engraftment seen to date is confirmed with additional patients, megadose of progenitor cells45 as utilized here, may not be required in the presence of a large memory T-cell fraction.
In conclusion, this treatment regimen demonstrated acceptable tolerability in heavily pretreated patients with poor-prognosis hematologic malignancy. CD45RA+ cell depletion and NK cell enrichment were reliable and effective procedures, providing therapeutic cell products that contain extremely low number of B and naïve T cells, but abundant memory T cells and NK cells. Complete donor engraftment was reliably achieved, with rapid normalization of neutrophil, NK cell, and CD8+ T cell counts. Early memory T-cell quantification and functional parameters are promising. There was also a low rate of acute GvHD and transplant related mortality with no infection-related deaths.
Supplementary Material
Acknowledgements
The authors would like to thank our colleagues for data collection and clinical management. Our thanks also go out to the many patients and families who participated in the transplantation and cellular therapy research program.
Support: This work is supported in part by the National Institutes of Health Cancer Center Support (CORE) grant P30 CA021765, the Assisi Foundation of Memphis, the Press On Fund, and the American Lebanese Syrian Associated Charities (ALSAC).
Footnotes
COI/Disclosure: The authors have no financial relationships or other conflicts of interest to disclose relevant to this manuscript. No author received an honorarium, grant, or other form of payment to produce the manuscript.
Authorship: B.M.T. and W.L. designed the research, analyzed and interpreted data, and wrote the manuscript; B.M.T., D.R.S., P.E., M.D., C.H., A.S., H.I., C.H.P., and W.L. provided study material and patient information and contributed to the interpretation of the data; G.K. provided statistical analysis; P.E., Y.L., W.K.C., and D.S. collected and performed laboratory analysis; and all authors contributed to the revisions of the draft and approval of the final manuscript.
Supplementary information is available at BMT’s website
References
- 1.Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354(17):1813–26. doi: 10.1056/NEJMra052638. [DOI] [PubMed] [Google Scholar]
- 2.Gragert L, Eapen M, Williams E, Freeman J, Spellman S, Baitty R, et al. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N Engl J Med. 2014;371(4):339–48. doi: 10.1056/NEJMsa1311707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marks DI, Aversa F, Lazarus HM. Alternative donor transplants for adult acute lymphoblastic leukaemia: a comparison of the three major options. Bone Marrow Transplant. 2006;38(7):467–75. doi: 10.1038/sj.bmt.1705464. [DOI] [PubMed] [Google Scholar]
- 4.Ballen KK, Koreth J, Chen YB, Dey BR, Spitzer TR. Selection of optimal alternative graft source: mismatched unrelated donor, umbilical cord blood, or haploidentical transplant. Blood. 119(9):1972–80. doi: 10.1182/blood-2011-11-354563. [DOI] [PubMed] [Google Scholar]
- 5.Brunstein CG, Fuchs EJ, Carter SL, Karanes C, Costa LJ, Wu J, et al. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood. 118(2):282–288. doi: 10.1182/blood-2011-03-344853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martelli MF, Di Ianni M, Ruggeri L, Pierini A, Falzetti F, Carotti A, et al. ”Designed” grafts for HLA-haploidentical stem cell transplantation. Blood. 2014;123(7):967–73. doi: 10.1182/blood-2013-10-531764. [DOI] [PubMed] [Google Scholar]
- 7.Oevermann L, Michaelis SU, Mezger M, Lang P, Toporski J, Bertaina A, et al. KIR B haplotype donors confer a reduced risk of relapse after haploidentical transplantation in children with acute lymphoblastic leukemia. Blood. 2014 doi: 10.1182/blood-2014-03-565069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Handgretinger R. Negative depletion of CD3(+) and TcRalphabeta(+) T cells. Curr Opin Hematol. 2012;19(6):434–9. doi: 10.1097/MOH.0b013e3283582340. [DOI] [PubMed] [Google Scholar]
- 9.Schumm M, Lang P, Bethge W, Faul C, Feuchtinger T, Pfeiffer M, et al. Depletion of T-cell receptor alpha/beta and CD19 positive cells from apheresis products with the CliniMACS device. Cytotherapy. 2013;15(10):1253–8. doi: 10.1016/j.jcyt.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Aversa F, Tabilio A, Velardi A, Cunningham I, Terenzi A, Falzetti F, et al. Treatment of high-risk acute leukemia with T-cell-depleted stem cells from related donors with one fully mismatched HLA haplotype. N Engl J Med. 1998;339(17):1186–93. doi: 10.1056/NEJM199810223391702. [DOI] [PubMed] [Google Scholar]
- 11.Leung W, Campana D, Yang J, Pei D, Coustan-Smith E, Gan K, et al. High success rate of hematopoietic cell transplantation regardless of donor source in children with very high-risk leukemia. Blood. 2011;118(2):223–30. doi: 10.1182/blood-2011-01-333070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klingebiel T, Cornish J, Labopin M, Locatelli F, Darbyshire P, Handgretinger R, et al. Results and factors influencing outcome after fully haploidentical hematopoietic stem cell transplantation in children with very high-risk acute lymphoblastic leukemia: impact of center size: an analysis on behalf of the Acute Leukemia and Pediatric Disease Working Parties of the European Blood and Marrow Transplant group. Blood. 2010;115(17):3437–46. doi: 10.1182/blood-2009-03-207001. [DOI] [PubMed] [Google Scholar]
- 13.Ciceri F, Labopin M, Aversa F, Rowe JM, Bunjes D, Lewalle P, et al. A survey of fully haploidentical hematopoietic stem cell transplantation in adults with high-risk acute leukemia: a risk factor analysis of outcomes for patients in remission at transplantation. Blood. 2008;112(9):3574–81. doi: 10.1182/blood-2008-02-140095. [DOI] [PubMed] [Google Scholar]
- 14.Martelli MF, Di Ianni M, Ruggeri L, Falzetti F, Carotti A, Terenzi A, et al. HLA-haploidentical transplantation with regulatory and conventional T-cell adoptive immunotherapy prevents acute leukemia relapse. Blood. 2014;124(4):638–44. doi: 10.1182/blood-2014-03-564401. [DOI] [PubMed] [Google Scholar]
- 15.Bashey A, Zhang X, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013;31(10):1310–6. doi: 10.1200/JCO.2012.44.3523. [DOI] [PubMed] [Google Scholar]
- 16.Wang Y, Chang YJ, Xu LP, Liu KY, Liu DH, Zhang XH, et al. Who is the best donor for a related HLA haplotype-mismatched transplant? Blood. 2014;124(6):843–50. doi: 10.1182/blood-2014-03-563130. [DOI] [PubMed] [Google Scholar]
- 17.Di Bartolomeo P, Santarone S, De Angelis G, Picardi A, Cudillo L, Cerretti R, et al. Haploidentical, unmanipulated, G-CSF-primed bone marrow transplantation for patients with high-risk hematologic malignancies. Blood. 2013;121(5):849–57. doi: 10.1182/blood-2012-08-453399. [DOI] [PubMed] [Google Scholar]
- 18.Lu DP, Dong L, Wu T, Huang XJ, Zhang MJ, Han W, et al. Conditioning including antithymocyte globulin followed by unmanipulated HLA-mismatched/haploidentical blood and marrow transplantation can achieve comparable outcomes with HLA-identical sibling transplantation. Blood. 2006;107(8):3065–73. doi: 10.1182/blood-2005-05-2146. [DOI] [PubMed] [Google Scholar]
- 19.Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14(6):641–50. doi: 10.1016/j.bbmt.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brunstein CG, Fuchs EJ, Carter SL, Karanes C, Costa LJ, Wu J, et al. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood. 2011;118(2):282–8. doi: 10.1182/blood-2011-03-344853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krenger W, Blazar BR, Hollander GA. Thymic T-cell development in allogeneic stem cell transplantation. Blood. 2011;117(25):6768–76. doi: 10.1182/blood-2011-02-334623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zheng H, Matte-Martone C, Li H, Anderson BE, Venketesan S, Sheng Tan H, et al. Effector memory CD4+ T cells mediate graft-versus-leukemia without inducing graft-versus-host disease. Blood. 2008;111(4):2476–84. doi: 10.1182/blood-2007-08-109678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andre-Schmutz I, Dal Cortivo L, Fischer A, Cavazzana-Calvo M. Improving immune reconstitution while preventing GvHD in allogeneic stem cell transplantation. Cytotherapy. 2005;7(2):102–8. doi: 10.1080/14653240510027118. [DOI] [PubMed] [Google Scholar]
- 24.Chen BJ, Deoliveira D, Cui X, Le NT, Son J, Whitesides JF, et al. Inability of memory T cells to induce graft-versus-host disease is a result of an abortive alloresponse. Blood. 2007;109(7):3115–23. doi: 10.1182/blood-2006-04-016410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bleakley M, Heimfeld S, Jones LA, Turtle C, Krause D, Riddell SR, et al. Engineering human peripheral blood stem cell grafts that are depleted of naive T cells and retain functional pathogen-specific memory T cells. Biol Blood Marrow Transplant. 2014;20(5):705–16. doi: 10.1016/j.bbmt.2014.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Teschner D, Distler E, Wehler D, Frey M, Marandiuc D, Langeveld K, et al. Depletion of naive T cells using clinical grade magnetic CD45RA beads: a new approach for GVHD prophylaxis. Bone Marrow Transplant. 2014;49(1):138–44. doi: 10.1038/bmt.2013.114. [DOI] [PubMed] [Google Scholar]
- 27.Mahnke YD, Brodie TM, Sallusto F, Roederer M, Lugli E. The who’s who of T-cell differentiation: human memory T-cell subsets. European journal of immunology. 2013;43(11):2797–809. doi: 10.1002/eji.201343751. [DOI] [PubMed] [Google Scholar]
- 28.Iyengar R, Handgretinger R, Babarin-Dorner A, Leimig T, Otto M, Geiger TL, et al. Purification of human natural killer cells using a clinical-scale immunomagnetic method. Cytotherapy. 2003;5(6):479–84. doi: 10.1080/14653240310003558. [DOI] [PubMed] [Google Scholar]
- 29.Rubnitz JE, Inaba H, Ribeiro RC, Pounds S, Rooney B, Bell T, et al. NKAML: a pilot study to determine the safety and feasibility of haploidentical natural killer cell transplantation in childhood acute myeloid leukemia. J Clin Oncol. 2010;28(6):955–9. doi: 10.1200/JCO.2009.24.4590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leung W, Iyengar R, Triplett B, Turner V, Behm FG, Holladay MS, et al. Comparison of killer Ig-like receptor genotyping and phenotyping for selection of allogeneic blood stem cell donors. J Immunol. 2005;174(10):6540–5. doi: 10.4049/jimmunol.174.10.6540. [DOI] [PubMed] [Google Scholar]
- 31.Chan WK, Rujkijyanont P, Neale G, Yang J, Bari R, Das Gupta N, et al. Multiplex and genome-wide analyses reveal distinctive properties of KIR+ and CD56+ T cells in human blood. J Immunol. 2013;191(4):1625–36. doi: 10.4049/jimmunol.1300111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu CJ, Chillemi A, Alyea EP, Orsini E, Neuberg D, Soiffer RJ, et al. Reconstitution of T-cell receptor repertoire diversity following T-cell depleted allogeneic bone marrow transplantation is related to hematopoietic chimerism. Blood. 2000;95(1):352–9. [PubMed] [Google Scholar]
- 33.Leung W, Neale G, Behm F, Iyengar R, Finkelstein D, Kastan MB, et al. Deficient innate immunity, thymopoiesis, and gene expression response to radiation in survivors of childhood acute lymphoblastic leukemia. Cancer epidemiology. 2010;34(3):303–8. doi: 10.1016/j.canep.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11(12):945–56. doi: 10.1016/j.bbmt.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 35.Srinivasan A, Wang C, Srivastava DK, Burnette K, Shenep JL, Leung W, et al. Timeline, epidemiology, and risk factors for bacterial, fungal, and viral infections in children and adolescents after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2013;19(1):94–101. doi: 10.1016/j.bbmt.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rizzo JD, Curtis RE, Socie G, Sobocinski KA, Gilbert E, Landgren O, et al. Solid cancers after allogeneic hematopoietic cell transplantation. Blood. 2009;113(5):1175–83. doi: 10.1182/blood-2008-05-158782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Phipps S, Rai SN, Leung WH, Lensing S, Dunavant M. Cognitive and academic consequences of stem-cell transplantation in children. J Clin Oncol. 2008;26(12):2027–33. doi: 10.1200/JCO.2007.13.6135. [DOI] [PubMed] [Google Scholar]
- 38.Leung W, Ahn H, Rose SR, Phipps S, Smith T, Gan K, et al. A prospective cohort study of late sequelae of pediatric allogeneic hematopoietic stem cell transplantation. Medicine. 2007;86(4):215–24. doi: 10.1097/MD.0b013e31812f864d. [DOI] [PubMed] [Google Scholar]
- 39.Rizzieri DA, Koh LP, Long GD, Gasparetto C, Sullivan KM, Horwitz M, et al. Partially matched, nonmyeloablative allogeneic transplantation: clinical outcomes and immune reconstitution. J Clin Oncol. 2007;25(6):690–7. doi: 10.1200/JCO.2006.07.0953. [DOI] [PubMed] [Google Scholar]
- 40.Shah AJ, Kapoor N, Crooks GM, Weinberg KI, Azim HA, Killen R, et al. The effects of Campath 1H upon graft-versus-host disease, infection, relapse, and immune reconstitution in recipients of pediatric unrelated transplants. Biol Blood Marrow Transplant. 2007;13(5):584–93. doi: 10.1016/j.bbmt.2007.01.076. [DOI] [PubMed] [Google Scholar]
- 41.Call SK, Kasow KA, Barfield R, Madden R, Leung W, Horwitz E, et al. Total and active rabbit antithymocyte globulin (rATG;Thymoglobulin) pharmacokinetics in pediatric patients undergoing unrelated donor bone marrow transplantation. Biol Blood Marrow Transplant. 2009;15(2):274–8. doi: 10.1016/j.bbmt.2008.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kohrt HE, Turnbull BB, Heydari K, Shizuru JA, Laport GG, Miklos DB, et al. TLI and ATG conditioning with low risk of graft-versus-host disease retains antitumor reactions after allogeneic hematopoietic cell transplantation from related and unrelated donors. Blood. 2009;114(5):1099–109. doi: 10.1182/blood-2009-03-211441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kohrt H, Lowsky R. Total lymphoid irradiation for graft-versus-host disease protection. Curr Opin Oncol. 2009;21(Suppl 1):S23–6. doi: 10.1097/01.cco.0000357471.68713.35. [DOI] [PubMed] [Google Scholar]
- 44.Lowsky R, Takahashi T, Liu YP, Dejbakhsh-Jones S, Grumet FC, Shizuru JA, et al. Protective conditioning for acute graft-versus-host disease. N Engl J Med. 2005;353(13):1321–31. doi: 10.1056/NEJMoa050642. [DOI] [PubMed] [Google Scholar]
- 45.Aversa F, Terenzi A, Tabilio A, Falzetti F, Carotti A, Ballanti S, et al. Full haplotype-mismatched hematopoietic stem-cell transplantation: a phase II study in patients with acute leukemia at high risk of relapse. J Clin Oncol. 2005;23(15):3447–54. doi: 10.1200/JCO.2005.09.117. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.