Abstract
Objective
To conduct a meta-analysis summarizing the effectiveness of school-based brief alcohol interventions (BAIs) among adolescents, and to examine possible iatrogenic effects due to deviancy training in group-delivered interventions.
Method
A systematic search for eligible studies was undertaken, current through December 31, 2012. Studies were eligible for inclusion if they used an experimental/quasi-experimental design; focused on school-based BAIs; enrolled adolescent participants; and reported an alcohol-related outcome measure. Studies were coded for key variables, and outcome effect sizes were analyzed as standardized mean differences adjusted for small samples (Hedges’ g). Analyses were conducted using inverse-variance weighted mixed effects meta-regression models. Sensitivity analyses were also conducted.
Results
Across all 17 studies eligible for inclusion, school-based BAIs were associated with significant improvements among adolescents, whereby adolescents in the BAI groups reduced their alcohol consumption relative to the control groups (ḡ = 0.34, 95% CI [0.11, 0.56]). Subgroup analyses indicated that whereas individually-delivered BAIs were effective (ḡ = 0.58, 95% CI [0.23, 0.92]), there was no evidence that group-delivered BAIs were associated with reductions in alcohol use (ḡ = −0.02, 95% CI [−0.17, 0.14]). Delivery format was confounded with program modality, however, such that motivational enhancement therapy was the most effective modality, but was rarely implemented in group-delivered interventions.
Conclusions
Some school-based BAIs are effective in reducing adolescent alcohol consumption, but may be ineffective if delivered in group settings. Future research should explore whether group-delivered BAIs that use motivational enhancement therapy components may yield beneficial outcomes like those observed in individually-delivered programs.
Keywords: adolescents, brief alcohol interventions, meta-analysis, school-based prevention
Alcohol use and misuse among adolescents continues to remain a public health problem. Worldwide, an estimated 4% of 11 year olds, 8% of 13 year olds, and 21% of 15 year olds drink alcohol weekly; 14% of 15 year olds have been drunk at least once by the age of 13; and 32% of 15 year olds have been drunk at least twice (Currie et al., 2012). Early alcohol initiation and early or sustained heavy drinking among youth can lead to neurological damage (Hanson, Medina, Padula, Tapert, & Brown, 2011) and engagement in behaviors leading to reduced quality of life or premature death (Kandel, Davies, Karus, & Yamaguchi, 1986), such as dropping out of school (DuPont et al., 2013), taking sexual risks (Hipwell, Stepp, Chung, Durand, & Keenan, 2012), and accidents (National Institute on Alcohol Abuse and Alcoholism, n.d.). Given the magnitude of the problem and detrimental outcomes associated with alcohol use during adolescence, it is of little surprise that numerous preventive interventions exist to target adolescent alcohol use. Many of these interventions are delivered in schools, which offer a clear point of access to youth. Previous literature reviews and meta-analyses have illustrated that school-based prevention programs can be effective in preventing or delaying adolescent substance use, including alcohol use (Foxcroft & Tsertsvadze, 2011; Gottfredson & Wilson, 2003). Yet, despite numerous school-based prevention programs, uncertainty remains regarding what program dose and modality are effective in reducing adolescent alcohol consumption.
Brief alcohol interventions (BAIs), defined here as preventive alcohol use interventions shorter than 5 hours in duration, are a low dose intervention option. They offer a resource efficient opportunity for schools interested in implementing interventions in circumscribed time periods. BAIs can use universal, selective, or indicated prevention strategies, as well as a variety of program modalities. The most common BAI program modalities involve cognitive behavioral/skills training, motivational enhancement, and/or psychoeducational therapy. Cognitive behavioral/skills training modalities focus on how individuals’ cognitions affect their actions, and might involve, for instance, teaching and practicing skills for identifying and dealing with risky drinking situations. Motivational enhancement modalities use a motivational interviewing approach to focus on enhancing participants’ motivations to self-evaluate and self-regulate their behavior, and often involve goal-setting or contracting and decisional balance exercises. Psychoeducational prevention modalities, in contrast, tend to be less interactive, and are typically didactic presentations focused on providing information and education around alcohol and alcohol-related harms.
Several literature reviews have established that BAIs can be effective in reducing alcohol use among non-treatment-seeking adults (Bien, Miller, & Tonigan, 1993; Vasilaki, Hosier, & Cox, 2006); yet, no review has specifically examined whether, and if so, under what conditions, school-based BAIs are similarly effective for adolescents. Indeed, most prior reviews or meta-analyses that have synthesized research on the effectiveness of adolescent substance use interventions have not focused specifically on school-based interventions (e.g., Barnett, Sussman, Smith, Rohrbach, & Spruijt-Metz, 2012; Carney & Myers, 2012; Jensen et al., 2011; Tait & Hulse, 2003; Tanner-Smith & Lipsey, in press) or brief interventions (e.g., Gottfredson & Wilson, 2003; Rundall & Bruvold, 1988). This gap is unfortunate given that schools might implement BAIs with relatively modest resources and time, while potentially gaining meaningful reductions in students’ alcohol use and related problems. Given the potential low cost and ease of dissemination of BAIs, an important question is thus whether and under what circumstances school-based BAIs are most (or least) effective.
Variability in Brief Alcohol Intervention Effects
Although schools may be appropriate settings in which to implement BAIs, there are likely conditions under which BAIs are more or less effective. Adolescent characteristics such as age and existing alcohol use, and intervention features such as program duration and modality, may be associated with larger or smaller program effects. For instance, Werch and Owen (2002) reviewed 17 substance use prevention programs and found that programs were more likely to produce negative outcomes if participants reported substance use prior to the prevention program. In another meta-analysis of school-based substance use prevention programs, Gottfredson and Wilson (2003) found that programs yielded better outcomes among younger participants, and if they were longer in duration. Other meta-analyses on substance use prevention and treatment also suggest that interactive program modalities (e.g., cognitive behavioral/skills or motivational enhancement) yield more beneficial effects than less interactive modalities such as psychoeducational therapy (e.g., Jensen et al., 2011; Rundall & Bruvold, 1988; Tanner-Smith, Wilson, & Lipsey, 2013; Tripodi, Bender, Litschge, & Vaughn, 2010).
In addition to these characteristics, another important consideration when providing preventive interventions to at-risk youth is the delivery format. Indeed, prior research has documented that interventions targeting risk behaviors among adolescents and delivered in a group setting may lead to iatrogenic, or harmful, effects (Dishion, Burraston, & Poulin, 2001; Dishion, McCord, & Poulin, 1999; Werch & Owen, 2002). Within group-delivered interventions, iatrogenic effects may occur because of deviancy training among participants, whereby adolescents reinforce each other’s delinquent conversations or actions during group activities (Dishion et al., 2001; Dishion et al., 1999). For example, using a group-based delivery format to implement a BAI with at-risk youth who are already consuming alcohol could foster deviancy training by permitting pro-alcohol or pro-binge-drinking group discussions that would not occur in individually-delivered interventions. Prior research suggests that certain group conditions or settings may be more likely to foster deviancy training and iatrogenic effects: for example, sensitivity to deviancy training may be increased in earlier adolescence (Dishion et al., 2001). Group composition also matters, that is, whether groups are composed of antisocial youth versus youth in mixed antisocial and prosocial groups (Ang & Hughes, 2001). Finally, a skilled leader may also reduce the likelihood of deviancy training (Dishion & Dodge, 2005). Thus, school-based group-delivered BAIs could potentially lead to iatrogenic effects such as increased alcohol consumption, particularly among young adolescents, when delivered in mixed composition groups, or in the absence of a skilled group leader.
Therefore, when examining the effectiveness of BAIs in school settings, it is necessary to consider the possibility of iatrogenic effects due to deviancy training. This is particularly important given that school administrators may be more likely to choose group- (versus individually-) delivered interventions based on perceived ease of implementation within existing school programs and procedures. Yet, if group-delivered BAIs are ineffective in reducing risk behaviors, schools should direct their resources to other evidence-based program formats.
Study Aims
In light of the potential benefits of BAIs for adolescents, the current study uses meta-analytic methods to synthesize findings from research studies identified in a systematic review of the literature. Specifically, this meta-analysis addresses the following research questions: (a) Are school-based BAIs effective in reducing alcohol use among adolescents, relative to those in control conditions; and (b) Is there a difference in BAI effectiveness for individually- versus group-delivered interventions? In post hoc exploratory analyses, we also explored study characteristics that might explain any observed differences in BAI effects for individually- versus group-delivered interventions.
Methods
Eligibility Criteria and Search Strategy
This meta-analysis includes a subset of studies that were part of a larger parent meta-analysis summarizing the effectiveness of BAIs for non-treatment-seeking adolescents and young adults (see Tanner-Smith & Lipsey, in press for full description). The larger meta-analysis focused on diverse types of BAIs for adolescents and young adults. To be eligible for inclusion in the larger meta-analysis, studies had to involve BAI programs designed to reduce participants’ (adolescents or young adults) alcohol consumption, delivered in less than 5 hours of total contact time and less than four weeks between the first and last session. Studies were required to compare BAIs with a no-treatment or treatment-as-usual comparison group, using either an experimental (randomized controlled trial [RCT]) design or a controlled quasi-experimental research design that provided enough information to permit estimation of a pretest effect size. Eligible studies also needed to provide enough information to permit estimation of a post-intervention effect size indexing differences between groups on at least one alcohol-consumption related outcome. To ensure relevance for contemporary programs addressing alcohol use, only studies conducted in or after 1980 were eligible. There were no geographic or language restrictions on eligibility. The meta-analysis reported here focuses on a narrower subset of participants and interventions from the larger parent meta-analysis; BAIs delivered to adolescents in secondary schools. To be eligible for inclusion in the current meta-analysis studies that were first eligible and coded for the larger meta-analysis were then re-reviewed under a second set of eligibility criteria. In this analysis, eligible participants only included adolescents enrolled in middle/high/secondary school who received a school-based BAI in either an individually- or group-delivered format.
The larger parent meta-analysis used a comprehensive search strategy to identify relevant published and unpublished studies; all studies in the current meta-analysis were identified in the larger parent meta-analysis search process. The following electronic bibliographic databases were searched, current through December 31, 2012: CINAHL, Clinical Trials Register, Dissertation Abstracts International, ERIC, International Bibliography of the Social Sciences, NIH RePORTER, PsycARTICLES, PsycINFO, PubMed, Social Services Abstracts, Sociological Abstracts, and WorldWideScience.org. Search terms were adapted for each database, but generally used three search term blocks: one set describing the BAI, a second describing alcohol outcomes, and a third with study design terms. The following sources are some of the websites searched for relevant grey literature (full list available from the authors): Australasian Medical Index, Campbell Collaboration Library, Canadian Evaluation Society’s Grey Literature Database, Cochrane Collaboration CENTRAL, Google Scholar, Index to Theses in Great Britain and Ireland, International Clinical Trials Registry, KoreaMed, NIAAA Website, NTIS, OpenSIGLE, SAMHSA website, and SveMed+. Bibliographies of all screened and eligible studies and those in prior narrative reviews and meta-analyses were reviewed. Hand-searches in the following journals’ table of contents were conducted: Alcoholism: Clinical & Experimental Research, American Journal on Addictions, and Journal of Substance Abuse Treatment.
Studies meeting these criteria were retrieved and coded by trained personnel. Prior to coding, personnel participated in several weeks of training where five studies were coded by all coders. Coders then convened as a group to resolve any coding discrepancies until 100% reliability was attained on all coded variables. Weekly meetings were held throughout coding, and the project’s PI checked all coding and resolved discrepancies via consensus with the coder.
Effect size moderators
The key effect size moderator1 of interest was delivery format, measured as individually-delivered (individual with provider) or group-delivered (group with provider). The following participant characteristics were collected for exploration as potential effect size moderators: participant age (years), percent male (intervention group), percent White (intervention group), and self-reported baseline alcohol use level among participants (ranging from 1 = mostly abstainers; 4 = hazardous users). Finally, the following intervention and study characteristics were also explored as potential effect size moderators: average attrition; focal modality (cognitive behavioral therapy [CBT]; motivational enhancement therapy [MET]; CBT and MET combined; psychoeducational therapy [PET]); intervention location (country); personalized feedback given (yes or no); program duration (minutes); program target (universal, indicated); time between program end and posttest (weeks); and study design (RCT, quasi-experimental).
Statistical Methods
Effect size metric
We measured our outcomes of interest with standardized mean difference effect sizes, coded so that positive effect sizes represent better outcomes (e.g., lower alcohol consumption). Standardized mean difference effect sizes were adjusted with the small-sample correction factor (Hedges, 1981). For binary outcomes (e.g., group differences in abstinence), the Cox transformation was used to convert log odds ratio effect sizes into standardized mean difference effect sizes (see Sánchez-Meca, Marín-Martínez, & Chacón-Moscoso, 2003). Effect size and sample size outliers, defined as three standard deviations above the mean, were Winsorized to less extreme values to prevent distortion of the meta-analysis results (Lipsey & Wilson, 2001). Standard errors of effect size estimates that originated from cluster-randomized trials were inflated for cases where the authors did not properly account for the cluster design in their own analyses. This was done by multiplying the standard error of the effect size by the square root of the design effect (see Higgins, Deeks, & Altman, 2008). When the intraclass correlation coefficient (ICC) required for this correction was missing, the estimated average ICC (.13) for all alcohol consumption outcomes across all studies, was used. If primary studies did not include the information needed to estimate effect sizes, we contacted primary study authors. If we could not obtain this data from authors, effect sizes were not imputed.
Analytic strategies
Given the presumed heterogeneity in interventions and participants, random effects statistical models were used, implemented with weighted analyses using inverse variance weights (Lipsey & Wilson, 2001). Because most studies reported multiple measures of alcohol consumption, and to ensure the statistical independence of effect sizes included within any given analysis, the following hierarchy was used to select one effect size from each study, in order of preference: alcohol consumption frequency, consumption quantity, frequency of heavy use, abstinence, and peak consumption. Some studies also reported results from multiple follow-up waves, so one effect size per outcome (across all waves) was randomly selected using a computer-generated random number. We used mixed-effects meta-regression models to explore hypothesized moderators and to conduct sensitivity analysis. Finally, contour enhanced funnel plots, trim and fill analysis, and regression tests for funnel plot asymmetry were used to assess the possibility of publication bias stemming from the potential underrepresentation of small sample size studies with null or negative findings (Rothstein, Sutton, & Borenstein, 2005).
Results
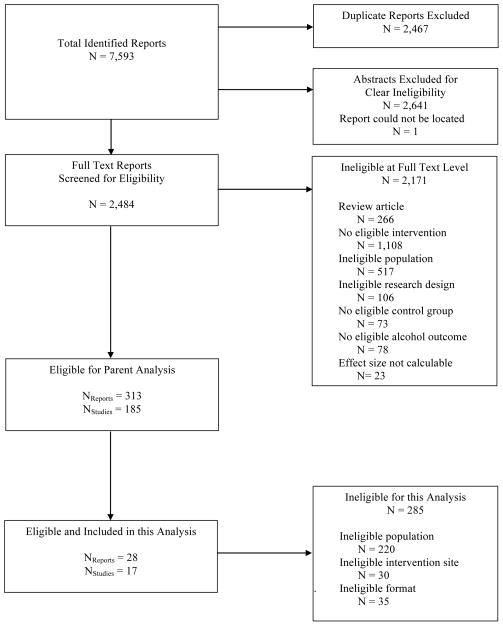
In the larger parent-meta-analysis (Tanner-Smith & Lipsey, in press), 7,593 reports were identified in the literature search: 2,467 were duplicates and removed, 2,641 were screened as ineligible at the abstract phase, and one report could not be located (see Figure 1). We retrieved 2,484 articles in full text format and of these, 2,456 were deemed ineligible for the present analysis. The remaining 28 documents (15 journal articles, eight theses/dissertations, four conference presentations, and one university technical report) reported findings for 17 unique study samples that were eligible for inclusion in the current meta-analysis.
Figure 1.
Study identification flow diagram.
Characteristics of the Included Studies
Study design
Table 1 summarizes the characteristics of the 17 eligible studies. Studies came from many world regions, although the most common study location was North America (k = 9). Sixty-five percent (k = 11) of studies were RCTs; the remainder used controlled quasi-experimental research designs. All of the studies reported using a scripted protocol or manual for the intervention, but the majority (76%) did not report any monitoring of implementation fidelity. Only two studies reported possible or apparent implementation problems. Average attrition was 13.03%, and attrition rates were similar across treatment and control groups (11.97% and 14.09%, respectively). Seven studies (41%) explicitly reported conducting intent-to-treat analysis. The majority of studies (71%, k = 12) were universal prevention programs. Of the five studies that implemented an indicated prevention program (i.e., screened students and only enrolled high-risk youth), four were individually-delivered and one was group-delivered. All studies collected self-reported alcohol outcome data, and six studies reported using a standardized scale to collect this information. Among the included effect sizes, 12% (k = 2) were measured between 0–1 month after the intervention, 35% (k = 6) were between 1–3 months, and 53% (k = 9) were between 3–6 months after the intervention.
Table 1.
Characteristics of Included Studies
| Study | Region | RCT | TX N (Total N) | TX age range (M) | TX % male | TX % White | Focal modality | Type of intervention provider | Program duration (minutes) |
|---|---|---|---|---|---|---|---|---|---|
| Group-delivered interventions
| |||||||||
| Collins, 1990 | North America | Ya | 20 (36) | 16–17 (16.5) | 51 | 45 | PET | Graduate student (Psychology)c | 180 |
| Comeau, 2003 | North America | Y | 69 (135) | NR (15.7) | 49 | 87 | CBT+ MET | 4 clinical therapists (provincial treatment program) and 1 graduate student (Clinical Psychology)c | 180 |
| Cruz, 2006 | North America | Ya | 65 (130) | NR (17) | 50 | 72 | PET | Graduate student (Psychology)c | 60 |
| Dempster et al., 2006 | Europe | Na | 121 (168) | 15–16 (NR) | 100 | NR | PET | “Consultant/senior lecturer in oral surgery and director of dental education”c | 20 |
| Gmel et al., 2012 | Europe | Na | 184 (364) | 15–19 (17) | 64 | NR | MET | “Counselors”- “experienced collaborators from alcohol and drug help information centers”c | 90 |
| Mushquash, 2011 | North America | N | 18 (25) | 14–18 (16) | 37 | 0 | CBT/Skillsb | School guidance counselors and police officers | 180 |
| Quigley, 2010 | Europe | Y | 120 (384) | 11–16 (13.6) | 47 | 72 | CBT/Skills | “Learning mentors” | 40 |
| Wooten, 1995 | North America | Ya | 18 (44) | 13–15 (13.7) | 49 | 62 | CBT/Skills | Graduate student (Psychology)c | 240 |
| Zhang, 2009 | Asia | Na | 290 (610) | NR (15.6) | 52 | NR | PET | High school teachers | 180 |
|
| |||||||||
| Individually-delivered interventions
| |||||||||
| Martínez Martínez et al., 2008a | Latin America | Y | 23 (40) | 14–18 (16) | 57 | 0 | MET | NR | 90 |
| Martínez Martínez, et al., 2008b | Latin America | Y | 13 (23) | 14–18 (NR) | NR | 0 | MET | NR | 90 |
| Martínez Martínez et al., 2010 | Latin America | Y | 20 (38) | 14–18 (16) | 62 | 0 | MET | “Group of trained therapists”c | 90 |
| Martins, 2008 | South America | N | 50 (100) | NR (16.2) | 49 | NR | METb | Research “team members”c | 50 |
| Werch et al., 1996 | North America | Y | 50 (101) | NR (13.8) | 50 | 12 | METb | “Physician or nurse”c | 17.1 |
| Werch et al., 2005a | North America | Y | 100 (201) | NR (17) | 42 | 53 | MET | “Risk reduction interventionist”c | NR |
| Werch et al., 2005b | North America | Y | 145 (289) | NR (13.5) | 48 | 61 | METb | Nursesc | 20.9 |
| Winters et al., 2012 | North America | N | 134 (189) | 13–17 (16.2) | 49 | 66 | MET | 2 therapistsc | 120 |
Note. RCT = Randomized Controlled Trial. TX = Treatment/intervention group. NR = Not reported by study authors. CBT = cognitive behavioral therapy. MET = motivational enhancement therapy. PET = psychoeducational therapy.
Indicates program was conducted during classroom time or participants were assigned at the classroom level.
Indicates programs used a branded intervention.
Indicates implementers were reported as non-school staff.
Intervention components
Eligible studies were divided almost equally by intervention delivery format: nine studies involved interventions delivered in a group and eight were delivered individually. The group-delivered interventions used a range of modalities (motivational enhancement therapy [MET] = 1; cognitive behavioral therapy/skills training = 3; cognitive behavioral and motivational enhancement therapy combined = 1; psychoeducational therapy = 4), whereas all of the individually-delivered interventions used an MET approach. Only one of the group-delivered interventions included giving an adolescent personalized feedback on his/her self-reported alcohol use, whereas six of the individually-delivered interventions included such feedback. Ten studies implemented BAIs in a single session (range was 1 – 4). Group-delivered interventions were on average twice as long as those delivered individually: 130 (SD = 78.10) versus 68.29 (SD = 39.35) minutes, respectively. Of the 15 studies that reported implementer background, 12 studies used non-school staff as implementers.
Participant demographics
In the BAI conditions, an average of 53% of participants were male and the average age was 15.58 (SD = 1.29) years. Among studies reporting participant ethnicity, an average of 41% of youth in the intervention conditions were Caucasian (k = 13) and 21% were Black/African American (k = 12). Alcohol use severity of participants as measured during screening or at baseline could be categorized as: abstainers (k = 1), low use/experimenters (k = 6), medium or regular users (k = 1), and risky/hazardous users (k = 9).
Effectiveness of School-Based Brief Alcohol Interventions
Synthesizing effect sizes from 17 studies, results indicated that school-based BAIs were associated with beneficial effects on adolescents’ post-intervention alcohol consumption (ḡ = 0.34, 95% CI [0.11, 0.56]). This effect of a 0.34 standard deviation improvement in the BAI group translates into a reduction of 1.4 drinking days per month, with adolescents in the intervention groups consuming an average of 3.7 days in the past month, versus 5.1 days in the past month for those in the control groups.2 Interpreted another way, if the median of the control group distribution is used to define a success threshold, this mean effect size translates into a 63% success rate among BAI participants, relative to a 50% success rate in the control group. There was evidence of heterogeneity in the observed effect sizes, however, as expected given the diversity of included interventions and participant samples (τ2 = 0.13, χ216 = 60.95, I2 = 73.7%).
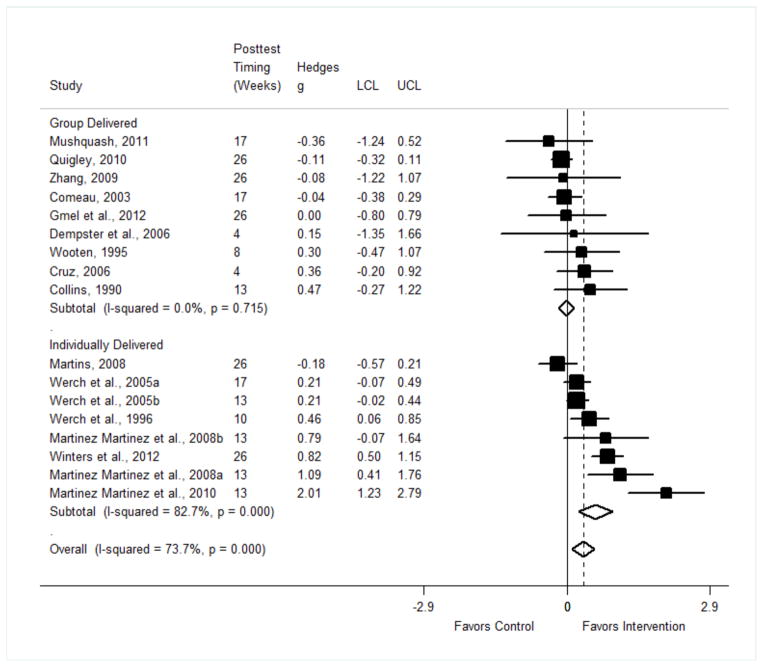
Delivery format
Figure 2 presents results from the meta-analysis examining the effects of school-based BAIs on alcohol consumption among adolescents, with results split by delivery format. Each effect size and its corresponding 95% confidence interval are shown, with boxes proportionate to each study’s weight in the meta-analysis (i.e., larger boxes indicate effect sizes with larger weights in the meta-analysis). Diamonds illustrate the random effects mean effect sizes (and corresponding confidence intervals). The solid vertical line is at the null value of zero, and the dashed vertical line is at the overall mean effect size value of 0.34.
Figure 2.
Forest plot of the effects of school-based brief alcohol interventions on adolescent alcohol consumption, by intervention delivery format.
Note. LCL = lower confidence limit (95%). UCL = upper confidence limit (95%).
As shown in Figure 2, individually-delivered interventions had a significant positive overall mean effect ḡ of 0.58 (95% CI [0.23, 0.92]; τ2 = 0.18; Q = 40.46, p < .001; I2 = 82.7%), whereas there was no evidence of an effect for group-delivered interventions (ḡ = −0.02, 95% CI [−0.17, 0.14]; τ2 = 0.0; Q = 5.39, p = .72; I2 = 0.0%). Indeed, five (56%) of the group-delivered studies reported negative effect sizes, and only one (13%) of the individually-delivered studies reported a negative effect size; yet, the likelihood of reporting a positive or negative effect was not significantly associated with delivery format (χ21 = 3.44, p = .06).
To address our research questions and given the observed differences in effects for group- versus individually-delivered school-based BAIs, we next estimated a series of meta-regression models to explore whether any study characteristics might explain those differences. Namely, we first focused on differences in effect size magnitude by delivery format (individual versus group), and then assessed whether those differences could be explained away by other study characteristics: participants’ age and risk level (hazardous baseline alcohol use); and program components (if personalized feedback was given and duration). First, we ran six separate bivariate meta-regression models that directly examined the association between each of these variables and the effect size outcome. We then estimated a series of meta-regression models that included a dummy variable for delivery format along with each one of the predictor variables in turn. Ideally, we would have used multivariable meta-regression models with all predictors to account for possible confounding among them, but this was not feasible given the small number of included studies. Instead, we examined bivariate correlations between all factors to assess possible confounding effects (table available in the electronic supplementary material).
Table 2 presents results from these meta-regression models, where Model 1 shows results from the six individual bivariate meta-regression models described above. Results from two of the six bivariate meta-regression models indicated marginally significant differences in effect size magnitude according to intervention characteristics: (1) group-delivered interventions exhibited smaller mean effects than individually-delivered interventions (b = −0.49, 95% CI [−1.00, 0.01]; τ2res = 0.15, adjusted R2 = 19.65%); and (2) interventions using motivational enhancement therapy components exhibited larger mean effects than those that did not (b = 0.44, 95% CI [−0.09, 0.97]; τ2res = 0.15, adjusted R2 = 15.84%). None of the other predictors were significant in these models. Models 2–6 in Table 2 show the meta-regression results for each predictor, in turn, but also include an indicator for delivery format (group = 1). Results indicated that delivery format retained a negative relationship with BAI effectiveness after separately controlling for participants’ age, hazardous alcohol use, program duration, and whether the intervention included personalized feedback. However, as shown in Model 6, the negative effect of group delivery format was attenuated to non-significance (p = .35) after controlling for whether the program used motivational enhancement therapy as its primary modality.
Table 2.
Effect of Intervention Delivery Format on Outcomes, Net of Other Intervention and Participant Characteristics
| Characteristics | Model 1a
|
Model 2 (k = 15)
|
Model 3 (k = 17)
|
Model 4 (k = 16)
|
Model 5 (k = 17)
|
Model 6 (k = 17)
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | |
| Format (Group = 1) | −0.49 † | [−1.00, 0.01] | −0.49† | [−1.08, 0.10] | −0.44† | [−0.95, 0.07] | −0.71* | [−1.32, −0.09] | −0.56† | [−1.19, 0.07] | −0.57 | [−1.85, 0.71] |
| Average age (years) | 0.05 | [−0.19, 0.30] | 0.06 | [−0.17, 0.28] | ||||||||
| Hazardous use (y = 1) | 0.36 | [−0.18, 0.90] | 0.28 | [−0.23, 0.79] | ||||||||
| Duration (minutes) | −0.00 | [−0.01, 0.00] | 0.00 | [−0.00, 0.01] | ||||||||
| Personal feedback (y = 1) | 0.22 | [−0.36, 0.79] | −0.12 | [−0.75, 0.51] | ||||||||
| MET modality (y = 1) | 0.44 † | [−0.09, 0.97] | −0.08 | [−1.38, 1.21] | ||||||||
| Constant | −0.33 | [−3.83, 3.18] | 0.41† | [−0.03, 0.84] | 0.48* | [−0.00, 0.97] | 0.65* | [0.08, 1.23] | 0.65 | [−0.69, 2.0] | ||
|
| ||||||||||||
| τ2 | 0.18 | 0.14 | 0.15 | 0.16 | 0.16 | |||||||
| I2res (%) | 72.17 | 63.66 | 64.78 | 65.92 | 69.46 | |||||||
| Adjusted R2 | 7.61 | 25.88 | 28.41 | 11.83 | 11.89 | |||||||
Note. k = number of studies. b = unstandardized coefficient from meta-regression model. CI = confidence interval. MET = motivational enhancement therapy.
Model 1 shows coefficients from six separate bivariate meta-regression models.
p < .10.
p < .05.
Sensitivity analyses
To assess the possibility of publication bias, we visually inspected a contour enhanced funnel plot, which was relatively symmetric and therefore provided no clear indication of small study bias. The regression test for funnel plot asymmetry was also non-significant (b = −0.01, p = .20, 95% CI [−0.43, 0.41]), providing additional reassurance against the possibility of small study bias. However, the trim and fill analysis yielded four trimmed/filled studies, and with their inclusion, the overall mean effect size was no longer statistically significant (ḡ= 0.11, 95% CI [−0.15, 0.36]). Thus, considered together, these analyses provide only partial reassurance that our findings are not biased due to small study or publication bias.
We conducted additional sensitivity analysis to explore the effect of study method and quality on the meta-analysis results (table available in the electronic supplementary material). This analysis examined whether research design, intervention implementation monitoring, or participant attrition were associated with BAI effects and whether these factors explained the observed differences between group- and individually-delivered interventions. Results from subgroup analyses indicated that among RCTs, BAIs had significant positive effects (ḡ = 0.41, 95% CI [0.15, 0.67]), whereas in non-RCTs there was no evidence for the effectiveness of BAIs over comparison conditions (ḡ = 0.11, 95% CI [−0.43, 0.63]). Nonetheless, when research design and average attrition were each separately included with delivery format in meta-regression models, the negative effect of group delivery format was not attenuated. However, the negative effect of group-delivery was attenuated to non-significance in the model controlling for study-reported monitoring of intervention fidelity, indicating that observed differences across delivery format might also be due to variability in study design and implementation.
Discussion
Based on this synthesis of findings from 17 controlled studies, we conclude that some school-based BAIs may be effective in reducing adolescent alcohol use. Overall, school-based BAIs were associated with approximately 1.4 days reduction in drinking in the past month for adolescents; a moderate effect that could potentially translate into improved health, educational, and social well-being for youth who participate in such preventive interventions. School-based BAIs were not all equally effective, however. Individually-delivered BAIs were consistently effective and associated with significant reductions in adolescents’ alcohol use. Conversely, there was no evidence that group-delivered BAIs were similarly effective: they used a variety of program modalities yet were statistically homogenous and produced null results on average. We found no evidence of iatrogenic (i.e., negative) effects, of group-delivered BAIs, but these programs nevertheless appear to have negligible effects on alcohol outcomes.
Although these results indicate the possibility of deviancy training in the group-delivered programs, post hoc exploratory analyses highlighted that the differing outcomes by delivery format may be due in part to other factors. Namely, delivery format and modality were almost completely confounded, such that all of the individually-delivered interventions used motivational enhancement therapy modalities whereas the group-delivered interventions used a variety of modalities (i.e., motivational, cognitive behavioral, and psychoeducational). Further, among the group-delivered interventions, one study screened and enrolled participants based on their risk level; three others did not screen for existing alcohol use, but enrolled participants who reported hazardous alcohol consumption at baseline. Thus, the null effects observed among group-delivered BAIs could be the result of enrolling deviant youth in a group-delivered intervention or could instead be due to the inability of providers to adequately address relevant alcohol consumption issues (Werch & Owen, 2002). This, and the fact that the negative effect of group format was attenuated to non-significance after separately controlling for program modality and implementation monitoring, suggests that there are program features in addition to delivery format to address when making recommendations for school-based BAIs.
Limitations
Findings from this meta-analysis should be interpreted in light of its limitations. First, results from the publication bias analysis were equivocal. Results indicated that the observed average effect of school-based BAIs might be upwardly biased due to the absence of primary studies with small sample sizes and null/negative results. This highlights a clear imperative for primary researchers to publish research findings regardless of the magnitude and direction of program effects. Second, primary study quality is always an important consideration in terms of the validity of meta-analysis findings. Similar to a prior meta-analysis (Wilson et al., 2001), we found that RCTs yielded larger program effects than studies using quasi-experimental controlled designs. Although the difference in effects across delivery format (group vs. individual) did not change when we statistically controlled for study design, this effect was attenuated to non-significance after controlling for implementation monitoring. Group-delivered school-based BAIs might therefore yield larger outcomes with more careful implementation monitoring and feedback to providers to ensure fidelity to program models. A third limitation of the meta-analysis is the length of follow-up periods available in the included primary studies. Prior meta-analyses of substance use prevention programs have illustrated that effect sizes tend to decrease in magnitude as the length of follow-up increases (Jensen et al., 2011; Tripodi et al., 2010); however, others have found positive outcomes two years post-intervention (Gottfredson & Wilson, 2003). Given these discrepancies, the combination of effect sizes from different follow-up periods and for only up to six months post-intervention must be considered when interpreting the results. It is premature to draw any conclusions regarding the long-term effects of school-based BAIs on adolescents’ alcohol use. Finally, an important moderator, but one that could not be explored in the current meta-analysis due to lack of variability across studies, is whether the school-based BAIs used universal, selective, or indicated prevention strategies. This is an important area for future inquiry, along with exploration of other underlying mechanisms of change for youth participants of school-based BAIs.
Future considerations
Despite our best prevention efforts, many adolescents still consume alcohol (Romer & Hennessy, 2007). Approximately two-thirds of U.S. adults are current drinkers without substance abuse problems (Center for Substance Abuse Research, 2013), and alcohol experimentation is often considered a normative part of adolescent development. As a result, understanding what interventions may be most appropriate for adolescents with subclinical levels of alcohol use is crucial. Results from the current study suggest that both delivery format and program modality may play an important role in school-based BAI effectiveness. Indeed, interactive and personalized approaches to alcohol prevention may offer the greatest promise, particularly those programs using motivational enhancement therapy and motivational interviewing techniques. The motivational enhancement approach aims to help individuals recognize personal strengths, balance the pros and cons of specific behaviors, and set goals for behavior change—personalized and interactive activities that may resonate with adolescents and be relevant to their lived experiences. Indeed, these personalized interactive approaches may be more effective than the didactic and non-interactive approaches that focus solely on provision of non-personalized education and information, which have often been utilized more frequently in group settings with adolescents.
When considering implications for school-based BAI programming, individually-delivered programs using motivational enhancement techniques (MET) are likely to yield beneficial outcomes among youth. Because individually-delivered BAIs may not be feasible for some schools to implement, more research is needed to examine whether group-delivered BAIs may be effective when implemented using MET approaches. Although conducting MET in groups may be seen as resource-intensive, prior research suggests it is possible. One group-delivered BAI using motivational interviewing techniques (ineligible for this meta-analysis because it was not school-based), reported several successful outcomes in an adolescent community sample (Bailey, Baker, Webster, & Lewin, 2004). Additional research is thus needed to explore whether group-delivered BAIs using MET components yield beneficial outcomes like those found in the individually-delivered programs in this meta-analysis.
Finally, our results highlight the importance of primary study reporting of program implementation data. For example, among the studies included in this meta-analysis, few studies reported details about program implementers and the implementation process. This is unfortunate given that staff characteristics, including training, experience, and ability to build relationships with youth have been proposed as moderators of program effectiveness (Dishion & Dodge, 2005; Gottfredson & Wilson, 2003; Handwerk, Field, & Friman, 2001). Complete reporting of study implementation characteristics will yield valuable information that can be used to further explore whether and under what conditions school-based brief alcohol interventions are most effective in reducing adolescent students’ alcohol consumption.
Supplementary Material
Acknowledgments
This work was supported by Award Number R01AA020286 from the National Institute on Alcohol Abuse and Alcoholism.
Footnotes
In most meta-analyses, the effect size indexes the relationship between two variables in a primary study (e.g., x = BAI delivery; y = post-intervention alcohol use). As such, variables used to predict the magnitude of effect sizes in a meta-analysis (e.g., z = intervention delivery format) are typically called moderators because they are hypothesized to modify the effect of the intervention on the outcome of interest (see Higgins & Green, 2011; Lipsey & Wilson, 2001). We use this standard meta-analysis terminology of “effect size moderators” in the current study.
This estimate is based on data from the larger meta-analysis (Tanner-Smith & Lipsey, in press), using the average mean and standard deviation of post-intervention alcohol consumption among control group participants on items measuring frequency of alcohol consumption in the past 30 days using a Timeline Follow-Back outcome measure.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
The authors declare that they have no conflict of interest.
References
References marked with an asterisk indicate studies included in the meta-analysis.
- Ang RP, Hughes JN. Differential benefits of skills training with antisocial youth based on group composition: A meta-analytic investigation. School Psychology Review. 2001;31:164–185. [Google Scholar]
- Bailey KA, Baker AL, Webster RA, Lewin TJ. Pilot randomized controlled trial of a brief alcohol intervention group for adolescents. Drug and Alcohol Review. 2004;23:157–166. doi: 10.1080/09595230410001704136. [DOI] [PubMed] [Google Scholar]
- Barnett E, Sussman S, Smith C, Rohrbach LA, Spruijt-Metz D. Motivational interviewing for adolescent substance use: A review of the literature. Addictive Behaviors. 2012;37:1325–1334. doi: 10.1016/jaddbeh.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bien TH, Miller WR, Tonigan SJ. Brief interventions for alcohol problems: A review. Addiction. 1993;88:315–336. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- Carney T, Myers B. Effectiveness of early interventions for substance-using adolescents: Findings from a systematic review and meta-analysis. Substance Abuse Treatment, Prevention, and Policy. 2012;7:1–28. doi: 10.1186/1747-597X-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Substance Abuse Research. Nearly two-thirds of US adults are current drinkers; Majority are infrequent or light drinkers (CESAR Fax) 21. Vol. 22. University of Maryland; College Park: Author; 2013. May, [Google Scholar]
- *.Collins DL. Unpublished master’s thesis. Francis Marion College; Florence, South Carolina: 1990. A study of a brief alcohol education program. [Google Scholar]
- *.Comeau MN. Framing solutions: Adolescent girls and their relationships with alcohol. Dissertation Abstracts International: Section B. Sciences and Engineering. 2003;64(09):4601. [Google Scholar]
- *.Cruz IY. Reducing alcohol consumption among high school students by challenging alcohol expectancies. Dissertation Abstracts International: Section B. Sciences and Engineering. 2006;67(09) [Google Scholar]
- Currie C, Zanotti C, Morgan A, Currie D, de Looze M, Roberts C, Barnekow V. Health Policy for Children and Adolescents, No 6. Copenhagen, Denmark: WHO Regional Office for Europe; 2012. Social determinants of health and well-being among young people. Health Behaviour in School-aged Children (HBSC) study: International report from the 2009–2010 survey. [Google Scholar]
- *.Dempster M, Newell G, Cowan G, Marley J. Facing up to binge drinking: Reducing binge drinking in adolescent males. British Dental Journal. 2006;201:587–590. doi: 10.1038/sj.bdj.4814204. discussion 578. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Burraston B, Poulin F. Peer group dynamics associated with iatrogenic effects in group interventions among high-risk adolescents. In: Erdley C, Nangle DW, editors. Damon’s new directions in child development: The role of friendship in psychological adjustment. San Francisco: Jossey-Bass; 2001. pp. 79–92. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Dodge KA. Peer contagion in interventions for children and adolescents: Moving towards an understanding of the ecology and dynamics of change. Journal of Abnormal Child Psychology. 2005;33:395–400. doi: 10.1007/s10802-005-3579-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, McCord J, Poulin F. When interventions harm. Peer groups and problem behavior. American Psychologist. 1999;54:755–764. doi: 10.1037//0003-066x.54.9.755. [DOI] [PubMed] [Google Scholar]
- DuPont RL, Caldeira KM, DuPont HS, Vincent KB, Shea CL, Arria AM. America’s dropout crisis: The unrecognized connection to adolescent substance use. Rockville, MD: Institute for Behavior and Health, Inc; 2013. Retrieved from www.cls.umd.edu/docs/AmerDropoutCrisis.pdf. [Google Scholar]
- Foxcroft DR, Tsertsvadze A. Universal school-based prevention programs for alcohol misuse in young people. Cochrane Database of Systematic Reviews. 2011;(5):Art. No.: CD009113. doi: 10.1002/14651858.CD009113. [DOI] [PubMed] [Google Scholar]
- Gottfredson DC, Wilson DB. Characteristics of effective school-based substance abuse prevention. Prevention Science. 2003;4:27–38. doi: 10.1023/a:1021782710278. [DOI] [PubMed] [Google Scholar]
- *.Gmel G, Venzin V, Marmet K, Danko G, Labhart F. A quasi randomized group trial of a brief alcohol intervention on risky single occasion drinking among secondary school students. International Journal of Public Health. 2012;57:935–944. doi: 10.1007/s00038-012-0419-0. [DOI] [PubMed] [Google Scholar]
- Handwerk ML, Field CE, Friman PC. The iatrogenic effects of group intervention for antisocial youth: Premature extrapolations? Journal of Behavioral Education. 2001;10:223–238. [Google Scholar]
- Hanson KL, Medina KL, Padula CB, Tapert SF, Brown SA. Impact of adolescent alcohol and drug use on neuropsychological functioning in young adulthood: 10-year outcomes. Journal of Child & Adolescent Substance Abuse. 2011;20:135–154. doi: 10.1080/1067828X.2011.55527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational Statistics. 1981;6:107–128. [Google Scholar]
- Higgins JPT, Deeks JJ, Altman DG, Green S, editors. Cochrane handbook for systematic reviews of interventions. Chichester, UK: John Wiley & Sons; 2008. Chapter 16: Special topics in statistics; pp. 481–529. [Google Scholar]
- Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions (Version 5.1.0, updated March 2011) Chichester, UK: John Wiley & Sons; 2011. [Google Scholar]
- Hipwell A, Stepp S, Chung T, Durand V, Keenan K. Growth in alcohol use as a developmental predictor of adolescent girls’ sexual risk taking. Prevention Science. 2012;13:118–128. doi: 10.1007/s11121-011-0260-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, Steele RG. Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2011;79:433–440. doi: 10.1037/a0023992. [DOI] [PubMed] [Google Scholar]
- Kandel D, Davies M, Karus D, Yamaguchi K. The consequences in young adulthood of adolescent drug involvement. Archives of General Psychiatry. 1986;43:746–54. doi: 10.1001/archpsyc.1986.0180008003200. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Wilson D. Practical meta-analysis (Applied Social Research Methods) Vol. 49. Thousand Oaks, California: SAGE Publications, Inc; 2001. [Google Scholar]
- *.Martínez Martínez KI, Pedroza Cabrera FJ, de los Ángeles Vacío M, Jiménez Pérez AL, Salazar Garza ML. Consejo breve para adolescentes escolares que abusan del alcohol. [School-based brief counseling for teenage drinkers] Revista Mexicana de Análisis de la Conducta. 2008a;34:245–262. [Google Scholar]
- *.Martínez Martínez KI, Pedroza Cabrera FJ, Salazar Garza ML, editors. Resultados iniciales de la aplicación de consejo breve sobre el consumo de alcohol en adolescentes rurales de México [Initial results of the application of brief advice on alcohol consumption in rural teenagers from Mexico] TIPICA: Boletín Electrónico de Salud Escolar. 2008b;4 Retrieved from http://www.tipica.org/ [Google Scholar]
- *.Martínez Martínez KI, Pedroza Cabrera FJ, Salazar Garza ML, de los Ángeles Vacío M. Evaluación experimental de dos intervenciones breves para la reducción del consumo de alcohol de adolescentes [Experimental evaluation of two brief interventions for the reduction of alcohol consumption in teenagers] Revista Mexicana De Análisis De La Conducta. 2010;36:35–53. doi: 10.5514/rmac.v36.i3.03. [DOI] [Google Scholar]
- *.Martins RA. Aplicação de intervenção breve em estudantes de ensino médio que apresentam beber de risco. Paper presented at the meeting of the International Network on Brief Interventions for Alcohol Problems; Ribeirão Preto, Brazil. 2008. [Google Scholar]
- *.Mushquash CJ. Unpublished Doctoral dissertation. Dalhousie University; Nova Scotia, Canada: 2011. Personality and motives for alcohol use in aboriginal adolescents: A culturally relevant approach to alcohol abuse early intervention. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Alcohol and Health. Underage drinking. n.d Retrieved from http://www.niaaa.nih.gov/alcohol-health/special-populations-co-occurring-disorders/underage-drinking.
- *.Quigley CF. Doctoral dissertation. University of Sheffield; England: 2010. A psychosocial model of drinking amongst young people and the effects of brief interventions. Available from ProQuest Dissertations and Theses database. (UMI No. U557325) [Google Scholar]
- Romer D, Hennessy M. A biosocial-affect model of adolescent sensation seeking: The role of affect evaluation and peer-group influence in adolescent drug use. Prevention Science. 2007;8:89–101. doi: 10.1007/s11121-007-0064-7. [DOI] [PubMed] [Google Scholar]
- Rothstein HR, Sutton AJ, Borenstein M. Publication bias in meta-analysis: Prevention, assessment and adjustments. West Sussex: Wiley; 2005. [Google Scholar]
- Rundall TG, Bruvold WH. A meta-analysis of school based smoking and alcohol use prevention programs. Health Education Quarterly. 1988;15:317–334. doi: 10.1177/109019818801500306. [DOI] [PubMed] [Google Scholar]
- Sánchez-Meca J, Marín-Martínez F, Chacón-Moscoso S. Effect-size indices for dichotomized outcomes in meta-analysis. Psychological Methods. 2003;8:448–467. doi: 10.1037/1082-989X.8.4.448. [DOI] [PubMed] [Google Scholar]
- Tait RJ, Hulse GK. A systematic review of the effectiveness of brief interventions with substance using adolescents by type of drug. Drug and Alcohol Review. 2003;22:337–346. doi: 10.1080/0959523031000154481. [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment. doi: 10.1016/j.jsat.2014.09.001. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE, Wilson SJ, Lipsey MW. The comparative effectiveness of outpatient treatment for adolescent substance abuse: A meta-analysis. Journal of Substance Abuse Treatment. 2013;44:145–158. doi: 10.1016/j.jsat.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripodi SJ, Bender K, Litschge C, Vaughn MG. Interventions for reducing adolescent alcohol abuse: A meta-analytic review. Archives of Pediatrics and Adolescent Medicine. 2010;164:85–91. doi: 10.1001/archpediatrics.2009.235. [DOI] [PubMed] [Google Scholar]
- Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol & Alcoholism. 2006;41:328–335. doi: 10.1093/alcalc/ag1016. [DOI] [PubMed] [Google Scholar]
- *.Werch CE, Anzalone DM, Brokiewicz LM, Felker J, Carlson JM, Castellon-Vogel EA. An intervention for preventing alcohol use among inner-city middle school students. Archives of Family Medicine. 1996;5:146–152. doi: 10.1001/archfami.5.3.146. [DOI] [PubMed] [Google Scholar]
- *.Werch C, Jobli E, Moore MJ, DiClemente CC, Dore H, Brown CH. A brief experimental alcohol beverage-tailored program for adolescents. Journal of Studies on Alcohol. 2005a;66:284–290. doi: 10.15288/jsa.2005.66.284. [DOI] [PubMed] [Google Scholar]
- *.Werch CE, Moore MM, Diclemente CC, Owen DM, Carlson JM, Jobli E. Single vs. multiple drug prevention: Is more always better? A pilot study. Substance Use & Misuse. 2005b;40:1085–1101. doi: 10.1081/ja-200030814. [DOI] [PubMed] [Google Scholar]
- Werch CE, Owen DM. Iatrogenic effects of alcohol and drug prevention programs. Journal of Studies on Alcohol. 2002;63:581–590. doi: 10.15288/jsa.2002.63.581. [DOI] [PubMed] [Google Scholar]
- Wilson DB, Gottfredson DC, Najaka SS. School-based prevention of problem behaviors: A meta-analysis. Journal of Quantitative Criminology. 2001;17:247–272. [Google Scholar]
- *.Winters KC, Fahnhorst T, Botzet A, Lee S, Lalone B. Brief intervention for drug-abusing adolescents in a school setting: Outcomes and mediating factors. Journal of Substance Abuse Treatment. 2012;42:279–288. doi: 10.1016/j.jsat.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Wooten BT. Challenging alcohol expectancies: An application to adolescents. Dissertation Abstracts International: Section B. Sciences and Engineering. 1995;56(12-B):706056. UMI No. 9610329. [Google Scholar]
- *.Zhang Y. Effects of an alcohol education program for high school students in Wuhan, China. Dissertation Abstracts International: Section A. Humanities and Social Sciences. 2009;70(30) UMI No. 3350261. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.