Abstract
Dengue is endemic in more than 100 countries in Southeast Asia, the Americas, the western Pacific, Africa and the eastern Mediterranean regions. The virus is transmitted by Aedes mosquitoes. Dengue disease is the most prevalent arthropod-borne viral disease in humans and is a global and national public health concern in several countries. A seasonal pattern of dengue disease is consistently observed. The highest incidences usually correspond to the period of highest rainfall and humidity, providing suitable conditions for Aedes aegypti breeding and survival. In Brazil for instance it is from January to June. Dengue may cause marked changes in bone marrow that result in hypocellularity and, consequently, thrombocytopenia and leucopenia, along with an increase in hematocrit, which is secondary to capillary leakage. However, those abnormalities are usually self-limited, and do not warrant further investigations, such as a marrow biopsy or a myelogram. The occurrence of persistent reactive hemophagocytosis is uncommon and usually leads to serious adverse outcomes. The authors report the case of an 8-year old girl complaining of high-grade fever, malaise, headache, abdominal pain and a cutaneous rash. Laboratory examination revealed atypical lymphocytosis on peripheral blood count, hyperbilirrunemia, abnormal liver enzymes and clotting tests. Serology was positive for dengue. Because of the persistence of fever and laboratory examinations were consistent with hemophagocytic lymphohistiocytosis (HLH) a bone marrow aspiration was performed, which confirmed the presence of hemophagocytosis. Hence we report a rare presentation of dengue accompanied by self-limited HLH that hopefully evolve to favorable outcome.
Keywords : Dengue; Lymphohistiocytosis, Hemophagocytic; Bone Marrow Examination; Diagnosis
CASE REPORT
An 8-year-old female patient presented to the emergency care with a history of high-grade fever, malaise, and headache for the past 8 days, followed by abdominal pain and a cutaneous rash. She had been treated with penicillin because of a diagnosis of streptococcal pharyngitis, but had no relief of symptoms. Physical examination disclosed jaundice, fever (axillary temperature of 39.2 °C), painful hepatosplenomegaly, and a positive Rumpel–Leede test.
Laboratory findings on admission showed a normal peripheral blood count; however, a moderate atypical lymphocytosis was present. According to the epidemiological data and clinical features, the diagnosis of dengue was highly considered and further investigation revealed the following results: albumin = 2.9 g/dL (reference value [RV]: 3-5 g/dL); total bilirubin = 4.65 mg/dL (RV: 0.3-1.2 mg/dL) with conjugated bilirubin predominance; clotting tests represented by prothrombin time with international normalized ratio = 1.37 (RV: 1); activated partial thromboplastin time ratio = 1.53 (RV: 1); alanine aminotransferase = 412 U/L (RV: 34 U/L); and aspartate aminotransferase = 975 U/L (RV: 10-49 U/L). The abdominal ultrasonography revealed homogenous hepatosplenomegaly and a small amount of free liquid in the abdominal cavity.
Taking into account the clinical picture and the presence of lymphocytic atypia and hepatocellular injury, a broad work-up was mandatory, including serologies for cytomegalovirus, viral hepatitis types A, B, and C, Epstein-Barr virus, and toxoplasmosis, which were negative for immunoglobulin G (IgG) and immunoglobulin M (IgM) antibodies. Because of the persistence of fever, the negative results of the aforementioned serologies, and the low probability of malignancy, the hypothesis of HLH was considered. In this setting the dosage of fibrinogen was 105 mg/dL (RV: 175-400 mg/dL); triglycerides was 664 mg/dL (RV: <100 mg/dL); lactic dehydrogenase 1536 U/L (RV: 120-246 U/L); ferritin was 16,500 ng/mL (RV: 10-291 ng/mL); and bicytopenia ensued (anemia and leukopenia). On the nineteenth day of fever, the serology results for dengue and yellow fever (YF) became available, confirming dengue infection (IgM was positive for dengue and negative for YF).
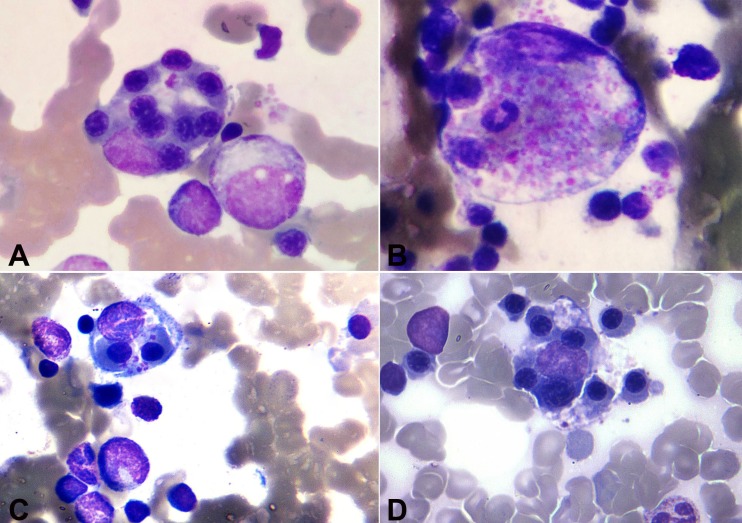
With these results, the hypothesis of HLH was strengthened and a myelogram was performed, which showed macrophages phagocyting red and white blood cells (Figure 1). Therefore, the diagnosis of HLH was confirmed based on the Histiocyte Society criteria.1 As HLH is a great cause of morbidity and mortality, our major concern was the path that the disease would follow; however, surprisingly, further physical examinations and laboratory tests improved progressively. The fever ceased without any specific treatment, which demonstrated a rare case of dengue that evolved with a self-limited HLH. The patient was discharged and periodically followed-up in the out-patient clinic without any further complaint.
Figure 1. A, B, C and D - Photomicrography of the bone marrow aspiration showing histiocytes phagocyting red blood cell precursors and white blood cell, characterizing hemophagocytosis.
DISCUSSION
Dengue is a viral self-limited infection with a broad spectrum of presentations ranging from classic dengue characterized by mild malaise and headache, the dengue hemorrhagic fever with increased capillary fragility and permeability associated with thrombocytopenia and bone marrow suppression,2-4 to the most severe form: dengue shock syndrome. The 2009 revised WHO criteria recommended the classification of dengue according to the severity of illness in: dengue without warning signs; dengue with warning signs (abdominal pain, persistent vomiting, fluid accumulation, mucosal bleeding, lethargy, liver enlargement, increasing hematocrit with decreasing platelets); and severe dengue (dengue with severe plasma leakage, severe bleeding, or organ failure).2,5
Although dengue is usually a self-limited disease, many complications have been described;2,6,7 among them the HLH has been increasingly reported.4-19
It is well known that HLH is associated with various infections—mainly viral.20 The syndrome is marked by an inflammatory cytokine storm with an overreaction of T-cell lymphocytes, which, in turn, activate and then recruit monocytes and macrophages, and eventually cause hemophagocytosis in the bone marrow, spleen and/or lymph nodes (one of the histologic criteria for diagnosis). The other criteria are cytopenia (at least two lineages), fever, splenomegaly, decreased fibrinogen and/or increased triglyceride determinations, low or absent natural killer cells activity, increased soluble CD25, and a marked increase in the serum ferritin levels. At least five of the aforementioned findings are required to confirm HLH. Diagnosis is usually challenging, as it can be easily mistaken with other clinical situations, such as sepsis or other systemic inflammatory response syndromes (SIRS).1,18,21
The association of dengue with HLH has been frequently reported.3,22 Many similarities involve dengue and HLH, such as a marked increase of cytokines dosages and thrombocytopenia. The diagnosis of dengue associated or not to HLH is somewhat challenging since hemophagocytic activity and increased determination of ferritin may be present in dengue without the development of HLH.1
While most HLH cases associated with dengue were observed in secondary and/or dengue with warning signs/severe dengue cases,9,16,18 our patient had a classic dengue without warning signs and only after developing HLH, did she presented liver injury, splenomegaly, and sustained bicytopenia. Therefore, clinicians should be alert to HLH not only during acute dengue infection, but also as a complication after the initial 7-day course of dengue infection, especially if there is a late onset of jaundice, splenomegaly, central nervous system symptoms, and SIRS.
Although HLH is generally a severe disease that requires specific and aggressive therapies (corticosteroids, etoposide, and cyclosporine A), the patient reported herein had a very uncommon clinical course. The prognosis of genetic HLH without treatment may be very poor, with a median survival of up to 2 months21 and a less than 10% likelihood of survival for 3 years.1 Therefore, bone marrow aspiration should be done, especially if fever persists or relapses along with other HLH symptoms and criteria.
Footnotes
Hein N, Bergara GH, Moura NBV, et al. Dengue fever as a cause of hemophagocytic lymphohistiocytosis. Autopsy Case Rep [Internet]. 2015;5(3):33-36. http://dx.doi.org/10.4322/acr.2015.016
REFERENCES
- 1.Aricò M, Janka G, Fischer A, et al. Hemophagocytic lymphohistiocytosis. Report of 122 children from the International Registry. FHL study group of the histiocyte society. Leukemia. 1996;10(2):197-203. PMid: [PubMed] [Google Scholar]
- 2.World Health Organization (WHO). Dengue: guidelines for diagnosis, treatment, prevention and control – new edition. Geneva: WHO/TDR; 2009. [PubMed] [Google Scholar]
- 3.Lei HY. Transient hemophagocytic activity in dengue immunopathogenesis. J Formos Med Assoc. 2009;108(8):595-8. http://dx.doi.org/10.1016/S0929-6646(09)60379-X. PMid: [DOI] [PubMed] [Google Scholar]
- 4.Lu PL, Hsiao HH, Tsai JJ, et al. Dengue virus-associated hemophagocytic syndrome and dyserythropoiesis: a case report. Kaohsiung J Med Sci. 2005;21(1):34-9. http://dx.doi.org/10.1016/S1607-551X(09)70274-8. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hadinegoro SRS. The revised WHO dengue case classification: does the system need to be modified? Paediatr Int Child Health. 2012;32(s1):33-8. http://dx.doi.org/10.1179/2046904712Z.00000000052. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rueda E, Méndez A, González G. Síndrome hemofagocítico asociado con dengue hemorrágico. Biomedica. 2002;22(2):160-6. http://dx.doi.org/10.7705/biomedica.v22i2.1155. PMid: [PubMed] [Google Scholar]
- 7.Vijayalakshmi AM, Ganesh VR. Hemophagocytic syndrome associated with dengue hemorrhagic fever. Indian Pediatr. 2009;46(6):545. PMid: [PubMed] [Google Scholar]
- 8.Lai M, Stirnemann J, Bibi-Triki T, et al. Dengue associée à un syndrome néphrotique et à un syndrome d’activation macrophagique. Med Mal Infect. 2012;42(1):30-2. http://dx.doi.org/10.1016/j.medmal.2011.09.008. PMid: [DOI] [PubMed] [Google Scholar]
- 9.Tan LH, Lum LCS, Omar SFS, Kan FK. Hemophagocytosis in dengue: comprehensive report of six cases. J Clin Virol. 2012;55(1):79-82. http://dx.doi.org/10.1016/j.jcv.2012.06.005. PMid: [DOI] [PubMed] [Google Scholar]
- 10.De Koninck AS, Dierick J, Steyaert S, Taelman P. Hemophagocytic lymphohistiocytosis and dengue infection: rare case report. Acta Clin Belg. 2014;69(3):210-3. http://dx.doi.org/10.1179/2295333714Y.0000000019. PMid: [DOI] [PubMed] [Google Scholar]
- 11.Srichaikul T, Punyagupta S, Kanchanapoom T, Chanokovat C, Likittanasombat K, Leelasiri A. Hemophagocytic syndrome in Dengue hemorrhagic fever with severe multiorgan complications. J Med Assoc Thai. 2008;91(1):104-9. PMid: [PubMed] [Google Scholar]
- 12.Nakamura I, Nakamura-Uchiyama F, Komiya N, Ohnishi K. [A case of dengue fever with viral-associated hemophagocytic syndrome]. Kansenshogaku Zasshi. 2009;83(1):60-3. PMid: [DOI] [PubMed] [Google Scholar]
- 13.Soler Rosario Y, Garcia R, Fernandez Sein A. Dengue virus associated hemophagocytic syndrome in children: a case report. Bol Asoc Med P R. 2010;102(1):49-54. PMid: [PubMed] [Google Scholar]
- 14.Jain D, Singh T. Dengue virus related hemophagocytosis: a rare case report. Hematology. 2008;13(5):286-8. http://dx.doi.org/10.1179/102453308X316095. PMid: [DOI] [PubMed] [Google Scholar]
- 15.Ribeiro E, Kassab S, Pistone T, Receveur MC, Fialon P, Malvy D. Primary dengue fever associated with hemophagocytic syndrome: a report of three imported cases, Bordeaux, France. Intern Med. 2014;53(8):899-902. http://dx.doi.org/10.2169/internalmedicine.53.1108. PMid: [DOI] [PubMed] [Google Scholar]
- 16.Kapdi M, Shah I. Dengue and haemophagocytic lymphohistiocytosis. Scand J Infect Dis. 2012;44(9):708-9. http://dx.doi.org/10.3109/00365548.2011.652667. PMid: [DOI] [PubMed] [Google Scholar]
- 17.Sharp TM, Gaul L, Muehlenbachs A, et al. Fatal hemophagocytic lymphohistiocytosis associated with locally acquired dengue virus infection - New Mexico and Texas, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(3):49-54. PMid: [PMC free article] [PubMed] [Google Scholar]
- 18.Rouphael NG, Talati NJ, Vaughan C, Cunningham K, Moreira R, Gould C. Infections associated with haemophagocytic syndrome. Lancet Infect Dis. 2007;7(12):814-22. http://dx.doi.org/10.1016/S1473-3099(07)70290-6. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wan Jamaludin WF, Periyasamy P, Wan Mat WR, Abdul Wahid SF. Dengue infection associated hemophagocytic syndrome: Therapeutic interventions and outcome. J Clin Virol. 2015;69:91-5. http://dx.doi.org/10.1016/j.jcv.2015.06.004. PMid: [DOI] [PubMed] [Google Scholar]
- 20.Simmons CP, Farrar JJ, van Vinh Chau N, Wills B. Dengue. N Engl J Med. 2012;366(15):1423-32. http://dx.doi.org/10.1056/NEJMra1110265. PMid: [DOI] [PubMed] [Google Scholar]
- 21.Henter JI, Samuelsson-Horne A, Aricò M, et al. Treatment of hemophagocytic lymphohistiocytosis with HLH-94 immunochemotherapy and bone marrow transplantation. Blood. 2002;100(7):2367-73. http://dx.doi.org/10.1182/blood-2002-01-0172. PMid: [DOI] [PubMed] [Google Scholar]
- 22.Nelson ER, Biebman HR, Chulajata R. Hematologic phagocytosis in postmortem bone marrows of dengue hemorrhagic fever: Hematologic phagocytosis in Thai hemorrhagic fever. Am J Med Sci. 1966;252(1):68-74. http://dx.doi.org/10.1097/00000441-196607000-00010. PMid: [PubMed] [Google Scholar]