Abstract
Gastrointestinal metastases from breast cancer are rare and generally occur several years after the diagnosis of the primary lesion. The diagnosis of gastric metastasis as the initial presentation of breast cancer is even rarer and can potentially mimic gastric carcinoma. We report the case of a 66-year-old female patient submitted to a total gastrectomy because of the histological diagnosis of undifferentiated gastric carcinoma. During the surgical procedure, biopsies of the peritoneum and the liver were performed, which were consistent with metastatic breast invasive lobular carcinoma (ILC). The primary lesion of the breast was detected during the post-operative period, when a 4-cm-long lesion was detected on physical examination and mammography. The revision of the gastric biopsy confirmed the diagnosis of ILC. The authors call attention to the rarity of gastrointestinal metastases as the initial presentation of breast ILC.
Keywords : Breast Neoplasm; Neoplasm Metastasis; Carcinoma, Lobular
INTRODUCTION
Metastatic breast cancer typically involves lymph nodes, bones, lung, liver, and brain.1 Gastrointestinal (GI) involvement and peritoneal carcinomatosis from primary breast cancer are rare with the incidence varying from 6% to 18% in autopsy series.2-5 In contrast to invasive ductal carcinoma (IDC), invasive lobular carcinoma (ILC) shows a distinct systemic metastatic pattern and has a higher incidence of metastases to the GI tract, gynecological organs, or peritoneum.6-8
Gastric metastases are slightly more frequent in autopsy reports;8,9 however, in the largest non-autopsy series involving women with breast cancer and GI metastases, 45% of the metastases involved the colon and the rectum, whereas the stomach accounted for 28%.10 Metastatic involvement of the stomach may occur many years after the diagnosis of the breast cancer, and is often part of an extensive systemic dissemination.10,11 The diagnosis of gastric metastasis as the initial presentation of breast cancer is rare, potentially mimicking gastric carcinoma.12,13
We report the case of a patient presenting with a pre-operative diagnosis of undifferentiated gastric carcinoma that was confirmed, subsequently, as metastatic ILC of the breast.
CASE REPORT
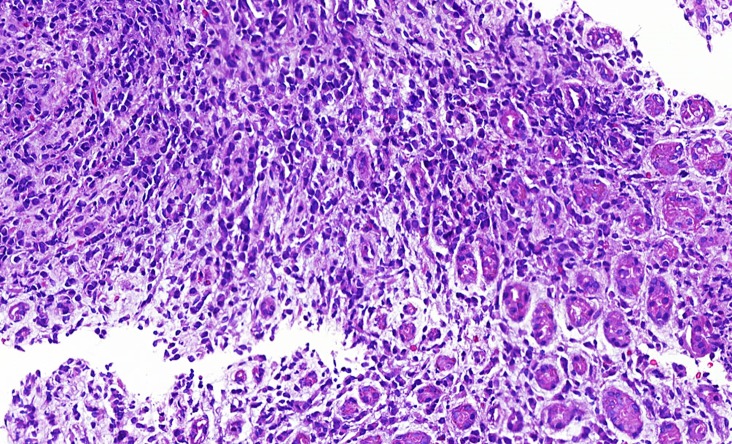
A 66-year-old woman presented with a 2-month history of epigastric pain, vomiting, and weight loss. The upper GI endoscopy demonstrated a circumferential lesion of body and antrum of the stomach with friable mucosa and areas of necrosis. A biopsy showed an undifferentiated neoplasm (Figure 1), which was initially diagnosed as adenocarcinoma by immunohistochemistry positivity for cytokeratin AE1/AE3 and negativity for CD20 and CD3.
Figure 1. Photomicrography of the biopsy of the stomach showing an undifferentiated neoplasm, infiltrative cords, and isolated small cells around the oxyntic gastric mucosa (H&E, 100X).
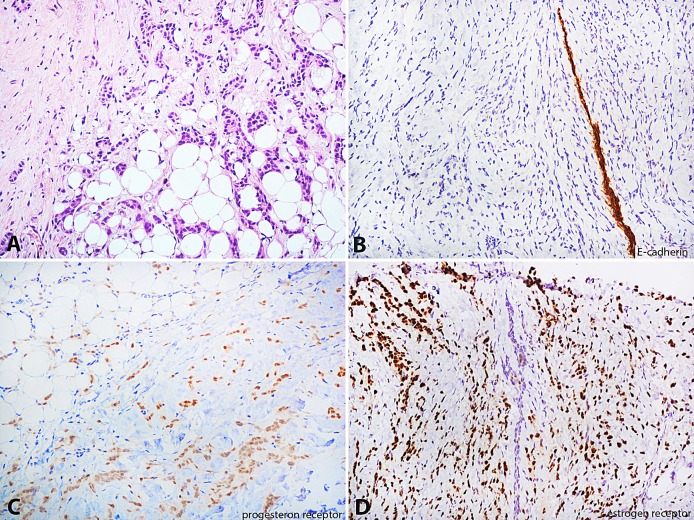
Subsequent abdominal computed tomography demonstrated parietal irregular thickening of the gastric wall, which was associated with densification of adjacent fat tissue determining gastric distension. The patient underwent a total gastrectomy accompanied by a lymphadenectomy and esophagojejunostomy with a Roux loop technique, a biopsy of the peritoneal lesions, and the resection of a liver nodule. In the post-operative period, a nodule in the lower medial quadrant of the left breast was evidenced on physical examination measuring 4 cm at its longest axis, which was subsequently evaluated by mammography and was irregular and spiculated. The histologic examination of the nodule’s biopsy revealed a low grade ILC, with the immunohistochemical positivity for estrogen receptors (90%), progesterone receptors (90%), negativity for Her2, E-cadherin, and Ki-67 of 10% (Figure 2).
Figure 2. Photomicrography of the breast nodule biopsy. A – Cords of small cells within the breast stroma (H&E, 200X); B – Infiltrating linear cords of cells E-cadherin negative around a positive normal breast duct (E-cadherin, 200X); C – Progesterone receptor positivity in neoplastic cells (progesterone receptor, 200X); D – Estrogen receptor positivity in neoplastic cells (estrogen receptor, 200X).
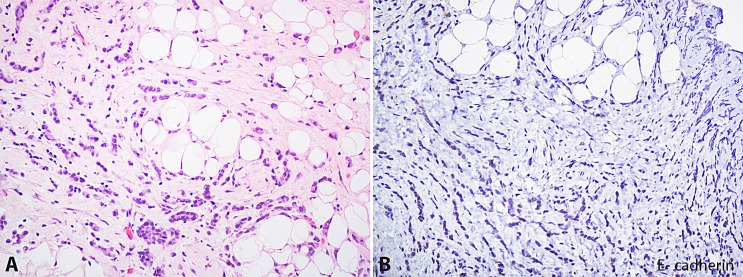
The histological analysis of the stomach, peritoneum, and liver showed metastatic ILC (Figure 3). The material from the upper GI endoscopy was reviewed and submitted to a new immunohistochemical panel showing positivity for cytokeratin 7 and estrogen receptors, and negativity for cytokeratin 20 and CDX-2, which was consistent with metastatic ILC.
Figure 3. Photomicrography of the peritoneal biopsy. A – Infiltrating linear cords of small malignant cells within the adipose tissue (H&E, 200X); B – Negative reaction for E-cadherin (E-cadherin, 200X).
The patient is currently being treated with anti-estrogen therapy (letrozole).
DISCUSSION
Breast cancer is one of the most common malignancies that metastasizes to the GI tract, along with melanoma and lung carcinoma.2,14 GI metastasis is far more commonly associated with ILC than IDC of the breast. During a 15-year study reported by a research team from Mayo Clinic in 2005, of the 53 patients with breast cancer and GI metastasis 64% were due to ILC.10 The loss of expression of E-cadherin in ILC is a probable explanation for this peculiar metastatic pattern compared with IDC.15
The metastasis to the GI tract generally occurs several years after the diagnosis of the primary breast lesion.10,11,16 McLemore et al.,10 in a retrospective review of 73 patients with breast cancer and GI tract or peritoneum metastasis, reported a median interval of 7 years between the primary diagnosis of breast cancer and GI metastatic presentation.
In our case, it seemed more reasonable to accept the diagnosis of gastric neoplasm, since there was a lack of previous history of breast malignancy, and the clinical presentation of gastric metastasis (from a breast cancer) is often indistinguishable from primary gastric cancer. The most frequent symptoms are anorexia, epigastric pain, dyspepsia, weight loss, vomiting, and melena.10,11,17 The endoscopic findings also may be very similar to primary gastric carcinoma.11 The most common pattern is a linitis plastica with diffuse infiltration of the submucosa and muscularis propria.11,18 However, the spectrum of endoscopic findings is large and includes polyps,11,18,19 erosions,20 ulcer lesions,21 and sometimes a normal exam.22
It is important to differentiate GI metastatic breast cancer from a potential surgically resectable primary gastric cancer. The histological features of a metastatic breast lobular carcinoma to the stomach consist of the infiltration of the gastric tissue by non-cohesive small tumor cells with an occasional intracytoplasmic lumen arranged in linear cords between the normal gastric glands.23 The signet ring morphology of lobular breast carcinoma may mimic that of the primary gastric cancer. Therefore, immunohistochemical staining is essential to reach the final diagnosis when a metastatic lesion is suspected. Metastatic breast carcinomas are usually positive for cytokeratin 7, estrogen receptors, progesterone receptors, GCDFP-15, and are negative for cytokeratin 20.16,24
Systemic therapy is the treatment for breast cancer that is metastatic to the stomach and other sites. The choice of systemic treatment (chemotherapy, hormonal therapy, or both) is based upon symptoms, age, performance status, and previous systemic treatments. Taal et al.11 reported a 46% response rate (17 out of 37 patients with gastric metastasis) in their patients treated with systemic therapy. The response to hormonal treatment and chemotherapy was similar in their group of patients. Palliative surgery is only recommended in cases of gastric obstruction.10,11 In the McLemore et al.10 series, 64% (47 out of 73 patients) underwent palliative surgical interventions for obstructive symptoms or mass effect. However, surgical palliation did not significantly improve the overall survival. Median overall survival of patients with gastric metastasis of the breast is equivalent to that of all women with metastatic breast disease, ranging from 24 to 36 months.10
Metastatic breast cancer involving the GI tract can produce a wide range of clinical and radiological presentations, often mimicking a GI malignancy. This report presents the case of a gastric metastasis as the first manifestation of an ILC of the breast. Unlike the majority of previously reported cases, in which the primary breast carcinoma had been well recognized, the breast lesion in this case was found after the metastatic approach. Despite the size of the breast lesion, the misdiagnosis most likely occurred because the patient's complaints were restricted to the dyspeptic symptoms, and a thorough examination was not performed. Breast examination should be carried out in all women with suspected neoplasia.
Footnotes
Dória MT, Maesaka JY, Martins SN Fo, et al. Gastric metastasis as the first manifestation of an invasive lobular carcinoma of the breast. Clinical Case Rep [Internet]. 2015;5(3):49-53. http://dx.doi.org/10.4322/acr.2015.018
REFERENCES
- 1.Kamby C, Sengeløv L. Pattern of dissemination and survival following isolated locoregional recurrence of breast cancer. A prospective study with more than 10 years of follow up. Breast Cancer Res Treat. 1997;45(2):181-92. http://dx.doi.org/10.1023/A:1005845100512. PMid: [DOI] [PubMed] [Google Scholar]
- 2.Menuck LS, Amberg JR. Metastatic disease involving the stomach. Am J Dig Dis. 1975;20(10):903-13. http://dx.doi.org/10.1007/BF01070875. PMid: [DOI] [PubMed] [Google Scholar]
- 3.Davis HL Jr, Murray RK, Korbitz BC. Breast carcinoma metastatic to the stomach. Report of a case in a male and review of an autopsy series. Am J Dig Dis. 1968;13(10):868-73. http://dx.doi.org/10.1007/BF02237571. PMid: [DOI] [PubMed] [Google Scholar]
- 4.Hartmann WH, Sherlock P. Gastroduodenal metastases from carcinoma of the breast. An adrenal steroid-induced phenomenon. Cancer. 1961;14(2):426-31. http://dx.doi.org/10.1002/1097-0142(196103/04)14:2<426::AID-CNCR2820140223>3.0.CO;2-H. PMid: [DOI] [PubMed] [Google Scholar]
- 5.Cummings MC, Simpson PT, Reid LE, et al. Metastatic progression of breast cancer: insights from 50 years of autopsies. J Pathol. 2014;232(1):23-31. http://dx.doi.org/10.1002/path.4288. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fondrinier E, Guérin O, Lorimier G. Etude comparative de l’évolution métastatique des carcinomes canalaires et lobulaires du sein à partir de deux séries appariées (376 patientes). Bull Cancer. 1997;84(12):1101-7. PMid: [PubMed] [Google Scholar]
- 7.Borst MJ, Ingold JA. Metastatic patterns of invasive lobular versus invasive ductal carcinoma of the breast. Surgery. 1993;114(4):637-41, discussion 641-2. PMid: [PubMed] [Google Scholar]
- 8.Taal BG, den Hartog Jager FCA, Steinmetz R, Peterse H. The spectrum of gastrointestinal metastases of breast carcinoma: I. Stomach. Gastrointest Endosc. 1992;38(2):130-5. http://dx.doi.org/10.1016/S0016-5107(92)70377-0. PMid: [DOI] [PubMed] [Google Scholar]
- 9.Taal BG, den Hartog Jager FCA, Steinmetz R, Peterse H. The spectrum of gastrointestinal metastases of breast carcinoma: II. The colon and rectum. Gastrointest Endosc. 1992;38(2):136-41. http://dx.doi.org/10.1016/S0016-5107(92)70378-2. PMid: [DOI] [PubMed] [Google Scholar]
- 10.McLemore EC, Pockaj BA, Reynolds C, et al. Breast cancer: presentation and intervention in women with gastrointestinal metastasis and carcinomatosis. Ann Surg Oncol. 2005;12(11):886-94. http://dx.doi.org/10.1245/ASO.2005.03.030. PMid: [DOI] [PubMed] [Google Scholar]
- 11.Taal BG, Peterse H, Boot H. Clinical presentation, endoscopic features, and treatment of gastric metastases from breast carcinoma. Cancer. 2000;89(11):2214-21. http://dx.doi.org/10.1002/1097-0142(20001201)89:11<2214::AID-CNCR9>3.0.CO;2-D. PMid: [PubMed] [Google Scholar]
- 12.Nazareno J, Taves D, Preiksaitis HG. Metastatic breast cancer to the gastrointestinal tract: a case series and review of the literature. World J Gastroenterol. 2006;12(38):6219-24. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vennapusa B, Oman SA, Parasher G, Cerilli LA. C-kit-positive gastric metastasis of lobular carcinoma of the breast masquerading as gastrointestinal stromal tumor. Breast Cancer. 2010;17(4):303-5. http://dx.doi.org/10.1007/s12282-009-0116-x. PMid: [DOI] [PubMed] [Google Scholar]
- 14.Taal BG, Boot H, van Heerde P, de Jong D, Hart AA, Burgers JM. Primary non-Hodgkin lymphoma of the stomach: endoscopic pattern and prognosis in low versus high grade malignancy in relation to the MALT concept. Gut. 1996;39(4):556-61. http://dx.doi.org/10.1136/gut.39.4.556. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sastre-Garau X, Jouve M, Asselain B, et al. Infiltrating lobular carcinoma of the breast. Clinicopathologic analysis of 975 cases with reference to data on conservative therapy and metastatic patterns. Cancer. 1996;77(1):113-20. http://dx.doi.org/10.1002/(SICI)1097-0142(19960101)77:1<113::AID-CNCR19>3.0.CO;2-8. PMid: [DOI] [PubMed] [Google Scholar]
- 16.Ayantunde AA, Agrawal A, Parsons SL, Welch NT. Esophagogastric cancers secondary to a breast primary tumor do not require resection. World J Surg. 2007;31(8):1597-601. http://dx.doi.org/10.1007/s00268-007-9099-y. PMid: [DOI] [PubMed] [Google Scholar]
- 17.Pectasides D, Psyrri A, Pliarchopoulou K, et al. Gastric metastases originating from breast cancer: report of 8 cases and review of the literature. Anticancer Res. 2009;29(11):4759-63. PMid: [PubMed] [Google Scholar]
- 18.Jones GE, Strauss DC, Forshaw MJ, Deere H, Mahedeva U, Mason RC. Breast cancer metastasis to the stomach may mimic primary gastric cancer: report of two cases and review of literature. World J Surg Oncol. 2007;5:1-6. http://dx.doi.org/10.1186/1477-7819-5-75. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dumoulin FL, Gupta RS. Breast cancer metastasis to the stomach resembling small benign gastric polyps. Gastrointest Endosc. 2009;69(1):174-5. http://dx.doi.org/10.1016/j.gie.2008.03.1082. PMid: [DOI] [PubMed] [Google Scholar]
- 20.Pera M, Riera E, Lopez R, Viñolas N, Romagosa C, Miquel R. Metastatic carcinoma of the breast resembling early gastric carcinoma. Mayo Clin Proc. 2001;76(2):205-7. http://dx.doi.org/10.1016/S0025-6196(11)63129-7. PMid: [DOI] [PubMed] [Google Scholar]
- 21.Reiman T, Butts CA. Upper gastrointestinal bleeding as a metastatic manifestation of breast cancer: a case report and review of the literature. Can J Gastroenterol. 2001;15(1):67-71. PMid: [DOI] [PubMed] [Google Scholar]
- 22.Critchley AC, Harvey J, Carr M, Iwuchukwu O. Synchronous gastric and colonic metastases of invasive lobular breast carcinoma: case report and review of the literature. Ann R Coll Surg Engl. 2011;93(5):49-50. http://dx.doi.org/10.1308/147870811X582800. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Almubarak MM, Laé M, Cacheux W, et al. Gastric metastasis of breast cancer: a single centre retrospective study. Dig Liver Dis. 2011;43(10):823-7. http://dx.doi.org/10.1016/j.dld.2011.04.009. PMid: [DOI] [PubMed] [Google Scholar]
- 24.Kaufmann O, Deidesheimer T, Muehlenberg M, Deicke P, Dietel M. Immunohistochemical differentiation of metastatic breast carcinomas from metastatic adenocarcinomas of other common primary sites. Histopathology. 1996;29(3):233-40. http://dx.doi.org/10.1111/j.1365-2559.1996.tb01396.x. PMid: [DOI] [PubMed] [Google Scholar]