Abstract
Study Objective
Emergency Department (ED) closures threaten community access to emergency services, but few data exist to describe factors associated with closure. We evaluated factors associated with ED closure in California and sought to determine if hospitals serving more vulnerable populations have a higher rate of ED closure.
Methods
Retrospective cohort study of California hospital EDs between 1998 and 2008, using hospital and patient level data from the California Office of Statewide Planning and Development (OSHPD), as well as OSHPD Patient Discharge Data. We examined the effects of hospital and patient factors on the hospital's likelihood of ED closure using Cox proportional hazards models.
Results
In 4,411 hospital-years of observation, 29 of 401 (7.2%) EDs closed. In a model adjusted for total ED visits, hospital discharges, trauma center and teaching status, ownership, operating margin, and urbanicity, hospitals with more black patients (OR 1.41 per increase in proportion of blacks by 0.1, 95% CI 1.16-1.72) and Medi-Cal recipients (OR 1.17 per increase in proportion insured by Medi-Cal by 0.1, 95% CI 1.02-1.34) had higher odds for ED closure, as did for-profit institutions (OR 1.65, 95% CI 1.13-2.41).
Conclusion
The population served by EDs and hospitals’ profit model are associated with ED closure. Whether our findings are a manifestation of poorer reimbursement in at-risk EDs is unclear.
Introduction
Emergency departments (EDs) are often referred to as the safety-net of the healthcare system.1 Nationally, the US population has experienced a decrease in availability of emergency care accompanied by an increase in patient volumes and simultaneous deterioration of health for those seen in EDs.2,3 Between 1990 and 2009, the annual number of ED visits increased over 40% (from 88.5 million to 127.3 million)4, as the number of EDs decreased 27%5, with an increasing proportion of the remaining EDs considered “safety-net EDs.” 3 Rise in ED use and fall in availability have stirred significant concern, particularly following passage of the Patient Protection and Affordable Care Act of 2010.6-12
California has experienced parallel trends in ED availability and usage. Between 1990 and 2001 the total number of California hospitals that had an ED fell by 12% (from 407 to 357).13,14 Over a similar period, there was a 27% increase in total patient visits per ED as well as a significant rise in critically ill patient visits.13-16 Polls suggest that Californians are similarly concerned about the availability, affordability, and quality of emergency care services.17,18
Data on risk factors predicting ED closure are sparse. Studies of hospital closures suggest that worsening strain on the healthcare system and financial insecurity may be associated with a decline in services that are less profitable, such as emergency care.7,19-21 Perhaps not surprisingly, decline in hospital services disproportionately affects indigent populations.22
The primary objective of this study was to determine characteristics associated with ED closure in California. A recent national analysis showed that ED closure was associated with for-profit ownership, safety-net status, low profit margin, location in a competitive market, and location in high-poverty communities.5 Here, we evaluated whether such results remain true at the regional level. Data for the national study was obtained from American Hospital Association (AHA) Annual Surveys, which suffer declining response rates by year and varying response rates by data item.5 California is an ideal case study, with more robust data available as well as several recent ED closures that have caught public and media attention.15,17 Given the paucity of data available on ED closures, it is important to evaluate if similar trends are demonstrated at the national and regional level. Additionally, such analysis may offer meaningful information for statewide policy officials and uncover findings that were not demonstrated on the national scale. In particular, we sought to determine if hospitals serving more vulnerable populations, defined as communities with higher proportion of minority and poorly insured individuals, have a higher rate of ED closure.
Methods
Study Design
We conducted a retrospective cohort study of California hospital EDs between 1998 and 2008.
Data sources and variables
Our study focused on California EDs and hospitals using publicly available data. These data came from multiple sources, including the California Office of Statewide Health Planning and Development (OSHPD), the American Hospital Association (AHA), and the United States Census data (2000). OSHPD hospital annual utilization reports, financial data, and patient discharge data (PDD) were our primary source of data. The OSPHD database used for this California analysis is very detailed and has a response rate of almost 100% every year for all acute care, non-federal hospitals (very rarely are there cases of delayed reporting due to circumstances such as closures, changes in ownership, or new openings; in rare instances hospitals must seek permission or obtain a waiver for not reporting); this is comparison to the AHA database used in a recent national analysis5, which is by self-report and where response rates vary by year (i.e., 92% from 1990-1994, 85% 1995-1999, 86% 2000-2007, and 84% for 2008-2009) and have declined over time. Therefore not all the hospitals within the sample are captured longitudinally every year. Our internal checks between our AHA data and the California OSHPD show that the California data are much more complete.
Our key OSHPD data included patient-level demographic variables as well as hospital structural characteristics previously reported to be associated with ED utilization and closure.13,14,19,20,23-26 Using OSHPD's socioeconomic information of patients seen in each hospital, we created hospital-level aggregates for each year to determine the racial/ethnic and insurance composition of the hospitals’ patient pool. Specifically, we used PDD information to identify patients’ race/ethnicity to calculate the proportion of white non-Hispanics, black non-Hispanics, Hispanics, and other (including Asian, Native American, Alaska Native, Hawaiian, Pacific Islanders, and unknown/masked), and also to calculate the proportions of Medicare, Medicaid (specifically, Medi-Cal, which is California's Medicaid program), uninsured, privately insured, and other forms of insurance (i.e., VA, Tricare, Champus, Workers Compensation etc.). We categorized the data into ten categories, each representing a 10% interval, in order to improve the interpretability of the estimated model coefficients.
For hospital structural characteristics, we included trauma center status, teaching affiliation (e.g., teaching hospital or non-teaching hospital), ownership (for profit, not-for-profit, county), and hospital-level characteristics including operating margin, annual number of ED visits, number of hospital beds, number of hospital discharges, and location in a rural/urban county. For degree of urbanicity, we used the 2003 Beale code of the US Department of Agriculture's Economic Research Service. We divided counties into metro (Beale code 1, 2, and 3) and non-metro counties (Beale codes 4-9). For trauma center status, we manually confirmed dates of availability and level of service with the Emergency Medical Services Authority (EMSA) yearly reports and called individual facilities if there was any missing information.27 For annual ED visits and hospital discharges, AHA data was used to supplement missing data from OSHPD data (using AHA admission data as a proxy for OSHPD discharges due to lack of full compatibility). This imputation of missing data contributed a small amount of the total data for those variables (4% and 5%, respectively).
After checking and correcting for obvious data errors and omissions (e.g., single year missing ED status in the 1998-2008 period), we imputed incomplete hospital data using a multivariate normal imputation model that retained the mean and variance-covariance structure of the data while allowing gaps to be filled in with reasonable estimates using all available information. We used the rnorm() function with the vector of variable means and their variance-covariance matrix in the statistical programming language and environment R (version 2.10.1). We obtained approval from the University of California at San Francisco Institutional Review Board.
Outcome
Our outcome was time until ED closure. ED closures could come from either closures of hospitals that had an ED, or ED-only closures (where the hospital remained open). We chose to measure ED closures as a whole because of our desire to analyze services from the patient perspective and evaluate access to emergency services. We detected closures using service line variables present in OSHPD data indicating whether or not each hospital had an ED and whether or not each hospital was open during each year. Similarly, openings of EDs were identified when a new hospital opened or an existing hospital opened an ED during the study time period. Closures were not compared with openings but rather, with all existing hospitals offering emergency medical services, regardless of opening year.
Primary Data Analysis
We started our analysis with the premise that both patient-level and hospital-level factors influence the decision to close an ED. Based on previous literature describing characteristics associated with decreased access to care we a priori included the following predictor variables:percent race/ethnicity, percent insurance status, total ED visits of the hospital, hospital discharges, trauma center status based on EMSA designation (Level I or II = yes; all others = no), teaching affiliation (yes/no), hospital ownership (for-profit, not-for-profit, and county), operating margin, and location in an urban county.20,23,28-36 Individual patient-level data were aggregated into hospital-level proportions of race/ethnicity (white non-Hispanic, black non-Hispanic, Hispanic, and other non-Hispanic) and insurance status (% with Medicare, Medi-Cal, uninsured, private insurance, and other). We log-transformed the annual number (in thousands) of ED visits and hospital discharges because of skew in these variables.
We first characterized our data using univariate and bivariate comparisons. We then used Cox proportional hazard models to examine the effects of the selected predictors on the closure of EDs during our study time period, with and without adjusting for annual ED visits and hospital discharges. We separately estimated the effects of hospital-level race/ethnicity mix, payor mix, and hospital characteristics with the base model (adjusting for annual ED visits and hospital discharges), respectively, and then performed a multivariate regression with all factors combined. All analyses were performed with SAS 9.2 (Cary, NC) and R version 10.1 (www.r-project.org).37
We checked the assumptions of the Cox proportional hazards model by testing each individual predictor in our final models both graphically and formally. Graphical tests included visual inspection for proportionality, i.e., parallel lines, of estimated survival functions and survival time as well as plots of log(-log(survival)) versus log(survival times). For continuous predictors and those with many levels, we primarily relied on formal tests of proportionality using scaled Schoenfeld residuals. Neither the plots nor formal testing indicated any serious violation of the proportional hazards assumption for any of the predictors. The fraction of missing data was small (4-5% substituted with AHA data and up to 12% imputed) and the multivariate normal imputation model produced plausible results and did not affect the marginal distribution of the original data nor the covariance structure. Due to the relatively small number of ED closures (29) we also performed a sensitivity analysis by conducting both a cross-validation of the data (validating on a randomly selected and reserved 25% of hospitals) and by drawing 500 blocked bootstrap samples and then re-estimating each of the models. The results were robust to our findings using the whole sample.
Results
Of 401 hospitals, we identified 29 (7.2%) ED closures over the available 4,411 hospital-years of observation. Hospitals experiencing ED closure had fewer annual ED visits and hospital discharges, and served a higher proportion of black patients and Medi-Cal patients, and lower proportion of white and privately insured patients (Table 1).
Table 1.
Characteristics of hospitals/patients that experienced Emergency Department closure compared with those that did not
| In EDs that experienced closure | In EDs that did not experience closure | |||||||
|---|---|---|---|---|---|---|---|---|
| N | Median or % of sample | IQR | N | Median or % of sample | IQR | Absolute difference | 95% CI for absolute difference | |
| Total ED visits | 29 | 2.46 | [1.30, 3.39] | 372 | 3.14 | [2.32, 3.67] 0.49 | [0.26, 0.73] | |
| Discharges | 29 | 0.66 | [0.00, 1.46] | 372 | 1.48 | [0.61, 2.23] | 0.52 | [0.37, 0.67] |
| Trauma center | 3 | 10.34% | -- | 65 | 17.47% | -- | 7.13% | [-4.26%, 18.52%] |
| Level I | 1 | 3.45% | -- | 16 | 4.30% | -- | 0.85% | [-5.85%, 7.56%] |
| Level II | 3 | 10.34% | -- | 41 | 11.02% | -- | 0.68% | [-10.44%, 11.79%] |
| Level IV | 0 | 0.00% | -- | 11 | 2.96% | -- | 2.96% | [1.24%, 4.68%] |
| Teaching | 4 | 13.79% | -- | 30 | 8.06% | -- | 5.73% | [-7.04%, 18.5%] |
| Rural | 27 | 93.10% | -- | 353 | 94.89% | -- | 1.79% | [-7.53%, 11.11%] |
| Control | 29 | 100.00% | -- | 363 | 97.58% | -- | 2.42% | [0.86%, 3.98%] |
| For-Profit | 11 | 37.93% | -- | 86 | 23.12% | -- | 14.81% | [-3.21%, 32.84%] |
| Non For-Profit | 18 | 62.07% | -- | 271 | 72.85% | -- | 10.78% | [-7.16%, 28.72%] |
| County | 3 | 10.34% | -- | 19 | 5.11% | -- | 5.24% | [-6.08%, 16.55%] |
| Operating margin | 29 | -0.1 | [-0.26, 0.03] | 372 | 0.01 | [-0.07, 0.06] | 0.11 | [0.07, 0.14] |
| Race/Ethnicity | ||||||||
| Whites | 29 | 28.33 | [13.97, 44.64] | 372 | 43.54 | [24.64, 60] | 11.7 | [8.28, 15.12] |
| Blacks | 29 | 1.87 | [0.52, 7.04] | 372 | 1.13 | [0.30, 4.61] | 3.02 | [1.07, 4.97] |
| Hispanics | 29 | 14.91 | [2.62, 27.37] | 372 | 11.92 | [3.61, 25.8] | 1.83 | [-1.58, 5.24] |
| Other race | 29 | 1.4 | [0.57, 2.52] | 372 | 2.01 | [0.70, 5.03] | 2.1 | [1.56, 2.65] |
| Insurance | ||||||||
| Medicare | 29 | 33.55 | [24.79, 44.78] | 372 | 34.84 | [26.16, 46.28] | 0.55 | [-3.35, 2.25] |
| Medi-Cal | 29 | 28.33 | [14.29, 45.24] | 372 | 20.32 | [9.65, 34.59] | 7.02 | [3.81, 10.23] |
| Private | 29 | 18.59 | [10.19, 30.79] | 372 | 28.85 | [17.91, 43.8] | 8.91 | [6.34, 11.47] |
| Uninsured | 29 | 1.87 | [0.81, 4.12] | 372 | 1.63 | [0.81, 3.27] | 0.91 | [-0.31, 2.13] |
| Other insurancet | 29 | 4.48 | [2.82, 7.69] | 372 | 3.62 | [2.16, 5.98] | 1.8 | [0.75, 2.86] |
Other insurance includes a combination of several smaller insurance groups, such as VA, Tricare, Champus, and Workers Compensation. Other insurance makes up 5-6% of the total insurance pool.
Table 2 displays both the unadjusted and adjusted associations with ED closure. In unadjusted analysis, county-owned hospitals (HR 2.79, 95% CI 1.61-4.84) and for-profit hospitals (HR 2.14, 95% CI 1.53-3.00) were more likely to close, as were hospitals with a higher proportion of black patients (HR 1.58 for every 0.1 increase in proportion served, 95% CI 1.33-1.89) and Medi-Cal recipients (HR 1.18, 95% CI 1.09-1.28). Higher operating margin and hospital discharges, as well as a higher proportion of Medicare patients, were associated with lower hazard of ED closure.
Table 2.
Hazard of ED closure
| Unadjusted Hazard Ratio | 95% CI | Adjusted Hazard Ratio | 95% CI | |
|---|---|---|---|---|
| Patient demographics | ||||
| Percent Race/ethnicity | ||||
| White (10%) | 0.74 | [0.69, 0.80] | Ref | -- |
| Blacks (10%) | 1.58 | [1.33, 1.89] | 1.41 | [1.16, 1.72] |
| Hispanics (10%) | 1.06 | [0.98, 1.16] | 0.92 | [0.81, 1.05] |
| All other (10%) | 1.10 | [1.00, 1.20] | 1.00 | [0.89, 1.11] |
| Percent Insurance (%) | ||||
| Private (10%) | 1.10 | [0.87, 1.39] | Ref | -- |
| Medicare (10%) | 0.90 | [0.82, 0.99] | 1.00 | [0.88, 1.14] |
| Medi-Cal (10%) | 1.18 | [1.09, 1.28] | 1.17 | [1.02, 1.34] |
| Uninsured (10%) | 1.10 | [0.87, 1.39] | 0.95 | [0.69, 1.31] |
| Other (10%) | 1.70 | [1.36, 2.12] | 1.70 | [1.19, 2.42] |
| Hospital and ED structura features | ||||
| Total ED visits (per 1000, log-transformed) | 0.87 | [0.76, 1.01] | 0.89 | [0.77, 1.02] |
| Hospital discharges (per 1000, log-transformed) | 0.84 | [0.74, 0.97] | 0.58 | [0.46, 0.72] |
| Trauma center | 1.31 | [0.76, 2.29] | 1.22 | [0.64, 2.33] |
| Teaching Hospital | 1.29 | [0.65, 2.56] | 0.59 | [0.24, 1.43] |
| Ownership | ||||
| For-Profit | 2.14 | [1.53, 3.00] | 1.65 | [1.13, 2.41] |
| County | 2.79 | [1.61, 4.84] | 0.90 | [0.38, 2.15] |
| Operating Margin | 0.43 | [0.33, 0.58] | 0.43 | [0.30, 0.63] |
| Urbanicity (metro) | 1.83 | [1.05, 3.22] | 1.44 | [0.79, 2.63] |
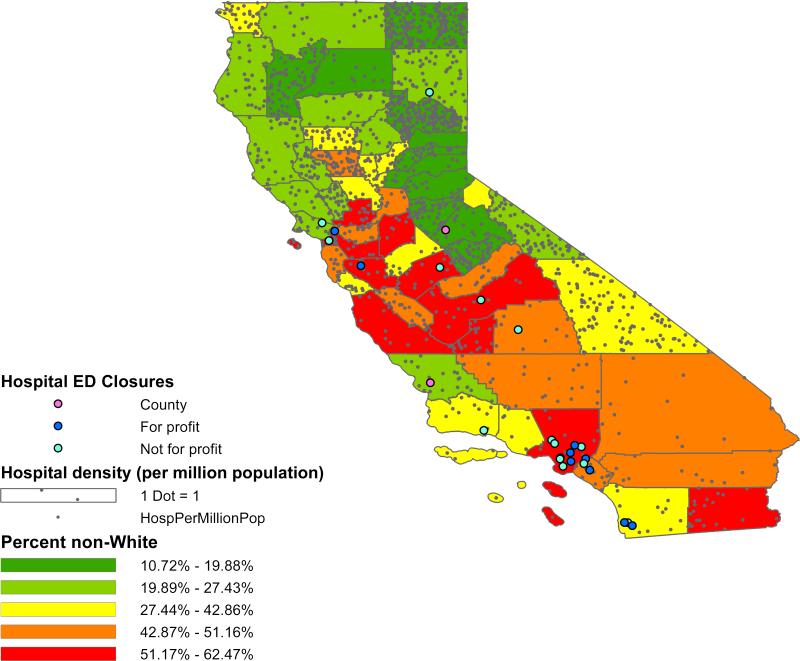
When all covariates were included in the model (Table 2), the proportion of patients admitted to the hospital who were black (HR 1.41, 95% CI 1.16-1.72) remained a strong risk factor for ED closure. We rescaled race/ethnicity and insurance status so that each unit change of each continuous variable represents a 10% increase in proportion of population. In other words, each increase of 0.1 in the proportion of black individuals increased the odds of closure by 41%. Figure 1 presents a map of California ED closures overlapped with proportion of non-white patients in the county and hospital density (measured as the number of hospitals per million population). This map illustrates that closures do appear to be occurring in areas with high proportions of non-white patients. These closures are not simply in areas with increased hospital density per population. Additionally, in the final model, the relationship of Medi-Cal insurance to ED closure persisted (HR 1.17, 95% CI 1.02-1.34). Facilities with higher hospital discharges (HR 0.58, 95% CI 0.46-0.72) and operating margin (HR 0.43, 95% CI 0.30-0.63) were less likely to experience ED closure. Finally, for-profit hospitals were over 50% more likely to close (HR 1.65, 95% CI 1.13-2.41) than not-for-profit hospitals.
Figure 1.
Hospital ED Closures, 1999-2008
In our sensitivity analyses, the results were nearly identical in the cross-validation and the 500 blocked bootstrap analyses, the most volatile predictor being hospital control (county, for-profit, not-for-profit). We then tested for collinearity between hospital- and patient-level measures that might be expected to group, and found no evidence for this potential threat. For example, the rank correlation coefficient using Kendall's tau between the proportion of blacks and those with Medi-Cal insurance was very low (0.09 to 0.13 over our study period).
Limitations
Our study has several limitations. First, our study timeframe from 1998 to 2008 covers 2 periods of substantial economic adjustment, the burst of the Internet bubble in 2000, and the economic and financial crises that began in 2007. How our data would apply to hospitals in the current economic environment, and upon the implementation of healthcare reform legislation is uncertain. However, given that healthcare financing and delivery remains largely private, it is conceivable that the trends in closures we report may well apply in the current environment. Second, ED closure was a fairly rare event in our study but the sample size is large enough to ensure validity of our results. Third, to determine the racial/ethnic and insurance composition of the hospitals’ patient pool, we used aggregate-level data, which may introduce bias. This is a common approach in healthcare research, and we attempted to control for relevant hospital and community factors to minimize any bias. Demographic differences seen in areas of higher population density may skew our results. For example, the relationship between ED closure and race may be driven by the higher density of African Americans living in LA County, and thus may not be generalizable to the rest of California. Both OSHPD and AHA data are self-reported and are susceptible to reporting errors. While our retrospective cohort approach has advantages for this type of analysis, we had limited control over the accuracy and completeness of the data included in the AHA survey. However, as long as the errors do not systematically differ by the community characteristics we examined, we do not expect to have a bias in the results. Our findings cannot differentiate between hospitals where both the hospital and ED close and hospitals where only the ED closes. There may be important differences between these groups, and it is conceivable that certain risk factors may be unique to one group. Finally, ED closure does not necessarily translate into subsequent poor access to emergency services or worse clinical outcomes. Other investigators have argued the impact of ED closures have largely been offset by increasing ED capacity at surrounding facilities13 or by alternative sites of care (i.e., an urgent care clinic on the Martin Luther King, Jr./Drew Medical Center). Even in these cases, however, patients obviously still experience significant differences in their geographic access to the same level of care, and it is well-documented that increased geographic distance is associated with decreased utilization.58,62
Discussion
Between 1998 and 2008, closure of emergency departments in California was relatively infrequent, but appeared more likely to occur in hospitals that admitted a higher proportion of black and Medi-Cal patients, and also in for-profit hospitals.
Our data suggest yet another mechanism whereby access to care may be reduced among vulnerable populations. An increasing proportion of Medicaid patients are using ED services for their care and have largely accounted for the increase in total number of ED visits experienced nationally.3,24,38 Black patients more frequently rely on ED use25 as they tend to lack access to primary care services.39,40 Our data provide support for a potential association between these factors and ED closure, and further suggest that the effects of payor mix, longer-term access to care issues, and race all exert important influences on ED closure rates. The exact pathways underpinning these interactions are not easily discerned from our data, but they appear to comprise independent effects on risk for ED closure. This suggests that the pathways leading to ED closures are diverse. While it is possible, and even likely, that poor Medicaid reimbursement rates are partially responsible for higher risk of ED closure, we cannot identify a similar underlying mechanism for black patients.
Of interest, for-profit ownership is associated with higher risk of ED closure, a finding that held after adjusting for other patient and hospital factors. Previous work suggests that for-profit hospitals typically exit markets as economic conditions warrant.41,42 Our data are concordant with the few previous studies available5, and confirm the notion that the higher likelihood of ED closure among for-profit centers represents a natural adaptation to financial stresses.
Overall, our findings are consistent with a recent report of a national trend of risk factors for ED closures which show that safety-net hospitals (which see a high proportion of patients with Medicaid) and for-profit ownership are associated with closures.5 Our study, in comparison with the national study, includes more detailed information regarding patient-level demographics, specifically insurance status. Rather than depending on the Area Resource File (ARF) for demographic characteristics (such as percent uninsurance as well as race/ethnicity) by county, our California-specific data allows us calculate the exact proportion of patients yearly by hospital rather than county. This is a distinct advantage especially in large counties such as Los Angeles, where clearly the composition of patient demographics varies widely across hospitals within the same county. Furthermore, county population characteristics available within the ARF provide only the percent uninsured and unfortunately do not contain information regarding the proportion of Medicaid, private, and Medicare patients. The granularity of our California data therefore allow more precise calculations of factors that are attributed to each hospital.
Our regional analysis substantiates and advances current knowledge by showing that EDs in California in particular are also more likely to close if they serve a high proportion of black patients. The etiology of this relationship is likely multifactorial, but could signal that these hospitals face other challenges in providing quality and cost-effective care.43,44 The same relationship was not seen with Hispanic patients, a population that has traditionally been considered vulnerable as well. Our finding is less surprising in California, which has a significantly higher proportion of Hispanic people relative to the national average45, and where prior studies have shown similar trends in racial/ethnic disparities.46 Our statewide analysis also reveals a cluster of ED closures in LA County. This may contribute to the relationship seen between ED closures and black patients, as LA County also has a higher proportion of black individuals compared to the remainder of California.47
The relationship between ED closure and race, as well as the cluster of closures in LA County, both demonstrate the importance of regional evaluation. Such findings were not noted in the recent national analysis of ED closures5, and should guide California policy officials. They may be illustrative of trends seen in other states.
Fewer EDs are located in areas with poorly insured residents after controlling for the community's household income,34 and hospitals are more likely to add ED capacity in suburban markets serving patients with more secure insurance profiles.7,34 With such hospitals (a significant proportion which carry non-profit status) becoming increasingly unwilling to provide benefit to vulnerable communities, some may question current tax benefits for these facilities. Some Californian counties have opted to increase property tax specifically to offset uncompensated traumatic and emergent care in LA County.48 The California senate recently approved legislation to guarantee improved Medi-Cal reimbursement rates at a new private hospital that will likely care for a vulnerable communities in south Los Angeles County.49 While the IOM has similarly advocated dedicated funding to reimburse uncompensated emergency care,50 we believe additional system-wide changes must also occur to alleviate current trends. Expanding access to and improving the quality of urgent care and primary care resources are crucial. Examples of this include expanding a) the network of community healthcare centers, b) evening and weekend hours, and c) access to patient-provider telephone and electronic communication. Such alternatives offer shorter waiting times, more convenient locations, and lower cost solutions to ED care.15,51,52 Some communities have opted to educate residents about primary care services and work toward better management of chronic diseases such as asthma and diabetes.53 Additionally, improving access to specialists, even through regionalization of services, is also imperative to the continued care of safety net communities.50,54 Addressing the racial and ethnic disparities will require a concerted effort and continued focus on workforce diversity and cultural competency.55,56
EDs are mandated under federal law to screen patients and provide urgent and emergent care regardless of the patient's ability to pay. ED closures can increase the geographic distance which has been shown to result in decreased utilization of care.57 ED closure disproportionately impacts vulnerable populations and leads to decreased ED utilization in these groups.21,58 Moreover, closure of an ED has also been associated with poor patient outcomes, as well as increased wait times, ambulance diversion to surrounding hospitals, and proportions of those who leave without having been seen.15,54,59-61 Given that EDs help care for a disproportionate share of vulnerable communities, it is concerning that the very populations that most rely on their services may experience declines in access to emergency care. Future research on ED closure must further delineate and quantify the impact of such trends on health outcomes.
Our study reveals important insights into factors contributing to the continued decline in availability of emergency health care services in California. Although California is experiencing similar increases in demands for ED services as ED availability falls, whether our results hold true elsewhere remains to be examined. Nonetheless, our results suggest that ED closures have the potential to magnify health disparities in vulnerable populations.
Acknowledgments and funding
We are grateful for the assistance of Amy J. Markowitz, JD, in the revision of this manuscript. We also thank Tiffany Wang, BA, for her administrative support. This publication was supported NIH/NCRR/OD UCSF-CTSI Grant Number KL2 RR024130 (RYH), the National Heart, Lung, and Blood Institute Grant Number K24HL098372 (ADA), and the Robert Wood Johnson Foundation Physician Faculty Scholars (RYH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of any of the funding agencies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
There are no other conflicts of interest.
Contributor Information
Renee Y. Hsia, Department of Emergency Medicine, University of California San Francisco, San Francisco General Hospital, San Francisco, CA USA.
Tanja Srebotnjak, University of California, San Francisco, San Francisco, CA USA.
Hemal K. Kanzaria, Department of Emergency Medicine, University of California, San Francisco, San Francisco General Hospital, San Francisco, CA USA.
Charles McCulloch, Department of Epidemiology and Biostatistics, University of California San Francisco, San Francisco, CA USA.
Andrew D. Auerbach, Department of Medicine, Division of Hospital Medicine, University of California, San Francisco, San Francisco, CA USA.
References
- 1.Felland LE, Hurley RE, Kemper NM. Safety Net Hospital Emergency Departments: Creating Safety Valves for Non-urgent Care. Center for Studying Health System Change; Washington D.C.: 2008. [PubMed] [Google Scholar]
- 2.Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data. 2007:1–32. [PubMed] [Google Scholar]
- 3.Tang N, Stein J, Hsia RY, et al. Trends and characteristics of US emergency department visits, 1997-2007. Jama. 2010;304:664–70. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.AHA. Avalere Health analysis of American Hospital Association Annual Survey data for community hospitals. US Census Bureau: National and State Population Estimates. Emergency Department Visits, Emergency Department Visits per 1,000, and Number of Emergency Departments, 1991–2009. 2009 [Google Scholar]
- 5.Hsia RY, Kellermann AL, Shen YC. Factors associated with closures of emergency departments in the United States. Jama. 2011;305:1978–85. doi: 10.1001/jama.2011.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dauner CD. Emergency capacity in California: a look at more recent trends. Health Aff (Millwood) 2004:W4–152-4. doi: 10.1377/hlthaff.w4.152. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 7.Fields WW. Emergency care in California: robust capacity or busted access? Health Aff (Millwood) 2004:W4–143-5. doi: 10.1377/hlthaff.w4.143. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 8.Scheck A. Is There Really a Crisis in California? EDs Close, Beds Increase, and the Problems Remain. Emergency Medicine News. 2003:10. [Google Scholar]
- 9.Schute N MM. Code Blue Crisis in the ER - Turning away patien surefire recipe for disaster. U.S. News & World Report. 2001 9/10/20. [PubMed] [Google Scholar]
- 10.Kellermann AL. Emergency care in California: no emergency? Health Aff (Millwood) 2004:W4–149-51. doi: 10.1377/hlthaff.w4.149. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 11.Melnick GA, Nawathe AC, Bamezai A, et al. Hospital emergency departments: the authors respond. Health Aff (Millwood) 2004:W4–155-6. doi: 10.1377/hlthaff.w4.155. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 12.Siegel B. The emergency department: rethinking the safety net for the safety net. Health Aff (Millwood) 2004:W4–146-8. doi: 10.1377/hlthaff.w4.146. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 13.Melnick GA, Nawathe AC, Bamezai A, et al. Emergency department capacity and access in California, 1990-2001: an economic analysis. Health Aff (Millwood) 2004:W4–136-42. doi: 10.1377/hlthaff.w4.136. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 14.Lambe S, Washington DL, Fink A, et al. Trends in the use and capacity of California's emergency departments, 1990-1999. Ann Emerg Med. 2002;39:389–96. doi: 10.1067/mem.2002.122433. [DOI] [PubMed] [Google Scholar]
- 15.McConville SLH. Emergency Department Care in California: Who Uses It and Why? Public Policy Institute of California; 2008. [Google Scholar]
- 16.CHCF . Is California's Hospital-Based ED System Eroding? California Healthcare Foundation; USC Center for Health Financing, Policy, and Management; 2009. [Google Scholar]
- 17.Lin RG PS, Welsh B, Yoshino K. California's dwindling emergency rooms. Los Angeles Times; [Google Scholar]
- 18. [October 31, 2010];Health Policy. 2010 at http://www.pollingreport.com/health.htm.)
- 19.Shen YC. Do HMO and its for-profit expansion jeopardize the survival of hospital safety net services? Health Econ. 2009;18:305–20. doi: 10.1002/hec.1366. [DOI] [PubMed] [Google Scholar]
- 20.Shen YC, Hsia RY, Kuzma K. Understanding the risk factors of trauma center closures: do financial pressure and community characteristics matter? Med Care. 2009;47:968–78. doi: 10.1097/MLR.0b013e31819c9415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shen YC, Hsia RY. Changes in emergency department access between 2001 and 2005 among general and vulnerable populations. Am J Public Health. 100:1462–9. doi: 10.2105/AJPH.2009.175828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rice H. UTMB criticized for turning away charity cases. Houston Chronicle. 2010 8/25/2010. [Google Scholar]
- 23.Hsia RY, Asch SM, Weiss RE, et al. Community and Hospital Determinants of ED Left Before Being Seen Rates’. Acad Emerg Med. 2010;17:S95–6. [Google Scholar]
- 24.Weber EJ, Showstack JA, Hunt KA, et al. Does lack of a usual source of care or health insurance increase the likelihood of an emergency department visit? Results of a national population-based study. Ann Emerg Med. 2005;45:4–12. doi: 10.1016/j.annemergmed.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 25.Xu KT, Nelson BK, Berk S. The changing profile of patients who used emergency department services in the United States: 1996 to 2005. Ann Emerg Med. 2009;5480:8–95. e1–7. doi: 10.1016/j.annemergmed.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 26.Zwanziger J, Khan N. Safety-net hospitals. Med Care Res Rev. 2008;65:47. doi: 10.1177/1077558708315440. [DOI] [PubMed] [Google Scholar]
- 27. [October 31, 2010];Emergency Medical Services Authority. at http://www.emsa.ca.gov/systems/trauma/default.asp.)
- 28.Horwitz JR. Making profits and providing care: comparing nonprofit, for-profit, and government hospitals. Health Aff (Millwood) 2005;24:790–801. doi: 10.1377/hlthaff.24.3.790. [DOI] [PubMed] [Google Scholar]
- 29.Horwitz JR, Nichols A. Hospital ownership and medical services: market mix, spillover effects, and nonprofit objectives. J Health Econ. 2009;28:924–37. doi: 10.1016/j.jhealeco.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 30.O'Toole TP, Gibbon JL, Seltzer D, et al. Urban homelessness and poverty during economic prosperity and welfare reform: changes in self-reported comorbidities, insurance, and sources for usual care, 1995-1997. J Urban Health. 2002;79:200–10. doi: 10.1093/jurban/79.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lucas JW, Barr-Anderson DJ, Kington RS. Health status of non-Hispanic U.S.-born and foreign-born black and white persons: United States, 1992-95. Vital Health Stat 10. 2005:1–20. [PubMed] [Google Scholar]
- 32.Singh GK, Hiatt RA. Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreignborn populations in the United States, 1979-2003. Int J Epidemiol. 2006;35:903–19. doi: 10.1093/ije/dyl089. [DOI] [PubMed] [Google Scholar]
- 33.Thamer M, Richard C, Casebeer AW, et al. Health insurance coverage among foreignborn US residents: the impact of race, ethnicity, and length of residence. Am J Public Health. 1997;87:96–102. doi: 10.2105/ajph.87.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ravikumar D, Hsia R. Do California counties with lower socioeconomic levels have less access to emergency department care? Acad Emerg Med. 17:508–13. doi: 10.1111/j.1553-2712.2010.00734.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Graddy EA, Ye K. When do we “just say no”? Policy termination decisions in local hospital services. The Policy Studies Journal. 2008;36:219–42. [Google Scholar]
- 36.Harrison MG, Montalvo CC. The financial health of California hospitals: a looming crisis. Health Aff (Millwood) 2002;21:118–26. doi: 10.1377/hlthaff.21.1.118. [DOI] [PubMed] [Google Scholar]
- 37.Ihaka R, Gentleman R. R: A Language for Data Analysis and Graphics. Journal of Computational and Graphical Statistics. 1996;5:299–314. [Google Scholar]
- 38.Niska R BF, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 Emergency Department Summary. National Health Statistics Reports. 2010 [PubMed] [Google Scholar]
- 39.Fact Sheet. Agency for Healthcare Research and Quality; Rockville, MD: Feb, 2000. Addressing Racial and Ethnic Disparities in Health Care. AHRQ Publication No. 00-PO41. http://www.ahrq.gov/research/disparit.htm. [Google Scholar]
- 40.Bach PB, Pham HH, Schrag D, et al. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575–84. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 41.Capps C, Dranove D, Lindrooth RC. Hospital closure and economic efficiency. J Health Econ. 29:87–109. doi: 10.1016/j.jhealeco.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 42.Ciliberto F, Lindrooth RC. Exit from the Hospital Industry. Economic Inquiry. 2007;45:71–81. [Google Scholar]
- 43.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA : the journal of the American Medical Association. 2011;305:675–81. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cakir B. Race, site of care, and hospital readmission rates. JAMA : the journal of the American Medical Association. 2011;305:1965–6. doi: 10.1001/jama.2011.640. author reply 6. [DOI] [PubMed] [Google Scholar]
- 45.US Census Bureau . State and County Quick Facts. California: [July 14th, 2011]. at http://quickfacts.census.gov/qfd/states/06000.html.) [Google Scholar]
- 46.Lee SL, Yaghoubian A, Stark R, et al. Equal Access to Healthcare Does Not Eliminate Disparities in the Management of Adults with Appendicitis. The Journal of surgical research. 2011 doi: 10.1016/j.jss.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 47.US Census Bureau . State & County QuickFacts. Los Angeles: [July 14th, 2011]. at http://quickfacts.census.gov/qfd/states/06/0644000.html.) [Google Scholar]
- 48.Evans M. LA County raises property tax rate to help pay for ER, trauma care. Press- Telegram; 2010. 8/24/10. [Google Scholar]
- 49.McGreevy P. Legislature OKs bill to assist new South Los Angeles area hospital. Los Angeles Times; 2010. 8/25/10. [Google Scholar]
- 50.Committee on the Future of Emergency Care in the United States Health System . Hospital-Based Emergency Care: At the Breaking Point. Institute of Medicine, The National Academies Press; Washington, D.C.: 2007. [Google Scholar]
- 51.CHCF. Overuse of Emergency Departments Among Insured Californias. California Healthcare Foundation; Oakland: 2006. [Google Scholar]
- 52.Katz MH. Future of the safety net under health reform. Jama. 304:679–80. doi: 10.1001/jama.2010.1126. [DOI] [PubMed] [Google Scholar]
- 53.O'Malley AS, Gerland AM, Pham HH, et al. Rising pressure: hospital emergency departments as barometers of the health care system. Issue Brief Cent Stud Health Syst Change. 2005:1–4. [PubMed] [Google Scholar]
- 54.IOM report: the future of emergency care in the United States health system. Acad Emerg Med. 2006;13:1081–5. doi: 10.1197/j.aem.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 55.Cone DC, Richardson LD, Todd KH, et al. Health care disparities in emergency medicine. Acad Emerg Med. 2003;10:1176–83. doi: 10.1111/j.1553-2712.2003.tb00600.x. [DOI] [PubMed] [Google Scholar]
- 56.IOM. Unequal treatment: confronting racial and ethnic disparities in health care. Institute of Medicine, National Academies Press; Washington, D.C.: 2003. [PubMed] [Google Scholar]
- 57.Ludwick A, Fu R, Warden C, et al. Distances to emergency department and to primary care provider's office affect emergency department use in children. Acad Emerg Med. 2009;16:411–7. doi: 10.1111/j.1553-2712.2009.00395.x. [DOI] [PubMed] [Google Scholar]
- 58.Lee JE, Sung JH, Ward WB, et al. Utilization of the emergency room: impact of geographic distance. Geospat Health. 2007;1:243–53. doi: 10.4081/gh.2007.272. [DOI] [PubMed] [Google Scholar]
- 59.Malone RE, Dohan D. Emergency department closures: policy issues. J Emerg Nurs. 2000;26:380–3. doi: 10.1067/men.2000.108629. [DOI] [PubMed] [Google Scholar]
- 60.Buchmueller TC, Jacobson M, Wold C. How far to the hospital? The effect of hospital closures on access to care. J Health Econ. 2006;25:740–61. doi: 10.1016/j.jhealeco.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 61.Sun BC, Mohanty SA, Weiss R, et al. Effects of hospital closures and hospital characteristics on emergency department ambulance diversion, Los Angeles County, 1998 to 2004. Ann Emerg Med. 2006;47:309–16. doi: 10.1016/j.annemergmed.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 62.Ludwick A, Fu R, Warden C, et al. Distances to emergency department and to primary care provider's office affect emergency department use in children. Academic mergency medicine : official journal of the Society for Academic Emergency Medicine 009. 16:411–7. doi: 10.1111/j.1553-2712.2009.00395.x. [DOI] [PubMed] [Google Scholar]